Abstract
Introduction:
Alveolar osteitis (AO) is a complication of tooth extraction which indicates inflammation of alveolar bone of either maxilla or mandible. This study uses Apitherapy where honey catalyses biological reactions to improve immune system, makes local environment unbearable for microorganisms in the affected socket and enhances healing.
Materials and Methods:
50 patients of AO were included in the study. After cleansing of the affected socket, honey dressing was applied. Dressings were changed daily for first 2 days and then altenatively. In biochemical investigations, CRP levels in the body were measured using Nephelometry method. Microbiological examination was done for the identification of microorganism and semi quantitative count of colony forming units.
Result:
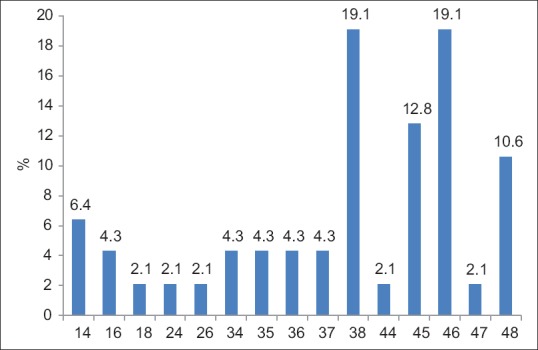
Results were assessed from clinical, microbiological, biochemical and radiological findings at 1st, 2nd, 3rd, 5th, 7th day based on VAS score, erythema, pus discharge, swelling, lymphadenitis, fever, bleeding on probing, exposed bone and necrotic debris. Pre-Treatment CRP was 2.08 ± 1.62 which significantly (P = 0.0001) decreased to 0.82 ± 0.48. Mean change and average percentage change were 1.25 ± 1.51 and 44.1% respectively.
Conclusion:
Majority of the patients with exposed bone got healed socket with evidance of granulation tissue and healing gingiva in about one week. CRP levels at the completion of treatment of AO with honey dressing showed a significant decrease from the pre-treatment values indicating fast recovery. Microbiological examination showed presence of normal commensal flora at AO sites like Streptococcus, Staphyloccocus and Enterococcus. So, the role of bacteria in the genesis of AO, if any, appears unclear.
Key words: Alveolar osteitis, C-reactive protein, dry socket, honey
INTRODUCTION
Alveolar osteitis (AO) is a complication of tooth extraction. It indicates inflammation of alveolar bone of either maxilla or mandible. This usually occurs in extraction socket where the blood clot is not formed or is dislodged. Hence, the empty socket is now exposed to the oral environment resulting in inflammation of lamina dura. Fibrinolysis is disruption of clot caused by the formation of kinins and plasmin.
A recent definition of the dry socket includes the development of postoperative pain around the alveolus that becomes worse 1–3 days after an extraction and is followed by partial or total loss of the clot in the alveolar interior and can be accompanied by halitosis. The intense pain radiates to the ear and neck and does not respond to analgesics. Other common symptoms include headache, insomnia, dizziness, trismus, and regional lymphadenopathy.[1]
A successful dentoalveolar surgery requires precise diagnosis and meticulous surgical technique. Furthermore, factors affecting various biological events influence it. Earlier various topical agents having medicinal properties were placed into extraction socket to enhance healing along with decreasing postoperative pain.[2]
Apitherapy uses honey which catalyses biological reactions to improve the immune system and makes local environment unbearable for microorganisms.
The philosophy of using honey in dry socket was derived from the basic research and clinical observation of the rapid epithelization in tissue injuries, coating the wound with honey retards tissue oxygenation by sealing the damaged mucosa from air (oxygen) this would dampen pain within 30 s after application.[3]
The important factors that influence the effectiveness of honey are its hygroscopic nature; acidic pH prevents bacterial growth when applied to the mucosa and inhibin (hydrogen peroxide) converted from glucose oxidase and gluconic acid, enzyme growth factors, and tissue nutritive minerals and vitamins help tissue repair directly.
Honey has shown to decrease the C-reactive protein (CRP) levels without affecting on blood glucose, insulin, and lipid levels, especially in diabetic and hyperlipidemic cases. The research has also revealed that honey is powerful even against drug-resistant hospital killer golden staph Staphylococcus aureus. It painlessly removes pus, scabs, and dead tissue from wounds and stimulates new tissue growth.
MATERIALS AND METHODS
Ethical committee
Approval of research “Effects of honey in the management of alveolar osteitis: A study” is given by the Ethical Committee of King George's Medical University (KGMU), Uttar Pradesh, Ref. code: 69 ECM IIB/P17.
The present study is comprised fifty patients who reported to the Outpatient Department (OPD) of Oral and Maxillofacial Surgery, Faculty of Dental Science, KGMU, Lucknow, from April 2013 to July 2014.
Patient selection
Inclusion criteria
Strict inclusion criteria were used, irrespective of age, gender, caste, and creed. All selected patients were informed about the experimental nature of the study and the possible complications were explained. Their cooperation was solicited, and a written consent was obtained before involving in the study.
The study group consists of the patients having AO. The diagnosis of AO was made based on the clinical signs, symptoms, and X-ray.
Exclusion criteria
Patients with systemic illness such as diabetes, cardiovascular diseases, pregnant and lactating female, and patients suffering from any other bacterial and fungal infection and taking any oral drug. Moreover, patients having symptoms similar to dry socket due to retained root pieces, oroantral communication, or any bony or soft tissue pathology were excluded from the study.
Radiological assessment
X-rays were performed in the Department of Oral Medicine and Radiology, Faculty of Dental Sciences, KGMU.
Intraoral periapical radiograph was taken from the respective area to visualize the condition of the socket, any bony pathology, retained root pieces, and presence of oroantral communication. In questionable cases, orthopantomogram was performed to visualize the basal bone.
The study group, comprising minimum of fifty patients, shall be selected from the patients attending OPD of Oral and Maxillofacial Surgery, Faculty of Dental Sciences, KGMU, Lucknow.
All the selected patients were diagnosed cases of dry socket. The treatment involved cleaning of the affected socket with autoclaved cotton pellets to remove any debris. The dry socket was found to be covered with food remnants, soft plaque, bony flecks, or any tooth or calculus debris. Sterile autoclaved cotton swab stick was taken. It was swabbed through the socket and placed into the culture tube. Then, the socket was thoroughly irrigated with normal saline. The bare bone was exposed which was without any covering of healing granulation tissue.
Honey dressing was prepared by mixing pure honey with sterilized cotton. This purest form of honey was procured from the National Botanical Research Institute, Lucknow. Honey was stored in cool and dry conditions. The involved socket was isolated from rest of the oral cavity and its secretions by dry autoclaved cotton rolls. Then, a small honey pellet was made. It was placed in the dry socket with all aseptic precautions with the help of tweezers and retracting the tissues with mouth mirror. Dressings were changed daily for first 2 days of starting honey dressing and then from third dressing onward it was changed every alternate day.
On starting and completion of treatment, a blood sample was sent for biochemical examination. The swab stick was for microbiological examination. Follow-up of all the patients was done on day 1, 2, 3, 5, 7, and 15th day.
Biochemical investigations
CRP levels in the body have been used as a marker or indicator of infections and inflammation. Quantitative determination of CRP will be performed in human serum/plasma.
Biochemical procedure
CRP levels at the start of treatment and after completion of treatment with honey dressing.
Clinical significance
CRP is a cytokine-induced, acute phase protein that increases in concentration as a result of inflammation. CRP levels in the body have been used as a marker of infections and inflammations. The assay of CRP is more sensitive than erythrocyte sedimentation rate and leukocyte count. The CRP levels return to reference ranges more rapidly after the disease has subsided.
Nephelometry method
The reagent is intended for in vitro quantitative determination of CRP in human serum or plasma:
Linear up to 320 mg/L
Ready to use reagents
No sample dilution is needed
No calibration is required
Lower detection limit of 0.5 mg/L.
Principle
This is a latex-enhanced turbid metric immunoassay. CRP samples binds to specific anti-CRP antibodies, which have been adsorbed to latex particles and agglutinates. The agglutination is directly proportional to the quantity of CRP in the sample.
-
Reagent composition
CRP R1-1 × 5.3 ml
-
Glycine buffer
CRP R2-1 × 5.3 ml.
Latex suspension coated with anti-CRP antibodies (rabbit polyclonal antibody).
Storage and stability
The sealed reagents are stable up to the expiry date given by the manufacturer, when stored at 2–8°C.
Linearity
The reagent is linear up to 320 mg/L. If the concentration is greater than linearity, dilute the sample with normal saline and repeat the assay. Multiply the result with dilution factor.
Reference range
The following value may be used as a guideline:
Serum up to 6 mg/L.
Sample
Fresh serum (hemolyzed or lipemic sample was not used).
Precautions
Bring the reagents to room temperature before use
To avoid contamination, clean laboratory wares were used. Direct exposure of reagent to light was avoided.
Procedure
Step 1: Insert card-to-card reader slot and display will prompt to add R1 + sample
Step 2: Pipette 150 µL R1 and 5 µL sample to cuvette and place the cuvette into cuvette holder
Step 3: After incubation, display will prompt to add R2
Step 4: Pipette 150 µL R2 using attached sensor pipette to the cuvette
Step 5: The result will show in the display and print out.
Performance characteristics
Measuring range: 0.5–320 mg/L
Lower detection limit: 0.5 mg/L.
Precision
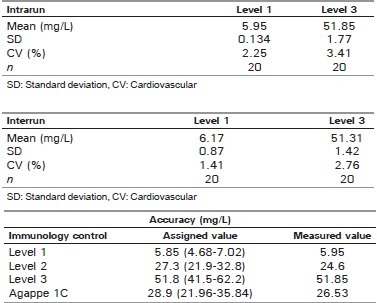
Interferences
Do not interfere for:
Hemoglobin up to 500 mg/dL
Bilirubin up to 10 mg/dL
Intrafat up to 500 mg/dL
Rheumatoid factor up to 500 mg/dL.
Microbiological examination
Methodology
Swab stick was immediately streaked on blood agar for identification of microorganism and semi-quantitative count of colony forming units
First streaking was done across the culture plate and then perpendicular to the first streak
Cultured plate was incubated at 37°C for 18–24 h
Colonies were differentiated on the basis of morphology, hemolysis, and Gram-staining
To get isolated colonies for identification purpose, subculture was done on the blood agar and nutrient agar in case of Gram-positive bacteria and on the MacConkey agar in case of Gram-negative bacteria
Single specific colony was picked up and subcultured. Loop was heated after every streak to get pure colonies
Isolated colonies were identified on the basis of colony morphology, Gram-stain, and biochemical tests.
Culture media
Following culture medias were used to grow and identify the microorganism.
Nutrient agar
Nutrient agar is the simple medium; many bacteria grow easily on it and provide the base for many other media. Mixed or isolated colonies are subcultured on it to see the pigment production and to perform a biochemical test which is interfered with the presence of blood like catalase test which is used to differentiate Streptococcus species from Staphylococcus species. Following ingredients are used to prepare the medium:
Peptone – 10 g
Meat extract – 10 g
Sodium chloride – 5 g
Water – 1 L.
To prepare nutrient agar, desired amount of peptone, meat extract, and sodium chloride were mixed in 1000 ml of water. Ingredients were dissolved by gentle heating; pH was made 7.5 and sterilized by autoclaving at 121°C for 15 min. Twenty-five milliliter medium was poured in 9 cm Petri dish, allowed to set, and storage is maintained at 4–8°C.
Blood agar
Blood agar is an enriched medium which supports the growth of most of the bacteria and also acts as indicator medium showing the hemolytic properties of Streptococcus species. The medium was prepared by adding sterile blood to sterile nutrient agar which has cooled just as 50°C. Ten percent was the usual concentration. Human, horse, or sheep blood is mostly used in blood agar.
MacConkey agar
It was used as a differential medium to distinguish the lactose fermenting colonies from nonlactose fermenting in Gram-negative bacteria.
Peptone – 20 g
Sodium taurocholate – 5 g
Water – 1 L
Agar – 20 g
Neutral red solution – 3.5 ml
Lactose 10% aqueous solution – 100 ml.
Peptone and sodium taurocholate were dissolved in the water by heating, agar was added and dissolved by steaming. pH was adjusted at 7.5. Well mixed lactose and neutral red were added to it and autoclaved with free steam at 100°C for 1 h, then at 115°C for 15 min. Medium was poured and stored as above.
Assessment criteria
Results were assessed on the basis of clinical, microbiological, biochemical, and radiological findings at 1, 2, 3, 5, and 7th day based on the following parameters:
Pain grades – visual analog scale (VAS) 0–10
-
Erythema
- Absent = 0
- minimal = 1+
- Mild = 2+
- Moderate = 3+
- Severe = 4+
-
Swelling
- Absent = 0
- Mild = 1
- Moderate = 2
- Severe = 3
-
Pus discharge
- Present = 1+
- Absent = 2+
-
Lymphadenitis
- Present = 1+
- Absent = 2+
-
Fever
- Present = 1+
- Absent = 2+
-
Bleeding on probing
- Present = 1+
- Absent = 2+
-
Exposed bone
- Present = 1+
- Absent = 2+
-
Necrotic debris
- Present = 1+
- Absent = 2+.
Statistical analysis
The following statistical tools were employed for the present study.
Mean
Mean was calculated as the central tendency of a group using the following formula:

where X = Mean score, n = Number of samples.
Standard deviation
Most frequently used, measure of dispersion, denoted by standard deviation (SD) and is calculated as:
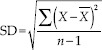
where X̄ = Individual value for the parameter, X = Arithmetic mean, n = Number of observations.
Paired t-test
This was done to see the difference between pre- and post-experiment values. The following formula was employed:
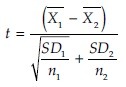
Where X̄ = Mean 1, X2 = Mean 2, SD1 = Standard deviation 1, SD2 = Standard deviation 2, n1 = Number of values in Group A, n2 = Number of values in Group B.
McNemar's test
In statistics, McNemar's test is a statistical test used on paired nominal data. It is applied to 2 × 2 contingency tables with a dichotomous trait, with matched pairs of cases, to determine whether the row and column marginal frequencies are equal (that is, whether there is “marginal homogeneity”).
The test is applied to a 2 × 2 contingency table, which tabulates the outcomes of two tests on a sample of n subjects, as follows:
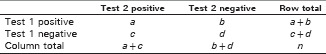
The null hypothesis of marginal homogeneity states that the two marginal probabilities for each outcome are the same, i.e., pa + pb = pa + pc and pc + pd = pb + pd.
Thus, the null and alternative hypotheses are:
H0: pb = pc
H1: pb ≠ pc.
Here, pa, etc., denote the theoretical probability of occurrences in cells with the corresponding label.
The McNemar's test statistic is:

OBSERVATION AND RESULTS
The present study included fifty patients of AO diagnosed in the OPD of Oral and Maxillofacial Surgery, Faculty of Dental Sciences, KGMU, Lucknow.
The patients were taken up randomly irrespective of age, sex, caste, creed, and socioeconomic status. Of the 50 patients, 47 patients completed the follow-up visit after 1 week of initial examination and starting of treatment.
The mean age of the patients was 34.60 ± 11.99 years with a range from 18 to 62 years. More than one-third of the patients were between 30 and 40 years (40.4%) followed by <30 (34%) and >40 (25.5%) years [Table 1 and Figure 1].
Table 1.
Distribution of patients according to age
Figure 1.
Distribution of patients according to age
More than half (53.2%) of the patients were males [Table 2 and Figure 2].
Table 2.
Distribution of patients according to gender
Figure 2.
Distribution of patients according to gender
The percentage of location of AO was 19.1% in the extraction sockets of mandibular left third molar and mandibular right first molar. It was followed by 12.8% at mandibular right premolar and 10.6% at mandibular right third molar. The percentage of other location of AO was <10% [Table 3 and Figure 3].
Table 3.
Distribution of patients according to location of teeth
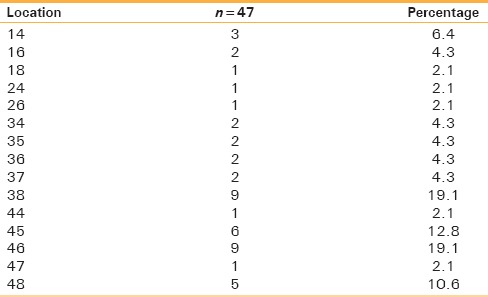
Figure 3.
Distribution of patients according to location of teeth
The pretreatment CRP was 2.08 ± 1.62 which significantly (P = 0.0001) decreased to 0.82 ± 0.48. The mean change and average percentage change were 1.25 ± 1.51 and 44.1%, respectively [Table 4 and Figure 4].
Table 4.
Comparison of change in C-reactive protein level
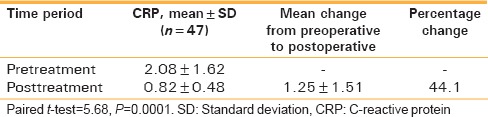
Figure 4.
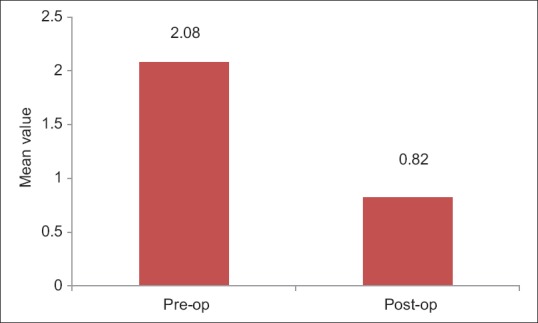
Comparison of change in C-reactive protein level
The intensity of pain (VAS) was 7.32 ± 1.16 at day 1 which decreased to 4.74 ± 1.18 at day 2, to 2.21 ± 0.80 at day 3 and to 0.72 ± 0.59 at day 5. This decrease was found to be statistically significant (P = 0.0001). The decrease was higher at day 5 from day 1 than day 2 and day 3 [Table 5 and Figure 5].
Table 5.
Comparison of intensity of pain (visual analog scale)
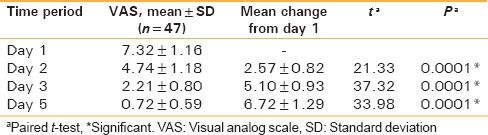
Figure 5.
Comparison of intensity of pain (visual analog scale)
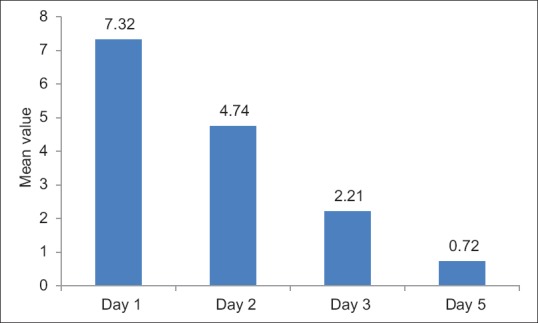
The average percent change in intensity of pain (VAS) was 90.1% at day 5 from day 1 which was 70.1% at day 3 and 35.6% at day 2 [Table 6 and Figure 6].
Table 6.
Average percent change in intensity of pain (visual analog scale) from day 1 to day 2, 3 and 5
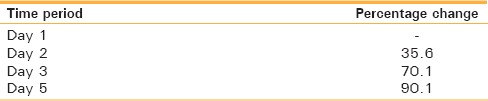
Figure 6.
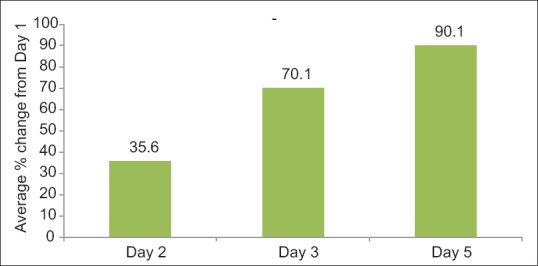
Average percent change in intensity of pain (visual analog scale) from day 1 to day 2, 3, and 5
A significant decreased in erythema was observed from day 1 to day 2 (P = 0.001), day 3 (P = 0.0001), and day 5 (P = 0.0001). The decrease was higher at day 5 from day 1 than day 2 and day 3 [Table 7 and Figure 7].
Table 7.
Comparison of erythema
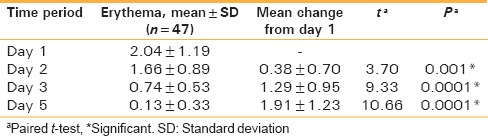
Figure 7.
Comparison of erythema
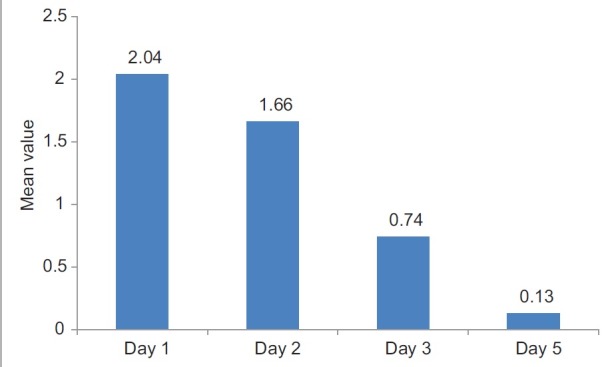
The average percent change in erythema was 94.4% at day 5 from day 1 which was 61.8% at day 3 and 12.9% at day 2 [Table 8 and Figure 8].
Table 8.
Average percent change in erythema from day 1 to day 2, 3, and 5

Figure 8.
Average percent change in erythema from day 1 to day 2, 3 and day 5
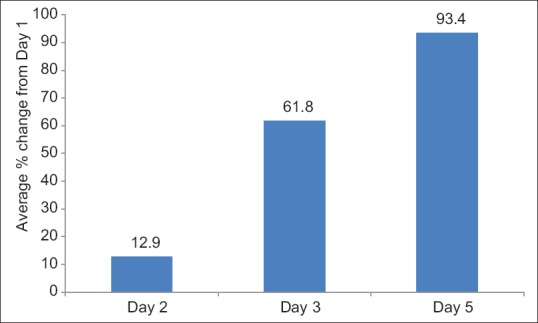
The swelling was 1.81 ± 1.37 at day 1 which decreased to 1.28 ± 1.13 at day 2, to 0.79 ± 0.80 at day 3 and to 0.23 ± 0.42 at day 5. This decrease was found to be statistically significant (P = 0.0001). The decrease was higher at day 5 from day 1 than day 2 and day 3 [Table 9 and Figure 9].
Table 9.
Comparison of swelling
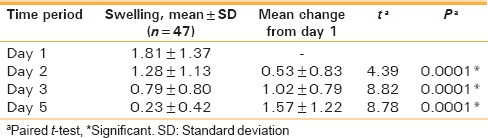
Figure 9.
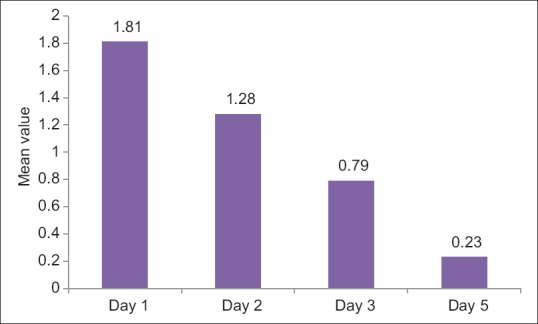
Comparison of swelling
The average percent change in swelling was 88.8% at day 5 from day 1 which was 62.6% at day 3 and 25.2% at day 2 [Table 10 and Figure 10].
Table 10.
Average percent change in swelling from day 1 to day 2, 3, and 5
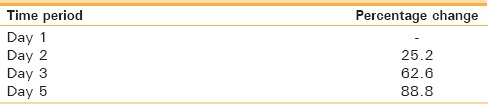
Figure 10.
Average percent change in swelling from day 1 to day 2, 3 and day 5
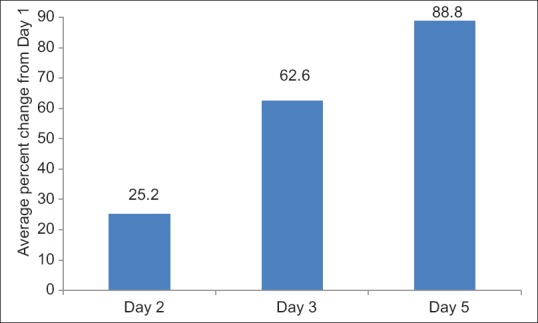
The pus discharge was present only at day 1 (6.4%) and day 5 (8.5%). However, Lymphadenitis was present at day 1 and day 2 (10.6%) which became nil at day 3 and day 5. Fever was present in only one patient at day 1 and absent in the subsequent days. Bleeding on probing was present at day 1 (85.1%). It gradually decreased on day 2 (80.9%), on day 5 it was reduced to 0%. Exposed bone was present on day 1 (74.5%). On day 2, it was 80.9% whereas on day 5, it decreased to 10.6% of patients. Necrotic debris on day 1 was 89.4% of patients which drastically reduced to 27.7% on day 2 [Table 11 and Figure 11].
Table 11.
Comparison of presence of clinical symptoms
Figure 11.
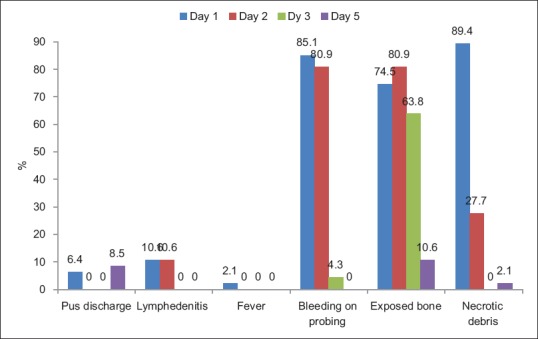
Comparison of presence of clinical symptoms
Streptococcus was found among 51.9% of the patients and Staphylococcus was found in 29.6% of the patients. However, both Streptococcus and Staphylococcus were in 11.1% of the patients. The percentage of Enterococcus was 7.4% all are normal commensal flora of mouth [Table 12 and Figure 12].
Table 12.
Distribution of patients according to organism
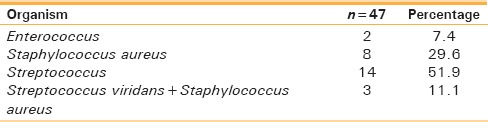
Figure 12.
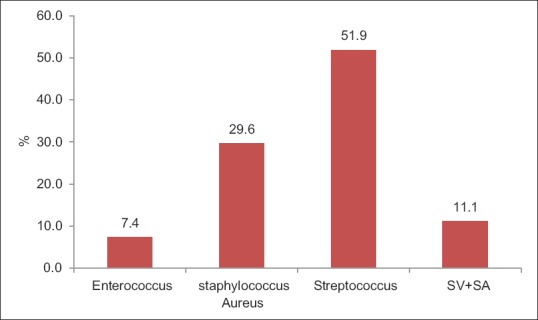
Distribution of patients according to organism
DISCUSSION
Despite the use of various regimens to reduce its occurrence, AO continues to be a common adverse event associated with the extraction of teeth.
According to Birn in 1973,[4] the extraction process traumatizes the tissue and releases tissue activators that diffuse into the blood clot and convert plasminogen to plasmin. This dissolves the clot, releases kinins, and produces pain.[2] Pain of AO is genuinely severe as is proved in our study. Twenty percent of patients had VAS score 10 and 60% of patients had a score of 7 on VAS scale on the 1st day of clinical examination. This pain poorly responds to over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) and narcotic analgesics.[5] Choice of analgesics varies from a short course of NSAIDs to narcotic-based preparations such as acetaminophen with codeine, hydroxycodone, or oxycodone. Most authors presently do not recommend curetting the socket as a means of eliciting bleeding because this procedure can increase pain.
From under 1% to 21% of extractions are complicated by dry socket with more cases occurring when third molars are removed. In seeking a simple, easily administered definitive treatment that general dental practitioners can apply safely in cases of AO; the intra-alveolar application of honey dressing was investigated.
Author came up with a descriptive definition that could be used universally as a standardized definition for AO: postoperative pain in and around the extraction site, which increases in severity at any time between 1 and 3 days after the extraction accompanied by a partially or totally disintegrated blood clot within the alveolar socket with or without halitosis. It is necessary to exclude any other cause of pain on the same side of the face. Occasionally, patients may also complain of a very unpleasant taste.[3]
The denuded alveolar bone may be painful and tender. We found that on the 1st day of clinical presentation exposed bone was present in 74.5% of patients. After thorough irrigation on the 1st day of treatment, it was found that some socket bone covered with debris was exposed as clean denuded bone. Hence, on day 2, exposed bone was in 80.9% of patients. Some patients may also complain of continuous intense pain irradiating from the empty socket, normally to the ipsilateral ear, temporal region, or the eye.
Regional lymphadenopathy is also noted occasionally in AO. However, in our study, lymphadenitis was present at day 1 and day 2 in 10.6% of patients which became nil at day 3 and day 5. Fever was present in only one patient at day 1 and absent in the subsequent days of treatment with honey dressing and its follow-up. Lymphadenitis, pus discharge, and fever were found in those patients where there was a history of difficult extraction and significant trauma to adjacent bone and gingiva. Surgical experience and the degree of traumatic insult are contributing factors as witnessed by our observations.[6]
Trauma is postulated to result in compression of the bone lining the socket, as well as possible thrombosis of the underlying vessels, reducing blood perfusion. Some associate trauma with a reduction in tissue resistance and consequently wound infection by anaerobes. Birn in 1973 relates damage to cells and alveolar bone to release of tissue activators of fibrinolytic activity (factor XII or Hageman factor, urokinase from blood, tissue, and endothelial plasminogen activators).[5]
Trismus is a rare occurrence, but in cases of mandibular third molar extractions, it is sometimes seen and is probably due to lengthy and traumatic surgery and not due to the pathophysiology of AO. Trismus after third molar surgery is usually caused by inflammation of the muscles of mastication leading to spasm secondary to the raising of a mucoperiosteal flap.[7]
In our study, results showed that more than half (53.2%) of the patients of AO participating in the study were males compared to females (46.8%). However, review of most of studies showed significantly higher incidence of AO occurring in females.[3] This can also be attributed to small sample size of the study.[5]
Most literature supports that dry socket rarely occurs in childhood and that incidence increases with the patient's age. The mean age of the patients in our study was 34.60 ± 11.99 years with a range from 18 to 62 years. More than one-third of the patients were between 30 and 40 years (40.4%). McGregor's follow-up study (1968) placed the highest incidence in the third and fourth decades of life. However, the prevalence of smoking in that age bracket might be a confounding factor.[5,6]
The incidence of AO found in this study was maximum in mandibular molars followed by mandibular premolars. This was consistent with the study carried out by Patrick J. Vezeau (2000). The percentage of location of AO was 19.1% in the extraction sockets of mandibular left third molar and mandibular right first molar. It was followed by 12.8% at mandibular right premolar and 10.6% at mandibular right third molar. The percentage of other location of AO was <10%. The incidence of dry socket is higher in the mandible, occurring up to 10 times more often for mandibular molars compared with maxillary molars.[5] This can also be attributed to the compact nature of posterior mandible as compared to the spongy type of maxillary bone.
A significant decrease in erythema over surrounding gingival tissues was observed from day 1 to day 2 (P = 0.001), day 3 and day 5.
The swelling on day 2 reduced to 25.2% from the 1st day of clinical examination and continued to decrease on follow-up visits. This decrease was found to be statistically significant (P = 0.0001). The average percent change in swelling was 88.8% at day 5 from day 1 which was 62.6% at day 3.
The pus discharge was present only at day 1 in 6.4% of patients with AO which dropped down to 0% after starting of honey dressing on subsequent days.
Bleeding on probing was present at day 1 (85.1%). It gradually decreased on day 2 (80.9%); on day 5, it was reduced to 0%.
Exposed bone was present on day 1 (74.5%); on day 5 of honey dressing, it decreased to 10.6% of patients.
Necrotic debris on day 1 was 89.4% of patients which drastically reduced to 27.7% on day 2 after through and profuse irrigation of dry sockets with normal saline.
These all clinical findings of our study correlate with the study carried out by Moghazy et al. where he had used bee honey dressing in the treatment of diabetic foot ulcer and noted the change in the ulcer size throughout the whole period of follow-up. The ulcer size decreased, with highly significant statistics rates. The study results proved that honey was an easy-to-use debriding agent. Honey impregnated gauze had rapidly cleansed the wounds from debris without the need for enzymatic, chemical or massive mechanical debridement. It was perfect in filling cavities and sinuses within the deep diabetic foot wounds. This study revealed rapid diminution of the inflammatory signs (e.g., edema, hotness, and redness) within 10 days in all patients. This was partially due to its antiedema effect and partially to its antimicrobial effect.[8]
No hospital-acquired infection was detected in their series. This might be referred to the viscosity of honey, which provided a protective barrier thus preventing cross-infection.
Honey-impregnated cotton pellet is easy to prepare (even by the patients or their relatives) and to apply. It can be removed off easily without pain or damage to the newly forming granulation tissue.
All these factors, in addition to the stimulating effect of honey on granulation tissue and epithelialization, resulted in rapid absorption of edema (from the wound and surrounding area), diminution of discharge, deodorization of the wound as early as 5th day. This rapid dramatic response might explain the perfect patient compliance throughout the whole period of the study.
The results from our study correlates with the study carried out by Subrahmanyam (1996). The high sugar content of honey renders it hyperosmolar. Due to this, it causes rapid absorption of edema fluid from the surrounding swollen gingival tissues. The viscosity of honey is high, and it forms a physical barrier which prevents bacterial colonization of wound. Chemical debridement action of honey is effective, and there is no need for surgical debridement. The antibacterial effects of honey also have been attributed to hydrogen peroxide. Due to the presence of the enzyme glucose oxidase from the hypopharyngeal glands of the bee, hydrogen peroxide accumulates in diluted honey. This helps in debridement of the wound due to the Fenton reaction; it can easily produce free hydroxyl radicals with a bactericidal effect. The antibacterial activity of honey may also be due to the low pH (3.6) and hygroscopic properties of honey. Due to the hygroscopic property of honey, bacteria are dehydrated and become inactive. The viscous barrier formed by honey creates a moist environment which helps in quicker wound healing. The nutrient contents of honey, such as levulose and fructose, improve the local nutrition and promote rapid epithelialization.[8]
Biochemically, the anti-inflammatory properties of honey were supported by decrease in CRP values after healing of dry sockets with honey dressing from pretreatment values.
CRP testing was performed in the research laboratory of biochemistry department using latex-enhanced turbidimetric immunoassay, which required a phlebotomy to collect 2 ml of whole blood sample first before starting treatment of AO and then after completion of treatment with honey dressing. Nephelometry method was carried out to analyze the serum CRP levels.
The findings of the present study indicated that serum CRP levels are often elevated in patients with odontogenic infections and postoperative complications following tooth extraction like AO. Approximately, 22% of the dental OPD patients enrolled in the study had serum CRP levels >3 mg/L. Rapid reduction in serum CRP levels was likely to occur following successful treatment of AO. Such elevation in CRP levels may be transient in some patients but more persistent in others. CRP levels may remain high after the resolution of clinical symptoms, especially in patients with periodontal abscesses or postoperative AO. Persistence in high serum CRP levels may be a useful marker indicative of underlying tissue damage in these patients.
The posttreatment CRP with honey dressing showed a significant decrease from the pretreatment CRP values with the average percentage change of 44.1%.
Serum CRP is nearly absent in healthy individuals and increases significantly when tissue damage occurs during infection, tissue injuries, or inflammation. The results of the present study provide preliminary data on serum CRP levels in patients with AO.
Bloomer recently showed that dry socket can be prevented by immediately packing sockets with a eugenol-containing dressing. However, such measures also are known to delay wound healing. Similarly, Turner (1982) used the reflection of a flap, removal of bone particles, curettage, and removal of granulation tissue with irrigation and found that this method required fewer visits than zinc oxide–eugenol or iodoform gauze with eugenol techniques. Turner (1982) also stated that packing of the socket could delay socket healing and increase the risk of an infection. Irrigation is known to remove debris, sequestra, and bacteria from the denuded bone. The use of petroleum-based carriers is discouraged to avoid myospherulosis, a complication of wound healing by the action of lipids on extravasated erythrocytes.[5,9]
The viridans streptococci are a large group of commensal streptococcal bacteria species that are either α-hemolytic, producing a green coloration on blood agar plates (hence the name “viridans,” from Latin “vĭrĭdis,” green), or nonhemolytic. In our study, S. aureus was present in 29.6% of patients, Streptococcus was found in 51.8% of patients, Enterococcus was in 7.4% of patients, and both Streptococcus and Staphylococcus was present in 11.1% of patients. These are all normal commensal flora of mouth.
There has been considerable debate as to whether bacteria play a role in the origin of the fibrinolytic process. Jensen (1978) labeled the role as “unclear.” Nitzan (1983) noted that commonly found bacteria are incapable of lysing clots. Noted that bacterial counts are elevated in AO sites, but this has not been translated to a proven cause-effect relationship. Trieger and Schlagel (1991) expressed the belief that anaerobic bacteria are involved but offered only indirect evidence.[6]
Finally, Treponema denticola exhibits plasmin-like fibrinolytic activity while other common oral bacteria have little such innate activity and is a late colonizer of the mouth, which implicated it further because dry socket rarely occurs in childhood. No papers, however, have been able to support a direct cause-effect relationship between bacteria and dry socket.[5]
In short, the role of bacteria in the genesis of AO, if any, appears unclear, and more data are needed from future, well-designed studies. Due to its acidic pH, honey can cause unpleasant or even painful feelings during application or ingestion that may limit its use. Allergy to honey or its ingredients and pollutants is extremely rare but possible. In our study, honey was well accepted by the patients. There was no report of any allergic or untoward reactions to honey in any patient.
The psychological factor is an important aspect in improving and impeding immunity and healing power of patients. As honey is well known in the Egyptian, as well as all oriental cultures, as a holy remedy; rendering it a perfect environmentally based dressing (in concordance with patients' cultural and religious beliefs) that enhanced healing.
The omnipresence and low price of honey are two important advantages. This was evident in direct cost savings when compared with conventional and modern dressings; 3 kg of honey was as expensive as 1 level of povidone-iodine used only for wound cleansing for <1 month. The other important level of cost reduction was in the rapid healing rates and simplicity of the technique. More cost saving was through the cessation of unnecessary antibiotics use that practitioners prescribe in AO cases, as well as reduction of hospital visits.
CONCLUSIONS
Based on the observation made, statistically analyzed and duly discussed, the following conclusions were drawn from the present study: The age group of 30–40 years was found to most commonly presented with AO. Male was more commonly affected, but the difference was not significant. Dry socket in mandibular molars was more common followed by mandibular premolar, maxillary premolar, and then maxillary molars. CRP levels at the completion of treatment of AO with honey dressing showed a significant decrease from the pretreatment values indicating fast recovery. There was a significant decrease in pain following application of honey dressing in dry socket. Clinical signs such as erythema and swelling showed a significant decrease on regular application of honey dressing. Majority of the patients with exposed bone got healed socket with evidence of granulation tissue and healing gingiva in about 1 week. Microbiological examination showed the presence of normal commensal flora at AO sites such as Streptococcus, Staphylococcus, and Enterococcus. Hence, the role of bacteria in the genesis of AO, if any, appears unclear. Honey is ideal as dressing material in cases of AO, particularly in the developing countries. It is biocompatible, with less cost and clinically effective dressing. More importantly, it is very safe as it did not result in any complication (local or systemic), or emergence of resistant bacterial strains. Honey not only heals the AO sites but also improves the general well-being of the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cardoso CL, Rodrigues MT, Ferreira Júnior O, Garlet GP, de Carvalho PS. Clinical concepts of dry socket. J Oral Maxillofac Surg. 2010;68:1922–32. doi: 10.1016/j.joms.2009.09.085. [DOI] [PubMed] [Google Scholar]
- 2.Vandamme L, Heyneman A, Hoeksema H, Verbelen J, Monstrey S. Honey in modern wound care: A systematic review. Burns. 2013;39:1514–25. doi: 10.1016/j.burns.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 3.Bergman A, Yanai J, Weiss J, Bell D, David MP. Acceleration of wound healing by topical application of Honey. An animal model. AM J Surg. 1983;145:374–6. doi: 10.1016/0002-9610(83)90204-0. [DOI] [PubMed] [Google Scholar]
- 4.Blum IR. Contemporary views on dry socket (alveolar osteitis): A clinical appraisal of standardization, aetiopathogenesis and management: A critical review. Int J Oral Maxillofac Surg. 2002;31:309–17. doi: 10.1054/ijom.2002.0263. [DOI] [PubMed] [Google Scholar]
- 5.Noroozi AR, Philbert RF. Modern concepts in understanding and management of the “dry socket” syndrome: Comprehensive review of the literature. J Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:30–35. doi: 10.1016/j.tripleo.2008.05.043. [DOI] [PubMed] [Google Scholar]
- 6.Alexander RE. Dental extraction wound management: A case against medicating postextraction sockets. J Oral Maxillofac Surg. 2000;58:538–51. doi: 10.1016/s0278-2391(00)90017-x. [DOI] [PubMed] [Google Scholar]
- 7.Kirk DG, Liston PN, Tong DC, Love RM. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. J Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e1–e6. doi: 10.1016/j.tripleo.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 8.Moghazy AM, Shams ME, Adly OA, Abbas AH, El-Badawy MA, Elsakka DM, et al. The clinical and cost effectiveness of bee honey dressing in the treatment of diabetic foot ulcers. J Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;89:276–81. doi: 10.1016/j.diabres.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 9.Bloomer CR. Alveolar osteitis prevention by immediate placement of medicated packing. J Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:282–4. doi: 10.1067/moe.2000.108919. [DOI] [PubMed] [Google Scholar]


