Abstract
In sub-Saharan Africa, biomass fuels account for approximately 90% of household energy consumption. Limited evidence exists on the association between different biomass fuels and health outcomes. We report results from a cross-sectional sample of 655 households in Malawi. We calculated odds ratios between hypothesized determinants of household air pollution (HAP) exposure (fuel, stove type, and cooking location) and five categories of health outcomes (cardiopulmonary, respiratory, neurologic, eye health, and burns). Reliance on high- or low-quality firewood or crop residue (vs. charcoal) was associated with significantly higher odds of shortness of breath, difficulty breathing, chest pains, night phlegm, forgetfulness, dizziness, and dry irritated eyes. Use of high-quality firewood was associated with significantly lower odds of persistent phlegm. Cooks in rural areas (vs. urban areas) had significantly higher odds of experiencing shortness of breath, persistent cough, and phlegm, but significantly lower odds of phlegm, forgetfulness, and burns. With deforestation and population pressures increasing reliance on low-quality biomass fuels, prevalence of HAP-related cardiopulmonary and neurologic symptoms will likely increase among cooks. Short- to medium-term strategies are needed to secure access to high-quality biomass fuels given limited potential for scalable transitions to modern energy.
Keywords: biomass fuels, cookstoves, deforestation, energy, household air pollution, Malawi
Introduction and Purpose
Approximately three billion people rely on biomass fuels to meet household energy demand (Guta 2014). Household air pollution (HAP) associated with burning biomass fuels is the seventh-largest risk factor for global burden of disease (Forouzanfar et al. 2015); HAP contains harmful pollutants including fine particulate matter (PM2.5), carbon monoxide (CO), and polycyclic aromatic hydrocarbons (PAH) (Rosenthal 2015). Unsustainable harvesting of biomass and use of inefficient technologies have adverse consequences for the environment, economic development, and climate (Martin et al. 2014).
While the literature establishes an association between use of biomass fuels and health, few studies examine a range of biomass fuels and their relative health impact. Bailis et al. (2005) suggest that a shift from fuelwood to charcoal could have large health benefits for African populations, but systematic comparisons of different biomass fuels and their health impacts are needed. At currently low levels of improved stove availability and adoption, and biomass constraining land-use change in sub-Saharan Africa (SSA) (Jagger and Shively 2014), rural households are losing access to high-quality and preferred types of biomass, which we hypothesize has implications for health.
We explore this issue in Malawi, a country with a current population of 17.2 million projected to double by 2030 (World Bank 2016), where HAP is the fifth-largest risk factor for burden of disease (Forouzanfar et al. 2015), and where the annual deforestation rate is 2.8% (MNREE 2013). Fuelwood accounts for over 90% of household energy (Jumbe and Angelsen 2011), and declining forest cover is affecting the quality, quantity, and type of biomass fuels available, leading households to cook with inferior fuels, alter cooking patterns, purchase rather than collect fuels, and walk longer distances to collect fuelwood (Brouwer et al. 1997; Lipper 2000; Bandyopadhyay et al. 2011). Access to modern fuels and improved cooking technologies is constrained by lack of resources, access, and reliability (Zulu 2010; Jagger and Jumbe 2016). Accordingly, HAP studies should examine the impact of the range and quality of biomass fuels used by households on health outcomes of cooks—the population most exposed to HAP.
HAP is associated with numerous cardiopulmonary health problems, including chronic obstructive pulmonary disease (COPD) (Hu et al. 2010; Kurmi et al. 2010; Po et al. 2011; McCracken et al. 2012; Finney et al. 2013), acute coronary syndrome (Fatmi et al. 2014), cardiovascular disease (Brook et al. 2010; McCracken et al. 2012; Noubiap et al. 2015; Sinha and Ray 2015), and blood pressure (Baumgartner et al. 2011, 2014; Peña et al. 2015). HAP emissions are also associated with cancers (lung, mouth, pharynx etc.) (Hosgood et al. 2011; Reid et al. 2012; Seow et al. 2014; Bruce et al. 2015; Josyula et al. 2015). Annually, COPD and lung cancer cause approximately 650,000 premature deaths among women (Van Gemert et al. 2015). Long-term exposure to PM2.5 is strongly associated with mortality from cardiovascular disease compared to non-malignant respiratory disease (Hoek et al. 2013).
Respiratory health problems associated with HAP include acute lower respiratory infections (ALRI) among children (Smith et al. 2000; Gurley et al. 2013), lung function decrement (Fullerton et al. 2011; Kurmi et al. 2014; Sinha and Ray 2015), reduced human macrophage oxidative burst, diminished inflammatory cytokine responses (Rylance et al. 2015), asthma, and tuberculosis (Smith 2000). Compared to clean fuels, cooking with biomass increases the risk of pneumonia by 80% (Dheerani et al. 2008).
Recent studies have found associations between long-term exposure to PM2.5 among adults (>65 years) and neurodegenerative diseases such as dementia, Alzheimer’s, and Parkinson’s diseases (Kioumourtzoglou et al. 2016). Women’s exposure to wood smoke during pregnancy’s third trimester is associated with school-going children’s low scores on neuropsychological tests (Dix-Cooper et al. 2012). Children with no neurological or cognitive risk factors living in Mexico City (high concentrations of O3, PM10, SO2, NO2, CO, and Pb) are more likely to report loss in fluid cognition, memory, and performance of executive functions, compared to similarly healthy children residing in less-polluted urban Polotitlán (Calderón-Garcidueñas et al. 2008). Other HAP-related health problems include cataracts (Pokhrel et al. 2013), eye diseases (West et al. 2013), low birth weight (Amegah et al. 2012; Thompson et al. 2014), and burns (Wong et al. 2014). Research also shows that young children exposed to smoke from biomass fuels are more likely to have nutritional deficiencies including anemia and stunted growth (Mishra and Retherford 2007 in Fullerton et al. 2008).
Our objective is to describe the relationship between use of biomass fuels in Malawi, and HAP-related health outcomes. Our conceptual model assumes fuel quality is a proximate cause of exposure to HAP, which in turn affects health outcomes. A laboratory-based study of stove emissions found that charcoal stoves produced higher CO emissions and lower PM emissions than stoves using fuel-wood (Jetter et al. 2012). Bhattacharya et al. (2002) also found that CO emissions from fuelwood stoves were lower than those from charcoal stoves. Tryner et al. (2014) found that emissions from crop residues were much higher than those from wood pellets. Moisture, an indicator of fuel quality, produces higher CO emissions than dry fuel, and wet charcoal produces higher PM emissions for most stoves/fuel combinations (Jetter et al. 2012).
We also consider stove type and ventilation as proximate causes of HAP. Improved cookstoves (ICS) offer greater fuel efficiency and emissions reductions, and stoves with chimneys remove harmful pollutants from the cooking environment (Smith et al. 2011). In laboratory-based investigations, Ruth et al. (2013) find that improvements in ventilation may lead to reductions in exposure, equivalent to ICS intervention studies. Grabow et al. (2013) found that increasing air exchange rates reduced PM2.5 1-h concentrations by 93–98% compared to closed kitchens, and CO concentrations by 83–95%. Rumchev et al. (2007) found a significant relationship between window area and concentrations of CO and respirable particles. Albalak et al. (2001) and Rosa et al. (2014) estimate median exposure reductions of 57–73% for outdoor (vs. indoor) kitchens.
Higher exposures to HAP resulting from fuel, stove, and ventilation choices have implications for health. In a field-based study in Uganda, Jagger and Shively (2014) find a positive relationship between reliance on low-quality fuelwood and ARI prevalence for children under 5 years. Studies report reductions in various categories of health symptoms among women using improved stoves compared to traditional stoves for systolic and diastolic blood pressure (McCracken et al. 2007; Smith et al. 2011; Neupane et al. 2015); cough, sneezing, phlegm, chest tightness, wheezing, bronchitis, tears while cooking (Khushk et al. 2005; Smith-Sivertsen et al. 2009; Accinelli et al. 2014; Choi et al. 2015); and headache, eye discomfort, backache, preeclampsia/eclampsia, small for gestational age births (Diaz et al. 2007, 2008; Agrawal and Yamamoto 2015; Yucra et al. 2014). The use of improved stoves also reportedly lowered kitchen concentrations of CO (Khushk et al. 2005; Masera et al. 2007; Smith et al. 2011), PM2.5 (Masera et al. 2007) and personal exposures of cooks and other household members to respirable particulates from biomass combustion (Balakrishnan et al. 2002).
Methods
We use cross-sectional data from a sample of 382 households1 collected in rural Malawi in October and November, 2013 in Machinga (18 villages) and Kasungu (26 villages) Districts. Data from 273 peri-urban households in Lilongwe District were collected in May–June, 2014. Our sample of 655 households is randomly drawn from representative villages, and data were collected using a consistent set of survey instruments. The same team of enumerators and community health nurses were involved in the rural and urban data collection.
Kasungu District is located roughly 300 km north of Lilongwe. The average land holding is 1.5 ha (National Census of Agriculture and Livestock 2010). The main agricultural crops planted are maize and tobacco; vegetables are grown in wetland areas; and many households keep cattle and goats. Access to major markets is limited. The study villages in Machinga District, about 200 km south of Lilongwe, are in a relatively population dense part of Malawi; the average land holding is 0.76 ha (National Census of Agriculture and Livestock 2010). The main agricultural crops are maize and paddy rice; there is limited investment in livestock. The study area has good market access with 3 of Malawi’s 15 largest urban centers within 100 km of the study area. Study villages were selected using a stratified random sampling approach; households were randomly selected from a village census.
The urban study site includes 5 ‘Areas’ east and south of Lilongwe Town Center characterized as high-density suburbs selected as broadly representative of peri-urban Lilongwe. Households reside on small plots; most rent rather than own their houses and land. There are numerous informal markets for fuelwood and charcoal. The majority of households in the high-density suburbs engage in daily wage labor and informal sector jobs, and grow maize and vegetables on small plots. Market access is generally very good with local markets providing a wide range of consumption goods. Due to the challenge of creating a census in dense informal urban settlements, our sampling strategy was to visit every third household, moving rightward at the end of a street, from a randomly selected direction determined at a central meeting location.
We administered a household questionnaire to the household decision maker asking questions about household demographics; assets; land, and livestock ownership; wage and business income, income from agriculture and livestock; other sources of income; cash expenditures and purchases in the past 12 months; and recent unexpected crises.
For each household, we conducted a separate interview with the primary cook, defined as those who cooked more than 50% of meals during the past 30 days. Data were collected on demographic characteristics and socio-economic status of cooks; cooking technologies and fuels used2; ventilation of kitchen/cooking area; seasonality; smoking habit; other environmental exposures; perceptions of impacts of cooking practices; and experience and perceptions of different stoves/fuels. A trained community health nurse asked the primary cook a series of questions about prevalence of symptoms of cardiopulmonary, respiratory, neurologic, and eye health and burns during the past 12 months. Our model for estimating differences in health outcomes is as follows:
where Yij denotes a health outcome for primary cook ‘i’ in household ‘j’; Ωi represents confounding variables at the primary cook-level; αj denotes potential household-level confounding variables; and εij is the error term.
We analyze self-reported binary (No/Yes) symptoms of primary cooks’ health outcomes in the past 12 months for five categories: cardiopulmonary; respiratory; neurologic; eye problems; and burns or scalds.3 Explanatory variables include (a) categorical variable for inferior biomass fuels (vs. charcoal); (b) binary variable for traditional stove (0 if other; 1 if three-stone open fire; (c) categorical variable for cooking location (0 if fully outdoors; 1 if partially outdoors; 2 if fully indoors); and (d) binary variable for rural location (0 if urban; 1 if rural). Confounding variables at the primary cook-level include age (in years), a categorical variable for education level (0 if no formal education; 1 if some primary education; 2 if some secondary education or above), and whether cook burns garbage (0 if no; 1 if yes). Household-level confounders include household size (and household size squared), number of household assets, and presence of biomass burning industry nearby. We estimate odds ratios and 95% confidence intervals (CIs) for the various health outcomes using the maximum likelihood estimation strategy (logit model) in Stata 14. The research was approved by the UNC-CH Institutional Review Board and the Malawi National Health Sciences Research Committee (NHSRC).
Results
In our rural sample, 42.2% of households reported using high-quality firewood as their primary fuel source, while 53.1% used low-quality fuelwood (Table 1). Crop residues and charcoal were used by 3.4 and 1.3% of rural households, respectively. The majority of households (89.8%) use the traditional three-stone fire as their main stove. Approximately 85% of households cook indoors, usually in a designated kitchen, the majority of which are well ventilated.4 Other environmental exposures are considerable: 46.3% of households own a biomass burning industry (e.g., brick making; beer brewing), and 86% of primary cooks burn garbage.
Table 1.
| Pooled sample | Rural | Urban | Range | |
|---|---|---|---|---|
| Main fuel used by household (%) | ||||
| High-quality firewood | 28.1 | 42.2 | 8.4 | 0–1 |
| Low-quality firewood | 31.5 | 53.1 | 1.1 | 0–1 |
| Charcoal | 38.3 | 1.3 | 90.1 | 0–1 |
| Crop residue | 2.1 | 3.4 | 0.4 | 0–1 |
| Main stove type used by household (%) | ||||
| Traditional three-stone fire | 56.6 | 89.8 | 10.3 | 0–1 |
| Metal charcoal stove | 38.0 | 1.8 | 88.6 | 0–1 |
| Other (e.g., fixed mud stoves, hot plate) | 5.3 | 8.4 | 1.1 | 0–1 |
| Cooking environment and other environmental exposures | ||||
| Indoor cooking (vs. fully or partially outdoors) (%) | 61.1 | 84.8 | 27.8 | 0–1 |
| Cooking area well ventilated (%) | 86.4 | 81.2 | 93.8 | 0–1 |
| Household owns biomass burning industry (%) | 37.6 | 46.3 | 25.3 | 0–1 |
| Primary cook burns garbage (%) | 71.2 | 86.1 | 50.2 | 0–1 |
| Primary cook’s time spent walking on tarmac roads daily (in minutes) | 2.5 (11.6) | 0.0 (0.0) | 6.0 (17.4) | 0–168 |
| Demographic variables | ||||
| Age of primary cook (years) | 37.3 (13.8) | 41.5 (15.0) | 31.6 (9.7) | 17–72 |
| Education of primary cook (%) | 0–2 | |||
| None | 13.9 | 18.9 | 7.0 | |
| Some primary education | 63.4 | 72.8 | 50.2 | |
| Some secondary education | 22.8 | 8.4 | 42.9 | |
| Household size (number of household members) | 5.7 (2.4) | 5.8 (2.5) | 5.5 (2.2) | 1–15 |
| Household assets (number of household assets currently owned) | 17.2 (10.3) | 13.3 (8.1) | 22.7 (10.6) | 1–40 |
| N | 655 | 382 | 273 | |
Difference of means test (t test) was conducted for all continuous variables, and Pearson’s χ2 tests for all categorical variables. Rural and urban samples are statistically significantly different at the 0.01 level for all variables except household size.
Standard deviations in parentheses.
In the urban sample, charcoal is most commonly used as the primary fuel (90.1%). Stove type mirrors fuel choice; 88.6% use metal charcoal stoves, 10.3% use the traditional three-stone fire, and 1.1% use “other stove type”. Only 27.8% of households cook indoors. Most cooking areas were well ventilated (93.8%). Environmental exposures experienced by urban cooks include ownership of biomass burning industry (25.3%), garbage burning (50.2%), and vehicle emission exposure (time walking on tarmac road).
On average, primary cooks in the sample are 37.3 years. Cooks in rural households are on average 10 years older than those in urban households. Cooks in urban settings are better educated, with 42.9% of the urban sample having some secondary education (vs. 8.4% in the rural sample). Household size did not vary significantly between rural and urban households. Asset ownership5 was higher for our urban sample (22.7 vs. 13.3 for rural households).
We found higher prevalence of all cardiopulmonary symptoms for rural households with shortness of breath while walking uphill (50%), difficulty breathing/chest tightness (23.6%), and chest pains/palpitations (27.2%) as the most common symptoms (Table 2). Prevalence of symptoms ranged from 8.1% (shortness of breath) to 11.7% (chest pains) for urban cooks. Prevalence of respiratory illness symptoms did not exhibit a consistent pattern. Cooks in rural households had relatively high prevalence of persistent cough (24.6 vs. 7.0% urban sample), whereas urban cooks experienced higher prevalence of phlegm at night (17.6%) and phlegm in the morning (19%) compared with cooks in rural households (5.0 and 9.7%, respectively). Neurologic symptoms were very common among both rural and urban cooks. Prevalence of forgetfulness was 42.9% for rural and 54.9% for urban cooks. Dizziness was also common (42.9 and 31.1%) in rural and urban samples. Prevalence of dry irritated eyes was more common for urban households (36.3% compared with 20.7% for rural sample). Most striking is the prevalence of burns in urban households: 86.1 vs. 42.9% for rural cooks.
Table 2.
Descriptive Statistics for Health Outcomes in the Past 12 Monthsa.
| Pooled sample | Rural | Urban | Range | |
|---|---|---|---|---|
| Cardiopulmonary symptoms (%) | ||||
| Shortness of breath (walking uphill) | 32.5 | 50.0 | 8.1 | 0–1 |
| Shortness of breath (at rest) | 10.5 | 13.1 | 7.0 | 0–1 |
| Rapid breathing | 7.2 | 9.7 | 3.7 | 0–1 |
| Difficulty breathing/chest tightness | 18.0 | 23.6 | 10.3 | 0–1 |
| Chest pains/palpitations | 20.8 | 27.2 | 11.7 | 0–1 |
| Respiratory symptoms (%) | ||||
| Difficulty breathing when cough and phlegm gets worse | 8.7 | 11.5 | 4.8 | 0–1 |
| Cough and phlegm gets worse | 14.8 | 15.7 | 13.6 | 0–1 |
| Night phlegm | 10.2 | 5.0 | 17.6 | 0–1 |
| Morning phlegm | 13.6 | 9.7 | 19.0 | 0–1 |
| Persistent phlegm | 5.3 | 7.3 | 2.6 | 0–1 |
| Persistent cough | 17.3 | 24.6 | 7.0 | 0–1 |
| Neurologic and other symptoms (%) | ||||
| Forgetfulness | 47.9 | 42.9 | 54.9 | 0–1 |
| Dizziness | 38.0 | 42.9 | 31.1 | 0–1 |
| Difficulty concentrating | 18.0 | 16.8 | 19.8 | 0–1 |
| Dry irritated eyes | 27.2 | 20.7 | 36.3 | 0–1 |
| Burns | 60.9 | 42.9 | 86.1 | 0–1 |
| N | 655 | 382 | 273 | |
Pearson’s χ2 tests were used for all the binary health outcomes. Rural and urban samples are statistically significantly different at the 0.01 level for all variables except ‘cough and phlegm gets worse’ and ‘difficulty concentrating’.
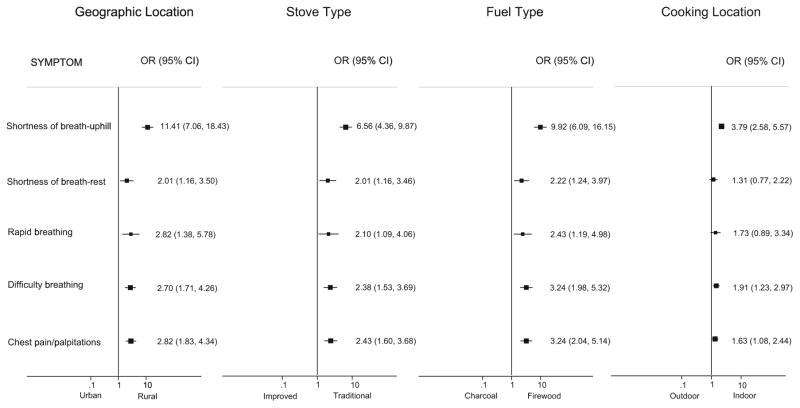
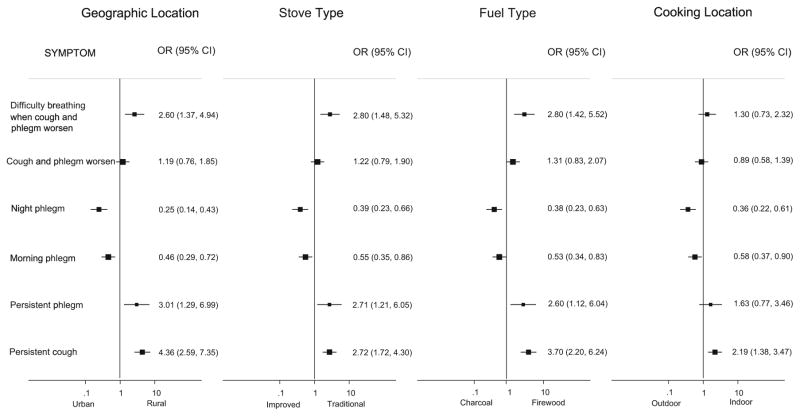
We leverage heterogeneity in biomass fuel type, stove type, and cooking location to understand crude associations between the prevalence of each of the health symptoms, and the proximate determinants of HAP exposure.6 We present crude prevalence odds ratios in forest plots for the pooled urban and rural samples (Figs. 1, 2, and 3). We also use a series of logistic regression models to estimate adjusted prevalence odds ratios for all health symptoms, controlling for individual- and household-level confounding (Tables 3, 4, and 5).
Figure 1.
Crude odds ratios for cardiopulmonary health outcomes by exposure category.
Figure 2.
Crude odds ratios for respiratory health outcomes by exposure category.
Figure 3.
Crude odds ratios for other health outcomes by exposure category.
Table 3.
Adjusted Odds Ratios for the Association Between Fuel and Stove Type, Cooking Location, & Primary Cooks’ Health Outcomes in the Past 12 Months (Cardiopulmonary Symptoms)a,b,c.
| Variables | Shortness of breath (walking uphill) | Shortness of breath (at rest) | Rapid breathing | Difficulty breathing/chest tightness | Chest pains/ palpitations |
|---|---|---|---|---|---|
| Fuel type | |||||
| High-quality firewood | 0.69 (0.15, 3.21) | 1.23 (0.33, 4.55) | 0.49 (0.05, 5.28) | 2.83★ (0.88, 9.08) | 2.95★ (0.94, 9.27) |
| Low-quality firewood | 1.38 (0.30, 6.39) | 1.02 (0.24, 4.32) | 0.61 (0.06, 6.54) | 2.54 (0.74, 8.71) | 3.00★ (0.91, 9.86) |
| Crop residue | 1.13 (0.18, 6.99) | 6.22★★ (1.13, 34.17) | 1.04 (0.07, 16.18) | 3.76 (0.72, 19.51) | 4.46★ (0.92, 21.66) |
| Traditional stove | 1.29 (0.59, 2.83) | 1.20 (0.45, 3.23) | 1.06 (0.34, 3.32) | 0.81 (0.39, 1.68) | 0.80 (0.35, 1.80) |
| Cooking location | |||||
| Partially outdoors | 0.87 (0.41, 1.84) | 1.16 (0.48, 2.81) | 0.78 (0.24, 2.56) | 1.21 (0.56, 2.63) | 0.82 (0.40, 1.68) |
| Fully indoors | 1.30 (0.71, 2.39) | 1.01(0.47, 2.15) | 1.00 (0.40, 2.50) | 1.19 (0.61, 2.33) | 0.83 (0.46, 1.52) |
| Rural location | 5.94★★★ (1.66, 21.26) | 1.13 (0.35, 3.71) | 3.28 (0.31, 34.31) | 0.80 (0.30, 2.12) | 1.08 (0.46, 2.55) |
| Observations | 655 | 655 | 655 | 655 | 655 |
95% confidence intervals in parentheses. Regression estimates were adjusted for age of cook, education level of cook, garbage burning by primary cook, minutes per day spent by primary cook walking on tarmac roads, household size, household size squared, number of household assets, and household ownership of biomass burning industry.
P < 0.01,
P < 0.05,
P < 0.1.
Charcoal is the referent category for fuel type.
Fully outdoor cooking is the referent category for cooking location.
No education is the referent category for education level of cook.
Table 4.
Adjusted Odds Ratios for the Association Between Fuel and Stove Type, Cooking Location, & Primary Cooks’ Health Outcomes in the Past 12 Months (Respiratory Symptoms)a,b,c.
| Variables | Difficulty breathing when cough and phlegm gets worse | Cough and phlegm gets worse | Night phlegm | Morning phlegm | Persistent phlegm | Persistent cough |
|---|---|---|---|---|---|---|
| Fuel type | ||||||
| High-quality Firewood | 1.00 (0.16, 6.44) | 1.83 (0.53, 6.31) | 2.93 (0.71, 12.12) | 1.55 (0.50, 4.79) | 0.31★ (0.08, 1.19) | 0.72 (0.28, 1.88) |
| Low-quality Firewood | 1.00 (0.14, 6.91) | 2.99 (0.772, 11.54) | 5.39★★ (1.06, 27.45) | 2.04 (0.59, 7.11) | 0.37 (0.07, 1.88) | 0.69 (0.24, 1.98) |
| Crop residue | 2.02 (0.19, 21.31) | 3.19 (0.46, 21.94) | 11.59★★ (1.38, 97.31) | 1.39 (0.13, 15.38) | 0.38 (0.03, 4.87) | 1.20 (0.28, 5.22) |
| Traditional stove | 1.99 (0.4, 9.67) | 0.88 (0.33, 2.33) | 0.70 (0.20, 2.43) | 0.87 (0.36, 2.09) | 2.25 (0.56, 9.08) | 0.78 (0.36, 1.71) |
| Cooking location | ||||||
| Partially outdoors | 1.30 (0.46, 3.64) | 1.48 (0.73, 2.99) | 0.79 (0.39, 1.58) | 1.11 (0.57, 2.16) | 1.67 (0.44, 6.43) | 0.87 (0.38, 2.02) |
| Fully indoors | 0.84 (0.38, 1.88) | 0.93 (0.48, 1.80) | 0.59 (0.29, 1.21) | 0.88 (0.43, 1.80) | 1.20 (0.38, 3.82) | 1.01 (0.52, 1.98) |
| Rural location | 1.40 (0.36, 5.46) | 0.66 (0.25, 1.76) | 0.13★★★ (0.04, 0.39) | 0.45★ (0.17, 1.16) | 4.61★★★ (1.79, 11.86) | 5.12★★★ (2.45, 10.70) |
| Observations | 655 | 655 | 655 | 655 | 655 | 655 |
95% confidence intervals in parentheses. Regression estimates were adjusted for age of cook, education level of cook, garbage burning by primary cook, minutes per day spent by primary cook walking on tarmac roads, household size, household size squared, number of household assets, and household ownership of biomass burning industry.
P < 0.01,
P < 0.05,
P < 0.1.
Charcoal is the referent category for fuel type.
Fully outdoor cooking is the referent category for cooking location.
No education is the referent category for education level of cook.
Table 5.
Adjusted Odds Ratios for the Association Between Fuel and Stove Type, Cooking Location, & Primary Cooks’ Health Outcomes in the Past 12 Months (Neurologic and Other Symptoms)a,b,c.
| Variables | Neurologic symptoms
|
Other symptoms
|
|||
|---|---|---|---|---|---|
| Forgetfulness | Dizziness | Difficulty concentrating | Dry irritated eyes | Burns | |
| Fuel type | |||||
| High-quality firewood | 1.80 (0.62, 5.23) | 0.92 (0.32, 2.62) | 0.51 (0.10, 2.65) | 1.13 (0.40, 3.16) | 0.83 (0.29, 2.37) |
| Low-quality firewood | 4.48★★ (1.42, 14.19) | 2.26 (0.75, 6.82) | 1.00 (0.19, 5.37) | 1.64 (0.54, 4.99) | 0.73 (0.23, 2.28) |
| Crop residue | 9.13★★★ (1.86, 44.95) | 4.72★★ (1.02, 21.76) | 0.90 (0.11, 7.19) | 3.75★ (0.81, 17.36) | 0.73 (0.16, 3.31) |
| Traditional stove | 1.19 (0.59, 2.42) | 0.95 (0.47, 1.93) | 1.17 (0.38, 3.54) | 0.70 (0.33, 1.49) | 1.26 (0.64, 2.50) |
| Cooking location | |||||
| Partially outdoors | 0.98 (0.58, 1.64) | 0.85 (0.50, 1.46) | 0.86 (0.45, 1.65) | 1.17 (0.68, 2.01) | 0.80 (0.39, 1.64) |
| Fully indoors | 1.06 (0.66, 1.70) | 1.15 (0.70, 1.88) | 0.82 (0.46, 1.46) | 0.97 (0.59, 1.61) | 0.60★ (0.34, 1.05) |
| Rural location | 0.11★★★ (0.04, 0.29) | 0.59 (0.24, 1.43) | 0.76 (0.24, 2.38) | 0.55 (0.25, 1.23) | 0.21★★★ (0.08, 0.57) |
| Observations | 655 | 655 | 655 | 655 | 655 |
95% confidence intervals in parentheses. Regression estimates were adjusted for age of cook, education level of cook, garbage burning by primary cook, minutes per day spent by primary cook walking on tarmac roads, household size, household size squared, number of household assets, and household ownership of biomass burning industry.
P < 0.01,
P < 0.05,
P < 0.1.
Charcoal is the referent category for fuel type.
Fully outdoor cooking is the referent category for cooking location.
No education is the referent category for education level of cook.
Estimation of crude odds ratios suggests that primary cooks living in rural areas (vs. urban), using traditional stoves (vs. improved), using firewood (vs. charcoal), and cooking indoors (vs. outdoors) have higher odds of experiencing cardiopulmonary symptoms (Fig. 1).
Cooks in high-quality and low-quality firewood-using households (vs. charcoal) are three times more likely to experience chest tightness and chest palpitations (95% CI; P < 0.10). Cooks using crop residues as their primary fuel are six times more likely to experience shortness of breath at rest (95% CI; P < 0.05) and four times more likely to experience chest pains (95% CI; P < 0.10), controlling for confounding. Though the crude odds ratios show significant associations between the use of traditional stoves and cooking indoors, and each of the cardiopulmonary symptoms, after adjusting, we do not find any statistically significant results. After adjusting for individual and household-level covariates, we find that cooks in rural areas have significantly higher odds (six times) of experiencing shortness of breath going uphill (95% CI; P < 0.01) compared to their urban counterparts. All other cardiopulmonary symptoms are not significantly different between rural and urban cooks.
Our analysis of stratified rural and urban samples confirms our overall findings.7 For cooks in the rural sample, use of low-quality firewood (vs. high-quality) doubles the prevalence of shortness of breath walking uphill, and use of crop residues increases the prevalence of shortness of breath at rest by 5 times (95% CI; P < 0.01).
Respiratory symptoms’ crude odds ratios for the pooled rural and urban sample do not reveal consistent patterns (Fig. 2). Controlling for other factors, high-quality firewood has a significant protective effect on persistent phlegm (0.31) (95% CI; P < 0.10) compared to charcoal; cooks in low-quality firewood- and crop residue-using households compared to those in households using charcoal have significantly higher odds (5.39 and 11.59, respectively) of experiencing night phlegm (95% CI; P < 0.05) (Table 4). Traditional stove use and cooking location have no significant associations with any respiratory symptoms. Primary cooks in rural areas have significantly higher odds of experiencing persistent cough and persistent phlegm (5.12 and 4.61, respectively) (95% CI; P < 0.01), but significantly lower odds of phlegm at night (0.13) (95% CI; P < 0.01) and in the morning (0.45) (95% CI; p < 0.10), compared to their urban counterparts controlling for cook and household-level factors.
For our rural sample, cooking indoors has a protective effect on the prevalence of phlegm in the morning (0.36) (95% CI; P < 0.05). For the urban sample of cooks, use of firewood and crop residue, compared to charcoal, significantly increases the prevalence of morning phlegm (3.36) (95% CI; P < 0.10). Use of a traditional stove (vs. improved) has a very large effect, increasing prevalence of difficulty breathing when cough and phlegm get worse by more than 10 times (95% CI; P < 0.01).
Crude odds ratios for the pooled sample do not reveal clear patterns of prevalence of neurologic and other symptoms (Fig. 3). Prevalence of dry eyes and burns was more likely in households using improved stoves, charcoal, cooking outdoors, and in urban households.
Adjusted odds ratios for neurologic and other health symptoms (Table 5) show that primary cooks in low-quality firewood-using households (vs. charcoal) have significantly higher odds of forgetfulness (4.48) (95% CI; P < 0.05). We find strong associations between use of crop residues and forgetfulness (9.13), dizziness (4.72), and dry irritated eyes (3.75) when compared with households that use charcoal (95% CI; P < 0.01, P < 0.05, P < 0.10, respectively). Traditional stove use has no significant association with any of these symptoms. Cooking fully indoors (vs. fully outdoors) is associated with significantly lower odds of burns (0.60) (95% CI; P < 0.10). Primary cooks in rural areas (vs. urban) have significantly lower odds of experiencing forgetfulness (0.11) and burns (0.21) (95% CI; P < 0.01).
We find strong associations between neurologic symptoms and use of low-quality firewood and crop residues (vs. high-quality) as primary fuel for the rural sample. Use of low-quality firewood increases the odds of forgetfulness, dizziness, and difficulty concentrating between 2 and 3 times (95% CI; P < 0.01); use of crop residues as primary fuel increases odds of forgetfulness and dizziness by more than 6 times (95% CI; P < 0.01). Cooking indoors (vs. outdoors) has a significant protective effect on the prevalence of burns (0.47) (95% CI; P < 0.05). Our only significant result for the urban sample is that use of a traditional stove (vs. improved) increases the odds of forgetfulness by 3 times (95% CI; P < 0.10).
Discussion
Our analysis of health symptoms for primary cooks in Malawi offers a mixed picture of associations between types of biomass fuels, stove type, cooking location, and health. We find that use of high-quality firewood, compared to charcoal, often considered a ‘cleaner’ fuel, has significant positive associations with chest tightness and pain, but significant negative associations with persistent phlegm. We also find significant positive associations between use of poor-quality firewood and chest pains and forgetfulness. Use of crop residues, has significant positive associations with shortness of breath at rest, chest pains, night phlegm, forgetfulness, dizziness, and dry irritated eyes. Our results suggest that the types of biomass fuels households are using are important. In light of recent evidence of the association between long-term exposure to PM2.5 and neurodegenerative diseases (Kioumourtzoglou et al. 2016), it is particularly noteworthy that we find significant positive associations between two inferior biomass fuels and most neurologic symptoms analyzed.
We use charcoal as a referent category, as it is considered to be higher on the energy ladder compared to the other biomass fuels (Rehfuess 2006). Though we find evidence of positive associations between firewood and crop residue, compared to charcoal, and most health symptoms, our results do not favor promoting charcoal over fuelwood for two reasons. First, charcoal is associated with lower PM2.5 exposure but higher than WHO recommended levels of CO exposure (Ellegård and Egneus 1992) when compared to burning fuelwood or crop residues, making it of clear concern for health outcomes (Hampson et al. 1994). Second, policy supporting household transitions to charcoal as a primary fuel could have catastrophic environmental implications; charcoal production is a major driver of deforestation in Malawi.
We find surprisingly few associations between stove use and health outcomes. This is likely because the majority of improved biomass stoves used in Malawi do not offer significant reductions in emissions. While Fullerton et al. (2009) found that respirable dust concentrations were comparable in rural and urban areas in Malawi; we find significant differences in the prevalence of HAP-related symptoms in rural and urban locations, owing to variability in type of biomass cooking fuel used.
Our analysis has been unable to account for environmental risks such as poor water quality and food insufficiency that could exacerbate HAP-exposed populations’ susceptibility to diseases. Future research should examine the exposure–response relationship between the types of biomass cooking fuels and other vital health indicators, such as lung function, and control for environmental confounders. Since the cross-sectional nature of our study does not allow for causal inferences, our findings must be confirmed in cohort studies, such as the Cooking and Pneumonia Study (CAPS) in Malawi—the world’s largest cookstove intervention trial (Ardrey et al. 2016).
Conclusion
Women in Malawi face numerous health risks associated with the use of biomass fuels. We find that the use of inferior biomass fuels, specifically low-quality firewood and crop residues are significantly positively associated with cardiopulmonary (shortness of breath), respiratory (phlegm at night), neurologic (forgetfulness, dizziness, and difficulty concentrating), and other (dry irritated eyes) symptoms.
Given high rates of population growth, forest loss, and lags in the delivery of modern energy services in Malawi, biomass stocks will decline in the coming years. Increasing the share of households relying on inferior biomass has implications for human health. Promoting cookstoves that significantly reduce fuel consumption could reduce the burden of disease from HAP if it allows households sustained access to higher quality fuelwood. A second policy option is establishing high-quality renewable biomass stocks through tree planting or other novel interventions (e.g., promotion of pigeon pea), which provide both food and a renewable source of fuel while fixing nitrogen in the soil. Interventions should be targeted to parts of the country where the share of households relying on inferior fuels is increasing. We fully acknowledge that burning biomass will not remove the health burden of HAP, but our results suggest that type of biomass households use has implications for health.
Acknowledgments
This research was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K01HD073329), the Fogarty International Center, and the National Heart, Lung and Blood Institute (R25TW009340). We are grateful to the Carolina Population Center (P2CHD050924) at The University of North Carolina at Chapel Hill for general support. Simon Chimwanza, Esther Giezendanner, and Laura Hamrick provided valuable inputs to this research. The opinions expressed herein are those of the authors and do not necessarily reflect the views of the sponsoring agency.
Footnotes
See http://fuel.web.unc.edu/mfls-survey/ for further details of the rural sample.
Household’s use of high- (e.g., wood sourced from natural forests, woodlots, or fuelwood markets, often hardwoods with relatively low moisture content) or low-quality firewood (woody plants and shrubs, smaller diameter trees, green, or wet wood) was based on respondents’ subjective assessment of the quality of firewood.
Though our study collected data on cook anthropometrics, pulse oximetry and blood pressure, these indicators are being analyzed in separate papers.
Well-ventilated kitchens were defined as those where most of the cooking was done partially or fully outdoors; there was a gap between the walls and roof; pitch of the roof in the cooking area was inverted “V”; and there were above average number of windows and ventilation holes.
The asset ownership variable is a count of the number of assets (e.g., solar panel, electric fan, working television and/or radio, bicycle, cellphone, furniture, mattresses, metal or clay cookstove, lantern, mosquito net) households own.
We exclude households that use crop residues as their primary fuel (n = 14) to limit the number of comparisons we make.
Tables showing results of decomposed rural and urban samples are available upon request.
Compliance with ethical standard
Conflict of interest None declared.
References
- Accinelli RA, Llanos O, López LM, Pino MI, Bravo YA, Salinas V, Lazo M, Noda JR, Sánchez-Sierra M, Zárate L, da Silva J. Adherence to reduced-polluting biomass fuel stoves improves respiratory and sleep symptoms in children. BMC Pediatrics. 2014;14:1–12. doi: 10.1186/1471-2431-14-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal S, Yamamoto S. Effect of indoor air pollution from biomass and solid fuel combustion on symptoms of preeclampsia/eclampsia in Indian women. Indoor Air. 2015;25:341–352. doi: 10.1111/ina.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albalak R, Bruce N, McCracken JP, Smith KR, De Gallardo T. Indoor respirable particulate matter concentrations from an open fire, improved cookstove, and LPG/open fire combination in a rural Guatemalan community. Environmental Science & Technology. 2001;35:2650–2655. doi: 10.1021/es001940m. [DOI] [PubMed] [Google Scholar]
- Amegah AK, Jaakkola JJ, Quansah R, Norgbe GK, Dzodzomenyo M. Cooking fuel choices and garbage burning practices as determinants of birth weight: a cross-sectional study in Accra, Ghana. Environmental Health. 2012;11:78. doi: 10.1186/1476-069X-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardrey J, Desmond N, Tolhurst R, Mortimer K. The Cooking and Pneumonia Study (CAPS) in Malawi: a nested pilot of Photovoice participatory research methodology. PloS One. 2016;11(6):e0156500. doi: 10.1371/journal.pone.0156500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailis R, Ezzati M, Kammen DM. Mortality and greenhouse gas impacts of biomass and petroleum energy futures in Africa. Science. 2005;308:98–103. doi: 10.1126/science.1106881. [DOI] [PubMed] [Google Scholar]
- Balakrishnan K, Sankar S, Parikh J, Padmavathi R, Srividya K, Venugopal V, Prasad S, Pandey VL. Daily average exposures to respirable particulate matter from combustion of biomass fuels in rural households of southern India. Environmental Health Perspectives. 2002;110:1069–1075. doi: 10.1289/ehp.021101069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandyopadhyay S, Shyamsundar P, Baccini A. Forests, biomass use and poverty in Malawi. Ecological Economics. 2011;70:2461–2471. [Google Scholar]
- Baumgartner J, Schauer JJ, Ezzati M, Lu L, Cheng C, Patz JA, Bautista LE. Indoor air pollution and blood pressure in adult women living in rural China. Environmental Health Perspectives. 2011;119:1390. doi: 10.1289/ehp.1003371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner J, Zhang Y, Schauer JJ, Huang W, Wang Y, Ezzati M. Highway proximity and black carbon from cookstoves as a risk factor for higher blood pressure in rural China. Proceedings of the National Academy of Sciences. 2014;111:13229–13234. doi: 10.1073/pnas.1317176111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharya SC, Albina DO, Abdul Salam P. Emission factors of wood and charcoal-fired cookstoves. Biomass and Bioenergy. 2002;23:453–469. [Google Scholar]
- Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A. Particulate matter air pollution and cardiovascular disease an update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- Brouwer ID, Hoorweg JC, Van Liere MJ. When households run out of fuel: responses of rural households to decreasing fuelwood availability, Ntcheu District, Malawi. World Development. 1997;25:255–266. [Google Scholar]
- Bruce N, Dherani M, Liu R, Hosgood HD, Sapkota A, Smith KR, Straif K, Lan Q, Pope D. Does household use of biomass fuel cause lung cancer? A systematic review and evaluation of the evidence for the GBD 2010 study. Thorax. 2015;70:433–441. doi: 10.1136/thoraxjnl-2014-206625. [DOI] [PubMed] [Google Scholar]
- Calderón-Garcidueñas L, Mora-Tiscareño A, Ontiveros E, Gómez-Garza G, Barragán-Mejía G, Broadway J, Chapman S, Valencia-Salazar G, Jewells V, Maronpot RR, Henríquez-Roldán C. Air pollution, cognitive deficits and brain abnormalities: a pilot study with children and dogs. Brain and Cognition. 2008;68:117–127. doi: 10.1016/j.bandc.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Choi JY, Baumgartner J, Harnden S, Alexander BH, Town RJ, D’Souza G, Ramachandran G. Increased risk of respiratory illness associated with kerosene fuel use among women and children in urban Bangalore, India. Occupational and Environmental Medicine. 2015;72:114–122. doi: 10.1136/oemed-2014-102472. [DOI] [PubMed] [Google Scholar]
- Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M, Bruce N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under 5 years: a systematic review and meta-analysis. Bulletin of the World Health Organization. 2008;86:390–398. doi: 10.2471/BLT.07.044529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz E, Smith-Sivertsen T, Pope D, Lie RT, Diaz A, McCracken J, Arana B, Smith KR, Bruce N. Eye discomfort, headache and back pain among Mayan Guatemalan women taking part in a randomized stove intervention trial. Journal of Epidemiology and Community Health. 2007;61:74–79. doi: 10.1136/jech.2006.043133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz E, Bruce N, Pope D, Díaz A, Smith KR, Smith-Sivertsen T. Self-rated health among Mayan women participating in a randomized intervention trial reducing indoor air pollution in Guatemala. BMC International Health and Human Rights. 2008;8:1. doi: 10.1186/1472-698X-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dix-Cooper L, Eskenazi B, Romero C, Balmes J, Smith KR. Neurodevelopmental performance among school age children in rural Guatemala is associated with prenatal and postnatal exposure to carbon monoxide, a marker for exposure to woodsmoke. Neurotoxicology. 2012;33:246–254. doi: 10.1016/j.neuro.2011.09.004. [DOI] [PubMed] [Google Scholar]
- Ellegård A, Egneus H. Health Effects of Charcoal and Woodfuel Use in Low-Income Households in Lusaka. Energy, Environment and Development Series-Stockholm Environment Institute. Cambridge: MIT Press; 1992. [Google Scholar]
- Fatmi Z, Coggon D, Kazi A, Naeem I, Kadir MM, Sathiakumar N. Solid fuel use is a major risk factor for acute coronary syndromes among rural women: a matched case control study. Public Health. 2014;128(1):77–82. doi: 10.1016/j.puhe.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney LJ, Feary JR, Leonardi-Bee J, Gordon SB, Mortimer K. Chronic obstructive pulmonary disease in sub-Saharan Africa: a systematic review. The International Journal of Tuberculosis and Lung Disease. 2013;17:583–589. doi: 10.5588/ijtld.12.0619. [DOI] [PubMed] [Google Scholar]
- Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A, Delwiche K. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2015;386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullerton DG, Bruce N, Gordon SB. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2008;102(9):843–851. doi: 10.1016/j.trstmh.2008.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullerton DG, Semple S, Kalambo F, Suseno A, Malamba R, Henderson G, Ayres JG, Gordon SB. Biomass fuel use and indoor air pollution in homes in Malawi. Occupational and Environmental Medicine. 2009;66(11):777–783. doi: 10.1136/oem.2008.045013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullerton DG, Suseno A, Semple S, Kalambo F, Malamba R, White S, Jack S, Calverley PM, Gordon SB. Wood smoke exposure, poverty and impaired lung function in Malawian adults. The International Journal of Tuberculosis and Lung Disease. 2011;15(3):391–398. [PubMed] [Google Scholar]
- Grabow K, Still D, Bentson S. Test kitchen studies if indoor air pollution from biomass cookstoves. Energy for Sustainable Development. 2013;17(5):458–462. [Google Scholar]
- Gurley ES, Homaira N, Salje H, Ram PK, Haque R, Petri W, Bresee J, Moss WJ, Breysse P, Luby SP, Azziz-Baumgartner E. Indoor exposure to particulate matter and the incidence of acute lower respiratory infections among children: a birth cohort study in urban Bangladesh. Indoor Air. 2013;23:379–386. doi: 10.1111/ina.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guta DD. Effect of fuelwood scarcity and socio-economic factors on household bio-based energy use and energy substitution in rural Ethiopia. Energy Policy. 2014;75:217–227. [Google Scholar]
- Hampson NB, Kramer CC, Dunford RG, Norkool DM. Carbon monoxide poisoning from indoor burning of charcoal briquets. JAMA. 1994;271:52–53. [PubMed] [Google Scholar]
- Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B, Kaufman JD. Long-term air pollution exposure and cardiorespiratory mortality: a review. Environmental Health. 2013;12:43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosgood HD, Wei H, Sapkota A, Choudhury I, Bruce N, Smith KR, Rothman N, Lan Q. Household coal use and lung cancer: systematic review and meta-analysis of case–control studies, with an emphasis on geographic variation. International Journal of Epidemiology. 2011;40:719–728. doi: 10.1093/ije/dyq259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu G, Zhou Y, Tian J, Yao W, Li J, Li B, Ran P. Risk of COPD from exposure to biomass smoke: a meta-analysis. Chest Journal. 2010;138:20–31. doi: 10.1378/chest.08-2114. [DOI] [PubMed] [Google Scholar]
- Jagger P, Jumbe C. Stoves or sugar? Willingness to adopt improved cookstoves in Malawi. Energy Policy. 2016;92:409–419. doi: 10.1016/j.enpol.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger P, Shively G. Land use change, fuel use and respiratory health in Uganda. Energy Policy. 2014;67:713–726. doi: 10.1016/j.enpol.2013.11.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jetter J, Zhao Y, Smith K, Khan B, Yelverton T, DeCarlo P, Hays M. Pollutant emissions and energy efficiency under controlled conditions for household biomass cookstoves and implications for metrics useful in setting international test standards. Environmental Science & Technology. 2012;46:10827–10834. doi: 10.1021/es301693f. [DOI] [PubMed] [Google Scholar]
- Josyula S, Lin J, Xue X, Rothman N, Lan Q, Rohan TE, Hosgood HD. Household air pollution and cancers other than lung: a meta-analysis. Environmental Health. 2015;14:24. doi: 10.1186/s12940-015-0001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jumbe CB, Angelsen A. Modeling choice of fuelwood source among rural households in Malawi: a multinomial probit analysis. Energy Economics. 2011;33:732–738. [Google Scholar]
- Khushk WA, Fatmi Z, White F, Kadir MM. Health and social impacts of improved stoves on rural women: a pilot intervention in Sindh, Pakistan. Indoor Air. 2005;15:311–316. doi: 10.1111/j.1600-0668.2005.00367.x. [DOI] [PubMed] [Google Scholar]
- Kioumourtzoglou MA, Schwartz JD, Weisskopf MG, Melly SJ, Wang Y, Dominici F, Zanobetti A. Long-term PM2.5 exposure and neurological hospital admissions in the Northeastern United States. Environmental Health Perspectives. 2016;124:23. doi: 10.1289/ehp.1408973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurmi OP, Semple S, Simkhada P, Smith WCS, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysis. Thorax. 2010;65:221–228. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- Kurmi OP, Semple S, Devereux GS, Gaihre S, Lam KBH, Sadhra S, Steiner MF, Simkhada P, Smith WC, Ayres JG. The effect of exposure to biomass smoke on respiratory symptoms in adult rural and urban Nepalese populations. Environmental Health. 2014;13:92. doi: 10.1186/1476-069X-13-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipper L. Forest degradation and food security. Unasylva (English ed) 2000;51:24–31. [Google Scholar]
- Martin WJ, II, Hollingsworth JW, Ramanathan V. Household air pollution from cookstoves: impacts on health and climate. In: Ford JD, Berrang-Ford L, editors. Global Climate Change and Public Health. New York: Springer; 2014. pp. 237–255. [Google Scholar]
- Masera O, Edwards R, Arnez CA, Berrueta V, Johnson M, Bracho LR, Riojas-Rodríguez H, Smith KR. Impact of Patsari improved cookstoves on indoor air quality in Michoacán, Mexico. Energy for Sustainable Development. 2007;11:45–56. [Google Scholar]
- McCracken JP, Smith KR, Díaz A, Mittleman MA, Schwartz J. Chimney stove intervention to reduce long-term wood smoke exposure lowers blood pressure among Guatemalan women. Environmental Health Perspectives. 2007;115(7):996–1001. doi: 10.1289/ehp.9888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken JP, Wellenius GA, Bloomfield GS, Brook RD, Tolunay HE, Dockery DW, Rabadan-Diehl C, Checkley W, Rajagopalan S. Household air pollution from solid fuel use: evidence for links to CVD. Global Heart. 2012;7:223–234. doi: 10.1016/j.gheart.2012.06.010. [DOI] [PubMed] [Google Scholar]
- Ministry of Natural Resources Energy and the Environment. Malawi policy brief Forests and Woodlands. Lilongwe, Malawi: 2013. [accessed August 30, 2016]. Available: http://www.unpei.org/sites/default/files/e_library_documents/Malawi_Policy_Brief_Forests_and_Woodlands_MSEOR.pdf. [Google Scholar]
- Mishra V, Retherford RD. Does biofuel smoke contribute to anaemia and stunting in early childhood? International Journal of Epidemiology. 2007;36:117–129. doi: 10.1093/ije/dyl234. [DOI] [PubMed] [Google Scholar]
- National Census of Agriculture and Livestock. Government of Malawi, National Statistical Office; 2010. [Google Scholar]
- Neupane M, Basnyat B, Fischer R, Froeschl G, Wolbers M, Rehfuess EA. Sustained use of biogas fuel and blood pressure among women in rural Nepal. Environmental Research. 2015;136:343–351. doi: 10.1016/j.envres.2014.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noubiap JJN, Essouma M, Bigna JJR. Targeting household air pollution for curbing the cardiovascular disease burden: a health priority in sub-Saharan Africa. The Journal of Clinical Hypertension. 2015;17:825–829. doi: 10.1111/jch.12610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peña MB, Romero KM, Velazquez EJ, Davila-Roman VG, Gilman RH, Wise RA, et al. Relationship between daily exposure to biomass fuel smoke and blood pressure in high-altitude Peru. Hypertension. 2015;65:1134–1140. doi: 10.1161/HYPERTENSIONAHA.114.04840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Po JY, FitzGerald JM, Carlsten C. Respiratory disease associated with solid biomass fuel exposure in rural women and children: systematic review and meta-analysis. Thorax. 2011;66:232–239. doi: 10.1136/thx.2010.147884. [DOI] [PubMed] [Google Scholar]
- Pokhrel AK, Bates MN, Shrestha SP, Bailey IL, DiMartino RB, Smith KR, Joshi ND. Biomass stoves and lens opacity and cataract in Nepalese women. Optometry and Vision Science: Official Publication of the American Academy of Optometry. 2013;90:257. doi: 10.1097/OPX.0b013e3182820d60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehfuess E. Fuel for Life: Household Energy and Health. Geneva: World Health Organization; 2006. [Google Scholar]
- Reid BC, Ghazarian AA, DeMarini DM, Sapkota A, Jack D, Lan Q, Winn DM, Birnbaum LS. Research opportunities for cancer associated with indoor air pollution from solid-fuel combustion. Environmental Health Perspectives. 2012;120:1495–1498. doi: 10.1289/ehp.1204962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa G, Majorin F, Boisson S, Barstow C, Johnson M, Kirby M, Ngabo F, Thomas E, Clasen T. Assessing the impact of water Filters and improved cookstoves on drinking water quality and household air pollution: a randomized control trial in Rwanda. PLoS One. 2014;9:e91011. doi: 10.1371/journal.pone.0091011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal J. The real challenge for cookstoves and health: more evidence. EcoHealth. 2015;12:8–11. doi: 10.1007/s10393-014-0997-9. [DOI] [PubMed] [Google Scholar]
- Rumchev K, Spickett JT, Brown HL, Mkhweli B. Indoor air pollution from biomass combustion and respiratory symptoms of women and children in a Zimbabwean village. Indoor Air. 2007;17(6):468–474. doi: 10.1111/j.1600-0668.2007.00494.x. [DOI] [PubMed] [Google Scholar]
- Ruth M, Maggio J, Whelan K, DeYoung M, May J, Peterson A, Paterson K. Kitchen 2.0: design guidance for healthier cooking environments. International Journal for Service Learning in Engineering. (2) 2013:151–169. http://ojs.library.queensu.ca/index.php/ijsle/article/view/5147/5037.
- Rylance J, Chimpini C, Semple S, Russell DG, Jackson MJ, Heyderman RS, Gordon SB. Chronic household air pollution exposure is associated with impaired alveolar macrophage function in Malawian non-smokers. PloS One. 2015;10:e0138762. doi: 10.1371/journal.pone.0138762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seow WJ, Hu W, Vermeulen R, Hosgood HD, III, Downward GS, Chapman RS, He X, Bassig BA, Kim C, Wen C, Rothman N. Household air pollution and lung cancer in China: a review of studies in Xuanwei. Chinese Journal of Cancer. 2014;33:471–475. doi: 10.5732/cjc.014.10132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha D, Ray MR. Health effects of indoor air pollution due to cooking with biomass fuel. In: Sies H, editor. Studies on Experimental Toxicology and Pharmacology. New York: Springer International Publishing; 2015. pp. 267–302. [Google Scholar]
- Smith KR. National burden of disease in India from indoor air pollution. Proceedings of the National Academy of Sciences. 2000;97:13286–13293. doi: 10.1073/pnas.97.24.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KR, Samet JM, Romieu I, Bruce N. Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax. 2000;55:518–532. doi: 10.1136/thorax.55.6.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KR, McCracken JP, Weber MW, Hubbard A, Jenny A, Thompson LM, Balmes J, Diaz A, Arana B, Bruce N. Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomized controlled trial. The Lancet. 2011;378:1717–1726. doi: 10.1016/S0140-6736(11)60921-5. [DOI] [PubMed] [Google Scholar]
- Smith-Sivertsen T, Diaz E, Pope D, Lie RT, Diaz A, McCracken J, Bakke P, Arana B, Smith KR, Bruce N. Effect of reducing indoor air pollution on women’s respiratory symptoms and lung function: the RESPIRE Randomized Trial, Guatemala. American Journal of Epidemiology. 2009;170:211–220. doi: 10.1093/aje/kwp100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank. [accessed August 3, 2016];Country At a Glance. 2016 Available: http://www.worldbank.org/en/country/malawi.
- Thompson LM, Valencia-Moscoso G, Peñaloza RA, Artiga AD, Canúz E, Smith KR, Hammond SK. Does household air pollution from cooking fires affect infant neurodevelopment? Developing methods in the NACER pilot study in rural Guatemala. The Lancet Global Health. 2014;2:S18. [Google Scholar]
- Tryner J, Wilson BD, Marchese AJ. The effects of fuel type and stove design on emissions and efficiency of natural-draft semi-gasifier biomass cookstoves. Energy for Sustainable Development. 2014;23:99–109. [Google Scholar]
- Van Gemert F, Kirenga B, Chavannes N, Kamya M, Luzige S, Musinguzi P, Turyagaruka J, Jones R, Tsiligianni I, Williams S, de Jong C. Prevalence of chronic obstructive pulmonary disease and associated risk factors in Uganda (FRESH AIR Uganda): a prospective cross- sectional observational study. The Lancet Global Health. 2015;3:e44–e51. doi: 10.1016/S2214-109X(14)70337-7. [DOI] [PubMed] [Google Scholar]
- West SK, Bates MN, Lee JS, Schaumberg DA, Lee DJ, Adair-Rohani H, Chen DF, Araj H. Is household air pollution a risk factor for eye disease? International Journal of Environmental Research and Public Health. 2013;10:5378–5398. doi: 10.3390/ijerph10115378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong JM, Nyachieo DO, Benzekri NA, Cosmas L, Ondari D, Yekta S, Montgomery JM, Williamson JM, Breiman RF. Sustained high incidence of injuries from burns in a densely populated urban slum in Kenya: an emerging public health priority. Burns. 2014;40:1194–1200. doi: 10.1016/j.burns.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yucra S, Tapia V, Steenland K, Naeher LP, Gonzales GF. Maternal exposure to biomass smoke and carbon monoxide in relation to adverse pregnancy outcome in two high altitude cities of Peru. Environmental Research. 2014;130:29–33. doi: 10.1016/j.envres.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zulu LC. The forbidden fuel: charcoal, urban woodfuel demand and supply dynamics, community forest management and woodfuel policy in Malawi. Energy Policy. 2010;38:3717–3730. [Google Scholar]