Abstract
Background
The definition of continence after robot-assisted laparoscopic radical prostatectomy (RARP) has not been consistently defined, with many studies only noting the amount of safety pads used. We therefore examined what definition of continence would be appropriate, employing both the International Consultation on Incontinence Modular Questionnaire Short Form (ICIQ-SF) and the number of pads used by patients. We also evaluated the relationship between the number of pads used and degree of incontinence.
Methods
Patients who underwent RARP between October 2010 and July 2014 in our department were included in the present study. All patients were evaluated by ICIQ-SF and the number of pads used 1, 3, 6 and 12 months after surgery. Frequency of incontinence and amount of incontinence were evaluated by ICIQ-SF Questions 1 and 2 respectively at 12 months. Quality of life (QOL) was evaluated by ICIQ-SF Question 3 at 1, 3, 6, and 12 months after RARP.
Results
The overall study population was 156 patients. In Question 1, 19 patients answered that they leaked urine several times a day, but 5 patients did not use pads, and 8 patients were using only 1 pad a day. In Question 2, 8 patients answered that they leaked a moderate amount of urine, but 2 patients did not use any pads, and 3 patients used only 1 pad a day. QOL showed significant differences between using no pad, 1 pad, or ≥ 2 pads at 1, 3, 6, and 12 months after RARP.
Conclusion
Simply noting the number of pads used by a patient is an insufficient way to evaluate incontinence after RARP. Assessment by an appropriate questionnaire is also needed.
Keywords: incontinence, International Consultation on Incontinence Modular Questionnaire Short Form, robot-assisted laparoscopic radical prostatectomy
Patients with localized prostate cancer are candidates for active surveillance, radiation therapy, and/or radical prostatectomy. Robot-assisted laparoscopic radical prostatectomy (RARP) has become widely used and is increasingly adopted as the best method of cure. Some reports have suggested that RARP offers short-term benefits over historical controls with open radical prostatectomy (ORP) in terms of better visualization, lower perioperative complication and transfusion rates, and shorter hospital stay.1 Various surgical techniques have been devised to reduce incontinence after RARP.2
Postoperative urinary incontinence after radical prostatectomy for prostate cancer has a relevant negative effect on satisfaction and quality of life (QOL).3 In addition, urinary incontinence has been suggested to have a higher impact on QOL than lack of sexual functioning.3 Some studies have shown that patients achieved continence much earlier after RARP than after ORP or laparoscopic radical prostatectomy (LRP). Ficarra et al. reported that a 12-month urinary recovery after ORP ranged from 60% to 93%, and after LRP, from 66% to 95%. A previous systematic review shows that the 12-month urinary recovery after RARP ranged from 84% to 97%.1 In addition, Sammon et al. reported that only 17.3% of patients undergoing RARP showed that they were able to achieve urinary continence right after catheter removal.4 On the other hand, the definition of continence after RARP has not been determined correctly. The most common definition of incontinence is the use of urinary safety pads.1 Many reports have determined that continence is defined as “no pad” or “one safety pad per day.”1 However, this definition excludes patients who may be incontinent but don’t use pads for whatever reason.
We therefore examined what definition of continence would be appropriate, employing both the International Consultation on Incontinence Modular Questionnaire Short Form (ICIQ-SF) and noting the number of pads used. We also evaluated the relationship between the number of pads used and degree of incontinence from information given by the patient on the questionnaire.
MATERIALS AND METHODS
Ethics
This study was conducted at the Division of Urology, Tottori University Hospital, Tottori, Japan. The study was approved by the Tottori University Ethics Committee (No. 2545).
Patients
All patients who underwent RARP between October 2010 and July 2014 in the Division of Urology at Tottori University Hospital for clinically localized prostatic cancer (stages cT1c–cT3a N0 M0) were included in the present study. All patients were evaluated by ICIQ-SF and the number of pads used.
Follow-up and Questionnaire
Frequency of incontinence was evaluated by ICIQ-SF Question 1: “How often does your urine leak?” Responses were scored as follows: “Never,” 0; “About once a week or less,” 1; “Two or three times a week,” 2; “About once a day,” 3; “Several times a day,” 4; and “All the time,” 5. The amount of incontinence was evaluated by ICIQ-SF Question 2: “How much urine usually leaks?” Responses were scored as follows: “None,” 0; “A small amount,” 2; “A moderate amount,” 4; and “A large amount,” 6. QOL was evaluated using ICIQ-SF Question 3: “Overall, how much does leaking urine interfere with your everyday life?” Responses were scored on a range from 0, “Not at all” to 10, “A great deal.”
Statistical analysis
All data were presented as number as the mean with standard deviation. Comparisons of mean values among the groups were done using ANOVA with the Tukey-test. A P value of less than 0.05 (P < 0.05) was considered significant. Statistical analysis was carried out using the Statistical Package for the Social Sciences, version 19 (IBM, Armonk, NY).
RESULTS
A total of 210 patients underwent RARP, but 54 patients were excluded from this study since there was a lack of data based on their questionnaires. As a result, 156 patients formed the overall study population. Mean patient age was 65.2 years (range, 50–75 years), mean prostate-specific antigen (PSA) concentration was 9.44 ng/mL (range, 4.20–25.7 ng/mL), and mean prostate volume was 32.1 mL (range, 8.9–75 mL). In terms of clinical stage, 33 patients were T1c, 67 patients were T2a, 7 patients were T2b, 34 patients were T2c, and 15 patients were T3a. Seventy-seven patients received nerve-sparing procedures on at least unilateral side (Table 1). One month after RARP, 31.4% of patients had achieved 0 pad usage and 58.3% had achieved 0–1; this increased to 67.3% with 0 pads and 90.1% with 0–1 pads after 6 months and 78.8% with 0 pads and 94.9% with 0–1 pads after 12 months (Table 2).
Table 1.
Characteristics of study patients
| Factors | Mean ± SD or number | |
| No. of patients | 156 | |
| Age (years old) | 65.2 ± 6.7 | |
| PSA (ng/mL) | 9.4 ± 6.8 | |
| Prostate volume (mL) | 32.1 ± 13.5 | |
| Clinical stage | ||
| T1c | 33 | |
| T2a | 67 | |
| T2b | 7 | |
| T2c | 34 | |
| T2c | 15 | |
| Nerve sparing | ||
| Yes | 77 | |
| No | 79 | |
No., number; PSA, prostate specific antigen.
Table 2.
Continent rates after RARP according to the definition of no pads or 1 pad as an objective measure of continence
| No. of pads | 1 month | 3 month | 6 month | 9 month | 12 month |
| 0 (%) | 31.4 | 51.9 | 67.3 | 72.4 | 78.8 |
| 0–1 (%) | 58.3 | 81.4 | 90.1 | 94.2 | 94.9 |
No., number; RARP, robot-assisted laparoscopic radical prostatectomy.
Twelve months after RARP, in response to ICIQ-SF Question 1, 73 patients answered that they never leaked urine, but 1 patient used 1 pad. Thirty-four patients answered that they leaked urine about once a week or less, and 4 patients used 1 pad. Sixteen patients answered that they leaked urine two or three times a week, and 6 patients used 1 pad. However, 19 patients answered that they leaked urine several times a day, but 5 of these patients did not use any pads and 8 of these patients used only 1 pad (Table 3).
Table 3.
Incontinent symptom scales based on ICIQ-SF and the number of pads used at 12 month after RARP
| ICIQ-SF / No. of pads | 0 | 1 | 2 or more | |
| Q1 (How often does your urine leak?) | ||||
| Never | 72 | 1 | 0 | |
| About once a week or less | 30 | 4 | 0 | |
| Two or three times a week | 10 | 6 | 0 | |
| About once a day | 5 | 7 | 0 | |
| Several times a day | 5 | 8 | 6 | |
| All the time | 0 | 0 | 2 | |
| Q2 (How much urine usually leaks?) | ||||
| None | 74 | 1 | 0 | |
| A small amount | 46 | 22 | 3 | |
| A moderate amount | 2 | 3 | 3 | |
| A large amount | 0 | 0 | 2 | |
ICIQ-SF, International Consultation on Incontinence Modular Questionnaire Short Form; No., number; Q, Question.
Twelve months after RARP, in response to ICIQ-SF Question 2, 75 patients answered that they never leak urine, but 1 patient used 1 pad. Of the 71 patients who answered that they leaked a small amount of urine, 3 patients used ≥ 2 pads. Of the eight patients who answered that they leaked a moderate amount of urine, 2 patients did not use any pads, 3 patients used 1 pad, and 3 patients used ≥ 2 pads (Table 3).
In terms of QOL, 12 months after RARP in ICIQ-SF Q3, there were significant differences between no pad, 1 pad, and 2 or more pads at 1, 3, 6 and 12 months (Table 4).
Table 4.
QOL scores based on ICIQ-SF by the number of pads used at 1, 3, 6, 12 month after RARP
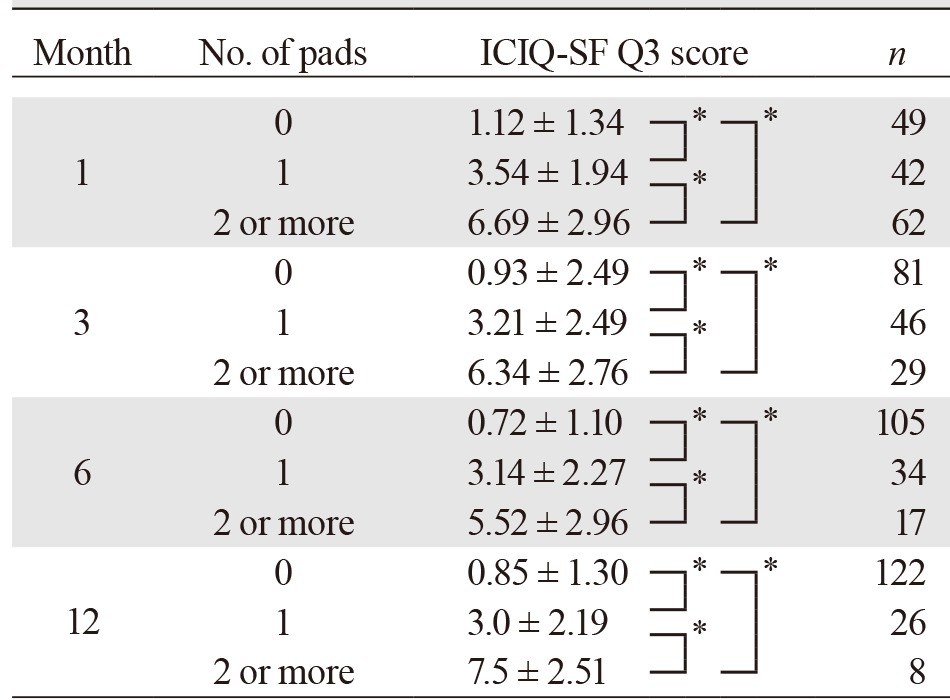
ICIQ-SF Question 3: “Overall, how much does leaking urine interfere with your everyday life?” Patients choice a number from 0 to 10, “Not at all” to “A great deal.” * P < 0.05.
ICIQ-SF, International Consultation on Incontinence Modular Questionnaire Short Form; No., number; QOL, quality of life.
DISCUSSION
Urinary incontinence after RARP is influenced by the preoperative characteristics of the patient, patient age, experience of the surgeon, and the surgical techniques applied, including nerve sparing.5 A systematic review showed that according to the definition of continence as using no pads, 12-month urinary incontinence rates ranged from 4% to 31%, with a mean of 16%. Considering studies that considered no pads or one safety pad as the definition of continence, 12-month urinary incontinence rates ranged from 8% to 11%, with a mean of 9%.1 However, an unambiguous definition of continence after RARP has yet to be established. Many definitions have been employed, including the number of pads used, leak-free status, and questionnaire responses.6–8 Many authors have used the definition of no pad or 1 safety pad as an objective measure of continence.1 On the other hand, some studies have reported pad count as an unreliable indicator in the severity of incontinence.8–10 We examined the relationship between the number of pads used and an incontinence symptom scale based on the ICIQ-SF.
In this study, the 12-month continence rate according to the definition of no pad use was 21.2%, lower than reported in previous studies.11–13 Some studies have previously demonstrated age and nerve sparing as associated with continence after surgery.14–16 We suggested that the reasons for the lower continence rate in our study were higher age and a lower nerve-sparing rate than in previous studies.
In this study, 72 (59.0%) of the 122 patients that did not use pads selected “Never” for Question 1 in the ICIQ-SF at 12 months after RARP. Although ten (8.2%) of these 122 patients complained of leaking urine once or more a day, the definition of no pad use seems relatively consistent with continence based on the ICIQ-SF. On the other hand, only one (3.8%) of 26 patients using one pad selected “Never” for Question 1 in the ICIQ-SF at 12 months after RARP. Fifteen (57.7%) of these 26 patients using 1 pad complained of leaking urine once or more a day, although leaked amounts were small. The definition of using 1 pad was not consistent with continence based on the ICIQ-SF.
Haga et al. found little correlation between the number of pads used and severity of incontinence. One possible reason was that patients wore various configurations and sizes of pads, unrelated to the actual volume of urinary incontinence.7 Pad count was thus not useful as an objective measure of incontinence after RARP. Some reports have used the number of pads and scores on various questionnaires including the ICIQ-SF and the Expanded Prostate Cancer Index Composite (EPIC) as definitions of continence after RARP.7, 17 Our findings support their definition of continence based on the number of pads used together with questionnaire-based symptom scales.
Concerning QOL, urinary incontinence after RARP has been suggested to have a higher impact on QOL than sexual functioning.18 Haga et al. reported that the number of pad exchanges per day, pad wetness, and the timing of pad exchanges were important factors affecting QOL.7 In our study, a significant difference in QOL was seen between no pad and 1 pad. The definition of using 1 pad is not consistent with continence based on ICIQ-SF. If we evaluate incontinence based solely on only the number of pads used, no pad use is appropriate as a definition of continence.
One study limitation was that we did not include a validated objective measure of the pad test. Nitti et al. reported that men with post-prostatectomy incontinence accurately described the number, size, and degree of wetness of pads that they collected during a 24-h pad test.8 However, this approach seems impractical as a pad test for every patient. A practical approach is to perform the pad test for those patients showing inconsistency between the number of pads used and symptom scales based on questionnaire responses.
In conclusion, we feel the number of pads used is an insufficient indicator for evaluating incontinence after RARP. Incontinence after RARP should be evaluated using a combination of noting the number of pads used, questionnaires, and possibly a pad test.
Further studies are needed to establish a unified definition of continence from clinical outcome evaluations of RARP and provisions for accurate information to and from patients.
The authors declare no conflict of interest.
REFERENCES
- 1. Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2012;62:405-17. [DOI] [PubMed] [Google Scholar]
- 2. Lei Y, Alemozaffar M, Williams SB, Hevelone N, Lipsitz SR, Plaster BA, et al. Altermal division and selective suture ligation of the dorsal vein complex during robot-assisted laparoscopic radical prostatectomy: description of technique and outcomes. Eur Urol. 2011;59:235-43. [DOI] [PubMed] [Google Scholar]
- 3. van der Poel HG, Tillier C, de Blok WM, Acar C, van Muilekom EH, van den Bergh RC. Interview-based versus questionnaire-based quality of life outcomes before and after prostatectomy. J Endourol. 2013;11:1411-6. [DOI] [PubMed] [Google Scholar]
- 4. Sammon JD, Sharma P, Trinh QD, Ghani KR, Sukumar S, Menon M. Predictors of immediate continence following robot-assisted radical prostatectomy. J Endourol. 2013;27:442-6. [DOI] [PubMed] [Google Scholar]
- 5. Lavigueur-Blouin H, Noriega AC, Valdivieso R, Hueber PA, Bienz M, Alhathal N, et al. Predictors of early continence following robot-assisted radical prostatectomy. Can Urol Assoc J. 2015;9:e93-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Geraerts I, Van Poppel H, Devoogdt N, Van Cleynenbreugel B, Joniau S, Van Kampen M. Prospective evaluation of urinary incontinence, voiding symptoms and quality of life after open and robot-assisted radical prostatectomy. BJU Int. 2013;112:936-43. [DOI] [PubMed] [Google Scholar]
- 7. Haga N, Yanagida T, Yabe M, Akaihata H, Hata J, Sato Y, et al. Timing of Urinary Pad Exchanges Was the Most Important Factor Affecting Quality of Life in the Early Postoperative Period After Robot-Assisted Laparoscopic Radical Prostatectomy. J Endourol. 2015;29:1044-51. [DOI] [PubMed] [Google Scholar]
- 8. Nitti VW, Mourtzinos A, Brucker BM; SUFU Pad Test Study Group. Correlation of patient perception of pad use with objective degree of incontinence measured by pad test in men with post-prostatectomy incontinence: the SUFU Pad Test Study. J Urol. 2014;192:836-42. [DOI] [PubMed] [Google Scholar]
- 9. Tsui JF, Shah MB, Weinberger JM, Ghanaat M, Weiss JP, Purohit RS, et al. Pad count is a poor measure of the severity of urinary incontinence. J Urol. 2013;190:1787-90. [DOI] [PubMed] [Google Scholar]
- 10. Dylewski DA, Jamison MG, Borawski KM, Sherman ND, Amundsen CL, Webster GD, et al. A statistical comparison of pad numbers versus pad weights in the quantification of urinary incontinence. Neurourol Urodyn. 2007;26:3-7. [DOI] [PubMed] [Google Scholar]
- 11. Kim SC, Song C, Kim W, Kang T, Park J, Jeong IG, et al. Factors determining functional outcomes after radical prostatectomy: robot-assisted versus retropubic. Eur Urol. 2011;60:413-19. [DOI] [PubMed] [Google Scholar]
- 12. Rocco B, Matei DV, Melegari S, Ospina JC, Mazzoleni F, Errico G, et al. Robotic vs open prostatectomy in a laparoscopically naïve center: a matched – pair analysis. BJU Int. 2009;104:991-5. [DOI] [PubMed] [Google Scholar]
- 13. Trabulsi EJ, Zola JC, Gomella LG, Lallas CD. Transition from pure laparoscopic to robotic-assisted radical prostatectomy: single surgeon institutional evolution. Urol Oncol. 2010;28:81-5. [DOI] [PubMed] [Google Scholar]
- 14. Park YH, Kwon OS, Hong SH, Kim SW, Hwang TK, Lee JY, et al. Effect of Nerve-Sparing Radical Prostatectomy on Urinary Continence in Patients With Preoperative Erectile Dysfunction. Int Neurourol J. 2016;20:69-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Suardi N, Moschini M, Gallina A, Gandaglia G, Abdollah F, Capitanio U, et al. Nerve-sparing approach during radical prostatectomy is strongly associated with the rate of postoperative urinary continence recovery. BJU Int. 2013;111:717-22. [DOI] [PubMed] [Google Scholar]
- 16. Kübler HR, Tseng TY, Sun L, Vieweg J, Harris MJ, Dahm P, et al. Impact of nerve sparing technique on patient self-assessed outcomes after radical perineal prostatectomy. J Urol. 2007;178:488-92. [DOI] [PubMed] [Google Scholar]
- 17. Davison BJ, Matthew A, Gardner AM. Prospective comparison of the impact of robotic-assisted laparoscopic radical prostatectomy versus open radical prostatectomy on health-related quality of life and decision regret. Can Urol Assoc J. 2014;8:e68-e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schroeck FR, Krupski TL, Sun L, Albala DM, Price MM, Polascik TJ, et al. Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2008;54:785-93. [DOI] [PubMed] [Google Scholar]


