Abstract
Purpose
Prostate cancer growth is dependent upon androgen receptor (AR) activation, regulated via phosphorylation. Protein kinase C (PKC) is one kinase that can mediate AR phosphorylation. This study aimed to establish if AR phosphorylation by PKC is of prognostic significance.
Methods
Immunohistochemistry for AR, AR phosphorylated at Ser-81 (pARS81), AR phosphorylated at Ser-578 (pARS578), PKC and phosphorylated PKC (pPKC) was performed on 90 hormone-naïve prostate cancer specimens. Protein expression was quantified using the weighted histoscore method and examined with regard to clinico-pathological factors and outcome measures; time to biochemical relapse, survival from biochemical relapse and disease-specific survival.
Results
Nuclear PKC expression strongly correlated with nuclear pARS578 (c.c. 0.469, p=0.001) and cytoplasmic pARS578 (c.c. 0.426 p=0.002). High cytoplasmic and nuclear pARS578 were associated with disease-specific survival (p<0.001 and p=0.036 respectively). High nuclear PKC was associated with lower disease-specific survival when combined with high pARS578 in the cytoplasm (p=0.001) and nucleus (p=0.038). Combined high total pARS81 and total pARS578 was associated with decreased disease-specific survival (p=0.005)
Conclusions
pARS578 expression is associated with poor outcome and is a potential independent prognostic marker in hormone-naïve prostate cancer. Furthermore, PKC driven AR phosphorylation may promote prostate cancer progression and provide a novel therapeutic target.
Keywords: androgen receptor, biomarker, phosphorylation, prostate cancer, protein kinase C
BACKGROUND
Over the last 10 years we have observed increasing incidence and decreasing mortality trends in prostate cancer. Incidence-mortality ratios were approximately 2:1 in Western Europe prior to the introduction of PSA testing. This ratio has now increased to over 7:1, illustrating the level of over-diagnosis [1]. Many patients have indolent tumours that, before PSA testing, would not have been clinically apparent in their lifetime. Such overdiagnosis often results in overtreatment. Treatment of prostate cancer with radiation, surgery or hormone therapy is costly and even surveillance strategies are expensive. The diagnosis, treatment and 5 year follow-up cost of prostate cancer in the UK was estimated at £136, 278, 237 in 2010 [2]. It is estimated that in 2030 prostate cancer will be the most common cancer in men, with rates expected to increase by 69% compared to the number of new cases in 2007 [3]. If the predicted exponential rise in prostate cancer incidence and prevalence materialises, the cost of treatment will be unsustainable to the UK economy. Therefore the main challenge for prostate cancer research and clinical care is the quandary of how to continue driving mortality rates downward while minimising over-treatment.
Although the underlying mechanisms driving prostate carcinogenesis remain elusive, it is widely accepted that prostate cancer cell growth and survival is exquisitely dependent upon activation of the androgen receptor (AR) by androgens. This explains the high response rate of prostate cancer patients to androgen deprivation therapy (ADT). ADT reduces the level of circulating androgens and therefore levels in the prostate cancer cells resulting in AR not being activated, causing cell cycle arrest and apoptosis [4]. Furthermore, the renewed expression of serum PSA levels and AR expression in castrate-resistant disease is evidence that, even in advanced disease, prostate cancer cells remain almost exclusively dependent on the AR [5, 6]. The AR and alterations affecting its functional status are therefore likely to play an important role in the development and progression of prostate cancer.
Post-translational modification of the AR occurs at 23 known sites by phosphorylation, acetylation, SUMOylation, methylation and ubiquitination [7, 8]. Phosphorylation of the AR at serine residues is thought to inhibit proteolytic degradation and stabilize AR homo-dimers, thereby enhancing its activity [9]. AR phosphorylation may also influence transactivation of the AR since AR transcriptional activity correlates strongly with phosphorylation of specific serine residues [9]. Each of the major AR domains contains at least one serine phosphorylation site. The majority of these sites are located in the N-terminal domain (NTD), which is important for AR transactivation [8]. The hinge region contains one serine phosphorylation site, Ser-650, which regulates nuclear localization, DNA binding, and coactivator recruitment [8, 10, 11]. AR Ser-578 is located within the DNA binding domain. Protein kinase C (PKC) is the kinase predicted to be responsible for phosphorylation of AR Ser-578 [12]. Phosphorylation via PKC at this site has been linked to nuclear-cytoplasmic shuttling, DNA binding and the modulation of other functional phosphorylation sites on the AR [13]. Site directed mutagenesis of Ser-578 on the AR in castrate-resistant prostate cancer cell lines demonstrated that PKC-dependent phosphorylation was reduced on average by 50% when compared to wild type cells [13]. In addition ligands such as epidermal growth factor (EGF) have been shown to increase AR transcriptional activity and cell growth via PKC dependent AR phosphorylation at serine site 578 [13]. It is therefore plausible that alterations in AR phosphorylation, in particular at Ser-578 by PKC, may drive prostate carcinogenesis. However, few studies have explored the significance of AR phosphorylation at this site in prostate cancer in the clinical setting.
In the current study we aim to determine whether AR phosphorylation at Ser-578 is associated with clinico-pathological parameters and outcome in a cohort of hormone-naïve prostate cancer patients and if AR phosphorylation at Ser-578 correlates with PKC expression. It is hypothesised that AR phosphorylation at this site may be associated with disease progression and therefore may provide a biomarker to inform treatment decision-making.
RESULTS
Patient characteristics
Analysis was based on 90 hormone-naïve prostate cancer patients. Patient characteristics recorded include age, Gleason score at diagnosis, PSA at diagnosis, presence of tissue lymphovascular invasion and PSA at recurrence (Table 1). Twenty-three patients had metastases to local lymph nodes (3), bone (13) and at both sites (7). Forty-seven patients had biochemical relapse (median time to biochemical relapse 2.7yr, interquartile range 1.5–3.8). Twenty-four patients were alive at time of analysis, median follow-up 11.7yr (interquartile range 9.9–14.0). Forty-six died from prostate cancer (median time to death 4yr, interquartile range 1.9–7.2) and twenty deaths were attributed to inter-current disease (median time to death of 4.1yr, interquartile range 0.9–5.5). Table 2 shows associations with clinico-pathological parameters and clinical outcome measures.
Table 1. Clinico-pathological characteristics of cohort.
| Patients, n (%) | |
|---|---|
| Age (<70/>70) | 34 (37.0)/56 (60.9) |
| Gleason (<7/7/>7) | 24 (26.1)/ 25 (27.2)/ 28 (30.4) |
| PSA at diagnosis (<10/10/>10) | 19 (20.7)/ 14 (15.2)/ 36 (39.1) |
| Lymphovascular invasion (no/yes) | 84 (91.3)/ 6 (6.5) |
| PSA at recurrence (<10/10/>10) | 38 (41.3)/ 1 (1.1)/ 10 (10.9) |
| Ki67 (≤median/>median) | 46 (50)/ 39 (42.4) |
Number of patients with missing data is not displayed. Values that do not give a sum of 100% is due to data being unavailable.
Table 2. Relationship between clinico-pathological parameters and clinical outcome measures.
| Univariate analysis | |||
|---|---|---|---|
| Clinico-pathological characteristic | Time to biochemical relapseP value, Hazard Ratio (95% CI) | Survival from biochemical relapseP value, Hazard Ratio (95% CI) | Disease-specific survivalP value, Hazard Ratio (95% CI) |
| Age (<70/>70) | 0.260, 1.40, (0.8-2.5) | 0.385, 1.44, (0.6-3.3) | 0.020, 2.11, (1.1-4.0) |
| Gleason (<7/7/>7) | 0.004, 1.94, (1.3-2.9) | 0.060, 1.48, (0.8-2.6) | 0.007, 1.91, (1.3-2.9) |
| PSA at diagnosis (<10/10/>10) | 0.002, 1.96, (1.3-2.9) | 0.078, 1.46, (0.8-2.7) | 0.001, 2.04, (1.3-3.3) |
| Lymphovascular invasion (no/yes) | 0.001, 4.6, (1.7-11.6) | 0.612, 1.32, (0.5-3.9) | 0.114, 2.09, (0.8-5.3) |
| PSA at recurrence (<10/10/>10) | <0.001, 5.86, (2.8-12.2) | <0.001, 2.82, (1.9-4.2) | |
| Metastases at any time (no/yes) | 0.001, 3.65, (1.7-8.0) | 0.008, 4.86, (1.4-17.4) | <0.001, 5.0, (2.0-12.4) |
| Ki67 (≤median vs >median) | 0.796, 1.08, (0.6-2.0) | 0.185, 1.68, (0.8-3.6) | 0.006, 2.28, (1.2-4.2) |
The clinical variables were grouped and analysed by Kaplan Meier methods with reference to clinical outcome measures as shown. Patients were considered to have biochemical relapse dependent on treatment; radical prostatectomy serum PSA >0.2ng/ml, radical radiotherapy serum PSA of 2.0ng/ml above the post treatment nadir level, hormone treatment 2-3 consecutive rises in serum PSA levels above the nadir obtained at intervals of >2 weeks [28, 29]. Numbers in bold denote significant associations with p value <0.05.
Protein expression analysis
In addition, any tumour exhibiting negative staining for pARS578 was demonstrated to have positive staining for other AR phosphorylation sites confirming that the negative expression was a true negative and not due to phospho-proteins being degraded in that particular sample. Expression of all proteins was observed at varying levels in the cytoplasm and nucleus of both stromal and epithelial cells (Figure 1). Protein expression was found to be heterogeneous throughout and less intense in the stromal cells. There was presence of prostatic intraepithelial neoplasia (PIN) and benign tissue, adjacent to the neoplastic tissue, in some of the TMA cores. Expression of proteins in the interspersed PIN and benign tissue and the normal prostate control core was heterogeneous and less intense than the neoplastic tissue. Only protein expression observed in the tumour cells was recorded. All intra-class correlation coefficient (ICCC) values were >0.80. Protein expression levels were subdivided into low (≤median) and high expression (>median) for analysis (Table 3).
Figure 1. Immunohistochemical staining of prostate cancer tissue for AR A., pARS578 B. PKC C. and phosphoPKC D.
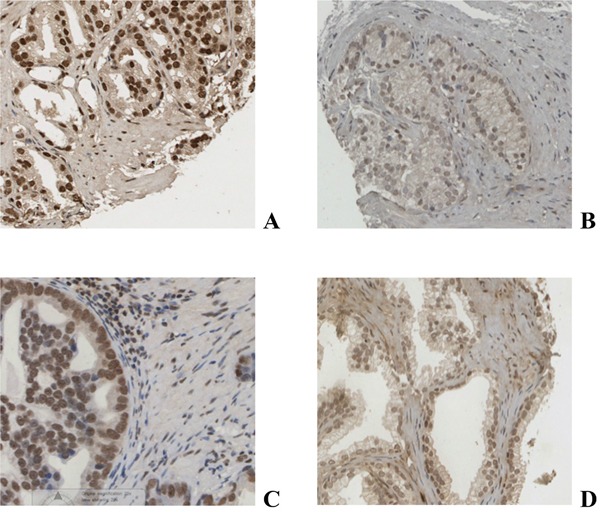
Table 3. Protein expression in patients with tissue available.
| Patients, n (%) | |
|---|---|
| AR Nuclear (low/high) | 44 (47.8)/ 45 (48.9) |
| AR Cytoplasmic (low/high) | 45 (48.9)/ 44 (47.8) |
| pARS578 Nuclear (low/high) | 30 (32.6)/ 30 (32.6) |
| pARS578 Cytoplasmic (low/high) | 32 (34.8)/ 28 (30.4) |
| PKC Nuclear (low/high) | 30 (32.6)/ 28 (30.4) |
| PKC Cytoplasmic (low/high) | 29 (31.5)/ 29 (31.5) |
| pPKC Nuclear (low/high) | 41 (44.6)/ 40 (43.5) |
| pPKC Cytoplasmic (low/high) | 41 (44.6)/ 40 (43.5) |
The proteins of interest were grouped as ≤median or >median. Number of patients with missing data is not displayed. Values that do not give a sum of 100% is due to data being unavailable.
Association between protein expression and clinico-pathologic outcome measures
High expression of cytoplasmic pARS578 protein was associated with increased Gleason score (p=0.008, Table 4). High expression of nuclear pARS578 protein was associated with increased PSA level at diagnosis (p=0.015, Table 4). High nuclear and cytoplasmic PKC protein expression was associated with increased age (p=0.032 and p=0.018 respectively, Table 4). High expression of nuclear PKC protein was associated with increased PSA level at diagnosis (p=0.009, Table 4). Expression of pPKC was not significantly associated with any clinico-pathological outcome measures.
Table 4. Clinico-pathological factors related to pAR578 and PKC expression.
| Nuclear pAR578 | Cytoplasmic pAR578 | Nuclear PKC | Cytoplasmic PKC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low expression | High expression | p-value | Low expression | High expression | p-value | Low expression | High expression | p-value | Low expression | High expression | p-value | |
| Age (<70/>70) | 14/16 | 10/20 | 0.296 | 16/16 | 8/20 | 0.94 | 17/13 | 8/20 | 0.032 | 17/12 | 8/21 | 0.018 |
| Gleason (<7/7/>7) | 9/10/7 | 8/7/12 | 0.324 | 13/9/6 | 4/8/13 | 0.008 | 10/10/7 | 10/3/12 | 0.431 | 10/7/8 | 10/6/11 | 0.630 |
| PSA at diagnosis (<10/10/>10) | 9/4/11 | 2/5/19 | 0.015 | 8/5/13 | 3/4/17 | 0.096 | 9/8/9 | 3/3/18 | 0.009 | 7/7/13 | 5/4/14 | 0.478 |
| Lymphovascular invasion (no/yes) | 27/3 | 27/3 | 1.000 | 30/2 | 24/4 | 0.305 | 27/3 | 26/2 | 0.701 | 26/3 | 27/2 | 0.643 |
| PSA at recurrence (<10/10/>10) | 13/0/3 | 13/0/6 | 0.394 | 15/0/2 | 11/0/7 | 0.071 | 12/0/6 | 11/0/4 | 0.683 | 12/0/5 | 11/0/5 | 0.910 |
| Metastases at any time (no/yes) | 11/6 | 8/10 | 0.236 | 12/9 | 7/7 | 0.682 | 9/7 | 11/6 | 0.625 | 13/5 | 7/8 | 0.141 |
| Ki67 (≤median/>median) | 17/10 | 18/10 | 0.920 | 16/12 | 19/8 | 0.312 | 17/9 | 16/12 | 0.539 | 17/9 | 16/12 | 0.539 |
Expression of pARS578 in the nucleus and cytoplasm was examined for significant relationships with clinical variables as shown. Protein expression was divided into high and low groups. Clinical variables were divided into groups and used for statistical analysis. When the clinical variable consisted of 2 independent groups the Mann-Whitney U test was performed, and >2 independent groups the Kruskal-Wallis test was used. Significant associations are highlighted in bold.
Kinase mediating AR phosphorylation
Scansite 2.0 predicted PKC as a strong candidate mediating phosphorylation of AR at Ser-578. In the clinical specimens nuclear PKC expression was significantly associated with pARS578 expression both in the cytoplasm (c.c. 0.426, p=0.002) and nucleus (c.c. 0.469, p=0.001) (Table 5, Figure 2). There was no association between pPKC expression and pARS578 expression.
Table 5. Associations between protein expression of pARS578 and kinase expression (PKC and pPKC).
| PKC | pPKC | |||
|---|---|---|---|---|
| NuclearP value, C.C | CytoplasmicP value, C.C | NuclearP value, C.C | CytoplasmicP value, C.C | |
| pAR578 Nuclear | 0.001, 0.469 | 0.044, 0.284 | 0.253, 0.155 | 0.256, 0.154 |
| pAR578 Cytoplasmic | 0.002, 0.426 | 0.894, 0.019 | 0.790, 0.036 | 0.649, 0.062 |
C.C. denotes Pearson's correlation co-efficient
Values in bold denotes associations with Pearson's correlation co-efficient > 0.4 and p value < 0.05.
Figure 2. Scatter plots illustrating the correlation of PKC nuclear expression with pARS578 nuclear A. and cytoplasmic B. expression.
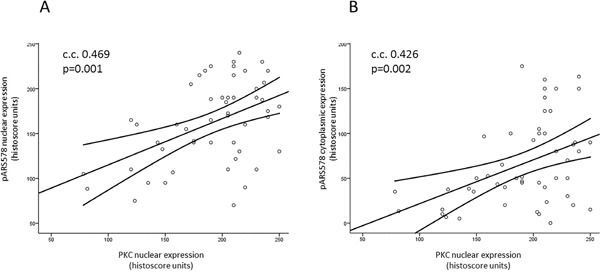
Line represents best fit line with mean 95% confidence intervals. Pearson's correlation coefficient (c.c.) >0.4 and p<0.05 is considered significant.
Correlation of clinical outcome with pARS578 and PKC expression
High nuclear AR was associated with shorter time to biochemical relapse (proportion of patients relapsed at 5yr 78.9% vs 46.7% HR 2.84 (95% CI 1.5–5.3), p=0.001). High cytoplasmic pARS578 was also associated with shorter time to biochemical relapse (proportion of patients relapsed at 5 yr 82.1% vs 51.9% HR 2.1 (95% CI 1.0-4.2), p=0.034). Interestingly, no association was observed between PKC expression and time to biochemical relapse (Table 6).
Table 6. Univariate analysis of AR, pARS578, PKC and pPKC expression and clinical outcome measures.
| Univariate analysis | |||
|---|---|---|---|
| Time to biochemical relapseP value Hazard Ratio (95% CI) | Survival from biochemical relapseP value Hazard Ratio (95% CI) | Disease-specific survivalP value Hazard Ratio (95% CI) | |
| AR Nuclear | 0.001, 2.84, (1.5-5.3) | 0.688, 1.18, (0.5-2.7) | 0.233, 1.44, (0.8-2.6) |
| AR Cytoplasmic | 0.466, 1.23, (0.7-2.2) | 0.922, 0.96, (0.4-2.1) | 0.517, 1.21, (0.7-2.2) |
| pARS578 Nuclear | 0.461, 1.30, (0.6-2.6) | 0.347, 1.62, (0.6-4.5) | 0.036, 2.24, (1.0-4.9) |
| pARS578 Cytoplasmic | 0.034, 2.1, (1.0-4.2) | 0.034, 3.19, (1.0-9.9) | <0.001, 4.54, (2.0-10.4) |
| PKC Nuclear | 0.712, 0.88, (0.4-1.8) | 0.450, 1.46, (0.5-3.9) | 0.203, 1.68, (0.8-3.7) |
| PKC Cytoplasmic | 0.938, 1.03, (0.5-2.1) | 0.799, 1.14, (0.4-3.1) | 0.269, 1.56, (0.7-3.5) |
| pPKC Nuclear | 0.764, 1.10, (0.6-2.0) | 0.403, 1.42, (0.6-3.2) | 0.890, 1.05, (0.6-2.0) |
| pPKC Cytoplasmic | 0.877, 0.96, (0.5-1.7) | 0.647, 0.82, (0.4-1.9) | 0.946, 0.98, (0.5-1.9) |
Univariate analysis of AR and pAR protein expression was carried out using Kaplan Meier methods with reference to the clinical outcome measures. Patients were considered to have biochemical relapse dependent on treatment; radical prostatectomy serum PSA >0.2ng/ml, radical radiotherapy serum PSA of 2.0ng/ml above the post treatment nadir level, hormone treatment 2-3 consecutive rises in serum PSA levels above the nadir obtained at intervals of >2 weeks [28, 29]. Numbers in bold denote significant associations with p value <0.05.
Survival following disease recurrence was calculated from biochemical relapse till death or last follow-up using cancer-specific deaths. High expression of cytoplasmic pARS578 was associated with less favourable survival outcomes following biochemical relapse (10 yr survival 24.3% vs 58.3% HR 3.2 (95% CI 1.0-9.9), p=0.034). No association was observed between PKC, pPKC or AR expression and survival from biochemical relapse. (Table 6)
Disease-specific survival was calculated from diagnosis till death or last follow-up using cancer-specific deaths. High nuclear pARS578 was associated with decreased disease-specific survival (10 yr survival 30.5% vs 63.8% HR 2.24 (95% CI 1.0-4.9), p=0.036) (Table 6, Figure 3). High cytoplasmic pARS578 was associated with decreased disease-specific survival (10 yr survival 19.7% vs 71.3% HR 4.54 (95% CI 2.0-10.4), p<0.001) (Table 6, Figure 3). High total pARS578 was associated with decreased disease-specific survival (10 yr survival 18.8% (both high) vs 75.9% (both low) HR 2.20, (95% CI 1.4-3.5) p=0.002) (Table 7). No association was observed between PKC, pPKC or AR expression and disease-specific survival.
Figure 3. Kaplan-Meier survival plots illustrating disease-specific survival in patients with high (dashed line) and low (solid line) nuclear A. and cytoplasmic B. pARS578 expression.
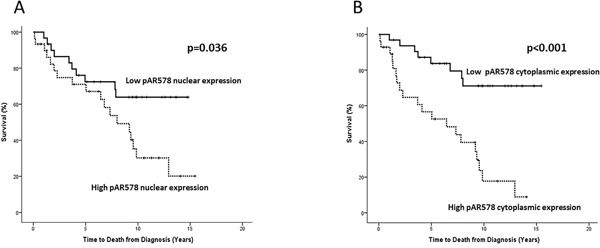
Table 7. Univariate analysis of combined phosphorylated AR sites and disease-specific survival.
| Univariate analysis | |
|---|---|
| Disease-specific survivalP value Hazard Ratio (95% CI) | |
| Total pARS578 | 0.002, 2.20, (1.4-3.5) |
| Total pARS81 | 0.034, 1.78, (1.1-2.7) |
| pARS578 cytoplasmic + pARS81 cytoplasmic | <0.001, 2.88, (1.7-5.0) |
| pARS578 nuclear + pARS81 nuclear | 0.011, 1.85, (1.2-2.9) |
| Total pARS578 + Total pARS81 | 0.005, 1.76, (1.3-2.4) |
Univariate analysis of total and combine pAR protein expression was carried out using Kaplan Meier methods with reference to disease-specific survival.
As nuclear PKC expression correlated strongly with pARS578 both in the cytoplasm and the nucleus it was investigated as to whether a combination of the two proteins could further inform on disease outcome. Nuclear PKC expression was therefore combined with cytoplasmic and nuclear pARS578 expression as follows: (i) low PKC and low pARS578, (ii) high PKC or high pARS578 and (iii) high PKC and high pARS578 expression. High PKC and cytoplasmic pARS578 expression was associated with disease-specific survival (10 yr survival 20.5% vs 46.8% vs 82% HR 2.6 (95% CI 1.5-4.6), p=0.001) (Figure 4). Similarly high PKC and nuclear pARS578 expression was associated with disease-specific survival (10 yr survival 30.9% vs 44.3% vs 75.6%) HR 2.0 (95% CI 1.2-3.4), p=0.038 (Figure 4).
Figure 4. Kaplan-Meier survival plots illustrating disease-specific survival in hormone-naïve prostate cancer patients with nuclear PKC expression combined with nuclear A. and cytoplasmic B. pARS578 expression.
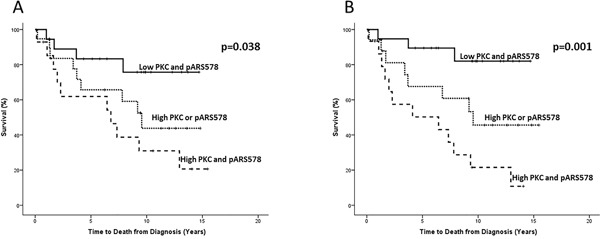
Protein expression was divided for analysis as low (≤median) and high (>median) and nuclear PKC expression was combined with pARS578 expression to give the following scores; low nuclear PKC and pARS578 (solid line), high nuclear PKC or pARS578 (dotted line) and high nuclear PKC and pARS578 (dashed line).
We have previously shown that phosphorylation of the androgen receptor at Ser-81 (pARS81) is associated with decreased disease-specific survival [14]. The androgen receptor is phosphorylated at Ser-81 in response to androgens, suggesting these patients would benefit from AR targeted therapies. As it is predicted that the AR is phosphorylated by PKC at Ser-578, patients with high expression of pARS578 may benefit form treatment with a PKC inhibitor. We investigated whether assessing pARS81 in combination with pARS578 would identify a population of patients that might benefit from dual targeted therapy (AR targeted therapies to inhibit phosphorylation at pARS81 and PKC inhibitors to inhibit phosphorylation at pARS578). The two phosphorylation sites were combined as follows: (i) high pARS81 and high pARS578, (ii) high pARS81 or high pARS578 and (iii) low pARS81 and low pARS578 expression. High nuclear pARS81 and nuclear pARS578 was associated with disease-specific survival (10 yr survival 20.0% vs 26.3% vs 73.2%, HR 1.85, (95% CI 1.2-2.9) p=0.011) (Table 7). High cytoplasmic pARS81 and cytoplasmic pARS578 was associated with disease-specific survival (10 yr survival 15.1% vs 24.4% vs 87.5%, HR 2.88, (95% CI 1.7-5.0) p=<0.001) (Table 7). Lastly, high total pARS81 and total pARS578 was associated with disease-specific survival (10 yr survival 0% (both high) vs 85.7% (both low), HR 1.76, (95% CI 1.3-2.4) p=0.005) (Table 7).
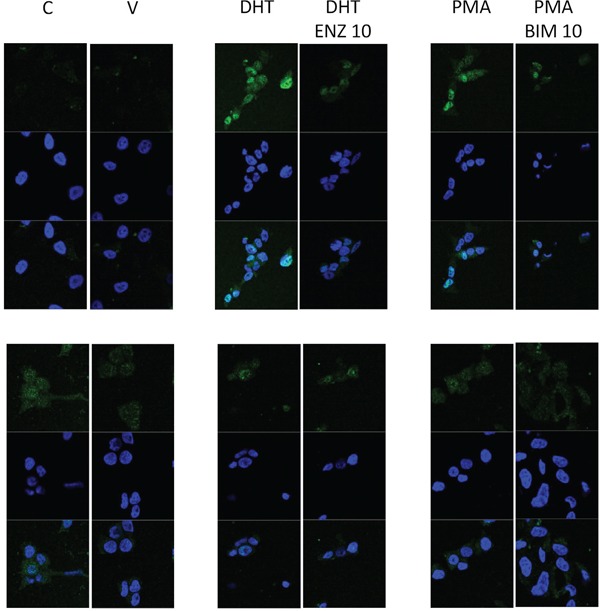
Immunofluorescence
In LNCaP cells DHT and PMA induced AR translocation to the nucleus was inhibited by the presence of DHT and BIM respectively. DHT induced nuclear translocation of AR578 was not clearly evident in LNCaP cells suggesting that this is not regulated by DHT, AR578 nuclear translocation was observed in response to PMA and again this was inhibited by BIM, but PMA induced AR578 nuclear translocation was to a lesser extend than that observed with AR (Figure 5).
Figure 5. Immunofluorescent image demonstrating that nuclear translocation of AR in response to DHT or PMA can be inhibited by enzalutamide and BIM and nuclear translocation of AR578 in response to PMA can be inhibited by BIM.
DISCUSSION
The current study demonstrates that phosphorylation of AR at Ser-578 is strongly associated with PKC expression. In addition, the expression of pARS578 in hormone-naïve prostate cancer was observed to be a negative prognostic marker associated with shorter time to biochemical relapse, decreased survival from biochemical relapse and decreased disease-specific survival. Although we were unable to demonstrate any significant association between pPKC expression and clinico-pathological outcome measures, there was a trend towards significance between high expression of both nuclear and cytoplasmic pPKC and increased Gleason score (p=0.09 and p=0.103 respectively).
In agreement with previous reports PKC expression correlated strongly with pARS578 expression [13]. Previous site directed mutagenesis work in castrate-resistant cell lines has demonstrated that PKC induced phosphorylation is reduced in pARS578 knock down cells [13]. The current study adds to this by suggesting that the link between PKC and AR phosphorylation is also present in hormone naïve prostate cancer tissue and therefore may have important implications in both early and late stages of the disease. Similar site directed mutagenesis studies are necessary in prostate cancer cell lines established from localised disease in order to confirm this finding.
We observed significant associations between protein expression and outcome measures for both nuclear and cytoplasmic pARS578. Indeed, the presence of cytoplasmic AR is expected as the AR localizes to the cytoplasm in the absence of ligand-binding due to a ligand-regulated nuclear export signal [15, 16]. Previous mutagenesis studies investigated the effect on subcellular localization of AR in COS cells. This work demonstrated that in wild type pARS578 cells AR is distributed between the nucleus and cytoplasm indicative of nuclear-cytoplasmic shuttling [13]. However in cells where the pARS578 site was mutated AR expression was found exclusively in the nucleus [13]. The current study is in agreement with this work and provides further evidence for the involvement of pARS578 in nuclear-cytoplasmic shuttling in neoplastic prostate tissue.
Protein kinase C is the kinase predicted to be responsible for phosphorylation at Ser-578 on the AR. We have found that whilst pARS578 predicts disease-specific survival, PKC expression alone does not. When expression of pARS578 was combined with PKC expression however, the two proteins together were still able to inform on disease-specific survival. No additive effect was observed in terms of significance when pARS578 was combined with PKC to predict disease-specific survival, suggesting that PKC and pARS578 are involved in the same pathway.
It is well established that Ser-81 is phosphorylated in response to androgen binding on the androgen receptor [8, 17]. We investigated whether there was a cumulative predictive effect in terms of disease-specific survival when two AR phosphorylation sites with two independent pathways were combined. Predictive power was increased when pARS81 and pARS578 expression was combined than compared to using pARS81 or pARS578 expression independently. These results are of great importance clinically, as it highlights a sub-population of patients who may benefit from dual targeted therapy with androgen deprivation therapy and PKC inhibitors. Unfortunately, to date, oncology clinical trials have had little success in utilising PKC inhibitors either due to poor efficacy, or significant intolerable side effects [18]. This study adds to the existing body of evidence that PKC has a role in prostate cancer, and as such encourages further work in drug development of an efficacious PKC inhibitor. Future work would consist of investigating expression of pARS81 and pARS578 in prostate cancer cell lines in response to treatment with androgen deprivation therapy and PKC inhibitors.
The prognostic significance of AR serine phosphorylation has been investigated previously by ourselves and others [14, 19, 20]. However, to our knowledge, this is the first in vivo report of the prognostic significance of AR phosphorylation at serine site 578. Previous work relating to total AR expression has demonstrated widely conflicting results. In support of its use as a negative prognostic marker in prostate cancer an investigation of 115 hormone naïve radical prostatectomy specimens demonstrated that higher tumour AR gene expression was associated with shorter time to biochemical recurrence [21]. Three further studies with a total of 788 patients demonstrated that higher AR expression was associated with a worse prognosis [22–24]. In support of this, AR gene amplification and corresponding increase in expression at the protein level has been shown in castrate-resistant tumour samples when compared to matched hormone sensitive samples from the same patient [25]. Similarly, hormone sensitive prostate cancer xenografts in castrated mice demonstrated an increase in AR gene and protein expression in addition to the acquisition of the ability of the AR to respond to anti-androgens and to aberrantly recruit coactivators to the promoters [26]. However, other work, including a large study involving a tissue microarray of 2805 prostate cancers, has shown no association of AR expression with prognosis [27]. These conflicting findings may depend on several factors such as tissue heterogeneity, timing of specimen dissection, and methods to detect AR expression including the use of different antibodies. In addition, the simple expression of AR does not reflect its function or its activity, and therefore may account for the variations reported with regards to prognostic significance. AR phosphorylation, which is known to provide molecular stability, may therefore be a marker of activation. This current study lends support to this argument as we have demonstrated that those patients who have a high level of pARS578 have reduced overall survival when compared to AR expression alone.
We acknowledge the possibility of cross-reactivity in the usage of a phospho-specific antibody particularly on a protein such as AR with multiple phosphorylation sites. However the specificity of phospho-AR antibodies has been stringently tested by our group previously and they have been found to be of suitable quality (Figure 6) [14]. To follow on from both the previous and the current study we intend to validate these findings in a larger independent patient cohort.
Figure 6. Blocking peptide experiments for pARS578 are shown.
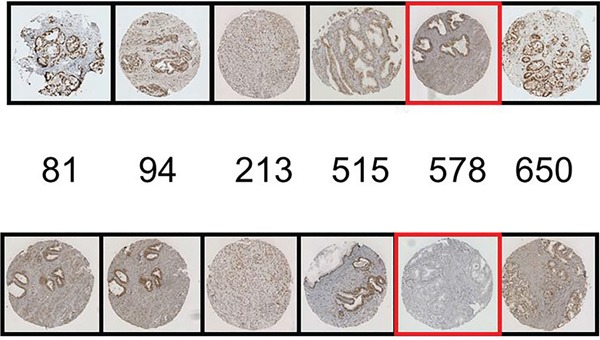
The top row represents the positive control i.e. IHC conducted with each AR phosphospecific antibody as indicated. The bottom row represents antibodies to AR phosphorylation sites pre-incubated with pARS578 peptide. The specific peptide utilised is boxed in red. No staining is demonstrated when the pARS578 peptide is incubated with pARS578antibody, whereas staining is maintained at the other phospho-AR sites.
An obvious limitation of this study is the small sample size and as such the results should be interpreted with caution and validated in a large independent cohort. However, even with low patient numbers, we have demonstrated that AR phosphorylation by PKC at serine 578 is of prognostic significance. These results are striking in particular when considered that this was a hormone-naïve cohort of patients who subsequently received a variety of treatments (surgery, radiotherapy and hormones) and that, due to small numbers, we were unable to unpick these groups. We were unable to show any significant associations between pPKC and pARS578 expression, nor with any clinical outcome measures. Again, this may be due to the small sample size. We now intend to repeat this work in two further cohorts: firstly a cohort of prostate cancer patients treated with active surveillance, and secondly a larger cohort of hormone-naïve prostate cancer patients.
conclusions
This study provides further evidence for the significance of androgen receptor signalling in the progression of prostate cancer. We have demonstrated that PKC may phosphorylate AR at serine 578 and that, in combination with current diagnostic tools, pARS578 protein expression could provide a desperately needed prognostic marker to aid treatment decision-making in prostate cancer patients at diagnosis. Furthermore, PKC-driven AR phosphorylation may be a potential novel therapeutic target. This finding has the potential to reduce over-treatment of clinically insignificant disease and prevent delay in treatment of occult aggressive disease.
MATERIALS AND METHODS
Patients
Ninety patients with hormone-naïve prostate cancer samples available were recruited at the Glasgow Royal Infirmary between 1992 and 2002. Last date of follow up was 11/01/2012. Patients gave written consent. Clinical data included age, Gleason score, tumour lymphovascular invasion (LVI), serum PSA levels at diagnosis, biochemical recurrence, serum PSA at biochemical recurrence and presence of metastases. Patients were considered to have biochemical recurrence dependent on treatment; radical prostatectomy serum PSA >0.2ng/ml, radical radiotherapy serum PSA of 2.0ng/ml above the post treatment nadir level, hormone treatment 2-3 consecutive rises in serum PSA levels above the nadir obtained at intervals of >2 weeks [28, 29]. Study end points were biochemical relapse, survival from biochemical relapse and disease-specific survival. West of Scotland Research Ethics Committee approved the study (reference: 05/S0704/94).
Identification of Kinases mediating AR phosphorylation
Scansite 2.0 was utilised to predict which sites on the AR would be phosphorylated by PKC [12]. The search was conducted using the protein ID “ANDR_HUMAN” (Accession number: P10275).
Tissue microarray (TMA) construction
Three 0.6mm2 cores of prostate cancer tissue, identified by a uropathologist, were removed from formalin-fixed paraffin-embedded blocks. Recipient array blocks were constructed in triplicate. Control cores of normal prostate, colon, breast, pancreas, tonsil, kidney, liver and lung tissue were included in each TMA.
Immunohistochemistry (IHC)
AR expression, pARS81 expression and proliferation index (Ki67) was already available for this cohort [14]. IHC was conducted in triplicate on aforementioned TMAs for the following proteins pARS578, PKC, and pPKC. Antibody to pARS578 was not commercially available and so was synthesized for this project by Covalab, Villeurbanne, France. In brief, host animals were immunized with conjugated phosphorylated peptide for the protein sequence HYGALTCG[Sp]CKVF. Animals were serially bled and following the final bleed phospho-specific antibodies were selected by affinity purification. Two affinity columns were used; the first column coupled with the non-phosphorylated peptide and the second column with the phosphorylated peptide. The serum was passed through the first column and the non-retaining elute kept and used for the second purification. The elute was purified on the second column in order to remove antibodies which might recognise the un-phosphorylated peptide. ELISA tests were performed to ensure that the recovered antibody was specific for phosphorylation of AR specifically at Ser-578.
TMAs were dewaxed in xylene and rehydrated through graded alcohol. Antigen retrieval for PKC and pPKC was performed using heat treatment under pressure in citrate buffer pH6, 5min. Antigen retrieval for pARS578 was performed using heat treatment under pressure in Tris-EDTA buffer (5mM Trizma Base, 1mM EDTA, pH8), 5min. Sections were cooled in buffer for 20min before washing in 3% H202. Sections were blocked using 5% horse serum in Tris-buffered saline (TBS). Antibodies for PKC (#ab59363, Abcam, UK), pPKC (SC -11760, Santa Cruz, USA) and pARS578 (Covalab, France) were incubated overnight at 4°C diluted at 1:100, 1:120 and 1:500 respectively. All antibodies were diluted in Dako antibody diluent (Dako UK Ltd.). Bound antibody complex was visualized using EnVision plus kit (#K5007, Dako UK Ltd.) followed by 3,3-diaminobenzidine tetrahydrochloride (DAB, Dako UK Ltd.). Nuclei were counterstained with haematoxylin and Scots Tap Water Substitute. Finally, sections were dehydrated through graded alcohol and xylene and mounted with Di-N-ButylePhthalate in Xylene.
Antibody validation
Peptide competition assays were performed to confirm pARS578 antibody specificity. pARS578 peptide (Protein sequence ALTCG-S(pS)-CKVFFKR raised in rabbit by Eurogentec Ltd., Seraing, Belgium) was incubated at ratio 200:1 with pARS81, pARS94, pARS308, pARS515, pARS578 and pARS650 antibodies overnight at 4°C. IHC was then performed as described above. Peptide competition assay demonstrated that only staining in response to antibody raised to pARS578 was blocked and staining to other phosphorylation sites was not altered (Figure 6).
Scoring
Tissue staining intensity was scored by two blinded independent observers using a weighted histo-score (H-score) method [30, 31]. H-score was calculated from the formula: (0 x % cells staining negative) + (1 x % cells staining weakly positive) + (2 x % cells staining moderately positive) + (3 x % cells staining strongly positive). The mean H-score from staining conducted in triplicate was used for analysis. Signals for nuclear and cytoplasmic pAR immunoreactivity were evaluated separately.
Statistical analysis
Statistical analysis was performed using SPSS version 19.0 for Windows (IBM). ICCCs confirmed histo-scoring consistency between observers. Pearson's rank correlation coefficients (c.c.) assessed associations between protein expression. Mann-Whitney U test or Kruskal-Wallis test assessed relationships between protein expression and clinico-pathologic characteristics. Kaplan-Meier methods, using the log-rank test, compared survival between patients according to clinico-pathologic parameters and high/low protein expression. A <0.05 significance level was used and Bonferroni correction was applied where applicable.
Immunofluorescence
LNCaP cells were seeded at 2.5 × 104 cells per well in a 6 well chamber slide. Cells were cultured in RPMI supplemented with Glutamax, penicillin streptomycin and fetal bovine serum at 37°C in 5% CO2 until cells had reached 70% confluency. Cells were cultured in serum-free media for 24 hours. The LNCaP cells were treated with 1 nM dihydrotestosterone (DHT) or 1 nM phorbol 12-myristate 13-acetate (PMA), a PKC activator, or 1 nM DHT and 10 nM enzalutamide (antiandrogen) or 1n M PMA and 10 nM Bisindolymaleimide 1 (BIM-1), a PKC inhibitor, for one hour. Cells were fixed with 4% PFA at 4°C for 30 minutes. Cells were washed twice with PBS for five minutes on a rocker. Cells were permeabilised by treating twice with 0.1% Triton X-100 for five minutes. Blocking solution (1.5% horse serum in 0.1% TBS-tween) was applied for thirty minutes on a rocker at room temperature. Primary antibody, diluted in blocking solution (AR, 1:200 (DAKO), pARS578, 1:100 (Covalab)) was applied for one hour at room temperature. Cells were washed three times in TBS for ten minutes. Secondary antibody, diluted in blocking buffer, (Goat anti-mouse IgG secondary Alexa-Fluor 488, 1:500 (ThermoFisher) and Goat anti-rabbit IgG secondary Alexa-Fluor 488, 1:500 (ThermoFisher) was applied to the cells treated with the respective primary antibodies for one hour in the dark at room temperature. Cells were washed three times in TBS for five minutes. Vectashield mounting medium with DAPI (Vectorlabs) was used to counterstain DNA in the nucleus. The cells were visualised using confocal microscopy. Each experiment was performed in triplicate and repeated 3 times.
Acknowledgments
This study was supported by funding from the Association of International Cancer Research, Think Pink and NHS Greater Glasgow and Clyde Research Endowment Fund.
Footnotes
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
- 1.Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O, Bray F. International variation in prostate cancer incidence and mortality rates. European urology. 2012;61:1079–1092. doi: 10.1016/j.eururo.2012.02.054. [DOI] [PubMed] [Google Scholar]
- 2.Roehrborn CG, Black LK. The economic burden of prostate cancer. BJU international. 2011;108:806–813. doi: 10.1111/j.1464-410X.2011.10365.x. [DOI] [PubMed] [Google Scholar]
- 3.Mistry M, Parkin DM, Ahmad AS, Sasieni P. Cancer incidence in the United Kingdom: projections to the year 2030. British journal of cancer. 2011;105:1795–1803. doi: 10.1038/bjc.2011.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agus DB, Cordon-Cardo C, Fox W, Drobnjak M, Koff A, Golde DW, Scher HI. Prostate cancer cell cycle regulators: response to androgen withdrawal and development of androgen independence. Journal of the National Cancer Institute. 1999;91:1869–1876. doi: 10.1093/jnci/91.21.1869. [DOI] [PubMed] [Google Scholar]
- 5.Chen Y, Sawyers CL, Scher HI. Targeting the androgen receptor pathway in prostate cancer. Current opinion in pharmacology. 2008;8:440–448. doi: 10.1016/j.coph.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fleming MT, Morris MJ, Heller G, Scher HI. Post-therapy changes in PSA as an outcome measure in prostate cancer clinical trials. Nature clinical practice Oncology. 2006;3:658–667. doi: 10.1038/ncponc0664. [DOI] [PubMed] [Google Scholar]
- 7.Kuiper GG, Brinkmann AO. Phosphotryptic peptide analysis of the human androgen receptor: detection of a hormone-induced phosphopeptide. Biochemistry. 1995;34:1851–1857. doi: 10.1021/bi00006a005. [DOI] [PubMed] [Google Scholar]
- 8.Gioeli D, Paschal BM. Post-translational modification of the androgen receptor. Molecular and cellular endocrinology. 2012;352:70–78. doi: 10.1016/j.mce.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Blok LJ, de Ruiter PE, Brinkmann AO. Forskolin-induced dephosphorylation of the androgen receptor impairs ligand binding. Biochemistry. 1998;37:3850–3857. doi: 10.1021/bi9724422. [DOI] [PubMed] [Google Scholar]
- 10.Gioeli D, Black BE, Gordon V, Spencer A, Kesler CT, Eblen ST, Paschal BM, Weber MJ. Stress kinase signaling regulates androgen receptor phosphorylation, transcription, and localization. Molecular endocrinology. 2006;20:503–515. doi: 10.1210/me.2005-0351. [DOI] [PubMed] [Google Scholar]
- 11.Zhou ZX, Kemppainen JA, Wilson EM. Identification of three proline-directed phosphorylation sites in the human androgen receptor. Molecular endocrinology (Baltimore, Md) 1995;9:605–615. doi: 10.1210/mend.9.5.7565807. [DOI] [PubMed] [Google Scholar]
- 12.Obenauer JC, Cantley LC, Yaffe MB. Scansite 2.0: Proteome-wide prediction of cell signaling interactions using short sequence motifs. Nucleic acids research. 2003;31:3635–3641. doi: 10.1093/nar/gkg584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ponguta LA, Gregory CW, French FS, Wilson EM. Site-specific androgen receptor serine phosphorylation linked to epidermal growth factor-dependent growth of castration-recurrent prostate cancer. The Journal of biological chemistry. 2008;283:20989–21001. doi: 10.1074/jbc.M802392200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Willder JM, Heng SJ, McCall P, Adams CE, Tannahill C, Fyffe G, Seywright M, Horgan PG, Leung HY, Underwood MA, Edwards J. Androgen receptor phosphorylation at serine 515 by Cdk1 predicts biochemical relapse in prostate cancer patients. British journal of cancer. 2013;108:139–148. doi: 10.1038/bjc.2012.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tyagi RK, Lavrovsky Y, Ahn SC, Song CS, Chatterjee B, Roy AK. Dynamics of intracellular movement and nucleocytoplasmic recycling of the ligand-activated androgen receptor in living cells. Molecular endocrinology. 2000;14:1162–1174. doi: 10.1210/mend.14.8.0497. [DOI] [PubMed] [Google Scholar]
- 16.Wen Y, Hu MC, Makino K, Spohn B, Bartholomeusz G, Yan DH, Hung MC. HER-2/neu promotes androgen-independent survival and growth of prostate cancer cells through the Akt pathway. Cancer research. 2000;60:6841–6845. [PubMed] [Google Scholar]
- 17.Gioeli D, Ficarro SB, Kwiek JJ, Aaronson D, Hancock M, Catling AD, White FM, Christian RE, Settlage RE, Shabanowitz J, Hunt DF, Weber MJ. Androgen receptor phosphorylation. Regulation and identification of the phosphorylation sites. The Journal of biological chemistry. 2002;277:29304–29314. doi: 10.1074/jbc.M204131200. [DOI] [PubMed] [Google Scholar]
- 18.Mochly-Rosen D, Das K, Grimes KV. Protein kinase C, an elusive therapeutic target? Nature reviews Drug discovery. 2012;11:937–957. doi: 10.1038/nrd3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ha S, Iqbal NJ, Mita P, Ruoff R, Gerald WL, Lepor H, Taneja SS, Lee P, Melamed J, Garabedian MJ, Logan SK. Phosphorylation of the androgen receptor by PIM1 in hormone refractory prostate cancer. Oncogene. 2013;32:3992–4000. doi: 10.1038/onc.2012.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCall P, Gemmell LK, Mukherjee R, Bartlett JM, Edwards J. Phosphorylation of the androgen receptor is associated with reduced survival in hormone-refractory prostate cancer patients. British journal of cancer. 2008;98:1094–1101. doi: 10.1038/sj.bjc.6604152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosner IL, Ravindranath L, Furusato B, Chen Y, Gao C, Cullen J, Sesterhenn IA, McLeod DG, Srivastava S, Petrovics G. Higher tumor to benign ratio of the androgen receptor mRNA expression associates with prostate cancer progression after radical prostatectomy. Urology. 2007;70:1225–1229. doi: 10.1016/j.urology.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 22.Inoue T, Segawa T, Shiraishi T, Yoshida T, Toda Y, Yamada T, Kinukawa N, Kinoshita H, Kamoto T, Ogawa O. Androgen receptor, Ki67, and p53 expression in radical prostatectomy specimens predict treatment failure in Japanese population. Urology. 2005;66:332–337. doi: 10.1016/j.urology.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 23.Li R, Wheeler T, Dai H, Frolov A, Thompson T, Ayala G. High level of androgen receptor is associated with aggressive clinicopathologic features and decreased biochemical recurrence-free survival in prostate: cancer patients treated with radical prostatectomy. The American journal of surgical pathology. 2004;28:928–934. doi: 10.1097/00000478-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Henshall SM, Quinn DI, Lee CS, Head DR, Golovsky D, Brenner PC, Delprado W, Stricker PD, Grygiel JJ, Sutherland RL. Altered expression of androgen receptor in the malignant epithelium and adjacent stroma is associated with early relapse in prostate cancer. Cancer research. 2001;61:423–427. [PubMed] [Google Scholar]
- 25.Edwards J, Krishna NS, Grigor KM, Bartlett JM. Androgen receptor gene amplification and protein expression in hormone refractory prostate cancer. British journal of cancer. 2003;89:552–556. doi: 10.1038/sj.bjc.6601127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen CD, Welsbie DS, Tran C, Baek SH, Chen R, Vessella R, Rosenfeld MG, Sawyers CL. Molecular determinants of resistance to antiandrogen therapy. Nature medicine. 2004;10:33–39. doi: 10.1038/nm972. [DOI] [PubMed] [Google Scholar]
- 27.Minner S, Enodien M, Sirma H, Luebke AM, Krohn A, Mayer PS, Simon R, Tennstedt P, Muller J, Scholz L, Brase JC, Liu AY, Schluter H, Pantel K, Schumacher U, Bokemeyer C, et al. ERG status is unrelated to PSA recurrence in radically operated prostate cancer in the absence of antihormonal therapy. Clinical cancer research. 2011;17:5878–5888. doi: 10.1158/1078-0432.CCR-11-1251. [DOI] [PubMed] [Google Scholar]
- 28.Cookson MS, Aus G, Burnett AL, Canby-Hagino ED, D'Amico AV, Dmochowski RR, Eton DT, Forman JD, Goldenberg SL, Hernandez J, Higano CS, Kraus SR, Moul JW, Tangen C, Thrasher JB, Thompson I. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. The Journal of urology. 2007;177:540–545. doi: 10.1016/j.juro.2006.10.097. [DOI] [PubMed] [Google Scholar]
- 29.Roach M, G 3rd Hanks, Thames H, Jr., Schellhammer P, Shipley WU, Sokol GH, Sandler H. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. International journal of radiation oncology, biology, physics. 2006;65:965–974. doi: 10.1016/j.ijrobp.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 30.Kirkegaard T, Edwards J, Tovey S, McGlynn LM, Krishna SN, Mukherjee R, Tam L, Munro AF, Dunne B, Bartlett JM. Observer variation in immunohistochemical analysis of protein expression, time for a change? Histopathology. 2006;48:787–794. doi: 10.1111/j.1365-2559.2006.02412.x. [DOI] [PubMed] [Google Scholar]
- 31.McCarty KS, Jr., Szabo E, Flowers JL, Cox EB, Leight GS, Miller L, Konrath J, Soper JT, Budwit DA, Creasman WT, et al. Use of a monoclonal anti-estrogen receptor antibody in the immunohistochemical evaluation of human tumors. Cancer research. 1986;46:4244s–4248s. [PubMed] [Google Scholar]


