Introduction
The increasing prevalence of multiple chronic conditions among individuals of all ages compels health services researchers to better understand the health-related quality of life (HRQOL) of co-occurring illness.1 About 1 in 4 adults and 2 in 3 Medicare beneficiaries have multiple chronic conditions.2,3 Co-occurring conditions are particularly common among individuals with substance use disorders: approximately 39% of adults in the U.S. who have a substance use disorder also have a mental health disorder4, and 50–80% of injection drug users are infected with both HIV and the Hepatitis C virus (HCV).5 Because the incidence of opioid use disorder is increasing dramatically6, understanding the HRQOL of opioid use disorder, its treatment, and co-occurring conditions, is critical to decisions about optimal intervention.
Comparative effectiveness research, including cost-utility and cost-effectiveness analysis (CUA and CEA), are useful to inform decision making. CUA and CEA use quality adjusted life years (QALYs) as the outcome measure to quantify benefits accrued by an intervention or treatment relative to costs. QALYs are a function of the quality and longevity of a person’s life; they are the product of their health-related quality of life (HRQOL) for a particular health state and the number of years that they live in that state. HRQOL is measured via health state utilities, which are an economic concept that quantifies HRQOL on a uniform scale so that it is comparable across conditions.7 Simultaneously-occurring conditions present challenges for CUA and CEA because we do not fully understand how having two (or more) conditions at once affects HRQOL. We therefore have difficulty predicting the health state utilities and QALYs that accompany an intervention or treatment directed toward one condition in someone with multiple conditions—we do not know how the utility resulting from the second (or third) condition may change, or not, by one being resolved.8 Because of the sheer volume of possible simultaneously-occurring health conditions, mechanisms for combining health state utilities for individually-occurring conditions into multiple-state utilities would be highly useful for CEA and CUA.8
Recent literature has posited methods of estimating multiple-state utility from the constituent individual (“single”) states—that is, taking known utilities for individual states and mathematically combining them to arrive at a utility for the combination state.9 Such methods are commonly called “joint utility estimation.” Simultaneously occurring health states can take many forms in how they affect an individual. They can vary from being independent, meaning the experience of one has no effect on the experience of the other, to being interdependent, meaning the experience of one affects the experience of the other. For most co-occurring conditions, one likely ameliorates or exacerbates the experience of the other to some degree. Conditions that are physiologically unrelated, for example, such as blindness and breast cancer, are likely experienced only minimally differently when they co-occur than when they are experienced individually. Breast cancer has little effect on the experience of blindness and vice versa. Those that are physiologically related, on the other hand, such as opioid use disorder and chronic pain, are likely experienced very differently when they co-occur. Pain is alleviated by opioids so it is ameliorated in the presence of opioid use disorder and would have a better HRQOL than when experiences alone. Estimating joint utilities is therefore a complicated task that involves assumptions about individuals’ experiences.
The literature has proposed five options for estimating joint health state utility from single states’ utility. Methods have been assessed based on their mathematical accuracy in predicting observed joint states’ utility from observed single states’ utility. More recent literature has attempted to incorporate psychological mechanisms to explain the relationship between the two. The five options are: (1) the minimum estimator, in which the lesser of two single states’ utilities is used as an estimate of their joint utility; (2) the additive, or constant decrement estimator, in which the sum of the two single states’ disutilities (i.e., 1-utility) is subtracted from perfect health (1.0) to estimate their joint utility (to a minimum of 0); (3) the multiplicative estimator, in which the product of the two single states’ utilities is used as an estimate of their joint utility10; (4) the “linear index estimator,” a parametric model that uses the weighted sum of the minimum and maximum of the two single state’s utilities and their interaction to estimate the joint state’s utility 11; and (5), the “adjusted decrement estimator,” a non-parametric model that combines the two single state’s utilities in proportion to the difference between them.12 There is a lack of consensus on the best estimator among this list and research has shown conflicting results.9 We conducted this study to assess the accuracy of joint health state utility estimators in the context of substance use disorders (SUD), a case in which co-occurring conditions are common and none of these estimators has been tested. Our goal was to inform the estimation of utility scores for use in economic evaluation of SUD treatments and interventions.
Methods
Study Design
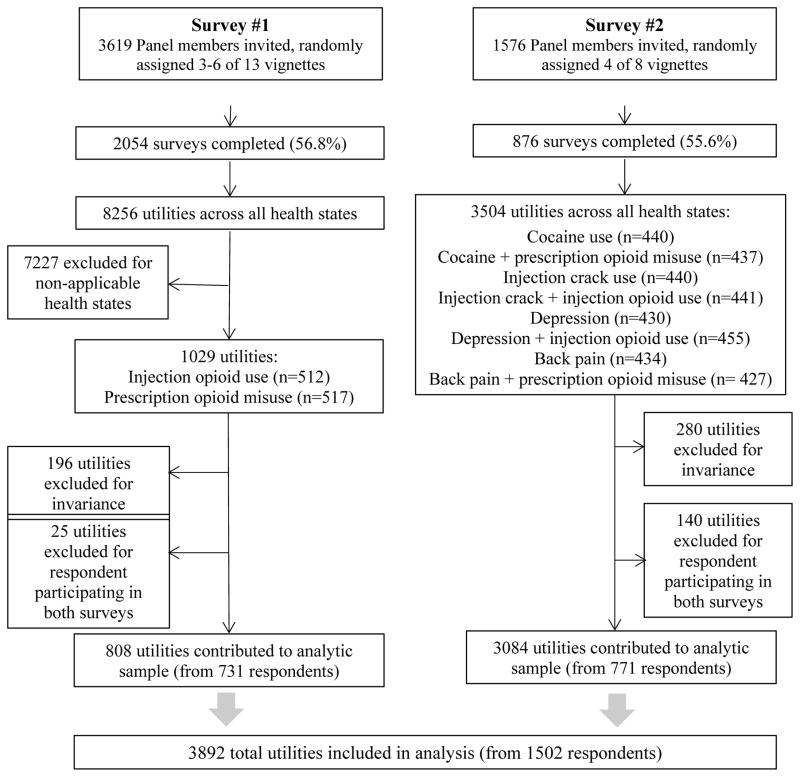
We conducted a series of two cross-sectional, internet-based utility surveys of a representative panel of the U.S. adult, non-institutionalized population (the GfK Knowledge Panel13), in December 2013–January 2014 and in March–April 2015. We administered the identical survey to a randomly selected sample of the panel at these two time points, varying only the health states that were evaluated. We elicited community perspective utilities by asking a sample of the general population to evaluate hypothetical health state descriptions, following accepted practice.7 We asked each respondent to evaluate between 3 and 6 randomly assigned hypothetical health state descriptions describing substance use disorder, common co-occurring conditions (depression and chronic pain), polysubstance use, and substance use disorder and co-occurring conditions occurring simultaneously. We estimated community-perspective utilities because of their usefulness for economic evaluation7,14, and used direct elicitation methods to avoid the need for recruiting patients with these conditions as is required in indirect utility assessment15 (direct measures ask a sample of the general population to evaluate hypothetical health state descriptions that they may or may not have personally experienced; indirect measures ask a sample of individuals with a particular condition to complete an assessment instrument to which population utilities are assigned7). Utility data from the two surveys were combined to create the analytic dataset; complete results from the first survey are reported elsewhere (Figure 1).16
Figure 1.
Data sources for analytic sample
For both surveys, respondents evaluated their own current health as a practice exercise before evaluating the hypothetical health states, and provided basic demographic information at the end (which was supplemented with additional demographic data provided by the survey research firm). A 100-point rating scale was used as a warm-up before standard gamble (SG) evaluations.7 The SG technique typically asks respondents to choose between living in a described (hypothetical) health state for the rest of their life and accepting a “gamble” that includes a chance of death and a chance of living in perfect health. The chance of death and perfect health in the gamble are varied until the point that the respondent is indifferent between living in the described health state and taking the gamble.7 We used visual aids to help respondents comprehend probabilities (dot matrices). Respondents finished the gamble exercise after multiple iterations when a desired level of precision was reached for the indifference point (0.01 utility for our surveys), or if they toggled back-and-forth between the same two values three times. They could also indicate indifference by selecting a response button labeled “too hard to choose”. A respondent could choose a button “I know my answer” to avoid the iterative chance presentation process, and type-in a value between 0 and 100%. Error messages were presented on the screen if a respondent selected a potentially illogical response, with an option to revise the answer (e.g., choosing to take a pill with 100% chance of death and 0% chance of perfect health, which is tantamount to selecting suicide in the face of a described health state).17
We followed established practice in developing the hypothetical health state descriptions18: for the first survey we collected qualitative data from individuals in substance abuse treatment programs and combined it with data from the literature and expert opinion; for the second survey we used data from the literature and expert opinion.16 All health state descriptions were reviewed by clinical practitioners and refined by the investigators before inclusion in the survey. All included similar domains and were of similar length; none was identified by name to respondents. We included a total of 10 health states in our analysis: injection opioid use, prescription opioid misuse, cocaine use, injection crack use, chronic back pain, and moderate depression, plus the simultaneously-occurring states of cocaine and prescription opioid misuse, injection crack and injection opioid use, back pain and prescription opioid misuse, and depression and injection opioid use. The simultaneously occurring states were described as one hypothetical state that an individual was experiencing, with all characteristics that would exist when the simultaneous states co-occur. Injection opioid use and prescription opioid misuse were evaluated in the first survey and the rest in the second survey (Figure 1; all health state descriptions are included in the Appendix).
The sample sizes for the surveys were designed to detect meaningful differences in mean values between health states based on existing estimates of values for similar health states using similar measures.19 Minimally important differences in utilities across measurement techniques and conditions range from 0.03–0.07.20,21 We sought a sample of approximately 425–475 responses per health state to detect these differences based on conservative assumptions about variation in observed means.
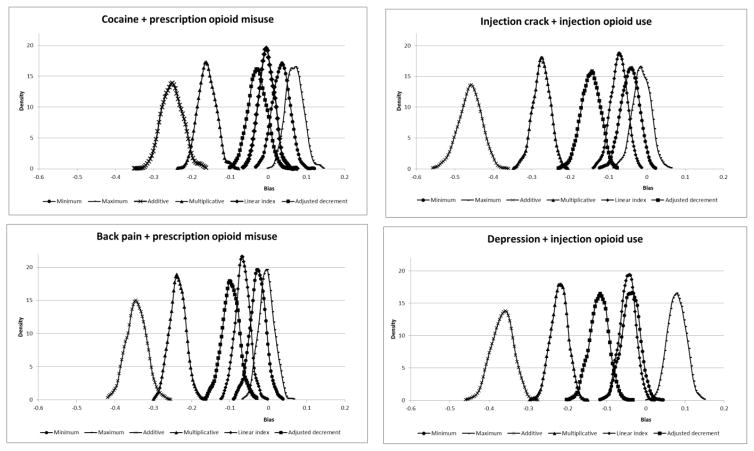
Statistical Analysis
We created an analytic data set that excluded responses that failed invariance criteria, which were defined as those responses in which all SG responses from a respondent including the practice question were the same and equal to 0 (the minimum), 0.5 (the starting point for the exercise) or 1.0 (the maximum).17 We also excluded utilities in both surveys provided by respondents who by chance participated in both. We calculated means and 95% confidence intervals for the SG utilities for all states. We calculated the predicted utility for the joint states using five joint health state estimators described in the literature (additive, multiplicative, minimum, linear index, and adjusted decrement) and one that we hypothesized to be relevant in this context (maximum), and descriptively compared each to the directly measured utility for each joint health state using measures reported in the literature (bias and root mean square error (RMSE)).9 We used 1,000 bootstrap iterations to estimate the bias (defined as the predicted mean using the estimator minus the observed mean) and RMSE (defined as the square root of the mean of the square of all errors between predicted and observed utilities) for the joint state estimators relative to the observed joint state utilities, and calculated the 95% confidence interval for the bias and the interquartile range for the RMSE. Finally, we visually depicted the bias for each estimator with bias density curves showing the dispersion of the bootstrapped estimates. This graphing technique allows for comparison among estimators relative to a zero bias line and indicates the precision of each estimator (i.e., curves further from 0 bias indicate larger bias and those broader in span indicate less precision). Analyses were conducted in Stata version 12 (Stata Corporation, College Park, TX); graphs were made using MS Excel.
The study was approved by the Harvard T.H. Chan School of Public Health and Weill Cornell Medicine institutional review boards. Financial support was provided by a grant from the National Institute on Drug Abuse, R01DA033424. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Results
A total of 876 respondents completed the second survey, providing 3504 utilities for 8 health states (55.6% completion rate; Figure 1). After excluding invariant responses (n=280) and utilities received from those respondents who participated in the first survey as well (n=140), we had 3084 utilities from 771 respondents for the analytic sample. We combined these with 808 utilities from 731 respondents from the first survey (after exclusions for invariant responses (n=196) and utilities from respondents who participated in both surveys (n=25)), for a total of 3,892 utilities from 1502 respondents for analysis.
Respondents to both surveys were about half female, nearly three-quarters white, over 60% married, and over half had completed at least some college and were employed (Table 1). Utilities for all health states are presented in Table 2, and ranged from 0.555 to 0.714. Comparing the directly measured utilities for the joint states with their constituent individually-occurring states, the mean utility for the cocaine use and prescription opioid misuse state was lower than that of each individually-occurring state, while the mean utility for moderate depression and injection opioid use state was between that of the two individually-occurring states. The mean utilities for the remaining joint states (injection crack use and injection opioid use, chronic back pain and prescription opioid misuse) were both higher than the utilities for their constituent, individually-occurring states.
Table 1.
Sample characteristics of first and second surveys’ complete and analytic samples and US population data
| First surveya | Second survey | US population | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Complete sample (n=900) | Analytic sample (n=731) | Complete sample (n=839) | Analytic sample (n=771) | ||||||
|
| |||||||||
| n | % | n | % | n | % | n | % | % | |
| Age | |||||||||
| 18–24 | 83 | 9.2 | 69 | 9.4 | 75 | 8.9 | 72 | 9.3 | 6.8b,c,24 |
| 25–44 | 275 | 30.6 | 212 | 29.0 | 258 | 30.8 | 226 | 29.3 | 26.5 |
| 45–64 | 350 | 38.9 | 284 | 38.9 | 328 | 39.1 | 303 | 39.3 | 26.4 |
| 65+ | 192 | 21.3 | 166 | 22.7 | 178 | 21.2 | 170 | 22.1 | 13.8 |
|
| |||||||||
| Education | |||||||||
| Less than high school | 83 | 9.2 | 67 | 9.2 | 66 | 7.8 | 58 | 7.5 | 13.725 |
| High school | 294 | 32.7 | 239 | 32.7 | 245 | 29.2 | 216 | 28.0 | 28.0 |
| Some college | 244 | 27.1 | 197 | 27.0 | 248 | 29.6 | 230 | 29.8 | 31.3 |
| Bachelor’s degree or higher | 279 | 31.0 | 228 | 31.2 | 280 | 33.4 | 267 | 34.6 | 27.0 |
|
| |||||||||
| Race/Ethnicity | |||||||||
| White NH | 669 | 74.3 | 550 | 75.2 | 604 | 72.0 | 566 | 73.4 | 62.824 |
| Black NH | 78 | 8.7 | 62 | 8.5 | 85 | 10.1 | 71 | 9.2 | 12.2 |
| Other NH | 54 | 6.0 | 41 | 5.6 | 73 | 8.7 | 66 | 8.6 | 25.0 |
| Hispanic | 99 | 11.0 | 78 | 10.7 | 77 | 9.2 | 68 | 8.8 | 16.9 |
|
| |||||||||
| Gender: male | 442 | 49.1 | 352 | 48.2 | 430 | 51.3 | 396 | 51.4 | 49.224 |
|
| |||||||||
| Marital Status | |||||||||
| Widowed/Separated/Divorced/Never married | 345 | 38.3 | 281 | 38.4 | 289 | 34.5 | 265 | 34.4 | 49.726 |
| Married/living with partner | 555 | 61.7 | 450 | 61.6 | 550 | 65.6 | 506 | 65.6 | 50.3d |
|
| |||||||||
| Household Annual Income | |||||||||
| (US $) | |||||||||
| <$25,000 | 174 | 19.3 | 135 | 18.5 | 161 | 19.2 | 140 | 18.2 | 24.027 |
| $25,000–$49,999 | 201 | 22.3 | 158 | 21.6 | 163 | 19.4 | 151 | 19.6 | 23.0 |
| $50,000–$99,999 | 290 | 32.2 | 236 | 32.3 | 281 | 33.5 | 258 | 33.5 | 29.0 |
| $100,000+ | 235 | 26.1 | 202 | 27.6 | 234 | 27.9 | 222 | 28.8 | 24.0 |
|
| |||||||||
| Currently employed | 502 | 55.8 | 406 | 55.5 | 485 | 57.8 | 446 | 57.9 | 59.6e,28 |
%s may not sum to 100 due to rounding
NH=non-Hispanic
Survey respondents who provided utilities for states used in this analysis. Complete sample characteristics reported previously.16
Ages 20–24.
Age proportions of entire US population.
Includes married only, excluding living with partner.
Civilian population.
Table 2.
Directly measured SG utilities for single states and joint states: mean, standard error, and 95% confidence interval
| Health state | n | Mean | SE | 95% CI | |
|---|---|---|---|---|---|
| Cocaine use | 380 | 0.714 | 0.015 | 0.685 | 0.743 |
| Prescription opioid misuse | 406 | 0.680 | 0.015 | 0.652 | 0.709 |
| Cocaine + prescription opioid misuse | 382 | 0.647 | 0.016 | 0.615 | 0.679 |
| Injection crack misuse | 394 | 0.582 | 0.017 | 0.548 | 0.615 |
| Injection opioid use | 402 | 0.555 | 0.017 | 0.523 | 0.588 |
| Injection crack + injection opioid use | 384 | 0.597 | 0.017 | 0.563 | 0.631 |
| Moderate depression | 383 | 0.672 | 0.015 | 0.643 | 0.702 |
| Injection opioid use | 402 | 0.555 | 0.017 | 0.523 | 0.588 |
| Moderate depression + injection opioid use | 402 | 0.594 | 0.017 | 0.562 | 0.627 |
| Chronic back pain | 382 | 0.664 | 0.015 | 0.634 | 0.693 |
| Prescription opioid misuse | 406 | 0.680 | 0.015 | 0.652 | 0.709 |
| Chronic back pain + prescription opioid misuse | 377 | 0.687 | 0.015 | 0.657 | 0.716 |
The prediction methods underestimated the directly measured joint health state utilities 83% of the time (20 out of 24 predictions by 6 predictors for 4 health states; Table 3). The bootstrapped bias and RMSE for all estimators are presented in Table 4. The minimum estimator’s 95% confidence intervals for bias included zero for all 4 joint states (Figure 2). The maximum estimator’s 95% confidence intervals for bias included zero for 2 of the 4 states (back pain and prescription opioid misuse, injection crack use and injection opioid use), and the linear index estimator and adjusted decrement estimators’ included zero for one state (cocaine use and prescription opioid misuse). The RMSE was smallest for the linear index estimator for one state (cocaine use and prescription opioid misuse), for the maximum estimator for two states (back pain and prescription opioid misuse, injection crack use + injection opioid use), and was negligibly different between the minimum and linear index estimator for the fourth state (depression and injection opioid use). The second smallest RMSE for 3 states was the minimum, and for 1 it was the linear index. The additive and multiplicative estimators had the largest RMSE for all states.
Table 3.
Directly measured and predicted joint health state utilities for 6 alternative estimation methods, and whether estimation over or under-predicted directly measured utility: minimum, maximum, additive, multiplicative, linear index estimator, and adjusted decrement estimator
| Joint health state | Directly measured | Minimum | Maximum | Additive | Multiplicative | Linear Index | Adjusted decrement |
|---|---|---|---|---|---|---|---|
| Cocaine + prescription opioid misuse | 0.647 | 0.680↑ | 0.714↑ | 0.394↓ | 0.485↓ | 0.642↓ | 0.618↓ |
| Injection crack + injection opioid use | 0.597 | 0.555↓ | 0.582↓ | 0.137↓ | 0.323↓ | 0.525↓ | 0.452↓ |
| Depression + injection opioid use | 0.594 | 0.555↓ | 0.672↑ | 0.228↓ | 0.373↓ | 0.548↓ | 0.475↓ |
| Backpain + prescription opioid misuse | 0.687 | 0.664↓ | 0.680↓ | 0.344↓ | 0.451↓ | 0.622↓ | 0.592↓ |
↑ = estimator over-predicted observed joint utility; ↓ = estimator under-predicted observed joint utility.
Table 4.
Comparison of different estimators for predicting joint health state utilities in terms of bias (and standard deviation and 95% confidence interval) and root mean squared error (RMSE; and interquartile range)
| Cocaine + prescription opioid use misuse | |||||
|---|---|---|---|---|---|
| Estimator | Bias | SD | 95% CI | RMSE | IQR |
| Minimum | 0.033 | 0.023 | −0.011, 0.077* | 0.0016 | 0.018, 0.049 |
|
| |||||
| Maximum | 0.066 | 0.022 | 0.023, 0.110 | 0.0051 | 0.052, 0.083 |
|
| |||||
| Additive | −0.253 | 0.028 | −0.308, −0.199 | 0.0642 | −0.272, −0.233 |
|
| |||||
| Multiplicative | −0.162 | 0.023 | −0.207, −0.117 | 0.0263 | −0.176, −0.145 |
|
| |||||
| Linear Index | −0.006 | 0.020 | −0.045, 0.034* | 0.0004 | −0.018, 0.009 |
|
| |||||
| Adjusted decrement | −0.029 | 0.024 | −0.077, 0.018* | 0.0014 | −0.045, −0.012 |
|
| |||||
| Injection crack + injection opioid use | |||||
| Estimator | Bias | SD | 95% CI | RMSE | IQR |
|
| |||||
| Minimum | −0.041 | 0.023 | −0.087, 0.004* | 0.0024 | −0.059, −0.027 |
|
| |||||
| Maximum | −0.015 | 0.024 | −0.061, 0.031* | 0.0007 | −0.030, 0.002 |
|
| |||||
| Additive | −0.459 | 0.030 | −0.518, −0.401 | 0.2124 | −0.480, −0.440 |
|
| |||||
| Multiplicative | −0.274 | 0.022 | −0.317, −0.230 | 0.0756 | −0.288, −0.258 |
|
| |||||
| Linear Index | −0.071 | 0.021 | −0.112, −0.031 | 0.0057 | −0.087, −0.058 |
|
| |||||
| Adjusted decrement | −0.145 | 0.024 | −0.192, −0.097 | 0.0220 | −0.162, −0.129 |
|
| |||||
| Depression + injection opioid use | |||||
| Estimator | Bias | SD | 95% CI | RMSE | IQR |
|
| |||||
| Minimum | −0.039 | 0.023 | −0.084, 0.006* | 0.0020 | −0.054, −0.023 |
|
| |||||
| Maximum | 0.078 | 0.023 | 0.034, 0.122 | 0.0067 | 0.063, 0.095 |
|
| |||||
| Additive | −0.367 | 0.028 | −0.421, −0.312 | 0.1345 | −0.385, −0.346 |
|
| |||||
| Multiplicative | −0.221 | 0.022 | −0.263, −0.179 | 0.0490 | −0.235, −0.206 |
|
| |||||
| Linear Index | −0.046 | 0.020 | −0.085, −0.007 | 0.0025 | −0.059, −0.033 |
|
| |||||
| Adjusted decrement | −0.120 | 0.024 | −0.166, −0.074 | 0.0148 | −0.135, −0.103 |
|
| |||||
| Back pain + prescription opioid use misuse | |||||
| Estimator | Bias | SD | 95% CI | RMSE | IQR |
|
| |||||
| Minimum | −0.023 | 0.020 | −0.063, 0.017* | 0.0012 | −0.040, −0.013 |
|
| |||||
| Maximum | −0.007 | 0.020 | −0.046, 0.033* | 0.0004 | −0.018, 0.009 |
|
| |||||
| Additive | −0.343 | 0.026 | −0.394, −0.292 | 0.1192 | −0.362, −0.327 |
|
| |||||
| Multiplicative | −0.235 | 0.021 | −0.276, −0.194 | 0.0564 | −0.250, −0.222 |
|
| |||||
| Linear Index | −0.065 | 0.019 | −0.102, −0.029 | 0.0049 | −0.079, −0.055 |
|
| |||||
| Adjusted decrement | −0.095 | 0.022 | −0.138, −0.051 | 0.0101 | −0.112, −0.083 |
95% confidence interval includes zero.
SD=standard deviation; CI=confidence interval; IQR=interquartile range.
Figure 2.
Bias density graphs across joint health state utility estimators
Bias = estimated utility minus observed utility, using bootstrapped estimator distribution. Zero bias indicates more accurate estimator. Negative bias indicates the estimator underestimated the observed utility; positive bias indicates the estimator overestimated the observed joint utility.
Discussion
In our dataset, the utility of combination health states describing polysubstance use and opioid use disorder in conjunction with common co-occurring conditions followed no clear pattern relative to their constituent single states: they were evaluated at higher, lower, in between and of equal utility to the single states. Of the available joint health state utility estimators, the minimum estimator performed the best across the entire group, showing bias that was statistically non-significantly different from zero for all four combination states. Other estimators performed better than the minimum estimator in some of our joint health states, but none had its consistent lack of statistically significant bias. The additive and multiplicative joint utility estimators performed consistently worst of those available, showing bias for all four states.
Utility estimation can be time-consuming and complex.7 It is helpful for both users and consumers of utilities to have estimation methods that are transparent and accessible. The volume of health states describing individually-occurring conditions is vast, and when co-occurring conditions are added the number increases exponentially. Utility estimation for all such states is untenable, so methods to arrive at joint state utilities from their constituent single states are immensely useful to economic evaluation. Five methods of joint state utility estimation have been proposed in the literature, from simple addition to more complex models.9 Criteria for assessing their usefulness prioritize accuracy in prediction, and specifically minimizing bias, although psychological underpinnings have also been considered relevant.8 The literature to date is inconclusive about the recommended approach. A recent review recommended the multiplicative estimator9, although others have supported the minimum estimator10, a linear combination model11, and an adjusted decrement model.12 While most studies of joint state utilities focus on community-perspective values, as is recommended for use in economic evaluation14, the literature has assessed approaches using both indirect and direct utility elicitation methods, a range of diseases and conditions, a variety of definitions of what constitutes a joint health state, and multiple criteria for comparison across methods.9 We opted to collect community perspective utilities from a U.S. population sample to enable economic evaluation following recommended guidelines14, and used direct utility elicitation because of the practical difficulties of collecting indirect utility estimates from representative samples of active opioid users with or without co-occurring conditions. Our definition of joint utilities is context specific for substance use disorders: we identified individual health conditions that commonly occur together, and considered these joint states. Some investigators have used approaches similar to ours, such as in prostate cancer11, while others have considered two states that are simply recorded as prevalent together in population datasets (such as the Medical Expenditures Panel Survey12). The variability in conclusions about estimators’ usefulness may be due to these differences, which calls for context-specific use—meaning some estimators perform best in some disease contexts, and some measurement methods are better in other contexts.
The substance use disorder context provides an illustration of utility interaction that has implications for our results. Our joint states combined conditions commonly seen in substance use disorders that are genuinely co-occurring conditions but may also interact from a utility perspective. For example, prescription opioid misuse and chronic pain independently result in diminished utility, but when experienced together opioid misuse may improve the utility of chronic pain—because opioids diminish pain. Similarly, injection opioid use may temporarily offset diminished health utility from depression when experienced in combination while both conditions have utility decrements when experienced independently. In these situations, we find it plausible that the utility for either single state could in fact be worse than the utility for them together, as one may moderate the other. The maximum estimator could reasonably perform well for these joint states, disputing the assumption that joint states’ utilities must by definition be lower than either constituent single state (which some have termed “logically inconsistent”22).
Opioid misuse may be unique in that opioids when properly used can increase utility by mitigating pain. Misuse is accompanied by deterioration in quality of life and therefore a utility decrement. But in combination with other conditions such as back pain or depression as we studied, there are multiple effects at play: opioid misuse decreases utility, as does pain and depression, but the co-occurrence may mitigate effects. Our combination states of opioid misuse and these conditions had utilities in one case between the two individual states’ utilities and in the other the same as one of the two. We speculate that there was a mitigation effect occurring in these joint states that ameliorated the negative quality of life effect of the individual states. In contrast, our polysubstance use states including opioid misuse had combinations state utilities that were in one case below either single state and in the other case above both single state’s. The explanation of these polysubstance joint state utilities is unclear and requires further study.
It is important to note some limitations in our study. First, the SG is the gold standard for utility elicitation but has limitations—it is subject to respondent misunderstanding and as with all direct elicitation methods, is contingent on the accuracy and veracity of the hypothetical health states.7 We exerted great care and thoughtfulness in designing our health state descriptions to accurately reflect the experience of the individual and joint states, but they are simplifications of reality. Importantly, our joint states represent the interaction between opioid use and co-occurring conditions, such that pain with opioid misuse was experienced as less severe than pain in the absence of opioids, as would be expected in their simultaneous occurrence. We excluded about 11% of our data for invariance, which is a substantial but unremarkable rate for SG surveys.17 Second, we administered our survey on-line, which is known to produce different results from face-to-face administration for some direct utility elicitation methods.23 While in-person administration is ideal, on-line administration allowed us to access a national sample of respondents within our budget constraint, which is a strength of our study. It is unlikely that mode effects are different for individual and joint state utilities, so confining our analysis to comparisons of single and joint state utilities collected with one mode of administration may diminish the risk of bias in our results. That said, an ideal replication would employ different modes to compare results. Third, we combined data from two surveys. The second survey was administered, however, with attention to consistency to allow for precisely the analysis that was conducted. We attained some protection from bias by the surveys being identical except for the health states that were evaluated, the sample for each being randomly selected from the same panel (with duplicate respondents excluded), and the time between surveys being relatively short. Fourth, we collected utilities for only 4 joint health states within the SUD context, so the external validity of our results is limited. Finally, we used just two measures of performance for joint estimators—bias and RMSE—and did not attempt to reconcile differences between them when they arose or examine any patterns in respondent characteristics (or other variables) that may affect the performance of the estimators. Further research is warranted to extend our work in these areas—to additional joint states in SUD, to potential differences within populations that could be leveraged to improve estimation methods, and to further characteristics of estimators that would reveal optimal performance.
Conclusion
In the states we assessed the minimum estimator performed—well it was most often unbiased, providing the most accurate estimate of joint utility. We found no evidence to support the additive or multiplicative estimators as these performed worst of those available—they were most biased, providing the least accurate estimates of joint utility. Further research will advance our knowledge of combining single state utilities to understand co-occurring conditions and whether these results are unique to substance use disorders or to the states we assessed. The simplicity, transparency, and accessibility of the minimum estimator are compelling rationales to consider this approach when joint SUD utilities are not empirically available.
Supplementary Material
Acknowledgments
Financial support for this study was provided by a grant from the National Institute on Drug Abuse, R01DA033424. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report. The results are solely those of the authors and do not represent the official views of the National Institutes of Health or the National Institute on Drug Abuse.
We gratefully acknowledge research assistance provided by Adrianna Saada, MPH, Jared Leff, MS, and Ashley Eggman, MS. We thank David Fiellin, MD and Alain Litwin, MD, MPH, for providing input on the health state descriptions.
Footnotes
Disclosures: The authors have no competing interests to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ford ES, Croft JB, Posner SF, Goodman RA, Giles WH. Co-occurrence of leading lifestyle-related chronic conditions among adults in the United States, 2002–2009. Prev Chronic Dis. 2013;10:E60. doi: 10.5888/pcd10.120316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Prev Chronic Dis. 2014;11:E62. doi: 10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Medicare and Medicaid Services. Chronic Conditions among Medicare Beneficiaries, Chartbook, 2012. Baltimore, MD: 2012. [Google Scholar]
- 4.Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. Rockville, MD: 2015. [Google Scholar]
- 5.Drug Abuse and HIV: Research Report Series. National Institute on Drug Abuse; 2012. [Accessed March 2, 2016, 2016]. at https://www.drugabuse.gov/publications/research-reports/hivaids/ [Google Scholar]
- 6.Park H, Bloch M. The New York Times 2106. Jan 19, 2016. How the Epidemic of Drug Overdose Deaths Ripples Across America. [Google Scholar]
- 7.Hunink M, Weinstein MC, Wittenberg E, et al. Decision Making in Health and Medicine Integrating Evidence and Values. 2. Cambrigde, UK: Cambridge University Press; 2014. [Google Scholar]
- 8.Dale W. What is the best model for estimating joint health states utilities? Comparing the linear index model to the proportional decrement model. Med Decis Making. 2010;30:531–3. doi: 10.1177/0272989X10381896. [DOI] [PubMed] [Google Scholar]
- 9.Ara R, Wailoo AJ. Estimating health state utility values for joint health conditions: a conceptual review and critique of the current evidence. Med Decis Making. 2013;33:139–53. doi: 10.1177/0272989X12455461. [DOI] [PubMed] [Google Scholar]
- 10.Fu AZ, Kattan MW. Utilities should not be multiplied: evidence from the preference-based scores in the United States. Med Care. 2008;46:984–90. doi: 10.1097/MLR.0b013e3181791a9c. [DOI] [PubMed] [Google Scholar]
- 11.Basu A, Dale W, Elstein A, Meltzer D. A linear index for predicting joint health-states utilities from single health-states utilities. Health Econ. 2009;18:403–19. doi: 10.1002/hec.1373. [DOI] [PubMed] [Google Scholar]
- 12.Hu B, Fu AZ. Predicting utility for joint health states: a general framework and a new nonparametric estimator. Med Decis Making. 2010;30:E29–39. doi: 10.1177/0272989X10374508. [DOI] [PubMed] [Google Scholar]
- 13. [Accessed 8/25/15];GfK KnowledgePanel. at http://www.gfk.com/us/Solutions/consumer-panels/Pages/GfK-KnowledgePanel.aspx.
- 14.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost Effectiveness in Health and Medicine. New York, N Y: Oxford University Press; 1996. [Google Scholar]
- 15.Prosser LA, Grosse SD, Wittenberg E. Health utility elicitation: is there still a role for direct methods? Pharmacoeconomics. 2012;30:83–6. doi: 10.2165/11597720-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 16.XXXXX [blinded].
- 17.Wittenberg E, Prosser LA. Ordering errors, objections and invariance in utility survey responses: a framework for understanding who, why and what to do. Appl Health Econ Health Policy. 2011;9:225–41. doi: 10.2165/11590480-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 18.Llewellyn-Thomas HA. Health state descriptions. Purposes, issues, a proposal. Med Care. 1996;34:DS109–18. doi: 10.1097/00001648-199601001-00001. [DOI] [PubMed] [Google Scholar]
- 19.Connock M, Juarez-Garcia A, Jowett S, et al. Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation. Health Technol Assess. 2007;11:1–171. iii–iv. doi: 10.3310/hta11090. [DOI] [PubMed] [Google Scholar]
- 20.Redelmeier DA, Guyatt GH, Goldstein RS. Assessing the minimal important difference in symptoms: a comparison of two techniques. J Clin Epidemiol. 1996;49:1215–9. doi: 10.1016/s0895-4356(96)00206-5. [DOI] [PubMed] [Google Scholar]
- 21.Luo N, Johnson J, Coons SJ. Using instrument-defined health state transitions to estimate minimally important differences for four preference-based health-related quality of life instruments. Med Care. 2010;48:365–71. doi: 10.1097/mlr.0b013e3181c162a2. [DOI] [PubMed] [Google Scholar]
- 22.Dale W, Bilir SP, Hemmerich J, Basu A, Elstein A, Meltzer D. The prevalence, correlates, and impact of logically inconsistent preferences in utility assessments for joint health states in prostate cancer. Med Care. 2011;49:59–66. doi: 10.1097/MLR.0b013e3181f37bf2. [DOI] [PubMed] [Google Scholar]
- 23.Norman R, King MT, Clarke D, Viney R, Cronin P, Street D. Does mode of administration matter? Comparison of online and face-to-face administration of a time trade-off task. Qual Life Res. 2010;19:499–508. doi: 10.1007/s11136-010-9609-5. [DOI] [PubMed] [Google Scholar]
- 24.Annual estimates of the resident population by sex, age, race and Hispanic origin for the United States and States: April 1, 2010–July 1, 2015. [Accessed July 5, 2016];2015 at http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk.
- 25. [Accessed July 5, 2016];Educational Attainment 2010–2014. 2014 at http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_14_5YR_S1501&src=pt.
- 26. [Accessed July 5, 2016];Families and Living Arrangements, 2015. 2015 at http://www.census.gov/hhes/families/data/cps2015A.html.
- 27.Selected characteristics of households by total money income. [Accessed July 5, 2106];All Races, 2014. 2014 at http://www.census.gov/data/tables/time-series/demo/income-poverty/cps-hinc/hinc-01.html.
- 28.Employment status of the civilian population by age and sex, Table A-1. [Accessed July 5, 2016];Household data. 2015 May;2015 at http://www.bls.gov/news.release/empsit.t01.htm. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.