Abstract
Context
Most hip fracture care models are grounded in curative models where the goal is to return the patient to independent function. In many instances, however, hip fractures contribute to continued functional decline and mortality. While the negative impact of hip fractures is appreciated once they have occurred, what is less understood is what proportion of older adults have high illness burden prior to experiencing hip fracture and might benefit from geriatric palliative care.
Objectives
Using data from the Health and Retirement Study linked to Medicare claims (January 1992 through December 2010), we sought to understand the extent of premorbid illness burden prior to hip fracture.
Methods
Characteristics were based on the interview before hip fracture. Features used to indicate need for geriatric palliative care included evidence of functional and medical vulnerability, pain and depression.
Results
856 older adults who experienced a hip fracture were compared to 851 age, gender and race-matched controls. Older adults with hip fractures had significantly more premorbid functional vulnerability (ADL dependent 25.7% vs 16.1% (p<0.001); dementia 16.2% vs 7.3% (p<0.001); use of helpers 41.2% vs 28.7% (p<0.001)). They also experienced more medical vulnerability (multimorbidity 43% vs 29.8% (p<0.001); high healthcare utilization 30.0% vs 20.9% (p<0.001); and poor prognosis 36.1% vs 25.4% (p<0.001) in controls). There was no difference in premorbid pain and depression between subsequent hip fracture patients and controls.
CONCLUSION
A significant proportion of older adults have evidence of functional and medical vulnerability prior to hip fracture. For these individuals, integration of geriatric palliative care may be particularly important for optimizing quality of life and addressing the high morbidity experienced by this population.
Keywords: hip fracture, geriatric palliative care, multimorbidity
Introduction
Over 250,000 older adults sustain hip fractures annually in the United States (1). By 2030, the absolute number of hip fractures is expected to increase to close to 290,000 (2). Hip fracture management has been grounded within traditional curative and rehabilitation models of care in which the focus is on restoring patients to independent function. But, the mortality rate after hip fracture is very high, and most surviving patients do not return to independent functioning. A third of previously independent older adults are in institutionalized long term care settings a year after hip fracture and one-fifth die within one year (3,4).
Although a subset of older adults regains some level of function, an even smaller group returns to their previous level of functioning after hip fracture (5). Despite these findings, most hip fracture care models are predicated on the subset who recovers. While it is important to apply modern geriatric rehabilitation principles to older adults with hip fractures who desire and can benefit from them, there is also an imperative to address the psychosocial, physical and spiritual needs of those who not only might not recover, but may have had high illness burden even before the hip fracture.
Geriatrics utilizes an interdisciplinary approach to perform a comprehensive geriatric assessment, address the needs of older patients and their families across all settings, and identify the unique features of disease presentation, interactions between medications and safe medication prescribing. Palliative care focuses on improving quality of life for patients and families by providing an added layer of support through pain and symptom management, goals of care discussions, care coordination, and attention to psychosocial and spiritual concerns. (6). While most hospitals in the US have palliative care teams (7), they are not typically part of the management of patients with hip fracture---even though it is now recognized that palliative care is appropriate throughout the course of serious illness.
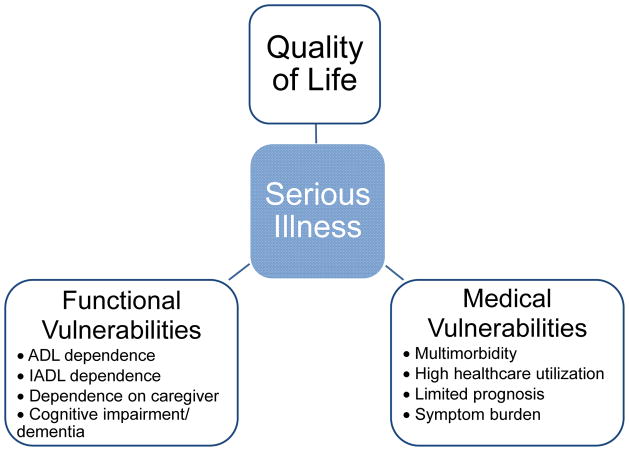
Geriatric palliative care “combines the principles and practice of geriatric medicine and palliative care; and focuses on comprehensive geriatric assessment; relief from pain and other symptoms; and management of physical and psychological problems, integrating social, spiritual, and environmental aspects of care (8).” Geriatric-palliative care integrates traditional geriatric assessment with holistic palliative care management to address both functional vulnerabilities brought on by disability, frailty and cognitive impairment and medical vulnerabilities brought on by multimorbidity and advanced illness. While not typically considered in the context of hip fractures, many components of geriatric palliative care may be appropriate for this population. Despite the substantial supportive needs that commonly ensue after hip fracture, comprehensive assessment, and targeted geriatric palliative care are not yet routine components of hip fracture management.
It could be argued that the need for geriatric palliative care might not be recognizable in persons with hip fracture until the post-operative and rehabilitative course have been completed. However, hip fractures typically occur in the oldest old, and hip fracture may occur in those who are frailer than even the typical older patient. For patients with multimorbidity or serious illness before their hip fracture, a model of care that attends to their geriatric palliative care needs after hip fracture may be particularly important to optimize quality of life and reduce suffering. The central hypothesis of this study was that a meaningful proportion of persons who experience hip fracture have substantial geriatric palliative care needs even before their hip fracture. Documenting these needs are important if we are to design better systems of care for vulnerable patients with hip fracture---and develop care plans for those who experience a catastrophic event against a background of pre-existing serious illness.
Methods
Participants were adults ≥ 65 between January 1992 and December 2010, who participated in the Health and Retirement Study. The Health and Retirement Study (HRS) is a nationally representative longitudinal community-based study of adults 50 years and older (9). Starting in 1992, HRS has subsequently conducted follow up surveys every two years. New community living participants are recruited every six years so that HRS remains representative of the US population. If a participant is not able to complete an interview, the interview is conducted with a proxy respondent.
Cases were participants older than 65 years who had a documented hip fracture while enrolled in HRS, ascertained by linking the HRS survey data to Medicare claims. Participants were identified as having a hip fracture event if one of the following two conditions was met: 1) the participant was admitted to a hospital with an admitting diagnosis ICD9 code for hip fracture “820.xx”; or 2) a surgeon’s charge for operative hip repair (CPT code 27230 – 27248) supported with either a) a second surgeon’s charge within 2 days or b) a supporting ICD9 procedure code for hip fracture surgery (ICD9 7855, 7905, 7915, 7925) (10,11,12). We excluded admissions which were considered late effects from a prior hip fracture, identified by ICD9 codes 733.81, 733.82, 905.3, V540-V549. Controls were matched on age, gender, race and year of interview.
Out of 25,146 HRS participants age 65 or older at any point between 1992 and 2010, 19,006 (76%) agreed to have their HRS surveys linked to the Medicare claims. We identified 1089 hip fracture events among those participants. Since we used Medicare claims to identify the presence of comorbid conditions prior to hip fracture event, we excluded hip fracture events that were not preceded by one continuous year of Medicare fee-for-service enrollment (72, 7%). Of the remaining 1017 hip fracture events, 161 (16%) had no HRS interview within 2.5 years before hip fracture event and were therefore excluded. This resulted in sample of 856 participants with hip fracture. For these participants, we used the HRS interviews to ascertain information about their socio-economic status, chronic conditions and functional status. For these 856 participants with hip fracture, we were able to identify 851 year-of-interview, age, gender and race-matched controls. For the matched control subjects, similar data were obtained from the interview conducted in the same year as the case patient.
Measures
We defined illness burden as being present when a patient was experiencing medical and functional vulnerabilities that likely would not resolve, could result in reduced quality of life and would benefit from geriatric palliative care (as defined earlier). Our model of illness burden emanating from functional and medical challenges is shown in Figure 1. To test our hypothesis that a meaningful subset of persons with hip fracture suffer from illness burden before hip fracture, we considered two domains of illness burden: functional vulnerability (dependence in activities of daily living (ADL), presence of dementia, need for helpers), and medical vulnerability (multimorbidity, symptom burden, high health care utilization and limited prognosis). Characteristics used to describe the population prior to hip fracture were based on the interview before hip fracture (mean 13 months, range 0–30 months). Activities of daily living (ADL) were ascertained by asking subjects if they had difficulty performing 5 ADLs (bathing, transferring, dressing, eating, toileting, and walking), or if they needed the help of another person to perform the ADLs. Subjects were classified as doing all ADLs without difficulty, having difficulty with one or more ADLs, but not needing help, or needing help with ADLs. “Need for helpers” was defined by the use of caregivers providing assistance with ADL and IADLs one or more hours per week. Dementia was defined by ICD-9 codes of 290.xx.
Figure 1.
Model of Serious Illness
We used the Charlson comorbidity score of >2 to characterize multimorbidity (13). Symptom burden was determined by the presence of pain (noted by an affirmative response to the presence of moderate or severe pain) or depression (CESD > 3). High healthcare utilization were defined as those who had two or more ED/Hospitalizations or 10 or more outpatient visits in last 12 months as identified in Medicare claims from the inpatient and outpatient files. We defined limited prognosis from the Lee index using a score of ≥13 (14). We created a summative score of illness burden giving one point to each domain of serious illness and illness burden likely to give rise to palliative and supportive care needs with the exception of symptom burden (excluded due to large number of missing data).
Statistical Analysis
We calculated the descriptive statistics for both cases with hip fracture event and matched controls. The differences between the two groups were evaluated using chi square tests. The analyses were weighted to account for the differential probability of subject selection and complex design of the HRS. Statistical analysis were done using Stata software, version 12 (StataCorp, College Station, Texas) and SAS software, version 9.3 (SAS institute, Cary, North Carolina).
The institutional review board at the University of California, San Francisco, approved this study.
Results
856 older adults (mean age 82.1 ± 7.4; 76.9 % women) who experienced a hip fracture were compared to 851 age, gender and race-matched controls. Across a diverse range of measures, persons with hip fracture had high levels of illness burden before their hip fracture, levels that were considerably higher than control subjects of the same age and gender. Characteristics of older adults who experienced hip fractures and their matched controls are described in Table 1.
Table 1.
Functional and Medical Vulnerability of Hip Fracture Cohort Compared to Controls
| Characteristic (missing) | Hip Fracture | HRS Matched No Hip Fracture | |||
|---|---|---|---|---|---|
| N = 856 | N = 851 | p-value | |||
| N | % | N | % | ||
| Functional Vulnerability | |||||
| Overall ADL Dependency (7) | |||||
| No Difficulty | 484 | 56.9% | 588 | 69.3% | <0.001 |
| Difficulty in 1 or more, No Dependence | 149 | 17.4% | 122 | 14.6% | |
| Dependent in one | 98 | 10.4% | 55 | 6.3% | |
| Dependent in two or more | 120 | 15.3% | 84 | 9.8% | |
| Overall IADL Dependency (6) | |||||
| Difficulty in 1 or more IADLs | 475 | 56.2% | 374 | 42.4% | <0.001 |
| Presence of Dementia | |||||
| Yes | 133 | 16.2% | 65 | 7.3% | <0.001 |
| Number of Helpers Needed (4) | |||||
| 0 | 511 | 58.9% | 600 | 71.3% | <0.001 |
| 1 | 174 | 20.7% | 139 | 16.4% | |
| 2+ | 170 | 20.5% | 109 | 12.3% | |
| Medical Vulnerability | |||||
| Charlson Comorbidity Score | |||||
| >2 | 364 | 43.1% | 255 | 29.8% | <0.001 |
| Peripheral Vascular Disease | 146 | 17.0% | 69 | 8.1% | <0.001 |
| Cerebrovascular Disease | 218 | 25.4% | 142 | 16.7% | <0.001 |
| Heart Failure | 253 | 29.5% | 146 | 17.2% | <0.001 |
| COPDc | 289 | 33.7% | 154 | 18.1% | <0.001 |
| Chronic Renal Failure | 105 | 12.3% | 28 | 3.3% | <0.001 |
| High Utilization a | |||||
| Yes | 255 | 30.0% | 179 | 20.9% | <0.001 |
| Lee Index b | |||||
| Lee≥13 | 308 | 36.1% | 222 | 25.4% | <0.001 |
| Symptom Burden | |||||
| Presence of Pain (232) | |||||
| No or Mild Pain | 542 | 73.7% | 559 | 75.9% | 0.2898 |
| Moderate or Severe Pain | 197 | 26.3% | 177 | 24.1% | |
| No, Mild or Moderate Pain | 687 | 92.8% | 685 | 93.8% | 0.3761 |
| Severe Pain | 52 | 7.2% | 51 | 6.2% | |
| Depression (255) | |||||
| Yes (CESD>3) | 232 | 33.0% | 225 | 29.1% | 0.2287 |
High utilization= ≥ED/Hospitalizations or 10+ outpatient visits in last 12 mo.
Lee Index signifies limited prognosis
Chronic Obstructive Pulmonary Disease
Compared to matched controls, older adults at baseline had higher levels of functional vulnerability. Older adults with hip fractures had significantly more premorbid impairment in ADLs (25.7% dependent in 1 or more ADLs compared to 16.1%) and IADLs (56.2% with IADL difficulty vs. 42.4%). At baseline, 16.2% had dementia among those who experienced hip fracture compared to 7.3% among the controls. Those who experienced hip fractures also had a higher proportion who received help from 1–2 helpers (41.2% vs 28.7%).
Older adults who subsequently sustained hip fractures also had higher levels of medical vulnerability. Forty-three percent had a Charlson Comorbidity Score of greater than 2 (compared to 29.8% among controls). Likewise, those who experienced a hip fracture had higher rates of multimorbidity (especially vascular disease, heart failure, COPD, and chronic renal failure), health care utilization and risk for mortality. Almost one-third (30.0%) were high utilizers compared to one-fifth (20.9%) among controls. A mortality risk index score of ≥ 13 was present in 36.1% of those who experienced hip fractures vs 25.4% in controls. Indication of illness burden was present in 61% in those with hip fracture compared to 40% in controls. Symptom burden (presence of pain or depression) was not significantly different between the two groups.
Discussion
Among a representative population of older adults we showed that those with hip fracture had higher illness burden (15,16). They were more likely to have ADL dependency and IADL difficulty and were more likely to have helpers. There was a two-fold higher rate of dementia and higher proportions of other serious illnesses like heart failure and COPD among those who subsequently suffered a hip fracture. These higher rates of morbidity likely intensified these older adults’ needs and overall healthcare use. Several other studies have demonstrated lower function among those who have hip fractures (17,18) but this is the first paper to comprehensively assess pre-fxr palliative needs grounded in a framework relevant for this very old population.
The implication of these findings is that a meaningful subset of older adults has comorbidity, functional dependency, and high risk for mortality prior to their hip fracture. These individuals likely have some degree of illness burden and have supportive and palliative care needs. This subset of older adults would benefit from geriatric palliative care services as an additional part of their care during their hip fracture admission.
Geriatric palliative care incorporates both the principles of geriatrics and palliative care, utilizing both traditional aspects of comprehensive geriatric assessment and thoughtful attention to patient/family goals and illness burden. For these patients, many of whom already have a broad array of concerns, the addition of a catastrophic injury will create major additional needs in the short term and probably in the long term. For these patients, care plans cannot just focus on the orthopedic injury but must also consider the enormous supportive needs of these patients in the short and long run.
Historically, older adults who experience hip fractures received care that was grounded solely in a curative and rehabilitative approach. More recently, orthogeriatric models of care have been advocated (19,20,21). This approach involves the routine performance of comprehensive geriatric assessment and care in a specialized orthogeriatric unit. While this approach is appropriate for many, for those with high illness burden, a curative approach alone is unlikely to meet the needs of patients who have substantial supportive and palliative needs even before their hip fracture, and are likely to have accelerating needs after their hip fracture. The illness burden demonstrated in 60% of those who in the hip fracture cohort prior to their hip fracture suggests that well over half of those with hip fracture would benefit from geriatric palliative care along with concurrent rehabilitative measures. A recent single-site randomized trial of comprehensive geriatric care which tested placement of hip fracture patients into a geriatric ward with structured assessment, management and discharge planning demonstrated improvement in mobility at 4 months, improved ADL scores and higher rates of discharge to home instead of to institutional care. The intervention had several components of geriatric palliative care including comprehensive geriatric assessment, attention to symptoms and psychosocial needs. However no mention was made of goals ascertainment, shared decision making, and care plan development in alignment with goals. Adoption of palliative care elements of geriatric palliative care into the orthogeriatric model would likely enhance this already promising approach to care. Specifically, integrating indications of distress along with symptom burden and ascertaining life goals and treatment preferences into the comprehensive geriatric assessment may provide an opportunity to identify those most in need of geriatric palliative care.
This study had three main limitations. The HRS relied on self-reported diagnosis and physical function that were not validated by objective measures. Cress et al. and others have shown self-perceived and performance-based measures are only moderately correlated with each other (22). Nevertheless, the Health Retirement Survey is one of only a few population-based studies that allow the assessment of illness burden prior to hip fracture. Additionally, because surveys in this longitudinal study occur every 2 years, specific functional status right before or after hip fracture is usually not captured. Finally, because health care utilization was captured from Medicare claims data, Medicare managed care patients (during the study period constituting 15% of patients with Medicare) were not included in this study.
Conclusion
Given the relatively high rates of illness burden, functional and medical vulnerability of those who subsequently experience a hip fracture, models of hip fracture care may benefit from systematically introducing elements of geriatric palliative care such as comprehensive geriatric assessment and goals ascertainment. Better assessment of premorbid functional and medial status would foster identification of palliative and supportive care needs and increase likelihood for referral and management.
Table 2.
Illness Burden in Hip Fracture Cohort Compared to Controls
| Hip Fracture | HRS Matched | ||||
|---|---|---|---|---|---|
| N = 856 | N = 851 | p-value | |||
| Characteristic (missing) | N | % | N | % | |
| Illness Burden a (7) | |||||
| 0 | 211 | 25% | 371 | 45% | <0.001 |
| 1 | 175 | 21% | 176 | 20% | |
| 2 | 168 | 19% | 110 | 14% | |
| 3 | 153 | 18% | 106 | 12% | |
| 4 | 91 | 11% | 47 | 5% | |
| 5 | 39 | 5% | 31 | 4% | |
| 6 | 14 | 2% | 8 | 1% | |
Summative score of illness burden giving one point for each domain of functional and medical vulnerability that creates palliative/supportive needs
Acknowledgments
Disclosures and Acknowledgments
This project was funded by the National Institute for Nursing Research (R01 NR013347). Dr. Ritchie was funded by a K07 Geriatric Academic Leadership Award from the National Institute on Aging (1K07AG31779-1A1) and Dr. Smith was funded by a K23 Beeson award from the National Institute on Aging (1K23AG040772) and the American Federation for Aging Research. Dr. Kelley was funded by a K23 Beeson award from the National Institute on Aging (1K23AG040774) and the American Federation for Aging Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Hospital Discharge Survey (NHDS), National Center for Health Statistics. [Accessed July 24, 2015]; Available from: http://205.207.175.93/hdi/ReportFolders/ReportFolders.aspx?IF_ActivePath=P,18.
- 2.Stevens JA, Rudd RA. The impact of decreasing U.S. hip fracture rates on future hip fracture estimates. Osteoporos Int. 2013;10:2725–2728. doi: 10.1007/s00198-013-2375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton JL. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50:1644–1650. doi: 10.1046/j.1532-5415.2002.50455.x. [DOI] [PubMed] [Google Scholar]
- 4.Farahmand BY, Michaelsson K, Ahlbom A, Ljunghall S, Baron JA Swedish Hip Fracture Study Group. Survival after Hip Fracture. Osteoporosis Int. 2005;16(12):1583–1590. doi: 10.1007/s00198-005-2024-z. [DOI] [PubMed] [Google Scholar]
- 5.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990;45(3):M101–M107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]
- 6.Center to Advance Palliative Care. [Accessed July 24, 2015];About palliative care. Available from: https://www.capc.org/about/palliative-care/
- 7. [Accessed July 27, 2015];Growth of Palliative Care in US Hospitals 2015 Snapshot (2000 – 2013) Available from: https://www.capc.org/media/filer_public/c5/af/c5afb02e-5e12-47f0-954a-ee23e55ea632/capc_growth_snapshot_2015.pdf.
- 8.Pautex S, Curiale V, Pfisterer M, et al. A common definition of geriatric palliative medicine. J Am Geriatr Soc. 2010;58(4):790–791. doi: 10.1111/j.1532-5415.2010.02791.x. [DOI] [PubMed] [Google Scholar]
- 9.Health and Retirement Study. [Accessed July 24, 2015];HRS data handbook. Available from: http://hrsonline.isr.umich.edu/index.php?p=dbook.
- 10.Fisher ES, Baron JA, Malenka DJ, et al. Hip fracture incidence and mortality in New England. Epidemiology. 1991;2(2):116–122. doi: 10.1097/00001648-199103000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Karagas MR, Baron JA, Barrett JA, Jacobsen SJ. Patterns of fracture among the United States elderly: geographic and fluoride effects. Ann Epidemiol. 1996;6(3):209–216. doi: 10.1016/1047-2797(96)00006-3. [DOI] [PubMed] [Google Scholar]
- 12.Karagas MR, Lu-Yao GL, Barrett JA, Beach ML, Baron JA. Heterogeneity of hip fracture: age, race, sex, and geographic patterns of femoral neck and trochanteric fractures among the US elderly. Am J Epidemiol. 1996;143(7):677–682. doi: 10.1093/oxfordjournals.aje.a008800. [DOI] [PubMed] [Google Scholar]
- 13.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 14.Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295(7):801–808. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- 15.Smith T, Pelpola K, Ball M, Ong A, Myint PK. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014;43(4):464–471. doi: 10.1093/ageing/afu065. [DOI] [PubMed] [Google Scholar]
- 16.Ranhoff AH, Holvik K, Martinsen MI, Domaas K, Solheim LF. Older hip fracture patients: three groups with different needs. BMC Geriatr. 2010:10–65. doi: 10.1186/1471-2318-10-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gonzalez-Zabaleta J, Pita-Fernandez S, Seoane-Pillado T, Lopez-Calvino B, Gonzalez-Zabaleta JL. Dependence for basic and instrumental activities of daily living after hip fractures. Arch Gerontol Geriatr. 2015;60(1):66–70. doi: 10.1016/j.archger.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 18.Seitz DP, Anderson GM, Austin PC, et al. Effects of impairment in activities of daily living on predicting mortality following hip fracture surgery in studies using administrative healthcare databases. BMC Geriatr. 2014:14–19. doi: 10.1186/1471-2318-14-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service—a literature review comparing different models. Osteoporos Int. 2010;21(4):S637–S646. doi: 10.1007/s00198-010-1396-x. [DOI] [PubMed] [Google Scholar]
- 20.Giusti A, Barone A, Razzano M, Pizzonia M, Pioli G. Optimal setting and care organization in the management of older adults with hip fracture. Eur J Phys Rehabil Med. 2011;47(2):281–296. [PubMed] [Google Scholar]
- 21.Sletvold O, Helbostad JL, Thingstad P, et al. Effect of in-hospital comprehensive geriatric assessment (CGA) in older people with hip fracture. The protocol of the Trondheim Hip Fracture Trial. BMC Geriatr. 2011:11–18. doi: 10.1186/1471-2318-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cress ME, Schechtman KB, Mulrow CD, et al. Relationship between physical performance and self-perceived physical function. J Am Geriatr Soc. 1995;43(2):93–101. doi: 10.1111/j.1532-5415.1995.tb06372.x. [DOI] [PubMed] [Google Scholar]