Abstract
Background The extent to which intracranial venous sinus obstruction contributes to idiopathic intracranial hypertension (IIH) is debated. The extent to which extracranial venous obstruction contributes to IIH is virtually unexplored. This article describes an interventional approach to extracranial venous outflow in a group of patients with severe intractable symptoms.
Objective To describe our technique and experience of styloidectomy combined with jugular stenting in the treatment of skull base narrowing of the jugular veins.
Methods Retrospective review of all styloidectomies undertaken at our institution (n = 34), as an adjunct or alternative to jugular venous stenting, with a view to improving cranial venous outflow.
Results Eleven styloidectomies were for delayed complications of jugular stenting. Of seven with stent dysfunction, three were improved and four unchanged. Of seven with accessory nerve compression (three had both), four resolved and three improved. In 23 instances, styloidectomy preceded or obviated jugular stenting. Two had a virtual resolution of symptoms, 13 were improved, and 8 were unchanged.
Conclusion Styloidectomy can replace, salvage, or complement jugular venous stenting in IIH and disturbances of cranial venous outflow.
Keywords: styloidectomy, jugular stenting, idiopathic intracranial hypertension, cranial venous outflow
Introduction
Idiopathic intracranial hypertension (IIH), a headache disorder that can give rise to severe symptoms, including visual loss, is defined by the presence of raised intracranial pressure and the absence of any known cause.1 2 Several etiological mechanisms have been proposed1 3 but the notion that cranial venous outflow obstruction is implicated has gained credence with studies showing raised intracranial venous pressures upstream of stenoses in the transverse sinuses.4 5 There is debate over whether these stenoses are the cause of raised intracranial pressure or the consequence of it. Nevertheless, the response of patients to venous sinus stenting suggests they are important.6 7 8 9 10 11
Although the most striking venous pressure gradients in patients with IIH are found at the junction between the transverse and sigmoid sinuses, smaller gradients are usually present elsewhere along cerebral venous outflow,4 5 the significance of which have not been seriously considered. Where these other gradients are intracranial the question over whether they are primary or secondary is unresolved. Where they are extracranial this question does not arise. Instead, it becomes one of how a small extracranial venous pressure gradient might be responsible for a large increase in intracranial pressure. Is it possible that jugular venous narrowing, for example, can initiate a cycle of raised intracranial pressure that is magnified in feedback by secondary narrowing of the transverse sinuses?
The response of patients with milder forms of IIH to jugular venoplasty suggests that this is an area that would merit further research.12 Moreover, recently there has been a report of two cases of IIH caused by jugular stenoses just below the skull base which were treated by jugular stenting in combination with styloidectomy.13 In both cases, the jugular veins were pinched between the styloid processes and lateral masses of C1 and styloidectomy was performed with the aim of making space for a stent.
Using catheter venography, venoplasty, and stenting, we have been exploring the role of jugular venous narrowing at this site in IIH12 and also in other conditions in which a nonmalignant and noninfective disturbance of intracranial pressure is likely an important part of the underlying pathology.12 14 The anatomy in these cases frequently shows the jugular veins flattened and narrowed between the styloid processes and the lateral masses of C1, these narrowings associated with small pressure gradients. Stenting would seem an obvious solution to this problem but sometimes there is insufficient space in which to place a stent, a situation where styloidectomy might be expected to be of value.
In this article, we present preliminary data regarding the safety and efficacy of styloidectomy performed in pursuit of improving cranial venous outflow.
Patients and Methods
The case notes of all patients (n = 29) who have had styloidectomy at our institution as part of a strategy to improve cranial venous outflow were reviewed by two of the authors (J. N. H. and P. R. A.). Most patients had IIH but there were several other diagnoses and some patients had more than one diagnosis (Table 1). All patients had disabling symptoms—often multiple but usually including severe headache—unresponsive to medical treatment with a mean length of history of 9 years, range 1 to 32 years. Most had had previous surgical procedures, some at other institutions (Table 2). Many patients had been investigated extensively during the course of their illness, including with cerebrospinal fluid (CSF) infusion studies or intracranial pressure monitoring.
Table 1. Diagnoses in the whole group of 29 patients.
| Diagnoses | N |
|---|---|
| IIH | 12 |
| Borderline IIHa | 9 |
| Cerebrospinal fluid leak or brain slump | 4 |
| Chiari I deformity | 4 |
| Hydrocephalus | 3 |
| Encephalocele | 3 |
| Chronic venous sinus thrombosis | 2 |
Abbreviation: IIH, idiopathic intracranial hypertension.
Intracranial pressure within normal limits but symptoms responsive to lumbar puncture.
Table 2. Previous surgical procedures in the patient group.
| Procedures | N |
|---|---|
| Intracranial stents | 12 |
| CSF diversion procedures | 7 |
| Foramen magnum decompressions | 4 |
| Encephalocele repairs | 3 |
| Gastric banding | 1 |
| Miscellaneous external ear operations | 1 |
Abbreviation: CSF, cerebrospinal fluid.
At our institution, previous tests were supplemented by an investigation of cranial venous outflow and the decision to address jugular venous narrowing made on a case by case basis taking into account the severity of the narrowing depicted on computed tomography, the pressure gradient recorded on catheter venography and the clinical response to a trial of jugular venoplasty.
Styloidectomies were performed in two situations, both in recognition of the particular anatomy constraining the jugular vein.
“Rescue styloidectomy” to resolve particular complications of jugular stenting, either accessory nerve compression or stent compromise.
“Primary styloidectomy” where jugular stenting was planned but styloidectomy was performed in advance because the space between the styloid process and the lateral mass of C1 was so restricted that the complications described above were considered likely.
Outcomes were assessed by consensus between the authors regarding a patient's condition in the follow-up period between styloidectomy (with or without jugular stenting) and their last clinic review or up to the point at which they had a further procedure (e.g., a shunt change), an average of 14 months (range, 1–39 months).
Styloidectomy Procedure
The following surgical technique describes an approach that removes the styloid process at its base.
The procedure is performed under general anesthesia using continuous intraoperative facial nerve monitoring. The patient is laid in a supine position with head slightly extended and turned away to the contralateral side. A postauricular incision is extended forward in front of the mastoid tip and then inferiorly into the neck avoiding the path of the marginal mandibular branch of the facial nerve. The anterior border of the sternocleidomastoid muscle is dissected free up to and in front of the mastoid tip. Further dissection medially through the deep cervical fascia toward the carotid sheath enables identification of the posterior belly of the digastric. Palpation of the inferior wound identifies the bony lateral mass of the C1 vertebra and further dissection superoanteromedially above the posterior belly of the digastric will bring you high onto the body of the styloid process.
Blunt dissection of the base of the styloid process above the inferior extent of the mastoid tip confirms its origin. Two small malleable retractors can be inserted in front and behind the styloid process so giving secure anchorage to hold the soft tissue from its surface. A 2 mm course cut diamond burr is used gently to create a hole that can be widened in an anteroposterior direction to drill across its diameter. Bone is removed until its medial extent is egg shelled. At this point the whole of the styloid process becomes mobile. A House bone curette is used to draw the base of the styloid process laterally until it can be safely held using a curved Spencer Wells forceps. An ophthalmic microsurgical blade is then used to gently strip the muscle attachments from its surface in an inferior direction while drawing the styloid laterally. The stylohyoid ligament is divided using scissors and the styloid process removed. Hemostasis is confirmed and a suction drain inserted. The wound is closed in layers.
Results
Overall, 29 patients (male to female ratio, 15:14; mean age, 45 years; range, 22–66 years) have had 34 styloidectomies. Three patients had a second styloidectomy on the contralateral side after the first produced a partial response. Two patients had repeat procedures on the same side after an inadequate excision on the first occasion.
Clinical Outcomes
Rescue Styloidectomy
Rescue styloidectomy was undertaken on 11 occasions. Four for shoulder weakness and discomfort, four for stent compromise and three for both. Shoulder weakness was taken to represent accessory nerve compression (and confirmed by electromyography in four cases). Stent compromise took the form, either of visible damage to the stent, or visible constriction of the stent between the styloid process and lateral mass of C1, or of intimal thickening inside the stent at the equivalent level, or a combination (Fig. 1).
Fig. 1.
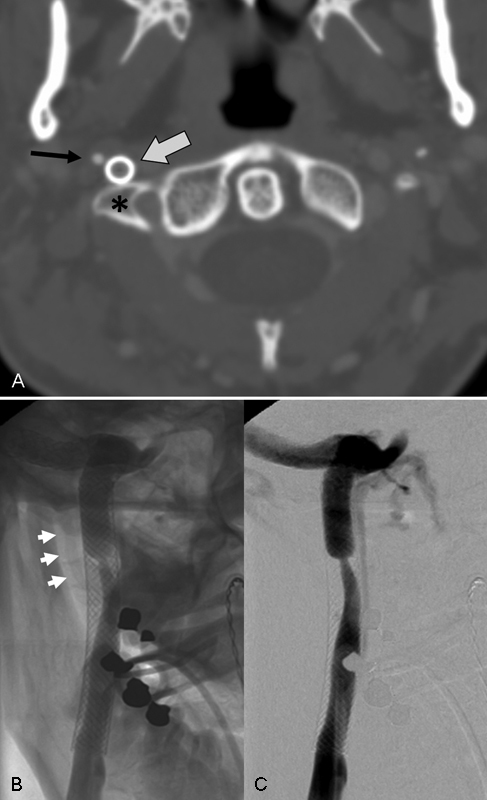
In-stent narrowing, presumed from intermittent compression between styloid process and lateral mass of C1: (A) Axial CT scan showing the styloid process (simple arrow) in close proximity to the lateral mass of C1 (asterisk) with the stent (block arrow) in between. Unsubtracted (B) and subtracted (C) frontal films during catheter venogram showing narrowing of the vascular lumen inside the jugular stent at the same level (arrowheads = styloid process). CT, computed tomography.
All patients with shoulder weakness/accessory nerve compression derived benefit from the procedure, this sometimes apparent immediately postoperatively, at other times emerging gradually over weeks or months (Table 3). In cases where styloidectomy was performed for stent compromise (Table 4), further endovascular procedures (angioplasty) were usually undertaken to attempt to re-establish a normal stent configuration or adequate vascular lumen, with limited success. These procedures are ongoing.
Table 3. Rescue styloidectomy for accessory nerve dysfunction.
| Outcome | N |
|---|---|
| Symptoms resolved | 4 |
| Symptoms improved | 3 |
Table 4. Rescue styloidectomy for stent compromise.
| Outcome | N |
|---|---|
| Stent configuration improved | 3 |
| Stent configuration unchanged | 4 |
Primary Styloidectomy
Primary styloidectomy was undertaken on 23 occasions in the expectation that it would be followed by jugular stenting (Fig. 2). In some instances, however, the clinical improvement was so impressive that stenting was no longer considered necessary. In other instances there has been no, or only minimal improvement and follow-up stenting is yet to be arranged. Most patients had follow-up stenting and most of these were improved afterward (Fig. 3). Stenting in these cases was usually performed 2 months or more after styloidectomy. In three instances internal jugular vein stenting was combined with intracranial stenting. In no case did styloidectomy adversely affect the jugular vein.
Fig. 2.
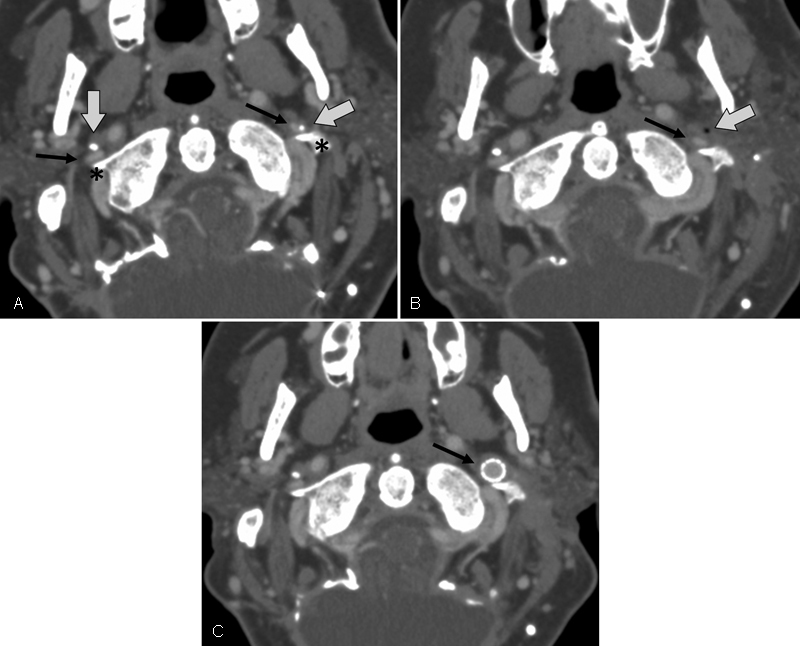
Primary styloidectomy followed by stenting: Axial CT scan after intravenous contrast at the C1 level show (A) the jugular veins (simple arrows) narrowed between the styloid processes (block arrows) and lateral masses of C1 (asterisks). (B) Following styloidectomy there is a locule of air at the site of resection (block arrow). (C) Following stenting the stent (simple arrow) dilates the internal jugular vein. CT, computed tomography.
Fig. 3.
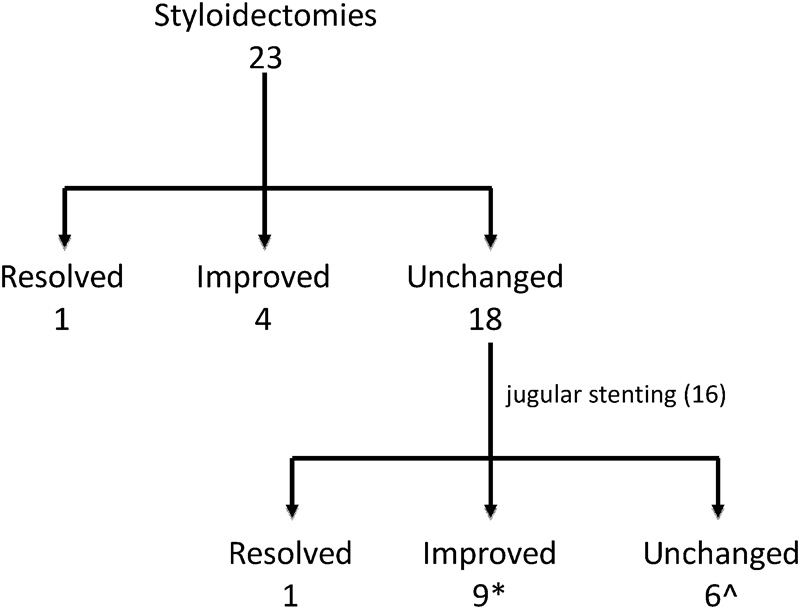
Schematic of clinical outcomes of 23 primary styloidectomies and follow-up jugular stentings. After styloidectomy symptoms virtually resolved in 1 case (resolved), improved to such an extent in 4 cases that no further treatment was contemplated (improved) and were unchanged or only minimally improved in 18 (unchanged). Of these 16 cases were stented. In one case, symptoms virtually resolved. In nine they were improved and in six unchanged. Some patients in these last two categories, on this level, had further procedures. *One patient in this group had contemporaneous ipsilateral sigmoid sinus and jugular stentings ^Two patients in this group had contemporaneous transverse sinus and jugular stentings. One had a fatal postoperative subdural hemorrhage.
Complications of Styloidectomy
One patient had a wound infection. One had a postoperative hematoma requiring exploration. One patient awoke with mild facial weakness, which resolved within 24 hours. One patient awoke with dysphasia (after a left styloidectomy), which resolved after a few hours, was unexplained and not accompanied by any evidence of cerebral damage on imaging. One patient awoke with a hemiparesis ipsilateral to the side of surgery. This was also unexplained and resolved quickly except that she was left with shoulder weakness. This is being investigated and probably represents accessory nerve injury. There were no deaths from styloidectomy (Table 5). One patient who had had styloidectomy 6 months previously, died from an acute posterior fossa subdural hemorrhage after jugular stenting was combined with stenting of the transverse sinus.
Table 5. Complications of styloidectomy.
| Complications | N |
|---|---|
| Mortality | 0 |
| Permanent neurological deficit (accessory nerve palsy) | 1 |
| Transient neurological deficit (< 24 h) | 3 |
| Wound hematoma requiring re-exploration | 1 |
| Wound infection | 1 |
Discussion
Although jugular venous narrowing has been identified as a probable risk factor for cerebral venous sinus thrombosis,15 the question of whether jugular narrowing is important in IIH, or in the other conditions considered in this article, is virtually unexplored.13 Our results, however, in which 15 of 23 patients undergoing styloidectomy as the initial procedure for jugular narrowing at the skull base had a clinical benefit (Fig. 3) suggest that this is an area worth further study. Moreover, the observation that most of those who benefited only did so after subsequent jugular stenting reinforces the notion that it is a venous obstruction that is responsible for symptoms and suggests that these procedures will often need to be combined to be effective.
A combined approach, of course, adds complexity to a problem that might be resolved by stenting alone but, in effect, is no more than a concession to the usual anatomy in this region in which the jugular vein has to pass through a relatively confined space between two bony structures—namely, the styloid process and the lateral mass of C1—likely to interfere with the proper functioning of a stent. Moreover, our experience of primary stenting in this situation is that stent dysfunction from external compression is difficult to resolve even when styloidectomy is performed subsequently (Table 4).
Regarding endovascular treatment of IIH, the venous narrowings that have received most attention have been those found at the junction between the transverse and sigmoid sinuses. These narrowings can often be reversed by CSF drainage, however,6 and our experience of stenting them has been that, although there is often symptomatic improvement, there is rarely a cure and often subsequent partial regression, this fueling the idea that they may not be the primary pathology and prompting a search for the index lesion.9
Narrowing of the jugular veins below the skull base is not an uncommon finding in routine clinical practice.16 So, it is difficult to connect such appearances with particular symptoms or syndromes. Catheter venography with pressure manometry will establish whether these narrowings are associated with pressure gradients.4 5 The clinical response to venoplasty might be an indicator of their clinical significance.12 The absence of normative data, however, makes the significance of any pressure gradient or response to venoplasty difficult to evaluate.
These caveats accepted, the report of two cases of IIH caused by jugular stenoses at the C1 level and, more recently, of another patient with brain slump treated purely by stenting the internal jugular veins are pertinent.13 14 The observations on primary styloidectomy we present in this article are similarly uncontrolled. Nevertheless, they lend weight to the idea that jugular venous narrowing should not be ignored.
Styloidectomy is a long-established procedure in the treatment of Eagle syndrome, a condition in which an elongated styloid process is thought to be responsible for pain and discomfort in the throat.17 18 Sometimes the styloid impinges on the carotid artery which may lead to stroke.19 What we are seeing here, however, is a variant in which the styloid process is not necessarily elongated but is orientated in such a way that its proximal segment impresses on the jugular vein. This has a significant bearing on the styloidectomy procedure, itself, often necessitating resection of the styloid process right up to its point of insertion into the skull base. Between the two traditional surgical approaches, therefore, transoral and transcervical,18 20 21 which only allow access to its lower segments and leave a sizeable remnant behind, we have modified the transcervical approach to give sufficient exposure to the area of interest. This may increase the risk facial nerve injury. Nevertheless, our results are the encouragement that this form of styloidectomy is possible with reasonable outcomes and an acceptable complication rate.
Six patients did not improve after styloidectomy and jugular stenting. This might raise questions about the disease model (cranial venous outflow obstruction) on which the treatment approach is based. One patient in whom treatment was successful, however, required combined procedures on both sides before a lasting result was achieved. Another had a partial response to treatment on one side, then experienced further improvement after treatment to the other. If cranial venous outflow obstruction is the underlying problem, therefore, treatment may need to be directed at several sites before it begins to have a clinical effect.
Conclusions
Extended styloidectomy can replace, salvage, or complement stenting of the upper jugular vein in the treatment of idiopathic intracranial hypertension and disturbances of cranial venous outflow, the results suggesting that jugular venous narrowing in these conditions may be more important than previously recognized.
References
- 1.Johnston I, Owler B, Pickard J. Cambridge, United Kingdom: Cambridge University Press; 2007. The Pseudotumor Cerebri Syndrome. [Google Scholar]
- 2.Friedman D I, Jacobson D M. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59(10):1492–1495. doi: 10.1212/01.wnl.0000029570.69134.1b. [DOI] [PubMed] [Google Scholar]
- 3.Fishman R A. The pathophysiology of pseudotumor cerebri. An unsolved puzzle. Arch Neurol. 1984;41(3):257–258. doi: 10.1001/archneur.1984.04050150035011. [DOI] [PubMed] [Google Scholar]
- 4.King J O, Mitchell P J, Thomson K R, Tress B M. Cerebral venography and manometry in idiopathic intracranial hypertension. Neurology. 1995;45(12):2224–2228. doi: 10.1212/wnl.45.12.2224. [DOI] [PubMed] [Google Scholar]
- 5.Karahalios D G, Rekate H L, Khayata M H, Apostolides P J. Elevated intracranial venous pressure as a universal mechanism in pseudotumor cerebri of varying etiologies. Neurology. 1996;46(1):198–202. doi: 10.1212/wnl.46.1.198. [DOI] [PubMed] [Google Scholar]
- 6.King J O, Mitchell P J, Thomson K R, Tress B M. Manometry combined with cervical puncture in idiopathic intracranial hypertension. Neurology. 2002;58(1):26–30. doi: 10.1212/wnl.58.1.26. [DOI] [PubMed] [Google Scholar]
- 7.Owler B K, Parker G, Halmagyi G M. et al. Cranial venous outflow obstruction and pseudotumor Cerebri syndrome. Adv Tech Stand Neurosurg. 2005;30:107–174. doi: 10.1007/3-211-27208-9_4. [DOI] [PubMed] [Google Scholar]
- 8.Higgins J N Owler B K Cousins C Pickard J D Venous sinus stenting for refractory benign intracranial hypertension Lancet 2002359(9302):228–230. [DOI] [PubMed] [Google Scholar]
- 9.Higgins J N, Cousins C, Owler B K, Sarkies N, Pickard J D. Idiopathic intracranial hypertension: 12 cases treated by venous sinus stenting. J Neurol Neurosurg Psychiatry. 2003;74(12):1662–1666. doi: 10.1136/jnnp.74.12.1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmed R M, Wilkinson M, Parker G D. et al. Transverse sinus stenting for idiopathic intracranial hypertension: a review of 52 patients and of model predictions. AJNR Am J Neuroradiol. 2011;32(8):1408–1414. doi: 10.3174/ajnr.A2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puffer R C, Mustafa W, Lanzino G. Venous sinus stenting for idiopathic intracranial hypertension: a review of the literature. J Neurointerv Surg. 2013;5(5):483–486. doi: 10.1136/neurintsurg-2012-010468. [DOI] [PubMed] [Google Scholar]
- 12.Higgins N Pickard J Lever A What do lumbar puncture and jugular venoplasty say about a connection between chronic fatigue syndrome and idiopathic intracranial hypertension? EJMINT Original Article 20141.448000223E9 (24 November 2014) [PMC free article] [PubMed] [Google Scholar]
- 13.Dashti S R, Nakaji P, Hu Y C. et al. Styloidogenic jugular venous compression syndrome: diagnosis and treatment: case report. Neurosurgery. 2012;70(3):E795–E799. doi: 10.1227/NEU.0b013e3182333859. [DOI] [PubMed] [Google Scholar]
- 14.Higgins N, Trivedi R, Greenwood R, Pickard J. Brain slump caused by jugular venous stenoses treated by stenting: a hypothesis to link spontaneous intracranial hypotension with idiopathic intracranial hypertension. J Neurol Surg Rep. 2015;76(1):e188–e193. doi: 10.1055/s-0035-1555015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jia L Y, Hua Y, Ji X M, Liu J T. Correlation analysis of internal jugular vein abnormalities and cerebral venous sinus thrombosis. Chin Med J (Engl) 2012;125(20):3671–3674. [PubMed] [Google Scholar]
- 16.Diehn F E, Schwartz K M, Hunt C H. et al. Prevalence of incidental narrowing of the superior segment of the internal jugular vein in patients without multiple sclerosis. Clin Neuroradiol. 2014;24(2):121–127. doi: 10.1007/s00062-013-0232-z. [DOI] [PubMed] [Google Scholar]
- 17.Eagle W W. Elongated styloid process: Report of two cases. Arch Otolaryngol. 1937;25(5):584–587. doi: 10.1001/archotol.1949.03760110046003. [DOI] [PubMed] [Google Scholar]
- 18.Ceylan A, Köybaşioğlu A, Celenk F, Yilmaz O, Uslu S. Surgical treatment of elongated styloid process: experience of 61 cases. Skull Base. 2008;18(5):289–295. doi: 10.1055/s-0028-1086057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.David J, Lieb M, Rahimi S A. Stylocarotid artery syndrome. J Vasc Surg. 2014;60(6):1661–1663. doi: 10.1016/j.jvs.2014.05.048. [DOI] [PubMed] [Google Scholar]
- 20.Strauss M, Zohar Y, Laurian N. Elongated styloid process syndrome: intraoral versus external approach for styloid surgery. Laryngoscope. 1985;95(8):976–979. [PubMed] [Google Scholar]
- 21.Chase D C, Zarmen A, Bigelow W C, McCoy J M. Eagle's syndrome: a comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol. 1986;62(6):625–629. doi: 10.1016/0030-4220(86)90253-7. [DOI] [PubMed] [Google Scholar]


