Highlights
-
•
Vaccine hesitancy is a global problem that is complex and multilayered. Vaccine hesitancy is context, time, place and vaccine specific.
-
•
Interviews with immunization managers were conducted to determine the breadth and perceived drivers of vaccine hesitancy at the countries’ level.
-
•
Our study results, not unexpectedly, revealed a wide variation in the reported basis for vaccine hesitancy across countries.
Keywords: Vaccine hesitancy, Immunization, Determinants, Vaccination, Interviews, Immunization managers
Abstract
The term vaccine hesitancy refers to delay in acceptance or refusal of vaccines despite the availability of vaccination services. Different factors influence vaccine hesitancy and these are context-specific, varying across time and place and with different vaccines. Factors such as complacency, convenience and confidence are involved. Acceptance of vaccines may be decreasing and several explanations for this trend have been proposed. The WHO Strategic Advisory Group of Experts (SAGE) on Immunization has recognized the global importance of vaccine hesitancy and recommended an interview study with immunization managers (IMs) to better understand the range of vaccine hesitancy determinants that are encountered in different settings. Interviews with IMs in 13 selected countries were conducted between September and December 2013 and various factors that discourage vaccine acceptance were identified. Vaccine hesitancy was not defined consistently by the IMs and most interpreted the term as meaning vaccine refusal. Although vaccine hesitancy existed in all 13 countries, some IMs considered its impact on immunization programmes to be a minor problem. The causes of vaccine hesitancy varied in the different countries and were context-specific, indicating a need to strengthen the capacity of national programmes to identify the locally relevant causal factors and to develop adapted strategies to address them.
1. Introduction
Attitudes to vaccination can be seen as a continuum ranging from total acceptance to complete refusal. Vaccine-hesitant individuals are a heterogeneous group within this continuum. Vaccine-hesitant individuals may refuse some vaccines, but agree to others, delay vaccination or accept vaccination although doubtful about doing so [1], [2]. Vaccine hesitancy is present when vaccine acceptance is lower than would be expected in the context of information provided and the services available. The phenomenon is complex and context-specific, varying across time and place and with different vaccines. Factors such as complacency, convenience, as well as confidence in vaccines(s) may all contribute to the delay of vaccination or refusal of one, some or almost all vaccines [3].
The WHO Strategic Advisory Group of Experts (SAGE) on Immunization has recognized the global importance of vaccine hesitancy as a growing problem. The SAGE Working Group on Vaccine Hesitancy was set up with the mandate to examine the evidence and provide advice to SAGE on how to address vaccine hesitancy and its determinants [4].
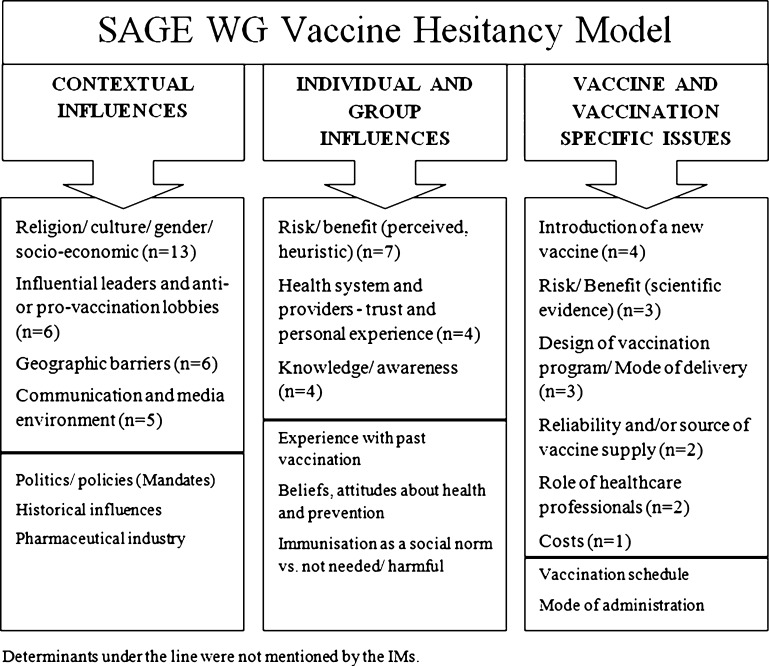
In order to map the influential contributing factors, the SAGE Working Group developed a matrix of determinants of vaccine hesitancy based on a systematic literature review [5]. This matrix acknowledges the scope of vaccine hesitancy, and differentiates between contextual, individual, group, and vaccine- or vaccination-specific factors that influence the acceptability for vaccination [6].
In April 2013, SAGE recommended that interviews be conducted with immunization managers (IMs) [7], who have oversight responsibility at state and national levels for an immunization programme, in order to better understand the variety of challenges existing in different settings [3], [8].
This paper reports the results of the interviews conducted between September and December 2013.
2. Methods
The SAGE Working Group developed a guide for the conduct of telephone-based interviews, designed for qualitative capture of unanticipated responses and assessment of known determinants of vaccine hesitancy. Data were collected using semi-structured interviews [9], [10].
To obtain a representative sample of countries with a broad range of socioeconomic settings and population sizes over all regions, a purposive sampling technique was used. Criteria for selection included:
-
i.
Representation from all six WHO Regions–—African (AFR), Americas (AMR), Eastern Mediterranean (EMR), European (EUR), South-East Asia (SEAR) and Western Pacific (WPR).
-
ii.
Representation from the three economic categories recognized by the World Bank—low, middle and high income countries [11].
-
iii.
The national IM had to be experienced and responsive.
In consultation with WHO regional advisors on immunization, 15 countries were selected that together met the range of criteria. The IMs from each of the selected countries were contacted and briefed by staff from the WHO regional offices. Interviews were conducted in English, Spanish or French by two interviewers from WHO.
The interviews were recorded and summarized by the interviewers. Interview transcriptions were sent back to the IMs for review, correction if necessary, and approval. A structured electronic data extraction form was developed with predefined data fields for extracting consistent data. For all interviews, data were extracted and entered by two independent researchers. A third independent senior researcher checked for accuracy and completeness of the two datasets. Data were analysed by question and mapped against matrix of determinants [6].
3. Results
Interviews were completed with 13 IMs from the six WHO regions: one from AMR (Panama), two from AFR (Republic of the Congo, Zimbabwe), two from EMR (Saudi Arabia, Yemen), three from EUR (Armenia, Belgium, Montenegro, one from SEAR (India), and four from WPR (Japan, Lao PDR, Malaysia, Philippines); most represented low and middle income countries (n = 11). Interviews lasted on average 30 min.
3.1. Definition of vaccine hesitancy
Four IMs explicitly defined their understanding of vaccine hesitancy, as follows: (i) those persons resisting to get vaccinated due to various reasons (Country K); (ii) someone who does not believe vaccines are working and are effective and that vaccines are not necessary (Country F); (iii) parents who would not allow immunization of their child and policy makers who hesitate to introduce a vaccine especially in regard to new vaccinesvs other existing public health interventions (Country L); (iv) an issue that should be addressed when reaching 90% vaccination coverage (Country C). Although the views of other IMs regarding vaccine hesitancy were less explicit, most associated vaccine hesitancy with parental refusal of one or more vaccines (n = 9). Vaccination delays were not included in the definition of vaccine hesitancy by IMs, except in one country, where the IM stated: There is not a problem with under-vaccinated or unimmunized. There are issues with timely vaccination—with following the schedule. Parents are delaying the vaccinations (Country F). Table 1 summarizes the opinions of the IMs regarding vaccine hesitancy in their countries.
Table 1.
Summary of immunization managers’ opinions on vaccine hesitancy.
| Countries | Immunization managers’ perspective on vaccine hesitancy in their country |
|---|---|
| A | Vaccine hesitancy is mostly associated with mass immunization campaigns, especially against polio. It is seen mainly in large cities and associated with particular religious groups. Routine immunization programs are not affected by vaccine hesitancy and access is the main issue. |
| B | Vaccine hesitancy is not considered a problem in the country. Instead, there is vaccine refusal, which is associated with religious groups and higher socioeconomic status. However, vaccine refusal is also not considered a major problem. |
| C | Vaccine hesitancy is not considered a major issue in the country. However, there is a small proportion of the whole population who has concerns about the safety of vaccines and could be categorized as vaccine-hesitant. This is mostly related to the new and costly vaccines, such as the pentavalent vaccine and is seen mainly in the well-educated population group. There are no issues of complacency or convenience (except for migrant populations). Vaccine hesitancy is not considered to have a significant impact on overall coverage rates. |
| D | Vaccine hesitancy is not an issue in the country. Vaccine hesitancy is limited to illegal settlers. |
| E | Although political conflict and instability negatively affect overall access to health services, vaccine hesitancy is not a major issue in the country. Some negative rumours about vaccination have circulated in specific regions and groups of people. Access to vaccination services is challenging for women and nomads. |
| F | Vaccine hesitancy is not a major issue in the country and most children are fully immunized by the age of two. Vaccine hesitancy is mainly associated with medical academics and health care workers who do not believe vaccines are safe and effective (especially combination vaccines and vaccines produced in developing countries). Additionally, there have been issues with religious groups being advised against vaccines because it is forbidden by their religion as well as concerns regarding the safety of combination vaccines. |
| G | In the country, vaccine hesitancy leading to vaccine refusal is not very frequent and is rather localized. Vaccine hesitancy issues have come up in particular groups such as anthroposophist schools, the orthodox Jewish community and Roma societies. Complacency and access to certain communities are bigger issues than hesitancy. |
| H | Vaccine hesitancy exists but is not a major issue in the country. It is not linked to particular groups or geographic areas. Vaccine hesitancy is associated with a lack of perceived benefit of vaccination due to low prevalence of vaccine-preventable disease in the country. There are also concerns regarding vaccine safety and the negative influence of “Internet stories”. |
| I | There are two major groups hesitant to get vaccinated: (1) a small minority of religious groups who do not believe in the benefit of vaccines due to religious or philosophical reasons and (2) the general public concerned by adverse events following immunization (AEFI). Vaccine hesitancy is associated with specific vaccines being in “the focus of attention” (such as HPV or OPV). Media reports of rare adverse events make parents hesitant to vaccinate their children, resulting in decreased uptake. While access and complacency are not important issues, it is speculated that vaccine hesitancy could explain up to 30% of the decrease observed in OPV vaccine coverage (prior to IPV introduction). |
| J | Vaccine hesitancy is an important issue in the country. Vaccine hesitancy is associated with particular ethnic minorities (ethnic Hmong) and remote communities, with a particular focus on the education level of the local population in remote communities. Vaccine hesitancy is associated with lack of perceived benefits of immunization and negative beliefs based on myths (such as vaccination of women leading to infertility). |
| K | Vaccine hesitancy exists in the country, but is rather small. Vaccine hesitancy is mostly associated with people of high socio-economic status living in urban areas who have concerns regarding vaccine safety (especially thimerosal containing vaccines). Concerns regarding porcine components in vaccines by Muslim populations also contribute to vaccine hesitancy in the country. |
| L | Vaccine hesitancy is mostly related to mass immunization campaigns against tetanus. As a result of vaccine hesitancy due to concerns with vaccine safety, up to 20% of eligible population is un- or under-vaccinated. Serious AEFI-inflammation at the site of injection and Catholic pro-life groups stating that TT vaccination was resulting in abortion or infertility have contributed to vaccine hesitancy regarding TT vaccination. Routine vaccination programs are not affected by vaccine hesitancy. |
| M | Vaccine hesitancy is not an important issue in the country and the immunization program has a positive image. However, vaccine hesitancy did occur in particular situations and populations. For example, vaccine hesitancy originated from the Catholic Church when HPV vaccine was introduced, and from health-care professionals when influenza vaccine and TDaP were recommended to be administered to pregnant women. Vaccine hesitancy also occurred among indigenous groups. Additionally, there are vaccine refusals among indigenous groups when vaccination week coincides with cultural events. Geographic barriers may limit the percent vaccinated in some remote areas, but is not linked with vaccine hesitancy. There are no anti-vaccine groups in the country and there is not much vaccine refusal. |
3.2. Impact of vaccine hesitancy on the country's immunization programme
At the time of the interview, all except one IM had heard reports of people reluctant to accept one or all vaccines in their country (Table 2). In the country where no such reports had been heard, the problem reported was vaccine refusal for reasons related to religious beliefs, not hesitancy. In another country, the IM had not heard of any reports of vaccine hesitancy, but acknowledged that a small proportion of the whole population had some concerns regarding vaccine safety and could be considered as vaccine-hesitant. In several countries, IMs reported current or past difficulties due to lack of acceptance related to one specific vaccine or to specific combinations of vaccines (e.g. HPV or TT).
Table 2.
Summary of vaccine hesitancy issues in countries.
| Countries |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | K | L | M | |
| Have you heard reports of people hesitating around whether or not to accept one or all vaccine(s) in your country? | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Does vaccine hesitancy impact on the immunization program? | N | N | N | N | N | N | N | N | Y | Y | N | N | N |
| Do you have an estimate of the % of un- and under-vaccinated in whom lack of confidence was a factor that influenced their decision to get immunized? | UN | 10% (ES) | <5% (ES) | <1% (ES) | UN | UNK | UN | UNK | 30%a (ME) | 30%b (ES) | <5% (ES) | 20%c (ES) | UNK |
| Is complacency a problem in some subpopulations? | UN | Y | N | N | UN | N | Y | Y | N | Y | N | N | N |
| Are there subpopulations where convenience is a barrier to immunization? | Y | Y | Y | Y | Y | N | Y | N | N | Y | N | Y | Y |
Y: Yes; N: No; UN: Unanswered; UNK: Unknown; ES: Estimated; ME: Measured.
Only for OPV vaccine.
In a specifically sub-population.
8% of vaccine refusal, measured.
Even if there had been reports of vaccine hesitancy in their country, 11 of the 13 IMs considered that vaccine hesitancy was not common and that it did not have a significant impact on vaccine uptake in the routine immunization programmes. IMs from two countries indicated that mass immunization campaigns, rather than routine immunization programmes, were affected by vaccine hesitancy. However, two IMs stated that vaccine hesitancy was an important issue in their country.
When IMs were asked about the percentage of non-vaccinated and under-vaccinated individuals in their country due to lack of confidence in vaccination, only six provided estimates ranging from less than 1% to 20% (Table 2).
Four IMs reported issues of complacency in their countries (Table 2). As an example, one IM cited a particular indigenous group which had refused vaccination because vaccination programme activities coincided with a cultural event. Four IMs stated that complacency was not a problem in their countries because immunization was perceived as a priority by most of the population.
Factors concerning convenience and ease of access were perceived to be important by nine of the IMs (Table 2). Convenience was a factor for sub-populations which did not use the health services provided and for hard-to-reach populations. For instance, in one country, more than 25% of the population had no access to health services and access was difficult for immigrants, refugees, nomad populations, those living in remote areas, and for women (mainly because of the socio-norms that require them be accompanied for travel to obtain health care).
3.3. Determinants of vaccine hesitancy using the Working Group matrix
Fig. 1 summarizes the opinions of IMs regarding the main determinants of vaccine hesitancy in the Working Group matrix.
Fig. 1.
Immunization manager's opinions regarding determinants of vaccine hesitancy*.
3.3.1. Contextual influences
Religious beliefs were often a causal factor in vaccine hesitancy (cited by nine IMs). Several IMs were able to specifically identify religious groups in their country that were known to be opposed to all vaccines, while others discussed “religious reasons” without specifying a religion or a group. Religious beliefs were usually linked to refusal of all vaccines, except in one country, where there were specific problems of acceptance of the HPV vaccine among Catholic groups. Other groups in which vaccine hesitancy was encountered included ethnic or indigenous groups, people of higher socioeconomic status, well-educated people and people living in urban areas. One IM indicated that the older generation was more hesitant than the younger generation, and another found that women were more hesitant than men.
The actual problem is vaccine refusal due to religious beliefs. This religion is apostolic. They are reluctant to bring their children to the hospital [for immunization] (Country B).
The role of influential leaders in increasing vaccine hesitancy among the population was noted by six IMs. These leaders were associated with anti-vaccination groups, religious groups or health professional groups.
A Catholic pro-life group started the rumour that the TT administered to pregnant women only contained a contraceptive hormone that stimulates the body to produce antibodies that results to abortion or allegedly infertility in women (Country L).
Causes of vaccine hesitancy linked to the “communication and media environment” were identified by five IMs. Two IMs spoke broadly about “rumours and misconceptions” regarding vaccination circulating in their country and three directly identified negative information conveyed in the mass media (television and internet) as causes of vaccine hesitancy.
The second important thing is all the internet stories. The internet is a useful thing for everybody, even for us, it is much easier to get information, but not always appropriate information. And there are a lot of stories about adverse events following immunization (Country H).
Geographic barriers were identified by six IMs as factors in reducing access to vaccination services, but the association with vaccine hesitancy was not clear. In one country, political conflicts and instability leading to poverty, internal population displacements and insecurity, could partially explain vaccine hesitancy.
It is easier to mobilize the vaccination team than the population, who are only coming little by little to the clinic. The problem of distance is the programs responsibility (Country M).
Finally, in one country, vaccine hesitancy was seen mainly among illegal settlers or immigrants without an official status. These individuals hesitated to use health services because of fear of being reported to the police, even though the Expanded Programme on Immunization (EPI) offers immunization with permission from the government.
The main reason for vaccine hesitancy is living illegally in the country so that theydo not seek or benefit from EPI service at Public Health Clinic in order not to be reported to police (Country D).
3.3.2. Individual and group influences
Three main determinants of vaccine hesitancy pertaining to individual and group influences were identified.
Risk perceptions were identified by seven IMs as causal factors. This included concerns regarding vaccine safety, lack of perceived benefits of vaccination and lack of understanding of the burden of vaccine-preventable diseases.
The new vaccine that we have recently introduced in the country was the DTap, Hepatitis B, Hib-containing pentavalent vaccine and concerns were raised around the safety of this combined vaccine (Country C).
There were certain groups that were very concerned about the safety of vaccines, in particular thimerosal-containing vaccines (Country K).
People's level of trust in the health system and health-care providers was identified by four IMs as a causal factor. One noted that the way people were treated in the health services could discourage them from returning, while another highlighted the fact that some religious groups were reluctant to bring their children to the hospital. In one country, women prefer to receive care from female providers, who are scarce in that country, and this could at least partially explain the lack of vaccination among women.
Women find it more difficult to access services, mainly because of the socio-norms that they need somebody to travel with them if they need to get health care. And they like to be seen by female health-care providers, who are not available in many health facilities, neither in sufficient number, nor with needed qualifications (Country E).
Lack of knowledge (or misinformation) in the population regarding vaccination was identified by four IMs as a contributing factor in vaccine hesitancy.
Reasons for this are that they are not properly informed or have fever following vaccination. These non-serious adverse events after immunization are misperceived by the population (Country C).
Further the families, in particular the fathers, need to be educated about the adverse events following immunization as they prohibit the mothers going back to the health clinic for consecutive doses if the child develops mild fever after vaccination (Country J).
3.3.3. Vaccine- and vaccination-specific factors
Risk of adverse events following vaccination was identified by three IMs as contributing to vaccine hesitancy.
Vaccine hesitancy is related to the report on the cluster of adverse events after immunization, inflammation at the site of injections. Investigation was done and immunization safety practices were strengthened and information dissemination on the safety of the vaccine was intensified. However, major vaccine hesitancy was still related to the vaccine (Country L).
The design of the vaccination programme was identified as a contributory factor by three IMs. In two countries, vaccine hesitancy was related to mass vaccination programmes but not to routine immunization programmes. In the other country, members of a religious group were refusing to bring their children to the hospital or health centres for immunization but agreed to have them immunized if offered at home.
They made seven mass vaccination campaigns in the past and that caused a lot of problems. Particularly, vaccine hesitancy was observed during those mass campaigns (…). Routine immunization was not affected by vaccine hesitancy (Country A).
Lack of knowledge about vaccination among health professionals was specified by two IMs as being linked to vaccine hesitancy in the population.
The lack of knowledge of their own doctors who are not updated and are not familiar with the updated information. Understanding leads to a change in attitude. If they [the doctors] do not have the updated information they will continue with the teachings of the old school (Country M).
Reliability of the vaccine supply was also noted as a difficulty in one country; because vaccines were out of stock, vaccination series were not completed. In another country, the provenance of the vaccines was linked to vaccine hesitancy; there was distrust of vaccines produced in developing countries (India and Indonesia) caused vaccine hesitancy among health-care workers who would prefer to use vaccines produced in Europe. In two countries, IMs noted that there were concerns among the Muslim population due to suspected use of porcine components in vaccines. Finally, introduction of new vaccines or new indications was perceived (more or less explicitly) as contributing to vaccine hesitancy in four countries. In one country, the introduction of new and costly vaccines was seen as triggering vaccine hesitancy.
The country will soon introduce PCV, and this may be a new reason for people to hesitate and for those who do not believe in vaccines to voice their opinions and be active against vaccination (Country F).
4. Discussion
This study revealed a number of challenges concerning vaccine hesitancy, starting with discrepancies in how the term was understood and interpreted by IMs. It was not consistently defined and several IMs interpreted it, explicitly or implicitly, as limited only to vaccine refusal. Several noted stock outs as a cause. Yet the definition developed by the Working Group specifies that vaccine hesitancy refers to delay in acceptance or refusal of vaccines despite availability of vaccine services. This indicates that the proposed definition, while broad and inclusive, will need to be promoted among IMs if vaccine hesitancy is to be comparably assessed in different settings
Some IMs considered the impact of vaccine hesitancy on immunization programmes to be a minor problem, possibly due to their interpretation of the terminology. The findings when questioned about lack of confidence in vaccination well illustrate the problem. The IMs all struggled when asked to provide an estimate of the percentage of non-vaccinated and under-vaccinated individuals in their countries for whom lack of confidence was a factor. This could be related to difficulty in quantifying such a variable and/or to lack of clarity and understanding of the term “lack of confidence” in this context.
The findings show that vaccine hesitancy was not restricted to any specific region or continent but exists worldwide. While some IMs considered the impact of vaccine hesitancy on immunization programmes to be a minor problem in their country, for others it was more serious. Although some IMs associated vaccine hesitancy with particular religious or ethnic groups, most agreed that vaccine hesitancy is not limited to specific communities, and exists across all socioeconomic strata of the population. Some IMs associated it with highly educated individuals, which is in agreement with previous studies in different settings showing that non-compliant individuals often appear to be well-informed people who have considerable interest in health-related issues and actively seek information [12], [13]. Two IMs emphasized that health professionals may themselves be vaccine-hesitant. This is of particular concern as health professionals’ knowledge and attitudes about vaccines have been shown to be an important determinant of their own vaccine uptake, their intention to recommend vaccines to their patients, and the vaccine uptake of their patients [14], [15], [16], [17].
The observation that vaccine hesitancy is not uniform throughout the country reveals another challenge. IMs may need not only to carry out a country assessment of hesitancy, but also a subnational and even a district level assessment, to fully understand the extent of the phenomenon within a country. This will be particularly important when planning for supplementary immunization activities, surveys, or specific campaigns to catch up the non-vaccinated or under-vaccinated, for which vaccine-hesitant persons could be selected as a specific target group.
Overall, the findings fit well within the matrix of determinants of vaccine hesitancy developed by the SAGE Working Group and no additional determinants were identified. The IMs noted variable and context-specific causes of vaccine hesitancy. Confidence, complacency and/or confidence issues were all raised during the interviews. Frequently identified determinants included concerns regarding vaccine safety, sometimes due to scientifically proven adverse events after vaccination or else triggered by rumours, misconceptions or negative stories conveyed in the media. Religious beliefs and the influence of religious leaders was another frequently identified determinant; refusal of some or all vaccines among some religious communities has been well-documented [18], [19]. The influence of communication and media, lack of knowledge or education, and the mode of vaccine delivery (i.e. mass vaccination campaigns) were other determinants identified by IMs. In low and middle income countries, causal factors included geographic barriers to vaccination services, political conflicts and instability, and illegal immigration.
This study is the first to report on how IMs understand and interpret the term vaccine hesitancy and has provided useful insights on the current situation in different countries and settings, showing the variability in manifestation of vaccine hesitancy and its impact on immunization programmes. However, the results should be considered in light of some limitations. The countries were selected by WHO in order to represent a diversity of regions and situations, but it was difficult to obtain the participation of some countries. Two IMs could not participate for different reasons. Most interviews were conducted in English and this may have been challenging for non-English speakers, resulting in information bias. Interviews were loosely conducted and some questions were not posed to every IM. As with any qualitative study, desirability bias cannot be excluded, nor can the findings be extrapolated to all countries. It should be noted that the country-specific situation was reported by a single IM, essentially based on his/her own opinions and estimations. Although IMs are generally very well-informed on issues surrounding vaccination, it is thus very possible that different views might have been expressed if another informant had been interviewed in the same country. Finally, although most of the research on vaccine hesitancy is conducted in high income countries [5], the majority of IMs interviewed in this study were from low and middle income countries. Indeed, the results could have differed if more IMs from high income countries had been interviewed, as they may be more aware of vaccine hesitancy and its determinants because this field of research is more developed in those countries. The choice of countries also limited the possibility of assessing differences in the perspective of IMs between regions and economic categories.
To conclude, understanding the specific concerns of the various groups of vaccine-hesitant individuals, including health professionals, is important as hesitancy may result in vaccination delays or refusals. Vaccine hesitancy is an individual behaviour, but is also the result of broader societal influences and should always be looked at in the historical, political and socio-cultural context in which vaccination takes place. The results of this study will be used by the SAGE Working Group on vaccine hesitancy in preparing its recommendations to the SAGE, which will then consider potential global health policy implications. The findings highlight the need to ensure that health professionals and those involved in immunization programmes are well informed about vaccine hesitancy and are able to identify and address its determinants. There is a need to strengthen the capacity of countries to identify the context-specific roots of vaccine hesitancy and to develop adapted strategies to address them.
Acknowledgements
We thank the participating national IMs and WHO staff at the regional and national offices for arranging the interviews. We also thank the members of the SAGE Working Group on vaccine hesitancy and the WHO SAGE secretariat for their contribution in the design of the study and interpretation of the results: Mohuya Chaudhuri, Philippe Duclos, Bruce Gellin, Susan Goldstein, Juhani Eskola, Heidi Larson, Xiaofeng Liang, Noni MacDonald, Mahamane Laouli Manzo, Arthur Reingold, Dilian Francisca Toro Torres, Kinzang Tshering and Yuqing Zhou. This study was sponsored by the World Health Organization.
Conflict of interest statement
Nothing to declare.
References
- 1.Benin A.L., Wisler-Scher D.J., Colson E., Shapiro E.D., Holmboe E.S. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117(5):1532–1541. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 2.Opel D.J., Taylor J.A., Mangione-Smith R., Solomon C., Zhao C., Catz S. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29:6598–6605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Meeting of the Strategic Advisory Group of Experts on Immunization, April 2013—Conclusions and Recommendations. Weekly Epidemiological Record 2013;88, 201–16.
- 4.The SAGE Vaccine Hesitancy Working Group. SAGE working group dealing with vaccine hesitancy (established March 2012). Available from: 〈http://www.who.int/immunization/sage/sage_wg_vaccine_hesitancy_apr12/en/index.html〉.
- 5.Larson H.J., Jarrett C., Eckersberger E., Smith D.M., Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 6.The SAGE Vaccine Hesitancy Working Group. What influences vaccine acceptance: A model of determinants of vaccine hesitancy; 2013 [cited November 6th, 2013]. Available from: 〈http://www.who.int/immunization/sage/meetings/2013/april/1_Model_analyze_driversofvaccineConfidence_22_March.pdf〉.
- 7.International Association of Immunization Managers, The role of immunization managers. 〈http://www.iaimanagers.org/〉 [page accessed 14.07.14].
- 8.Larson H.J., Cooper L.Z., Eskola J., Katz S.L., Ratzan S. Addressing the vaccine confidence gap. Lancet. 2011;378(9790):526–535. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
- 9.Morse J.M., Field P.A. 2nd ed. SAGE Publications Inc.; Thousand Oaks, CA: 1995. Qualitative research methods for health professionals; p. 254. [Google Scholar]
- 10.Wolcott H.F. AltaMira Press; Walnut Creek, CA: 1999. Ethnography: a way of seeing; p. 335. [Google Scholar]
- 11.World Bank List of Economies as of Nov 19 [cited 19.11.13]. Available from: 〈http://worldbank_level_of_income.com〉.
- 12.Burton-Jeangros C., Golay M., Sudre P. Compliance and resistance to child vaccination: a study among Swiss mothers. Rev Epidemiol Sante Publique. 2005;53(4):341–350. doi: 10.1016/s0398-7620(05)84616-4. [DOI] [PubMed] [Google Scholar]
- 13.Cassell J.A., Leach M., Poltorak M.S., Mercer C.H., Iversen A., Fairhead J.R. Is the cultural context of MMR rejection a key to an effective public health discourse? Public Health. 2006;120(9):783–794. doi: 10.1016/j.puhe.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Clark S.J., Cowan A.E., Wortley P.M. Influenza vaccination attitudes and practices among US registered nurses. Am J Infect Control. 2009;37(7):551–556. doi: 10.1016/j.ajic.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Hollmeyer H.G., Hayden F., Poland G., Buchholz U. Influenza vaccination of health care workers in hospitals—a review of studies on attitudes and predictors. Vaccine. 2009;27(30):3935–3944. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 16.Posfay-Barbe K.M., Heininger U., Aebi C., Desgrandchamps D., Vaudaux B., Siegrist C.A. How do physicians immunize their own children? Differences among pediatricians and nonpediatricians. Pediatrics. 2005;116(5):e623–e633. doi: 10.1542/peds.2005-0885. [DOI] [PubMed] [Google Scholar]
- 17.Katz-Sidlow R.J., Sidlow R. A look at the pediatrician as parent: experiences with the introduction of varicella vaccines. Clin Pediatr (Phila) 2003;42(7):635–640. doi: 10.1177/000992280304200710. [DOI] [PubMed] [Google Scholar]
- 18.Streefland P.H. Public doubts about vaccination safety and resistance against vaccination. Health Policy. 2001;55(3):159–172. doi: 10.1016/s0168-8510(00)00132-9. [DOI] [PubMed] [Google Scholar]
- 19.Ruijs W.L., Hautvast J.L., van Ijzendoorn G., van Ansem W.J., van der Velden K., Hulscher M.E. How orthodox protestant parents decide on the vaccination of their children: a qualitative study. BMC Public Health. 2012;12:408. doi: 10.1186/1471-2458-12-408. [DOI] [PMC free article] [PubMed] [Google Scholar]