Abstract
An impaired ability to suppress currently irrelevant mental-sets is a key cognitive deficit in depression. Mindfulness-based cognitive therapy (MBCT) was specifically designed to help depressed individuals avoid getting caught in such irrelevant mental-sets. In the current study, a group assigned to MBCT plus treatment-as-usual (n = 22) exhibited significantly lower depression scores and greater improvements in irrelevant mental-set suppression compared to a wait-list plus treatment-as-usual (n = 18) group. Improvements in mental-set-suppression were associated with improvements in depression scores. Results provide the first evidence that MBCT can improve suppression of irrelevant mental-sets and that such improvements are associated with depressive alleviation.
Electronic supplementary material
The online version of this article (doi:10.1007/s00406-016-0746-x) contains supplementary material, which is available to authorized users.
Keywords: Mindfulness-based cognitive therapy, Depression, Mental-set, Competitor rule suppression
Introduction
Depression is a leading cause of disability and one of the most common mental disorders [1]. It is characterized by impaired ability to suppress competing or currently irrelevant mental-sets [2–8], such as distracting ruminative thoughts. Impairments in mental-set suppression have been found to predict onset and recurrence of depression, correlate with depressive rumination [9, 10], and mediate symptom severity [4, 11]. However, little is known about whether or how suppression impairments can be improved and if this would affect depressive symptomatology. This study aims to determine whether mindfulness training can improve mental-set suppression and whether such improvement is associated with depressive alleviation.
Mindfulness-based cognitive therapy (MBCT) specifically targets avoiding getting caught in ruminative mental-sets [12–14] and can prevent depressive relapse [13, 15]. While mindfulness training can improve cognitive functioning [16] including mental-set suppression [17–19] primarily among healthy adults, cognition improvements among depressed individuals remain largely unexplored.
The current study focuses on Competitor Rule Suppression CRS [20] as a measure of mental-set suppression. CRS refers to suppression of mental-sets which implicate a response that competes with the correct or currently relevant response (for example, suppressing self-critical thoughts of giving up rather than staying focused on a difficult task). CRS specifically counters “troublemaking” irrelevant mental-sets by tagging them in episodic memory as “to-be-suppressed” [21], thus facilitating adherence to current task demands. CRS is measured within a task-switching paradigm [22, 23], in which the context and task requirements are in constant flux. This design permits examination of dynamic fine-tuning of suppression processes [20, 24, 25], rather than more crude and consistent suppression of a single process or stimulus seen in other suppression measures such as the Stroop [20, 26]. We hypothesized that MBCT will improve CRS and that such improvements will be linked to depressive symptom reduction.
Methods
Participants
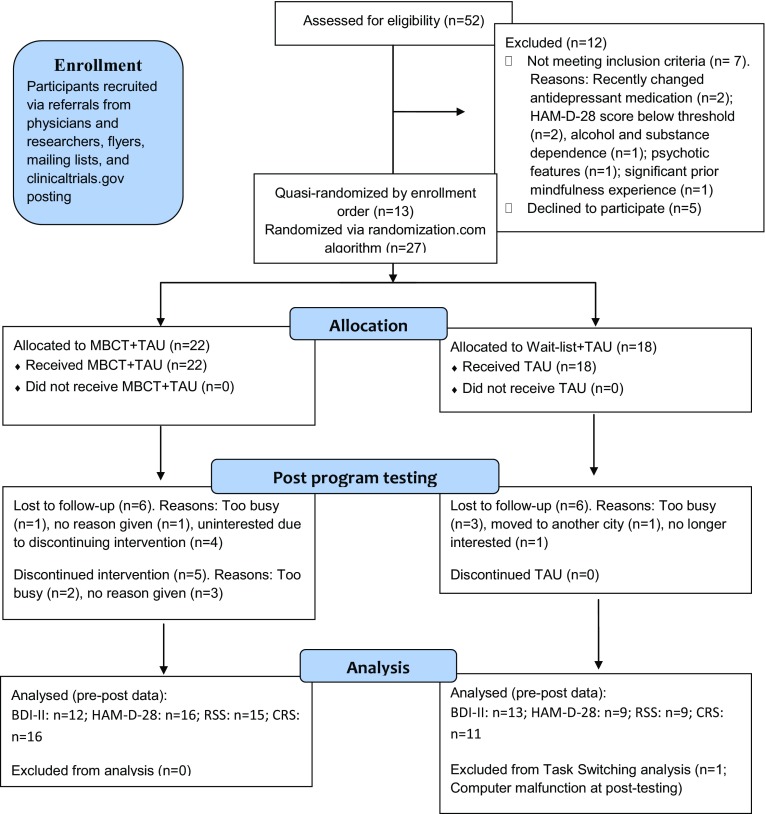
Fifty-two participants with mild to severe depression were recruited (Fig. 1). Inclusion criteria included a score of ≥11 on the 28-item Hamilton Depression Scale (HAM-D-28; [27]), dysphoria or low mood for at least two months prior, no history of substance dependence or abuse, psychotic features, or suicidal attempts in the past six months, and no prior experience with systematic mindfulness programs. Antidepressants were allowed only if doses were stable for ≥6 weeks. Forty participants were assigned to MBCT + treatment-as-usual (TAU) or wait-list + TAU. The first 13 participants were quasi-randomized and assigned in order of enrollment. Following an increase in recruitment, the next 27 participants were randomized after completing baseline testing. Groups were statistically equivalent in age (t(38) = 0.69, ns) and gender, meeting MDD criteria, and having a comorbid anxiety condition (minimal p = 0.44; Fisher’s exact test; Table 1). The study was approved by the Massachusetts General Hospital’s Institutional Review Board and registered at clinicaltrials.gov (NCT02457936).
Fig. 1.
Participant flow
Table 1.
Baseline demographic and clinical characteristics of participants (all baseline group differences are nonsignificant; minimal p = 0.49)
| MBCT + TAU | Wait-list + TAU | |
|---|---|---|
| Gender | 59% Women | 66% Women |
| Age | ||
| Mean | 39.77 | 36.89 |
| SD | 10.6 | 15.83 |
| BDI-II score | ||
| Mean | 23.51 | 22.18 |
| SD | 7.09 | 9.39 |
| HAM-D-28 score | ||
| Mean | 22.80 | 24.00 |
| SD | 8.62 | 6.34 |
| Meeting major depressive disorder criteria (%) | 86 | 72 |
| Comorbid anxiety disorder (%) | 54 | 44 |
Mindfulness-based cognitive therapy program
The 8-week MBCT program was led by two MBCT teachers with 8–13 years experience of teaching mindfulness-based group programs and blind to the study’s hypotheses. The program followed the guidelines of Segal, Williams, and Teasdale [12].
Measures
Clinical measures
The Mini International Neuropsychiatric Interview [28] version 5.0.0 and the HAM-D-28; [27, 29] were administered by trained and certified psychiatrists and psychologists from Mass. General Hospital to assess inclusion criteria. The Beck Depression Inventory-II (BDI-II [30]) was administered 0–2 weeks prior to the MBCT program and every 2–3 weeks during the program to measure changes in depressive symptoms. The Rumination Response Scale was also administered. These data are detailed in the electronic supplementary material.
Competitor rule suppression
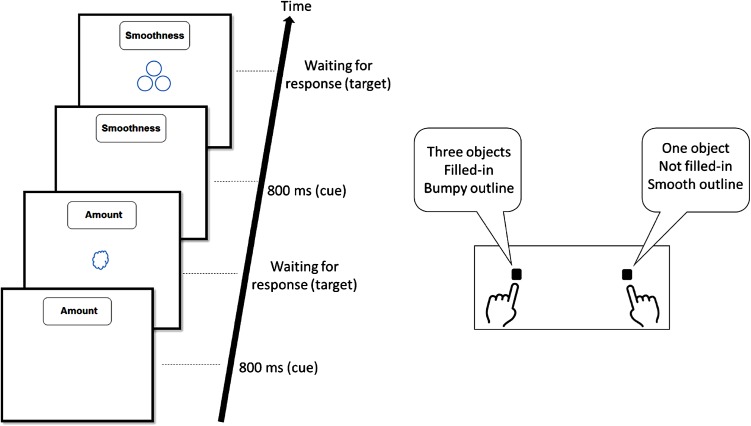
CRS was assessed via a task-switching paradigm based on [31] (Fig. 2). Briefly, a text-cue indicated which of three tasks was to be performed (“Amount” to indicate whether one or three objects are presented, “Filled-In” to indicate whether the object is filled with color or not, or “Smoothness” to indicate whether the object’s outline is smooth or bumpy). Tasks were presented in random order, with no repetition on two consecutive trials in order to maximize the number of CRS trials [19, 20]. Participants completed 20 practice trials, followed by three experimental blocks of 120 trials each. CRS was calculated by subtracting reaction time (RT) and error rates in trials in which the current rule was not the competing rule in the previous trial (non-CRS trials) from trials in which the current rule was the competing rule in the previous trial (CRS trials; [19–21, 32]; Fig. 2). RT analyses were performed on trials in which the current and last responses were correct. RT of over 3500 ms (ms) was excluded [19]. Information regarding Backward Inhibition, an additional measure assessed with the same task, is detailed in the electronic supplementary material.
Fig. 2.
Illustration of events in the task-switching paradigm. In the first presented trial, the relevant rule is “Amount” and correct answer is the right key. “Smoothness” in this trial is a conflicting rule as it indicates the left key as the correct response. CRS is evident by hampered performance (indicating rule suppression) when on the following trial the previously conflicting rule (“Smoothness”) becomes the relevant rule, as in the illustrated example
Procedure
Participants completed a phone screen, then signed the consent form, and underwent the MINI and the clinician-rated HAM-D-28 to assess eligibility. They then completed the CRS task, the BDI-II, and other measures outside the scope of this report. Testing procedures were repeated for all participants 0–3 weeks after the MBCT program. Clinical assessors were blind to group allocation.
Results
Depression scores
BDI-II
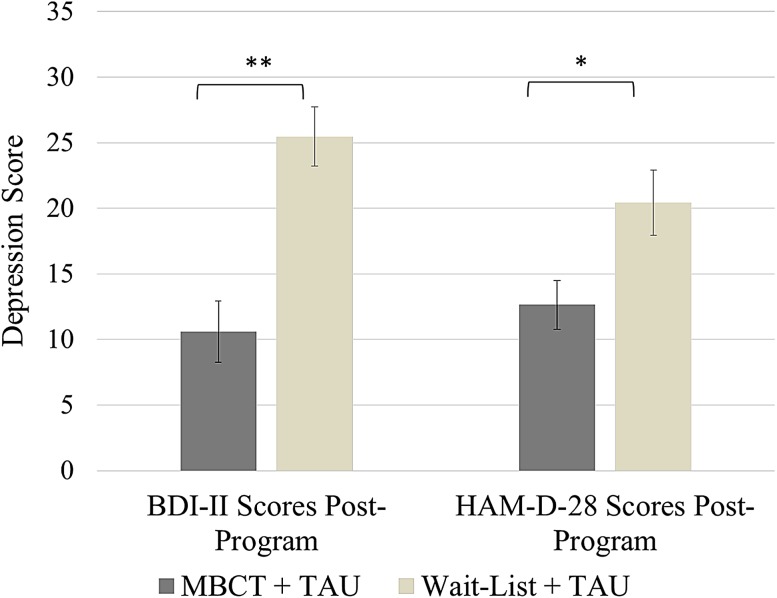
Groups had statistically equivalent BDI-II scores at baseline, both when examining all participants (t(36) = 0.50, ns) and participants with post-program data, (t(23) = 0.16, ns; Table 1). A one-way analysis of covariance (ANCOVA) with group as the independent variable conducted on post-program BDI-II scores while controlling for baseline BDI-II scores revealed a highly significant effect for group, with MBCT + TAU (M = 10.60, SD = 8.12) exhibiting lower BDI-II scores post-program than controls (M = 25.46, SD = 14.91; F(1,22) = 22.51, p < 0.001, η 2p = 0.505, 90% CI (0.23, 0.65); Fig. 3). BDI-II scores from week 6 were used for four participants who discontinued before post-testing. This effect remained highly significant after excluding these participants F(1,18) = 29.14, p < 0.001, η 2p = 0.618, 90% CI (0.33, 0.74).
Fig. 3.
ANCOVAs of BDI-II and HAM-D-28 scores post-program with baseline scores as covariates; **F(1,22) = 22.51, p < 0.001; *F(1,22) = 4.77, p < 0.05
HAM-D-28
Groups had statistically equivalent baseline HAM-D-28 scores, both when examining all participants t(35) = 0.47, ns (Table 1) and when examining only participants with post-program data (t(23) = 0.71, ns). ANCOVA conducted on post-program HAM-D-28 scores while controlling for baseline scores revealed a significant effect for group, with MBCT + TAU (M = 12.63, SD = 8.76) exhibiting lower HAM-D-28 scores post-program than wait-list + TAU (M = 20.44, SD = 6.35), F(1,22) = 4.77, p < 0.05, η 2p = 0.178, 90% CI (0.005, 0.39; Fig. 3).
CRS
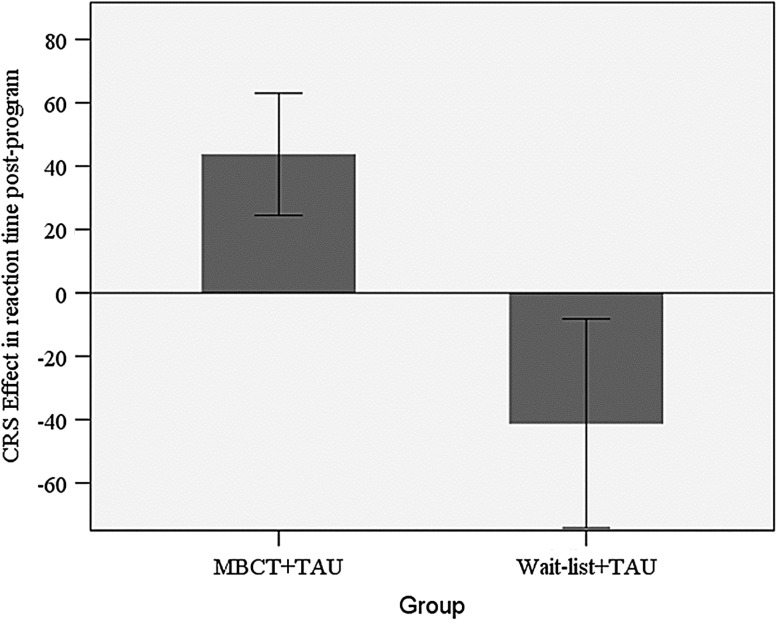
Groups were equivalent at baseline in reaction time (RT; t(38) = 0.36, ns) and error rates (t(38) = 1.00, ns) when including all participants and when including only participants with post-program data (maximal t(25) 1.38, ns). An ANCOVA with group as the independent variable conducted on post-program RT while controlling for baseline RT revealed a significant effect for group, with the MBCT + TAU group (M = 44 ms, SD = 77 ms) exhibiting an increased CRS effect compared to the control group (M = −41 ms, SD = 109 ms; F(1,24) = 6.13, p = 0.02, η 2p = 0.20, 90% CI (0.02, 0.40); Fig. 4). A similar ANCOVA conducted on post-program error rates while controlling for baseline error rates did not reach significance (F(1,24) = 1.57, ns).
Fig. 4.
ANCOVA of CRS in RT post-program with baseline scores as a covariate; *F(1,24) = 6.13, p = 0.02
The relationship between CRS and depressive symptoms
Multiple regression was used to predict change in BDI-II based on change in CRS error rates and RT. A significant regression model was found (F(1,19) = 6.91, p = 0.02) with change in error rates associated with change in depressive symptoms. The multiple correlation coefficient was 0.52, indicating that overall improvement in irrelevant mental-set suppression explained 26.7% of the variance in BDI-II scores (β = 0.52, p = 0.02; R 2 = 0.267). A similar regression was calculated with group as an additional factor. A significant model was found (F(2,18) = 19.20, p < 0.001), with a multiple correlation coefficient of 0.82 (R 2 = 0.64). Group (β = 0.68, p < 0.001) was a significant factor and error rates just attained significance (β = 0.30, p = 0.05).
Discussion
This study found significantly lower depression scores and significantly higher CRS following MBCT compared to wait-list + TAU. Moreover, improvements in CRS were significantly associated with improvements in BDI-II scores. These results constitute the first empirical evidence indicating MBCT can help improve mental-set suppression, as well as the first evidence linking such improvements to depressive alleviation.
CRS has been labeled “smart inhibition” [33] since it measures the ability to detect and target only conflicting and “troublemaking” mental-sets. CRS operates on a higher order and abstract level than most inhibition measures in the sense that it does not merely involve suppression a competing response but of a competing rule, regardless of the specific response [20, 21]. This type of finely tuned suppression mechanism fits particularly well with the mindfulness training practiced in MBCT, which focuses on avoiding getting caught in depression-related thoughts that often conflict with one’s ability to focus on current task demands. Our findings suggest that reductions in depressive symptoms are associated with such specialized and specific suppression. These benefits following improved specific suppression contrast with broad and more general thought suppression among depressed individuals, which may prolong or worsen depressive symptoms [34, 35].
The primary limitation of this study was the small sample. Possibly some null effects would have reached significance in a larger sample. The small sample is somewhat less problematic with regard to the significant differences found in this study, since the more probable statistical error in this case is of type I. Second, the use of a wait-list rather than an active control program limits us to only attribute findings to the MBCT program as a whole, rather than to mindfulness training specifically. Finally, although group assignment for most participants was random, the first few participants were quasi-randomized by enrollment order.
Although the current results should be confirmed in larger samples, they provide preliminary evidence that MBCT can improve mental-set suppression, a key cognitive deficit in depression. Furthermore, these findings demonstrate that these improvements in are associated with improvements in depressive symptoms.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Authors wish to thankfully acknowledge Dr. Gaelle Desbordes, Prof. Nachshon Meiran, Dr. Javeria Ali Hashmi, Ms. Kathryn Meade, and Ms. Ana Acevedo-Barga for their contributions to this work. This work was funded by a research grant to the first author from the AlterMed Research Foundation.
Compliance with ethical standards
Conflict of interest
Authors declare no conflict of interest.
References
- 1.Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2011;18:23–33. doi: 10.1017/S1121189X00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stordal KI, Lundervold AJ, Egeland J, et al. Impairment across executive functions in recurrent major depression. Nord J Psychiatry. 2004;58:41–47. doi: 10.1080/08039480310000789. [DOI] [PubMed] [Google Scholar]
- 3.Gotlib IH, Joormann J. Cognition and depression: current status and future directions. Annu Rev Clin Psychol. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Letkiewicz AM, Miller GA, Crocker LD, et al. Executive function deficits in daily life prospectively predict increases in depressive symptoms. Cognit Ther Res. 2014 doi: 10.1007/s10608-014-9629-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snyder HR. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychol Bull. 2013;139:81–132. doi: 10.1037/a0028727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cotrena C, Branco LD, Shansis FM, Fonseca RP. Executive function impairments in depression and bipolar disorder: association with functional impairment and quality of life. J Affect Disord. 2016;190:744–753. doi: 10.1016/j.jad.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Snyder HR (2012) Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychol Bull [DOI] [PMC free article] [PubMed]
- 8.Biringer E, Lundervold A, Stordal K, et al. Executive function improvement upon remission of recurrent unipolar depression. Eur Arch Psychiatry Clin Neurosci. 2005;255:373–380. doi: 10.1007/s00406-005-0577-7. [DOI] [PubMed] [Google Scholar]
- 9.Whitmer AJ, Banich MT. Inhibition versus switching deficits in different forms of rumination. Psychol Sci. 2007;18:546–553. doi: 10.1111/j.1467-9280.2007.01936.x. [DOI] [PubMed] [Google Scholar]
- 10.Whitmer AJ, Gotlib IH. Switching and backward inhibition in major depressive disorder: the role of rumination. J Abnorm Psychol. 2012;121:570–578. doi: 10.1037/a0027474. [DOI] [PubMed] [Google Scholar]
- 11.Trivedi MH, Greer TL. Cognitive dysfunction in unipolar depression: implications for treatment. J Affect Disord. 2014;152–154:19–27. doi: 10.1016/j.jad.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 12.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression. 2. New York: Guilford Press; 2012. [Google Scholar]
- 13.van der Velden AM, Kuyken W, Wattar U, et al. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin Psychol Rev. 2015;37:26–39. doi: 10.1016/j.cpr.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Huijbers MJ, Spijker J, Donders ART, et al. Preventing relapse in recurrent depression using mindfulness-based cognitive therapy, antidepressant medication or the combination: trial design and protocol of the MOMENT study. BMC Psychiatry. 2012;12:125. doi: 10.1186/1471-244X-12-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res. 2011;187:441–453. doi: 10.1016/j.psychres.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Chiesa A, Calati R, Serretti A. Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clin Psychol Rev. 2011;31:449–464. doi: 10.1016/j.cpr.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Heeren A, Van Broeck N, Philippot P. The effects of mindfulness on executive processes and autobiographical memory specificity. Behav Res Ther. 2009;47:403–409. doi: 10.1016/j.brat.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 18.Zeidan F, Johnson SK, Diamond BJ, et al. Mindfulness meditation improves cognition: evidence of brief mental training. Conscious Cogn. 2010;19:597–605. doi: 10.1016/j.concog.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 19.Greenberg J, Reiner K, Meiran N (2013) “Off with the old”: mindfulness practice improves backward inhibition. Front Psychol 3 [DOI] [PMC free article] [PubMed]
- 20.Meiran N, Hsieh S, Dimov E. Resolving task rule incongruence during task switching by competitor rule suppression. J Exp Psychol Learn Mem Cogn. 2010;36:992–1002. doi: 10.1037/a0019761. [DOI] [PubMed] [Google Scholar]
- 21.Hsieh S, Chang CC, Meiran N. Episodic retrieval and decaying inhibition in the competitor-rule suppression phenomenon. Acta Psychol. 2012;141:316–321. doi: 10.1016/j.actpsy.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Vandierendonck A, Liefooghe B, Verbruggen F. Task switching: interplay of reconfiguration and interference control. Psychol Bull. 2010;136:601–626. doi: 10.1037/a0019791. [DOI] [PubMed] [Google Scholar]
- 23.Meiran N. Task switching: mechanisms underlying rigid vs. flexible self-control. Self Control Soc Mind. 2010 [Google Scholar]
- 24.Koch I, Gade M, Schuch S, Philipp AM. The role of inhibition in task switching: a review. Psychon Bull Rev. 2010;17:1–14. doi: 10.3758/PBR.17.1.1. [DOI] [PubMed] [Google Scholar]
- 25.Meiran N, Diamond GM, Toder D, Nemets B. Cognitive rigidity in unipolar depression and obsessive compulsive disorder: examination of task switching, Stroop, working memory updating and post-conflict adaptation. Psychiatry Res. 2011;185:149–156. doi: 10.1016/j.psychres.2010.04.044. [DOI] [PubMed] [Google Scholar]
- 26.Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18:643–662. doi: 10.1037/h0054651. [DOI] [Google Scholar]
- 27.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12:232–241. doi: 10.1016/S0924-9338(97)83297-X. [DOI] [Google Scholar]
- 29.Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- 30.Beck A, Steer R, Brown G (1996) Beck Depression Inventory-II
- 31.Regev S, Meiran N. Post-error slowing is influenced by cognitive control demand. Acta Psychol. 2014;152:10–18. doi: 10.1016/j.actpsy.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 32.Katzir M, Ori B, Hsieh S, Meiran N. Competitor rule priming: evidence for priming of task rules in task switching. Psychol Res. 2015;79:446–462. doi: 10.1007/s00426-014-0583-3. [DOI] [PubMed] [Google Scholar]
- 33.Meiran N, Hsieh S, Chang C-C. “Smart inhibition”: electrophysiological evidence for the suppression of conflict-generating task rules during task switching. Cogn Affect Behav Neurosci. 2011;11:292–308. doi: 10.3758/s13415-011-0037-y. [DOI] [PubMed] [Google Scholar]
- 34.Wenzlaff RM, Bates DE. Unmasking a cognitive vulnerability to depression: how lapses in mental control reveal depressive thinking. J Pers Soc Psychol. 1998;75:1559–1571. doi: 10.1037/0022-3514.75.6.1559. [DOI] [PubMed] [Google Scholar]
- 35.Wenzlaff RM, Luxton DD. The role of thought suppression in depressive rumination. Cognit Ther Res. 2003;27:293–308. doi: 10.1023/A:1023966400540. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.