Abstract
Introduction
Accurate delivery of radiation while reducing dose to organs at risk is essential in prostate treatment. The Calypso motion management system detects and corrects both inter‐ and intra‐fraction motion which offers potential benefits over standard alignment to fiducial markers. The aims of this study were to implement Calypso with Dynamic Edge™ gating and to assess both the motion seen, and interventions required.
Methods
An implementation group was formed which assessed changes needed to standard workflows. Three patients had Calypso beacons inserted into their prostate. All patients were treated using volumetric modulated arc therapy to a dose of 80 Gy in 40 fractions. Standard inter‐fraction motion correction using either kilovoltage (kV) orthogonal paired imaging or cone beam computed tomography (CBCT) image‐guided radiotherapy techniques, were used along with the Calypso system to compare accuracy. A gating threshold of >0.5 cm was used during treatment. Workflow variations along with inter‐ and intra‐fraction motion and interventions required were assessed.
Results
A total of 116 fractions were treated using Calypso with Dynamic Edge™ gating. There was a strong concordance between aligning beacons using kV orthogonal imaging or CBCT and Calypso (mean variation ≤0.06 cm). The mean intra‐fraction motion detected was ≤0.2 cm in all directions with the largest motion recorded being 2.2 cm in the left direction while the treatment beam was off. Prostate rotation was largest in the pitch direction and 28 fractions exceeded the 10° tolerance. A total of 78 couch shift corrections of ≥0.3 cm were required, usually following standard imaging, and before treatment starting. Three gating events due to intra‐fraction motion occurred during treatment.
Conclusions
Intra‐fraction motion monitoring with Calypso was successfully implemented. Greatest movement was seen between time of standard imaging and treatment starting with more than half the treatments requiring a ≥0.3 cm adjustment. This would not have been detected without intra‐fraction monitoring.
Keywords: calypso, implementation, intra‐fraction motion, prostate, radiation treatment
Introduction
A systematic review of literature estimated that approximately 61% of men with prostate cancer will require radiotherapy treatment at some point during their illness.1 Increasing the radiation dose delivered to the prostate has been shown to improve outcomes for patients2, 3 so it is important that the treatment is accurate to allow high doses to be delivered while minimising dose to surrounding organs at risk (OAR).
Calypso with Dynamic Edge™ gating (Varian Medical Systems, Palo Alto, CA) is a motion management system which detects both inter‐ and intra‐fraction motion without delivering any additional radiation dose to the patient. Calypso has additional benefit over standard alignment to fiducial markers because all prostate motion during the treatment is detected and can be corrected to allow accurate treatment and avoidance of OARs.
Calypso requires three electromagnetic transponders or beacons to be implanted into the left base, right base and apex of the prostate. The beacons are 1.85 mm in diameter and 8.7 mm in length and the recommended minimum distance required between each beacon is 10 mm. Each beacon has a different frequency. The centroid of the beacons is used to calculate the position of the prostate during treatment.4
The Calypso system includes a tracking station located in the control area of the treatment machine. Inside the treatment room is a console that is moved into positioned next to the treatment couch. It houses a second tracking station, which is used to set the patient up, and the array that is positioned over the patient during treatment that detects the beacons and therefore prostate position.4
Calypso has been successfully implemented and evaluated in other centres. Kupelian et al.5 conducted a multi‐institutional evaluation of Calypso and found that it was clinically efficient and performed accurately.
The aims of this study were to implement the Calypso motion management system with Dynamic Edge™ gating for definitive prostate patients and assess the motion seen and the interventions required.
Methods
In September 2013, Calypso was implemented into Northern Sydney Cancer Centre (NSCC) as a part of a definitive prostate multileaf collimator (MLC) tracking clinical trial.6 Ethics approval was granted by the Northern Sydney Local Health District Human Research Ethics Committee. The first three patients were treated using Calypso with Dynamic Edge™ gating.
An implementation group was formed that included radiation oncologists (ROs), radiation oncology medical physicists (ROMPs), radiation therapists (RTs), clinical trials staff, and the genitourinary cancer nurse co‐ordinator (GU CNC). This group worked through the changes required to standard workflows.
Patient bladder and bowel preparation for simulation and treatment remained the same for these patients as those being treated with fiducial markers. All patients were treated using volumetric modulated arc therapy (VMAT) to a dose of 80 Gy in 40 fractions using a Trilogy Linear Accelerator (Varian Medical Systems). Dose coverage and OAR constraints remained the same as patients treated with fiducial markers.
Standard online inter‐fraction motion correction for prostate patients at NSCC is completed online daily using an On‐Board Imager (Varian Medical Systems). Matching was to fiducial marker using either cone beam computed tomography (CBCT) imaging (fraction 1, 2, 3 then weekly) or kilovoltage (kV) orthogonal paired (all fraction when not acquiring CBCT) image‐guided radiotherapy (IGRT) techniques. This was continued with the initial Calypso patients, matching to the beacons, to compare accuracy.
During treatment if the prostate moved >0.5 cm, the radiation beam would be gated by the Calypso system until either the prostate moved back into position or the treating RTs determined that the prostate was not going to move back into position and a couch correction was applied remotely to correct the motion. Couch shifts were also applied during Calypso tracking when the treatment beam was off if the movement detected by Calypso in any direction was >0.2 cm.
Statistical analysis was completed to assess both the prostate motion detected and interventions required. The inter‐fraction motion detected by standard IGRT and Calypso was compared. Intra‐fraction motion was assessed for all fractions and any interventions that were required. This was assessed using descriptive statistical analysis. Linear regression analysis was also performed on the geometric residue of the beacons and treatment times. Microsoft Excel (Microsoft Corporation, Redmond, WA) was used to complete the statistical analysis.
Results
The first three patients that were eligible for Calypso beacon implantation were treated using Calypso with Dynamic Edge™ gating. Of the 120 fractions, only 4 fractions (3.33% of all fractions) were not completed using Calypso. For 3 of these fractions, the patients were treated out of hours where the appropriate support staff were unavailable and the other fraction was due to a linear accelerator fault.
Changes in standard workflow
Two main changes needed to be made to the existing pre‐simulation gold fiducial marker workflow. A patient size assessment needed to be completed at the initial consultation to ensure that the Calypso array could remain over the patient during treatment to track the prostate. The GU CNC was trained to take these measurements so the RO could determine if the patient was eligible for Calypso or if gold fiducial markers were to be used instead. The second change was the timing of the magnetic resonance image (MRI) scan that was used for contouring purposes. Traditionally, this scan was taken the same day as the planning simulation computed tomography (CT) scan with the gold fiducial markers in situ. Due to the significant artefact with the electromagnetic transponders on MRI imaging, the MRI was acquired before implantation so the RO had access to a higher quality scan for contouring.
Minor changes were also made to the radiotherapy simulation process. Scanning slice thickness was decreased from 0.2 cm to 0.15 cm to allow for better definition of the Calypso beacons. To ensure that the Calypso array would fit over the patient during treatment, only the low knee block was used during treatment and the hands were placed as high as possible on the patient's chest.
Some changes were required in the planning process. The beacons needed to be contoured individually and reference points placed at the centre of each beacon to calculate their co‐ordinates for use in the Calypso system. The isocentre of the treatment plan needed to be located at the centroid of the three beacons. The beacon co‐ordinates also needed to be exported from the planning system, Eclipse (Version 10, Varian Medical Systems), ready for the treatment staff to import to the Calypso system. The export and import processes were completed by two RTs and/or ROMPs to ensure quality assurance of the process. A KVue™ Calypso IGRT couch with Calypso compatible top (QFix Corporation, Avondale, PA) was also installed. This couch top was different to our standard couch as it had couch rails which can be moved to either the lateral edges or centre of the couch top. These needed to be accounted for during planning to ensure that treatment gantry arc angles avoided the rails. These patients were treated with the bars moved into the central position and the arc angles were selected to avoid treating through the bars. This added no additional time to treatment.
There were a number of changes required to the treatment process when using Calypso. First, the co‐ordinates for the beacons needed to be imported into the Calypso terminal at the treatment machine. The KVue Calypso compatible couch insert needed to be used when treating these patients to ensure the accuracy of the detection of the beacons and a couch rail avoidance check completed before the first fraction to ensure treatment field clearance. Previously, inter‐fraction motion correction for prostate patients was completed matching to fiducial markers using either kilovoltage (kV) orthogonal paired or cone beam computed tomography (CBCT) image‐guided radiotherapy (IGRT) techniques; however, during setup, the Calypso system allows inter‐fraction motion correction to be completed by the RTs before leaving the treatment room. For the first three patients, standard image guidance was also used to check the accuracy of the new technique. During treatment if the prostate moved >0.5 cm, the radiation beam would be gated by the Calypso system. The treating RTs would wait to see if the prostate moved back into position. If it did not, a couch correction was required. The couch correction was applied from the Calypso system to the linear accelerator by the RTs and the couch was moved remotely to correct the motion. Couch shifts were also applied during Calypso tracking when the treatment beam was off if the movement detected by Calypso in any direction was >0.2 cm.
Inter‐fraction motion recorded by Calypso and comparison to standard IGRT
The maximum and mean inter‐fraction motion detected is shown in Table 1. The largest motion recorded was −2 cm in the superior–inferior plane. The largest mean motion was 0.5 cm and was seen in the anterior–posterior direction.
Table 1.
Inter‐fraction and intra‐fraction motion, prostate rotation and comparison of standard IGRT and Calypso inter‐fraction motion calculation
| Anterior(+ve)–Posterior(−ve) | Superior(+ve)–Inferior(−ve) | Left(+ve)–Right(−ve) | |||||
|---|---|---|---|---|---|---|---|
| IGRT & Calypso shift difference | Mean (cm) | 0.02 | −0.06 | 0.06 | |||
| Inter‐fraction motion (during the time patient on treatment couch) | Max (cm) | 1.7 | −2.0 | 1.2 | |||
| Mean (cm) | 0.5 | 0.1 | −0.1 | ||||
| Pitch | Roll | Yaw | |||||
| Prostate rotation | Range (degrees) | 7 to −14 | 3 to −6 | 12 to −1 | |||
| Anterior | Posterior | Superior | Inferior | Left | Right | ||
| Intra‐fraction motion (during the time patient on treatment couch) | Max (cm) | 1.1 | 0.8 | 1 | 0.6 | 2.2 | 0.6 |
| Mean (cm) | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.1 | |
The mean variation between the standard inter‐fraction IGRT techniques and Calypso is shown in Table 1. There was strong concordance between standard IGRT techniques and Calypso with the largest variations seen in the superior–inferior and left–right directions (−0.06 cm and 0.06 cm, respectively). Variation in all directions was ≤0.06 cm.
Intra‐fraction motion recorded
Figure 1 displays the maximum intra‐fraction motion recorded when the treatment beam was on for each patient. The maximum and mean intra‐fraction motion seen while the patients were on the treatment couch is shown in Table 1. The largest motion recorded was 2.2 cm in the left direction. This occurred while the treatment beam was off. The mean motion was ≤0.2 cm in all directions.
Figure 1.
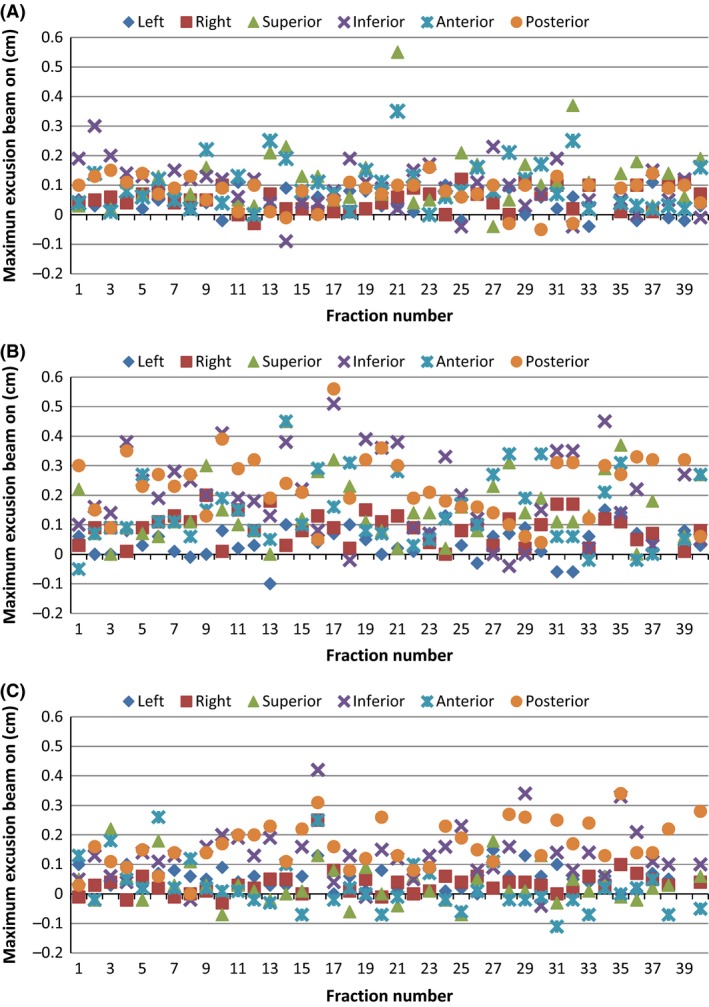
Intra‐fraction motion displacement. The maximum excursion of the beacons in each direction during the time that the treatment beam was on for (A) Patient 1, (B) Patient 2 and (C) Patient 3.
Couch shifts and gating events during treatment
Table 2 shows the number of couch corrections and number of gating events that occurred during treatment for each patient. Patient 2 had a large number of couch shifts applied during the course of treatment. The majority of all corrections occurred after standard IGRT imaging and prior to the first treatment beam. This motion would not have been detected without the use of real‐time motion monitoring and might have resulted in an undetected geographic miss.
Table 2.
Corrections for intra‐fraction motion, gating events and prostate rotation for each patient during the course of treatment
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Total couch shifts over course of treatment | 3 | 63 | 12 |
| When couch shifts occurred during treatment | |||
| Before standard imaging | 0 | 7 | 1 |
| Between imaging and treatment arc 1 | 1 | 18 | 7 |
| During treatment arc 1 | 0 | 0 | 0 |
| Between treatment arc 1 and 2 | 2 | 21 | 1 |
| During treatment arc 2 | 0 | 0 | 0 |
| Between treatment arc 2 and 3 | 0 | 17 | 3 |
| During treatment arc 3 | 0 | 0 | 0 |
| Number of gating events during beam on | 1 | 2 | 0 |
| Prostate rotation >10° | 20 | 0 | 8 |
There was a low number of gating events with a 5 mm gating tolerance. Two of the three patients had gating events. These gating events did not result in a couch correction shift because the prostate moved back into the gating threshold within a few seconds. A correction strategy was used where if Calypso detected a motion of >0.2 cm while the treatment beam was off a couch shift would be applied before delivering the treatment beam. This strategy might have been the cause of the low rate of gating events.
Geometric residual
Calypso provides a geometric residual measurement each day of the goodness of fit of the three beacons to ensure that migration has not occurred. The daily measurements for each patient are displayed in Figure 2. All patients were within the 0.2 cm tolerance for all fractions.
Figure 2.
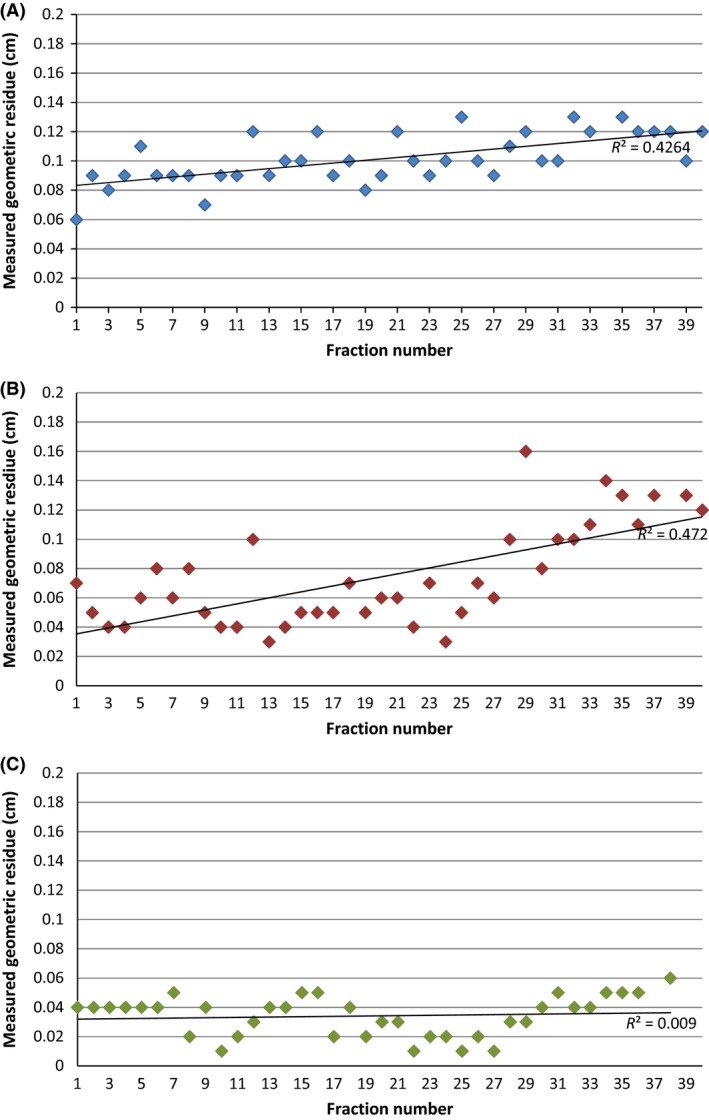
Geometric residue. Geometric residue (goodness of fit) measurement of the three Calypso beacons for (A) Patient 1, (B) Patient 2 and (C) Patient 3 for each fraction.
Prostate rotation
Figure 3 shows the pitch, roll and yaw rotation measurement for the beacons for each patient and fraction. For all patients, the pitch rotation recorded the largest rotation value. The Calypso default rotation tolerance of >10° was exceeded in 28 fractions associated with two of the patients (see Table 2). In these cases, a CBCT scan was taken to ensure the prostate was covered by the planning target volume (PTV) margin prior to treatment. No comparison was made to bony anatomy rotation.
Figure 3.
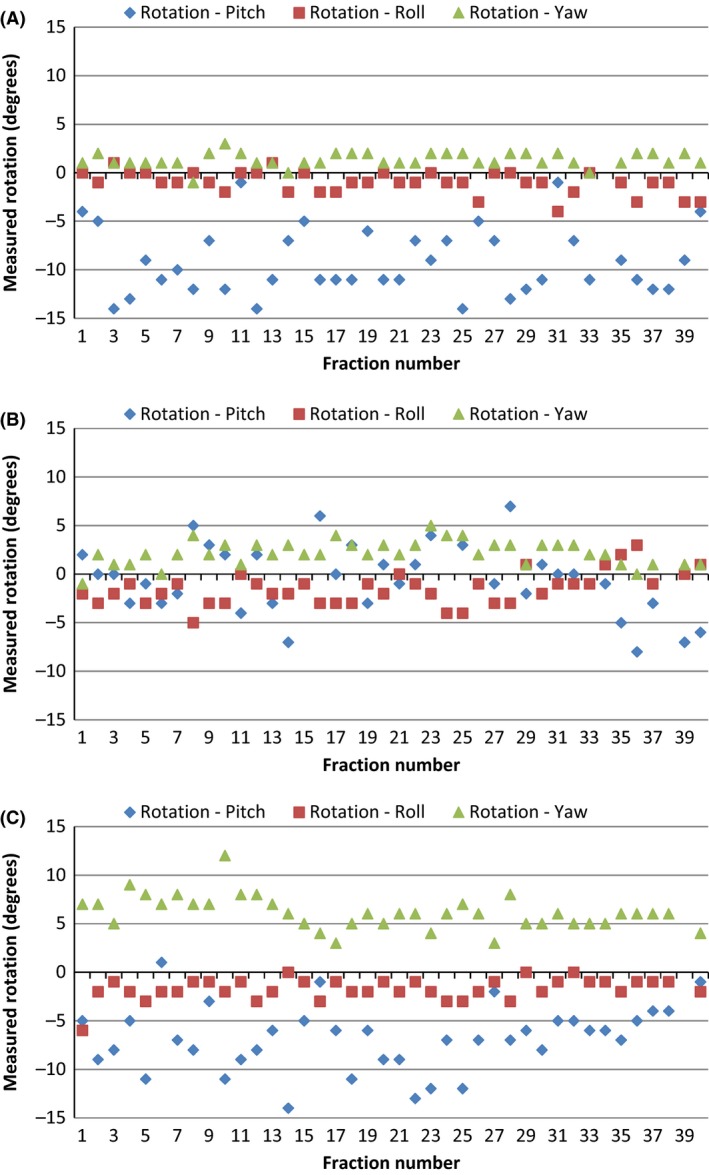
Prostate rotation. The pitch, roll and yaw rotation measurement of the beacons for (A) Patient 1, (B) Patient 2 and (C) Patient 3 for each treatment fraction.
Appointment times
The time taken to treat the patients was assessed using the time that the Calypso tracking station was detecting the beacons (see Figure 4). Standard treatment time allocation for prostate patients is 15 min in our department. Only 4 fractions had a tracking time >15 min. The linear regression line indicates that there was a reduction in tracking times over the treatment course for two of the patients, however, the R 2 values are low.
Figure 4.
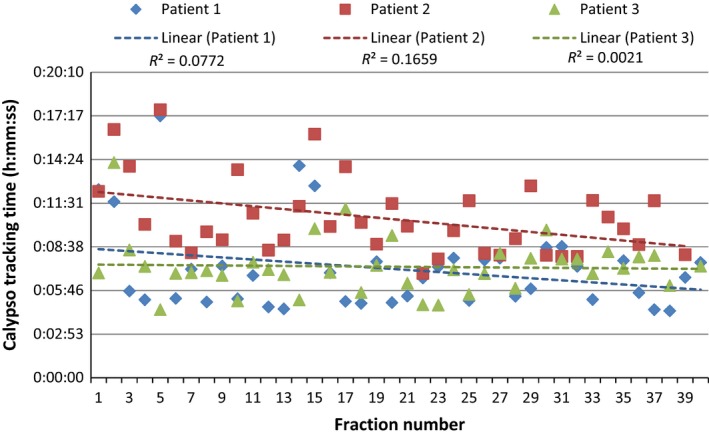
Treatment times. This graph shows the time that the Calypso tracking station was detecting the beacons for each patient and fraction. Standard appointment time allocation for prostate patients is 15 min.
Discussion
Overall, Calypso with Dynamic Edge™ gating was able to be implemented with minimal effect on resources. Initially, additional training was required for the ROs, RTs and ROMPs from a vendor application specialist. Planning times were not largely effected due to the minimal extra steps required. Extra quality assurance steps were added when exporting the beacon co‐ordinates from Eclipse and importing them to Calypso to ensure accuracy but they too had a minimal effect on resources.
Intra‐fraction motion is an important error in radiotherapy to account for but has traditionally been difficult to detect and correct. A number of other groups have also assessed prostate intra‐fraction motion using the Calypso system.5, 7, 8 Kupelian et al.5 assessed intra‐fraction motion in 35 prostate patients and found that the number of fractions with displacements of >0.3 cm or >0.5 cm ranged from 3% to 87% and 0% to 56%, respectively, in each patient. Willoughby et al.7 found that two of the 11 patients that Calypso intra‐fraction motion detected demonstrated significant organ motion of >1 cm, with some motion lasting longer than 1 min. Tanyi et al.8 used Calypso on 14 patients and recorded maximum intra‐fraction movements of 0.48 cm left–right, 0.91 cm anterior–posterior, and 0.86 cm in the superior–inferior directions. In comparison, our study also found that most intra‐fraction motion detected was small with the mean intra‐fraction motion displacement measuring <0.3 cm in all directions; however, there were some large motions detected of up to 2.2 cm. It is acknowledged that this study includes fewer patients than the previous studies. More robust comparison might be achieved with increased patient numbers.
The most interesting finding from this study is the number of couch corrections that needed to be applied and when these shifts occurred. All the couch shifts occurred after standard IGRT imaging was acquired which would mean that this movement would not have been seen or corrected for without intra‐fraction motion monitoring. Most of the movement and shifts also occurred before the first treatment arc which suggests that time needs to be allowed for the patient to settle prior to inter‐fraction motion evaluation. One such fraction is shown in Figure 5. The patient was setup and Calypso tracking was commenced. During the CBCT acquisition, no intra‐fraction motion was shown on the Calypso tracking station. However, while the CBCT was being matching and assessed, a continual drift was detected by Calypso in the vertical and longitudinal planes. This drift was able to be corrected by a remote couch shift prior to the commencement of the treatment arcs but if Calypso was not being used this drift might have caused an undetected geographic miss.
Figure 5.
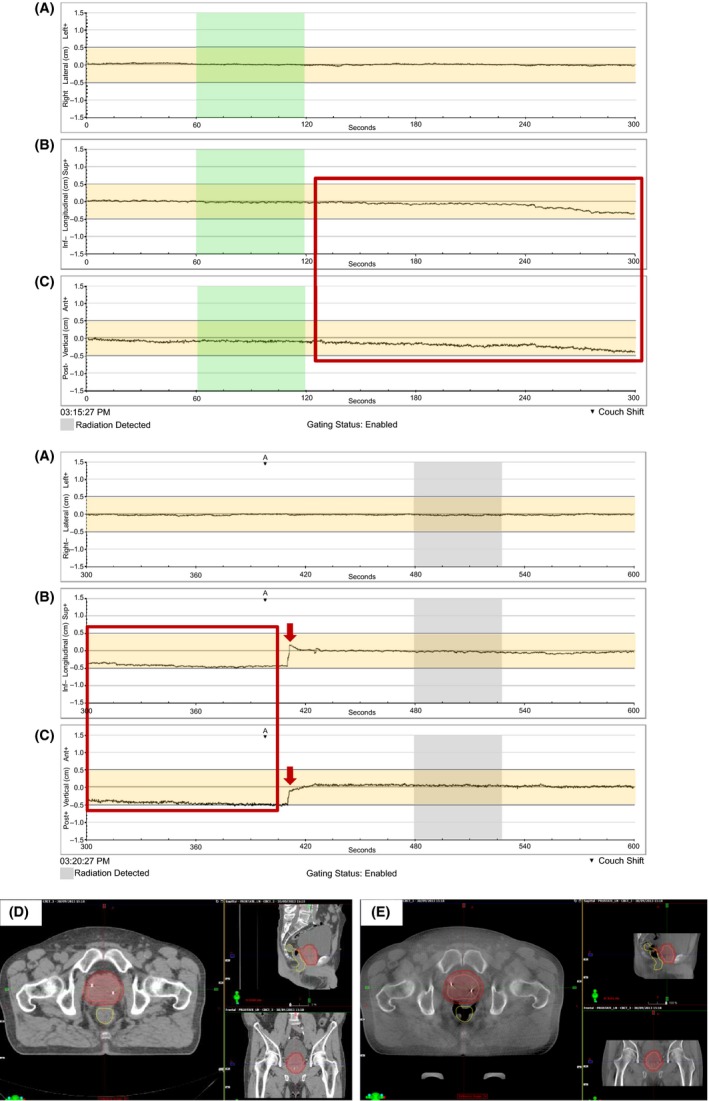
Case showing benefit of real‐time intra‐fraction motion detection. Prostate intra‐fraction motion as recorded by Calypso for a patient's fraction is shown in the lateral (A), longitudinal (B) and vertical (C) directions. The planning CT (D) and CBCT scan (E) from the same fraction are also shown. The orange shaded area indicates the 5 mm gating tolerance used. The green shaded area shows the time when the CBCT (E) was acquired. The trace inside the red box shows the continual drift of the prostate in the longitudinal and vertical planes after the CBCT was acquired and before the treatment began (grey shaded area). This motion was not seen on the CBCT but was shown by Calypso allowing a correction to be made prior to treatment (red arrows). If Calypso was not being used, the drift would not have been detected and might have continued and caused an undetected geographic miss.
Strong concordance between the standard IGRT technique and Calypso was seen with the variation being ≤0.06 cm in all directions. Other studies have also found a good agreement between standard IGRT practices and Calypso for inter‐fraction motion correction.5, 7 Standard imaging was reduced for future patients to CBCT scanning on the first 3 fractions then once weekly to allow verification of bladder and rectal preparation and contour variation. This decreases the amount of imaging radiation dose delivered to the patient because Calypso does not use radiation to detect prostate motion.
Rotation >10° was detected in 28 of the 116 fractions. On the occasions when the rotation tolerance was exceeded, a CBCT scan was taken to ensure that all soft tissue contoured as the clinical target volume (CTV) was being covered by the PTV before treatment commenced. In all cases, treatment was able to be delivered without intervention. Rotation is an important movement that needs to be assessed because it can cause geographic miss. The effect of rotation will depend on the PTV expansion margins used. The effect of prostate rotation on treatment accuracy is an area that requires further investigation in the future.
The use of intra‐fraction motion monitoring also allows for the consideration of reducing CTV to PTV expansions. Tanyi et al.8 assessed the PTV expansions required when using image‐guided marker alignment versus the use of Calypso with intra‐fraction motion monitoring. The PTV margin required decreased from 0.28 cm left–right, 0.37 cm superior–inferior and 0.32 cm anterior–posterior for image‐guided marker alignment to 0.14 cm left–right, 0.26 cm superior–inferior and 0.23 cm anterior–posterior with the use of intra‐fraction motion monitoring. Due to the limited cohort size, calculations were not completed during this study on PTV margins and were out of the scope of this study.
Mean intra‐fraction motion was small in this group of patients so it could be argued that with standard fraction treatment, intra‐fraction motion monitoring is not required. It could also be argued that Calypso would be more beneficial in other treatment sites that are more mobile such as the lung.9 However, intra‐fraction motion monitoring is becoming increasingly important in the prostate setting as treatment techniques change.10, 11 These changes include intra‐prostatic dominant nodule boosts,10 and stereotactic treatments.11 Intra‐prostatic dominant nodule boost is where a simultaneous boost dose is delivered to the dominate nodule of the prostate as detected by imaging such as positron emission tomography (PET). Kuang et al.10 showed that an increased dose of 100–105 Gy could be delivered to the dominate nodule using VMAT while still observing OAR constraints and concluded that this could increase the likelihood of tumour control. Stereotactic hypofractionated radiotherapy for prostate cancer is also becoming more common. Madsen et al.11 showed that 33.5 Gy in 5 fractions could be safely delivered in prostate cancer patients with minimal acute or late toxicity. They also suggested that further dose escalation could be possible. Increasing the dose either to the entire or part of the prostate with the close proximity of pelvic OARs and the sharp dose falloff generated by VMAT is where intra‐fraction motion monitoring will be essential to ensure accurate prostate radiotherapy treatment.
There are a number of limitations to this study. The main limitation is that it only involves a small number of patients. This makes it difficult to draw definitive conclusions. However, when implementing new technology, it is important to review the process and the data collected early. This enabled checking of the processes put in place and a review of the motion seen and interventions required. This work has also been hypothesis generating and enables an evaluation of the implementation process to be published to help other departments looking to implement the same technology.
Conclusion
Intra‐fraction motion monitoring with Calypso Dynamic Edge™ gating was successfully implemented at NSCC. Calypso detected motion after standard imaging that resulted in a total of 78 couch shifts being applied over the 116 fractions evaluated. This motion would not have been detected without the use of real‐time motion detection.
Conflict of interest
Northern Sydney Cancer Centre has a research agreement with Varian Medical Systems.
Acknowledgements
The authors gratefully acknowledge all the staff at Northern Sydney Cancer Centre.
J Med Radiat Sci 64 (2017) 25–34
References
- 1. Foroudi F, Tyldesley S, Barbera L, Huang J, Mackillop WJ. Evidence‐based estimate of appropriate radiotherapy utilization rate for prostate cancer. Int J Radiat Oncol Biol Phys 2003; 55: 51–63. [DOI] [PubMed] [Google Scholar]
- 2. Pollack A, Zagars GK, Starkschall G, et al. Prostate cancer radiation dose response: Results of the M. D. Anderson phase III randomized trial. Int J Radiat Oncol Biol Phys 2002; 53: 1097–105. [DOI] [PubMed] [Google Scholar]
- 3. Eade TN, Hanlon AL, Horwitz EM, Buyyounouski MK, Hanks GE, Pollack A. What dose of external‐beam radiation is high enough for prostate cancer? Int J Radiat Oncol Biol Phys 2007; 68: 682–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Varian.Medical.Systems . Calypso System Operator's Manual Version 3.0. 2013.
- 5. Kupelian P, Willoughby T, Mahadevan A, et al. Multi‐institutional clinical experience with the Calypso System in localization and continuous, real‐time monitoring of the prostate gland during external radiotherapy. Int J Radiat Oncol Biol Phys 2007; 67: 1088–98. [DOI] [PubMed] [Google Scholar]
- 6. Keall PJ, Colvill E, O'Brien R, et al. The first clinical implementation of electromagnetic transponder‐guided MLC tracking. Med Phys 2014; 41: 020702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Willoughby TR, Kupelian PA, Pouliot J, et al. Target localization and real‐time tracking using the Calypso 4D localization system in patients with localized prostate cancer. Int J Radiat Oncol Biol Phys 2006; 65: 528–34. [DOI] [PubMed] [Google Scholar]
- 8. Tanyi JA, He T, Summers PA, et al. Assessment of planning target volume margins for intensity‐modulated radiotherapy of the prostate gland: Role of daily inter‐ and intrafraction motion. Int J Radiat Oncol Biol Phys 2010; 78: 1579–85. [DOI] [PubMed] [Google Scholar]
- 9. Shah AP, Kupelian PA, Waghorn BJ, et al. Real‐time tumor tracking in the lung using an electromagnetic tracking system. Int J Radiat Oncol Biol Phys 2013; 86: 477–83. [DOI] [PubMed] [Google Scholar]
- 10. Kuang Y, Wu L, Hirata E, Miyazaki K, Sato M, Kwee SA. Volumetric modulated arc therapy planning for primary prostate cancer with selective intraprostatic boost determined by 18F‐choline PET/CT. Int J Radiat Oncol Biol Phys 2015; 91: 1017–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Madsen BL, Hsi RA, Pham HT, Fowler JF, Esagui L, Corman J. Stereotactic hypofractionated accurate radiotherapy of the prostate (SHARP), 33.5 Gy in five fractions for localized disease: First clinical trial results. Int J Radiat Oncol Biol Phys 2007; 67: 1099–105. [DOI] [PubMed] [Google Scholar]


