Abstract
Background
Childhood maltreatment, particularly physical abuse (PA), increases the risk of alcohol use during young adulthood. Although prior research underscores the importance of examining the roles of PA-event characteristics such as timing of and chronicity of PA in initiating and maintaining alcohol use, few studies have explored the risk of developing alcohol use based on the timing and chronicity of PA.
Methods
Using a community sample of 300 young adults (ages 18-25), the present study examined how variations in timing and chronicity of PA relate to four distinct drinking behaviors including drinking frequency, binge drinking, alcohol-related problems, and alcohol use disorder in the past 12 months. We controlled for sociodemographic information, other types of maltreatment and common risk factors for alcohol use, such as psychological distress, parental alcoholism, and peer alcohol use in all analyses. The present study used person-centered and developmental-stage-based characterizations of PA timing and chronicity to explore the relationship between timing and chronicity of PA and later drinking behaviors.
Results
Overall, individuals who were physically abused, particularly during adolescence, and who chronically experienced PA, reported higher levels of monthly drinking frequency and more pathological drinking behaviors such as binge drinking, alcohol-related problems, and alcohol use disorder.
Conclusions
The present study describes the specific roles of timing and chronicity of PA in understanding the increased vulnerability to alcohol use among victims of PA. Our findings suggest that PA during adolescence and chronic PA are related to problematic drinking behaviors in young adulthood.
Keywords: Child maltreatment, sensitive periods, alcohol use, maltreatment timing, chronicity
Introduction
Child abuse and neglect is a major public health problem in the United States, which affects approximately 679,000 children every year (U.S. Department of Health and Human Services, 2014). It is estimated that one in four children experiences at least one form of maltreatment during childhood, 18% of whom are victims of physical abuse (U.S. Centers for Disease Control and Prevention, 2014). Childhood physical abuse (CPA) markedly increases the risk for an array of adverse health and behavioral outcomes throughout a child’s life, including alcohol use (Dube et al., 2006, Fenton et al., 2013). For example, using a population-based epidemiological dataset of 8,503 adolescents and young adults, our previous longitudinal study found that CPA occurring prior to 6th grade was associated with faster increases in binge drinking during adolescence and persistently elevated binge drinking over much of young adulthood (Shin et al., 2013). Further, victims of child maltreatment including CPA are a subpopulation of alcohol users, particularly resistant to alcohol treatment (Francke et al., 2013).
Although a large body of research substantiates the strong relationship between CPA and later alcohol use, this relationship is undoubtedly complex, and is influenced by a large number of factors including characteristics of maltreatment such as developmental timing and chronicity. For instance, emerging studies have suggested that health and behavioral outcomes of child maltreatment are partially dependent on the timing of each maltreatment episode (Cowell et al., 2015, Thornberry et al., 2010). Recent neurobiological studies also support such hypotheses in that different brain regions have individual neurodevelopmental sensitive periods when they are maximally susceptible to the effects of early stress (Andersen, 2008, Pechtel et al., 2014). There is a dearth of research investigating how variations in the developmental stages in which the physical abuse occurs and in the number of developmental stages in which children experienced CPA influences later alcohol use. Therefore, research into the developmental timing and chronicity of CPA and its impact on later alcohol use might provide important insights into the increased vulnerability to alcohol use among victims of CPA.
The examination of specific impacts of developmental timing of CPA is particularly necessary due to researchers’ increasing recognition of diverse childhood experiences and the dynamic nature of maltreatment episodes (Manly, 2005). Previous studies examining timing effects of child maltreatment on later behavioral adjustments have found the detrimental impact of maltreatment that occurred in early childhood such as infancy and toddlerhood (Kaplow and Widom, 2007, Keiley et al., 2001). Using a growth modeling analysis of a sample of 578 children followed from kindergarten to eighth grade, Keiley and colleagues (2001) found that compared to non-physical abuse and late physical abuse (abuse onset between age 6 and 9), early physical abuse (onset before age 5) was related to higher initial levels of internalizing and externalizing problems, and higher and more stable levels of externalizing problems over the nine years (Keiley et al., 2001). Furthermore, in a prospective longitudinal study of 494 children who had substantiated child abuse or neglect court records, Kaplow and Widom (2007) found that compared to late child maltreatment (ages 6-11 years), early child maltreatment (ages 0-5 years) was associated with higher levels of internalizing problems such as anxiety and depressive symptoms at age 40 (Kaplow and Widom, 2007). Supporting these findings, some theories of human development, such as developmental psychopathology perspectives, emphasize the primacy of early childhood development (Cicchetti and Toth, 1995). It suggests that since early childhood is a time of rapid growth in numerous developmental domains, the earlier maltreatment occurs the greater the possibility of experiencing adverse childhood outcomes, which interfere with further adolescent development and leave a lasting impact on later alcohol use.
Contrary to the hypothesis proposed by the developmental psychopathology perspectives, some studies have reported the opposite findings (Smith et al., 2005, Thornberry et al., 2001). For example, Thornberry, Ireland and Smith (2001) interviewed 738 at-risk youth who lived in a high crime area, and found that compared to adolescents whose maltreatment occurred in either early (ages 0-5 years) or late (ages 6-11years) childhood, young people who experienced maltreatment in adolescence (ages 12-17 years) are more likely to be involved in illicit drug use, including alcohol use, during late adolescence (Thornberry et al., 2001). Following the same youth into young adulthood, Smith and colleagues (2005) also found that compared to young people abused in childhood, young adults who are maltreated during adolescence were more at risk of alcohol and other illicit drug use at ages 20–22, after controlling for demographics, SES, and prior problem behaviors (Smith et al., 2005). Similarly, some theorists have argued that increased sense of self and cognitive abilities during adolescence may increase the likelihood of experiencing shame and self-blame among adolescent victims of maltreatment, which lead to alcohol use (Shaver and Drown, 1986). Furthermore, since adolescence is often characterized by reduced social and parental control, and greater autonomy, adolescents, more so than younger children, tend to respond to victimization and maltreatment by engaging in antisocial behavior or unhealthy coping strategies such as binge drinking.
Exploring the significance of the timing in which the maltreatment occurred, researchers argued that the timing of maltreatment might interact with chronicity of maltreatment (e.g., single episode vs. chronic maltreatment) in guiding child development and influencing the well-being of maltreated children. For instance, Jaffee and Maikovich-Fong (2011) found in a longitudinal sample of 1,777 children (ages 0-9 years) that compared to maltreatment experienced only at one developmental stage, maltreatment at multiple developmental stages led to an increase in internalizing and externalizing problems as well as a lower IQ score (Jaffee and Maikovich-Fong, 2011). Thornberry and his colleagues (2001) also found that compared to childhood-only maltreatment, persistent maltreatment across childhood and adolescence increased the risk for adolescent alcohol and drug use (Thornberry et al., 2001). The above findings demonstrate that based on when the maltreatment occurs and how long the victimization episodes last, different trajectories of psychosocial development can be experienced into young adulthood, dealing with a multitude of problem behaviors as a result of the specific timing and chronicity of maltreatment. While recent studies have highlighted the importance of developmental timing of maltreatment, there is still much to uncover before enough is known about the mechanisms explaining the association between timing of maltreatment and its sequelae.
The majority of research on the impact of developmental timing of child maltreatment has classified the timing by artificially grouping children by all possible combinations of maltreatment timing. However, such a classification technique hardly allows for the identification of the combinations of maltreatment timing that most commonly occurred in a sample. Instead, it might potentially result in cumbersome and less useful findings, particularly when a sample contains multiple combinations of maltreatment timing. Therefore, recent studies have recognized the utility of person-centered approaches such as latent class analysis (LCA) (Villodas et al., 2012). Since LCA allows for identifying unobserved groups of individuals with similar characteristics of maltreatment timing, it helps researchers empirically identify only those developmental timings that occur most frequently in a given sample and classify individuals into classes (i.e., groups), each one of which contains individuals who are similar to each other in maltreatment timing and different from individuals in other classes. LCA is particularly useful in child maltreatment research, where data often include heterogeneous groups of individuals who are maltreated in different stages of life course.
Since the majority of maltreatment timing studies have manually grouped children together based on developmental stages in which child maltreatment occurred, we employed both LCA and “developmental” classification of CPA timing to explore the relationship between developmental timing of CPA and later drinking behaviors, and to examine the utility of two different characterizations of maltreatment timing. The present study used a community sample of young adults and examined whether timing and chronicity of CPA play a significant role in linking exposure to CPA to alcohol use in young adulthood. We hypothesized that (a) physical maltreatment occurring during adolescence would be more associated with alcohol use in young adulthood than no-CPA and physical abuse that occurred before adolescence; and (b) chronic maltreatment would be related to more pathological alcohol use than maltreatment occurring in only one developmental period.
Materials and Methods
Participants
Participants for the study were recruited through community advertisements within a metropolitan area, using online and offline bulletin postings. The advertisements sought healthy young people between the ages of 18 and 25 with no major chronic or life-threatening illnesses, who were interested in a “study about childhood, family, and health.” Respondents were initially screened with telephone interviews to obtain age information and determine whether any exclusion criteria were met. Respondents were excluded if they were not in the age range or rated their health as either bad or very bad. Eligible respondents were invited to an hour-long, structured in-person interview administered by a trained interviewer. Data was collected from 300 people who completed the interview. The average age of the sample was 21.73 years (SD=2.10) and slightly more than half was female (51.5%). Our sample characteristics are fully described in Table 1. All participants were provided with a thorough explanation of procedures and gave written informed consent for participation. A University Institutional Review Board approved all study procedures.
Table 1.
Sample characteristics (N = 300).
| Range | Mean (SD)* or % (n) |
|
|---|---|---|
| Demographics | ||
| Age* | 18-25 | 21.7(2.1) |
| Gender | ||
| Male | 48.5(145) | |
| Female | 51.5(154) | |
| Race/Ethnicitya | ||
| White | 58.2 (174) | |
| Black | 16.1 (48) | |
| Hispanic | 7.4 (22) | |
| Asian | 8.4 (25) | |
| Other | 10.0 (30) | |
| Alcohol Use | ||
| Monthly frequency* | 0-31 | 7.1 (6.1) |
| Past year binge-drinking | 40.0 (120) | |
| Alcohol-related problem* | 0-59 | 8.7 (10.7) |
| AUD | 28.1 (84) | |
| Peer binge drinkinga | ||
| None | 41.8 (125) | |
| One | 12.0 (36) | |
| Less than half | 22.1 (66) | |
| More than half | 15.7 (47) | |
| Almost all | 8.4 (25) | |
| Parental alcoholism* | 0-6 | 1.2 (2.0) |
| Psychological symptoms* | 33-78 | 50.8 (10.4) |
| Developmental timing of physical abuseab | ||
| Preschool | 14.5 (42) | |
| Middle childhood | 26.6 (77) | |
| Pubertal | 29.4 (85) | |
| Adolescence | 28.4 (82) | |
| Chronicity of physical abuseabc | ||
| Situational | 25.5 (29) | |
| Limited | 27.5 (32) | |
| Chronic | 47.0 (55) |
Mean values (standard deviations). All other measures reported in proportion (%).
Valid percentages are reported.
The sub-sample size to determine percentage is 116 respondents who reported CPA at least in one developmental stage. The sample sizes for other statistics reported in the table range from 297 to 300 due to missing data.
“Situational” refers to experiencing CPA in one developmental period, “limited” in two developmental periods, and “chronic” in three or all developmental periods.
Measures
CPA and other types of child maltreatment
Childhood maltreatment including physical abuse was measured using a combined version of the Childhood Trauma Questionnaire (CTQ) (Bernstein et al., 1994) and the Maltreatment and Abuse Chronology of Exposure (MACE) scale (Teicher and Parigger, 2015). The CTQ determines severity scores for three types of childhood maltreatment (i.e., physical abuse, sexual abuse, and neglect) with each score separated into four severity categories: None to Minimal, Low to Moderate, Moderate to Severe, and Severe to Extreme. Based on previously established procedures described in empirical studies, participants with a score of ‘Moderate to Severe’ and above were categorized as positive for childhood maltreatment in the present study (Bernstein et al., 1994). In the present study, 116 participants (38.7% of the sample) were classified as having experienced CPA. The CTQ has shown sufficient reliability with internal consistency reliability ranging from .73 to .92, and validity supported by associations with official records, such as court and social service agency records (Bernstein and Fink, 1998). The internal consistency for CPA in our sample was .88. The MACE measures developmental timing and chronicity of exposure to ten forms of childhood victimization (prior to age 18) including CPA. The MACE provides 18 boxes for each item to indicate the years when the exposure occurred. The scale was developed using item response theory and has excellent psychometric properties (e.g., test-retest reliability (r =.88-.91)).
Timing of CPA
Using the MACE scale, we specified the age in which the respondents experienced physical abuse. Two different classifications of CPA timing were used: 1) person-centered classification using LCA; and 2) “developmental” classification. The LCA of CPA timing is fully described below (See data analysis). For the developmental classification, we first determined four developmental stages between the ages of 0 and 18 in order to detect possible time periods of vulnerability: preschool (0-5), middle childhood (6-9), pubertal (10-13), and adolescence (14-18). The existence of CPA was depicted for each participant with a 1 (yes) or 0 (no) for each time period. Next, consistent with previous research on developmental timing of child maltreatment (Thornberry et al., 2001, Kaplow and Widom, 2007), we classified the developmental timing of CPA into three categories including PA (physical abuse) before adolescence (birth though 9), PA during adolescence (ages 10-18), and extensive PA (PA occurred in both childhood and adolescence).
Chronicity of CPA
Consistent with previous studies of child maltreatment chronicity (Jaffee and Maikovich-Fong, 2011, English et al., 2005), we derived a measure of chronicity using the number of developmental stages (i.e., preschool, middle childhood, pubertal, and adolescence) in which a respondent experienced CPA, regardless of the timing of CPA onset. We defined experiencing CPA in one developmental period as situational, in two developmental periods as limited, and in three or all developmental periods as chronic.
Alcohol use
Monthly drinking frequency was measured with the question “in the past 12 months, on how many days did you drink alcohol per month?” Similarly, the frequency of past-year binge drinking was determined through the question “over the past 12 months, on how many days did you drink five (or four) or more drinks in a row?” (1 = every day, 2 = 3-5 days a week, 3 = 1 or 2 days a week, 4 = 2 or 3 days a month, 5 = once a month or less, 6 = 1 or 2 days in the past year, 7 = never). Subjects were classified as having participated in binge drinking if males consumed five or more drinks in a row and females four or more drinks in a row at least 2-3 days per month in the past 12 months (i.e., “every day” to “2 or 3 days a month” coded as “1”) (Wechsler et al., 1994). Further, the Rutgers Alcohol Problem Index (RAPI) was utilized to measure alcohol-related problems in the past 12 months. The RAPI is a 23-item Likert scale, which provides a total negative alcohol-related consequences score, ranging from 0 to 69 (White and Labouvie, 1989). Internal consistency reliability for the RAPI for the current sample was .90. Alcohol use disorder (AUD) in the past 12 months was assessed through the Composite International Diagnostic Interview (CIDI) alcohol section, which asked about the Diagnostic and Statistical Manual (DSM-IV) symptoms of AUD (Cottler et al., 1991, Ustun et al., 1997).
Psychological distress, peer alcohol use, and parental alcoholism
Psychological distress was measured by the Brief Symptom Inventory 18 (BSI-18) (Derogatis, 1993). The BSI-18 includes 18 items evaluating certain features of psychological distress, such as somatization, depression, and anxiety. A higher BSI score indicated a higher level of psychological distress. Internal consistency of the BSI-18 in our sample was .93. Further, peer alcohol use was measured through questions addressing the number of subjects’ close friends who drink alcohol once a week or more. Finally, parental alcoholism was measured using the 6-item Children of Alcoholics Screening Test (CAST-6) (Hodgins et al., 1993). Internal consistencies reliability coefficients for the BSI-18 and CAST-6 for our study sample were .93 and .92, respectively.
Data analysis
At the outset, we performed LCA of timing of CPA based on four developmental stages (i.e., preschool, middle childhood, pubertal, adolescence) to empirically classify respondents whose CPA timing patterns are similar to each other, yet clearly different from respondents in other timing groups. We estimated LCA models with increasing numbers of classes to determine the best fitting model for our data. A combination of statistical and substantive consideration is used to decide the optimal number of classes. In testing model fits and selecting the number of latent classes (i.e., groups), we used the Bayesian information criterion (BIC) statistics and the Lo–Mendell–Rubin adjusted likelihood ratio test (Lo et al., 2001). The best fitting LCA model has the smallest BIC and non-significant p-value (i.e., p > 0.05) from the LMR test at k + 1 class. Specifically, the LMR provides testing of k−1 versus k classes where k is a number of latent classes. LCA is characterized by two probabilities: (1) probabilities of class membership assignment for individuals and (2) probabilities of fulfilling each criterion given class membership.
Using the two CPA timing classifications (i.e., LCA and developmental) and one developmental chronicity measure, we conducted a series of multiple linear or logistic regression analyses to examine the relationships between timing/chronicity of CPA and each alcohol use outcome, controlling for demographics, family income, other types of maltreatment, psychological distress, and parental and peer alcohol use. Specifically, monthly drinking frequency, binge drinking, alcohol-related problems, and AUD were regressed (in separate models) on CPA timing and chronicity. For monthly drinking frequency and alcohol-related problems, we observed non-normality (i.e., sample kurtosis and skewness were 4.07 and 1.08 for drinking frequency and 6.88 and 1.87 for alcohol related problems) and applied log-transformation adding 0.5 for 0 value prior to linear regression modeling. Using the entire sample, we first investigated the association between the presence of CPA and alcohol use and then the association between the timing/chronicity of CPA and alcohol use. In latter analysis, we used the Bonferroni corrections for multiple comparisons within each timing/chronicity variable and each outcome (Bretz et al., 2010). Next, in order to examine and compare how variations in the developmental timing and chronicity of CPA among maltreated individuals relate to alcohol use, we created a sub-sample of respondents who reported CPA in at least one developmental stage (N=116), and conducted similar regression analyses described above. For group comparisons, we used F-test in linear regression and chi-square test in logistic regressions.
Results
Exposure to CPA and alcohol use
First, we found that regardless of timing or chronicity, the presence of CPA was positively related to monthly drinking frequency, binge drinking, and AUD, controlling for age, gender, race/ethnicity, family income, other types of maltreatment, psychological distress, and parental and peer alcohol use (Table 2).
Table 2.
Multiple regression analyses indicating the relationship between exposure to physical abuse through adolescence (ages 0-18) and alcohol use in young adulthood.
| Frequency of alcohol use |
Binge drinking | Alcohol- related problems |
AUD | |
|---|---|---|---|---|
|
|
||||
| β (SE) | OR (CI) | β (SE) | OR (CI) | |
| Physical abuse | 0.49 (0.13)*** | 2.60 (1.41-4.80)** | 0.27(0.18) | 2.41 (1.31-4.45)** |
| Age | 0.10 (0.03)*** | 0.97 (0.85-1.11) | −0.02 (0.04) | 0.95 (0.83-1.09) |
| Gender | 0.00 (0.12) | 1.85 (1.04-3.32)* | −0.47 (0.17)** | 0.46 (0.25-0.82)** |
| Race/ethnicity | ||||
| Black | −0.15 (0.18) | 0.64 (0.27-1.52) | −0.17 (0.25) | 1.00 (0.42-2.39) |
| Hispanic | −0.46 (0.24) | 0.77 (0.27-2.25) | −0.11 (0.34) | 0.51 (0.15-1.77) |
| Asian | −0.95 (0.23)*** | 0.31 (0.09-1.01) | 0.18 (0.37) | 0.76 (0.22-2.59) |
| Others | −0.31 (0.20) | 0.40 (0.13-1.20) | −0.23 (0.28) | 0.70 (0.24-2.07) |
| Parental alcoholism | 0.05 (0.03) | 1.15 (1.01-1.32)* | 0.11 (0.04)* | 1.12 (0.97-1.30) |
| Peer alcohol use | 0.20 (0.05)*** | 1.86 (1.50-2.31)*** | 0.17 (0.06)** | 1.60 (1.29-1.99)*** |
| Family income | 0.15 (0.08) | 1.15 (0.78-1.69) | −0.00 (0.12) | 0.80 (0.53-1.19) |
| Psychological distress | 0.00 (0.01) | 1.00 (0.97-1.03) | 0.01 (0.01) | 1.00 (0.97-1.03) |
| Other maltreatment | ||||
| Sexual abuse | −0.48 (0.20)* | 0.45 (0.17-1.23) | 0.20 (0.28) | 1.09 (0.41-2.93) |
| Neglect | −0.07 (0.13) | 1.14 (0.61-2.14) | 0.07 (0.18) | 0.78 (0.40-1.53) |
Note: All regression analyses were controlled for demographics, family income, other types of maltreatment, psychological distress, and parental and peer alcohol use. The alcohol-related problems model also controlled for frequency of alcohol use.
p < 0.05
p< 0.01
p< 0.001
LCA results
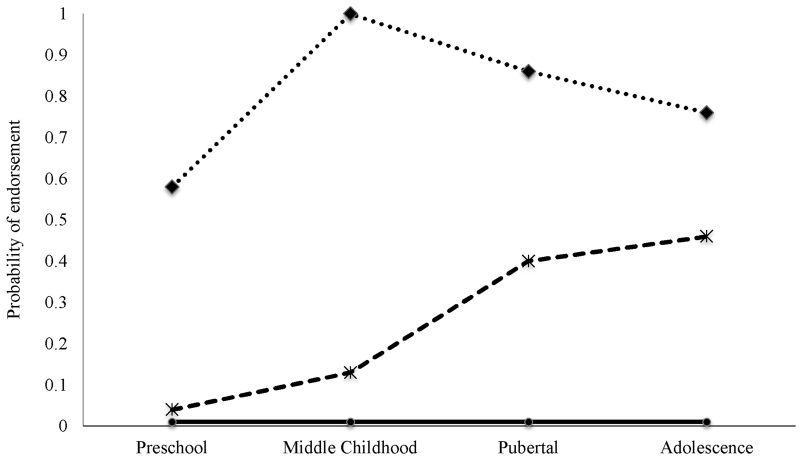
Giving the most parsimonious description of our sample, LCA identified a 3-class model of CPA timing, which had the lowest BIC (BICs: two classes = 979.71, three classes = 960.27, four classes = 973.01, five classes = no convergence), and LMR also pointed to a 3-class model (LMR: two classes (p) = .001, three classes (p) = .02, four classes (p) = .12, five classes = no convergence). In Figure 1, we present the item-response probabilities which referred to the probability for CPA at each of the four developmental timing for each of the 3 classes derived from the 3-class model. The three classes for developmental timing of CPA were named: low physical abuse (PA) (Class 1: 60.2%), post-pubertal PA (Class 2: 14.5%), and persistent PA (Class 3: 25.3%). We noted that these names were subjectively chosen based on the patterns of item endorsement within the response profile. Verifying the quality of classification, the high average latent class probability (0.91–0.97) of being in a latent class given the vector of CPA timing suggested good differentiation of classes. Therefore, the 3-class model of CPA timing was used in further analysis.
Figure 1.
Probability of physical abuse timing for a three class model.
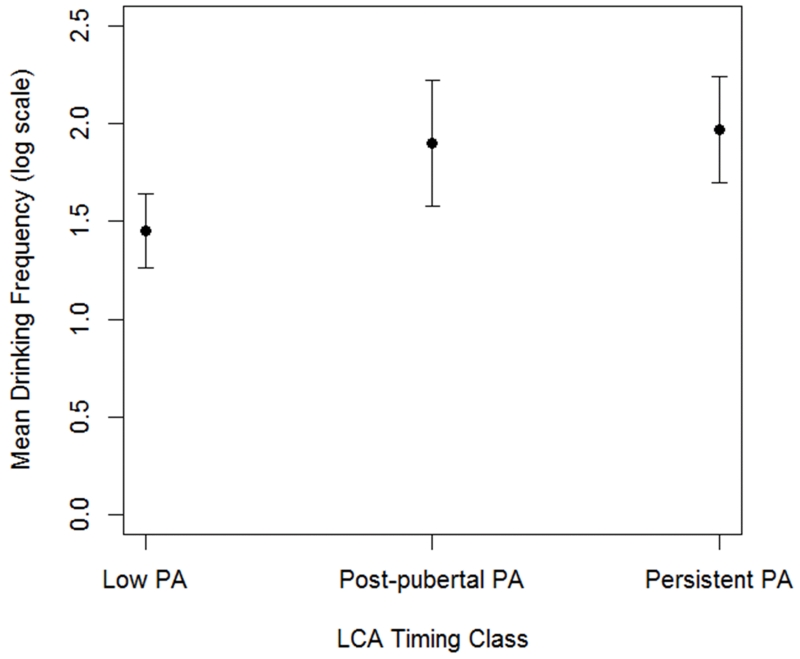
Timing of CPA and alcohol use
Using the LCA classification scheme (low PA as the reference category), we found that post-pubertal PA was positively associated with monthly drinking frequency and alcohol-related problems whereas persistent PA was positively associated with all drinking behaviors with the exception of alcohol-related problems, controlling for age, gender, race/ethnicity, family income, other types of maltreatment, psychological distress, and parental and peer alcohol use (Table 3). Additionally, figure 2 presents the estimated mean monthly drinking frequency (in log scale) for each LCA class, which indicated an increasing pattern in drinking frequency as the LCA class changes from low PA to persistent PA. We conducted pairwise comparisons (i.e., low vs. post-pubertal PA, low vs. persistent PA, and post-pubertal vs persistent PA) with the Bonferroni corrections for multiple comparisons. Pairwise comparisons showed that the differences were significant between low PA and post-pubertal PA (p < 0.01) and between low PA and persistent PA (p < 0.001), but not between post-pubertal PA and persistent PA. Furthermore, the developmental classification-based analyses showed that PA during adolescence was positively associated with monthly drinking frequency whereas extensive PA was related to all drinking outcomes, excluding alcohol-related problems, after adjusting for sociodemographic variables, other types of maltreatment, psychological distress, and parental and peer alcohol use (Table 3).
Table 3.
Multiple regression analyses indicating the relationship between LCA timing classes, developmental timing and developmental chronicity of physical abuse, and alcohol use in young adulthood.
| Frequency of alcohol use |
Binge drinking | Alcohol- related problems |
AUD | |
|---|---|---|---|---|
|
|
||||
| B (SE) | OR (CI) | B (SE) | OR (CI) | |
| LCA timing | ||||
| Post-pubertal PA | 0.45 (0.18)* | 2.42 (1.22-6.17) | 0.54 (0.24)* | 2.21 (0.89-5.50) |
| Persistent PA | 0.52 (0.15)** | 2.74 (0.99-6.04)* | 0.09 (0.21) | 2.56 (114-5.75)* |
| Developmental timing |
||||
| PA before adolescence |
0.05 (0.32) | 4.07 (0.66-25.23) | 0.15 (0.41) | 4.20 (0.80-21.99) |
| PA during adolescence |
0.52 (0.19)* | 2.20 (0.79-6.16) | 0.58 (0.25) | 1.86 (0.65-5.32) |
| Extensive PA | 0.55 (0.16)** | 2.69 (1.11-6.51)* | 0.11 (0.21) | 2.51 (1.04-6.02)* |
| Developmental a chronicity |
||||
| Situational | 0.34 (0.21) | 3.31 (1.07-10.26)* | 0.35 (0.27) | 2.53 (0.84-7.67) |
| Limited | 0.65 (0.20)** | 1.78 (0.57-5.53) | 0.24 (0.27) | 1.87 (0.59-5.94) |
| Chronic | 0.47 (0.18)* | 2.87 (1.07-7.66)* | 0.23 (0.24) | 2.74 (1.04-7.22)* |
“Situational” refers to experiencing CPA in one developmental period, “limited” in two developmental periods, and “chronic” in three or all developmental periods.
Note: PA = physical abuse; Table 3 reports results of three separate analyses including LCA timing, Developmental timing, and Developmental chronicity models. For LCA timing, “Low PA” was the reference group whereas for Developmental timing and Developmental chronicity, no PA was the reference group. Each regression analysis was controlled for demographics, family income, other types of maltreatment, psychological distress, and parental and peer alcohol use. The alcohol-related problems model also controlled for frequency of alcohol use.
p<0.05
p<0.01
P<0.001
Figure 2.
Monthly drinking frequencies by LCA timing class membership.
Note: PA = physical abuse; the differences were significant between low PA and post-pubertal PA (p < 0.01) and between low PA and persistent PA (p < 0.001).
Chronicity of CPA and alcohol use
Examining the association between developmental chronicity of CPA and alcohol use in young adulthood (Table 3), we found that compared to no-CPA, situational PA was positively related to binge drinking. In addition, limited PA was positively associated with monthly drinking frequency whereas chronic PA was positively related to all drinking behaviors except alcohol-related problems.
Variations in CPA timing/chronicity and alcohol use
Using the respondents who reported CPA at least in one developmental stage, we examined whether variations in CPA timing and chronicity among CPA victims were associated with alcohol use during young adulthood. In the LCA classification system, individuals who experienced persistent PA were not different from those who experienced post-pubertal PA in reporting monthly drinking frequency (p =.85), binge drinking (p =.98), alcohol-related problems, (p =.32) and AUD (p =.87). Using the developmental classification of CPA timing, we also found that there were little group differences in reporting the four patterns of drinking behaviors (p-values =.09 - 92) among the PA before adolescence, PA during adolescence, and extensive PA groups. Furthermore, examining within-in group differences in alcohol use based on CPA chronicity, we found no group differences in any drinking behavior (p values =.14 - .89) among the situational, limited and chronic CPA groups.
Interactions between CPA timing and chronicity
Finally, using the entire sample, we conducted an additional analysis to examine the interactive effects of timing and chronicity of CPA on alcohol use during young adulthood. Specifically, we included the CPA timing and chronicity variables, and their interaction terms in each regression model. For example, we explored whether among individuals whose PA occurred only before adolescence, those participants experiencing CPA in one developmental period (i.e., the situational chronicity group) differ from those experiencing it in two developmental periods (i.e., the limited chronicity group) in reporting alcohol use outcomes. Testing potential interactive effects of all CPA timing and chronicity combinations, we found no moderation effects of timing and chronicity of CPA on alcohol use (p values =.12 - .83).
Discussion
The present study explored whether the nature and magnitude of alcohol use in young adulthood would differ according to the timing and chronicity of CPA, controlling for sociodemographic characteristics, other types of maltreatment and common risk factors for alcohol use such as psychological distress, parental alcoholism, and peer alcohol use. Results generally supported our hypotheses in that compared to respondents who had no history of CPA, young adults who were physically maltreated, particularly during adolescence, and who chronically experienced CPA throughout the first 18 years of their lives, demonstrated higher levels of monthly drinking frequency and more pathological drinking behaviors such as binge drinking, alcohol-related problems, and AUD.
We found that there were some overlap between two important dimensions of maltreatment events such as timing and chronicity of CPA. For example, the “extensive” category in the developmental timing and “chronic” category in the developmental chronicity classification systems demonstrated similar results in predicting alcohol use outcomes. The present study also found that a LCA classification of maltreatment timing, particularly when it uses developmental stages in which child maltreatment occurred as class indicators, might be particularly useful to account for two different dimensions of maltreatment such as timing and chronicity, simultaneously. Comparing the results of the LCA-based regression models to those in the separate developmental timing- and chronicity-based models, the LCA models concurrently captured timing, continuity and distribution of the CPA experience over time in our sample, and had the most balanced sensitivity across alcohol outcomes. Given the deleterious effects of exposure to CPA on alcohol use, it is critical to develop a classification system that precisely identifies critical periods or sensitive periods for the maximum impact of CPA on later alcohol use and reliably characterizes those children at risk for serious alcohol use in young adulthood. A LCA classification system presumably extends the practice of identifying and characterizing maltreatment timing and chronicity by grouping children together who have similar probabilistic patterns of maltreatment timing and continuity, simultaneously. This person-centered classification method is particularly relevant to the study of child maltreatment because there is great heterogeneity among this population in terms of their CPA timing and chronicity, which are often overlooked clinically and empirically. Characterizing a critical period for the development of alcohol use and identifying determinants and pathways of risk and resilience would accelerate the development of effective interventions for young adult victims of CPA.
The findings on chronicity of PA seem noteworthy. The results showed that once PA occurs in childhood, it is likely to persist in subsequent developmental periods. Prior research suggests that chronic exposure to child maltreatment can fundamentally change a child’s ecology, has enduring harmful effects on child developmental trajectory, and produces lifelong adverse consequences for health and well-being (Sinha, 2008, Shonkoff and Garner, 2012). Consistent with prior research, young adult victims of CPA whose maltreatment exposures were persistent and chronic, regardless of the classification systems used (i.e., person-centered, developmental), were at greater risks for pathological alcohol use. Recent neurobiological studies suggest that the more prolonged the childhood adversity the greater the impairments in the stress response systems and risk for alterations in brain regions that are involved in initiating and maintaining addictive behavior (De Bellis and Zisk, 2014, Teicher et al., 2003). Although specific windows of vulnerability to the effects of childhood adversity on alcohol use have not been fully identified, research also shows that longer periods of maltreatment are more likely to intersect with the windows of vulnerability (Andersen, 2008).
Chronic maltreatment is often found in a family experiencing various life challenges and stressors, including low parental education, low family income, parental substance use and mental health problems, low social support, and single parenthood (Jonson-Reid et al., 2012). Therefore, further understanding of the family needs in chronic maltreatment cases is vital to preventing additional victimization as well as alcohol use among young adult victims of chronic maltreatment. Future research of the specific individual and family characteristics among problematic drinkers who have chronic exposure to child maltreatment might inform the development of interventions designed for chronic maltreatment, timing of intervention and target behavior associated with each intervention.
The findings regarding the lack of association of chronic CPA with alcohol-related problems are interesting. We found that whereas chronic CPA was significantly related to alcohol use and AUD, it was not associated with alcohol-related problems, after the adjustment for frequency of alcohol use. Given that chronic CPA was significantly associated with drinking frequency, which significantly related to alcohol-related problems, it is possible that chronic CPA influences alcohol-related problems (e.g., passing out and having a fight as a result of alcohol use) through drinking frequency in young adulthood. Although more evidence is needed to understand the specific pathways or mechanisms by which chronic CPA leads to the problematic drinking behavior, our results suggest that timing and chronicity of CPA might differently relate to distinct drinking behaviors during young adulthood.
The results of our study also indicated that individuals whose maltreatment began in adolescence or whose maltreatment occurred during childhood and continued into adolescence were highly vulnerable to alcohol use during young adulthood. Adolescent maltreatment might have particularly damaging impacts on alcohol use. In a recent young adult study, adolescent maltreatment was associated with structural and functional alterations in the brain, which may lead to impairments in handling stressful situations, processing traumatic memory, and modulating emotion (Andersen et al., 2008, Strange and Dolan, 2006, Miller and Cohen, 2001). Previous studies also found that PA during pubertal periods might be specifically detrimental because increasing sex steroid levels may interfere with the regulation of stress response systems and exert harmful effects on the developing brain, particularly in the areas of the prefrontal cortex, which play a significant role in initiating alcohol use and progressing into pathological use and dependence (Romeo and McEwen, 2006, McCormick and Mathews, 2007, Sinha, 2009). Acknowledging that more evidence is needed to determine precise critical periods for the maximum impact of exposure to CPA on later alcohol use, future studies might also consider investigating the neurobiological mechanisms that give rise to sensitive periods of adolescent maltreatment. Identifying such mechanisms might help the development of behavioral interventions to modify the saliency of a sensitive period in conferring risk for alcohol use and abuse during young adulthood.
Adolescence is characterized by an increased autonomy, cognitive ability, risk taking behavior, and shared negative experiences with peers, which may put youth at an elevated risk for alcohol use (Erikson, 1968, Brown et al., 2008, Tarter, 2002). For example, enhanced psychological capabilities in adolescence such as increased self-awareness, advanced reasoning, and abstract thinking might make interpreting and coping with adverse experiences over which they have no control more difficult. Therefore, adolescents may be more likely than younger children to react to CPA by adapting maladaptive coping strategies and participating in antisocial behaviors such as alcohol and other illicit drug use, which are less available to younger children (Laurent et al., 1997). Furthermore, intensified affiliation with, reliance on, and pressure to be “in-sync” with peers might facilitate shared negative experiences with peers of adverse life events such as CPA, which makes adolescent victims of CPA more vulnerable to alcohol use (Hawkins et al., 1992, Trickett et al., 2011). Increasingly oppositional behavior in adolescence may also have the effects of obscuring and limiting attention to adolescent maltreatment that potentially promotes and reinforces it. Research on child maltreatment tends to focus on early childhood maltreatment, assuming that it has the most devastating sequelae and that adolescents are better protected against maltreatment (Smith et al., 2005, Thornberry et al., 2010). Given the high prevalence of adolescent maltreatment found in recent national surveys, our findings suggest that future research on the relation of maltreatment to alcohol use should include adolescent maltreatment, and the age of the maltreatment onset should be assessed in order to examine its effects on later alcohol use and dependence.
Limitations
There are several limitations to this study. Child maltreatment manifests in several different forms including CPA, sexual abuse and neglect. Therefore, there might be varying sensitive periods when exposure to specific forms of maltreatment is most likely to increase risk for later alcohol use. Although the present study focused on CPA, and controlled for other types of child maltreatment in examining the association between CPA timing, chronicity and alcohol use, potential interactive effects of child maltreatment types and age of maltreatment onset were not explored in the present study. In addition, we did not measure frequency of CPA events, which is used in some studies to define maltreatment chronicity. However, an empirical study comparing the utility of three different definitions of chronicity such as frequency, calendar, and developmental definition found that developmental definition which was used in the present study was the most salient and sensitive definition of chronicity, in terms of its effects on child behavioral and emotional functioning (English et al., 2005). Second, although the proportion reporting CPA in our sample is similar to the prevalence of CPA reported in recent studies of community-based young adult samples (Allem et al., 2015, MacMillan et al., 2013), it was relatively higher than those reported in adult populations (Thompson et al., 2004). While a shorter interval between the assessment and the target CPA experience may contribute to this finding, our results may not generalize to individuals in different life stages. Next, exposure to CPA came from retrospective self-reports, which are subject to certain limitations such as recall bias and social desirability. However, a few studies providing data on convergent validity of retrospective childhood maltreatment reports have concluded that when respondents report childhood maltreatment, their self-reports are relatively concordant with official records and reports from other informants (e.g., siblings, parents) (Bifulco et al., 1997). Furthermore, in a recent longitudinal study, adolescent self-reports of child maltreatment surpassed child protective services (CPS) determinations of child maltreatment in predicting psychological disturbance (Everson et al., 2008). Furthermore, the present study is limited by the use of a cross-sectional design, which does not allow examining how timing of and recency of CPA are related to changes in drinking behavior over time. Next, although the age range of our sample matches the peak period of risk for pathological alcohol use, the 12-month timeframe used in reporting alcohol outcomes might not capture the period of problematic drinking, particularly for those closer to age 25. Other significant characteristics of timing in alcohol research such as age of drinking onset and duration were also not measured in our study, which might allow exploring the length of time between onset of CPA and initiation of alcohol use or progression into pathological alcohol involvement. Finally, other substance use (e.g., marijuana) was not examined in the present study, a topic that could be explored in further studies. In addition, CPA may manifest in high-risk behaviors other than alcohol use or AUD, including depression and anxiety.
In summary, using a LCA classification of maltreatment timing, the present study found that PA during adolescence and persistent PA across childhood and adolescence increased the risk for alcohol use and AUD in young adulthood. In order to gain a more thorough understanding of the impact of child maltreatment on later alcohol use, future studies are warranted to explore how maltreatment event-characteristics including timing and chronicity of maltreatment influence the course and patterns of alcohol use. In translational perspectives, investigation of the significance, if any, of the role of developmental timing and chronicity of maltreatment is important in creating timely sensitive preventive and treatment interventions for victims of child maltreatment.
Acknowledgments
This research was supported by grants from NIDA DA030884 (Shin) and the AMBRF/The Foundation for Alcohol Research (Shin). The funding sources had no role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
Contributor Information
Sunny H. Shin, School of Social Work, Virginia Commonwealth University, Richmond, Virginia; Department of Psychiatry, School of Medicine, Virginia; Commonwealth University, Richmond, Virginia
Yeonseung Chung, Department of Mathematical Sciences, Korea Advanced Institute of Science and Technology, Daejeon, Republic of Korea
Rachel D. Rosenberg, School of Social Work, Virginia Commonwealth University, Richmond, Virginia.
References
- Allem JP, Soto DW, Baezconde-Garbanati L, Unger JB. Adverse childhood experiences and substance use among Hispanic emerging adults in Southern California. Addict Behav. 2015;50:199–204. doi: 10.1016/j.addbeh.2015.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen SL, Tomada A, Vincow ES, Valente E, Polcari A, Teicher MH. Preliminary evidence for sensitive periods in the effect of childhood sexual abuse on regional brain development. J Neuropsych Clin N. 2008;20:292–301. doi: 10.1176/appi.neuropsych.20.3.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: a retrospective self-report. Harcourt Brace, Psychological Corporation; San Antonio, TX: 1998. [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiat. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Brown GW, Lillie A, Jarvis J. Memories of childhood neglect and abuse: corroboration in a series of sisters. J Child Psychol Psyc. 1997;38:365–374. doi: 10.1111/j.1469-7610.1997.tb01520.x. [DOI] [PubMed] [Google Scholar]
- Bretz F, Hothorn T, Westfall P. Multiple comparisons using R. CRC Press; 2010. [Google Scholar]
- Brown SA, Mcgue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, Martin C, Chung T, Tapert SF, Sher K, Winters KC, Lowman C, Murphy S. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. 2008;121:S290–310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. A developmental psychopathology perspective on child abuse and neglect. J Am Acad Child Psy. 1995;34:541–565. doi: 10.1097/00004583-199505000-00008. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Robins LN, Grant BF, Blaine J, Towle LH, Wittchen HU, Sartorius N. The CIDI-core substance abuse and dependence questions: cross-cultural and nosological issues. The WHO/ADAMHA Field Trial. T Br J Psychiatry. 1991;159:653–8. doi: 10.1192/bjp.159.5.653. [DOI] [PubMed] [Google Scholar]
- Cowell RA, Cicchetti D, Rogosch FA, Toth SL. Childhood maltreatment and its effect on neurocognitive functioning: timing and chronicity matter. Dev Psychopathol. 2015;27:521–33. doi: 10.1017/S0954579415000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD, Zisk A. The biological effects of childhood trauma. Child Adolesc Psychiatr Clin N Am. 2014;23:185–222. vii. doi: 10.1016/j.chc.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. BSI Brief Symptom Inventory. Administration, scoring, and procedures manual. National Computer Systems; Minneapolis: 1993. [Google Scholar]
- Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, Anda RF. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006;38:1–44. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- English DJ, Graham JC, Litrownik AJ, Everson M, Bangdiwala SI. Defining maltreatment chronicity: Are there differences in child outcomes? Child Abuse Negl. 2005;29:575–595. doi: 10.1016/j.chiabu.2004.08.009. [DOI] [PubMed] [Google Scholar]
- Erikson EH. Idenitity and the Life Cycle. International Universities Press; New York: 1968. [Google Scholar]
- Everson MD, Smith JB, Hussey JM, English D, Litrownik AJ, Dubowitz H, Thompson R, Dawes-Knight E, Runyan DK. Concordance between adolescent reports of childhood abuse and child protective service determinations in an at-risk sample of young adolescents. Child Maltreat. 2008;13:14–26. doi: 10.1177/1077559507307837. [DOI] [PubMed] [Google Scholar]
- Fenton MC, Geier T, Keyes K, Skodol AE, Grant BF, Hasin DS. Combined role of childhood maltreatment, family history, and gender in the risk for alcohol dependence. Psychol Med. 2013;43:1045–57. doi: 10.1017/S0033291712001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francke ID, Viola TW, Tractenberg SG, Grassi-Oliveira R. Childhood neglect and increased withdrawal and depressive severity in crack cocaine users during early abstinence. Child Abuse & Negl. 2013;37:883–9. doi: 10.1016/j.chiabu.2013.04.008. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescense and early adulthood. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Maticka-Tyndale E, El-Guebaly N, West M. The CAST-6: Development of a short-form of the Children of Alcoholics Screening Test. Addict Behav. 1993;18:337–45. doi: 10.1016/0306-4603(93)90035-8. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Maikovich-Fong AK. Effects of chronic maltreatment and maltreatment timing on children’s behavior and cognitive abilities. J Child Psychol Psychiatry. 2011;52:184–94. doi: 10.1111/j.1469-7610.2010.02304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonson-Reid M, Kohl PL, Drake B. Child and adult outcomes of chronic child maltreatment. Pediatrics. 2012;129:839–45. doi: 10.1542/peds.2011-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. Journal Abnorm Psychol. 2007;116:176–187. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]
- Keiley MK, Howe TR, Dodge KA, Bates JE, Pettit GS. The timing of child physical maltreatment: a cross-domain growth analysis of impact on adolescent externalizing and internalizing problems. Dev Psychopathol. 2001;13:891–912. [PMC free article] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Callan MK. Stress, alcohol-related expectancies and coping preferences: a replication with adolescents of the Cooper et al. (1992) model. J Stud Alcohol. 1997;58:644–51. doi: 10.15288/jsa.1997.58.644. [DOI] [PubMed] [Google Scholar]
- Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- MacMillan HL, Tanaka M, Duku E, Vaillancourt T, Boyle MH. Child physical and sexual abuse in a community sample of young adults: Results from the Ontario Child Health Study. Child Abuse & Neglect. 2013;37(1):14–21. doi: 10.1016/j.chiabu.2012.06.005. [DOI] [PubMed] [Google Scholar]
- Manly JT. Advances in research definitions of child maltreatment. Child Abuse & Negl. 2005;29:425–39. doi: 10.1016/j.chiabu.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Mccormick CM, Mathews IZ. HPA function in adolescence: role of sex hormones in its regulation and the enduring consequences of exposure to stressors. Pharmacol Biochem Behav. 2007;86:220–33. doi: 10.1016/j.pbb.2006.07.012. [DOI] [PubMed] [Google Scholar]
- Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Annu Rev Neurosci. 2001;24:167. doi: 10.1146/annurev.neuro.24.1.167. [DOI] [PubMed] [Google Scholar]
- Pechtel P, Lyons-Ruth K, Anderson CM, Teicher MH. Sensitive periods of amygdala development: the role of maltreatment in preadolescence. NeuroImage. 2014;97:236–44. doi: 10.1016/j.neuroimage.2014.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romeo RD, Mcewen BS. Stress and the adolescent brain. Ann N Y Acad Sci. 2006;1094:202–14. doi: 10.1196/annals.1376.022. [DOI] [PubMed] [Google Scholar]
- Shaver KG, Drown D. On causality, responsibility, and self-blame: a theoretical note. J Pers Soc Psycho. 1986;50:697–702. doi: 10.1037//0022-3514.50.4.697. [DOI] [PubMed] [Google Scholar]
- Shin SH, Miller DP, Teicher MH. Exposure to childhood neglect and physical abuse and developmental trajectories of heavy episodic drinking from early adolescence into young adulthood. Drug Alcohol Depend. 2013;127:31–8. doi: 10.1016/j.drugalcdep.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatric. 2012;129:e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–30. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R. Stress and addiction: a dynamic interplay of genes, environment, and drug intake. Biol Psychiatry. 2009;66:100–1. doi: 10.1016/j.biopsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CA, Ireland TO, Thornberry TP. Adolescent maltreatment and its impact on young adult antisocial behavior. Child Abuse & Negl. 2005;29:1099–119. doi: 10.1016/j.chiabu.2005.02.011. [DOI] [PubMed] [Google Scholar]
- Strange BA, Dolan RJ. Anterior medial temporal lobe in human cognition: memory for fear and the unexpected. Cogn Neuropsychiatr. 2006;11:198–218. doi: 10.1080/13546800500305096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarter RE. Etiology of adolescent substance abuse: a developmental perspective. Am J Addict. 2002;11:171–91. doi: 10.1080/10550490290087965. [DOI] [PubMed] [Google Scholar]
- Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neurosci Biobehav Rev. 2003;27:33–44. doi: 10.1016/s0149-7634(03)00007-1. [DOI] [PubMed] [Google Scholar]
- Teicher MH, Parigger A. The ‘Maltreatment and Abuse Chronology of Exposure’ (MACE) scale for the retrospective assessment of abuse and neglect during development. PLoS One. 2015;10:e0117423. doi: 10.1371/journal.pone.0117423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson MP, Kingree JB, Desai S. Gender differences in long-term health consequences of physical abuse of children: Data from a nationally representative survey. Am J Public Health. 2004;94(4):599–604. doi: 10.2105/ajph.94.4.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Henry KL, Ireland TO, Smith CA. The causal impact of childhood-limited maltreatment and adolescent maltreatment on early adult adjustment. J Adolesc Health. 2010;46:359–65. doi: 10.1016/j.jadohealth.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Ireland TO, Smith CA. The importance of timing: the varying impact of childhood and adolescent maltreatment on multiple problem outcomes. Dev Psychopathol. 2001;13:957–979. [PubMed] [Google Scholar]
- Trickett PK, Negriff S, Ji J, Peckins M. Child maltreatment and adolescent development. J Res Adolesc. 2011;21:3–20. [Google Scholar]
- U.S. Centers For Disease Control And Prevention . children. 2014. Child mlatreatment: Facts at a Glance 2012. [Google Scholar]
- U.S. Department Of Health And Human Services . Child Maltreatment 2013. Government Printing Office; Washington, DC: 2014. [Google Scholar]
- Ustun B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, Cottler L, Gogus A, Mavreas V, Peters L, Pull C, Saunders J, Smeets R, Stipec MR, Vrasti R, Hasin D, Room R, Van Den Brink W, Regier D, Blaine J, Grant BF, Sartorius N. WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: Overview of methods and results. Drug & Alcohol Depend. 1997;47:161–9. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- Villodas MT, Litrownik AJ, Thompson R, Roesch SC, English DJ, Dubowitz H, Kotch JB, Runyan DK. Changes in Youth’s Experiences of Child Maltreatment Across Developmental Periods in the LONGSCAN consortium. Psychol Violence. 2012;2:325–338. doi: 10.1037/a0029829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall G, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college. JAMA. 1994;272:1672. [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]