Abstract
Objective: To determine the effects of functional fatigue on active multijoint position reproduction in overhead-throwing athletes.
Design and Setting: A standard, repeated-measures, randomized-ordered, counterbalanced, 2-period (crossover) design was used. During the first test session, we randomly assigned subjects to either the nonfatigue or fatigue condition. Subjects underwent pretest measurements and then either a functional fatigue protocol or rest period, followed by posttest measurements. After a recovery period, subjects crossed over to the opposing condition for the second testing session.
Subjects: Thirteen overhead-throwing athletes competing in National Collegiate Athletic Association Division I or club baseball, with no history of upper extremity or central nervous system disorders, volunteered for this study.
Measurements: We measured active multijoint position reproduction accuracy in 3 dimensions using an electromagnetic tracking device. We noted each subject's ability to reproduce 3 positions corresponding with distinct moments of his throwing motion. A variable error score was calculated to compare the locations of the reproduced points with reference to the target point.
Results: A significant difference occurred between the pretest and posttest error scores in the fatigue condition. Comparisons between positions indicated that more errors were seen in the arm-cocked position than in the follow-through position under both fatigue and nonfatigue conditions.
Conclusions: Functional fatigue decreased joint position sense acuity in overhead-throwing athletes. Our findings using this novel testing measurement method are in agreement with past research, with one exception. The trend toward higher error scores in the arm-cocked position would appear to contradict findings that sensorimotor system acuity increases toward end ranges of motion.
Keywords: joint position sense, 3-dimensional motion analysis
The sensorimotor system is responsible for the body's coordination and stability and is a major component of function and performance in athletic activity.1–3 Proper function of the sensorimotor system is essential for injury-free athletics, especially with complex motor activities such as overhead throwing.4 Fatigue decreases sensorimotor system function5–8 and may predispose the athlete to injury. Research models that have been used to investigate the effects of fatigue on the sensorimotor system have commonly employed a single-joint and single-plane measure of joint position sense (JPS), typically after an isokinetic-type fatiguing protocol testing focused on single-joint and single-plane motions.1,3,5–11 However, the physiologic and biomechanical effects of the fatigue accompanying a functional activity may not be accurately simulated by isokinetic fatigue protocols. Additionally, athletic activities such as the overhead throw require multiple joints and take place in multiple planes. Hence, the findings of previous studies may have limited application with regard to functional, multidirectional movement, such as that seen in the overhead-throwing population.
Recent investigations into fatigue of the upper extremity have shown that fatigue has negative effects on sensorimotor system function and acuity.5–9 The shoulder,2,12 elbow,13 and hand11 have shown the ability to reorganize muscle activity patterns with fatigue.14 The shoulder's reorganization strategy is believed to combat overload of specific muscles, minimize fatigue, and postpone exhaustion.14,15 In complex kinetic chain movements, such as throwing, this reorganization of multiple joint angles or muscle firing patterns may compensate for fatigue of one muscle or synergistic muscles. Upper extremity sensorimotor system studies have historically been confined to single-joint and single-plane motions: either the sagittal5,6,8,14 or horizontal (transverse) planes,7 with subjects' JPS error scores calculated in the same plane. In such studies, the body's normal biomechanics as well as natural alterations and reorganizations of muscle firing patterns are, if not prohibited, severely restricted.
To date, the effects of fatigue from a multijoint and multiplanar activity on sensorimotor system function using 3-dimensional acuity of active joint reposition sense have not been definitively investigated. Therefore, the purpose of our study was to determine the effects of functional fatigue on multijoint position reproduction in the overhead-throwing athlete using a 3-dimensional sensorimotor system testing method.
METHODS
Design and Setting
To decrease the influence of individual subject differences, we used a standard, repeated-measures design. We implemented a 2-period, crossover, counterbalanced design to minimize learning effects and biasing of test sequence. During the first test session, we randomly assigned subjects to either the nonfatigue or fatigue condition. After a recovery period, subjects were crossed over to the opposing condition for the next testing session.
Subjects
Subjects were 13 overhead-throwing athletes competing in National Collegiate Athletic Association Division I (n = 7) or club baseball (n = 6). Healthy subjects (age = 20.0 ± 1.7 years, height = 180.7 ± 3.8 cm, mass = 82.9 ± 4.7 kg) with no history of upper extremity injury or abnormality or central nervous system disorder participated in this study. Subjects included 3 pitchers, 2 catchers, 4 infielders, and 4 outfielders, with 13.3 ± 1.36 years of baseball experience. Before participating, all subjects read and signed an informed consent form and received verbal instructions for the testing and fatigue protocols as approved by the University of Virginia's Institutional Review Board for the Social and Behavioral Sciences.
Instrumentation
We measured active multijoint position reproduction (AMPR) using the Flock of Birds (FOB) electromagnetic tracking device (Ascension Technology, Burlington, VT) with the default settings of 40 Hz, AC wide filter on, and DC low-pass filter on and a 4th-order Butterworth filter. This instrumentation measures the relation of points in 3-dimensional space. We calculated a 3-dimensional variable error score by comparing a target point location and the reproduced point location in the horizontal, vertical, and transverse planes (x, y, and z, respectively) with respect to a reference point.16,17 The error score represents a single measure of the 3-dimensional dispersion between the 2 points.
Procedures
Using the AMPR test, we compared pretest and posttest joint reposition-sense measurements. At each testing session, we measured subjects' pretest AMPR accuracies in 3 arm positions through the throwing arc. The fatigue-condition participants then performed a functional fatigue protocol consisting of a throwing program, after which we measured AMPR accuracy a second time in the same manner. Non-fatigue–condition members underwent the same procedures as fatigue-condition participants, with the exception of a 5-minute waiting period in place of the throwing protocol.
Active Multijoint Position Reproduction Measure
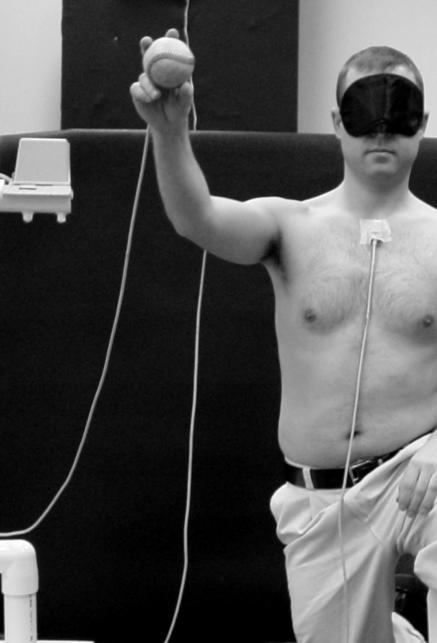
We tested subjects in a single-knee stance position, standardized as follows: kneeling with the nondominant hip at 90° and the foot placed flat on the ground in front of the subject, throwing the dominant-side knee on the ground (Figure 1). We instructed subjects to rotate their trunks as needed but to maintain 90° angles at both knees. We taped the electromagnetic system reference leads to the participants at the sternal notch, deltoid tuberosity of the humerus, and third metacarpal of the dominant arm. We blindfolded subjects and tested their ability to reproduce 3 specific, self-determined positions that corresponded with 3 distinct moments of the throwing motion.
Figure 1. Standard test position: kneeling with the nondominant hip at 90° and the foot placed flat on the ground in front of the subject, with the knee on the side of the throwing shoulder on the ground.
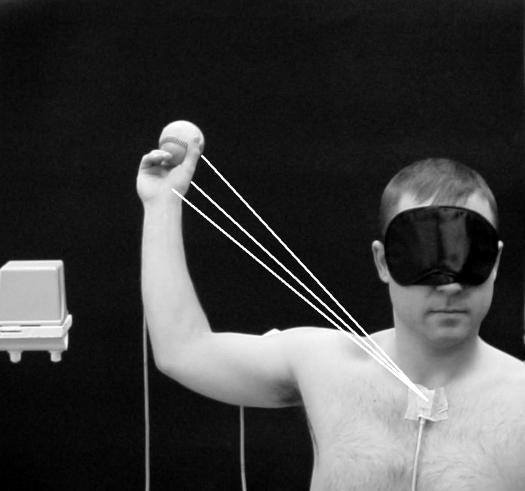
For the first position, subjects were instructed to hold the arm-cocked position at which forward acceleration of the arm would begin. They determined the second position by finding and holding the ball-release point. Participants established the final position in the same manner, holding the finishing point or follow-through position. Subjects then practiced the testing procedure once by moving through the throwing motion, pausing, and verbally indicating when they believed the extremity was in the first position. For the first recorded trial, the subject went through the throwing motion, stopping at position 1, while the FOB recorded the position for 5 seconds. The position of the hand sensor (in reference to the thorax) during the initial trial represented the target position for the following 3 trials. The position that each subject identified was used as a target only for that specific test condition. Subjects identified new target positions at the beginning of each testing period (ie, 1 set for pretest and another set for posttest under each condition). We used this method of subject-selected targets to control for any decay in recall over time and any changes in the position identified over time. These methods only required subjects to replicate positions they identified 4 to 10 seconds earlier. After identification of the target positions, participants replicated each position 3 times. The average of the latter 3 trials' dispersion from the target location (in cm) served as the subject's error score for that position (Figure 2). Subjects repeated these procedures for the second (ball-release) position and finally the third (follow-through) position.
Figure 2. Error scores for each position, calculated as dispersion from the end point to the target position.
Functional Fatigue
The functional fatigue protocol consisted of an overhead-throwing program in the single-knee stance position. We removed the FOB leads and marked their locations. Participants used a standard baseball (circumference = 9 in [22.86 cm], mass = 5 oz [0.16 kg], Rawlings Sporting Goods Co, Inc, St Louis, MO), and faced a target 20 ft [6.10 m] away. Before beginning, participants underwent a 5-minute throwing warm-up, followed by the determination of their maximum throwing velocity. We calculated maximum velocity as the mean velocity of the 5 throws recorded using a JUGS radar gun (JUGS Pitching Machine Co, Tualatin, OR).
During the throwing program, investigators required subjects to throw each ball with maximum velocity every 5 seconds until they reached fatigue. We instructed subjects to maintain 90° of flexion at the forward hip and both knees. We prompted subjects during the protocol as needed to maintain these angles. These methods were chosen to maintain continuity between the testing and fatigue-protocol positions, limit the contribution of the lower extremity to force production, and further challenge the upper extremity. In order to ensure maximal effort, we prompted subjects when their velocity of throws fell below 90% of maximum velocity. Each subject rated the local (upper extremity) exertion level on the Borg Rating of Perceived Exertion (RPE) scale18 after every 20 throws. We considered subjects fatigued when they reported an exertion level of 15 or above. This technique has been used to measure local fatigue as opposed to systemic or overall fatigue.19 The local upper extremity RPE rating of 15 on a scale of 6 to 20 has been reported to be highly correlated with the metabolic responses of fatigue, including respiratory exchange, heart rate, absolute oxygen consumption, and blood lactate.20
Participants assigned to the nonfatigue condition performed the pretest, waited 5 minutes, and performed the posttest in the same manner. We asked them to return later the same day (6.1 ± 1.7 hours) for retesting under the opposite condition.
Data Reduction and Statistical Analysis
To compare differences in the pre- and posttest AMPR accuracy, we calculated a 3-dimensional variable error score, defined as a global standard deviation of end-position dispersions using the following equation16,17:
| 3-dimensional variable error score >= ([SD(dx)]2 + [SD(dy)]2 + [SD(dz)]2}1/2 |
The dx, dy, and dz are differences (in cm) between the coordinates of the target and final position in the x axis (anterior-posterior direction), the y axis (vertical direction), and the z axis (lateral direction), respectively.16 The data were entered and analyzed in SPSS (version 10.0; SPSS Inc, Chicago, IL). We performed a repeated-measures analysis of variance with 3 within-group factors (condition at 2 levels, fatigue and nonfatigue; time at 2 levels, pretest and posttest; and position at 3 levels, arm cocked, ball release, and follow through). Statistical significance for all comparisons was set a priori at P < .05.
RESULTS
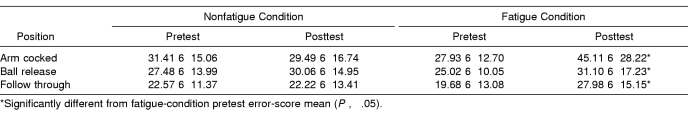
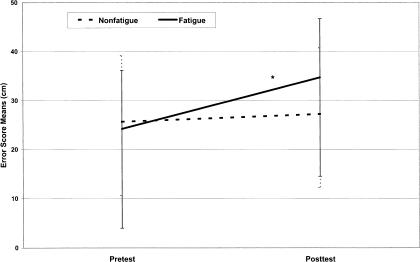
Subjects completed the fatigue protocol, reaching or exceeding 15 on the RPE scale, reporting “hard/heavy work or strain and fatigue on muscles” after 61.5 ± 15.1 throws. Error-score means and standard deviations for both the fatigue and nonfatigue conditions are listed in the Table. A 3-way repeated-measures analysis of variance revealed no significant interaction for condition × time × position (F2,24 = 1.078, P = .356). We observed a significant condition × time interaction (F1,12 = 5.194, P = .042), with this increase being attributed to the fatigue condition (Figure 3). On average, error scores increased (10.5 ± 8.3) from pretest to posttest in the fatigue condition, while there was no difference (0.1 ± 1.6) pretest to posttest in the control condition. No time × position interaction was noted for the fatigue condition (F2,24 = 1.078, P = .35, β = .216). However, a statistically significant main effect for position was demonstrated (F1,12 = 5.991, P = .008). Pairwise comparisons with a Bonferroni correction indicated errors were not statistically different between the arm-cocked and ball-release positions (P = .42), but the arm-cocked position produced significantly higher error scores than the follow-through position (P = .02). These differences by arm position were not affected by time (F2,24 = 0.423, P = .66) or condition (F2,24 = 0.813, P = .45), indicating that the differences were similar at pretest and posttest and in the fatigue and nonfatigue conditions. We observed no other statistically significant pairwise differences.
Pretest and Posttest 3-Dimensional Variable Error Scores (cm) Measured at 3 Static Positions in Nonfatigue and Fatigue Conditions.
Figure 3. Pretest and posttest mean error scores (cm) for the nonfatigue and fatigue conditions.
* Significantly different from nonfatigue condition
DISCUSSION
Our purpose was to determine if functional fatigue had a significant effect on sensorimotor system function. Our primary findings indicate that functional fatigue decreased sensorimotor system acuity in the overhead-throwing athlete as measured by the AMPR test. The general observation that fatigue decreases sensorimotor system acuity is in agreement with previous literature.5,6,8 These findings support the dysfunctional mechanoreceptor theory proposed by Voight et al,5 in which muscle fatigue is believed to desensitize muscle spindle thresholds. This desensitization would serve to decrease afferent feedback to the central nervous system.5 Proposed mechanisms for this include local metabolism interfering at the muscular level,7,8,21–24 central nervous system fatigue, and neuromuscular fatigue.8,25
It is important to note that our findings reflect JPS acuity of the upper extremity as a whole. Our measurement technique, however, did not allow us to identify specific sources of reproduction error. Our findings nonetheless raise questions regarding the effects of individual joints on JPS acuity of the entire chain. We observed less JPS acuity in the arm-cocked position (position 1) compared with the ball-release and follow-through positions. However, previous authors specifically investigating the shoulder joint reported JPS improved toward the end ranges of motion in positions such as the arm-cocked position.3,6,8 Researchers postulated that increased JPS is enabled by enhanced afferent input provided by the tightening and maximal deformation of the joint capsule as the glenohumeral joint moves toward full external rotation.3,6,8 Our observations would, therefore, indicate that, although the shoulder joint itself has enhanced JPS in the arm-cocked position, JPS acuity of the extremity as a whole is not improved when compared with the other 2 positions. The integration of our results into the literature underscores the importance of gaining a better understanding of how the JPS of individual joints affects overall upper extremity JPS.
The ostensible inconsistencies between our findings and the previous literature may be accounted for by examining the differences in testing methods. We used a functional fatigue protocol as opposed to isokinetic fatigue protocols.5–8,11 Also, our measure of JPS incorporated multiple joints measured in 3 dimensions rather than a single joint measured in a single plane.5–8 Our functional fatigue protocol incorporated throwing, which is a multijoint, coordinated ballistic motion that has shown kinematic changes in response to fatigue.14 The dynamic alterations in multijoint interactions during the functional fatigue protocol elude the confined nature of isokinetic protocols. The unique nature of our multijoint, 3-dimensional testing measures may have allowed us to observe higher error scores in the arm-cocked position. The unconfined and self-determined nature of the AMPR test is in stark contrast with the single-joint and single-plane testing methods commonly employed.1,3,5–11 Our measure of endpoint reproduction acuity across multiple joints does, however, bear limitations. Because we are unable to determine JPS acuity for each individual joint, we can only conclude that changes occur over the upper extremity kinetic chain as a whole. Additionally, our findings are only applicable to healthy, college-aged male baseball players.
Clinical Relevance
The observation that functional fatigue decreases JPS acuity over multiple joints is important for preventing injuries and rehabilitating overhead-throwing athletes. Clinicians should stress careful monitoring of prolonged overhead athletic or rehabilitative activity for both subjective reports and observable signs of fatigue. Our results indicate the presence of sensorimotor system deficits in conjunction with a fatigued state. These deficits are proposed to contribute to overuse injury and subtle instability26; thus, athletes should be monitored during bouts of prolonged training to avoid these deficits.
The unique finding that errors were significantly greater in the arm-cocked position as compared with the ball-release and follow-through positions raises clinical concern for the overhead-throwing population. Many athletes suffer from impingement syndromes attributed to microinstability in this position.27 During conditions of sensorimotor system deficit, lack of dynamic stability may increase stress placed on the static and dynamic joint stabilizers. This paradigm, originally described by Lephart and Henry,26 may lead to injury and the progressive decline of the joint. Clinicians develop and implement many exercises that aim to increase sensorimotor system acuity in rehabilitation or prophylactic programs. Because few sensorimotor system exercises employ multijoint training methods,1,4 it is important to understand that these sensorimotor system deficits are taking place during multijoint motions. Future research is needed, however, to evaluate the efficacy of such sensorimotor system training protocols. In addition, further investigation is needed to determine the roles both fatigue and the sensorimotor system play in pathophysiology in overhead-throwing athletes.
CONCLUSIONS
Functional fatigue decreased JPS in overhead-throwing athletes as measured by the AMPR test. We were able to observe, quantify, and compare these deficits in functional upper extremity positions. Additional research examining functional multijoint motions is warranted to compare JPS among planes of motion within individual joints and to compare JPS among the joints contributing to the kinetic chain.
REFERENCES
- Lephart SM, Riemann BL, Fu FH. Champaign, IL: Human Kinetics; 2000. Proprioception and Neuromuscular Control in Joint Stability. [Google Scholar]
- Chen SK, Simonian PT, Wickiewicz TL, Otis JC, Warren RF. Radiographic evaluation of glenohumeral kinematics: a muscle fatigue model. J Shoulder Elbow Surg. 1999;8:49–52. doi: 10.1016/s1058-2746(99)90055-1. [DOI] [PubMed] [Google Scholar]
- Safran MR, Borsa PA, Lephart SM, Fu FH, Warner JJ. Shoulder proprioception in baseball pitchers. J Shoulder Elbow Surg. 2001;10:438–444. doi: 10.1067/mse.2001.118004. [DOI] [PubMed] [Google Scholar]
- Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–137. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- Voight ML, Hardin JA, Blackburn TA, Tippett S, Canner GC. The effects of muscle fatigue on and the relationship of arm dominance to shoulder proprioception. J Orthop Sports Phys Ther. 1996;23:348–352. doi: 10.2519/jospt.1996.23.6.348. [DOI] [PubMed] [Google Scholar]
- Carpenter JE, Blasier RB, Pellizzon GG. The effects of muscle fatigue on shoulder joint position sense. Am J Sports Med. 1998;26:262–265. doi: 10.1177/03635465980260021701. [DOI] [PubMed] [Google Scholar]
- Pedersen J, Lonn J, Hellstrom F, Djupsjobacka M, Johansson H. Localized muscle fatigue decreases the acuity of the movement sense in the human shoulder. Med Sci Sports Exerc. 1999;31:1047–1052. doi: 10.1097/00005768-199907000-00019. [DOI] [PubMed] [Google Scholar]
- Myers JB, Guskiewicz KM, Schneider RA, Prentice WE. Proprioception and neuromuscular control of the shoulder after muscle fatigue. J Athl Train. 1999;34:362–367. [PMC free article] [PubMed] [Google Scholar]
- Brindle TJ, Nyland J, Shapiro R, Caborn DN, Stine R. Shoulder proprioception: latent muscle reaction times. Med Sci Sports Exerc. 1999;31:1394–1398. doi: 10.1097/00005768-199910000-00006. [DOI] [PubMed] [Google Scholar]
- Allegrucci M, Whitney SL, Lephart SM, Irrgang JJ, Fu FH. Shoulder kinesthesia in healthy unilateral athletes participating in upper extremity sports. J Orthop Sports Phys Ther. 1995;21:220–226. doi: 10.2519/jospt.1995.21.4.220. [DOI] [PubMed] [Google Scholar]
- Hagbarth KE, Bongiovanni LG, Nordin M. Reduced servocontrol of fatigued human finger extensors and flexors. J Physiol. 1985;485:865–872. doi: 10.1113/jphysiol.1995.sp020776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen BR, Sogaard K, Hargens A. Dissociation between intramuscular pressure and EMG during prolonged submaximal contraction. Acta Physiol Scand. 1995;115:12A–C10. [Google Scholar]
- Miles MP, Ives JC, Vincent KR. Neuromuscular control following maximal eccentric exercise. Eur J Appl Physiol Occup Physiol. 1997;76:368–374. doi: 10.1007/s004210050263. [DOI] [PubMed] [Google Scholar]
- Forestier N, Nougier V. The effects of muscular fatigue on the coordination of a multijoint movement in human. Neurosci Lett. 1998;252:187–190. doi: 10.1016/s0304-3940(98)00584-9. [DOI] [PubMed] [Google Scholar]
- Bente J, Bjarne L, Sjogaard G. Aspects of shoulder function in relation to exposure demands and fatigue: a mini review. Clin Biomech. 2000;15:S17–S20. doi: 10.1016/s0268-0033(00)00054-1. [DOI] [PubMed] [Google Scholar]
- Poizner H, Fookson OI, Berkinblit MB, Hening W, Feldman G, Adamovich S. Pointing to remembered targets in 3-D space in Parkinson's disease. Motor Control. 1998;2:251–277. doi: 10.1123/mcj.2.3.251. [DOI] [PubMed] [Google Scholar]
- Adamovich SV, Berkinblit MB, Fookson O, Poizner H. Pointing in 3D space to remembered targets, I: kinesthetic versus visual target presentation. J Neurophysiol. 1998;79:2833–2846. doi: 10.1152/jn.1998.79.6.2833. [DOI] [PubMed] [Google Scholar]
- Borg G. Champaign, IL: Human Kinetics; 1998. Borg's Perceived Exertion and Pain Scales. [Google Scholar]
- Pandolf KB, Billings DS, Drolet LL, Pimental NA, Sawka MN. Differential ratings of perceived exertion and various physiological responses during prolonged upper and lower body exercise. Eur J Appl Physiol Occup Physiol. 1984;53:5–11. doi: 10.1007/BF00964681. [DOI] [PubMed] [Google Scholar]
- Edwards RH, Melcher A, Hesser CM, Wigertz O, Ekelund LG. Physiological correlates of perceived exertion in continuous and intermittent exercise with the same average power output. Eur J Clin Invest. 1972;2:108–114. doi: 10.1111/j.1365-2362.1972.tb00578.x. [DOI] [PubMed] [Google Scholar]
- Skinner HB, Wyatt MP, Hodgdon JA, Conard DW, Barrack RL. Effect of fatigue on joint position sense of the knee. J Orthop Res. 1986;4:112–118. doi: 10.1002/jor.1100040115. [DOI] [PubMed] [Google Scholar]
- Djupsjobacka M, Johansson H, Bergenheim M, Wenngren BI. Influences on the gamma-muscle spindle system from muscle afferents stimulated by increased intramuscular concentrations of bradykinin and 5-HT. Neurosci Res. 1995;22:325–333. doi: 10.1016/0168-0102(95)00906-a. [DOI] [PubMed] [Google Scholar]
- Djupsjobacka M, Johansson H, Bergenheim M, Sjolander P. Influences on the gamma-muscle-spindle system from contralateral muscle afferents stimulated by KCl and lactic acid. Neurosci Res. 1995;21:301–309. doi: 10.1016/0168-0102(94)00864-c. [DOI] [PubMed] [Google Scholar]
- Djupsjobacka M, Johansson H, Bergenheim M. Influences on the gamma-muscle-spindle system from muscle afferents stimulated by increased intramuscular concentrations of arachidonic acid. Brain Res. 1994;663:293–302. doi: 10.1016/0006-8993(94)91276-9. [DOI] [PubMed] [Google Scholar]
- Powers SK, Howley ET. Dubuque IA: Wm C Brown; 1990. Exercise Physiology: Theory and Application to Fitness and Performance. [Google Scholar]
- Lephart SM, Henry TJ. The physiological basis for open and closed kinetic chain rehabilitation for the upper extremity. J Sport Rehabil. 1996;5:71–87. [Google Scholar]
- Jobe CM. Superior glenoid impingement: current concepts. Clin Orthop. 1996;330:98–107. [PubMed] [Google Scholar]