Abstract
Background:
Ginger has been used as an herbal drug for a long time for the treatment of chronic inflammatory conditions.
Materials and Methods:
This randomized, double-blind clinical trial was conducted on 67 healthy adults with at least one impacted lower third molar. Participants were randomly allocated into three groups: Ibuprofen, Ginger, and placebo. Evaluation of inflammation was done by measuring cheek swelling, mouth opening ability, serum C-reactive protein (CRP) levels, and visual analog scale (for pain scoring). The number and the time of using rescue medication were recorded too.
Results:
Sixty patients completed the study. In all three groups, there was a significant increase in the mean cheek swelling measures, compared with the baseline, until day 5. The reduction in mouth opening ability was significant in all three groups, compared with the baseline, until day 5. There was no significant difference between ibuprofenand ginger groups in pain scores in all follow-up days. Number of required rescue medication on the day of surgery was significantly more in the placebo group. No significant or strong correlations were found between CRP levels and clinical findings.
Conclusion:
Within the limitations of this study, it can ban be concluded that gingerpowder is as effective as ibuprofenin the management of postsurgical sequelae. Furthermore, CRP levels alone are not suggested for the assessment of anti-inflammatory effects of drugs.
Keywords: C-reactive protein, Ginger, Ibuprofen, surgery, third molar
INTRODUCTION
Ginger, the rhizome of Zingiber officinale, has been used as an herbal drug for a long time. In traditional Chinese and Indian medicine, gingerhas been used to treat a wide range of diseases including stomach ache, diarrhea, nausea, asthma, respiratory disorders, toothache, gingivitis, and arthritis. A number of studies have shown interest in gingerfor the treatment of chronic inflammatory conditions. This interest can be traced to the discovery in the early 1970s that nonsteroidal anti-inflammatory drugs (NSAIDs) insert their effects by inhibiting the biosynthesis of prostaglandins (PGs). Soon thereafter, ginger was found to contain constituents that inhibit PG synthesis too. This finding provided a sound scientific rationale for its anti-inflammatory effects. Subsequent studies revealed that some of the constituents of ginger have pharmacological properties similar to the novel class of dual-acting NSAIDs. Compounds in this class can inhibit arachidonic acid metabolism through both the cyclooxygenase (COX) and lipoxygenase (LOX) pathways and have notably fewer side effects than conventional NSAIDs.[1,2] Different animal studies revealed that orally prescribed dried ginger or ginger extract can reduce acute inflammation.[3,4,5,6] Several clinical studies support the value of ginger for the treatment of osteoarthritis, and in some cases, a significant reduction in knee pain was reported.[1,7,8,9] In some of these trials, it was resulted that Ginger relieved pain and swelling to varying degrees in patients with osteoarthritis, rheumatoid arthritis, and muscular pain without causing serious adverse effects even after long periods of use.[10] Ozgoli et al. tested ginger in primary dysmenorrhea in comparison with ibuprofen and mefenamic acid, and no significant differences were found between the study groups in relief, stability, or aggravation of symptoms.[11]
In this study, dental pain model is used because it is a widely employed, validated, and highly standardized acute pain model and is the most appropriate model to investigate the onset of analgesic action.[12] The model is widely accepted and has a proven record of assay sensitivity. Therefore, it is often used as the primary clinical pain model for the investigation of analgesic drugs.[13] Compounds with anti-inflammatory properties provide better analgesia than centrally acting analgesics in this model.[12]
The common postoperative sequelae of surgical removal of impacted teeth are pain, trismus, and swelling with COX and PGs playing a central role.[13] The efficacy of ibuprofen in the treatment of postoperative dental pain has been demonstrated in several clinical trials. However, NSAIDs are contraindicated in patients with gastrointestinal ulcers, bleeding disorders, and renal dysfunctions.[13,14,15,16,17] Therefore, there is a need for an effective analgesic with a more favorable safety profile. In the literature, despite high anti-inflammatory potential of ginger constituents, it was used mainly against chronic inflammatory conditions while its effect on acute inflammation was assessed in animal studies and rare clinical trials. Therefore, our aim was to investigate the ability of ginger powder to reduce postoperative sequelae after mandibular third molar surgery.
MATERIALS AND METHODS
The protocol of this randomized, double-blind, placebo-controlled study was approved by the Ethics Committee of the local institution in Qazvin. In the limited time of 12 months, all patients fulfilling the criteria of the study were entered. All the study protocols were explained to each patient, and an informed written consent was obtained from all volunteers.
Patients
Sixty-seven outpatients undergoing elective surgical removal of impacted mandibular third molars participated in the present study. All patients were of the American Society of Anesthesiologists class I, aged 18–35 of either sex, with at least high school graduation diploma educational degree and at least one impacted mandibular third molar. Reasons for exclusion from the study were known allergy to the study medications, pregnancy or lactating, history of peptic ulceration, history of corticosteroid use, history of any kind of inflammatory conditions or taking any medication since 1 month before surgery, duration of surgery more than 30 min, any infection, fever or suffering any kind of disease during the following days, any mouthwash (except normal saline) or applying ice pack use during the following days, failure to attend the follow-up, using any kind of medication other than prescribed in this study, mentally incapable of understanding or complying with the study protocol, or refusing to sign the informed consent.
Baseline investigations including a panoramic view of the jaws and clinical evaluation of the third molars were done by a single oral and maxillofacial surgeon to score the difficulty.[18]
Study design
Patients fulfilling the criteria were randomly allocated into one of the three groups to receive one capsule of ginger containing 500 mg of ginger rhizome powder (Zintoma; Goldaru Co., Iran), one capsule of ibuprofen 400 mg (ibuprofen; Arya Co., Iran), or placebo. All medications were prepared by a pharmacist and packed in similar capsules and packages. All the packages were coded by the pharmacist. Operator, and other members of the team had no knowledge of the medications under each code. The placebo was a capsule containing starch. All medications were administered orally and 6 hourly. The first dose was administered immediately after completion of surgery and before terminating of the anesthetic effect. Rescue medication in the form of acetaminophen (500 mg with at least 4 h intervals) was allowed when required after surgery for all the patients. Patients were encouraged not to use any rescue medication for the first 4 h postoperatively. The time and number of rescue medication each patient took was recorded by the patient in the prepared questioners. All patients received amoxicillin 500 mg 8 hourly for 1 week postoperatively to prevent infection of the surgical site.
All the surgeries were accomplished by a single maxillofacial surgeon. Surgery was carried out under routine local anesthesia (lidocaine 2% +1:80,000 epinephrine, inferior alveolar nerve block with long buccal nerve block). The surgical procedure consisted of a buccal incision started from ascending ramus to the mesial of second molar, mucoperiosteal flap elevation, buccal and distal bone removal, splitting and elevation of the impacted tooth, rinsing the socket by normal saline and interrupted simple suturing using 3/0 braided silk. The exact time at which surgery ended, duration of each operation and the quantity of the consumed local anesthetic cartridges were recorded. Written forms containing standard postoperative instructions were given to patients in addition to researchers’ explanations. Patients were not allowed to use any kind of mouthwashes (except normal saline) or ice packs until the last follow-up day. After surgery, it was explained for all patients how they have to use the medications and fill in the questionnaires.
Postoperatively, parameters of cheek swelling, pain, amount of mouth opening, and serum high-sensitivity C-reactive protein (hsCRP) concentration were measured. Cheek swelling was recorded by cheek thickness measurement using standard calipers,[18] from the mucosal lingual aspect of the cheek opposite to the mid-portion of the crown of the mandibular first molar to the tangent of the skin of the cheek, before surgery (baseline) and on days 1, 3, and 5 postoperatively. To have similar and consistent amount of mouth opening in patients at the time of measuring the cheek thickness, we used a modified bite block in premolar area for all patients. With this bite block, patients had the minimum amount of mouth opening (4–5 mm), in which measuring the cheek thickness was possible.
Mouth opening ability was assessed by measuring the distance between the upper and lower central incisal edges at maximal mouth opening before surgery (baseline) and on days 1, 3, and 5 after surgery. Pain was assessed using a 100 mm visual analog scale (VAS) stretching from “no pain” (0 mm) to “the worse pain I’ve ever had” (100 mm) before surgery, at 1 h intervals in the first 12 h following the surgery and every 6 h until day 4 after surgery. Pain intensity measurement was made by the patient at home and in prepared questionnaires. To measure serum CRP concentrations, the first venous blood sample (4 ml) was collected immediately after surgery and before taking the medication and the second sample was collected 72 h after surgery (5 ml). Samples immediately delivered to the laboratory and centrifuged. The separated serums were assessed using sandwich ELISA technique to quantitatively determine CRP concentrations.
Any adverse drug reaction during the study was recorded by patients or the investigator.
Statistical analysis
Statistical analysis was performed using SPSS version 15(SPSS Inc. IBM Corporation). Repeated measure and ANOVA tests were used to assess the significance of changes of mean cheek swelling (mCS) and mean maximum mouth opening (mMMO). To analyze the VAS scores’ variations, Mann–Whitney and ANOVA tests were used. To assess the changes in CRP amounts and the correlation between CRP levels and clinical symptoms, ANOVA test and Pearson correlation coefficient were used, respectively. Statistical significance was assumed at 0.05.
RESULTS
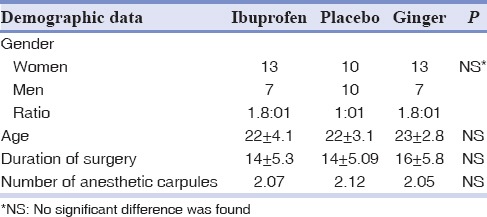
Out off 67 participants entered into the study (26 men, 41 women), seven (two men, five women) were excluded due to two follow-up visits failure, one because blood sampling was not possible, two for catching cold in the follow-up days, one for not taking the drugs, and one for reporting heartburn on the second day after surgery. Hence, data of sixty patients were analyzed. There were no significant differences in demographic and baseline characteristics, operation time, and amount of consumed local anesthetic for the surgery [Table 1].
Table 1.
Demographic characteristics of the study patients (n=60), duration of surgery and amount of local anesthetic used (mean±standard deviation)
Parameters of mouth opening and cheek swelling were assessed three times in each follow-up visit, and the mean was used in analyses [Tables 2 and 3]. The mean amount of cheek swelling (mCS) and mean amount of mMMO were recorded in the follow-up days (baseline, days 1, 3, and 5 postoperatively) and their changes were assessed in and between groups. In the intergroup assessment, the amount of mCS and mMMO of each drug in each follow-up day was compared to the baseline and to the first postoperative day (in which the maximum amount of mCS and minimum amount of mMMO were observed). In the intragroup assessment, the amount of mCS and mMMO changes of each drug in each follow-up day was compared with other drugs. Regarding mCS, the intergroup assessments demonstrated that in all three groups, there was a significant increase in the mCS compared with the baseline until day 5. In addition, in all three groups, no significant reduction in amounts of mCS was observed on days 3 and 5 compared with day 1. The intragroup assessment showed no significant differences of mCS changes in follow-up days between three groups.
Table 2.
Mean of cheek swelling of patients on the day of surgery and follow-up sessions (mean±standard deviation)
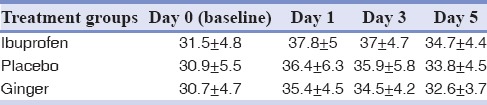
Table 3.
Mean of maximum mouth opening of patients on the day of surgery and follow-up sessions (mean±standard deviation)
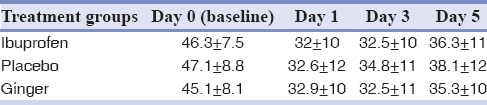
In all follow-up days, no significant increase in the amount of mMMO was observed in follow-up days compared with the baseline in any of three groups. In addition, there was no significant increase in amounts of mMMO on days 3 and 5 compared with day 1. There was no significant difference between three groups and in any of the follow-up days in mMMO amounts.
There was no significant difference in CRP concentrations in the immediate postoperative samples among the groups. Blood samples collected 72 h postoperatively showed significant elevations in CRP levels. However, this difference was not significant between the groups. Correlations of CRP levels and severity of clinical symptoms (VAS, mCS and mMMO) between day 3 and baseline were assessed too. Results revealed no significant and strong correlations between these parameters.
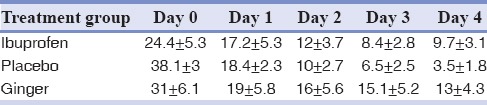
There was no significant difference in presurgical pain intensity between groups [Table 4 and Figure 1]. In all groups, the maximum pain score was reported on the day of surgery (day 0). In this day, in ibuprofen and ginger groups, the mean pain score was in mild range (30–45), and in placebo group, it was in moderate range (45–70). There was no significant difference between ibuprofen and ginger groups in reported pain scores of the day of surgery (day 0); however, in some of the postoperative hours, ginger and ibuprofen decreased pain intensity significantly more than placebo. None of the groups showed a significant reduction in pain intensity scores on day 1 in comparison with day 0. In both ibuprofen and ginger groups, the mean pain scores were reduced significantly from day 2 onward in comparison with placebo, but this amount was not significantly different between ibuprofen and ginger groups. The mean pain intensity scores of days 1, 2, 3, and 4 were not significantly different between three groups [Table 5].
Table 4.
Median pain score (mm) on the day of surgery (day 0) (median±standard error)
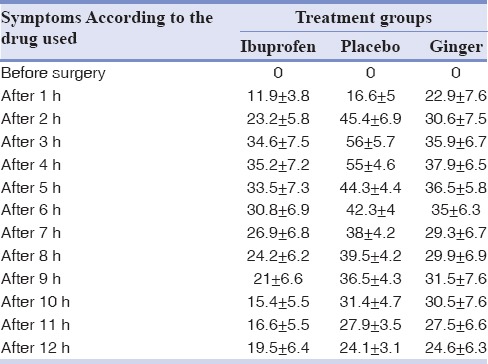
Figure 1.
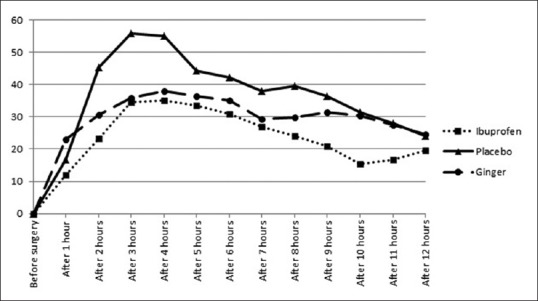
Median pain score (mm) of three study groups on the day of surgery (day 0).
Table 5.
Mean pain score (mm), day 0 through day 4 (mean±standard deviation)
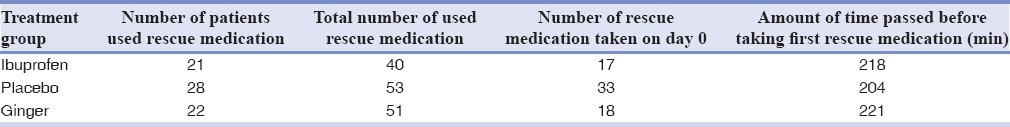
Data regarding the use of rescue medication in all groups are presented in Table 6. The placebo group required acetaminophen significantly more than other groups on the day 0. In placebo group, 80% of patients took their first rescue medication in the first 2–4 h after surgery, but in other groups, only 35% of patients did.
Table 6.
Amount and time of used rescue medications
No abnormal wound bleeding was observed in the follow-up sessions. Only two patients in Ginger group complained of their wound oozing 48 h after surgery. No adverse drug reactions that need any alteration in the treatment were reported.
DISCUSSION
The common postsurgical sequelae of third molar surgery are related to local inflammatory reactions with COX pathway and PGs playing an important role in it.[12] The efficacy of corticosteroids and NSAIDs which directly affect this inflammatory pathway has been evaluated in several studies.[14,16,17] In the present study, regarding the dual COX and LOX inhibitory reaction of ginger, we tried to assess ginger's ability to control the postoperative sequelae of this acute pain model.
No significant differences were observed in mean mouth opening ability and mCS between ibuprofen, ginger, and placebo groups. All patients were experienced their greatest level of pain on the day of surgery with a peak of 4 h after surgery which was in the range of previous studies’ reports. On the surgery day and all postoperative follow-up days, ginger was as effective as ibuprofen in reducing postoperative pain intensity. The total number of used rescue medications was not significantly different between groups; however, on the day of surgery, the placebo group took rescue medication two times more than the other groups.
Ibuprofen is the most commonly used drug for pain relief after oral surgery. In the previous studies, ibuprofen was not superior to placebo in reducing postoperative swelling but was significantly effective in reducing the pain on the day of surgery.[14] Our results about ibuprofen confirmed the earlier studies. It has been shown that ginger was as effective as ibuprofen and mefenamic acid in relieving menstrual pain.[11] Different studies have assessed the efficacy of ginger in reducing osteoarthritic pain and symptoms. Haghighi et al. indicated that ginger extract could be used as an alternative to ibuprofen and as a supplement drug in patients with osteoarthritis.[9] Bliddal et al. found that ibuprofen was significantly more effective than ginger and ginger was significantly more effective than placebo in relieving chronic pain and the same trend was found for acetaminophen consumption.[8] In a crossover study, Wigler et al. reported that in the 12 weeks period of the first phase (before crossover), ginger showed the placebo effect, but at the end of the second phase and after 24 weeks, the groups reached a statistically significant difference. They concluded that these results were due to delayed effect of ginger extract and lack of a washout period in the research.[7] Following reasons limit the exact comparison of our results with the previously mentioned studies: Chronic inflammatory process of assessed disease, a different form of prescribed ginger (extract vs. powder), duration of treatment, and difference in assessed clinical signs and symptoms. In our study, the difference between ibuprofen and ginger groups was not significant in any of the postoperative sequelae. Our results indicate that ginger was almost as effective as ibuprofen in relieving postoperative sequelae. In some of the studies which used third mandibular molar surgery pain model, only CRP concentration was assessed to indicate the anti-inflammatory effect of different drugs and methods.[19,20] We found no strong or significant correlations between CRP levels and clinical symptoms in this study. Assessment of different ginger extracts and more specific inflammatory mediators besides clinical symptoms are our suggestions for further studies.
CONCLUSION
Within the limitations of this study, it can be concluded that ginger is as effective as ibuprofen in controlling postoperative sequelae, especially pain, and it can be an efficient substitute for this synthetic agents. Considering the standard deviation and interquartile range which indicated more data scattering in ginger group, however, it seems that ibuprofen, at least in some parts of the day of surgery, may be more efficient in pain control. Lack of significant correlations between CRP levels and severity of clinical symptoms makes using serum CRP concentrations as the only criteria for anti-inflammatory effect assessment, inappropriate.
Financial support and sponsorship
This research was financially supported by the research deputy of Qazvin University of Medical Sciences.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
Acknowledgments
The authors wish to thank Dr. Mehran Pourghasemi for his valuable assistance in preparing the study drugs.
REFERENCES
- 1.Grzanna R, Lindmark L, Frondoza CG. Ginger – An herbal medicinal product with broad anti-inflammatory actions. J Med Food. 2005;8:125–32. doi: 10.1089/jmf.2005.8.125. [DOI] [PubMed] [Google Scholar]
- 2.Ali BH, Blunden G, Tanira MO, Nemmar A. Some phytochemical, pharmacological and toxicological properties of ginger (Zingiber officinale Roscoe): A review of recent research. Food Chem Toxicol. 2008;46:409–20. doi: 10.1016/j.fct.2007.09.085. [DOI] [PubMed] [Google Scholar]
- 3.Chrubasik S, Pittler MH, Roufogalis BD. Zingiberis rhizoma: A comprehensive review on the ginger effect and efficacy profiles. Phytomedicine. 2005;12:684–701. doi: 10.1016/j.phymed.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 4.Ojewole JA. Analgesic, antiinflammatory and hypoglycaemic effects of ethanol extract of Zingiber officinale (Roscoe) rhizomes (Zingiberaceae) in mice and rats. Phytother Res. 2006;20:764–72. doi: 10.1002/ptr.1952. [DOI] [PubMed] [Google Scholar]
- 5.Aimbire F, Penna SC, Rodrigues M, Rodrigues KC, Lopes-Martins RA, Sertié JA. Effect of hydroalcoholic extract of Zingiber officinalis rhizomes on LPS-induced rat airway hyperreactivity and lung inflammation. Prostaglandins Leukot Essent Fatty Acids. 2007;77:129–38. doi: 10.1016/j.plefa.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Fouda AM, Berika MY. Evaluation of the effect of hydroalcoholic extract of Zingiber officinale rhizomes in rat collagen-induced arthritis. Basic Clin Pharmacol Toxicol. 2009;104:262–71. doi: 10.1111/j.1742-7843.2008.00363.x. [DOI] [PubMed] [Google Scholar]
- 7.Wigler I, Grotto I, Caspi D, Yaron M. The effects of Zintona EC (a ginger extract) on symptomatic gonarthritis. Osteoarthritis Cartilage. 2003;11:783–9. doi: 10.1016/s1063-4584(03)00169-9. [DOI] [PubMed] [Google Scholar]
- 8.Bliddal H, Rosetzsky A, Schlichting P, Weidner MS, Andersen LA, Ibfelt HH, et al. A randomized, placebo-controlled, cross-over study of ginger extracts and ibuprofen in osteoarthritis. Osteoarthritis Cartilage. 2000;8:9–12. doi: 10.1053/joca.1999.0264. [DOI] [PubMed] [Google Scholar]
- 9.Haghighi M, Khalvat A, Toliat T, Jallaei SH. Comparing the effects of ginger (Zingiber officinale) extract and ibuprofen on patients with osteoarthritis. Arch Iran Med. 2005;8:267–71. [Google Scholar]
- 10.Abascal K, Yarnel E. Clinical uses of Zingiber officinale (ginger) J Altern Complement Med. 2009;15:231–7. [Google Scholar]
- 11.Ozgoli G, Goli M, Moattar F. Comparison of effects of ginger, mefenamic acid, and Ibuprofen on pain in women with primary dysmenorrhea. J Altern Complement Med. 2009;15:129–32. doi: 10.1089/acm.2008.0311. [DOI] [PubMed] [Google Scholar]
- 12.Kleinert R, Lange C, Steup A, Black P, Goldberg J, Desjardins P. Single dose analgesic efficacy of tapentadol in postsurgical dental pain: The results of a randomized, double-blind, placebo-controlled study. Anesth Analg. 2008;107:2048–55. doi: 10.1213/ane.0b013e31818881ca. [DOI] [PubMed] [Google Scholar]
- 13.Daniels S, Reader S, Berry P, Goulder M. Onset of analgesia with sodium ibuprofen, ibuprofen acid incorporating poloxamer and acetaminophen – A single-dose, double-blind, placebo-controlled study in patients with post-operative dental pain. Eur J Clin Pharmacol. 2009;65:343–53. doi: 10.1007/s00228-009-0614-y. [DOI] [PubMed] [Google Scholar]
- 14.Chopra D, Rehan HS, Mehra P, Kakkar AK. A randomized, double-blind, placebo-controlled study comparing the efficacy and safety of paracetamol, serratiopeptidase, ibuprofen and betamethasone using the dental impaction pain model. Int J Oral Maxillofac Surg. 2009;38:350–5. doi: 10.1016/j.ijom.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Hupp RJ. Postoperative patient management. In: Hupp RJ, Eliss E 3rd, Tucker RM, editors. Contemporary Oral and Maxillofacial Surgery. Chicago: Mosby; 2008. p. 179. [Google Scholar]
- 16.Jung YS, Kim DK, Kim MK, Kim HJ, Cha IH, Lee EW. Onset of analgesia and analgesic efficacy of tramadol/acetaminophen and codeine/acetaminophen/ibuprofen in acute postoperative pain: A single-center, single-dose, randomized, active-controlled, parallel-group study in a dental surgery pain model. Clin Ther. 2004;26:1037–45. doi: 10.1016/s0149-2918(04)90175-0. [DOI] [PubMed] [Google Scholar]
- 17.Litkowski LJ, Christensen SE, Adamson DN, Van Dyke T, Han SH, Newman KB. Analgesic efficacy and tolerability of oxycodone 5 mg/ibuprofen 400 mg compared with those of oxycodone 5 mg/acetaminophen 325 mg and hydrocodone 7.5 mg/acetaminophen 500 mg in patients with moderate to severe postoperative pain: A randomized, double-blind, placebo-controlled, single-dose, parallel-group study in a dental pain model. Clin Ther. 2005;27:418–29. doi: 10.1016/j.clinthera.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 18.Marciani RD. Third molar removal: An overview of indications, imaging, evaluation, and assessment of risk. Orall Maxillofac Surg Clin North Am. 2007;19:1–13. doi: 10.1016/j.coms.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 19.El-Sharrawy EA, El-Hakim IE, Sameeh E. Attenuation of C-reactive protein increases after exodontia by tramadol and ibuprofen. Anesth Prog. 2006;53:78–82. doi: 10.2344/0003-3006(2006)53[78:AOCPIA]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freitas AC, Pinheiro AL, Miranda P, Thiers FA, Vieira AL. Assessment of anti-inflammatory effect of 830 nm laser light using C-reactive protein levels. Braz Dent J. 2001;12:187–90. [PubMed] [Google Scholar]


