Abstract
Novel ideas are needed to increase adherence to antihypertensive medication. The current study used data from the Counseling African Americans to Control Hypertension (CAATCH) study, a sample of 442 hypertensive African Americans, to investigate the mediating effects of expectation of hypertension care, social support, hypertension knowledge, and medication adherence, adjusting for age, sex, number of medications, diabetes, education, income, employment, insurance status, and intervention. Sixty‐six percent of patients had an income of $20,000 or less and 56% had a high school education or less, with a mean age of 57 years. Greater expectation of care was associated with greater medication adherence (P=.007), and greater social support was also associated with greater medication adherence (P=.046). Analysis also showed that expectation of care mediated the relationship between hypertension knowledge and medication adherence (P<.05). Expectation of care and social support are important factors for developing interventions to increase medication adherence among blacks.
Hypertension (HTN) is a major public health problem that contributes to 1000 deaths each day, with its highest prevalence among blacks, and might explain disparities in morbidity and mortality observed between blacks and whites.1, 2 Blacks develop HTN at younger ages and have higher rates of: (1) severe HTN (ie, elevated blood pressure [BP] levels >180/110 mm Hg); (2) comorbid diseases such as type 2 diabetes mellitus (T2DM) and chronic kidney disease (CKD); and (3) are less likely to have controlled BP <140/90 mm Hg.3 These disparate outcomes explain in part why blacks have an 80% greater rate of fatal stroke, 420% greater rate of end‐stage kidney disease, and higher rates of heart disease mortalities greater than whites.3, 4 Blacks have nearly 8000 excess BP‐related deaths annually compared with whites.5
It is well documented that adequate BP control can reduce cardiovascular related mortality and provide major cardiovascular benefits, eg, fewer strokes and decreased heart failure events.6 Studies show that although blacks are prescribed more antihypertensive medications than whites, their odds of BP control were lower.5, 7 Studies examining the association between race and adherence have consistently found that blacks are more nonadherent to prescribed medications than whites or other racial and ethnic groups.8, 9, 10 In a study examining racial differences in adherence to cardiac medications in a sample of veterans, blacks had a lower adherence rate than whites (59.9% vs 74.1%; P<.001).8 Several studies have found that adherence to antihypertensive medications among blacks in the Department of Veterans Affairs healthcare system was worse compared with other racial and ethnic groups.9, 10
Of the many factors that contribute to medication nonadherence, lack of adequate HTN knowledge (a barrier) and social support (a facilitator) are the two most salient factors that can contribute to disproportionate rates of poor BP control and medication nonadherence among hypertensive blacks.11, 12, 13, 14 Unmet expectation of care is another factor associated with nonadherence to medication.15, 16, 17 Specifically, knowledge about HTN (ie, knowing the appropriate BP parameters, disease duration, and lifestyle changes required for HTN control) has been associated with greater medication adherence and better BP control.18, 19 Adequate HTN knowledge can influence patients' HTN self‐management by: (1) being more proactive in their care; (2) increasing self‐monitoring and reporting inappropriate BP readings to their provider (>140/90 mm Hg); (3) eating less salty foods; (4) engaging in more physical activities; and (5) taking appropriate prescribed medication that could help to lower their BP. Social support is also an important factor that could facilitate medication adherence.20, 21, 22 An engaged family member can motivate hypertensive patients to adhere to certain lifestyle changes, such as decreased dietary salt intake, and adherence to antihypertensive medication as prescribed.23 Another important factor related to medication adherence is patients' expectation of care, which, when solicited, may provide necessary information about adherence to prescribed treatments.15 Understanding a patient's attitude and belief about care can foster a closer patient‐provider relationship, improve patient satisfaction, and thereby improve adherence to prescribed treatment.15, 16
To our knowledge, no study has examined the influence of expectation of care on HTN knowledge, social support, and medication adherence among hypertensive patients in a minority sample. Using data from the Counseling African Americans to Control Hypertension (CAATCH) trial supported by the National Heart, Lung, and Blood Institute (NHLBI), we examined the influence of expectation of care on HTN knowledge, social support, and medication adherence among blacks. We hypothesized that expectation of care would mediate the relationship between: (1) HTN knowledge and medication adherence and (2) social support and medication adherence.
Patients and Methods
The CAATCH trial is a two‐arm cluster randomized controlled trial. Details of the study design and methodology have been described elsewhere.24 In brief, the purpose of the CAATCH trial was to compare the effectiveness of a multilevel BP control intervention vs usual care among blacks between the years 2004 and 2008.
The current paper focused on baseline sociodemographic and clinical data. Of the 1059 patients enrolled in the randomized controlled trial, 617 were excluded from this cross‐sectional study because they had missing or incomplete data on the primary study measures, resulting in a final sample of 442. The institutional review boards of Columbia University, New York University, and the Clinical Directors Network approved the study protocol. All enrolled patients provided written informed consent.
Patients were eligible for the study if they: (1) self‐identified as African American or black; (2) were 18 years or older;24 (3) were fluent in English; (4) had been diagnosed with HTN according to International Statistical Classification of Disease and Related Health Problems––Ninth Revision (code 401‐401.9) on at least two prior primary care medical visits in the previous year; (5) were taking at least one antihypertensive medication;24 and (6) had uncontrolled BP (systolic BP ≥140 mm Hg or diastolic BP ≥90 mm Hg)24 at the time of consent. BP was measured by a trained research assistant using an automated BP device BPTru (VSM model BPM‐300; Medtech, Indianapolis, IN), an automated oscillometric validated BP monitor.25, 26 Patients were excluded if they had an arm circumference >42 cm, participated in other HTN‐related trials, used home BP monitoring, had cognitive impairment determined by a Mini‐Mental Status Examination (MMSE) score <24 for those with an eighth‐grade education or higher, or an MMSE score <17 for those who had lower than an eighth‐grade education.27
Measures
Medication Adherence
Medication adherence was assessed with the Morisky Medication Adherence Scale,28, 29 a four‐item self‐report survey that measures medication‐taking behavior, consisting of yes/no responses. Questions include “Have you ever forgotten to take your BP medication?” and “When you feel badly due to the medicine, do you skip it?” A “no” answer receives a score of 0, with total scores ranging from 0 to 5. Each “yes” answer receives a score of 1, indicating a problem with adherence; thus, higher scores indicate greater nonadherence to prescribed medications. The scale has demonstrated excellent internal consistency with Cronbach's α of 0.90 using inner‐city patients with HTN.28
HTN Knowledge
HTN knowledge was assessed using a 12‐item questionnaire, which was developed by the NHLBI for use among nonmedical personnel.30 The score was developed based on the literature that evaluated HTN or cardiovascular awareness and indexes used to measure HTN knowledge related to BP.31, 32 The scores were coded as 0 for no and 1 for yes. All items were scored in the positive direction, with higher scores indicating greater HTN knowledge.
Perceived Social Support
Perceived social support was assessed with the Medical Outcomes Study survey, a self‐reported survey consisting of 19 items that represent various aspects of social support.33 Participants were asked about their ability to access various types of social support. Responses were coded using a five‐point Likert scale with responses ranging from 1, “none of the time” to 5, “all of the time.” An example of possible support would be “Someone to give you advice about a crisis.” The total scores are calculated, and higher scores indicate greater social support. The scale has excellent internal consistency reliability with Cronbach's α >0.91.33 For this study's sample, the Cronbach's α was 0.97, indicating excellent internal consistency.
Expectation of Care
Expectation of care (EOC) in hypertensive patients was assessed with the Outcome Expectations Scale, a self‐report questionnaire that consists of 20 questions (score range from 1 to 20). Higher scores indicate appropriate expectations and lower scores indicate inappropriate expectations.24 This scale is based on social learning theory, which purports that individuals' behavior is a function of how much they value the outcome of their behavior.34 For example, individuals' behavior such as taking medications, eating a low‐salt diet, and increasing physical activity, and their value for achieving optimal BP (<140/90 mm Hg) results, may or may not be highly valued at a particular time.34 Examples of outcome expectations of care questions include: “I expect the medication to control my high blood pressure;” “I will take my blood pressure medication as long as my doctor says I need it.”24 Expectation of care has been shown to improve patients' active role in their relationships with providers, invigorate negotiations with their care, and promote adherence.35 Consistent with such findings, a qualitative study found that hypertensive African Americans expected to follow their physicians' order, such as taking their medications.36
Although some information exists on what patients' expectations are for diagnostic tests, little is known about what hypertensive patients expect or what will be expected of them during treatment.37 In the current study, we sought to investigate the outcome expectations scale that provides a simple, readily applicable way of estimating what hypertensive patients expect to get from treatment, from their providers, and, in turn, what their level of involvement ought to be in treatment. For this study, the Outcome Expectations Scale had a modest but acceptable internal consistency (Cronbach's α of 0.68), which may indicate that expectations for one's behavior may not represent a singular construct.
Statistical Analysis
The purpose of this study was to examine whether expectation of care mediated the relationships of HTN knowledge and social support in adherence to antihypertensive medications among hypertensive blacks. Patient characteristics were described by using frequency and percentage distributions for categorical variables. For continuous variables, mean and standard deviations were calculated. General linear models with maximum likelihood estimation were used to examine the effects of HTN knowledge, social support, and expectation of care and control on medication adherence. We entered the outcome variable, medication adherence, predictors (HTN knowledge, social support, and expectation of care), and covariate (age, sex, number of medications, diabetes, education, yearly income, employment status, intervention status, and insurance) variables. A variable was computed for missing data and correlated with the outcome, predictors, and covariates to test whether values of these variables differed between the study sample and the total sample. In model I, the potential interaction effects among expectation of care, HTN knowledge, and social support on medication adherence were examined. Predictive variables showing a two‐tailed P value <.05 were considered to be statistically significant. We also conducted bootstrapped mediation analyses using the PROCESS macro developed by Andrew Hayes.38 Indirect and direct effects were evaluated using 95% confidence intervals (CIs).39 All analyses were performed using SPSS version 21.0 (IBM, Armonk, NY).
Results
There were no significant differences in sociodemographic variables such as age, income, insurance, and employment status among patients in the final sample of 442 compared with the total sample. We also ran comparisons between the study sample and total sample on our outcome and primary predictors. None of the correlations were significant, indicating that data were likely missing at random. The study sample had a mean age of 56.57±12.18 years, 70.4% were female, 56.6% had a high school education or less, 63% were unemployed, 91% had insurance, and 71% had an annual income of $20,000 or less as presented in Table 1.
Table 1.
Patient Characteristics (N=442)
| Characteristic | No. (%) | Mean (Standard Deviation) |
|---|---|---|
| Age, y | 56.57 (12.18) | |
| Sex | ||
| Male | 131 (29.6) | – |
| Female | 311 (70.4) | – |
| Education | ||
| <High school | 109 (24.7) | – |
| High school | 141 (31.9) | – |
| Yearly income, $ | ||
| <10,000 | 194 (43) | – |
| 10,000–20,000 | 101 (23) | – |
| >20,000 | 147 (33) | – |
| Unemployed | 278 (62.9) | – |
| Insurance | ||
| Yes | 91.9 | – |
| No | 8.1 | – |
| Medication adherence | ||
| Nonadherent | 278 (62.9) | – |
| Adherent | 164 (37.1) | – |
| Patients' self‐report measures | ||
| Adherence score | 3.67 (1.39) | |
| Hypertension knowledge | 0.884 (0.102) | |
| Social support | 3.79 (1.39) | |
| Outcome expectation | 14.4 (3.43) | |
Based on general linear model analyses controlling for treatment effect, there was no significant effect for HTN knowledge on medication adherence at baseline, while adjusting for age, sex, number of medications, diabetes, education, yearly income, employment status, intervention and insurance (estimate, 0.322; standard error [SE], 0.698; 95% CI, −1.045 to 1.690). In the same model with HTN knowledge, expectation of care and social support had significant effects on medication adherence (estimate, 0.054; SE, 0.020; CI, 0.014–0.093; estimate, 0.151; SE, 0.077; CI, 0.003–0.300), respectively. Of the covariates entered into this model, age significantly predicted medication adherence (estimate, 0.025; SE, 0.006; CI, 0.013–0.037) (Table 2).
Table 2.
Mixed‐Effects Regression Model of HTN Knowledge, Social Support, and Expectation of Outcome Care on Medication Adherence (N=442)
| Model | Variables | Estimate | Standard Error | P Value | 95% Lower | 95% Upper |
|---|---|---|---|---|---|---|
| HTN knowledge | 0.322 | 0.698 | .644 | −1.045 | 1.690 | |
| Social supporta | 0.151 | 0.077 | .046 | 0.003 | 0.300 | |
| EOCa | 0.054 | 0.020 | .007 | 0.014 | 0.093 | |
| Ageb | 0.025 | 0.006 | <.001 | 0.013 | 0.037 | |
| Male | −0.022 | 0.157 | .887 | −0.330 | 0.285 | |
| No. of medications | 0.113 | 0.068 | .098 | −0.021 | 0.246 | |
| Diabetes | −0.005 | 0.148 | .973 | −0.295 | 0.285 | |
| Education | 0.031 | 0.042 | .462 | −0.051 | 0.113 | |
| Income | −0.079 | 0.076 | .301 | −0.227 | 0.070 | |
| Employment | −0.180 | 0.170 | .288 | −0.513 | 0.152 | |
| Insurance | 0.026 | 0.250 | .917 | −0.464 | 0.516 | |
| Intervention | −0.068 | 0.144 | .224 | −0.351 | 0.215 |
Abbreviations: EOC, expectation of outcome care; HTN, hypertension. Education indicates highest earned degree; income, annual family income. a P<.05. b P<.001.
When examining for potential moderation of expectation of care with HTN knowledge on medication adherence, no significant interaction effects were found (F=1.08; P=.299; estimate, 0.156; SE, 0.150). We also found no significant interaction between expectation of care and social support in predicting adherence to medication (F=0.053; P=.817; estimate, −0.003; SE, 0.014). Using a covariate‐adjusted mediational model, we examined for the potential that expectations of care may mediate the effect of HTN knowledge on medication adherence (Figure). The results showed that expectation of care mediated the effect of HTN knowledge on medication adherence (estimate, 0.198; SE of the estimate, 0.131; 95% CI, 0.014–0.544) as presented in Table 3.
Figure 1.
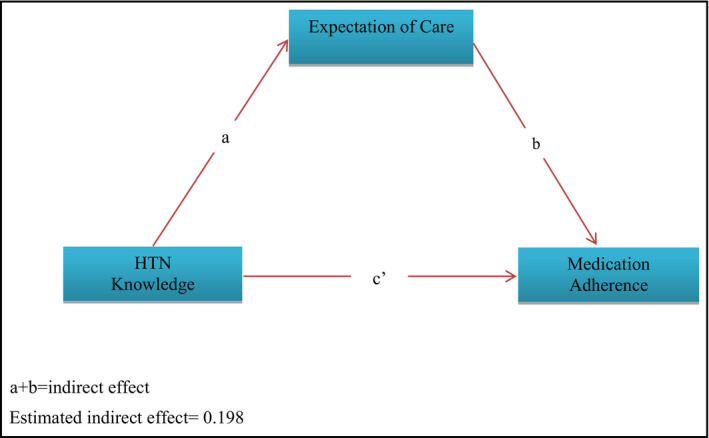
Indirect effect of expectation of care on the relationship between hypertension (HTN) knowledge and medication adherence among blacks.
Table 3.
Mediation of HTN on Adherence Through Expectation of Care
| Path | Estimate | SE of the Estimate | 95% CI |
|---|---|---|---|
| Direct (cʹ) | 0.609 | 0.661 | −0.690–1.907 |
| Indirect (a+b)a | 0.198 | 0.131 | 0.014–0.544 |
Abbreviations: CI, confidence interval; HTN, hypertension; SE, standard error.
P<.05.
Discussion
Adherence to antihypertensive medications was significantly influenced by social support and patients' expectation of their care. Although HTN knowledge did not directly impact medication adherence, it appears that the effect of HTN knowledge may have been mediated by expectation of care. Patients who perceived that they had greater social support were more likely to report that they were adherent with taking antihypertensive medications. Patients with higher expectation of their HTN care reported higher levels of medication adherence. These findings are consistent with other studies among hypertensive blacks.19, 20 In a randomized pretest and post‐test study participants (n = 1367) who had positive familial social support were significantly more likely to have higher levels of medication adherence.19 In another study with 106 participants from two urban primary care practices, social support was found to be a facilitator of medication adherence.20 In a qualitative study of African American patients with uncontrolled and controlled BP, support from family members and a positive relationship with doctors increased BP self‐management, including increased antihypertensive medication adherence.23 Results from a limited number of studies showed a positive association between expectation of care and adherence.15, 36, 40 A qualitative study of 93 hypertensive blacks showed that the majority of the sample expected that their risk for stroke, heart attack, and kidney failure would be lowered if they took their antihypertensive medications.36 Another study showed that patients who perceived an unmet expectation for care also reported less satisfaction with their visits and weaker intention to adhere to their providers' prescriptions.15 Researchers of a qualitative study of 146 hypertensive participants found that knowing patients' priorities regarding essential aspects of their care relating to adherence is important for improving HTN management.40 These findings suggest that social support and expectation of care are important factors for influencing medication adherence in hypertensive blacks.
In our study, HTN knowledge was not associated with medication adherence. Similarly, other studies have found no association with HTN knowledge and medication adherence among blacks.12, 41 On the contrary, previous studies have found associations with HTN knowledge and medication adherence, with patients with greater HTN knowledge more likely to have higher levels of medication adherence.19 Other studies have found associations between poor HTN knowledge and poor medication adherence14, 37
With expectation of care, we found mediation between HTN knowledge and medication adherence among blacks. Since we did not find any studies that examined the relationships among HTN knowledge, expectation of care, and medication adherence among blacks, we are not able to compare our findings with previous studies. The mechanisms by which expectation of care affects medication adherence are unclear and possibly complex. Some potential mechanisms including perceptions of HTN, consequences of HTN, and self‐efficacy are a function of and/or reflective of an individual's perception of their capabilities in accomplishing a specific task, a function of self‐efficacy.42 Some studies indicate that self‐efficacy is associated with medication adherence in hypertensive blacks.43, 44
In a previous study that explored patient‐related barriers to BP control, 23.4% of participants knew two or more complications of poor BP control, while 64% expected a cure from the treatment and 68.7% reported low adherence to antihypertensive medication.37 Inadequate HTN knowledge and unrealistic expectation of care negatively influences medication adherence.37 Consistent with this finding of unrealistic expectation of care, Ogedegbe and colleagues36 found that although hypertensive patients knew why they should take their antihypertensive medications (prevention of strokes, heart attacks, and kidney failure), a substantial proportion of patients had inappropriate expectations of care, such as expecting to be cured from HTN, not expecting to take their medications for life, and inconsistent medication‐taking behaviors in spite of symptoms. Unrealistic expectations of care could be reflected in patients not adhering to medications as prescribed. Evidence suggests that patients holding beliefs discordant from traditional biomedical concepts of HTN have lower medication adherence and lower BP control rates than patients with concordant beliefs.45 For this sample, both HTN knowledge and expectation of care are important factors that influence medication adherence.
Our finding that expectation of care increases medication adherence has been implied in previous studies that investigated the effect pharmacists have on improving patient engagement and adherence to medical treatment. Pharmacists' care has been shown to improve patients' BP control and satisfaction with care, as well as induce patients' beliefs that their needs are being advocated for.46 Increasing patients' expectations of care allows patients to take a more active role in their HTN management. An effective doctor‐patient relationship is another strategy that has been shown to improve patients' participation in their care. When primary care providers exhibit positive attitudes toward patients and educate them about necessary lifestyle changes, realistic patient expectation of care is likely to follow.15, 47
Another way to achieve BP control is by implementing validated standardized BP control treatment protocols for providers to treat hypertensive patients. For example, in a large‐scale observational study of 652,763 hypertensive patients in Northern California, the use of a validated BP control protocol contributed to improving BP control rates from 43.6% in 2001 to 80.4% in 2009.48 As impressive as these improvements in BP control rates are, important characteristics such as race and ethnicity have not been fully factored into evidenced‐based protocols. For example, there are certain recommended antihypertensive treatments that cause increased adverse side effects for black patients, such as swelling of the lips and coughing, that increase the likelihood of nonadherence.49 Hence, when providers assess ethnicity and race with the use of standardized high BP control protocols, adherence can be improved. In addition, when providers target interventions for patients' expectations of care, social support, and HTN knowledge, there is greater likelihood of BP control.
Age was also found to be significant in predicting antihypertensive medication adherence among this population of blacks. Findings were conflicting. Older participants were more likely to be adherent with taking their antihypertensive medications. Similarly, previous research has found an association between age and antihypertensive medication adherence, particularly for younger hypertensive blacks reporting worse adherence compared with their older black counterparts.12, 28, 43 Other studies have shown no association between age and medication adherence.41, 44 These studies used self‐report measures to assess medication adherence and the methodology involved a cross‐sectional analysis.
Study Limitations
There are some limitations that should be taken into consideration when interpreting the results of this study. The study sample consisted of predominantly low‐income black women, which prevents us from generalizing our findings to other hypertensive subgroups and populations. We therefore recommend that future studies include more men and individuals from more diverse socioeconomic backgrounds. Although our main findings are compelling, we are unable to make causal claims since we used cross‐sectional analyses. We recommend that future studies investigate the long‐term effects of expectation of care and social support on medication adherence. Additionally, since, medication adherence, expectation of care, and HTN knowledge were assessed using self‐report questionnaires, they are subject to recall bias, underestimation or over estimation of responses, and socially desirable bias in patterns of response. Furthermore, individuals diagnosed with HTN may be more exposed to, aware of, and responsive to lifestyle recommendations to manage their HTN. Even with the awareness of HTN lifestyle recommendations, it is the patient's attitude toward the health information and its consequence on their health that will promote engaged behavior. Despite these potential limitations, the rate of medication nonadherence in the current study is similar to that reported in previous studies, suggesting that our participants did not exhibit any greater or significant recall bias than other samples.
Conclusions
The study's findings suggest that social support and expectation of care influence medication adherence. HTN knowledge, when facilitated by expectations of care, influences medication adherence among hypertensive blacks. Mechanisms underlying this relationship warrant further examination. Further research should consider patients' perceptions of HTN, its treatment, and self‐efficacy in relation to medication adherence and BP control. Implications for practice would be to develop interventions to increase social support and appropriate expectations of care and to assess the adequacy of HTN knowledge. In clinical and outpatient settings, patients should be screened for nonadherence to medications, especially younger patients who may be at greater risk for medication nonadherence, and clinical staff should receive continual training on factors that contribute to adherence, such as expectation of care among blacks.
Disclosure
All authors declare that they have no proprietary, financial, professional, nor any other personal interest of any nature or kind in any product or services and/or company that could be construed or considered to be a potential conflict of interest that might have influenced the views expressed in this manuscript.
Authors' Contributions
All authors intellectually contributed to the design, analysis, and interpretation of the results and to drafting the critical review of manuscript. All authors reviewed and approved the final version of the manuscript.
Acknowledgment
This work was supported by a grant from the National Heart, Lung and Blood Institute (grant number R01 HL78566) (PI: Gbenga Ogedegbe) and the Jonas Nurse Leader Scholarship. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
J Clin Hypertens (Greenwich). 2016;18:690–696. DOI: 10.1111/jch.12736 © 2015 Wiley Periodicals, Inc.
[Correction added after initial online publication on November 23, 2015: changes have been made to author degrees and affiliations; several grammatical changes were made as well.]
References
- 1. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;128:1–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wong MD, Shapiro MF, Boscardin WJ, et al. Contribution of major disease to disparities in mortality. N Engl J Med. 2002;347:1585–1592. [DOI] [PubMed] [Google Scholar]
- 3. Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics‐2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–e146. [DOI] [PubMed] [Google Scholar]
- 4. Bosworth HB, Powers B, Grubber JM, et al. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med. 2008;23:692–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fiscella K, Holt K. Racial disparity in hypertension control: tallying the death toll. Ann Fam Med. 2008;6:497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chobanian AV, Bakris G, Black HR, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 7. Batson B, Belletti D, Wogenthan J. Effect of African American Race on hypertension management: a real world observational study among 28 US physician practices. Ethn Dis. 2010;10:409–415. [PubMed] [Google Scholar]
- 8. Charles H, Good C, Hanusa B, et al. Racial differences in adherence to cardiac medications. J Natl Med Assoc. 2003;95:17–27. [PMC free article] [PubMed] [Google Scholar]
- 9. Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the department of veterans affairs. Am J Med. 2007;120:26–32. [DOI] [PubMed] [Google Scholar]
- 10. Poon I, Lal LS, Ford ME, et al. Racial/ethnic disparities in medication use among veterans with hypertension and dementia: a national cohort study. Ann Pharmacother. 2009;43:199–206. [DOI] [PubMed] [Google Scholar]
- 11. Knight EL, Bohn RL, Wang PS, et al. Predictors of uncontrolled hypertension in ambulatory patients. Hypertension. 2001;38:809–814. [DOI] [PubMed] [Google Scholar]
- 12. Hyre AD, Krousel‐Wood MA, Muntner P, et al. Prevalence and predictors of poor antihypertensive medication adherence in urban health clinic setting. J Clin Hypertens (Greenwich). 2007;9:179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Egan BM, Lackland DT, Cutler NE. Awareness, knowledge, and attitudes of older Americans about high blood pressure: implications for health care policy, education, and research. Arch Intern Med. 2003;163:6681–6687. [DOI] [PubMed] [Google Scholar]
- 14. Douglas JG, Ferdinand KC, Bakis GL, et al. Barriers to blood pressure control in African Americans. Overcoming obstacles is challenging, but target goals can be attained. Postgrad Med. 2002;112:51–52 59–62. [DOI] [PubMed] [Google Scholar]
- 15. Bell RA, Kravitz RL, Thom D, et al. Unmet expectations for care and the patient‐physician relationship. J Gen Intern Med. 2002;17:817–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Miller RH, Williams PC, Napolitana G, et al. Malpractice: a case control study of claimants. J Gen Intern Med. 1990;5:244–248. [DOI] [PubMed] [Google Scholar]
- 17. Uhlmann RF, Inui TS, Carter WB. Patient requests and expectations. Definitions and clinical applications. Med Care. 1984;22:681–685. [DOI] [PubMed] [Google Scholar]
- 18. Kim EY, Han HR, Jeong S, et al. Does knowledge matter? Intentional medication non‐adherence among middle‐aged Korean Americans with high blood pressure. J Cardiovasc Nurs. 2007;22:397–404. [DOI] [PubMed] [Google Scholar]
- 19. Morisky DE, Ang A, Krousel‐Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008;10:348–354. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20. Ogedegbe G, Harrison M, Robbins L, et al. Barriers and facilitators of medication adherence in hypertensive African Americans: a qualitative study. Ethn Dis. 2004;14:3–13. [PubMed] [Google Scholar]
- 21. Fongwa MN, Evangelista LS, Hays RD, et al. Adherence treatment factors in hypertensive African American women. Vasc Health Risk Manag. 2008;4:157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lewis LM, Askie P, Randleman S, et al. Medication adherence beliefs of community‐dwelling hypertensive African Americans. J Cardiovasc Nurs. 2010;25:199–206. [DOI] [PubMed] [Google Scholar]
- 23. Flynn SJ, Ameling JM, Hill‐Briggs F, et al. Facilitators and barriers to hypertension self‐management in urban African Americans: perspectives of patients and family members. Patient Prefer Adherence. 2013;7:741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ogedegbe G, Tobin JN, Fernandez S, et al. Counseling African Americans to Control Hypertension (CAATCH) trial: a multi‐level intervention to improve blood pressure control in hypertensive blacks. Circ Cardiovasc Qual Outcomes. 2009;2:249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Allison C. BpTRU(tm) blood pressure monitor for use in a physician's office. Issues Emerg Health Technol. 2006;86:1–4. [PubMed] [Google Scholar]
- 26. Myers MG, Valdivieso M, Kiss A. Use of automated office blood pressure measurement to reduce the white coat response. J Hypertens. 2009;27:280–286. [DOI] [PubMed] [Google Scholar]
- 27. Crum RM, Anthony JC, Bassett SS. Population‐based norms for the Mini‐Mental State Examination by age and educational level. JAMA 1993;269:2386–2391. [PubMed] [Google Scholar]
- 28. Shea S, Misra D, Ehrlich MH, et al. Correlates of non‐adherence to hypertension treatment in an inner‐city minority population. Am J Public Health. 1992;82:1607–1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self‐reported measure of medication adherence. Med Care. 1986;24:67–74. [DOI] [PubMed] [Google Scholar]
- 30. Carter‐Edwards L, Jackson SA, Runaldue MJ, et al. Diet‐ and blood pressure‐related knowledge, attitudes, and hypertension prevalence among African Americans: KDBP study. Knowledge of diet and blood pressure. Ethn Dis 2002;12:S1‐72–82. [PubMed] [Google Scholar]
- 31. Ford ES, Jones DH. Cardiovascular health knowledge in the United States: findings from the National Health Interview Survey, 1985. Prev Med. 1991;20:725–736. [DOI] [PubMed] [Google Scholar]
- 32. National High Blood Pressure Education Program (NHBPEP) . Check Your High Blood Pressure Prevention IQ (Questionnaire). Bethesda, MD: US‐DHHS; 1994, NIH Publi. No. 94‐3471. [Google Scholar]
- 33. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. [DOI] [PubMed] [Google Scholar]
- 34. Rotter JB. Social Learning and Clinical Psychology. New York: Prentice‐Hall; 1954. [Google Scholar]
- 35. Lazare A, Eisenthal S, Frank A. Clinician/patient relations II: conflict and negotiation. In: Lazare A, ed. Outpatient Psychiatry: Diagnosis and Treatment. Baltimore, MD: Williams and Wilkins; 1989:137–152. [Google Scholar]
- 36. Ogedegbe G, Mancuso CA, Allegrante JP. Expectations of blood pressure management in hypertensive African‐American patients: a qualitative study. J Natl Med Assoc. 2004;96:442–449. [PMC free article] [PubMed] [Google Scholar]
- 37. Okwuonu CG, Ojimadu NE, Okaka EI, et al. Patient‐related barriers to hypertension control in a Nigerian population. Int J Gen Med. 2014;7:345–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression‐Based Approach. New York: Guildford Press; 2014. [Google Scholar]
- 39. Preacher KJ, Hayes AF. SPSS and SAS Procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. [DOI] [PubMed] [Google Scholar]
- 40. Gascón JJ, Sánchez‐Ortuño M, Llor B, et al. Why hypertensive patients do not comply with the treatment: results from a qualitative study. Fam Pract. 2004;21:125–130. [DOI] [PubMed] [Google Scholar]
- 41. Kressin NR, Wang F, Long J, et al. Hypertensive patients' race, health beliefs, process of care, and medication adherence. J Gen Intern Med. 2007;22:768–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bandura A. Self‐efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. [DOI] [PubMed] [Google Scholar]
- 43. Lewis LM, Schoenthaler AM, Ogedegbe G. Patient factors, but not provider and health care system factors, predict medication adherence in hypertensive black men. J Clin Hypertens (Greenwich). 2012;14:250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schoenthaler A, Ogedegbe G, Allegrante JP. Self‐efficacy mediates the relationship between depressive symptoms and medication adherence among hypertensive African Americans. Health Educ Behav 2009;36:127–137. [DOI] [PubMed] [Google Scholar]
- 45. Heurtin‐Roberts S, Reisin E. The relation of culturally influenced lay models of hypertension to compliance with treatment. Am J Hypertens. 1992;5:787–792. [DOI] [PubMed] [Google Scholar]
- 46. Wal P, Wal A, Bhandari A, et al. Pharmacist involvement in the patient care improves outcome in hypertension patients. J Res Pharm Pract. 2013;2:123–129. doi: 10.4103/2279-042X.122386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rashid A, Rahman A, Wang J, et al. Perception of hypertension management by patients and doctors in Asia: potential to improve blood pressure control. Asia Pac Fam Med. 2015;14:2–11. doi: 10.1186/s12930-015-0018-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jaffe MG, Lee GA, Young JD, et al. Improved blood pressure control associated with a large‐scale hypertension program. JAMA. 2013;310:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bangalore S, Ogedegbe G, Gyamfi J, et al. Outcomes with angiotensin‐converting enzyme inhibitors vs other antihypertensive agents in hypertensive blacks. Am J Med. 2015; 9343; 00445–3. [DOI] [PubMed] [Google Scholar]


