ABSTRACT
Exercise-induced increases in core body temperature could negative impact performance and may lead to development of heat-related illnesses. The use of cooling techniques prior (pre-cooling), during (per-cooling) or directly after (post-cooling) exercise may limit the increase in core body temperature and therefore improve exercise performance. The aim of the present review is to provide a comprehensive overview of current scientific knowledge in the field of pre-cooling, per-cooling and post-cooling. Based on existing studies, we will discuss 1) the effectiveness of cooling interventions, 2) the underlying physiological mechanisms and 3) practical considerations regarding the use of different cooling techniques. Furthermore, we tried to identify the optimal cooling technique and compared whether cooling-induced performance benefits are different between cool, moderate and hot ambient conditions. This article provides researchers, physicians, athletes and coaches with important information regarding the implementation of cooling techniques to maintain exercise performance and to successfully compete in thermally stressful conditions.
KEYWORDS: core body temperature, exercise performance, mid-cooling, pre-cooling, per-cooling, post-cooling, thermoregulation
Introduction
Human core body temperature (Tc) is regulated to ensure normal body function, while any increase of Tc above its normal range (set-point) is defined as hyperthermia.1-3 During exercise only ∼20–30% of the produced energy is converted to mechanical work, whereas ∼70–80% of the energy is released as heat.4,5 The exercise-induced increase in heat production typically exceeds the heat loss capacity and results in Tc elevation.6,7 Previous studies showed significant increases in Tc in athletes exercising in cold,8 warm,9 and humid10 environmental conditions. There is evidence of exercise-induced fatigue beyond a Tc threshold of > 40°C11 and a Tc >40.5°C may lead to the development of heat-related illnesses such as heat exhaustion, heat injury and heat stroke.12,13 In addition to the exercise-induced elevations in Tc, prolonged exercise also increases skin temperature.14 A combination of an increased core- and skin temperature, resulting in a lower core-to-skin gradient, is associated with a decreased exercise performance.14-16 Strategies to reduce the thermal strain prior to, during and directly after exercise are therefore of great importance.
Cooling interventions could increase heat storage capacity (pre-cooling), attanuate the exercise-induced increase in Tc (per-cooling) and accelerate recovery following intense exercise (post-cooling). In the past decade, several reviews and meta-analysis have been published with respect to cooling and exercise. Early reviews were primarily focused on the effects of pre-cooling on thermoregulation and exercise performance.17-21 More recently, several overviews were published on the benefits of per-cooling and the differences between pre- and per-cooling.22-25 However, an important limitation of previous work is that a comprehensive summary of the potential benefits of all cooling modalities for different types of sports performing exercise under different environmental conditions is missing. Furthermore, additional insight in the underlying mechanisms that are responsible for the pre-, per-, and post-cooling benefits is needed.
Therefore, the aim of the present review is to provide a comprehensive overview of current scientific knowledge in the field of pre-cooling, per-cooling and post-cooling. Based on existing studies, we will discuss 1) the effectiveness of cooling interventions on improving exercise performance, 2) the underlying physiological mechanisms and 3) practical considerations regarding the use of different cooling techniques. This article provides researchers, physicians, athletes and coaches with important information regarding the implementation of cooling techniques to maintain exercise performance and to successfully compete in thermally stressful conditions.
Methodological considerations
The use of cooling techniques prior to, during or directly after exercise is widely described in literature, whereas large differences in study setup were found across studies. The study protocols differ with respect to cooling technique (i.e. cooling vests, cold water immersion, ice slurry ingestion, cooling packs, menthol cooling, facial water spray), exercise protocol (time trial, total distance covered, time to exhaustion, fixed exercise protocols), types of exercise (endurance versus strength) and ambient conditions (temperature, humidity). Furthermore, the sample size and study population (age, sex, level of fitness) also differed substantially across studies. This lack of standardization makes a direct comparision between studies difficult. A standardized effect size (ES) can be calculated to compare studies with different study protocols.26 In the present review, we decided to present relative changes as well as effect sizes to demonstrate the effect of cooling on exercise performance.
In addition to the methodological differences among studies, publication bias could also influence overall outcomes. Two previous meta-analyses demonstrated a potential publication bias,22,24 whereas other reviews did not report a potential publication bias.21,27 This descripancy suggests that publication bias might be present, which may implicate in an overestimation of the overall effect of cooling.
Pre-cooling
Pre-cooling can be described as the rapid removal of heat from the body before exercise to create a larger heat storage capacity.28 An overview of used cooling techniques is shown in Table 1. Many pre-cooling techniques were proven to be effective, ranging from whole body pre-cooling such as cold water immersion20,29 and cold air exposure30-32 to local cooling using cooling vests33,34 or cooling packs,35,36 or internal cooling strategies such as the ingesting of cold water or ice slurry.20,37,38 Furthermore, a combination of these cooling techniques (i.e., mixed method cooling), is often used to obtain a greater cooling power and larger reduction in Tc.34,36,39
Table 1.
Overview of the different cooling techniques.
| Cooling technique | Timing of cooling | Intervention temperature (°C) | Advantages of cooling technique | Disadvantages and practical considerations |
|---|---|---|---|---|
| Cooling vest | Pre-cooling | 10–20°C | - Light weight | - Less aggressive |
| Per-cooling | - Easily applicable in field-based settings | - Quick decrease in cooling power | ||
| - Covers a large part of the body | ||||
| Ice vest | Pre-cooling | < 0°C | - Aggressive cooling technique | - Heavy weight |
| Per-cooling | - Covers a large part of the body | - Difficult to use in field-based settings | ||
| Post-cooling | ||||
| Cold water ingestion | Pre-cooling | 1–5°C | - Direct effect on core body temperature | - Covers a small part of the body |
| Per-cooling | - Easily applicable in field-based settings | - Less aggressive | ||
| Ice slurry ingestion | Pre-cooling | < 0°C | - Direct effect on core body temperature | - Covers a small part of the body |
| Per-cooling | - Easily applicable in field-based settings | - Potential gastrointestinal discomfort | ||
| Menthol cooling | Pre-cooling | Not applicable | - Easily applicable in field-based settings | - Best way of application is not yet known |
| Per-cooling | ||||
| Facial wind/water spray | Pre-cooling | Wind and water temperature | - Covers a large part of the body | - Difficult to use in field-based settings |
| Per-cooling | 10–20°C | - No direct contact with the skin | ||
| Cooling packs | Pre-cooling | <0°C | - Aggressive cooling technique | - Covers a small part of the body |
| Per-cooling | - Easily applicable in field-based settings | - Can restrict movement and improve air resistance | ||
| Post-cooling | - Heavy weight, less suitable for per-cooling | |||
| Cold water immersion | Pre-cooling | 10–25°C | - Covers a large part of the body | - Not suitable in field-based settings |
| Post-cooling | - Direct contact with the skin | |||
| Cryotherapy | Pre-cooling | < −100°C | - Covers a large part of the body | - No direct contact with the skin |
| Post-cooling | - Aggressive cooling technique | - Expensive |
The effects of different pre-cooling techniques on exercise performance were examined within various ambient conditions and using different exercise protocols (i.e., endurance exercise vs. (intermittent) sprint exercise). We previously demonstrated in a meta-analysis that pre-cooling improves exercise performance in the heat (ambient temperature >30°C) with 5.7 ± 0.9% (ES = 0.44).22 Mixed method cooling appeared to be the most effective strategy to enhance exercise performance, followed by cold water immersion, cold water/ice slurry ingestion, cooling packs and cooling vests (Fig. 1).22 These findings suggest that vigorous cooling of a large surface of the body is more effective than local body and/or less powerful cooling techniques to improve exercise performance.
Figure 1.
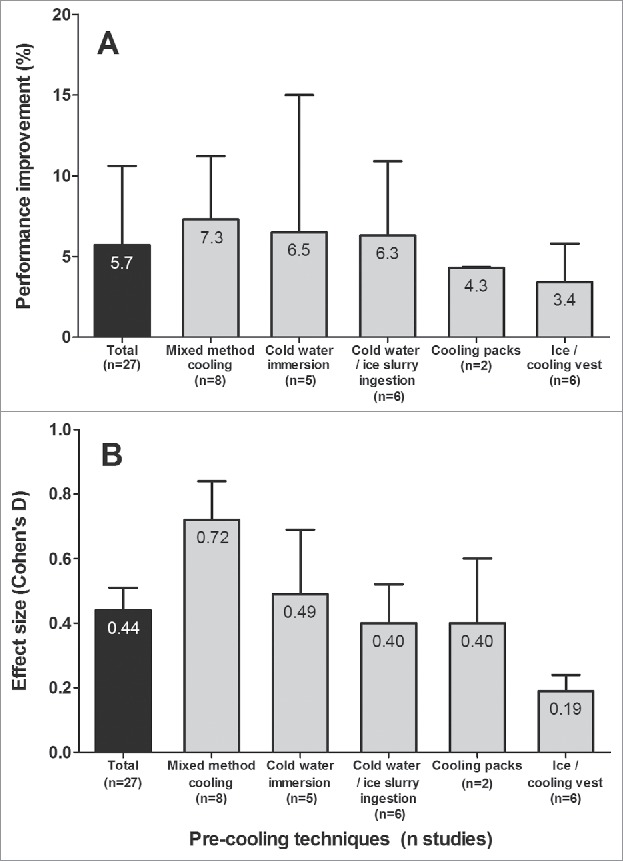
An overview of the average performance improvement (%) (A) and effect size (B) of pre-cooling (black bar) and the beneficial effects of different precooling strategies (gray bars). Data are presented as mean ± standard deviation. The figure is adapted from our previous meta-analysis.22
Ambient conditions could also impact the performance benefits associated with pre-cooling. Although most pre-cooling studies were performed in simulated heat (>30°C), professional and recreational athletes will not solely practice and compete in hot ambient temperatures, but also in cool and moderate environmental conditions. Ninety minutes of cold air (0–18°C) exposure prior to exercise in moderate ambient conditions (18°C) resulted in an increased time to exhaustion32 and an increased 1 hour work rate (172 W vs. 161 W for cooling and control respectively).30 In contrast, upper body pre-cooling using an ice vest did not improve intermittent sprint exercise in a moderately warm environment (22°C dry bulb temperature, 40% relative humidity).40 Moreover, a decrease in exercise performance was found after 30 min of exposure to cold air (5°C) prior to 30 minutes of cycling at 50% of VO2 max in a cold ambient temperature (5°C).41 The association between ambient temperature and pre-cooling induced performance benefits was reinforced in a meta-analysis which found greater effects with increasing ambient temperatures.21
The performance benefits of pre-cooling were confirmed by another meta-analysis,24 as pre-cooling significantly improved intermittent sprint exercise and endurance exercise performance. However, pre-cooling deteriorated single sprint performance.24 The different impact of pre-cooling on single vs. intermittent sprint exercise may be explained by the longer exercise duration (45–70 sec vs. 40–80 min) and thus higher thermal stress in the intermittent sprint exercise protocols (i.e., soccer, field hockey, tennis and volleyball). Sprint exercise is mainly influenced by muscle temperature and anaerobic metabolism, rather than thermoregulatory factors.24,42 Cooled muscles have a decreased voluntary power output and might have a reduced anaerobic metabolism during sprint exercise.43,44 In contrast, endurance exercise includes performance of prolonged activities on a moderate to high intensity, which results in a greater thermoregulatory burden than sprint exercise. The benefits of pre-cooling are therefore larger for endurance athletes than for (intermittent) sprint athletes.24
Taken together, the effects of pre-cooling greatly depend on the cooling strategy, exercise setting and ambient conditions. The optimal pre-cooling strategy to improve exercise performance includes a vigorous cooling technique that covers a major part of the body and is used during endurance exercise protocols in hot and humid environmental conditions.
Per-cooling
More recently, the use of cooling techniques during exercise became of greater interest. The beneficial effects of pre-cooling normally attenuate after 20–25 minutes of exericse.45 Therefore, cooling athletes during exercise may extend the duration of the performance benefits of a cooling intervention. Additionally, the thermal strain during exercise is much higher compared to resting or warming-up condions,6 which suggests that per-cooling should have a larger potential benefit on thermoregulation and exercise performance compared to pre-cooling. We defined per-cooling as any opportunity to reduce thermal stress during an exercise performance trial. Due to practical feasibility and sporting regulations, less cooling techniques can be applied during exercise compared to pre-cooling. Consequently, the effects of per-cooling were investigated using cooling packs,46-48 cooling vests,49,50 cold water/ice slurry ingestion,37,51 facial wind or water spray cooling52,53 and menthol cooling.54-56 Interestingly, menthol cooling could be applied as a mouth rinse, a gel on the face or as a spray on the clothing of the athlete.
Four reviews were published with respect to per-cooling and exercise performance,22-25 of which 3 conducted a meta-analysis. Per-cooling literature predominantly demonstrated improvements in exercise performance, as 15 out of 21 studies found a positive effect. In our meta-analyses, we concluded that ice vest cooling appeared to be the most effective method followed by cold water ingestion and cooling packs,22 whereas other reviews did not define the most effective per-cooling technique.23,24 The extrapolation of these findings were however limited, as only a single study for ice vest cooling and cold water ingestion was included in the initial analysis, whereas studies with an ambient temperature <30°C were excluded.22 Therefore, we repeated our initial meta-analyses and added 12 recent per-cooling studies to our original approach (Table 2). On average per-cooling results in a 9.3% (ES = 0.35) performance improvement (Fig. 2), which did not differ from pre-cooling (5.7%, ES = 0.44, p = 0.32). Furthermore, per-cooling using cold water/ice slurry ingestion appeared to be the most effective strategy to enhance exercise performance (5.7%, ES = 0.88), followed by an ice- or cooling vest (11.1%, ES = 0.67), facial wind or water spray (18.5%, ES = 0.54), cooling packs (4.4%, ES = 0.33), and menthol cooling (8.7%, ES = 0.23, Fig. 2). These findings suggest that per-cooling is effective in improving exercise performance. However, one must realize that wearing a (heavy) ice vest (∼1 kg)50 or using facial wind or water spray cooling57 may be feasible in laboratory conditions, but is generally not practical during competitive, field-based, settings.
Table 2.
An overview of the studies using per-cooling in relation with exercise performance.
| Study | Exercise protocol | Method of Cooling | Change in exercise performance | Change in temperature | Ambient conditions | Conclusion |
|---|---|---|---|---|---|---|
| Ansley et al. 200846 | Cycling to exhaustion at 75% of VO2 max | Facial water spray cooling (a spray every 30 s) | 51% improvement in time to performance | No difference in Trec | 29°C 50% rh |
Facial water spray cooling improved exercise capacity |
| Barwood et al. 201542 | 16.1-km cycling time trial | Menthol spray on cycling jersey after 10 km | No difference in time trial performance | No difference in Trec | 33.5°C 33% rh |
Menthol spray cooling did not improve time trial performance |
| de Carvalho et al. 201447 | 40-km cycling time trial | Cold water ingestion (10°C, ad libitum) | No difference in time trial performance | No difference in Trec | 35°C 60% rh |
Cold water ingestion did not improve time trial performance |
| Cuttel et al. 2016102 | Cycling to exhaustion at 60% of maximal power output | Ice vest during cycling | 16.7% improvement in time to exhaustion | No difference in Trec | 35°C | Wearing an ice-vest is effective in improving exercise capacity, whereas a neck cooling collar is not effective |
| Neck cooling collar during cycling | No difference in time to exhaustion | No difference in Trec | 50% rh | |||
| Eijsvogels et al. 201436 | 5-km running time trial | Cooling vest during exercise | No difference in time trial performance | No difference in Tgi | 25°C 55% rh |
Wearing a cooling vest did not improve time trial performance |
| Hsu et al. 200549 | 30-km cycling time trial | Hand cooling (22°C) during cycling | 6.6% improvement in exercise time | No difference in Ttymp | 32°C 24% rh |
Hand cooling improved 30-km cycling time trial performance |
| Luomala et al. 201237 | 70 min cycling trial (60% VO2 max) with intermittent-sprints (80% VO2 max) | Ice vest applied after 30 min of exercise, until point of exhaustion | 21.5% improvement of exercise time until exhaustion | No change in Tc | 30°C 40% rh |
Wearing an ice-vest during exercise enhances exercise performance |
| Minetti et al. 201133 | 90 min preloaded running (75 min 60% of VO2 max and 15 min time trial) | Neck collar (−80°C, left in ambient conditions for 5 min before use) | 11.3% improvement of covered distance during 15 min time trial | No difference in Trec | 30°C 53% rh |
Neck collar cooling is effective in improving exercise performance |
| Mündel et al. 200638 | Cycling to exhaustion at 65% of peak aerobic power | Cold water ingestion (3.6°C vs. 19.4°C) | 11% improvement in time to exhaustion | Trec ∼0.25↓ in second half of exercise protocol | 33°C 28% rh |
Cold fluid ingestion improved exercise capacity in the heat |
| Mündel and Jones 201041 | Cycling to exhaustion at 65% of peak aerobic power | 25 mL menthol ingestion every 10 min | 8.6% improvement in time to exhaustion | No difference in Trec | 34°C 27% rh |
Menthol ingestion improved exercise capacity |
| Scheadler et al. 201348 | Running at 75% of VO2 max until exhaustion | Hand cooling | 11.6% impairment of exercise time until exhaustion | No difference in Tc | 30°C 50% rh |
Time to exhaustion was decreased by hand cooling |
| Schlader et al. 201139 | Cycling to exhaustion at RPE of 16 | Facial wind cooling (20°C, 0.74 m/s) | 17.8% improvement in time to exhaustion | No difference in Trec | 20°C | Facial wind cooling as well as menthol gel cooling improved time to exhaustion |
| Facial menthol gel cooling (0.5 g/100 cm2 of skin) | 20.7% improvement in time to exhaustion | No difference in Trec | 48% rh | |||
| Stevens et al. 201640 | 5-km running time trial | Facial water spray cooling (3 sprays every 0.2 km mark) | 2.4% improvement in time trial performance | No difference in Trec | 33°C 34% rh |
Water spray cooling improved time trial performance |
| Stevens et al. 201643 | 5-km running time trial | Menthol mouth rinse cooling (25 mL every 0.2 km mark) | 2.8% improvement in time trial performance | No difference in Trec | 33°C 46% rh |
Menthol mouth rinse improved time trial performance |
| Teunissen et al. 2013103 | 15-km cycling time trial performance | Wind cooling (4 m/s) during kilometers 3–12 | 4.4% improvement in time trial performance | No difference in Trec | 28°C 80% rh |
Wind cooling improved time trial performance |
| Tyler et al. 201035 | Study A: 75 min running 60% of VO2 max and a 15 min self-paced time trial | Neck collar (−80°C, left in ambient conditions for 5 min before use) | Study A: 5.9% improvement of covered distance during time trial | Study A: no difference in neck Tskin | 30°C 50% rh |
Cooling the neck can improve exercise performance in a hot environment. |
| Study B: 15 min running time trial | Study B: no difference total covered distance | Study B: Neck Tskin is lower in cooling condition | 30°C 50% rh |
|||
| Tyler and Sunderland 2011104 | 90 min preloaded running trial (75 min 60% of VO2 max and 15 min self-paced | Neck collar (−80°C, left in ambient conditions for 10 min before use) | 7.0% improvement in time trial performance | Neck temperature is reduced by wearing a neck collar | 30°C 53% rh |
Neck cooling improved time trial performance |
| Tyler and Sunderland 201134 | Running at 70% of VO2 until exhaustion | Neck collar (−80°C, left in ambient conditions for 5 min before use) | 13.5% improvement of exercise time until exhaustion | Neck Tskin is reduced | 32°C | Cooling the neck increased the time until exhaustion |
| Trec = 0.43↑ | 53% rh |
Tc = core body temperature; Tskin = skin temperature; Trec = rectal temperature; Ttymp = tympanic temperature; Tgi = gastrointestinal temperature;
VO2 max = maximal oxygen consumption; rh = relative humidity; RPE = rate of perceived exertion
Figure 2.
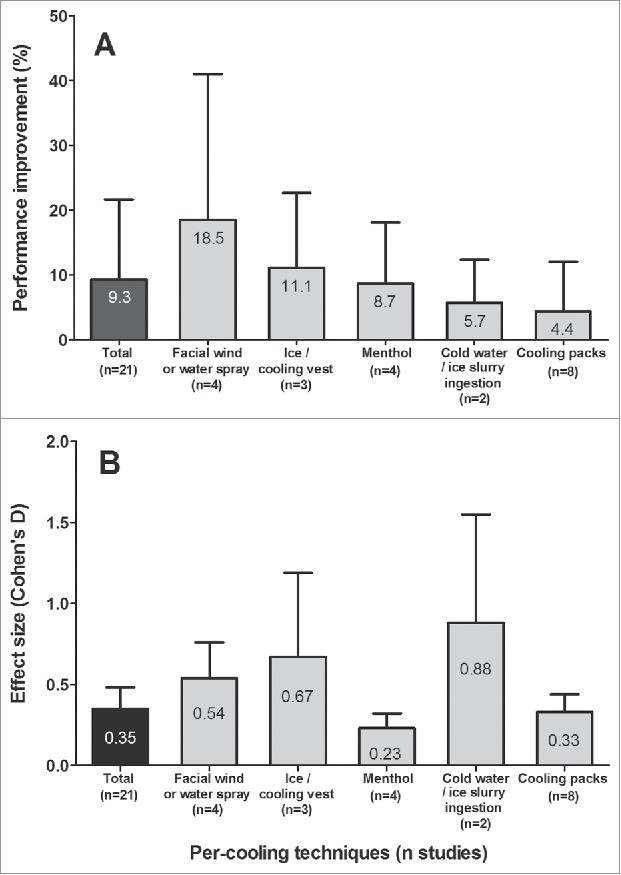
An overview of the average performance improvement (%) (A) and effect size (B) of per-cooling (black bar) and the beneficial effects of different per-cooling strategies (gray bars). Data are presented as mean ± standard deviation.
It is important to note that we have found a discrepancy between the most effective cooling strategy based on the relative performance benefits and the effect size. An explanation for this finding may relate to the low number of per-cooling studies and subsequently low number of tested subjects. Hence, the effect-size is probably a better reflection of the true effects, as it allows a comparison across studies with different setups and sample sizes. Future per-cooling studies are needed to confirm the most effect per-cooling strategy.
The ambient temperature seems to impact the effects of per-cooling, as our analyses revealed a greater performance benefit in moderate (< 30°C, 24.4 ± 4.2°C) compared to hot (≥ 30°C, 32.3 ± 1.9°C) ambient conditions (18.1%, ES = 1.27 vs. 5.9%, ES = 0.28 respectively, p = 0.015), whereas the effects of per-cooling in cold ambient conditions have not be investigated yet. This observation is unexpected, because the thermal load is larger in hot ambient conditions, 58 which should facilitate the potential benefits of cooling. However, there is a large variation in performance benefits in the studies performed in moderate ambient conditions, ranging from a small non-significant negative effect (−0.6%, ES = 0.08)49 to a very large positive effect (51%, ES = 1.17)57 of per-cooling. This variation may possibly be explained by methodological differences in the exercise protocol and outcome measures, as a subjective outcome (rate of perceived exertion) was used as a surrogate for exercise intensity and may therefore influence the time to exhaustion.52 Alternatively, the moderate training status of athletes that were included in these studies may contribute to the large within subject variability of performance benefits using facial water spray cooling.57
A few studies (n = 5, 24% of per-cooling publications) found no difference in exercise performance between the per-cooling and control condition. An explanation may relate to the cooling power of the used interventions. One study used an evaporative cooling vest (∼10°C),49 while another study used cold water ingestion (10°C) to enhance performance.59 The relatively high intervention temperature may be insufficient to elicit a performance benefit. Furthermore, the timing of cooling may explain the absence of an effect. In a menthol cooling study, the menthol spray was applied to the participants cycling jersey after they covered 10 km (62%) of a 16.1-km cycling time trial.55 Accordingly, the menthol spray could only impact performance for a relatively short period of time. Finally, the lack of an effect of per-cooling might be explained by the short exercise duration (15 min) of an experiment,48 in which increases in Tc were insufficient to attenuate exercise performance (peak Tc = 38.4 ± 0.3°C). Taken together, ‘negative-studies’ provide important information to researchers, coaches and athletes as they may aid in the selection of an appropriate cooling protocol.
Only 1 study demonstrated a substantial negative impact (−11.6%, ES = −0.17) of per-cooling on exercise performance.60 In this randomized crossover study, 12 subjects completed 2 time to exhaustion runs at 75% of VO2 max with and without palm cooling in an ambient temperature of (30°C). Time to exhaustion was ∼5.5 minutes longer in the control condition compared to the palm cooling condition. In contrast, another study reported that palm cooling improves 30 km cycling time trial performance in the heat (32°C) with 4 minutes (6.6%, ES = 1.54).61 Therefore, the effects of palm cooling are still unclear and future studies are warranted.
Two studies explored the effects of per-cooling on resistance exercise performance. Intermittent palm cooling between 4 subsets of leg press resistance exercise resulted in a delayed decrement of average power output, resulting in a higher power output in the fourth subset of leg press exercise.62,63 A potential explanation for this finding may relate to temporarily overriding sensations of fatigue.62 The peripheral thermal input may result in a lower awareness of effort while using palm cooling. Therefore, the motor output to contracting muscles is adjusted, by allowing less inhibition of the number of activated motor units, resulting in a higher power output and number of repetitions.63
Concisely, the majority of per-cooling techniques are effective in improving exercise performance in the heat, in which cold water/ice slurry ingestion and wearing an ice-vest seemed to be most effective in laboratory conditions. It is recommended to use sufficient cooling power and continuous cooling exposure during the exercise trial to reach an optimal effect.
Combination of pre- and per-cooling
In addition to the studies that examined the effects of pre-cooling and per-cooling separately, some studies evaluated the combined effect of both types of cooling. We previously hypothesized that combining the advantages of pre-cooling and per-cooling should be more effective in improving exercise performance than a single cooling strategy.22 Until now, 5 studies (with 9 individual comparisons) have examined the effects of a combination of pre- and per-cooling on endurance exercise performance. An overall improvement in exercise performance of 5.6% (range: −1.7% to +23%, ES = 0.63) was found, which did not differ from pre- and percooling (p = 0.23).
Only 1 study found a negative effect (−1.7%, ES = 0.18) of using cold water ingestion (3°C) prior to and during a 20 km cycling time trial in the heat (31°C), whereas pre/per-cooling using an ice slurry (−1°C) or a combination of cold water or ice slurry with a menthol solution were effective in improving performance (3.5%, 5.3% and 8.9% respectively, ES = 0.50, 0.68 and 0.97).64 Furthermore, only 1 study was performed in moderate ambient conditions (28°C).65 Within this study, the ingestion of a menthol aromatized beverage of 3°C was not effective in improving exercise performance (3%, ES = 0.32), whereas a menthol ice slurry (0.2°C) did significantly improve performance (6.2%, ES = 0.67). This may suggest that vigorous cooling or a combination of cooling techniques may have a greater impact on performance, but there is no influence of ambient temperature on the potential benefits.
Post-cooling
Post-cooling is defined as any opportunity to reduce the core, skin and/or muscle temperature directly after exercise, to enhance recovery from exercise and to reduce the exercise-induced muscle soreness. Different post-cooling interventions were described in literature,66 from which cold water immersion (5–15°C) is most frequently used. Furthermore, cold air exposure (−30°C) and local cooling using cooling packs were reported.67,68 Recently, (whole body) cryotherapy has been introduced as a popular post-cooling strategy. Cryotherapy involves exposures to extremely cold dry air (< −100°C) for short periods of time (2–4 minutes).69,70 During cryotherapy individuals wear minimal clothing, gloves, a woolen headband covering the ears, a nose and mouth mask and dry shoes and socks to reduce the risk to develop cold injury.69
In a recent meta-analysis, the effects of post-cooling were subdivided in subjective and objective outcomes for recovery.66 It was found that post-cooling applied directly after exercise improves subjective recovery, since it lowers the symptoms of delayed onset muscle soreness after 24 and 96 hours of recovery.66 Cold water immersion (5–15°C) appeared to be more effective compared to the other post-cooling strategies (cold air exposure, cooling packs and cryotherapy). Post-cooling also reduced subjective rate of perceived exertion after 24 hours of recovery, but not after 48 hours of recovery, whereas similar benefits were observed across different post-cooling techniques. In contrast, there was no evidence that post-cooling had an impact on objective recovery outcomes such as blood lactate, creatinine kinase and c-reactive protein concentration.66 These findings were confirmed in a Cochrane review, which are recognized as the highest standard in evidence-based health care resources. Whole body cold water immersion did not impact maximal strength and maximal power output after 1 to 72 hours of recovery.71 Moreover, no difference in biomarkers for muscle damage (creatine kinase) and inflammatory response (interleukine-6 and c-reactive protein) were found directly post-exercise and after 96 hours of follow-up.71
Another Cochrane review focused solely on the effects of whole body cryotherapy on exercise recovery.69 Four randomized controlled trials were included, with a total of 64 physically active predominantly male subjects. The cryotherapy intervention consisted of an exposure to an ambient temperature ranging from −110°C to −195°C for 3 minutes. Results demonstrated lower levels of delayed onset muscle soreness after 1 hour, 24 hours and 48 hours of recovery in the cryotherapy condition compared to passive rest.69 Objective improvements in recovery after cryotherapy were assessed using a maximal strength measurement. Interestingly, significantly greater maximal strength (range: 5.6% to 12.6%) was found at 24 to 120 hours after post-cooling compared to control.69 Additionally, another study demonstrated that 5 d of cryotherapy (−110°C for 2 min) after a normal daily training program (3 hours) in highly trained athletes induced an increase in anti-inflammatory interleukin-10 and a decrease in the pro-inflammatory interleukin-8 and interleukin-2, suggesting that cryotherapy improves recovery after exercise by reducing the inflammatory response.72 In contrast, 2 minutes of cryotherapy (−135°C) did not impact on plasma interleukin-6 levels after a competitive elite rugby match.73 Although the effects of cryotherapy on the inflammatory response were not consistent, post-exercise cryotherapy seems to attenuate inflammatory response after exercise.
In summary, post-cooling lowers the subjective symptoms of delayed onset muscle soreness, in which cold water immersion is most effective (Fig. 3). In contrast, cryotherapy did impact on objective recovery outcomes such as muscle strength and biomarkers for muscle damage in some studies, whereas cold water immersion did not impact on these objective outcomes. Additionally, cryotherapy may reduce the exercise-induced inflammatory response.
Figure 3.
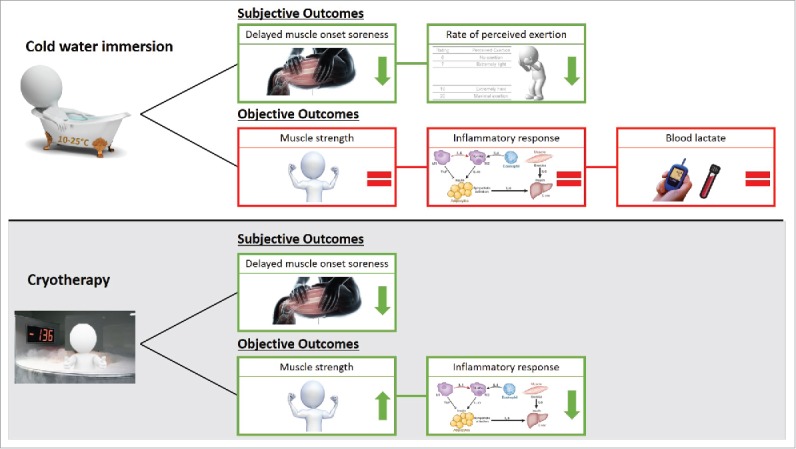
Overview of the effects of post-cooling on recovery from prolonged exercise, in which the effects were divided in subjective and objective outcomes. The ‘arrows’ represents a beneficial effects of post-cooling (↑ = higher, ↓ = lower), whereas the ‘ = sign’ represents no impact of post-cooling.
Theories and mechanisms for pre- and per-cooling benefits
The basis of pre-cooling and per-cooling strategies is to reduce heat stress of the thermoregulatory system prior to and during exercise by increasing the heat storage capacity.17,21 Pre-cooling aims to lower Tc prior the onset of exercise, thereby increasing the margin for metabolic heat production and heat gain.17 The pre-cooling-induced heat buffer enables athletes to perform more work before the critical limit for Tc is reached. Per-cooling aims to attenuate the exercise-induced rise in Tc, which delays the onset of hyperthermia-induced fatigue.22
Critical core temperature theory
It has been shown that muscle power output, and thus heat production, is reduced by elevations in Tc.74 The reduction in muscle power output is regulated by the central nervous system to protect the body to develop heat stroke.74,75 In fact, there may be a neural safeguard mechanism to terminate exercise once a critically high Tc (∼40°C)76 is obtained. This critical core temperature theory is supported by the observation that subjects quitted exercise at a similar Tc, but after dissimilar exercise durations, following repeated exercise bouts at different exercise intensities and starting temperatures.11 Although the study participants voluntary ceased exercise at a Tc of 40.1 ± 0.1°C, the hyperthermia-induced fatigue should not be considered as an all-or-none action.77 It appears to be more likely a dynamic process of progressive inhibition of the brain areas responsible for motor activation with increasing Tc that, together with sensory feedback from the exercising muscles and the cardiovascular system, provokes hyperthermia-induced fatigue during exercise in the heat.77,78 Therefore, a reduction in Tc prior (pre-cooling) or during (per-cooling) exercise may be effective in delaying the hyperthermia-induced fatigue. Pre-cooling predominantly results in a reduced Tc at the end of exercise compared to the control condition, 22 whereas the majority of per-cooling research have found performance improvements without reductions in Tc.22 Therefore, it is likely that other mechanisms are responsible for the beneficial effects of per-cooling.
Anticipatory theory
The rate of heat gain is continuously detected by our body, which could anticipatorily adjust the work rate to ensure that the exercise can be completed within the homeostatic limits of the body.18,22 More specifically, muscle activation during exercise in the heat may be reduced as a feed forward downregulation of muscle drive as an anticipatory reaction to avoid the development of heat-related illnesses.79 This anticipatory concept is supported by a previous study, in which subjects completed 2 20 km self-paced time trials, one in the heat (35°C) and one in the cold (15°C).79 In the hot conditions, subjects reduced power output after 30% of time trial completion, whereas a similar phenomenon occurred at 50% of time trial completion in the cool condition. Furthermore, the rate of Tc increase was comparable between both conditions (0.085 ± 0.030°C/km vs. 0.070 ± 0.017°C/km, p > 0.05).79 So, power output was adjusted well before reaching the critical limiting Tc. Therefore, the anticipatory response of the body may allow that exercise can be completed safely without the development of premature fatigue or heat stroke.79
Core to skin temperature theory
Another mechanism that may contribute to the performance improvements following cooling relates to skin temperature and core to skin temperature gradient. This is confirmed by a recent study that examined time to exhaustion in 4 different groups runners that exercised under different ambient conditions (18°C, 26°C, 34°C and 42°C).14 A significant longer time to exhaustion was found in the 18°C and 26°C condition, with a greater core to skin temperature gradient but similar finishing Tc compared to the 34°C and 42°C condition.14 Therefore, the core to skin temperature gradient has been identified as an important determinant for exercise performance in the heat, in which a larger gradient is advantageous for heat loss.80,81 The ability to sustain endurance exercise performance at a Tc above the critical Tc (>40°C) may be explained by the preservation of a cool skin temperature, which ensures a sufficient core to skin temperature gradient and the ability to stimulate heat loss.81 These findings suggest that retaining a large core to skin temperature gradient may be even more important than keeping Tc below the critical Tc to preserve exercise performance. Therefore, any opportunity to reduce skin temperature prior to or during exercise may be beneficial to increase the core to skin temperature gradient and improve exercise performance.
Cardiovascular and metabolic mechanisms
Next to the direct effects of cooling on thermoregulation and exercise performance, cooling has also an indirect impact on performance via cardiovascular and metabolic mechanisms. Heat stress during endurance exercise is characterized by an increased metabolic82 and cardiovascular strain.83 Moderate heat strain is associated with a reduction in lactate threshold, which is a valid predictor for exercise performance in the heat.84 The heat stress-induced downwards shift in lactate threshold as well as the increased blood lactate accumulation observed during heat stress may be an explanation for performance decrements during heat strain.38,85 Next to metabolic strain, heat stress induces an increase in skin blood flow to dissipate heat, which leads to a reduction in left ventricular stroke volume and limits muscular blood flow and oxygen delivery at the exercising limbs.83 Cooling reduces the stress on the metabolic and cardiovascular system19 as Tc reductions may inhibit blood lactate accumulation and increase the lactate threshold.38 Furthermore, a lower Tc has been shown to reduce heart rate at a given workload,31,32 and to reduce the cutaneous circulation that inhibits cardiac filling.38
Psychophysiological mechanisms
Several studies used menthol application to investigate the effects of changes in thermal perception without changes in Tc and skin temperature.,54,55 Menthol is thought to stimulate a cool feeling 52,56 via stimulation of cold receptors located in the skin86 or oropharyngeal cavity.54 The head and neck region appears to be the best area for menthol cooling,46,48,52 due to a greater density of cold-sensitive afferent thermal receptors.87 Moreover, the mucous membranes of the oropharyngeal cavity are also sensitive for menthol.54 As a result, oral application of menthol may enhance cold sensation in the mouth.88 The menthol-induced cold perception may permit a higher self-selected exercise intensity and subsequent exercise performance improvement.86,89 Interestingly, a single menthol administration on the skin in resting conditions induces a greater increase in cutaneous vasoconstriction, rectal temperature and heat storage compared to oral menthol application and a control condition.90 These results suggests that the modified perceptual signal is stronger than the physiological signal. As a result, the physiological system is overruled, leading to an increased metabolic rate and thus an increased heat production. Therefore, atlethes should be careful while using techniques that evoke a false thermal afferent signal as the discrepance between cold perception and actual Tc / skin temperature may increase the risk to develop heat-related illnesses.
Proposed mechanisms for post-cooling
In many sports, intensive training periods are alternated with strenuous competition phases, in which athletes have to maintain their best performance level for longer periods. Therefore, it is important to stimulate a fast recovery period between intense bouts of exercise. Exercise-induced physiological stress is related to hyperthermia, muscle damage, oxidative stress, inflammation and nervous system fatigue, which can result in a reduced performance potential.91 This reduced capability to perform exercise might be explained by an increased muscle soreness and a decreased muscle function,92 a disturbed muscle reaction time or muscle stiffness that persists for several days.91,93 The application of cold directly after exercise (post-cooling) is often used to improve post-exercise recovery.66,94 Different proposed mechanisms for the recovery benefits of post-cooling were described, including a reduction in inflammatory response,95 a decrease in cardiovascular strain,96 and a decrease in muscle temperature and muscle damage.97 However, the exact mechanisms through which post-cooling affects recovery from exercise are not well understood. Therefore, several suggested potential benefits of post-cooling on exercise recovery are described below.
Inflammatory response
Exercise induces metabolic stress in the active skeletal muscles, resulting in an increased generation of reactive oxygen species (ROS).98 ROS can denaturate proteins, nucleic acids and lipids, resulting in a destabilization of muscle cell structures such as the sarcolemma,99 and the excitation-contraction coupling system.100 Damage to these structures modifies the muscle contraction kinetics, thereby reducing the force-generating capacity and exercise performance.101 Furthermore, a destabilized sarcolemma makes the muscle fibers more permeable,101 which increases the potential to develop muscle fiber edema.102 Edema increases the mechanical stress on muscle fibers, by impairing the oxygen delivery and waste removal, while it also causes muscle soreness.103 Simultaneously with the muscle damage by ROS and muscle fiber edema, an exercise-induced inflammatory response is initiated that causes secondary muscle damage. This type of muscle damage is caused by inflammation in response to exercise and not the exercise per se, which results in muscle soreness and a lower muscle force generating capacity in the days after exercise.104 Cold-induced vasoconstriction of the muscle vasculature and a decreased muscle tissue temperature due to post-cooling may cause reductions in cellular, lymphatic, and capillary permeability, which reduces the fluid diffusion into the interstitial space and decreases the risk of muscle fiber edema.91,95 Moreover, the decreased fluid diffusion, due to cooling, may assist in diminishing the acute inflammatory response to muscle damage. A lower inflammatory response is associated with less pain and lower decrease in muscle force generation.105 Furthermore, the lower inflammatory response after post-cooling can be defined as an increase in an anti-inflammatory cytokine (IL-10), and a decrease in pro-inflammatory cytokines (IL-2, IL-8 and prostaglandin E2).106 Therefore, post-cooling may have an anti-inflammatory response and may be effective in reducing secondary muscle damage, and may therefore enhance muscle recovery.
Cardiovascular & thermoregulatory mechanisms
The implementation of post-cooling directly after a strenuous bout of exercise resulted in a faster reduction in heart rate and core, skin and muscle temperature.68,107 As a result of the faster decrease in heart rate, the cardiovascular strain during recovery is less. In addition, the rapid decrease in skin temperature, due to vigorous whole body cooling (cold water immersion or cryotherapy), causes a peripheral vasoconstriction of the skin. This leads to a diminished peripheral blood flow, resulting in a circulatory shift to the central blood circulation and a quick recovery of the central blood volume.69 The augmented central blood volume and flow increases the ability of an athlete to remove waste products, such as lactate, and therefore may enhance recovery from exercise.
Additionally, post-cooling may immediately reduce the amount of muscle damage. Directly after exercise the muscle fibers are stressed, due to an increased energy demand to repair structural exercise-induced damage and replace energy stores.98 The use of post-cooling decreases the muscle tissue temperature, which causes a decrease in muscle metabolism and therefore a decrease in muscle energy demand.98 Accordingly, the experienced metabolic stress by a muscle may be reduced due to a lower disparity between oxygen supply and oxygen demand. Furthermore, metabolic stress increases the mitochondrial energy production, which significantly contributes to the ROS production of a muscle cell.108 Reducing the mitochondrial energy production by post-cooling may limit the ROS-medicated muscle damage after strenuous exercise. Therefore, it can be suggested that cooling may decrease the muscle stress directly after exercise, resulting in lower muscle soreness.
Furthermore, some studies described an association between muscle tissue temperature and nerve conduction velocity.109,110 Post-cooling is known to reduce the sensory and motor nerve conduction velocity,111 which is associated with an increased pain tolerance and a decreased pain sensation.110 Therefore, a post-exercise decrease in muscle temperature induced by cooling may have a temporary hypoalgesic effect, which attenuates the subjective perception of muscle soreness.
Taken together, post-cooling may enhance recovery from strenuous exercise by reducing the intramuscular temperature and muscle metabolism to reduce the metabolic stress and ROS generation associated with muscle damage, while local vasoconstriction may reduce the formation of edema, the inflammatory response and the associated secondary muscle damage. The subjective pain response to muscle soreness may be diminished by a cooling-induced decrease in nerve conduction velocity.
Cooling and exercise-induced hyperthermia
Next to the effects of pre- and per-cooling on exercise performance, using cooling prior to or during exercise may also attenuate the increase in Tc and reduce the risk to develop heat-related illnesses. We previously described that the finishing Tc was lower in the cooling condition compared to the control condition for pre-cooling experiments (38.9 vs. 39.1, p = 0.03), but not for per-cooling experiments (38.9 vs. 38.9, p = 0.91).22 After adding recently published per-cooling studies to our initial analysis (Table 2), we still did not find a difference in finishing Tc between the per-cooling and control condition (38.7 vs. 38.7, p = 0.95). Based on these data, we may suggest that pre-cooling is effective in reducing thermal stress and lowering the final Tc, whereas it is not known whether pre- or per-cooling reduces the risk to develop heat-related illnesses. The greater metabolic work due to the cooling-induced performance benefit may also contribute to the comparable Tc between the cooling intervention and control conditions. Furthermore, one must realize that none of the included studies reported any heat-related disorders among their participants. This suggests that our body is well able to use internal heat loss mechanisms to cope with an increase in Tc and to avoid critical high Tc that may lead to health problems.
Practical considerations of cooling
The International Association of Athletics Federations World Championships of 2015 were held in Beijing, with expected ambient temperatures between 26–33°C.112 In a cohort study preceding the World Championships, 957 athletes (49% of registered athletes) were included and asked to fill in a precompetition heat strategy questionnaire.112 Based on the questionnaire, approximately 52% of the athletes have a prearranged pre-cooling strategy, from which ice slurry ingestion is most prevalent (24%).112 Additionally, approximately 47% of the athletes planned to use cold water immersion as a recovery strategy.112 These findings highlight the popularity of cooling strategies in professional athletes, but also emphasize that more athletes could benefit from cooling interventions while competing in the heat.
The feasibility and applicability of implementing cooling interventions during training and competition is probably more important than its efficiency in improving exercise performance.21,39 The balance between efficiency and feasibility is reflected in the used
pre- and post-cooling strategies applied during the Athletic World Championships.112 Cold water/ice slurry ingestion and cold water immersion are not the most effective pre-cooling strategies, but can be easily applied in field based settings. In contrast, the use of per-cooling was not observed during this World Championchip. Internal cooling can be particularly suitable as a per-cooling strategy in competitive settings. However, a potential problem of these internal cooling methods is that the intake of large volumes of cold water/ice during exercise may cause gastrointestinal discomfort in some of the subjects.113 Athletes should therefore experiment with the use of internal cooling during regular training sessions, to avoid any discomfort during competitive settings. An alternative easy applicable cooling intervention is the use of local cooling strategies. Cooling packs and evaporative cooling vests are very portable and can be implemented very easily prior to competition as a pre-cooling strategy. Moreover, local cooling as well as internal cooling have the practical benefit that it can be used simultaneously while fulfilling their normal preparations for competition. For post-exercise cooling strategies, cryotherapy may be an effective alternative to cold water immersion. However, it is important to use a maximal exposure duration of 2 to 4 minutes,73 since longer durations do not affect thermal and cardiovascular responses, but increase thermal discomfort of the participants.114 Furthermore, access to cryotherapy is limited, which make it less applicable for recreational athelethes.
Conclusion
Exercise-induced increases in Tc can negatively impact exercise performance and can lead to development of heat-related illnesses. The use of cooling techniques prior to, during or after exercise may attenuate the rise in Tc and may enhance exercise performance. Within this review, we demonstrated that pre-cooling as well as per-cooling are effective in improving exercise performance in both moderate and hot ambient conditions. More specifically, using a mixed method pre-cooling strategy is most effective in improving exercise performance of athletes, whereas cold water/ice slurry ingestion is most favorable per-cooling strategy. Vigorous cooling techniques that cover a large part of the body, or techniques that can be applied frequently, appear to be the best for improvement of exercise performance. An overview of the benefits of cooling interventions is presented in Figure 4. The beneficial effects of pre-cooling and per-cooling may be explained by thermoregulatory as well as cardiovascular and metabolic mechanisms. Post-cooling is primarily focused on facilitating recovery after a strenuous bout of exercise, in which whole body cold water immersion is most effective in reducing the subjective rate of muscle soreness. Furthermore, cryotherapy may have a positive effect on objective outcomes of exercise recovery such as an increased maximal muscle strength and a decreased inflammatory response, whereas these effects were absent after cold water immersion. Taken together, any opportunity to reduce thermal strain prior to, during and/or directly after exercise is an effective strategy to improve time trial performance, exercise capacity and recovery from a stressful bout of exercise.
Figure 4.
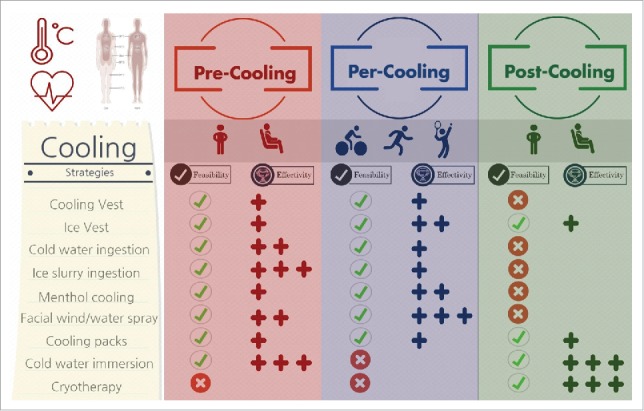
Infographic of the feasibility and effectivity of pre-, per- and post-cooling strategies. The effectivity of cooling techniques is classified as small (+), moderate (++) or large (+++).
Biographies
Coen C.W.G. Bongers is working as a PhD student at the department of Physiolgy of the Radboud university medical center in Nijmegen, the Netherlands. Coen's main research interests are the thermoregulatory and fluid balance responses to prolonged exercise, but he is also interested in potential beneficial strategies to reduce thermal and fluid balance related strain.

Maria T.E. Hopman is a Professor Human Physiology and is interested in the relationship between physical (in)activity and cardiovascular outcomes in healthy and diseased populations. She investigates theadaptation to exercise training and inactivity/deconditioning in humans.

Dr. Thijs M.H. Eijsvogels is an exercise physiologist with a background in thermophysiology and cardiovascular sciences. He aims to understand factors that contribute to variation in exercise-induced elevations in core body temperature, to allow implementation of optimal cooling strategies for preservation of health and enhancement of exercise performance.
Abbreviations
- ES
Effect size
- Per-cooling
Cooling during exercise
- Pre-cooling
Cooling prior to exercise
- Post-cooling
Cooling directly after exercise
- ROS
Reactive oxygen species
- Tc
Core body temperature
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Funding
The work of T.M.H.E is supported by a European Commission Horizon 2020 grant (Marie Sklodowska-Curie Fellowship 655502) and C.C.W.G.B is financially supported by STW (12864).
References
- [1].Bouchama A, Knochel JP. Heat stroke. N Engl J Med 2002; 346:1978-88; PMID:12075060; http://dx.doi.org/ 10.1056/NEJMra011089 [DOI] [PubMed] [Google Scholar]
- [2].W.J. Germann CLS. Principles of human physiology. San Francisco: Benjamin Cummings, 2002. [Google Scholar]
- [3].Commission IT. Glossary of terms for thermal physiology - Third edition (Reprinted from the Japanese Journal of Physiology). J Therm Biol 2003; 28:75-106. [Google Scholar]
- [4].Ament W, Verkerke GJ. Exercise and fatigue. Sports Med 2009; 39:389-422; PMID:19402743; http://dx.doi.org/ 10.2165/00007256-200939050-00005 [DOI] [PubMed] [Google Scholar]
- [5].Edwards RH, Hill DK, Jones DA. Heat production and chemical changes during isometric contractions of the human quadriceps muscle. J Physiol 1975; 251:303-15; PMID:1185666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kenefick RW, Cheuvront SN, Sawka MN. Thermoregulatory function during the marathon. Sports Med 2007; 37:312-5; PMID:17465596 [DOI] [PubMed] [Google Scholar]
- [7].Cheuvront SN, Haymes EM. Thermoregulation and marathon running: biological and environmental influences. Sports Med 2001; 31:743-62; PMID:11547895 [DOI] [PubMed] [Google Scholar]
- [8].Veltmeijer MT, Eijsvogels TM, Thijssen DH, Hopman MT. Incidence and predictors of exertional hyperthermia after a 15-km road race in cool environmental conditions. J Sci Med Sport 2015; 18:333-7; PMID:24930073; http://dx.doi.org/ 10.1016/j.jsams.2014.04.007 [DOI] [PubMed] [Google Scholar]
- [9].Byrne C, Lee JK, Chew SA, Lim CL, Tan EY. Continuous thermoregulatory responses to mass-participation distance running in heat. Med Sci Sports Exerc 2006; 38:803-10; PMID:16672830; http://dx.doi.org/ 10.1249/01.mss.0000218134.74238.6a [DOI] [PubMed] [Google Scholar]
- [10].Muhamed AMC, Atkins K, Stannard SR, Mündel T, Thompson MW. The effects of a systematic increase in relative humidity on thermoregulatory and circulatory responses during prolonged running exercise in the heat. Temperature 2016; 3:455-64; http://dx.doi.org/ 10.1080/23328940.2016.1182669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gonzalez-Alonso J, Teller C, Andersen SL, Jensen FB, Hyldig T, Nielsen B. Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol (1985) 1999; 86:1032-9; PMID:10066720 [DOI] [PubMed] [Google Scholar]
- [12].Wendt D, van Loon LJ, Lichtenbelt WD. Thermoregulation during exercise in the heat: strategies for maintaining health and performance. Sports Med 2007; 37:669-82; PMID:17645370 [DOI] [PubMed] [Google Scholar]
- [13].Casa DJ, DeMartini JK, Bergeron MF, Csillan D, Eichner ER, Lopez RM, Ferrara MS, Miller KC, O'Connor F, Sawka MN, et al.. National athletic trainers' association position statement: exertional heat illnesses. J Athl Train 2015; 50:986-1000; PMID:26381473; http://dx.doi.org/ 10.4085/1062-6050-50.9.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Cuddy JS, Hailes WS, Ruby BC. A reduced core to skin temperature gradient, not a critical core temperature, affects aerobic capacity in the heat. J Therm Biol 2014; 43:7-12; PMID:24956952; http://dx.doi.org/ 10.1016/j.jtherbio.2014.04.002 [DOI] [PubMed] [Google Scholar]
- [15].Kenefick RW, Cheuvront SN, Palombo LJ, Ely BR, Sawka MN. Skin temperature modifies the impact of hypohydration on aerobic performance. J Appl Physiol (1985) 2010; 109:79-86; http://dx.doi.org/ 10.1152/japplphysiol.00135.2010 [DOI] [PubMed] [Google Scholar]
- [16].Buono MJC. P. Hyperthermia during exercise – a double edged sword. Temperature 2016; 3:512-513; http://dx.doi.org/ 10.1080/23328940.2016.1194954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Marino FE. Methods, advantages, and limitations of body cooling for exercise performance. Br J Sports Med 2002; 36:89-94; PMID:11916888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Quod MJ, Martin DT, Laursen PB. Cooling athletes before competition in the heat - Comparison of techniques and practical considerations. Sports Medicine 2006; 36:671-82; PMID:16869709; http://dx.doi.org/ 10.2165/00007256-200636080-00004 [DOI] [PubMed] [Google Scholar]
- [19].Reilly T, Drust B, Gregson W. Thermoregulation in elite athletes. Curr Opin Clin Nutr Metab Care 2006; 9:666-71; PMID:17053417; http://dx.doi.org/ 10.1097/01.mco.0000247475.95026.a5 [DOI] [PubMed] [Google Scholar]
- [20].Siegel R, Mate J, Watson G, Nosaka K, Laursen PB. Pre-cooling with ice slurry ingestion leads to similar run times to exhaustion in the heat as cold water immersion. J Sports Sci 2012; 30:155-65; PMID:22132792; http://dx.doi.org/ 10.1080/02640414.2011.625968 [DOI] [PubMed] [Google Scholar]
- [21].Wegmann M, Faude O, Poppendieck W, Hecksteden A, Frohlich M, Meyer T. Pre-cooling and sports performance: a meta-analytical review. Sports Med 2012; 42:545-64; PMID:22642829; http://dx.doi.org/ 10.2165/11630550-000000000-00000 [DOI] [PubMed] [Google Scholar]
- [22].Bongers CC, Thijssen DH, Veltmeijer MT, Hopman MT, Eijsvogels TM. Precooling and percooling (cooling during exercise) both improve performance in the heat: a meta-analytical review. Br J Sports Med 2015; 49:377-84; PMID:24747298; http://dx.doi.org/ 10.1136/bjsports-2013-092928 [DOI] [PubMed] [Google Scholar]
- [23].Ruddock A, Robbins B, Tew G, Bourke L, Purvis A. Practical cooling strategies during continuous exercise in hot environments: a systematic review and meta-analysis. Sports Med 2016; PMID:27480762; http://dx.doi.org/ 10.1007/s40279-016-0592-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Tyler CJ, Sunderland C, Cheung SS. The effect of cooling prior to and during exercise on exercise performance and capacity in the heat: a meta-analysis. Br J Sports Med 2015; 49:7-13; PMID:23945034; http://dx.doi.org/ 10.1136/bjsports-2012-091739 [DOI] [PubMed] [Google Scholar]
- [25].Stevens CJ, Taylor L, Dascombe BJ. Cooling during exercise: an overlooked strategy for enhancing endurance performance in the heat. Sports Med 2016; http://dx.doi.org/ 10.1007/s40279-016-0625-7 [DOI] [PubMed] [Google Scholar]
- [26].Ellis PD. The essential guide to effect sizes. Cambridge: Cambridge University Press; 2010. [Google Scholar]
- [27].Jones PR, Barton C, Morrissey D, Maffulli N, Hemmings S. Pre-cooling for endurance exercise performance in the heat: a systematic review. BMC Med 2012; 10; http://dx.doi.org/ 10.1186/1741-7015-10-166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ross M, Abbiss C, Laursen P, Martin D, Burke L. Precooling methods and their effects on athletic performance a systematic review and practical applications. Sports Medicine 2013; 43:207-25; PMID:23329610; http://dx.doi.org/ 10.1007/s40279-012-0014-9 [DOI] [PubMed] [Google Scholar]
- [29].Duffield R, Green R, Castle P, Maxwell N. Precooling can prevent the reduction of self-paced exercise intensity in the heat. Med Sci Sport Exer 2010; 42:577-84; http://dx.doi.org/ 10.1249/MSS.0b013e3181b675da [DOI] [PubMed] [Google Scholar]
- [30].Hessemer V, Langusch D, Bruck LK, Bodeker RH, Breidenbach T. Effect of slightly lowered body temperatures on endurance performance in humans. J Appl Physiol Respir Environ Exerc Physiol 1984; 57:1731-7; PMID:6096319 [DOI] [PubMed] [Google Scholar]
- [31].Olschewski H, Bruck K. Thermoregulatory, cardiovascular, and muscular factors related to exercise after precooling. J Appl Physiol (1985) 1988; 64:803-11; PMID:3372438 [DOI] [PubMed] [Google Scholar]
- [32].Schmidt V, Bruck K. Effect of a precooling maneuver on body temperature and exercise performance. J Appl Physiol Respir Environ Exerc Physiol 1981; 50:772-8; PMID:7263359 [DOI] [PubMed] [Google Scholar]
- [33].Arngrimsson SA, Petitt DS, Stueck MG, Jorgensen DK, Cureton KJ. Cooling vest worn during active warm-up improves 5-km run performance in the heat. J Appl Physiol (1985) 2004; 96:1867-74; PMID:14698992; http://dx.doi.org/ 10.1152/japplphysiol.00979.2003 [DOI] [PubMed] [Google Scholar]
- [34].Duffield R, Marino FE. Effects of pre-cooling procedures on intermittent-sprint exercise performance in warm conditions. Eur J Appl Physiol 2007; 100:727-35; PMID:17476523; http://dx.doi.org/ 10.1007/s00421-007-0468-x [DOI] [PubMed] [Google Scholar]
- [35].Castle PC, Macdonald AL, Philp A, Webborn A, Watt PW, Maxwell NS. Precooling leg muscle improves intermittent sprint exercise performance in hot, humid conditions. J Appl Physiol (1985) 2006; 100:1377-84; PMID:16339344; http://dx.doi.org/ 10.1152/japplphysiol.00822.2005 [DOI] [PubMed] [Google Scholar]
- [36].Minett GM, Duffield R, Marino FE, Portus M. Volume-dependent response of precooling for intermittent-sprint exercise in the heat. Med Sci Sports Exerc 2011; 43:1760-9; PMID:21311362; http://dx.doi.org/ 10.1249/MSS.0b013e318211be3e [DOI] [PubMed] [Google Scholar]
- [37].Byrne C, Owen C, Cosnefroy A, Lee JK. Self-paced exercise performance in the heat after pre-exercise cold-fluid ingestion. J Athl Train 2011; 46:592-9; PMID:22488183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].James CA, Richardson AJ, Watt PW, Gibson OR, Maxwell NS. Physiological responses to incremental exercise in the heat following internal and external precooling. Scand J Med Sci Sports 2015; 25:190-9; PMID:25943670; http://dx.doi.org/ 10.1111/sms.12376 [DOI] [PubMed] [Google Scholar]
- [39].Duffield R, Steinbacher G, Fairchild TJ. The use of mixed-method, part-body pre-cooling procedures for team-sport athletes training in the heat. J Strength Cond Res 2009; 23:2524-32; PMID:19910821; http://dx.doi.org/ 10.1519/JSC.0b013e3181bf7a4f [DOI] [PubMed] [Google Scholar]
- [40].Cheung S, Robinson A. The influence of upper-body pre-cooling on repeated sprint performance in moderate ambient temperatures. J Sports Sci 2004; 22:605-12; PMID:15370490; http://dx.doi.org/ 10.1080/02640410310001655813 [DOI] [PubMed] [Google Scholar]
- [41].Kruk B, Pekkarinen H, Harri M, Manninen K, Hanninen O. Thermoregulatory responses to exercise at low ambient-temperature performed after precooling or preheating procedures. Eur J Appl Physiol O 1990; 59:416-20; http://dx.doi.org/ 10.1007/Bf02388622 [DOI] [PubMed] [Google Scholar]
- [42].Girard O, Brocherie F, Bishop DJ. Sprint performance under heat stress: a review. Scand J Med Sci Sports 2015; 25:79-89; PMID:25943658; http://dx.doi.org/ 10.1111/sms.12437 [DOI] [PubMed] [Google Scholar]
- [43].Bigland-Ritchie B, Thomas CK, Rice CL, Howarth JV, Woods JJ. Muscle temperature, contractile speed, and motoneuron firing rates during human voluntary contractions. J Appl Physiol (1985) 1992; 73:2457-61; PMID:1490958 [DOI] [PubMed] [Google Scholar]
- [44].Febbraio MA, Snow RJ, Stathis CG, Hargreaves M, Carey MF. Effect of heat stress on muscle energy metabolism during exercise. J Appl Physiol (1985) 1994; 77:2827-31; PMID:7896628 [DOI] [PubMed] [Google Scholar]
- [45].Bolster DR, Trappe SW, Short KR, Scheffield-Moore M, Parcell AC, Schulze KM, Costill DL. Effects of precooling on thermoregulation during subsequent exercise. Med Sci Sports Exerc 1999; 31:251-7; PMID:10063814 [DOI] [PubMed] [Google Scholar]
- [46].Minniti A, Tyler CJ, Sunderland C. Effects of a cooling collar on affect, ratings of perceived exertion, and running performance in the heat. Eur J Sport Sci 2011; 11:419-29; http://dx.doi.org/ 10.1080/17461391.2010.536577 [DOI] [Google Scholar]
- [47].Tyler CJ, Sunderland C. Cooling the neck region during exercise in the heat. J Athl Training 2011; 46:61-8; http://dx.doi.org/ 10.4085/1062-6050-46.1.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Tyler CJ, Wild P, Sunderland C. Practical neck cooling and time-trial running performance in a hot environment. Eur J Appl Physiol 2010; 110:1063-74; PMID:20694731; http://dx.doi.org/ 10.1007/s00421-010-1567-7 [DOI] [PubMed] [Google Scholar]
- [49].Eijsvogels TM, Bongers CC, Veltmeijer MT, Moen MH, Hopman M. Cooling during exercise in temperate conditions: impact on performance and thermoregulation. Int J Sports Med 2014; 35:840-6; PMID:24771132; http://dx.doi.org/ 10.1055/s-0034-1368723 [DOI] [PubMed] [Google Scholar]
- [50].Luomala MJ, Oksa J, Salmi JA, Linnamo V, Holmer I, Smolander J, Dugue B. Adding a cooling vest during cycling improves performance in warm and humid conditions. J Therm Biol 2012; 37:47-55; http://dx.doi.org/ 10.1016/j.jtherbio.2011.10.009 [DOI] [Google Scholar]
- [51].Mundel T, King J, Collacott E, Jones DA. Drink temperature influences fluid intake and endurance capacity in men during exercise in a hot, dry environment. Exp Physiol 2006; 91:925-33; PMID:16777932; http://dx.doi.org/ 10.1113/expphysiol.2006.034223 [DOI] [PubMed] [Google Scholar]
- [52].Schlader ZJ, Simmons SE, Stannard SR, Mundel T. The independent roles of temperature and thermal perception in the control of human thermoregulatory behavior. Physiol Behav 2011; 103:217-24; PMID:21315099; http://dx.doi.org/ 10.1016/j.physbeh.2011.02.002 [DOI] [PubMed] [Google Scholar]
- [53].Stevens CJ, Kittel A, Sculley DV, Callister R, Taylor L, Dascombe BJ. Running performance in the heat is improved by similar magnitude with pre-exercise cold-water immersion and mid-exercise facial water spray. J Sports Sci 2016; 1-8; PMID:27267974; http://dx.doi.org/ 10.1080/02640414.2016.1192294 [DOI] [PubMed] [Google Scholar]
- [54].Mundel T, Jones DA. The effects of swilling an L(-)-menthol solution during exercise in the heat. Eur J Appl Physiol 2010; 109:59-65; PMID:19727797; http://dx.doi.org/ 10.1007/s00421-009-1180-9 [DOI] [PubMed] [Google Scholar]
- [55].Barwood MJ, Corbett J, Thomas K, Twentyman P. Relieving thermal discomfort: Effects of sprayed L-menthol on perception, performance, and time trial cycling in the heat. Scand J Med Sci Sports 2015; 25:211-8; PMID:25943672; http://dx.doi.org/ 10.1111/sms.12395 [DOI] [PubMed] [Google Scholar]
- [56].Stevens CJ, Thoseby B, Sculley DV, Callister R, Taylor L, Dascombe BJ. Running performance and thermal sensation in the heat are improved with menthol mouth rinse but not ice slurry ingestion. Scand J Med Sci Sports 2016; 26:1209-16; PMID:26408395; http://dx.doi.org/ 10.1111/sms.12555 [DOI] [PubMed] [Google Scholar]
- [57].Ansley L, Marvin G, Sharma A, Kendall MJ, Jones DA, Bridge MW. The effects of head cooling on endurance and neuroendocrine responses to exercise in warm conditions. Physiol Res 2008; 57:863-72; PMID:18052690 [PubMed] [Google Scholar]
- [58].Junge N, Jørgensen R, Flouris AD, Nybo L. Prolonged self-paced exercise in the heat – Environmental factors affecting performance. Temperature 2016; 3:1-10; http://dx.doi.org/ 10.1080/23328940.2016.1216257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].De Carvalho MV, De Andrade MT, Ramos GP, Maia-Lima A, Pereira ER, Mendes TT, Marins JC, Amorim FT, Silami-Garcia E. The temperature of water ingested ad libitum does not influence performance during a 40-km self-paced cycling trial in the heat. J Sports Med Phys Fitness 2015; 55:1473-9; PMID:25286889 [PubMed] [Google Scholar]
- [60].Scheadler CM, Saunders NW, Hanson NJ, Devor ST. Palm cooling does not improve running performance. Int J Sports Med 2013; 34:732-5; PMID:23444094; http://dx.doi.org/ 10.1055/s-0032-1327576 [DOI] [PubMed] [Google Scholar]
- [61].Hsu AR, Hagobian TA, Jacobs KA, Attallah H, Friedlander AL. Effects of heat removal through the hand on metabolism and performance during cycling exercise in the heat. Can J Appl Physiol 2005; 30:87-104; PMID:15855685 [DOI] [PubMed] [Google Scholar]
- [62].Caruso JF, Barbosa A, Erickson L, Edwards R, Perry R, Learmonth L, Potter WT. Intermittent palm cooling's impact on resistive exercise performance. Int J Sports Med 2015; 36:814-21; PMID:26038879; http://dx.doi.org/ 10.1055/s-0035-1547264 [DOI] [PubMed] [Google Scholar]
- [63].Kwon YS, Robergs RA, Mermier CM, Schneider SM, Gurney AB. Palm cooling and heating delays fatigue during resistance exercise in women. J Strength Cond Res 2015; 29:2261-9; PMID:23722108; http://dx.doi.org/ 10.1519/JSC.0b013e31829cef4e [DOI] [PubMed] [Google Scholar]
- [64].Riera F, Trong TT, Sinnapah S, Hue O. Physical and perceptual cooling with beverages to increase cycle performance in a tropical climate. PLoS One 2014; 9: e103718; PMID:25084009; http://dx.doi.org/ 10.1371/journal.pone.0103718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Tran Trong T, Riera F, Rinaldi K, Briki W, Hue O. Ingestion of a cold temperature/menthol beverage increases outdoor exercise performance in a hot, humid environment. PLoS One 2015; 10: e0123815; PMID:25856401; http://dx.doi.org/ 10.1371/journal.pone.0123815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Hohenauer E, Taeymans J, Baeyens JP, Clarys P, Clijsen R. The effect of post-exercise cryotherapy on recovery characteristics: a systematic review and meta-analysis. PLoS One 2015; 10: e0139028; PMID:26413718; http://dx.doi.org/ 10.1371/journal.pone.0139028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Guilhem G, Hug F, Couturier A, Regnault S, Bournat L, Filliard JR, Dorel S. Effects of air-pulsed cryotherapy on neuromuscular recovery subsequent to exercise-induced muscle damage. Am J Sports Med 2013; 41:1942-51; PMID:23739686; http://dx.doi.org/ 10.1177/0363546513490648 [DOI] [PubMed] [Google Scholar]
- [68].Pointon M, Duffield R, Cannon J, Marino FE. Cold application for neuromuscular recovery following intense lower-body exercise. Eur J Appl Physiol 2011; 111:2977-86; PMID:21445604; http://dx.doi.org/ 10.1007/s00421-011-1924-1 [DOI] [PubMed] [Google Scholar]
- [69].Costello JT, Baker PR, Minett GM, Bieuzen F, Stewart IB, Bleakley C. Whole-body cryotherapy (extreme cold air exposure) for preventing and treating muscle soreness after exercise in adults. Cochrane Database Syst Rev 2015): CD010789; http://dx.doi.org/ 10.1002/14651858.CD010789.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Bleakley CM, Bieuzen F, Davison GW, Costello JT. Whole-body cryotherapy: empirical evidence and theoretical perspectives. Open Access J Sports Med 2014; 10:25-36; http://dx.doi.org/ 10.2147/OAJSM.S41655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Bleakley C, McDonough S, Gardner E, Baxter GD, Hopkins JT, Davison GW. Cold-water immersion (cryotherapy) for preventing and treating muscle soreness after exercise. Cochrane Database Syst Rev 2012; 15: CD008262; http://dx.doi.org/ 10.1002/14651858.CD008262.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Banfi G, Melegati G, Barassi A, Dogliotti G, d'Eril GM, Dugue B, Corsi MM. Effects of whole-body cryotherapy on serum mediators of inflammation and serum muscle enzymes in athletes. J Therm Biol 2009; 34:55-9; http://dx.doi.org/ 10.1016/j.jtherbio.2008.10.003 [DOI] [Google Scholar]
- [73].Selfe J, Alexander J, Costello JT, May K, Garratt N, Atkins S, Dillon S, Hurst H, Davison M, Przybyla D, et al.. The effect of three different (−135°C) whole body cryotherapy exposure durations on elite rugby league players. PLoS One 2014; 9:e86420; PMID:24489726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Cheung SS. Hyperthermia and voluntary exhaustion: integrating models and future challenges. Appl Physiol Nutr Metab 2007; 32:808-17; PMID:17622299; http://dx.doi.org/ 10.1139/H07-043 [DOI] [PubMed] [Google Scholar]
- [75].Siegel R, Laursen PB. Keeping your cool: possible mechanisms for enhanced exercise performance in the heat with internal cooling methods. Sports Med 2012; 42:89-98; PMID:22175533; http://dx.doi.org/ 10.2165/11596870-000000000-00000 [DOI] [PubMed] [Google Scholar]
- [76].Nybo L. Hyperthermia and fatigue. J Appl Physiol (1985) 2008; 104:871-8; PMID:17962572; http://dx.doi.org/ 10.1152/japplphysiol.00910.2007 [DOI] [PubMed] [Google Scholar]
- [77].Nybo L, Rasmussen P, Sawka MN. Performance in the heat-physiological factors of importance for hyperthermia-induced fatigue. Compr Physiol 2014; 4:657-89; PMID:24715563; http://dx.doi.org/ 10.1002/cphy.c130012 [DOI] [PubMed] [Google Scholar]
- [78].Nybo L, Nielsen B. Hyperthermia and central fatigue during prolonged exercise in humans. J Appl Physiol (1985) 2001; 91:1055-60; PMID:11509498 [DOI] [PubMed] [Google Scholar]
- [79].Tucker R, Rauch L, Harley YXR, Noakes TD. Impaired exercise performance in the heat is associated with an anticipatory reduction in skeletal muscle recruitment. Pflug Arch Eur J Phy 2004; 448:422-30; http://dx.doi.org/ 10.1007/s00424-004-1267-4 [DOI] [PubMed] [Google Scholar]
- [80].Cheuvront SN, Kenefick RW, Montain SJ, Sawka MN. Mechanisms of aerobic performance impairment with heat stress and dehydration. J Appl Physiol (1985) 2010; 109:1989-95; PMID:20689090; http://dx.doi.org/ 10.1152/japplphysiol.00367.2010 [DOI] [PubMed] [Google Scholar]
- [81].Ely BR, Ely MR, Cheuvront SN, Kenefick RW, Degroot DW, Montain SJ. Evidence against a 40°C core temperature threshold for fatigue in humans. J Appl Physiol (1985) 2009; 107:1519-25; PMID:19713430; http://dx.doi.org/ 10.1152/japplphysiol.00577.2009 [DOI] [PubMed] [Google Scholar]
- [82].Parkin JM, Carey MF, Zhao S, Febbraio MA. Effect of ambient temperature on human skeletal muscle metabolism during fatiguing submaximal exercise. J Appl Physiol (1985) 1999; 86:902-8; PMID:10066703 [DOI] [PubMed] [Google Scholar]
- [83].Gonzalez-Alonso J, Crandall CG, Johnson JM. The cardiovascular challenge of exercising in the heat. J Physiol 2008; 586:45-53; PMID:17855754; http://dx.doi.org/ 10.1113/jphysiol.2007.142158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Lorenzo S, Minson CT, Babb TG, Halliwill JR. Lactate threshold predicting time-trial performance: impact of heat and acclimation. J Appl Physiol (1985) 2011; 111:221-7; PMID:21527667; http://dx.doi.org/ 10.1152/japplphysiol.00334.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Hargreaves M. Physiological limits to exercise performance in the heat. J Sci Med Sport 2008; 11:66-71; PMID:17720623; http://dx.doi.org/ 10.1016/j.jsams.2007.07.002 [DOI] [PubMed] [Google Scholar]
- [86].Cheung SS. Interconnections between thermal perception and exercise capacity in the heat. Scand J Med Sci Spor 2010; 20:53-9; http://dx.doi.org/ 10.1111/j.1600-0838.2010.01209.x [DOI] [PubMed] [Google Scholar]
- [87].Cotter JD, Taylor NA. The distribution of cutaneous sudomotor and alliesthesial thermosensitivity in mildly heat-stressed humans: an open-loop approach. J Physiol 2005; 565:335-45; PMID:15760945; http://dx.doi.org/ 10.1113/jphysiol.2004.081562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Green BG. Menthol modulates oral sensations of warmth and cold. Physiol Behav 1985; 35:427-34; PMID:4070414 [DOI] [PubMed] [Google Scholar]
- [89].Mundel T, Raman A, Schlader ZJ. Head temperature modulates thermal behavior in the cold in humans. Temperature 2016; 3:298-306; PMID:27857959; http://dx.doi.org/ 10.1080/23328940.2016.1156214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Valente A, Carrillo AE, Tzatzarakis MN, Vakonaki E, Tsatsakis AM, Kenny GP, Koutedakis Y, Jamurtas AZ, Flouris AD. The absorption and metabolism of a single L-menthol oral versus skin administration: Effects on thermogenesis and metabolic rate. Food Chem Toxicol 2015; 86:262-73; PMID:26429629; http://dx.doi.org/ 10.1016/j.fct.2015.09.018 [DOI] [PubMed] [Google Scholar]
- [91].Leeder J, Gissane C, van Someren K, Gregson W, Howatson G. Cold water immersion and recovery from strenuous exercise: a meta-analysis. Br J Sports Med 2012; 46:233-40; PMID:21947816; http://dx.doi.org/ 10.1136/bjsports-2011-090061 [DOI] [PubMed] [Google Scholar]
- [92].McHugh MP, Connolly DA, Eston RG, Gleim GW. Exercise-induced muscle damage and potential mechanisms for the repeated bout effect. Sports Med 1999; 27:157-70; PMID:10222539 [DOI] [PubMed] [Google Scholar]
- [93].Paschalis V, Nikolaidis MG, Giakas G, Jamurtas AZ, Owolabi EO, Koutedakis Y. Position sense and reaction angle after eccentric exercise: the repeated bout effect. Eur J Appl Physiol 2008; 103:9-18; PMID:18172668; http://dx.doi.org/ 10.1007/s00421-007-0663-9 [DOI] [PubMed] [Google Scholar]
- [94].Poppendieck W, Faude O, Wegmann M, Meyer T. Cooling and performance recovery of trained athletes: a meta-analytical review. Int J Sports Physiol Perform 2013; 8:227-42; PMID:23434565 [DOI] [PubMed] [Google Scholar]
- [95].Ascensao A, Leite M, Rebelo AN, Magalhaes S, Magalhaes J. Effects of cold water immersion on the recovery of physical performance and muscle damage following a one-off soccer match. J Sports Sci 2011; 29:217-25; PMID:21170794; http://dx.doi.org/ 10.1080/02640414.2010.526132 [DOI] [PubMed] [Google Scholar]
- [96].Vaile J, O'Hagan C, Stefanovic B, Walker M, Gill N, Askew CD. Effect of cold water immersion on repeated cycling performance and limb blood flow. Br J Sports Med 2011; 45:825-9; PMID:20233843; http://dx.doi.org/ 10.1136/bjsm.2009.067272 [DOI] [PubMed] [Google Scholar]
- [97].Eston R, Peters D. Effects of cold water immersion on the symptoms of exercise-induced muscle damage. J Sports Sci 1999; 17:231-8; PMID:10362390; http://dx.doi.org/ 10.1080/026404199366136 [DOI] [PubMed] [Google Scholar]
- [98].White GE, Wells GD. Cold-water immersion and other forms of cryotherapy: physiological changes potentially affecting recovery from high-intensity exercise. Extrem Physiol Med 2013; 2:26; PMID:24004719; http://dx.doi.org/ 10.1186/2046-7648-2-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Powers SK, Jackson MJ. Exercise-induced oxidative stress: Cellular mechanisms and impact on muscle force production. Physiol Rev 2008; 88:1243-76; PMID:18923182; http://dx.doi.org/ 10.1152/physrev.00031.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Zembron-Lacny A, Naczk M, Gajewski M, Ostapiuk-Karolczuk J, Dziewiecka H, Kasperska A, Szyszka K. Changes of muscle-derived cytokines in relation to thiol redox status and reactive oxygen and nitrogen species. Physiol Res 2010; 59:945-51; PMID:20533854 [DOI] [PubMed] [Google Scholar]
- [101].Kendall B, Eston R. Exercise-induced muscle damage and the potential protective role of estrogen. Sports Med 2002; 32:103-23; PMID:11817996 [DOI] [PubMed] [Google Scholar]
- [102].Yanagisawa O, Niitsu M, Takahashi H, Goto K, Itai Y. Evaluations of cooling exercised muscle with MR imaging and P-31 MR spectroscopy. Med Sci Sport Exer 2003; 35:1517-23; http://dx.doi.org/ 10.1249/01.Mss.0000084418.96898.2e [DOI] [PubMed] [Google Scholar]
- [103].Swenson C, Sward L, Karlsson J. Cryotherapy in sports medicine. Scand J Med Sci Sports 1996; 6:193-200; PMID:8896090 [DOI] [PubMed] [Google Scholar]
- [104].Butterfield TA, Best TM, Merrick MA. The dual roles of neutrophils and macrophages in inflammation: a critical balance between tissue damage and repair. J Athl Train 2006; 41:457-65; PMID:17273473 [PMC free article] [PubMed] [Google Scholar]
- [105].Smith LL. Acute inflammation: the underlying mechanism in delayed onset muscle soreness? Med Sci Sports Exerc 1991; 23:542-51; PMID:2072832 [PubMed] [Google Scholar]
- [106].Banfi G, Lombardi G, Colombini A, Melegati G. Whole-body cryotherapy in athletes. Sports Med 2010; 40:509-17; PMID:20524715; http://dx.doi.org/ 10.2165/11531940-000000000-00000 [DOI] [PubMed] [Google Scholar]
- [107].Roberts LA, Muthalib M, Stanley J, Lichtwark G, Nosaka K, Coombes JS, Peake JM. Effects of cold water immersion and active recovery on hemodynamics and recovery of muscle strength following resistance exercise. Am J Physiol Regul Integr Comp Physiol 2015; 309: R389-98; PMID:26062633; http://dx.doi.org/ 10.1152/ajpregu.00151.2015 [DOI] [PubMed] [Google Scholar]
- [108].Debold EP. Recent insights into muscle fatigue at the cross-bridge level. Front Physiol 2012; 3; PMID:22675303; http://dx.doi.org/ 10.3389/fphys.2012.00151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Herrera E, Sandoval MC, Camargo DM, Salvini TF. Effect of walking and resting after three cryotherapy modalities on the recovery of sensory and motor nerve conduction velocity in healthy subjects. Rev Bras Fisioter 2011; 15:233-40; PMID:21829988 [DOI] [PubMed] [Google Scholar]
- [110].Algafly AA, George KP. The effect of cryotherapy on nerve conduction velocity, pain threshold and pain tolerance. Br J Sports Med 2007; 41:365-9; discussion 9; PMID:17224445; http://dx.doi.org/ 10.1136/bjsm.2006.031237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Herrera E, Sandoval MC, Camargo DM, Salvini TF. Motor and sensory nerve conduction are affected differently by ice pack, ice massage, and cold water immersion. Phys Ther 2010; 90:581-91; PMID:20185615; http://dx.doi.org/ 10.2522/ptj.20090131 [DOI] [PubMed] [Google Scholar]
- [112].Periard JD, Racinais S, Timpka T, Dahlstrom O, Spreco A, Jacobsson J, Bargoria V, Halje K, Alonso JM. Strategies and factors associated with preparing for competing in the heat: a cohort study at the 2015 IAAF World Athletics Championships. Br J Sports Med 2016; http://dx.doi.org/ 10.1136/bjsports-2016-096579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Stevens CJ, Dascombe B, Boyko A, Sculley D, Callister R. Ice slurry ingestion during cycling improves Olympic distance triathlon performance in the heat. J Sports Sci 2013; 31:1271-9; PMID:23506436; http://dx.doi.org/ 10.1080/02640414.2013.779740 [DOI] [PubMed] [Google Scholar]
- [114].Fonda B, De Nardi M, Sarabon N. Effects of whole-body cryotherapy duration on thermal and cardio-vascular response. J Therm Biol 2014; 42:52-5; PMID:24802149; http://dx.doi.org/ 10.1016/j.jtherbio.2014.04.001 [DOI] [PubMed] [Google Scholar]
- [115].Cuttell SA, Kiri V, Tyler C. A comparison of 2 practical cooling methods on cycling capacity in the heat. J Athl Train 2016; 51:525-32; PMID:27571045; http://dx.doi.org/ 10.4085/1062-6050-51.8.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Teunissen LP, de Haan A, de Koning JJ, Daanen HA. Effects of wind application on thermal perception and self-paced performance. Eur J Appl Physiol 2013; 113:1705-17; PMID:23385657; http://dx.doi.org/ 10.1007/s00421-013-2596-9 [DOI] [PubMed] [Google Scholar]
- [117].Tyler CJ, Sunderland C. Neck cooling and running performance in the heat: single versus repeated application. Med Sci Sport Exer 2011; 43:2388-95; http://dx.doi.org/ 10.1249/MSS.0b013e318222ef72 [DOI] [PubMed] [Google Scholar]


