Abstract
Objectives
There is a paucity of research evaluating the risk tolerance of Emergency Department (ED) patients. We hypothesized that a significant percentage of ED patients surveyed would be comfortable with ≥5% risk of adverse outcome if they avoided testing in several hypothetical scenarios.
Materials and methods
This was a cross-sectional study of a convenience sample of stable inner-city ED patients. Patients completed a written survey and were asked four closed-answer questions regarding risk tolerance/willingness to refuse a test/procedure, including the following scenarios: #1: LP following CT head; #2 overnight serial troponins for rule out myocardial infarction; #3 CT for possible appendicitis, #4 parent deciding whether child should undergo head CT for low risk head injury. Risk preferences were stratified to ≥5% (high) and <5% (low). Multivariate logistic regressions performed for each scenario to control for confounding factors.
Results
There were 217 patients in the study group; mean age 42 ± 15 years, 48% female, 66% Hispanic, 87% income < $40,000 income group. A substantial percentage of patients rated high risk tolerance for each scenario, including 31% for #1 (avoid LP), 25% for #2 (avoid cardiac rule-out admission), 27% for #3 (avoid CT for appendicitis), and 19% for #4 (avoid head CT for child).
Discussion
For 3 of 4 scenarios, 25% or more of our patients would accept a high risk tolerance of adverse outcome to avoid further testing.
Conclusion
Our findings contribute further evidence to the growing body of literature supporting patient interest in shared decision making in the ED.
Keywords: Risk tolerance, Emergency department, Shared decision making
1. Introduction
Despite higher spending per capita, research suggests that the US does not provide its citizens with objectively better quality and access to health care.1 Kanzaria et al note that unnecessary testing and unwarranted hospital admissions are a reflection of physician risk intolerance that contributes to rising health care costs.2 Further, they contend that physicians are significantly influenced by fear of litigation when they order extensive testing for patients.
While there are a significant number of studies that focus on the risk tolerance of physicians, there is a paucity of information regarding the risk tolerance of patients, particularly with respect to care they receive in the emergency department (ED) setting.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 From the standpoint of autonomy, beneficence, and cost, it is important to understand whether physicians are ordering tests to reduce risk well beyond what patients might otherwise tolerate. We conducted a cross-sectional study to test the hypothesis that a significant percentage of patients surveyed in our ED would be comfortable with ≥ 5% risk of adverse outcome if they avoided testing within several hypothetical scenarios.
2. Materials and methods
2.1. Study design
This was a prospective, cross-sectional study of emergency department patients designed to assess their risk tolerance for adverse events, including death, when presented with 4 different common clinical scenarios in the ED.
2.2. Setting
The study was conducted in the Emergency Department at Christus Spohn Memorial Hospital (Corpus Christi, Texas, USA). The facility is a teaching affiliate of the Texas A&M Health Science Center, a level-two trauma center, and serves an inner-city population. The annual Emergency Department census is 45,000 patients. The study was reviewed and provided with exempt status by the Christus Spohn Institutional Review Board prior to initiation of patient enrollment.
2.3. Population
All consenting, medically stable, oriented, adult patients age >18 years were eligible for inclusion into the study group. Patients were excluded for any of the following reasons: cognitively impaired, medically unstable, or if they refused to provide verbal consent. Our ED census is represents a predominantly Hispanic, indigent, inner-city, population.
3. Study protocol
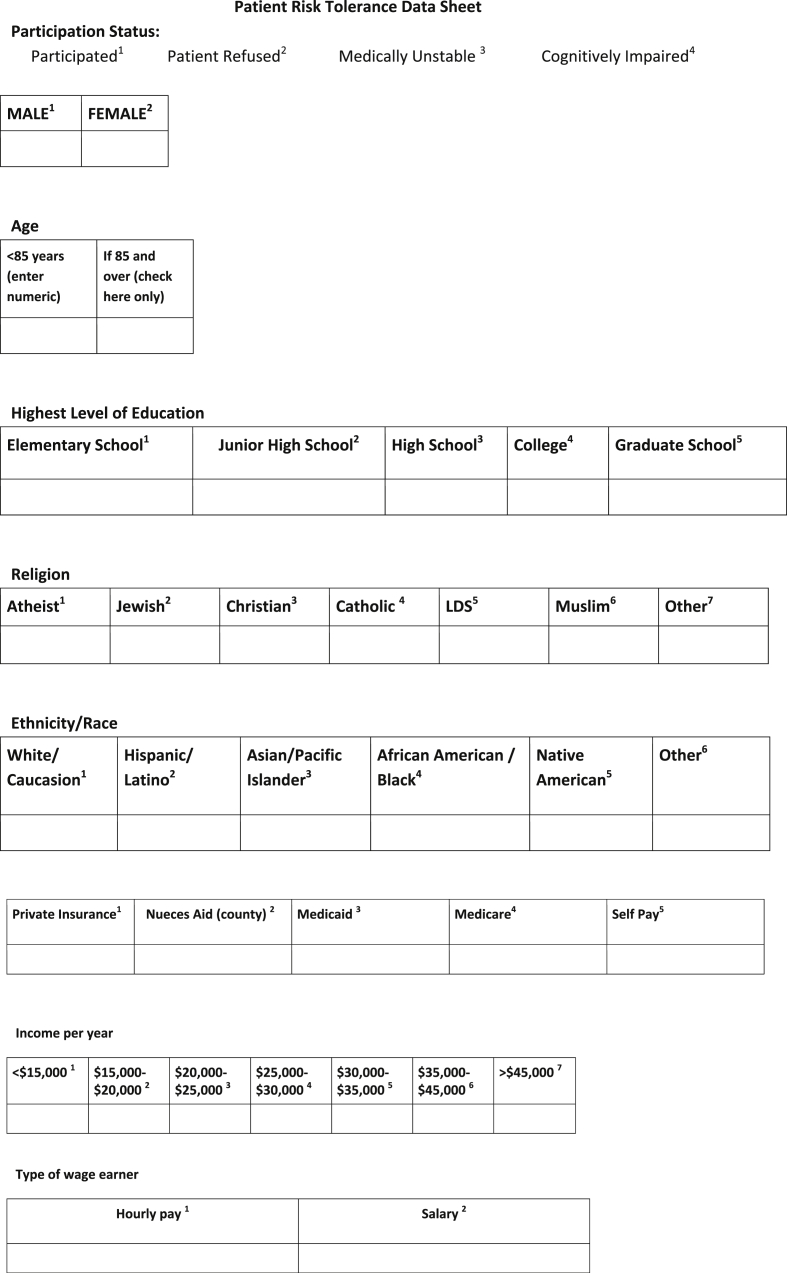
Consenting patients were consecutively enrolled at times when trained research associates were available to assist with the study protocol (convenience sample). Such hours were variable but did include normal business type hours, evenings, overnights, and weekends. Demographic/historical features were recorded on a structured form (Fig. 1). Among the variables collected, we asked patients to provide insurance information. In the U.S., while many patients have private insurance, government sponsored insurance is made available to the poor (Medicaid) and to the elderly (Medicare). We provided a written survey in English to the patients that included 4 common clinical scenarios of ED patients who were undergoing evaluation for chief complaints in which the differential diagnosis included conditions with high rates of morbidity/mortality for missed diagnosis. Patients filled out their survey responses in writing. The survey instrument was developed by the senior investigator who has extensive experience in the design of emergency medicine-based survey instruments.
Fig. 1.
Survey instrument.
The scenarios then revealed detailed descriptions of each potential step in management, including tests and procedures (see Appendix 1). The risks and benefits of those were related as well. Finally, each scenario detailed potential adverse outcomes if tests/procedures were refused. Scenario #1 was in the setting of the patient with headache and possible SAH with indeterminate head CT necessitating lumbar puncture Scenario #2 involved chest pain, use of serial cardiac enzyme assays, and subsequent stress testing with hospital admission or observation Scenario #3 involved undifferentiated abdominal pain (posed as potential appendicitis) and recommended CT imaging for further diagnostic assurance The optional fourth scenario involved obtaining a head CT for a child after minor head trauma. The last scenario (#4) was listed as optional, because it has been our practical experience that patients in our setting are more likely to not participate if survey material is more lengthy.
3.1. Statistical analysis
Data was entered into STATA (College Station, TX) for analysis. Variables were coded in binary fashion (with dependent variables being high or low risk aversion). Risk preferences were stratified to ≥5% (high) and <5% (low) for each scenario. Multivariate logistic regression was utilized to control for confounding factors. We calculated odds ratios and 95% confidence intervals. The primary outcome parameter of the study was to test the null hypothesis that patients would not accept a high risk preference (≥5%) for each hypothetical clinical scenario.
4. Results
A total of 217 patients were in the final study group. Our ED population is relatively young, poor, and predominantly Hispanic. Their characteristics are summarized in Table 1.
Table 1.
Study group characteristics (N = 217).
| Mean age (years) | 42 ± 15 |
|---|---|
| % Female | 48% |
| % Hispanic | 66% |
| % Income < $40,000/annual | 87% |
Within the study group, 31% of patients rated high risk tolerance to avoid LP after negative CT in the evaluation for subarachnoid hemorrhage (scenario #1). For scenario #1, the results of multivariate logistic regression are summarized in Table 2. Individuals whose annual income was > $40,000/yr (OR 4.1; 95 CI 1.5–11.1) and those with Medicaid (OR 3.4; 95% CI 1.2–9.3) were more risk tolerant.
Table 2.
Scenario #1 Multivariate Regression (Refusal of lumbar puncture after negative CT).
| Characteristic | Odds ratio | 95% Confidence interval |
|---|---|---|
| % Female | 0.51 | 0.27–0.97 |
| Age ≥ 65 years | 1.26 | 0.37–4.2 |
| Hispanic race | 1.74 | 0.84–3.6 |
| Income > $40,000 | 4.1 | 1.51–11.1 |
| Education > high school | 0.60 | 0.30–1.21 |
| Insurance: Clinic Card | 1.55 | 0.52–4.6 |
| Insurance: Medicaid | 3.39 | 1.2–9.3 |
| Insurance: Medicare | 1.59 | 0.29–8.3 |
| Insurance: self-pay | 1.62 | 0.63–4.2 |
Table 3 summarizes the results of multivariate logistic regression for scenario #2. We observed that 25% of patients rated high risk tolerance to avoid cardiac rule-out admission. Patients with Medicaid or who were self-pay were more likely to be risk tolerant (OR 4.2; 95% CI 1.4–12.4 and OR 3.3; 95% CI 1.2–9.0).
Table 3.
Scenario #2 Multivariate Regression (Refusal of cardiac “rule-out” testing, admission).
| Characteristic | Odds ratio | 95% Confidence interval |
|---|---|---|
| % Female | 0.76 | 0.41–1.4 |
| Age ≥ 65 years | 1.26 | 0.39–4.0 |
| Hispanic race | 1.35 | 0.64–2.85 |
| Income > $40,000 | 2.04 | 0.76–5.44 |
| Education > high school | 0.76 | 0.39–1.5 |
| Insurance: Clinic Card | 1.80 | 0.55–5.9 |
| Insurance: Medicaid | 4.2 | 1.4–12.5 |
| Insurance: Medicare | 1.2 | 0.18–8.5 |
| Insurance: self-pay | 3.3 | 1.2–9.0 |
For scenario #3 the results of multivariate logistic regression are summarized in Table 4. We found that 27% of patients rated high risk tolerance to avoid CT for appendicitis. When analyzing patient characteristics and their relationship to risk high risk tolerance, Hispanics were more likely to accept such risk (OR 2.9; 95% CI 1.2–6.5).
Table 4.
Scenario #3 Multivariate Regression (CT to evaluate for possible appendicitis).
| Characteristic | Odds ratio | 95% Confidence interval |
|---|---|---|
| % Female | 0.84 | 0.45–1.6 |
| Age ≥ 65 years | 1.1 | 0.30–4.2 |
| Hispanic race | 2.9 | 1.3–6.5 |
| Income > $40,000 | 1.3 | 0.47–3.7 |
| Education > high school | 0.74 | 0.38–1.4 |
| Insurance: Clinic Card | 1.4 | 0.49–4.1 |
| Insurance: Medicaid | 1.3 | 0.50–3.5 |
| Insurance: Medicare | 0.26 | 0.026–2.7 |
| Insurance: self-pay | 0.90 | 0.35–2.3 |
Finally, for the optional scenario #4, which was answered by a portion of our overall study group (n = 159), 19% of patients rated high risk tolerance to have their child avoid head CT. For scenario #4 the results of multivariate logistic regression are summarized in Table 5. There were no significant associations with this risk tolerance and the independent variables.
Table 5.
Scenario #4 Multivariate Regression (Parent refusal of CT head to evaluate minor head trauma for child).
| Characteristic | Odds ratio | 95% Confidence interval |
|---|---|---|
| % Female | 0.99 | 0.46–2.1 |
| Age ≥ 65 years | 1.1 | 0.17–6.6 |
| Hispanic race | 1.3 | 0.48–3.4 |
| Income > $40,000 | 1.2 | 0.32–4.5 |
| Education > high school | 1.6 | 0.68–3.8 |
| Insurance: Clinic Card | 2.4 | 0.60–10 |
| Insurance: Medicaid | 3.3 | 0.90–12.4 |
| Insurance: Medicare | 0.57 | 0.05–6.3 |
| Insurance: self-pay | 2.0 | 0.5 8–7.2 |
5. Discussion
With advancing medical research and the widespread availability of highly sensitive imaging modalities, physicians are increasingly able to reduce the chance of missed diagnosis for serious conditions. While physicians employ more of these tests to reduce the risk of adverse events, these strategies are contributing to higher health care costs.2 There have been numerous studies that have examined the risk related behavior of physicians.2, 3, 4, 5, 6, 7, 8
The majority of investigations specific to emergency physician decision making have confirmed the influence of malpractice and fear of uncertainty on test ordering. Wong et al surveyed 246 Michigan-based board eligible/certified emergency physicians and found that in one of two hypothetical clinical scenarios there was an association between physician fear of malpractice and increased ordering of a head CT for Pediatric minor trauma.7 Katz et al studied the influence of emergency physician fear of malpractice on their management of patients with possible cardiac ischemic in two academic settings.6 They reported that malpractice fear was associated with a higher admission rate as well as increased use of diagnostic tests such as Troponin. In a similar fashion, Kanzaria et al found that 97% of the 435 emergency physicians they surveyed routinely ordered medically unnecessary imaging for fear of missing a low-probability diagnosis or fear of litigation.2
By way of contrast, Pines et al explored more deeply into the risk related behavior of emergency physicians by breaking the concept into several components, including malpractice fear, risk taking, and stress from uncertainty as measured by distinct scales. Their study involved the evaluation of 2871 ED patients with chest pain that were evaluated by any one of 31 emergency physicians. The authors found that the decision by physicians to utilize coronary CT angiography, order cardiac markers and admit patients was influenced most strongly by risk aversion rather than fear of malpractice and stress from uncertainty.
Several studies have examined a patient's tolerance for risk related to medical treatment,9, 10, 11, 12, 13 but less so as it relates to treatment in the emergency setting. In a pilot study, Brown et al evaluated the risk tolerance for adverse events for 68 patients with chest pain. The median acceptable threshold for adverse event was 6.5%10 This threshold is relatively consistent with our definition of 5% as the cut-off for high risk in the current study. Subsequently, Chen et al conducted a cross-sectional study of 213 patients assess emergency department (ED) patients' risk thresholds for preferring admission versus discharge when presenting with chest pain.13 The authors found that approximately one-quarter of patients reported their risk tolerance threshold inconsistently depending on whether the provider gave a numeric assessment of risk versus showing the patient a visual aid to define the risk.
Our ED-based study is novel in its attempt to assess risk tolerance for several different clinical scenarios. Within our study group, we found that at least 19% of patients in each of the respective 4 scenarios were in the high risk tolerant group. For 3 of the 4 scenarios, > 25% of patients were in the high risk tolerance group. These findings suggest some overall stability in risk preference for ED patients across different clinical scenarios. Recent multi-center investigation has shown that shared decision making between physicians and patients can significantly reduce the use of cardiac testing (stress test and coronary CT) when applied within the emergency department setting. Our results present opportunities to expand research on shared decision making to such areas as LP following negative CT in the work-up of subarachnoid hemorrhage, CT for patients with abdominal pain but relatively low suspicion for acute appendicitis, and CT imaging for pediatric head injury. Further study is warranted to confirm that the views of our patients would be similar to those who are actually confronted with point-of-care decision making for these symptoms.
5.1. Limitations and future directions
This study has several limitations that warrant discussion. Due to logistical constraints, we did not track potential participant refusals. Our trained research associates work variable hours and days/nights of the week such that the study group demographics are representative of the low-income, predominantly Hispanic population to which the ED serves and consistent with previous data collected at our center. While the authors took great effort in the construction of each written scenario to help patients understand the clinical implications of testing and the risk of refusal, the questions didn't necessarily correlate with the purpose of each respective patient visit to the ED that day. It may have been difficult for patients to relate to the hypothetical clinical scenario in the context of a different current symptom. Thus, we cannot be certain that patients would make the same choices if they were confronted with the similar scenarios under real circumstances.
In addition, as the survey instrument utilized here has not been previously validated, it is possible that wording of the scenarios and/or the survey questions might have also led to a different result. Along the same lines, our decision to define high risk tolerance as greater than 5% is somewhat arbitrary, though consistent with the tolerance of adverse outcome noted by Brown et al for chest pain patients (6.5%)10 With most emergency physicians seeing several thousand patients per year, it is hard to imagine that many would hold their “acceptable miss rate” at 50 per thousand patients seen. It is also uncertain how our results might have varied had we utilized a continuous scale for risk tolerance ranking. Patients may also have responded differently based on the degree of pain that they were respectively experiencing at the end of an encounter, but we did not provide information nor control for this possibility in our data collection/analysis. We also note that some of our demographic variables are collinear (e.g education and income level), but this is a common problem for this type of research and, nonetheless, researchers typically include these variables to control for confounding in a multivariate regression. Future investigators should also conduct larger studies to better understand the degree of significance of the independent variable associations with higher risk tolerance.
Finally, another limitation of our study is related to the educational level, which may influence their ability to understand the term “risk” and the associated short and long term complications associated with a missed diagnoses. The fact that our patients provided a level of risk tolerance does not provide us with any information regarding their comprehension. Our results may also not be generalizable to a more educated and/or wealthier population who surely would understand the scenarios and implications of risk taking in a more sophisticated fashion. Future studies should be conducted to examine this question in other diverse settings, and to examine whether physician risk tolerance would increase if they were more aware of their patients' own tolerance for risk.
6. Conclusions
For 3 of 4 scenarios, 25% or more of our patients would accept a high risk tolerance of adverse outcome to avoid further testing. If future studies validate our findings in other settings, there may be opportunities for physicians to engage patients in shared decision making when pre-test probability assessment is low.
Financial disclosures/conflicts
None.
Footnotes
Peer review under responsibility of The Emergency Medicine Association of Turkey.
Appendix 1. Scenarios
Scenario 1
You go to visit your doctor because you have a headache. After your doctor talks with you he or she decides that a head CT should be performed to look for a possible brain bleed. You decide to get the CT scan and the head CT does not show any evidence of bleeding. Now your doctor decides that a spinal tap should be performed to further rule out a brain bleed because a brain bleed may be present even though it cannot be seen with the head CT. Brain bleeds may progress rapidly and can lead to coma, permanent brain damage, require surgery, or even death. What level of risk of still having a brain bleed would you accept to avoid getting the spinal tap after getting the head CT? In other words what chance of still having a brain bleed would you be okay with if the spinal tap is not performed?
Lumbar puncture (Spinal tap)
A lumbar puncture is when a needle is stuck into your lower back so it can go through the lining that covers the nerves inside your spine. This is done to collect your spinal fluid which bathes your spinal cord and brain. The spinal fluid will be looked at to see if you have an infection or bleeding in your brain or spinal cord. Problems that can happen if you have a lumbar puncture are bleeding, infections, and nerve damage. Patients often say that the pain level from a lumbar puncture is low to medium.
| Treatment/procedure | <1% | 1% | 2% | 5% | 10% | 15% | Fill in blank % | Don't understand question 8 |
|---|---|---|---|---|---|---|---|---|
| Head CT |
Scenario 2
You come into the emergency department with chest pain. The tests that your doctor in the Emergency room ordered are not conclusive that your chest pain is caused by your heart. Your doctor determines that further testing should be done to examine your heart including a cardiac stress test and overnight observation or admission in the hospital. What level of risk of still having a heart attack in the next 6 months would you accept to avoid admission/observation to the hospital and cardiac stress test?
Cardiac stress test
A cardiac stress test is performed by stressing the heart. This may be achieved by injecting drugs into your blood or by exercising your body. After stressing the heart then radioactive fluid is injected into your blood and pictures are taken of your heart. This information may then be used by your doctor to determine how well your heart is functioning. Problems that can happen with the stress test include chest pain, shortness of breath, heart attack. If you experience any chest pain during the stress test then the test is immediately stopped.
| Treatment/procedure | <1% | 1% | 2% | 5% | 10% | 15% | Fill in blank % | Don't understand question 8 |
|---|---|---|---|---|---|---|---|---|
| Cardiac stress Test |
Scenario 3
You come into the emergency department because you are having abdominal (belly) pain. After reviewing your blood work, urine sample, x-rays, etc. the doctor is unable to determine the cause of your abdominal pain and decides to order a CT scan of your abdomen and pelvis. What level of risk of having a serious medical condition such as an appendicitis (which requires emergent surgery and if left untreated may lead to death) would you accept to avoid an abd/pelvic CT?
Abdominal and pelvic computed tomography (Abd/pelvic CT)
An abd/pelvic CT is an imaging study that uses a series of 100's of x-rays to view the organs and bones of the abdomen and pelvis. Patients are placed on a narrow table and slid in and out of the CT machine while the imaging is being performed. The imaging takes less than 20 min to perform. Patients are exposed to radiation during the imaging which increases your lifetime risk of developing cancer. The younger you are when you have the CT scan the greater the risk of developing cancer. The imaging produces no pain but people who are afraid of confined spaces may be uncomfortable. Your doctor may decide that IV contrast dye will be necessary to get the best images. The IV contrast dye is toxic to the kidneys and may cause damage to your kidneys or an allergic reaction.
Imaging may reveal bleeds, tumors, fractures, inflammation, etc.
| Treatment/procedure | <1% | 1% | 2% | 5% | 10% | 15% | Fill in blank % | Don't understand question 8 |
|---|---|---|---|---|---|---|---|---|
| Abd/pelvic CT |
Scenario 4 (optional)
You bring your child into the emergency department after your child has suffered a minor head injury. Your child is now behaving normally. The doctor states that a Head CT can be performed now to look for a brain bleed or that you can take your child home and bring him/her back for further evaluation if they begin acting abnormally. Brain bleeds may progress rapidly and can lead to coma, permanent brain damage, require surgery, or even death. What level of risk of still having a brain bleed would you accept to avoid getting the head CT for your child?
Head computed tomography (Head CT)
A Head CT is an imaging study that uses a series of 100's of x-rays to view the skull and its contents. Patients are placed on a narrow table and slid in and out of the CT machine while the imaging is being performed. The imaging takes less than 10 min to perform. Patients are exposed to radiation during the imaging which increases your lifetime risk of developing cancer. The younger you are when you have the CT scan the greater the risk of developing cancer. The imaging produces no pain but people who are afraid of confined spaces may be uncomfortable. Your doctor may decide that IV contrast dye will be necessary to get the best images. The IV contrast dye is toxic to the kidneys and may cause damage to your kidneys or an allergic reaction. Imaging may reveal bleeds, tumors, fractures, inflammation, etc.
| Treatment/procedure | <1% | 1% | 2% | 5% | 10% | 15% | Fill in blank % | Don't understand question 8 |
|---|---|---|---|---|---|---|---|---|
| Head CT |
References
- 1.Angrisano C., Farrel D., Kocher B. McKinsey Global Institute; Jan 2007. Accounting for the cost of health care in the United States. [Google Scholar]
- 2.HK1 Kanzaria, Hoffman J.R., Probst M.A. Emergency physician perceptions of medically unnecessary advanced diagnostic imaging. Acad Emerg Med. 2015 Apr;22(4):390–398. doi: 10.1111/acem.12625. Epub 2015 Mar 23. [DOI] [PubMed] [Google Scholar]
- 3.Andruchow J.E., Raja A.S., Prevedello L.M. Variation in head computed tomography use for emergency department trauma patients and physician risk tolerance. Arch Intern Med. 2012;172(8):660–661. doi: 10.1001/archinternmed.2011.2243. [DOI] [PubMed] [Google Scholar]
- 4.Pines J.M., Isserman J.A., Szyld D. The effect of physician risk tolerance and the presence of an observation unit on decision making for ED patients with chest pain. Am J Emerg Med. 2010 Sep;28(7):771–779. doi: 10.1016/j.ajem.2009.03.019. Epub 2010 Feb 25. [DOI] [PubMed] [Google Scholar]
- 5.Pines J.M., Hollander J.E., Isserman J.A. The association between physician risk tolerance and imaging use in abdominal pain. Am J Emerg Med. 2009 Jun;27(5):552–557. doi: 10.1016/j.ajem.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 6.Katz D.A., Williams G.C., Brown R.L. Emergency physicians' fear of malpractice in evaluating patients with possible acute cardiac ischemia. Ann Emerg Med. 2005 Dec;46(6):525–533. doi: 10.1016/j.annemergmed.2005.04.016. Epub 2005 Jul 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong A.C., Kowalenko T., Roahen-Harrison S. A survey of emergency physicians' fear of malpractice and its association with the decision to order computed tomography scans for children with minor head trauma. Pediatr Emerg Care. 2011 Mar;27(3):182–185. doi: 10.1097/PEC.0b013e31820d64f7. [DOI] [PubMed] [Google Scholar]
- 8.Allen A.S., Orav E.J., Lee T.H. Clinician personality and the evaluation of higher-risk patient symptoms. J Patient Saf. 2011 Sep;7(3):122–126. doi: 10.1097/PTS.0b013e318223cb41. [DOI] [PubMed] [Google Scholar]
- 9.Johnson F.R., Ozdemir S., Mansfield C. Crohn's disease patients' risk-benefit preferences: serious adverse event risks versus treatment efficacy. Gastroenterology. 2007 Sep;133(3):769–779. doi: 10.1053/j.gastro.2007.04.075. [DOI] [PubMed] [Google Scholar]
- 10.Brown T.B., Cofield S.S., Iyer A. Assessment of risk tolerance for adverse events in emergency department chest pain patients: a pilot study. J Emerg Med. 2010 Aug;39(2):247–252. doi: 10.1016/j.jemermed.2009.03.026. [DOI] [PubMed] [Google Scholar]
- 11.Boutis K., Cogollo W., Fischer J. Parental knowledge of potential cancer risks from exposure to computed tomography. Pediatrics. 2013 Aug;132(2):305–311. doi: 10.1542/peds.2013-0378. Epub 2013 Jul 8. [DOI] [PubMed] [Google Scholar]
- 12.Johnson F.R., Ozdemir S., Mansfield C. Are adult patients more tolerant of treatment risks than parents of juvenile patients? Risk Anal. 2009 Jan;29(1):121–136. doi: 10.1111/j.1539-6924.2008.01135.x. Pub 2008 Sep 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen J.C., Cooper R.J., Lopez-O'Sullivan A. Measuring patient tolerance for future adverse events in low-risk emergency department chest pain patients. Ann Emerg Med. 2014 Aug;64(2):127–136. doi: 10.1016/j.annemergmed.2013.12.025. 136.e1-3 Epub 2014 Feb 13. [DOI] [PubMed] [Google Scholar]