Abstract
BACKGROUND/OBJECTIVES
To perform an economic evaluation of a primary care-based physical activity counseling intervention that improved physical activity levels and rapid gait speed in older veterans.
DESIGN
Secondary objective of randomized trial that assessed the effect of exercise counseling (relative to usual care) on physical performance, physical activity, function, disability and medical resource use and cost.
SETTING
Veterans Affairs Medical Center, Durham, North Carolina.
PARTICIPANTS
Male veterans aged ≥ 70 years (n=398).
INTERVENTION
An experienced health counselor provided baseline in-person exercise counseling, followed by telephone counseling at 2, 4, and 6 weeks, and monthly thereafter through one year. Each participant’s primary care physician provided initial endorsement of the intervention, followed by monthly automated telephone messages tailored to the patient. Individualized progress reports were mailed quarterly.
MEASUREMENTS
Intervention costs were assessed. Health care resource use and costs were estimated from enrollment through one year follow-up. The incremental cost of achieving clinically significant changes in major trial endpoints was calculated.
RESULTS
The total direct cost of the intervention per participant was $459, 85% of which was counselor effort. With overhead, program cost totaled $696 per participant. Medical costs during follow-up reached $10,418 with the intervention, versus $12,052 with usual care (difference = −$1,634 (95% confidence interval=−$4,683 to $1,416; p=0.29)). Expressed in terms of short-term clinical outcomes, the intervention cost $4,971 per additional patient reaching target exercise levels, or $4,640 per patient achieving a clinically significant change in rapid gait speed.
CONCLUSION
Improvements in physical activity and rapid gait speed in the physical activity counseling group were obtained at a cost that represents a small fraction of patients’ annual health care costs.
Keywords: physical activity, cost, counseling, randomized clinical trial
INTRODUCTION
Physical inactivity is associated with elevated risks of chronic disease, disability and mortality and has been recognized by national and international health agencies alike as an important contributor to public health.1-3 Nevertheless, 44% of young adults in the U.S. are insufficiently active, and by the seventh decade of life 70% of adults have too sedentary a lifestyle according to established guidelines.4,5 While best initiated early in life, engaging in regular physical activity can be beneficial at any age. Older adults, including frail elderly and those over 75 years of age, have improved their functional status, mobility and well-being through adoption of habitual physical activity6-10 However, successfully engaging adults of any age in regular, consistent physical activity can be challenging, and older individuals may face obstacles that make participation even less likely, such as inability to travel to centers with supervised programs, health concerns related to unsupervised physical activity and lack of knowledge regarding appropriate exercise activities.
Physical activity programs that are initiated in the primary care setting and offer expertise and support at regular intervals by phone and other media may provide a necessary bridge for successful home-based exercise. The Veterans Learning to Improve Fitness and Function in Elders (VA-LIFE) trial found that a multicomponent physical activity counseling (PAC) intervention that began in the primary care setting and was delivered over time through telephone and mail follow-up improved physical activity and rapid gait speed in a population of elderly, physically inactive veterans.11 While promising, adoption of the intervention in clinical settings may depend on its cost and value relative to competing health care programs. To shed light on these issues, we performed an economic evaluation as part of VA-LIFE. Specifically, we assessed the cost of the intervention itself (excluding research-related costs), explored whether intervention costs were offset by differences in health care resource use and cost in the PAC group relative to usual care, and estimated the incremental cost of achieving observed gains in physical activity and gait speed.
METHODS
Overview of VA-LIFE Design and Results
Patients at least 70 years of age who were followed by a primary care physician at the Durham Veterans Affairs Medical Center (VAMC) were eligible for the study if they were physically inactive, could walk 30 feet without human assistance and did not meet exclusion criteria (terminal diagnosis, conditions precluding increased activity, dementia or severe loss of vision or hearing).11 Patients’ primary care providers confirmed their eligibility prior to recruitment. Between July 2004 and March 2006, 398 male patients were randomized to either the PAC intervention or usual care. The intervention included a baseline face-to-face structured exercise counseling session with an experienced health counselor, followed by structured telephone sessions with the counselor at 2, 4, and 6 weeks, and monthly thereafter through 12 months. In addition, patients’ primary care providers endorsed the intervention at their first clinic visit after enrollment and in monthly automated telephone messages personalized to each patient. Target activity levels included a minimum of 30 minutes of walking or lower extremity physical activity at least 5 days per week and 15 minutes of lower extremity strength training three days per week. Individualized progress reports were mailed to participants quarterly. The Durham VAMC institutional review board approved the VA-LIFE protocol, and written consent was obtained from all patients.
At one year follow-up, the frequency and duration of weekly physical activity improved significantly more in the intervention group than with usual care.11 This increased activity with PAC was accompanied by a significant and clinically meaningful improvement in rapid gait speed and an insignificant positive differential in usual gait speed relative to usual care. Self-reported physical function and disability were not appreciably affected. Measures of quality of life were not collected.
Economic Evaluation
(i) Intervention Costs
Counselor effort was the primary intervention expense. Time spent with patients in baseline and follow-up counseling sessions was recorded prospectively by the counselor. To estimate counselor time devoted to intervention activities other than counseling sessions, work sampling was performed at the midpoint of the study for three weeks.12 Work activity was recorded by the counselor in response to random reminders generated at a rate of 5 per hour using a Divilbiss JD-8 random sampler. Response categories reflected the primary intervention activities of the counselor (baseline counseling, call preparation, follow-up calls, and consults with clinicians) as well as non-intervention activities. Effort associated with research activities, such as chart reviews performed as part of screening potential participants, was excluded. Counselor time was valued using 2014 VAMC salary schedules at a level consistent with the counselor’s experience in delivering exercise interventions. The average time spent endorsing exercise by primary care physicians during clinic visits was reported by physicians in a questionnaire completed midway through the study. Physician time was converted to costs using representative VAMC 2014 salaries (midpoint of non-manager primary care specialty range). Salaries were supplemented with fringe benefits at rate of 36%. Other project expenses (development of automated calls, printing of National Institute of Aging exercise workbooks and poster illustrating leg strengthening exercises, and equipment purchases (elastic resistance bands, pedometers)) were based on project expense records, and updated to 2014 dollars using appropriate price indices.13 Overhead cost was estimated based on indirect costs for outpatient clinics reported in the Veterans Affairs Decision Support System National Extract.14
(ii) Health Care Costs During Follow-up
The cost of inpatient and observation stays, emergency room visits, outpatient clinic visits and medications received in the Veterans Affairs (VA) health care system was obtained from the VA Decision Support System National Extract files through one year of follow-up for all patients enrolled in the study.14 These files contain activity-based estimates of cost for health care encounters (including physician services). Hospitalizations at non-VA facilities were identified by the health counselor during follow-up calls. VA Medical Inpatient databases were used as a supplementary and confirmatory source for identifying institutional stays at VA facilities and non-VA admissions and emergency room visits paid for by the VA. Charges for non-VA encounters were extracted from Uniform Bills (UB-04) provided by hospitals and converted to costs using hospital and department specific cost-to-charge ratios obtained from hospitals’ annual Medicare Cost Reports.15 All hospital costs were updated to 2014 using the hospital component of the producer price index.13 Physician services delivered during non-VA hospitalizations, including daily hospital care and major procedures, were identified from information on billing forms and mapped to corresponding Current Procedural Terminology codes. National rates from the 2014 Medicare Fee Schedule were then applied.16
(iii) Analysis
Baseline demographic and clinical characteristics of patients were summarized by treatment group (mean and standard deviation for continuous variables and proportions for categorical variables). Intervention components, component costs and total intervention costs were summarized with means, with standard deviations for costs that varied among patients. Total health care costs, as well as cost subtotals by care type (inpatient, outpatient, emergency room visits without admission, pharmacy), were summarized by treatment group in three month intervals. Unadjusted one year resource use and costs were compared between treatments; proportions were compared using the Pearson chi-square test and continuous resource use and cost variables were compared using the normal approximation (two sample t-test).17 In supplementary analyses, the effects of patient characteristics on total costs were explored using generalized linear models, and effect of covariate adjustment on the magnitude and significance of estimated treatment effect was examined. The generalized linear model was specified with a log link that assumes a multiplicative influence of covariates on cost, and an inverse Gaussian distribution that assumes the residual variance is proportional to the cube of the mean. The inverse Gaussian distribution was chosen after inspecting deviance residual plots and results of the modified Park test.
Given VA-LIFE’s focus on intermediate clinical outcomes (i.e., gait speed, physical activity) measured over a short follow-up period, we did not perform a formal cost-effectiveness analysis, which would have required estimates of the intervention’s effect on life expectancy. To place the results in the context of other physical activity interventions, the incremental cost of achieving improvements in intermediate outcomes was calculated. Analyses were performed using SAS, versions 9.3 and 9.4 (SAS Institute, Cary, NC).
RESULTS
Baseline Characteristics and Activity Levels
VA-LIFE study participants were elderly male veterans, with a mean age of 77 years (range 70-92).11 Three quarters were white, and about half completed some post-secondary education. Three quarters were eligible for VA health care without copays. The most prevalent chronic illnesses reported by patients were hypertension (74%), arthritis (67%), heart disease (48%), peripheral circulation problems (38%) and diabetes (34%). The most common patient-reported symptoms were shortness of breath with exertion (68%), balance problems (46%), numbness or tingling (44%), sleeping difficulties (34%) and anxiety, worry or tension (28%). As expected with successful randomization, baseline characteristics were well balanced between groups (Table 1). On average, patients spent an average of about an hour per week engaging in endurance or strengthening activities. Half reported doing neither activity.
Table 1.
Baseline Characteristicsa
| PAC | Usual Care | |
|---|---|---|
| (n=199) | (n=199) | |
| Age (mean (SD)) | 77.7 (5) | 77.4 (5) |
| White | 76 | 79 |
| Education | ||
| ≤ High school | 46 | 46 |
| Some college, technical/trade school | 28 | 26 |
| College graduate | 26 | 28 |
| Enrollment Priority | ||
| Service-connected or disabled (priorities 1-4) | 30 | 43 |
| Below means test threshold or receiving VA pension, Medicaid | 46 | 34 |
| or other specified VA compensation (priorities 5-6) | ||
| Copay requirements, above means test threshold (priorities 7-8) | 24 | 23 |
| Self-Reported Clinical History | ||
| High blood pressure | 74 | 74 |
| Arthritis | 63 | 71 |
| Heart disease | 46 | 49 |
| Circulation problems (arms or legs) | 38 | 39 |
| Diabetes | 34 | 35 |
| Sleep Problems | 29 | 33 |
| Stomach, intestinal or gall bladder problems | 20 | 21 |
| Cataracts | 40 | 40 |
| Cancer | 14 | 16 |
| Emphysema or chronic bronchitis | 10 | 16 |
| Joint Replacement | 11 | 13 |
| Effects of stroke | 10 | 8 |
| Chronic obstructive pulmonary disease | 6 | 8 |
| Renal Disease | 6 | 7 |
| Skin Disorders | 6 | 5 |
| Amputation | 6 | 2 |
| Epilepsy | 0.5 | 2 |
| Self-Reported Symptoms | ||
| Balance problems | 44 | 48 |
| Numbness or tingling anywhere in body | 41 | 47 |
| Dizzy or light-headed | 34 | 37 |
| Difficulty sleeping at night | 31 | 38 |
| Anxiety, worry or tension | 25 | 32 |
| Fear of falling | 26 | 25 |
| Feel sad, blue or depressed | 25 | 21 |
| Confused thinking | 19 | 19 |
| Shortness of breath with exertion | 64 | 72 |
| Chest pain/pressure with exertion | 17 | 19 |
| Shortness of breath at rest | 14 | 19 |
| Chest pain/pressure at rest | 10 | 11 |
Percent unless otherwise indicated. PAC=physical activity counseling.
Intervention Cost
(i) Counselor Effort
The primary intervention component was health counselor time. All patients received baseline counseling, which lasted 49 minutes on average and cost an average of $40. (Table 2). All fourteen follow-up calls were completed for 183 patients (92%). Total call time per patient during follow-up averaged 248 minutes, with a mean cost of $198. Follow-up sessions decreased in length over time, from an average of 26 minutes initially to 16 minutes during the second half of follow-up.
Table 2.
Cost of Intervention Components
| Mean (SD) | |
|---|---|
| Baseline | |
| Counselor effort | |
| Initial counseling session | |
| Minutes | 49.4 (13) |
| Direct call cost ($) | 39.50 (10) |
| Cost of othera counselor effort ($) | 25.25 (7) |
| Total baseline counselor cost ($) | 64.75 (17) |
| Other baseline costs ($) | |
| Physician clinic endorsement | 5.03 |
| Supplies | 35.09 |
| Total baseline ($) | 104.87 (17) |
| Follow-up | |
| Counselor effort | |
| Follow-up calls | |
| Number | 13.4 (2) |
| Minutes | 248.0 (89) |
| Direct call cost ($) | 198.27 (71) |
| Cost of othera counselor effort ($) | 126.77 (46) |
| Total follow-up counselor cost ($) | 325.04 (117) |
| Other follow-up costs ($) | |
| Automated calls | |
| Call service contract | 19.99 |
| Recording of personalized physician message | 9.34 |
| Total follow-up cost ($) | 354.37 (117) |
| Total direct cost ($) | 459.24 (121) |
| Total cost (including overhead) ($) | 695.82 (184) |
Call preparation (including chart review) and consultation with primary care providers as needed. SD=standard deviation.
Time spent on the intervention by the health counselor that did not involve patient contact, such as call preparation and physician consultations, was estimated using work sampling midway through the study. Activities directly related to the intervention accounted for 86% of the counselor’s time, with the residual consumed by breaks and transitions. Most intervention time was spent in counseling sessions (70%), followed by call preparation (29%). Only 1% of counselor time involved clinician consults. Based on these data, we inflated the time spent in counseling sessions by a factor of 1.6 (1/(.86 × .70)) to capture the additional effort required to deliver the intervention, yielding a total of 488 minutes per patient (81 baseline and 407 follow-up minutes). This adjustment increased the cost of counselor effort from $238 to $390 ($65 baseline, $325 follow-up; Table 2).
(ii) Other Intervention Costs
Exercise endorsements were delivered in clinic to 180 patients and averaged 3 minutes in length; the cost of this additional physician time during the clinic visit was estimated to be $5 per patient enrolled. The automated call service cost $20 per patient, and the value of physician time spent recording personalized messages averaged $9 per patient. Exercise books, equipment and supplies totaled $35 per patient. Combining miscellaneous costs with counselor effort, total direct intervention costs averaged $459 per patient ($105 baseline, $354 follow-up; Table 2). Valuing overhead cost at 51% of direct cost (34% of total cost), one-year intervention cost totaled $696 per patient.
Health Care Resource Use and Cost
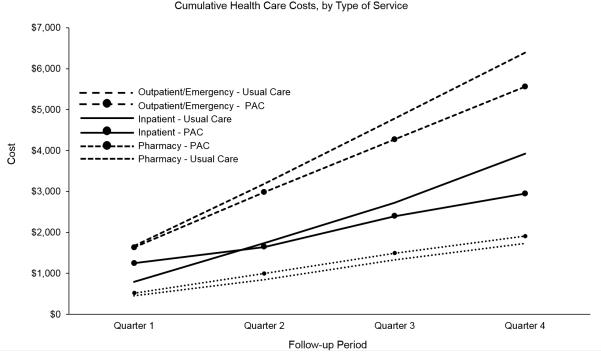
After one year of follow-up, 13.6% of intervention patients and 17.1% of patients randomized to usual care were hospitalized; 3% of intervention patients and 6% of usual care patients had multiple admissions (Table 3). Two thirds of hospitalizations occurred at VAMCs. The most common reason for inpatient admission in both intervention and usual care groups was circulatory disease (40% versus 43%), followed by musculoskeletal issues (12% versus 14%) and digestive system disease (10% versus 8%). Hospitalization for respiratory illness was slightly less frequent among intervention patients (2% versus 10%). The total cost of hospitalizations during the study per enrolled patient was slightly lower in the intervention group ($2,948 versus $3,928) but the difference was not statistically significant (p=.39) (Table 3, Figure 1). Visits to the emergency room that did not result in admission were infrequent in both groups (4 in intervention versus 3 in usual care) and their cost, averaged over all patients, did not differ between groups ($11 versus $10; p=.88). VAMC outpatient care was received by all patients during the study and was slightly lower in the intervention group ($5,550 versus $6,383, p=0.18) (Table 3, Figure 1). VAMC pharmacy costs, which approached $2,000 for the year and were incurred by all but one patient in each group, did not differ substantially between groups ($1,909 versus $1,731, p=0.51) (Table 3, Figure 1). For all care settings combined, total health care cost per patient at one year reached $10,418 in the intervention group, versus $12,052 with usual care (difference=−$1,634 (95% confidence interval=−$4,683 to $1,416; p=.29) (Table 3).
Table 3.
One Year Health Care and Intervention Costs, by Treatmenta
| PAC | Usual Care | Difference | P Value | |
|---|---|---|---|---|
| (n=199) | (n=199) | (PAC–Usual Care) | ||
| Hospitalization frequencyb | ||||
| 0 | 172 (86.4) | 165 (82.9) | n/a | 0.24 |
| 1 | 21 (10.6) | 22 (11.1) | ||
| 2 | 4 (2.0) | 10 (5.0) | ||
| ≥3 | 2 (1.0) | 2 (1.0) | ||
| Number of hospitalizations | 0.20 (0.11 / 0.29) |
0.24 (0.16 / 0.32) |
−0.04 (−0.16 / 0.08) |
0.53 |
| Hospital days | 1.28 (0.50 / 2.06) |
1.18 (0.56 / 1.81) |
0.10 (−0.89 / 1.09) |
0.84 |
| Hospital cost ($) | 2,948 (1,378 / 4,519) |
3,928 (2,331/ 5,526) |
−979 (−3,213 / 1,254) |
0.39 |
| Emergency Room ($)c | 11 (−3 / 25) |
10 (−4 / 24) |
1 (−18 / 21) |
0.89 |
| Outpatient cost ($) | 5,550 (4,766 / 6,334) |
6,383 (5,437 / 7,329) |
−833 (−2,058 / 392) |
0.18 |
| Pharmacy cost ($) | 1,909 (1,476 / 2,341) |
1,731 (1,433 / 2,029) |
177 (−346 / 701) |
0.51 |
| Total health care cost ($) | 10,418 (8,295 / 12,542) |
12,052 (9,851 / 14,253) |
−1,634 (−4,683 / 1,416) |
0.29 |
| Intervention cost ($) | 696 (670 / 721) |
0 | 696 (670 / 721) |
|
| Grand total costd ($) | 11,114 (8,989 / 13,239) |
12,052 (9,851 / 14,253) |
−938 (−3,988 / 2,112) |
0.55 |
Mean with 95% confidence interval in parentheses unless otherwise specified.
Number of patients with percent in parentheses.
Includes emergency room visits that did not result in hospital admission. Costs of emergency room encounters that resulted in hospitalization are subsumed under hospital costs.
Health care cost plus intervention cost. PAC=physical activity counseling.
Figure 1.
The mean cumulative health care costs are shown in quarterly intervals for each service type (inpatient, pharmacy and outpatient (including emergency room visits not resulting in hospitalization), by treatment group. PAC=physical activity counseling.
The effect of the intervention on health care costs at one year was not substantially affected after adjusting for baseline patient characteristics (mean difference (with covariates evaluated at group means)=$1,656, 95% confidence interval=−$3,890 to $1,230; p=0.23). Factors positively associated with cost included higher eligibility priority for VA care (service-connected and pension/income priority categories versus category with copay requirements), respiratory problems, digestive disorders, amputation, cataracts, chest pain, numbness and confusion (Supplemental Table 1).
Intervention and Health Care Costs Combined
Combining the cost of the intervention with health care costs resulted in an estimate of slightly lower, but not statistically different costs in the PAC group relative to usual care ($11,114 versus $12,052; difference = −$938 (95% confidence interval=−$3,988 to $2,112; p=.55)) (Table.3).
Intervention Cost per Improvement in Outcomes
The percent of enrolled patients reaching an activity level of at least 150 minutes per week of combined endurance and strength activities increased 16% between baseline and one year follow-up with the intervention (12% to 28%) compared to 2% (13% to 15%) with usual care. Assuming intervention costs were not offset by reductions in health care costs, the VA-LIFE intervention cost an additional $4,971 per additional patient reaching target exercise levels, compared to usual care ($696/.14). In terms of primary outcomes, only the cost per unit improvement in rapid gait speed was calculated, since differential improvements in usual gait speed were not observed in the intervention group. The incremental cost per patient of achieving a clinically significant change of 0.1 meter/second in rapid gait speed (44% versus 29% in intervention versus control) was $4,640 ($696/.15).
DISCUSSION
As previously reported, the VA-LIFE physical activity counseling intervention improved physical activity levels and rapid gait speed, relative to usual care, in a sample of older veterans. Our economic evaluation of the program suggests that these gains were achieved at a modest average program cost ($696 per patient) that represents about 6% of participants’ estimated annual health care expenditures. In addition, while our estimate of differences in health care costs between the physical activity counseling and usual care groups was not statistically significant, the estimate lacked precision and we cannot rule out the possibility that differences in health care costs offset program expenses to some extent over the study period.
Few other randomized studies of physical activity interventions have compared health care costs between treatments, and significant differences were not found in those that have.18-20 However, an inverse relation between physical activity and health care costs has been reported in observational studies. A recent examination of health care expenditures and physical activity levels among 51,165 U.S. adults suggests costs related to inactivity constitute 8% to 11% of aggregate health care expenditures, with a mean in the range of $920 to $1,313 per individual (2012 dollars).21 A large cross-sectional study of Medicare retirees found annual health care charges of moderately active individuals to be about $1,456 less than those of sedentary retirees (2002 dollars),22 and a smaller retrospective cohort study of Medicare managed care enrollees found health care costs of those who participated in a group-based physical activity program to be similar to nonparticipants in the first year, but $1,186 lower per participant in year two (2005 dollars).23 Such findings must be interpreted cautiously, given the difficulty of dealing with the endogeneity of inactivity in observational research (i.e., inactivity may be determined in part by health status, which is correlated with health care costs). This limitation notwithstanding, the reduction in health care costs we observed in VA-LIFE is of a similar magnitude.
The VA-LIFE program was well accepted by providers in the primary care setting and required relatively little investment from providers themselves; counselor effort was the primary expense. Our estimates of the amount and cost of this effort were based on experience in VA-LIFE. Although the VA-LIFE counselor followed structured protocols, the cost (and effectiveness) of implementing the intervention elsewhere may vary with the salary and experience of the counselor. In addition, staffing costs per participant in any particular program would depend upon rates of enrollment and drop-out and the ability to match counselor time allocated to the program to program census. Nonetheless, estimated intervention costs per participant in the VA-LIFE program ($696) were comparable to those reported for other interventions in the U.S. that promote home-based physical activity tailored to patients ($400 to $1,200 annually per participant in 2014 dollars).24,25 Similarly, our estimate of the cost of shifting a patient in VA-LIFE from inactivity to the recommended physical activity target, assuming no reduction in health care costs, was of comparable magnitude to prior reports in the literature ($4,971 versus $1,337 to $5,554 in 2014 dollars).25 While such metrics are informative, they by no means fully capture the potential impact of a program that increases physical activity.26 Elderly participants with chronic disease may fail to reach target levels of activity, but can still reap important benefits from avoidance of sedentary behavior. Indeed, current physical activity guidelines state that older adults with chronic disease should do as much physical activity as they can.5
Although home-based programs are less intensive and less effective than center-based initiatives in improving health related quality of life and functional status,7 they have the potential to reach a broader segment of the population at considerably lower cost. However, evidence suggests that these programs must provide ongoing support to maintain activity levels in the long term.27 As advances in information technology continue and are more widely adopted among older adults, it may be possible to introduce more potent and efficient modes of delivery that increase levels of habitual activity and fitness in this population.28-30 One determinant of service delivery efficiency is the extent to which an intervention targets individuals who are physiologically and/or psychologically receptive. While interventions such as VA-LIFE typically incorporate established mediators of physical activity, such as self-efficacy, ongoing research may identify additional determinants in a variety of domains (e.g., genetic, psychological, physical, social, cultural) that pinpoint key factors underlying individuals’ propensities to engage in physical activity in various environments. A better understanding of such factors is needed to design programs in settings that maximize the likelihood of success in heterogeneous populations of inactive adults.31
Several limitations should be considered when interpreting our results. First, estimates of between-group differences in health care costs had wide confidence intervals that include economically relevant amounts that could either offset program expenses or add to health expenditures. Both scenarios are compatible with the data and neither outcome can be ruled out statistically.32,33 Second, indirect costs, such as patient time, were not collected and were excluded from analyses. Third, outpatient and pharmacy services received outside the VA health care system could not be collected and were excluded. However, all participants received ongoing care from a primary care provider at the Durham VAMC and all received outpatient services from VAMCs during the follow-up period (all but two received pharmacy services). Therefore, it is unlikely that any non-VA outpatient or pharmacy care received by participants would be of a sufficient quantity to substantially affect results. Fourth, the sample included only older male veterans and results may not be generalizable to females or younger populations. However, as most exercise studies have enrolled predominantly female participants, this study may contribute valuable knowledge regarding exercise outcomes and cost in older men. Fifth, physical activity was self-reported and was likely overestimated in quantity and intensity, potentially biasing results. Sixth, intervention overhead costs were estimated based on facility averages for outpatient care and may vary across settings and time horizons. However, these costs were clearly identified so as to allow readers to interpret in context. Finally, the study was not large enough and did not have sufficient follow-up to support a formal analysis of the cost-effectiveness of the VA-LIFE intervention (in terms of cost per quality-adjusted life years gained). Nonetheless, the program appears competitive in terms of the cost of increasing physical activity, and it provided objectively measured clinical benefit.
In conclusion, improvements in physical activity and rapid gait speed achieved in VA-LIFE were obtained at a cost that represents a small fraction of patients’ annual health care costs. Larger multi-site studies with longer follow-up are needed to determine the net financial impact and value of implementing a tailored home-based physical activity counseling program for older adults in a primary care setting.
Supplementary Material
ACKNOWLEDGMENTS
All researchers who contributed significantly to this paper have been included as authors.
Sponsor’s Role: Funding agencies (The Department of Veterans Affairs and National Institutes of Health) were not involved in development of study design/methods, subject recruitment, data collection, analysis or paper preparation. The opinions contained in this paper are those of the authors and do not necessarily reflect those of the U.S. Department of Veterans Affairs.
Grant Support:
Veterans Affairs Rehabilitation Research and Development Research Grant E3386R and National Institutes of Health Grant AG028716. KH is supported by a Career Development Award (11K2RX001316) from the Department of Veterans Affairs, Veterans Health Administration, Rehabilitation Research and Development Service.
Footnotes
Trial Registration: clinicaltrials.gov; identifier NCT00435188
SUPPLEMENTAL MATERIAL
Supplemental Table 1. Results of Multivariable Analysis of Total Health Care Costs
Conflict of Interest
| Element | PAC | MJP | CFP | RJS | KSH | ESM | HBB | CCE | MPP | MCM |
|---|---|---|---|---|---|---|---|---|---|---|
| Employment or affiliation | No | No | No | No | No | No | No | No | No | No |
| Grants or funding | No | No | No | No | No | No | No | No | No | No |
| Honoraria | No | No | No | No | No | No | No | No | No | No |
| Speaker forum | No | No | No | No | No | No | No | No | No | No |
| Consultant | No | No | No | No | No | No | No | No | No | No |
| Stock ownership/options | No | No | No | No | No | No | No | No | No | No |
| Royalties | No | No | No | No | No | No | No | No | No | No |
| Expert testimony | No | No | No | No | No | No | No | No | No | No |
| Advisory board | No | No | No | No | No | No | No | No | No | No |
| Patents | No | No | No | No | No | No | No | No | No | No |
| Personal relationship | No | No | No | No | No | No | No | No | No | No |
Authors’ Contributions
| Element | PAC | MJP | CFP | RJS | KSH | ESM | HBB | CCE | MPP | MCM |
|---|---|---|---|---|---|---|---|---|---|---|
| Condition 1 | ||||||||||
| Conception / design | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Acquisition of data | Yes | Yes | No | No | No | No | No | Yes | Yes | Yes |
| Analysis /
interpretation of data |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Condition 2 | ||||||||||
| Drafting article | Yes | No | No | No | No | No | No | No | No | Yes |
| Critical revision of
article |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Condition 3 | ||||||||||
| Final approval of
article |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
REFERENCES
- 1.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–29. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myers J, Kaykha A, George S, et al. Fitness versus physical activity patterns in predicting mortality in men. Am J Med. 2004;117:912–8. doi: 10.1016/j.amjmed.2004.06.047. [DOI] [PubMed] [Google Scholar]
- 3.Kohl HW, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- 4.Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat 10. 2014;260:1–161. [PubMed] [Google Scholar]
- 5.Physical Activity Guidelines Advisory Committee . Physical Activity Guidelines Advisory Committee Report, 2008. U.S. Department of Health and Human Services; Washington, DC: 2008. [DOI] [PubMed] [Google Scholar]
- 6.Kerse N, Elley CR, Robinson E, et al. Is physical activity counseling effective for older people? A cluster randomized, controlled trial in primary care. J Am Geriatr Soc. 2005;53:1951–6. doi: 10.1111/j.1532-5415.2005.00466.x. [DOI] [PubMed] [Google Scholar]
- 7.Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311:2387–96. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stessman J, Hammerman-Rozenberg R, Cohen A, et al. Physical activity, function, and longevity among the very old. Arch Intern Med. 2009;169:1476–83. doi: 10.1001/archinternmed.2009.248. [DOI] [PubMed] [Google Scholar]
- 9.Lobo A, Carvalho J, Santos P. Comparison of functional fitness in elderlies with reference values by Rikli and Jones and after one-year of health intervention programs. J Sports Med Phys Fitness. 2011;51:111–20. [PubMed] [Google Scholar]
- 10.Peterson MJ, Sloane R, Cohen HJ, et al. Effect of telephone exercise counseling on frailty in older veterans: project LIFE. Am J Mens Health. 2007;1:326–34. doi: 10.1177/1557988307306153. [DOI] [PubMed] [Google Scholar]
- 11.Morey MC, Peterson MJ, Pieper CF. The Veterans Learning to Improve Fitness and Function in Elders Study: a randomized trial of primary care-based physical activity counseling for older men. J Am Geriatr Soc. 2009;57:1166–74. doi: 10.1111/j.1532-5415.2009.02301.x. at al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oddone E, Weinberger M, Hurder A, et al. Measuring activities in clinical trials using random work sampling: implications for cost-effectiveness analysis and measurement of the intervention. J Clin Epidemiol. 1995;48:1011–8. doi: 10.1016/0895-4356(94)00229-j. [DOI] [PubMed] [Google Scholar]
- 13.Databases, tables & calculations by subject. Available at: www.bls.gov/data/. Accessed 6/3/2015.
- 14.Barnett PG, Rodgers JH. Use of the decision support system for VA cost-effectiveness research. Med Care. 1999;37:AS63–70. doi: 10.1097/00005650-199904002-00009. [DOI] [PubMed] [Google Scholar]
- 15.Riley GF. Administrative and claims records as sources of health care cost data. Med Care. 2009;47:S51–5. doi: 10.1097/MLR.0b013e31819c95aa. [DOI] [PubMed] [Google Scholar]
- 16.CMS Physician Fee Schedule Search. Available at: http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx. Accessed 6/3/2015.
- 17.Glick HA, Doshi JA, Sonnad SS, et al. Economic Evaluation in Clinical Trials. Oxford University Press Inc.; New York: 2007. [Google Scholar]
- 18.Golsteijn RH, Peels DA, Evers SM, et al. Cost-effectiveness and cost-utility of a Web-based or print-delivered tailored intervention to promote physical activity among adults aged over fifty: an economic evaluation of the Active Plus intervention. Int J Behav Nutr Phys Act. 2014;11:122. doi: 10.1186/s12966-014-0122-z. Available at: http://www.ijbnpa.org/content/11/1/122. Accessed 9/25/2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dubbert PM, Morey MC, Kirchner KA, et al. Counseling for home-based walking and strength exercise in older primary care patients. Arch Intern Med. 2008;168:979–86. doi: 10.1001/archinte.168.9.979. [DOI] [PubMed] [Google Scholar]
- 20.Elley R, Kerse N, Arroll B, et al. Cost-effectiveness of physical activity counselling in general practice. N Z Med J. 2004;117(1207):U1216. [PubMed] [Google Scholar]
- 21.Carlson SA, Fulton JE, Pratt M, et al. Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis. 2015;57:315–23. doi: 10.1016/j.pcad.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang F, McDonald T, Reffitt B, et al. BMI, physical activity, and health care utilization/costs among Medicare retirees. Obes Res. 2005;13:1450–7. doi: 10.1038/oby.2005.175. [DOI] [PubMed] [Google Scholar]
- 23.Ackermann RT, Williams B, Nguyen HQ, et al. Healthcare cost differences with participation in a community-based group physical activity benefit for medicare managed care health plan members. J Am Geriatr Soc. 2008;56:1459–65. doi: 10.1111/j.1532-5415.2008.01804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis BA, Williams DM, Neighbors CJ, et al. Cost analysis of internet vs. print interventions for physical activity promotion. Psychol Sport Exerc. 2010;11:246–249. doi: 10.1016/j.psychsport.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sevick MA, Napolitano MA, Papandonatos GD. Cost-effectiveness of alternative approaches for motivating activity in sedentary adults: results of Project STRIDE. Prev Med. 2007;45:54–61. doi: 10.1016/j.ypmed.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vogel T, Brechat PH, Leprêtre PM, et al. Health benefits of physical activity in older patients: a review. Int J Clin Pract. 2009;63:303–20. doi: 10.1111/j.1742-1241.2008.01957.x. [DOI] [PubMed] [Google Scholar]
- 27.Hall KS, Sloane R, Pieper CF, et al. Long-term changes in physical activity following a one-year home-based physical activity counseling program in older adults with multiple morbidities. J Aging Res 2010 Dec. 2011;26:308407. doi: 10.4061/2011/308407. doi: 10.4061/2011/308407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pratt M, Sarmiento OL, Montes F, et al. The implications of megatrends in information and communication technology and transportation for changes in global physical activity. Lancet. 2012;380:282–93. doi: 10.1016/S0140-6736(12)60736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shuger SL, Barry VW, Sui X, et al. Electronic feedback in a diet- and physical activity-based lifestyle intervention for weight loss: a randomized controlled trial. Int J Behav Nutr Phys Act. 2011;8:1–8. doi: 10.1186/1479-5868-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wijsman CA, Westendorp RG, Verhagen EA, et al. 2013;15:e233. doi: 10.2196/jmir.2843. Available at: http://www.jmir.org/2013/11/e233/. Accessed 9/25/2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bauman AE, Reis RS, Sallis JF. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380:258–71. doi: 10.1016/S0140-6736(12)60735-1. at al. [DOI] [PubMed] [Google Scholar]
- 32.Wasserstein RL, Lazar NA. The ASA's Statement on p-values: context, process, and purpose. The American Statistician. 2016;70:129–133. [Google Scholar]
- 33.Goodman SN, Berlin JA. The use of predicted confidence intervals when planning experiments and the misuse of power when interpreting results. Ann Intern Med. 1994;121:200–206. doi: 10.7326/0003-4819-121-3-199408010-00008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.