Abstract
Background
Previous studies have demonstrated an association between migraine and major depressive disorder. However, relatively little is known about the relationship between suicidal ideation, with or without concurrent depression, and migraine.
Objective
We conducted a systematic literature review to synthesize the available research focused on investigating the association of migraine with suicidal ideation.
Methods
Relevant research papers were identified through searches of major electronic databases including PubMed, Embase (Elsevier), Web of Science (Thomson Reuters), PsycINFO (EBSCO), and Google Scholar. We performed a meta-analysis to estimate the pooled unadjusted and adjusted odds ratios (ORs) and 95% confidence intervals (95%CI) for the association between migraine and suicidal ideation extracted from each study.
Results
A total of 148,977 participants in six studies were included in this analysis. Overall, findings from available studies documented elevated odds of suicidal ideation among individuals with migraines. In unadjusted models, the odds of suicidal ideation was 2.49-fold higher among individuals with migraine (OR: 2.49; 95%CI: 2.34–2.65) compared to those without migraine. In multivariate-adjusted models, the pooled adjusted OR of suicidal ideation was 1.31 (OR: 1.31; 95%CI: 1.10–1.55).
Conclusions
A meta-analysis of available studies suggests a modest positive association between migraine and suicidal ideation. Further studies allowing for a more comprehensive investigation of the association between migraine and the full range of suicidal behaviors are warranted. A larger and more robust evidence-base may be useful to inform the clinical screening and diagnoses of comorbid conditions in migraineurs.
Introduction
Migraines are recurrent disabling headaches associated with neurologic symptoms including severe throbbing head pain, with or without visual disturbances [1]. The estimated prevalence of migraine is between 11–23% globally [2–5]. Migraines are a common disabling illness known to be comorbid with neurological and psychiatric disorders including fibromyalgia [6], epilepsy [7], stroke [8], multiple sclerosis [9], panic disorder [10], depression [11, 12], and post-traumatic stress disorder [13].
The association of migraine with suicidal behaviors, however, has been infrequently studied [14–19], and results from available studies have varied depending on the specific types of suicidal behaviors studied. For example, some studies have observed positive associations between migraine and self-harm [20], suicide attempt [14, 17, 21], or suicide mortality [22]. Suicide is the second leading cause of death among young adults with over 800,000 suicide deaths per year worldwide. The number of suicide deaths is likely higher than this, as many go unreported, and many more people make suicide attempts [23]. Risk factors for suicidal behaviors include male gender, family history of mental disorders, previous suicide attempts, substance abuse, and comorbid disorders including severe depression and chronic pain [24, 25]. Suicidal ideation is a prominent risk factor for escalating suicidal behavior, and diagnosis of suicidal ideation may provide opportunities for clinical screening and intervention prior to suicide attempts and completed suicide [26, 27].
In light of the global burden of migraine [5] and the high prevalence of suicidal ideation [26], we conducted a systematic review and meta-analysis of the published literature to examine the association between migraine and suicidal ideation. Further, we sought to quantify the association between migraine and suicidal ideation after adjusting for confounders.
Methods
We conducted the review and meta-analysis according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) statement (Supplementary Table 1) [28].
Study selection and criteria for study inclusion
Studies were identified by searching major electronic databases including PubMed, Embase (Elsevier), Web of Science (Thomson Reuters), PsycINFO (EBSCO), and Google Scholar. Controlled vocabulary terms (MeSH terms) were used when appropriate. The specific search criteria are presented in Supplementary Table 2. Bibliographies of relevant articles were reviewed to identify additional studies. Observational studies, including cohort, case-control, and cross-sectional studies, that address associations between migraine and suicidal ideation were included. Articles were rejected on abstract review if they were review articles, case studies, or qualitative studies. No date or language limitations were applied to the search.
Data extraction and quality assessment
We merged search results using Endnote from database searches and removed duplicate articles. We retrieved full text of potentially relevant articles and examined full text articles for compliance with eligibility criteria. The following types of data were extracted from all articles: authors, year of publication, country of origin, study design, total sample size, measure used to assess suicidal ideation, measure used to assess migraine diagnosis, and whether the study considered migraine subtypes (migraine with aura or migraine without aura). We extracted both adjusted and unadjusted odds ratios (OR), when available, from relevant studies. When not reported, ORs were calculated using published study data. Authors were also contacted for this information. We assessed methodological quality for each study using a modified Newcastle-Ottawa Scale (NOS) for cross-sectional studies [29]. Study quality assessment is presented in Supplementary Table 3.
Data synthesis and statistical analysis
We used Stata (Stata, College Station, TX) to generate summary statistics and pooled ORs using a random effects model. In studies that evaluated ORs for migraine with aura and migraine without aura separately, migraine without aura adjusted ORs were used for the summary analysis. This conservative approach may have underestimated the association, since the migraine without aura ORs were consistently lower than those for migraine with aura. Summary and pooled ORs were represented as point estimates and 95%CIs on a forest plot. Funnel plots were used to evaluate publication bias. We also conducted a sensitivity analysis for the unadjusted pooled ORs excluding one study [19] which was heavily weighted in the unadjusted pooled OR analysis.
Results
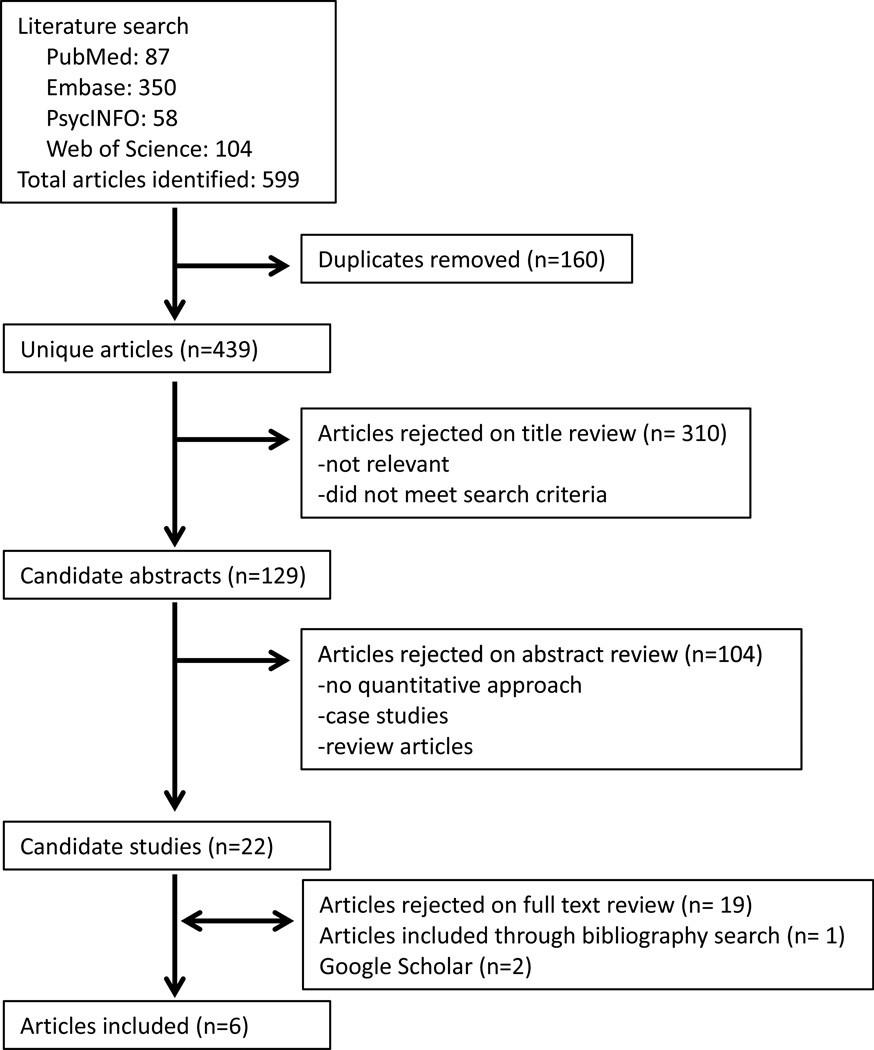
Our initial search identified a total of 599 potentially relevant articles (Figure 1). After removing duplicates, we had a total of 439 unique articles. Articles (N=310) were rejected on title review for not being relevant or not meeting our search criteria. Abstracts of the remaining 129 candidate articles were reviewed. Articles were rejected if they were review articles, case studies, or qualitative studies.
Figure 1.
Flowchart of systematic literature review
The results of the remaining six population- or community-based cross-sectional studies, comprising a total of 148,977 participants, were included in the meta-analysis (Table 1). Migraines were assessed using structured questionnaires based on IHS criteria [14–16] or self-reported physician diagnosed migraine [17–19]. Four studies used a single question to assess presence or absence of suicidal ideation in participants [16–19]. Breslau et al. used four questions to assess suicidal ideation and suicide attempt [14]. In their study, Breslau et al. used one question (“have you ever felt so low you thought about committing suicide”) that was similar to the suicidal ideation question used in other studies [14]. Wang et al. used the Mini-International Neuropsychiatric Interview-Kid for children and adolescents Suicidality Module (MINI-Kid), a scaled questionnaire that included questions on both suicidal ideation and suicide attempt to assess participants’ overall suicidal risk [15].
Table 1.
Descriptions of principal characteristics of cross-sectional articles included in the systematic review and meta-analysis (N =6)
| First Author and Year |
Country of Origin |
Sample Size (n) |
Measures Used to Assess Suicidal Ideation |
Measures Used to Assess Migraine |
Stratified by Migraine Subtype |
Unadjusted OR (95%CI) |
Adjusted OR (95%CI) | OR Adjustment Variables |
|---|---|---|---|---|---|---|---|---|
| Breslau 1992 | USA | 1,007 | Ask “have you ever felt so low you thought about committing suicide?” |
Structured questionnaire that uses IHS criteria (1988) |
Yes | NA | MA: 2.4 (1.1–5.3) MO: 1.7 (0.8–3.4) |
coexisting mania, dysthymia, anxiety disorders, substance use disorders |
| Wang 2007 | Taiwan | 121 | Mini- International Neuropsychiatric Interview-Kid for children and adolescents Suicidality Module |
Structured questionnaire that uses IHS criteria (2006) |
Yes | 4.3 (1.2–15.5) | MA: 7.8 (1.4–44.6) MO: 2.1 (0.5–8.5) |
age, gender, major depression, anxiety disorders |
| Ratcliffe 2008 | Canada | 36,984 | Ask “have you ever seriously considered committing suicide or taking your own life?” |
Self-reported physician diagnosed migraine headache |
No | 2.60 (2.29–2.95)† | 1.45 (1.14–1.84) | sex, age, marital status, education, mood disorder, anxiety disorder, substance dependence disorder, 3+ mental disorder comorbidity, other chronic pain disorders |
| Wang 2009 | Taiwan | 3,963 | Adolescent Depression Inventory (Item 17) |
Structured questionnaire that uses IHS criteria (2004) |
Yes | 2.9 (2.3–3.6) | MA: 1.79 (1.07–2.99) MO: 1.04 (0.77–1.40) |
age, gender, depression, living arrangements |
| Fuller-Thomson 2013 | Canada | 5,788 | Ask “have you ever seriously considered committing suicide or taking your own life?” |
Self-reported physician diagnosed migraine headache |
No | 2.08 (1.4–3.08)† | 1.25 (0.64–2.45) | gender, school attendance, race, living arrangement, did not have enough food to eat due to lack of money, smoking, alcohol dependency, self-perceived health status, activities prevented by pain, number of chronic conditions, depression, asthma, back problems |
| Colman 2016 | Canada | 101,114 | Ask “have you ever seriously considered committing suicide or taking your own life?” |
Self-reported physician diagnosed migraine headache |
No | 2.43 (2.29–2.58)† | NA | NA |
MA = migraine with aura, MO = migraine without aura, NA = not applicable
Unadjusted ORs calculated based on study information provided
Published studies documented comorbidity between diagnosed migraine and suicidal ideation, even when controlling for prior depression and other covariates (Table 1). Among members of a large Health Maintenance Organization in Michigan, Breslau et al. found that migraine with aura was associated an increased odds of suicidal ideation (OR:2.4, 95%CI: 1.1–5.3) [14]. However, migraine without aura was not statistically significantly associated with suicidal ideation (OR:1.7, 95%CI: 0.8–3.4) [14]. Ratcliffe et al., using the nationally representative Canadian Community Health Survey Cycle in 2001–2002, showed a positive significant association between suicidal ideation and migraine (OR:1.45, 95%CI: 1.14–1.84) [17]. Recently, Colman et al., found that among residents of Ontario, Canada in 2003, 2005, or 2007, migraines were associated with increased risk of self-harm (hazard ratio (HR):1.48; 95%CI: 1.11–1.96) [19].
Three recent studies focused in adolescents showed a relationship between migraines and suicidal ideation [15, 16, 18]. In 12–15 year old Taiwanese students, there was a significant association between migraine and suicide risk score, a scaled measure including suicidal ideation and attempts (OR:4.3, 95%CI: 1.2–15.5) [15]. The association was statistically significant for students’ with migraine with aura (OR:7.8, 95%CI: 1.4–44.6); however, no statistically significant association was observed for students with migraine without aura and suicide risk score (OR:2.1, 95%CI: 0.5–8.5) compared to students without migraines [15]. Similarly, in a prospective community-based study of Taiwanese adolescents (mean age: 14.0 ± 0.9 years), migraines were significantly associated with suicidal ideation (OR:2.9, 95%CI: 2.3–3.6). Migraine with aura was significantly associated with suicidal ideation (OR:1.79, 95%CI: 1.07–2.99); however, migraine without aura was not statistically significantly associated with suicidal ideation (OR:1.04, 95%CI: 0.77–1.40) [16]. Finally, Fuller-Thomson and colleagues, in their 2000–2001 community-based Canadian Community Health Survey, found no evidence of an association of migraine with suicidal ideation (OR:1.25; 95%CI: 0.64–2.45) [18].
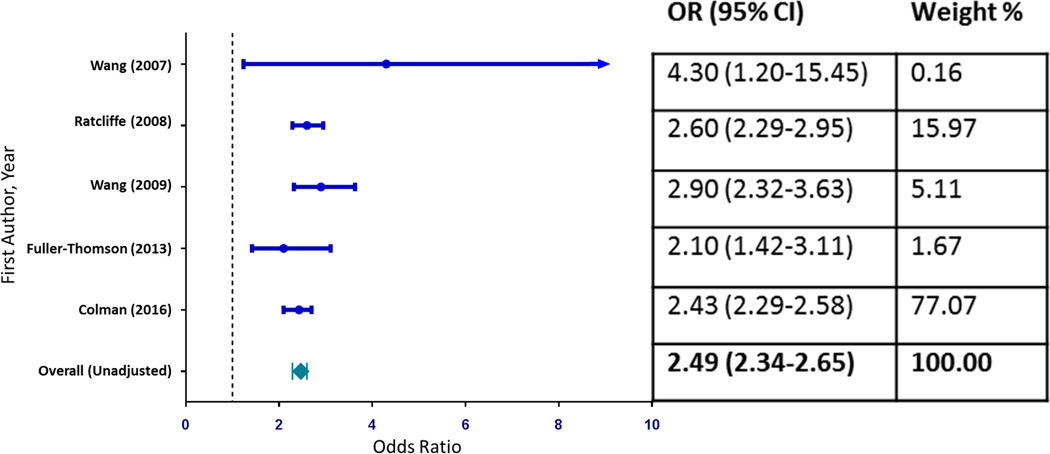
The pooled unadjusted OR of the association between migraine and suicidal ideation was 2.49 (OR: 2.49; 95%CI: 2.34–2.65). The studies’ specific ORs ranged from 2.10 (95%CI: 1.42–3.11) to 4.30 (95%CI: 1.20–15.45) (Figure 2). Visual inspection of the funnel plot did not show evidence of publication bias, confirmed by the Egger’s test for publication bias (H0: intercept = 0.70; p-value = 0.385) (Supplemental Figure 1). We performed a sensitivity analysis excluding the study with the largest sample size [19] from the unadjusted OR summary analysis. In this sensitivity analysis, the unadjusted OR for the remaining four studies (OR:2.63; 95%CI: 2.37–2.93) was similar to the unadjusted pooled OR for the complete dataset (Supplemental Figure 2).
Figure 2.
Forest plot showing articles unadjusted ORs (95% CI) of the association between migraine and suicidal ideation and the pooled summary (N = 5)
Note: Breslau 1992 was excluded due to missing information.
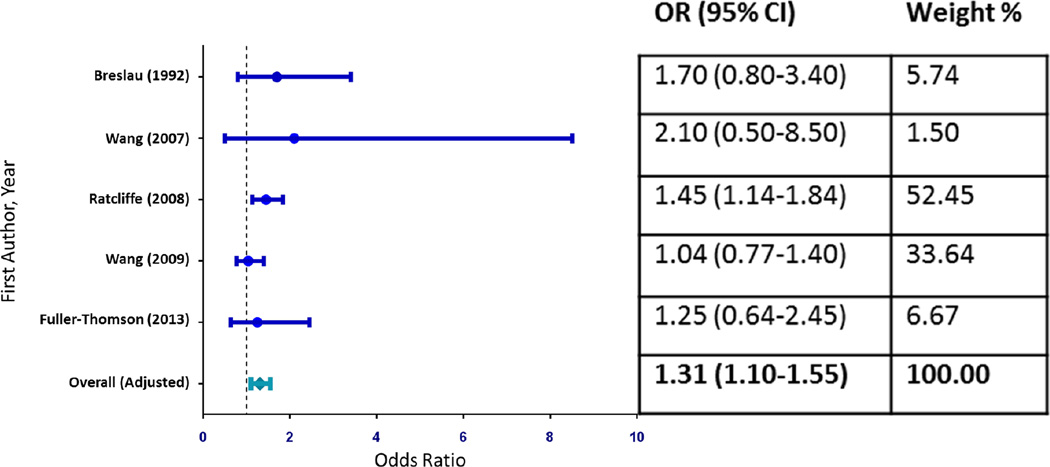
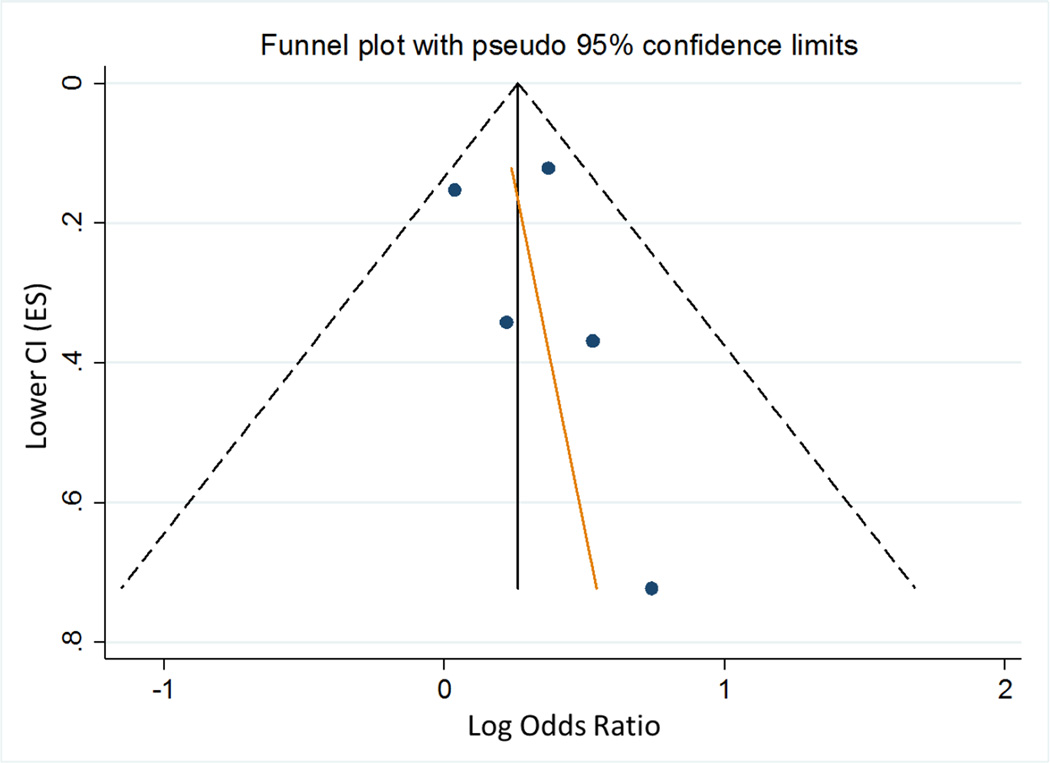
The pooled adjusted OR for the five studies with multivariable adjusted ORs was 1.31 (95%CI: 1.10–1.55) with specific measures of association ranging from 1.04 (95% CI: 0.77–1.40) to 2.10 (95%CI: 0.50–8.50) (Figure 3). This is likely a conservative estimate, since the migraine without aura ORs were included in this analysis for three studies. A visual inspection of the associated funnel plot did not show evidence of a significant publication bias, and this was confirmed by the Egger’s test for publication bias (H0: intercept = 0.50; p-value = 0.633) (Figure 4).
Figure 3.
Forest plot showing articles with multivariable adjusted ORs (95% CI) of the association between migraine and suicidal ideation and the pooled summary (N = 5)
Note: Colman 2016 was excluded due to missing information. Fully-adjusted migraine without aura ORs were used when both migraine with aura and migraine without aura were reported separately (Breslau 1992, Wang 2007, Wang 2009).
Figure 4.
Funnel plot of articles included with adjusted ORs (95% CI) of the association between migraine and suicidal ideation (N = 5)
Note: Colman 2016 was excluded due to missing information
Discussion
To our knowledge, this is the first meta-analysis examining the association between migraine and suicidal ideation. In a pooled analysis, we observed a significant association between migraine and suicidal ideation (Figure 3; OR:1.31; 95%CI: 1.10–1.55) after adjusting for confounders.
Migraine, major depressive disorder, and suicidal ideation may be influenced by both genetics and environmental stimuli, including stressful life events, which affect a person’s neurobiological systems [30–32]. Allelic variation in the serotonin transporter gene affects neurons’ ability to adapt to changes in external stimulations including acute stressors [31]. Although studies have found evidence of the association between allelic variation and suicidal behaviors, the association is controversial [33, 34]. Serotonin transporter polymorphisms may also be associated with the frequency of migraine attacks, depressive symptoms, and suicidal behaviors [32, 35–37]. Stress and serotonin interactions may be moderated by brain-derived neurotrophic factor (BDNF) polymorphisms [11, 32] and dopamine [38]. Ovarian hormones affect neurotransmitters and are known to be strongly associated with both migraine and depression in premenopausal women [36, 39].
Stressful life events, both during childhood and adulthood, also play a role in the development of major depressive disorder and suicidal ideation through dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis which affects the ability to respond to stress [31, 40, 41]. The abnormal function of the HPA axis and other hormones can also lead to neurobiological abnormalities and structural changes in the brain [31, 42, 43]. The dysregulation of the HPA axis, changes in brain matter volume, and sensitization to high levels of stress contribute to migraine, depressive disorders, and suicidal behaviors [36, 44]. Additionally, suicidal ideation has been linked to pain conditions, including increased headache frequency [16, 17, 22, 25, 45]. For example, Ilgen et al. (2008) found suicidal ideation was associated with head pain (OR:1.9; 95%CI:1.2–3.0) and pain summary score (OR: 2.3; 95%CI: 1.2–4.4) compared to adults without chronic pain [45]. Suicide ideation was also associated with more frequent headaches in adolescents after controlling for depression and sociodemographic characteristics (>7 days/month; OR:1.69; 95%; CI:1.12–2.56) [16]. Chronic pain conditions, including migraines, have been associated with an increase in suicidal ideation, suicide attempts, and suicide mortality [25]. Psychological and social factors also influence headache development, pain severity, impact on functioning, and treatment prognosis [46]. Negative emotional states, including anxiety, depression and anger, are associated with headache triggers, intensity of headache pain, and response to treatment [46, 47]. Coping skills have also been shown to moderate the relationship between headache severity and depression [48].
The strengths of this review include an extensive literature search of five online databases, use of the Newcastle-Ottawa Scale (NOS) scale for quality assessment of selected studies, and a combined quantitative summary of the study findings using conservative estimates of the association between migraine and suicidal ideation. Our summary statistics are based on 148,977 participants from 6 peer-reviewed articles. Additionally, our review and meta-analysis builds on a previous review article [49] that focused on the association between migraine and suicidal behaviors, including ideation, plans and attempts. In the first year of suicidal ideation, individuals are more likely to progress to suicide plans or attempts [50]. For screening and diagnostic purposes, it is therefore essential to identify individuals who are at risk for these behaviors. Therefore, our review and meta-analysis focuses specifically on the association between migraine and suicidal ideation.
Despite these strengths, there are also limitations that should be considered. First, reviewed studies had variability in criteria for migraine and suicidal ideation which could have resulted in heterogeneity in diagnoses. The variability in magnitude affects may be related to how suicidal ideation was measured across the included studies. The present studies do not use a specific assessment tool and measure suicidal ideation using either a single question or MINI-Kid score. Secondly, depression status was not uniformly controlled in studies, despite the well-established comorbidity between major depressive disorder and suicidal ideation [24, 51]. Finally, our meta-analysis is based on results from observational cross-sectional studies, and so the temporal relationship between migraine and suicidal ideation cannot be established with certainty.
This systematic review and meta-analysis shows a significant association between migraine and suicidal ideation. Further research is needed to identify the mechanisms underlying the relationship between migraine and suicidal ideation. For example, migraine with aura is consistently more strongly associated with suicidal ideation compared with migraine without aura (Table 1), although the mechanisms underlying this association are not yet understood. There are currently no specific guidelines for screening migraine and associated psychiatric conditions. However, our study highlights the importance of a wider clinical role for screenings of comorbid migraine and suicidal ideation. Migraine patients would benefit from routine screening for depression and suicidal ideation. Therefore, clinicians should have a risk assessment protocol in place to identify and treat migraineurs at risk for suicidal ideation. A focus on migraine comorbidities, including suicidal behaviors, is important for diagnosis and effective treatment of these disorders.
Supplementary Material
Acknowledgments
This research was supported by awards from the National Institutes of Health (NIH), National Institute of Minority Health and Health Disparities (T37-MD-001449) and Eunice Kennedy Shriver Institute of Child Health and Human Development (R01-HD-059835). The NIH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
References
- 1.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 2.Lipton R, Bigal M, Diamond M, Freitag F, Reed M, Stewart W, Group AA. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343–349. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 3.Steiner T, Scher A, Stewart W, Kolodner K, Liberman J, Lipton R. The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity. Cephalalgia. 2003;23:519–527. doi: 10.1046/j.1468-2982.2003.00568.x. [DOI] [PubMed] [Google Scholar]
- 4.Smitherman TA, Burch R, Sheikh H, Loder E. The prevalence, impact, and treatment of migraine and severe headaches in the United States: a review of statistics from national surveillance studies. Headache. 2013;53:427–436. doi: 10.1111/head.12074. [DOI] [PubMed] [Google Scholar]
- 5.Stovner LJ, Al Jumah M, Birbeck GL, Gururaj G, Jensen R, Katsarava Z, Queiroz LP, Scher AI, Tekle-Haimanot R, Wang SJ, Steiner TJ. The methodology of population surveys of headache prevalence, burden and cost: principles and recommendations from the Global Campaign against Headache. The Journal of Headache and Pain. 2014;15:5. doi: 10.1186/1129-2377-15-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcus D, Bhowmick A. Fibromyalgia comorbidity in a community sample of adults with migraine. Clinical Rheumatology. 2013;32:1553–1556. doi: 10.1007/s10067-013-2310-7. [DOI] [PubMed] [Google Scholar]
- 7.Nye B, Thadani V. Migraine and epilepsy: review of the literature. Headache. 2015;55:359–380. doi: 10.1111/head.12536. [DOI] [PubMed] [Google Scholar]
- 8.Harriott A, Barrett K. Dissecting the association between migraine and stroke. Current Neurology and Neuroscience Reports. 2015;15:5. doi: 10.1007/s11910-015-0530-8. [DOI] [PubMed] [Google Scholar]
- 9.Pakpoor J, Handel A, Giovannoni G, Dobson R, Ramagopalan S. Meta-analysis of the relationship between multiple sclerosis and migraine. PLoS One. 2012;7:e45295. doi: 10.1371/journal.pone.0045295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Breslau N, Schultz L, Stewart W, Lipton R, Welch K. Headache types and panic disorder: directionality and specificity. Neurology. 2001;56:350–354. doi: 10.1212/wnl.56.3.350. [DOI] [PubMed] [Google Scholar]
- 11.Moschiano F, D'Amico D, Canavero I, Pan I, Micieli G, Bussone G. Migraine and depression: common pathogenetic and therapeutic ground? Neurological Sciences. 2011;32(Suppl 1):S85–S88. doi: 10.1007/s10072-011-0545-0. [DOI] [PubMed] [Google Scholar]
- 12.Breslau N, Schultz L, Stewart W, Lipton R, Lucia V, Welch K. Headache and major depression: is the association specific to migraine? Neurology. 2000;54:308–313. doi: 10.1212/wnl.54.2.308. [DOI] [PubMed] [Google Scholar]
- 13.Peterlin B, Nijjar S, Tietjen G. Post-traumatic stress disorder and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51:860–868. doi: 10.1111/j.1526-4610.2011.01907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Breslau N. Migraine, suicidal ideation, and suicide attempts. Neurology. 1992;42:392–395. doi: 10.1212/wnl.42.2.392. [DOI] [PubMed] [Google Scholar]
- 15.Wang S, Juang K, Fuh J, Lu S. Psychiatric comorbidity and suicide risk in adolescents with chronic daily headache. Neurology. 2007;68:1468–1473. doi: 10.1212/01.wnl.0000260607.90634.d6. [DOI] [PubMed] [Google Scholar]
- 16.Wang S, Fuh J, Juang K, Lu S. Migraine and suicidal ideation in adolescents aged 13 to 15 years. Neurology. 2009;72:1146–1152. doi: 10.1212/01.wnl.0000345362.91734.b3. [DOI] [PubMed] [Google Scholar]
- 17.Ratcliffe G, Enns M, Belik S, Sareen J. Chronic pain conditions and suicidal ideation and suicide attempts: an epidemiologic perspective. Clinical Journal of Pain. 2008;24:204–210. doi: 10.1097/AJP.0b013e31815ca2a3. [DOI] [PubMed] [Google Scholar]
- 18.Fuller-Thomson E, Hamelin G, Granger S. Suicidal ideation in a population-based sample of adolescents: implications for family medicine practice. ISRN Family Medicine. 2013;2013:282378. doi: 10.5402/2013/282378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colman I, Kingsbury M, Sareen J, Bolton J, Walraven CV. Migraine headache and risk of self-harm and suicide: A population-based study in Ontario, Canada. Headache. 2016;56:132–140. doi: 10.1111/head.12710. [DOI] [PubMed] [Google Scholar]
- 20.Singhal A, Ross J, Seminog O, Hawton K, Goldacre M. Risk of self-harm and suicide in people with specific psychiatric and physical disorders: comparisons between disorders using English national record linkage. Journal of the Royal Society of Medicine. 2014;107:194–204. doi: 10.1177/0141076814522033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breslau N, Schultz L, Lipton R, Peterson E, Welch K. Migraine headaches and suicide attempt. Headache. 2012;52:723–731. doi: 10.1111/j.1526-4610.2012.02117.x. [DOI] [PubMed] [Google Scholar]
- 22.Ilgen M, Kleinberg F, Ignacio R, Bohnert A, Valenstein M, McCarthy J, Blow F, Katz I. Noncancer pain conditions and risk of suicide. JAMA Psychiatry. 2013;70:692–697. doi: 10.1001/jamapsychiatry.2013.908. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. Preventing suicide: a global imperative. 2014 [Google Scholar]
- 24.Hawton K, Casanas I, Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. Journal of Affective Disorders. 2013;147:17–28. doi: 10.1016/j.jad.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Tang NK, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychol Med. 2006;36:575–586. doi: 10.1017/S0033291705006859. [DOI] [PubMed] [Google Scholar]
- 26.Nock M, Borges G, Bromet E, Cha C, Kessler R, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turecki G, Brent DA. Suicide and suicidal behaviour. The Lancet. 2016;387:1227–1239. doi: 10.1016/S0140-6736(15)00234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moher D, Liberati A, Tetzlaff J, Altman D, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International Journal of Surgery. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 29.Herzog R, Alvarez-Pasquin M, Diaz C, Barrio JD, Estrada J, Gil A. Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Montagna P. Molecular genetics of migraine headaches: a review. Cephalalgia. 2000;20:3–14. doi: 10.1046/j.1468-2982.2000.00003.x. [DOI] [PubMed] [Google Scholar]
- 31.Rot Mah, Mathew S, Charney D. Neurobiological mechanisms in major depressive disorder. Canadian Medical Association Journal. 2009;180:305–313. doi: 10.1503/cmaj.080697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mandelli L, Serretti A. Gene environment interaction studies in depression and suicidal behavior: an update. Neuroscience & Biobehavioral Reviews. 2013;37:2375–2397. doi: 10.1016/j.neubiorev.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 33.Serafini G, Pompili M, Innamorati M, Gentile G, Borro M, Lamis DA, Lala N, Negro A, Simmaco M, Girardi P, Martelletti P. Gene variants with suicidal risk in a sample of subjects with chronic migraine and affective temperamental dysregulation. Eur Rev Med Pharmacol Sci. 2012;16:1389–1398. [PubMed] [Google Scholar]
- 34.McGuffin P, Marušic A, Farmer A. What can psychiatric genetics offer suicidology? Crisis. 2001;22:61–65. doi: 10.1027//0227-5910.22.2.61. [DOI] [PubMed] [Google Scholar]
- 35.Hamel E. Serotonin and migraine: biology and clinical implications. Cephalalgia. 2007;27:1293–1300. doi: 10.1111/j.1468-2982.2007.01476.x. [DOI] [PubMed] [Google Scholar]
- 36.Baskin S, Smitherman T. Migraine and psychiatric disorders: comorbidities, mechanisms, and clinical applications. Neurological Sciences. 2009;30(Suppl 1):S61–S65. doi: 10.1007/s10072-009-0071-5. [DOI] [PubMed] [Google Scholar]
- 37.Sullivan G, Oquendo M, Milak M, Miller J, Burke A, Ogden R, Parsey R, Mann J. Positron emission tomography quantification of serotonin(1A) receptor binding in suicide attempters with major depressive disorder. JAMA Psychiatry. 2015;72:169–178. doi: 10.1001/jamapsychiatry.2014.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peroutka S, Price S, Wilhoit T, Jones K. Comorbid migraine with aura, anxiety, and depression is associated with dopamine D2 receptor (DRD2) NcoI alleles. Molecular medicine (Cambridge, Mass) 1998;4:14–21. [PMC free article] [PubMed] [Google Scholar]
- 39.Peterlin B, Katsnelson M, Calhoun A. The associations between migraine, unipolar psychiatric comorbidities, and stress-related disorders and the role of estrogen. Current Pain and Headache Reports. 2009;13:404–412. doi: 10.1007/s11916-009-0066-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim J, Stewart R, Kim S, Yang S, Shin I, Kim Y, Yoon J. Interactions between life stressors and susceptibility genes (5-HTTLPR and BDNF) on depression in Korean elders. Biological Psychiatry. 2007;62:423–428. doi: 10.1016/j.biopsych.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 41.Giletta M, Calhoun C, Hastings P, Rudolph K, Nock M, Prinstein M. Multi-Level Risk Factors for Suicidal Ideation Among at-Risk Adolescent Females: The Role of Hypothalamic-Pituitary-Adrenal Axis Responses to Stress. Journal of Abnormal Child Psychology. 2015;43:807–820. doi: 10.1007/s10802-014-9897-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burstein R, Jakubowski M. Neural substrate of depression during migraine. Neurological Sciences. 2009;30(Suppl 1):S27–S31. doi: 10.1007/s10072-009-0061-7. [DOI] [PubMed] [Google Scholar]
- 43.Yu D, Yuan K, Zhao L, Liang F, Qin W. Regional homogeneity abnormalities affected by depressive symptoms in migraine patients without aura: a resting state study. PLoS One. 2013;8:e77933. doi: 10.1371/journal.pone.0077933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pandey G. Biological basis of suicide and suicidal behavior. Bipolar Disorders. 2013;15:524–541. doi: 10.1111/bdi.12089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ilgen MA, Zivin K, McCammon RJ, Valenstein M. Pain and suicidal thoughts, plans and attempts in the United States. Gen Hosp Psychiatry. 2008;30:521–527. doi: 10.1016/j.genhosppsych.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nicholson R, Houle T, Rhudy J, Norton P, Montagna P. Psychological Risk Factors in Headache. Headache. 2007;47:413–426. doi: 10.1111/j.1526-4610.2006.00716.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abbate-Daga G, Fassino S, Lo Giudice R, Rainero I, Gramaglia C, Marech L, Amianto F, Gentile S, Pinessi L. Anger, depression and personality dimensions in patients with migraine without aura. Psychotherapy and Psychosomatics. 2007;76:122–128. doi: 10.1159/000097971. [DOI] [PubMed] [Google Scholar]
- 48.Heath RL, Saliba M, Mahmassani O, Major SC, Khoury BA. Locus of control moderates the relationship between headache pain and depression. The Journal of Headache and Pain. 2008;9:301–308. doi: 10.1007/s10194-008-0055-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Novic A, Kolves K, O'Dwyer S, De Leo D. Migraine and Suicidal Behaviors: A Systematic Literature Review. Clinical Journal of Pain. 2016;32:351–364. doi: 10.1097/AJP.0000000000000256. [DOI] [PubMed] [Google Scholar]
- 50.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, Chiu WT, Girolamo Gd, Gluzman S, Graaf Rd, Gureje O, Haro JM, Huang Y, Karam E, Kessler RC, Lepine JP, Levinson D, Medina-Mora ME, Ono Y, Posada-Villa J, Williams DR. Cross-National Prevalence and Risk Factors for Suicidal Ideation, Plans, and Attempts. The British Journal of Psychiatry. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Juang K, Yang C. Psychiatric comorbidity of chronic daily headache: focus on traumatic experiences in childhood, post-traumatic stress disorder and suicidality. Current Pain and Headache Reports. 2014;18:405. doi: 10.1007/s11916-014-0405-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.