Abstract
Objective To assess the cost effectiveness of adding spinal manipulation, exercise classes, or manipulation followed by exercise (“combined treatment”) to “best care” in general practice for patients consulting with low back pain.
Design Stochastic cost utility analysis alongside pragmatic randomised trial with factorial design.
Setting 181 general practices and 63 community settings for physical treatments around 14 centres across the United Kingdom.
Participants 1287 (96%) of 1334 trial participants.
Main outcome measures Healthcare costs, quality adjusted life years (QALYs), and cost per QALY over 12 months.
Results Over one year, mean treatment costs relative to “best care” were £195 ($360; €279; 95% credibility interval £85 to £308) for manipulation, £140 (£3 to £278) for exercise, and £125 (£21 to £228) for combined treatment. All three active treatments increased participants' average QALYs compared with best care alone. Each extra QALY that combined treatment yielded relative to best care cost £3800; in economic terms it had an “incremental cost effectiveness ratio” of £3800. Manipulation alone had a ratio of £8700 relative to combined treatment. If the NHS was prepared to pay at least £10 000 for each extra QALY (lower than previous recommendations in the United Kingdom), manipulation alone would probably be the best strategy. If manipulation was not available, exercise would have an incremental cost effectiveness ratio of £8300 relative to best care.
Conclusions Spinal manipulation is a cost effective addition to “best care” for back pain in general practice. Manipulation alone probably gives better value for money than manipulation followed by exercise.
Introduction
Back pain is a major economic problem. Before the accompanying clinical paper,1 little evidence existed for the effectiveness of two commonly used treatments—exercise classes and spinal manipulation. Until the UK BEAM trial, little evidence existed for the cost effectiveness of those treatments.2,3
An economic evaluation in British primary care found that physiotherapy led exercise classes were less expensive and more effective than general practice care alone.4 In contrast, a Finnish study found that patients randomised to exercise, different from that investigated by the British study, had higher costs and poorer outcomes than those randomised to the control group and encouraged to keep active.5 A Swedish study found no differences in costs or outcomes between physiotherapy and chiropractic manipulation.6 In contrast, a UK trial comparing private chiropractic and NHS outpatient treatment found that reductions in time off work more than offset the net health service cost incurred by chiropractic.7 To reduce the uncertainty surrounding the cost effectiveness of these physical treatments for back pain, we report the economic evaluation of the UK BEAM trial.
Methods
Interventions
“Best care” in general practice (the “comparator” treatment)—We trained practice teams in “active management” and provided The Back Book for patients.8,9
Exercise programme—This comprised an initial assessment and up to nine classes in community settings over 12 weeks.10
Spinal manipulation package—The UK chiropractic, osteopathic, and physiotherapy professions agreed to use a package of techniques developed by a multidisciplinary group, during eight sessions over 12 weeks.11
Combined treatment—Participants received six weeks of manipulation followed by six weeks of exercise. Treatments were otherwise those given to the manipulation only or exercise only groups.
Study design
We randomised participants between these four interventions. We also randomised participants receiving manipulation between private and NHS premises. Thus the study had a three by two factorial design. As the accompanying clinical paper did not find statistically significant differences in outcome between manipulation in NHS and private premises, this paper analyses the simpler two by two factorial trial.
Data collection
Participants completed questionnaires, including the EQ-5D health status instrument,12,13 at baseline, three months, and 12 months. Over the same period they recorded use of health care—including hospital stays, visits to secondary and primary care, and physical therapists, both private and within the NHS—whether related to back pain or not. Physical therapists completed record forms, including the number of treatments they delivered.
Unit costs
To contribute to health policy for an expensive condition, we conducted an economic analysis from the perspective of health care. Participants' follow up periods lay between August 1999 and April 2002. We therefore used unit costs in pounds sterling at 2000-1 prices to value the resources they used (table 1). We did not adjust or discount the costs, as we focused on effects over only one year. We costed NHS care from national averages for England.14,15 We costed private care by using information from a major insurance provider.16 As the accompanying paper found no difference in clinical outcome between manipulation in private and NHS premises,1 our main economic analysis used costs for the less expensive NHS premises. Nevertheless, we explored this assumption in a sensitivity analysis.
Table 1.
Reported cost of units of healthcare resource
| Healthcare resource | Unit | Cost per unit (c=p) |
|---|---|---|
| Spinal manipulation package15: |
||
| Initial consultation (40 minutes) |
Session |
24.33 |
| Treatment session (20 minutes) |
Session |
12.17 |
| Exercise programme: |
||
| Initial assessment (40 minutes)15 |
Session |
25.34 |
| Class (assuming mean of 10 participants per class)6 |
Session |
4.35 |
| Hospital inpatient stay: |
||
| NHS routine admission14,15 |
Day |
181.00 |
| NHS emergency admission14,15 |
Admission |
282.00 |
| Private hospital admission16 |
Day |
395.00 |
| Outpatient attendance: |
||
| NHS specialist15 |
Visit |
68.00 |
| Private specialist16 |
Visit |
120.00 |
| NHS physiotherapist15 |
Visit |
24.54 |
| Private physiotherapist16 |
Visit |
76.00 |
| Other NHS15 |
Visit |
24.54 |
| Other private16 |
Visit |
76.00 |
| General practice consultation: |
||
| General practitioner15 |
Visit |
21.50 |
| Practice nurse15 |
Visit |
8.50 |
| Physiotherapist15 |
Visit |
15.00 |
| Other healthcare professional15 | Visit | 15.00 |
Health outcomes
The EQ-5D measures health on five three point scales—mobility, self care, usual activities, pain-discomfort, and anxiety-depression—thus putting participants into one of 243 (= 35) health states.12 A large British sample valued these states on a “utility” scale on which being dead scores zero and perfect health scores one.13 We estimated how many quality adjusted life years (QALYs) participants had experienced over their year in the UK BEAM trial by calculating “areas under (health utility) curves.”17 For example, if they reported that their utility averaged 0.5, we calculated that they had experienced half a QALY over the year in UK BEAM. To avoid bias we adjusted for differences in baseline EQ-5D scores.18
Cost utility analysis
Because the accompanying clinical paper found statistically significant interactions between manipulation and exercise,1 it compares four distinct treatments within the factorial design.19 Although costs show no interaction between treatments, this paper also compares these four treatments for three reasons. Firstly, as costs vary much more than clinical outcomes, this is prudent. Secondly, those people responsible for allocating resources need to choose between these four treatments. Finally, this epitomises the Bayesian statistical approach adopted in this paper.
So we estimated the mean costs of, and mean QALYs gained by, each of four distinct treatments. As most trials compare just two treatments, we adopted a more general approach. Firstly, we ranked treatments by mean cost, starting from the least costly. Secondly, we calculated incremental cost effectiveness ratios for all treatments by dividing incremental costs by incremental QALYs. Finally, we excluded from the comparison “dominated” treatments and treatments subject to “extended dominance,”20 and we recalculated ratios if necessary. A treatment is dominated if it generates worse health outcomes and costs more than an alternative treatment. Extended dominance occurs when a treatment is less effective and has a higher incremental cost effectiveness ratio than an alternative treatment.20
Trial participants registered with the same general practice formed clusters within centres, and centres formed clusters within the trial. In these circumstances, the use of standard cost utility methods may yield misleading results.21 Hence we used Bayesian Markov Chain Monte Carlo methods within the statistical package MLwiN to undertake bivariate multilevel analysis.22 Because evidence about the cost effectiveness of physical treatments for back pain is weak, we started by giving each of the four treatments “uninformative” prior probabilities. In other words, we made no assumptions about the probabilities before UK BEAM that one treatment was more effective or cost more than another.
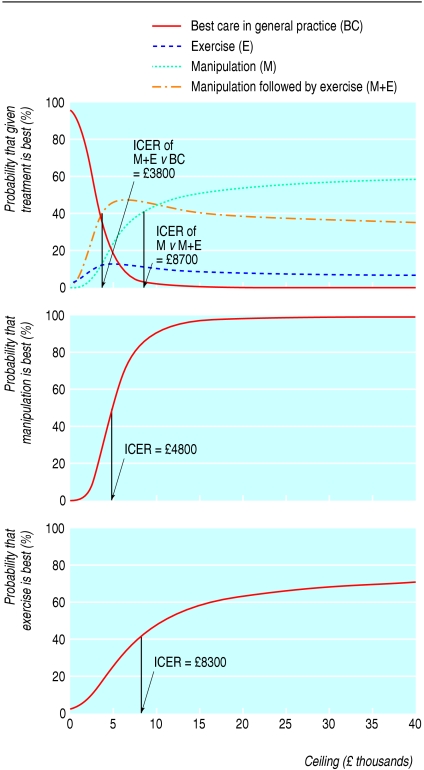
To report the uncertainty due to sampling variation, we calculated Bayesian credibility intervals (Bayesian analogue of 95% confidence intervals) and plotted cost effectiveness acceptability curves.23,24 As UK BEAM compared four rather than two treatments, we plotted multi-treatment cost effectiveness acceptability curves. These curves show the posterior (after UK BEAM) probability that each strategy is better than the other three across the range of values that decision makers may pay to achieve an additional QALY. This assumes that these people have maximum values that they are willing to pay for an additional QALY. It is this “ceiling” against which they should compare estimated incremental cost effectiveness ratios and read the probability that the corresponding treatment is “best.” This decision oriented formulation selects as “best” or “cost effective” that treatment, with an incremental cost effectiveness ratio below the ceiling, likely to be more effective than competing treatments. This is not necessarily the strategy with the lowest ratio, as that may generate fewer QALYs.23 To cover scenarios in which either exercise or manipulation is not available, we also plotted two-treatment cost effectiveness acceptability curves to compare best care with manipulation alone or exercise alone.
Finally, we did three sensitivity analyses to explore how dependent the results were on participants' estimates of total costs and our estimates of unit costs. The first analysis examined the influence of cost “outliers,” very large healthcare costs reported by a few participants. We excluded those participants whose costs exceeded £2000 ($3700; €2900) (more than eight times the median cost) in case their chance allocation between groups had distorted the results.
The other two sensitivity analyses assessed the influence of the unit costs of manipulation. One did so by costing the scenario in which the NHS buys all manipulation from the private sector using private manipulation costs. The other did so by costing the scenario in which the NHS buys half its manipulation from the private sector, using private costs when trial manipulation took place in private premises and NHS costs when in NHS premises.
Results
Recruitment
We recruited 1334 participants from 181 practices around 14 centres across the United Kingdom. Of these, 1287 (96.5%) yielded enough data for inclusion in the economic analysis; 326 received best care in general practice, 297 received best care plus exercise, 342 received best care plus manipulation, and 322 received best care plus combined treatment.
Clinical outcomes
The accompanying clinical paper reports that exercise achieved a small functional benefit at three months but not at one year; manipulation achieved a small to moderate benefit at three months and a small benefit at one year; and combined treatment achieved a moderate benefit at three months and a small benefit at one year (all statistically significant).1 These benefits were specific to back pain, in contrast to the general health benefits determined in this paper.
Costs
Combined treatment had the highest therapy costs but the lowest subsequent hospital costs (table 2). So it cost only £125 (95% credibility interval £21 to £228) more than best care, whereas exercise cost £140 (£3 to £278) more than best care, and manipulation cost £195 (£85 to £308) more.
Table 2.
Reported mean (SD) cost (£) of health care over 12 months by treatment group
| Healthcare resource | Best care in general practice (n=326) | Best care plus exercise alone (n=297) | Best care plus manipulation alone (n=342) | Best care plus manipulation and exercise (n=322) |
|---|---|---|---|---|
| Spinal manipulation within UK BEAM |
0 |
0 |
147 (53) |
115 (53) |
| Exercise class within UK BEAM |
0 |
41 (22) |
0 |
37 (22) |
| Hospital inpatient stay: |
||||
| NHS routine admission |
28 (148) |
31 (197) |
17 (91) |
19 (114) |
| NHS emergency admission |
11 (86) |
17 (112) |
20 (128) |
14 (106) |
| Private hospital admission |
6 (66) |
5 (85) |
5 (71) |
7 (86) |
| Outpatient attendance: |
||||
| NHS specialist |
63 (186) |
63 (234) |
51 (150) |
34 (121) |
| Private specialist |
14 (85) |
42 (470) |
16 (110) |
13 (110) |
| NHS physiotherapist |
22 (103) |
27 (195) |
27 (165) |
11 (60) |
| Private physical therapist* |
56 (280) |
44 (335) |
103 (428) |
49 (216) |
| Other NHS |
20 (146) |
11 (62) |
14 (90) |
12 (69) |
| Other private |
23 (145) |
28 (195) |
23 (196) |
13 (79) |
| General practice consultation: |
||||
| General practitioner |
88 (139) |
63 (129) |
94 (146) |
73 (118) |
| Practice nurse |
4 (18) |
7 (48) |
9 (44) |
5 (33) |
| Physiotherapist |
1 (4) |
102 (125) |
4 (28) |
57 (63) |
| Other |
11 (55) |
5 (30) |
11 (51) |
10 (44) |
| Total cost | 346 (602) | 486 (907) | 541 (768) | 471 (490) |
Including spinal manipulation or exercise class outside UK BEAM.
Health outcomes
Physical interventions improved EQ-5D scores more than did best care (table 3). Relative to best care, manipulation generated a mean of 0.041 (95% credibility interval 0.016 to 0.066) QALYs per participant, combined treatment generated 0.033 (-0.001 to 0.067), and exercise generated 0.017 (-0.017 to 0.051).
Table 3.
Utilities and QALYs over 12 months by treatment group
| Best care in general practice (n=326) | Best care plus exercise alone (n=297) | Best care plus manipulation alone (n=342) | Best care plus manipulation and exercise (n=322) | |
|---|---|---|---|---|
| Mean (SD) utility from EQ-5D* at: |
||||
| Baseline |
0.597 (0.233) |
0.556 (0.270) |
0.592 (0.247) |
0.596 (0.241) |
| Three months |
0.626 (0.249) |
0.620 (0.262) |
0.675 (0.261) |
0.660 (0.241) |
| One year |
0.629 (0.263) |
0.618 (0.267) |
0.664 (0.277) |
0.679 (0.268) |
| Mean (SD) QALYs over 12 months* |
0.618 (0.232) |
0.635 (0.245) |
0.659 (0.241) |
0.651 (0.237) |
| Difference (95% credibility interval) in mean QALYs relative to best care in general practice* | Not applicable | 0.017 (−0.017 to 0.051) | 0.041 (0.016 to 0.066) | 0.033 (−0.001 to 0.067) |
QALY=quality adjusted life year.
Estimated by analysis of covariance with adjustment for baseline EQ-5D score and then rounded to three significant figures.
Cost utility analysis
When manipulation and exercise are both available, combined treatment generates 0.033 more QALYs than does best care at an additional cost of £125, yielding an incremental cost effectiveness ratio of £3800 (table 4). This achievement dominates that of exercise alone, which costs more and achieves less over 12 months. Manipulation alone, however, can generate 0.008 more QALYs than combined treatment for an extra £70, yielding a ratio of £8700 relative to combined treatment. If exercise is not available, however, manipulation generates 0.041 more QALYs than best care, yielding an incremental cost effectiveness ratio of £4800. If manipulation is not available, exercise generates 0.017 more QALYs than best care, yielding a ratio of £8300.
Table 4.
Cost utility analysis by scenario and treatment group*
| Treatment group | Mean cost*(£) | Mean adjusted QALYs*† | Incremental cost effectiveness ratio to nearest £100 or comment |
|---|---|---|---|
|
Manipulation and exercise both available (n=1287) |
|||
| Best care in general practice |
346 |
0.618 |
|
| Best care plus exercise |
486 |
0.635 |
Dominated by combined treatment, which costs less and gains more QALYs |
| Best care plus manipulation and exercise |
471 |
0.651 |
£3800 |
| Best care plus manipulation |
541 |
0.659 |
£8700 relative to manipulation and exercise |
|
Exercise not available (n=623) |
|||
| Best care in general practice |
346 |
0.622 |
|
| Best care plus manipulation |
541 |
0.663 |
£4800 relative to best care |
|
Manipulation not available (n=668) |
|||
| Best care in general practice |
346 |
0.610 |
|
| Best care plus exercise | 486 | 0.627 | £8300 relative to best care |
QALY=quality adjusted life year.
Markov Chain Monte Carlo estimates from bivariate multilevel model.
Estimated by analysis of covariance with adjustment for baseline EQ-5D score and then rounded to three significant figures.
The cost effectiveness acceptability curves in the top panel of the figure show the probability that each of the four treatments is better than the other three when all are available. If the ceiling was only £2000 per QALY, the top panel shows 74% probability that best care would be the best strategy. If the ceiling was £5000 per QALY, combined treatment has a lower incremental cost effectiveness ratio than this; the top panel of the figure shows a 46% chance that it would be best. If the ceiling was £15 000 per QALY (lower than implied by previous recommendations by the National Institute for Clinical Excellence25), manipulation alone has a lower incremental cost effectiveness ratio than this; the top panel shows a 50% probability that it would be best. The cost effectiveness acceptability curve in the middle panel of the figure shows the probability that manipulation is better than best care when exercise is not available; and vice versa for the curve in the bottom panel.
Figure 1.
Cost effectiveness acceptability curves. Top: manipulation and exercise available; middle: exercise not available; bottom: manipulation not available. ICER=incremental cost effectiveness ratio
Sensitivity analyses
To assess the robustness of these results to the presence of “outliers,” we excluded the 51 participants (9, 16, 16, and 10 from best care, exercise alone, manipulation alone, and combined treatment respectively) whose healthcare costs exceeded £2000. Manipulation achieves extended dominance over both exercise and combined treatment (table 5). It is thus the only alternative to best care, with an incremental cost effectiveness ratio of £3000 per additional QALY. At a ceiling of £10 000 per QALY, manipulation has a 73% chance of being best. If manipulation alone were not available, exercise would have a ratio of £4100.
Table 5.
Sensitivity analyses by treatment group*
| Treatment group | Mean cost*(£) | Mean adjusted QALYs*† | Incremental cost effectiveness ratio to nearest £100 or comment |
|---|---|---|---|
|
Excluding participants with health care costing more than £2000 over 12 months (n=1266) |
|||
| Best care in general practice |
277 |
0.621 |
|
| Best care plus exercise |
322 |
0.632 |
Subject to extended dominance by manipulation |
| Best care plus manipulation and exercise |
403 |
0.647 |
Subject to extended dominance by manipulation |
| Best care plus manipulation |
411 |
0.665 |
£3000 relative to best care |
|
NHS provides manipulation for only 50% of patients (n=1287) |
|||
| Best care in general practice |
346 |
0.616 |
|
| Best care plus exercise |
486 |
0.628 |
Subject to extended dominance by manipulation and exercise |
| Best care plus manipulation and exercise |
537 |
0.645 |
£6600 relative to best care |
| Best care plus manipulation |
624 |
0.655 |
£8700 relative to manipulation and exercise |
|
Manipulation provided only in private premises (n=1287) |
|||
| Best care in general practice |
346 |
0.616 |
|
| Best care plus exercise |
486 |
0.628 |
Subject to extended dominance by manipulation and exercise |
| Best care plus manipulation and exercise |
595 |
0.645 |
£8600 relative to best care |
| Best care plus manipulation | 701 | 0.655 | £10 600 relative to manipulation and exercise |
QALY=quality adjusted life year.
Markov Chain Monte Carlo estimates from bivariate hierarchical multilevel model.
Estimated by analysis of covariance with adjustment for baseline EQ-5D score and then rounded to three significant figures.
The second sensitivity analysis used private costs for manipulation that took place in private premises. Combined treatment now achieves extended dominance over exercise, with an incremental cost effectiveness ratio of £6600 compared with best care (table 5). Manipulation alone then has a ratio of £8700 relative to combined treatment
The third sensitivity analysis used private unit costs for all manipulation within the trial. The findings are analogous to those in the second scenario. Exercise is subject to extended dominance, and combined treatment has an incremental cost effectiveness ratio of £8600 compared with best care (table 5). Manipulation alone then has a ratio of £10 600 relative to combined treatment.
Discussion
Principal findings
This economic evaluation supports and extends the findings of the clinical evaluation of the UK BEAM trial reported in the accompanying paper.1 If decision makers value additional quality adjusted life years (QALYs) at much less than £3800, “best care” in general practice is probably the best strategy. If their valuation lies between £3800 and £8700, spinal manipulation followed by exercise classes (“combined treatment”) is likely to be the best treatment. If their valuation is well above £8700, manipulation alone is probably the best treatment.
Strengths and weaknesses of the study
Although two of our three sensitivity analyses—those that used larger unit costs in whole or in part—changed these critical thresholds a little, they did not alter the essentials of these conclusions. The other sensitivity analysis, which removed 51 “outliers” from the UK BEAM dataset, was more favourable to manipulation than was the primary analysis. Under this scenario manipulation cost only £3000 per QALY relative to best care in general practice.
We believe that this is the first study of physical therapy for low back pain to show convincingly that both manipulation alone and manipulation followed by exercise provide cost effective additions to care in general practice. Indeed, as we trained practice teams in the best care of back pain, we may have underestimated the benefit of physical therapy when compared with “usual care” in general practice. The detailed clinical outcomes reported in the accompanying paper reinforce these findings by showing that the improvements in health status reported here reflect statistically significant improvements in function, pain, disability, physical and mental aspects of quality of life, and beliefs about back pain.1
Unanswered questions
Funding constraints prevented us from following up participants for more than 12 months. Given that they continued to show benefits of treatment at 12 months, the cost effectiveness of both manipulation and combined treatment may be better than we have reported.
Commissioning decisions should depend on local circumstances, notably the availability of spinal manipulation and exercise physiotherapists. Although combined therapy is an attractive option, this depends on an ample supply of both trained manipulators prepared to work for the NHS and exercise physiotherapists with access to suitable premises. As back pain is a common problem, making manipulation generally available will require many therapists. In the United Kingdom there are 2100 registered chiropractors, 3200 registered osteopaths, and about 5000 manipulative physiotherapists (Ann Thomson, Chair of British Association of Chartered Physiotherapists in Manipulation, on behalf of the Chartered Society of Physiotherapy, personal communication, 2003). According to the unit costs we used in our analysis, they can achieve higher incomes in private practice than in the NHS. In the short term it may be difficult to make manipulative or combined treatment generally available within the NHS.
Whereas physiotherapists can rapidly train to deliver the exercise package, insufficient trained manipulators are available in the United Kingdom to meet potential demand, and it will take several years to produce additional manipulators. Indeed, if this needs new training programmes, it may be decades before the NHS can implement these findings. Fortunately, using private costs for manipulation had little effect on the choice of best treatment. Purchasing manipulation from the private sector to provide treatment within the NHS would still represent good value for money if decision makers were willing to pay £10 000 per additional QALY.
What is already known on this topic
Back pain is a major economic problem
Little evidence exists for the effectiveness and cost effectiveness of two commonly used treatments—exercise classes and spinal manipulation
What this study adds
Spinal manipulation, exercise classes, and manipulation followed by exercise all increased participants' quality of life over 12 months by more than did “best care” in general practice
Adding spinal manipulation to best care in general practice is effective and cost effective for patients in the United Kingdom
If the NHS can afford at least £10 000 for each quality adjusted life year yielded by physical treatments, manipulation alone probably gives better value for money than manipulation followed by exercise
Meaning of the study
Adding spinal manipulation to best care in general practice is effective and cost effective for patients with back pain in the United Kingdom. If the NHS can afford more than £10 000 for an extra QALY, manipulation alone probably gives better value for money than manipulation followed by exercise. These conclusions hold even if the NHS has to buy spinal manipulation from the private sector.
Full authorship details are given in the accompanying paper (doi: 10.1136/bmj.38282.669225.AE).
We thank all participants—patients, primary care staff, and collaborators listed in the accompanying clinical paper—for their contributions. We thank Mark Sculpher and Daphne Russell for advice on analysis. Members of the UK BEAM Trial Team: Ian Russell, Martin Underwood, Stephen Brealey, Kim Burton, Simon Coulton, Amanda Farrin, Andrew Garratt, Emma Harvey, Louise Letley, Andrea Manca, Jeannett Martin, Jennifer Klaber Moffett, Veronica Morton, David Torgerson, Madge Vickers, Ken Whyte, Melanie Williams.
Contributors: See accompanying clinical paper. Funding: Medical Research Council (research costs); NHS in England, Northern Ireland, Scotland, and Wales (excess treatment and service support costs).
Competing interests: LL, JM, MU, MV, and KW have received salaries from the MRC. MU has received fees for speaking from Menarini Pharmaceuticals, the manufacturers of dexketoprofen and ketoprofen, and Pfizer, the manufacturers of celecoxib and valdecoxib. The other 12 authors have nothing to declare.
Ethical approval: The Northern and Yorkshire multicentre research ethics committee and 41 local research ethics committees approved the trial protocol.
Amendment
This is Version 2 of the paper. In this version, the text relating to the figure has been amended to state that the curve in the middle panel shows the probability that manipulation is better than best care when exercise is not available, and vice versa for the curve in the bottom panel [these were incorrectly given the other way round in the previous version].
References
- 1.UK BEAM Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ 2004;329:doi: 10.1136/bmj.38282.669225.AE. [DOI] [PMC free article] [PubMed]
- 2.Baldwin ML, Côté P, Frank JW, Johnson WG. Cost-effectiveness studies of medical and chiropractic care for occupational low back pain: a critical review of the literature. Spine J 2001;1: 138-47. [DOI] [PubMed] [Google Scholar]
- 3.Maetzel A, Li L. The economic burden of low back pain: a review of studies published between 1996 and 2001. Best Pract Res Clin Rheumatol 2002;16: 23-30. [DOI] [PubMed] [Google Scholar]
- 4.Klaber Moffett J, Torgerson D, Bell-Syer S, Jackson D, Llewlyn-Phillips H, Farrin A, et al. Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. BMJ 1999;319: 279-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malmivaara A, Hakkinen U, Heinrichs M, Koskenniemi L, Kuosma E, Lappi S, et al. The treatment of acute low back pain—bed rest, exercises, or ordinary activity? N Engl J Med 1995;332: 351-5. [DOI] [PubMed] [Google Scholar]
- 6.Skargren EI, Carlsson PG, Oberg BE. One-year follow-up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain. Spine 1998;23: 1875-84. [DOI] [PubMed] [Google Scholar]
- 7.Meade TW, Dyer S, Browne W, Townsend J, Frank AO. Low back pain of mechanical origin: randomised comparison of chiropractic and hospital outpatient treatment. BMJ 1990;300: 1431-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Underwood M, O'Meara S, Harvey E, UK BEAM Trial Team. The acceptability to primary care staff of a multidisciplinary training package on acute back pain guidelines. Fam Pract 2002;19: 511-5. [DOI] [PubMed] [Google Scholar]
- 9.Roland M, Waddell G, Klaber Moffett J, Burton AK, Main CJ, Cantrell T. The back book. Norwich: Stationery Office, 1996.
- 10.Klaber Moffett J, Frost H, UK BEAM Trial Team. Back to fitness programme: the manual for physiotherapists to set up the classes. Physiotherapy 2000;85: 295-305. [Google Scholar]
- 11.Harvey E, Burton AK, Moffett JK, Breen A, UK BEAM Trial Team. Spinal manipulation for low-back pain: a treatment package agreed to by the UK chiropractic, osteopathy and physiotherapy professional associations. Man Ther 2003;8: 46-51. [DOI] [PubMed] [Google Scholar]
- 12.Kind P. The EuroQoL instrument: an index of health-related quality of life. In: Spilker B, ed. Quality of life and pharmacoeconomics in clinical trials. Philadelphia: Lippincott-Raven, 1996.
- 13.Kind P, Hardman G, Macran S. UK population norms for EQ-5D. York: Centre for Health Economics, University of York, 1999. (Discussion paper 172.)
- 14.Chartered Institute of Public Finance and Accountancy. The health service database 2002. Croydon: CIPFA, 2002.
- 15.Netten A, Dennett J, Knight J. Unit costs of health and social care. Canterbury: Personal Social Services Research Unit, University of Kent, 2002.
- 16.BUPA Hospitals UK. How much will it cost? www.bupahospitals.co.uk/asp/paying/priceguides.asp (accessed 17 Nov 2004).
- 17.Matthews JNS, Altman DG, Campbell MJ, Royston P. Analysis of serial measurements in medical research. BMJ 1990;300: 230-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2004. Oct 20 [Epublication ahead of print]. [DOI] [PubMed]
- 19.McAlister FA, Straus SE, Sackett DL, Altman DG. Analysis and reporting of factorial trials: a systematic review. JAMA 2003;289: 2545-53. [DOI] [PubMed] [Google Scholar]
- 20.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. New York: Oxford University Press, 1996.
- 21.Manca A, Rice N, Sculpher MJ, Briggs AH. Assessing generalisability by location in trial-based cost-effectiveness analysis: the use of multilevel models. Health Econ 2004. Jun 14 [Epublication ahead of print]. [DOI] [PubMed]
- 22.Rasbash J, Browne W, Goldstein H. A user's guide to MLwiN Version 2.1. London: Institute of Education, University of London, 2000.
- 23.Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10: 779-87. [DOI] [PubMed] [Google Scholar]
- 24.Fenwick E, O'Brien BJ, Briggs AH. Cost-effectiveness acceptability curves—facts, fallacies and frequently asked questions. Health Econ 2004;13: 405-15. [DOI] [PubMed] [Google Scholar]
- 25.Raftery J. NICE: faster access to modern treatments? Analysis of guidance on health technologies. BMJ 2001;323: 1300-3. [DOI] [PMC free article] [PubMed] [Google Scholar]