Abstract
The aims of this study were to investigate the ankle position, the changes and persistence of ankle kinematics after neuromuscular training in athletes with chronic ankle instability (CAI). A total of 21 national women’s field hockey players participated (CAI = 12, control = 9). Ankle position at heel strike (HS), midstance (MS), and toe touch (TT) in the frontal plane during walking, running and landing were measured using 3D motion analysis. A 6-week neuromuscular training program was undertaken by the CAI group. Measurements of kinematic data for both groups were measured at baseline and the changes in kinematic data for CAI group were measured at 6 and 24 weeks. The kinematic data at HS during walking and running demonstrated that the magnitude of the eversion in the CAI group (−5.00° and −4.21°) was less than in the control group (−13.45°and −9.62°). The kinematic data at MS also exhibited less ankle eversion in the CAI group (−9.36° and −8.18°) than in the control group (−18.52° and −15.88°). Ankle positions at TT during landing were comparable between groups. Following the 6-week training, the CAI participants demonstrated a less everted ankle at HS during walking and running (−1.77° and −1.76°) compared to the previous positions. They also showed less ankle eversion at MS (−5.14° and −4.19°). Ankle orientation at TT changed significantly to an inverted ankle position (from −0.26° to 4.11°). The ankle kinematics were restored back to the previous positions at 24 weeks except for landing. It appeared that athletes with unstable ankle had a relatively inverted ankle position, and that 6-week neuromuscular training had an immediate effect on changing ankle orientation toward a less everted direction. The changed ankle kinematics seemed to persist during landing but not during walking and running.
Key points.
Athletes with unstable ankles had a relatively inverted ankle position during the initial contact and midstance.
Six-week neuromuscular training for unstable ankles had an immediate effect on changing ankle orientation toward a relatively more inverted direction.
The changed ankle kinematics persisted during jump landing but not during walking and running.
Key words: Ankle position, motion analysis, heel strike, midstance, toe touch
Introduction
Chronic ankle instability (CAI) is a subjectively reported phenomenon that has been defined as a tendency for the ankle to give way during normal or sports activities (Monaghan et al., 2006). A recent epidemiologic study reported that 23.4% of high school and collegiate athletes were identified as having CAI (Tanen et al., 2014). It could therefore be reasonable to infer that many elite-level athletes are participating fully in their various activities with mild to moderate CAI, although the exact prevalence of CAI among them has not been reported. Due to the prevalence of CAI and the disability it creates (Hiller et al., 2004; Ryan, 1994), considerable attention has been directed toward understanding the underlying cause of this phenomenon (Lahde et al., 1988).
Current evidence suggests that the dynamic control of ankle stability depends on feed-forward motor control of the central nervous system (Konradsen et al., 1997). In particular, inappropriate positioning of the ankle joint before ground contact during walking has been suggested to have important implications for ankle joint stability (Tropp, 2002). A recent study has shown that individuals with CAI exhibit altered ankle joint kinematics and kinetics during over ground walking at their self-selected velocities (Monaghan et al., 2006). In this study, the participants with ankle instability were found to have a more inverted position of the ankle joint before and immediately after heel strike (HS) compared with a control group. In another recent study examining the rearfoot/shank coupling at heel strike, individuals with chronic ankle instability also demonstrated a more inverted ankle than healthy controls throughout the entire gait cycle (Drewes et al., 2009). In jogging, this alteration was most apparent just prior to heel strike. This altered positioning may be related to an altered neuromuscular control of CAI, which results in an increased predisposition to suffering recurrent ankle sprain (Drewes et al., 2007).
Thus, identification of altered movement patterns in those with CAI compared to healthy controls may indicate adaptive changes attributable to CAI. Then, with the aim of improving and optimizing impaired movement control, specifically for athletes, rehabilitation training after ankle sprain injuries should focus on the restoration and enhancement of neuromuscular abilities (Zech et al., 2009). This approach may lead to improved therapeutic and prophylactic intervention for athletes with this condition in the future. However, to date, no study has investigated the patterns of ankle joint kinematics and the time-related changes and persistence of neuromuscular training effects in a group of athletes with CAI compared with a healthy control group. Therefore, the primary aim of this study was to identify rearfoot angle kinematics occurring at the early stance phase of the gait cycle during the walking, running, and initial jump landing phases, and to compare these to matched controls. The secondary aim was to examine the time-related changes and persistence of the effects of a 6-week neuromuscular training program, which specifically focused on the element of functional ankle instability, in elite women field hockey players with CAI who underwent the training program while they were participating fully in their training and competition.
Methods
Participants and training program
The present study was designed as a case-control group comparison and prospective observational study of elite women field hockey players who were drafted in as national players and were commencing their training at the national training center of the Korean Olympic Committee (KOC). The committee for ethics in research at our institute approved this study, and all subjects provided written informed consent. All study-related procedures were conducted in accordance with tenets of the Declaration of Helsinki.
Twenty-five women hockey players of the Korea Team were eligible for this study (Figure 1). Each participant completed a self-report questionnaire (Cumberland Ankle Instability Tool; CAIT, a 9-item 30-point scale), which was developed to measure the severity (cut-off score < 24) of functional ankle instability (Hiller et al., 2006). The definition of CAI endorsed by the International Ankle Consortium for enrolling participants was adapted in the present study, which included a history of at least one significant ankle inversion sprain that occurred at least 12 months prior to study enrollment and created at least 1 interrupted day of desired physical activity, followed by repeated sprains with weight bearing or the subjective feeling of the ankle “giving way” or both within a year prior to the study (Gribble et al., 2014). Ultrasound was performed using a 3- to 12-MHz real-time linear-array transducer (HD15; Philips Medical System, Bothell, WA) to exclude a complete rupture of the above two lateral ankle ligaments. An experienced physician, with additional training in musculoskeletal ultrasound, carried out all the examinations.
Figure 1.
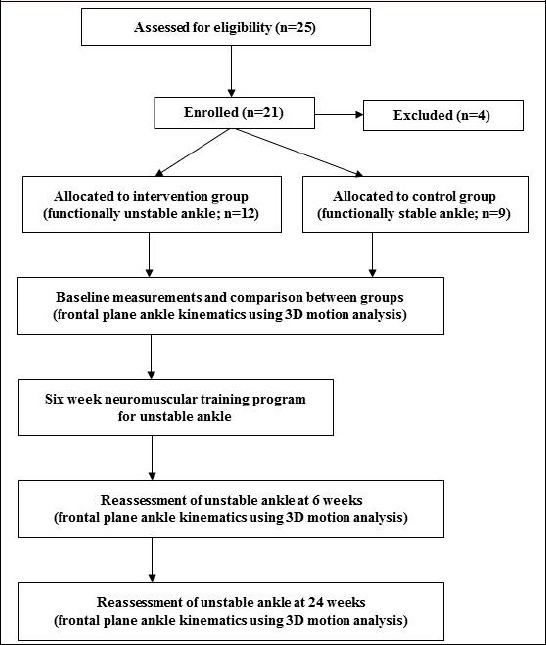
Flow chart of participants and assessments through the study.
Athletes who had reported functional instability of one ankle were included in the CAI group. Participants were excluded from the group if they reported bilateral ankle instability, a subtalar joint problem, medial ankle ligament lesion, syndesmosis injury, spring ligament injury, history of ankle fracture, ankle injury within the 3 months prior to participation, a history of anterior cruciate ligament injury, or participating in an ankle rehabilitation program 6 weeks prior to this study. Additionally, they were also excluded when there was a complete rupture of lateral ankle ligaments on ultrasound examination. Based on the aforementioned criteria, 4 subjects were excluded and the remaining 21 elite women hockey players (mean age 26 years) participated in this study. Thus, 12 women elite hockey players with CAI and 9 women elite hockey players without CAI as controls participated in the study. Among athletes in the CAI group, 10 participants in the CAI group and 3 in the control group exhibited partial tears of the lateral ankle ligaments upon ultrasound examination. Participants in the CAI group completed all follow-up assessments without any dropout, and there were no adverse events reported such as an ankle inversion sprain that necessitate immobilization during the p are presented in Table 1.
Table 1.
Physical characteristics and Cumberland ankle instability tool score of the participants.
| Groups | Site(n) | CAIT score | Age(years) | Height(cm) | Weight(kg) | BMI(kg/m2) | |
|---|---|---|---|---|---|---|---|
| R | L | ||||||
| CAI (n = 12) | 7 | 5 | 17.00 (10.75,20.00) |
26.00 (23.25,28.00) |
163.00 (160.50,164.50) |
59.00 (58.00,63.50) |
22.65 (21.83,23.46) |
| Control (n = 9) | 5 | 4 | 26.50 (24.50,29.50) |
27.00 (25.25,31.00) |
164.00 (161.50,166.75) |
59.00 (58.00,59.75) |
21.88 (20.83,23.17) |
|
Z (p) |
-2.169 (.030) |
-1.243 (.214) |
-.980 (.327) |
-.470 (.638) |
-1.200 (.230) |
||
BMI, body mass index; CAI, chronic ankle instability; CAIT, Cumberland ankle instability tool; L, left; R, right. Site means affected leg side in CAI group and dominant leg in control group.Values are presented as median (quartile 1, quartile 3).
In addition to their daily training regimen for field hockey, athletes with CAI took part in a progressive 6-week (5 sessions per week) rehabilitation exercise program incorporating postural stability, strength, plyometric, and speed/agility drills (Table 2). Each exercise session lasted approximately 60 minutes and included gentle warm-up and cool-down phases. The exercise progression was designed to ensure that participants experienced continuous changes in intensity and demand throughout the course of the program on a weekly basis. Exercise sessions were conducted by two experienced athletic trainers, who emphasized the importance of maintaining the correct technique throughout the program.
Table 2.
6-week neuromuscular training program.
| Range of motion | Achilles tendon stretch, Writing each letter of the alphabet from A to Z, (pain free × 3 repetitions, Increase up to 7 set gradually) |
|||||
|---|---|---|---|---|---|---|
| 1st week | 2nd week | 3rd week | 4th week | 5th week | 6th week | |
| Static postural stability | Single-leg stance on Airex® cushion (3 min) | Single-leg stance on tilt board (3 min) | Single-leg stance on Bosu® ball (3 min) | Single-leg stance while kicking against resistance (10 reps × 3sets) | Single-leg stance and hold in squat up to 90°on BOSU® ball (3 min) | Single-leg stance on BOSU® ball with rebounding ball catch (3 min) |
| Dynamic postural stability | Single-leg lunge forward (10 reps × 3sets) |
Single-leg lunge side to side (10 reps × 3sets) |
Single-leg hopping forward (12 reps × 3sets) |
Single-leg hopping sideways (12 reps × 3sets) |
Single-leg hopping onto BOSU® ball (12 reps × 3sets with 10 sec stabilization) |
Lateral single-leg hopping onto BOSU® ball (12 reps × 3sets with 10 sec stabilization) |
| Strength | Double-leg heel raises (12 reps × 3sets) Double-leg bridge (10 reps × 2sets) Clam-shell gluteus medius (10 reps × 2sets– both sides) Dorsiflexion and eversion exercise (12 reps × 3sets, progression using Thera-band®) |
Single-leg heel raises (12 reps × 3sets) Single-leg bridge (10 reps × 2sets) Figure-4 gluteus medius (10 reps × 2sets– both sides) Dorsiflexion and eversion exercise (12 reps × 3sets, progression using Thera-band®) |
Resisted single-leg heel raises (12 reps × 3sets, 10kg ~ 20kg) Double/single-leg squat (10 reps × 2sets– both sides) Resisted lateral side-steps (10 reps × 2sets– both sides) Dorsiflexion and eversion exercise (12 reps × 3sets, progression using Thera-band®) |
|||
| Plyometrics | Tuck jumps (12 reps × 3sets) |
Broad jumps (12 reps × 3sets) |
180° tuck jumps each direction (5 reps × 3sets in each direction) |
90° hop turns clockwise & counterclockwise (10 reps × 2sets) |
Double-leg lateral jumps over mini-hurdle (12 reps × 3sets) |
Single-leg lateral jumps over mini-hurdle (12 reps × 3sets) |
| Speed/Agility | Figure of 8 runs (10 min, 5reps in each direction) |
Ladder: forward runs (10m,10 reps) |
Ladder: lateral runs (10m, 10 reps in each way) | Ladder: lateral hops (10m, 10 reps in each way ) |
Ladder: hopping slalom drills (10m, 10 reps × 2sets) | Lateral shuttle runs (10m, 10 reps × 2sets) |
Experimental Procedures and Kinematic Data Analysis
Kinematic data acquisition during gait and landing was performed using 12 infrared cameras and a visual 3-dimensional program (C-Motion, standard version 4.91.0; C-Motion Inc., Germantown, MD) was used to quantitatively analyze the collected data. Before collecting the kinematic data, all cameras were arranged and installed to smoothly measure the motion, and the global frame was created on the basis of the calibration frame using Wand calibration methods to set the 3-dimensional coordinate system. The X-axis was oriented in the right-left direction, the Y-axis in anterior-posterior direction, and the Z-axis in the superior-inferior direction. The sampling rate of images was set at 120 Hz. Before testing, fifteen markers were placed on the lower leg and foot in accordance with the protocols of previous studies (Figure 2) (Henley et al., 2008; Seo et al., 2014): knee (2 markers), tibial shank (3 markers), the medial and lateral malleolus (2 markers), the calcaneus (2 markers), navicular (1 marker), cuboid (1 marker), the metatarsal area (3 markers), and the hallux (1 marker). After the attachment of the markers, all participants were instructed to walk barefoot on a 10 m walkway at their comfortable normal walking speed and then to run at 7 km/h on a treadmill. Afterwards, participants were directed to stand on a 25 cm tall box and to jump and land on an indicated spot on the force plate (Pfile et al., 2013). They were instructed to look at a distant mark to inhibit them from looking down at the floor and they practiced each task until they were acclimatized to the laboratory environment before starting the test. Then, 5 test trials were collected for analysis. The initial point of acquisition occurred once the participants were comfortable at the given speed and jump landing. The participants were not made aware of the precise period of data acquisition in order to allow them to assume their normal gait or landing patterns. A trial was terminated if a reflective marker or wand became loose; it was reapplied in the same position in accordance with markings made on the subject’s skin before the test recommenced. All participants took a rest for 10 min between tests to minimize any carry-over effects.
Figure 2.

Position of markers attached to each participant for kinematic analysis.
During the normal walking, running, and landing, each event was calculated through the trajectory of the heel marker. Kinematic data were calculated by comparing the angular orientations of the coordinate systems of the adjacent limb segments. Joint angular displacements were calculated for the ankle joints in the frontal planes (inversion [+], eversion [-]) (Figure 3). When the foot was initially in contact with the floor, the point of HS was identified as the point at which the vertical acceleration of the heel marker crossed the horizontal axis (X-axis) of the graph fora testing gait cycle. The point of midstance (MS) was inferred from the point where the opposite ankle crossed the leg of which the foot is in contact with the floor on the sagittal plane (Mahmoudian et al., 2016). The point of toe touch (TT) was identified using the vertical component of ground reaction force using 15 N as a threshold for detection of impact. Kinematic variables in the frontal planes were averaged over time at each speed (walking, 7 km/h running, and landing) for each participant at HS, MS, and TT. The 4th-order Butterworth low-pass filter with cut-off frequency of 15Hz was used to eliminate the noises from skin movements or labeling errors and the data were processed using C-Motion software. Measurements of kinematic data for both the CAI and the control group at each gait speed and landing were measured at baseline and changes in the kinematic data for the CAI group were measured at 6 weeks and 24 weeks.
Figure 3.
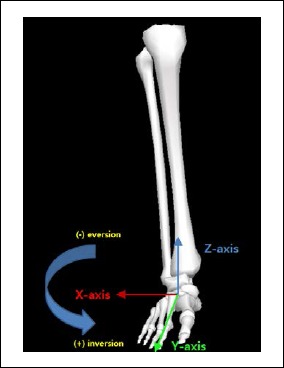
Angular orientation of ankle joint in the frontal plane.
Statistical analyses
All statistical analyses were performed using SPSS software (ver. 21.0, SPSS Inc., Chicago, IL, USA). Due to the small study sample size, non-parametric tests were used to evaluate changes in the outcome measures. The Mann-Whitney test was used to compare the initial rearfoot angle kinematics (inversion or eversion) before the commencement of the 6-week neuromuscular training between groups. The Wilcoxon signed-ranks test was used to evaluate rearfoot angle measurements at each assessment (baseline, 6 week and 24 week) within the CAI group. A value of p < 0.05 was considered to indicate statistical significance. All data are expressed as median and quartiles (1st> and 3rd).
Results
The analyses of the kinematic data at HS in the frontal plane during participants’ comfortable normal walking speed and running (7 km/h) demonstrated that the magnitude of the eversion in the CAI group (-5.00°; -6.59° ~ -4.50° and -4.21°; -6.35° ~ -2.92°) was less than in the control group (-13.45°; -13.46° ~ -13.09° and -9.62°; -13.13° ~ -8.13°). Significant differences in the ankle joint orientations during walking and running between groups were observed (p = 0.002 at each speed). The kinematic data at MS also exhibited less ankle eversion during walking and running in the CAI group (-9.36°; -9.79° ~ -7.62° and -8.18°; -8.46° ~ -6.99°) than in the control group (-18.52°; -18.68° ~ -17.61° and -15.88°; -17.23° ~ -10.89°) (p =0.002; p= 0.005, respectively). Ankle positions at TT during jump landing were comparable between the groups (p = 0.120) (Figure 4).
Figure 4.
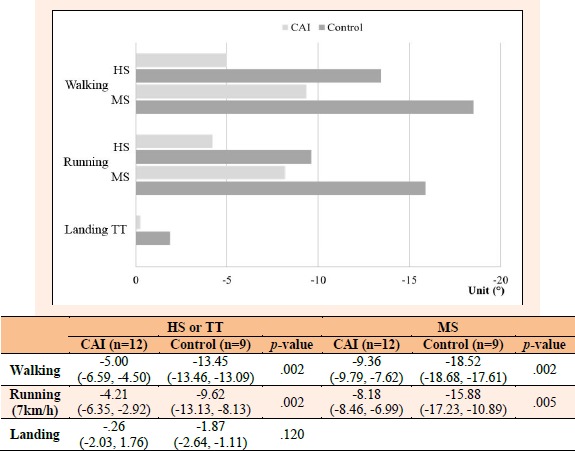
Ankle position in the frontal plane during walking, running and landing between groups. Values are presented as median (quartile 1, quartile 3), CAI; chronic ankle instability, HS; Heel strike, MS; Midstance, TT; Toe touch, +; inversion, -; eversion.
Following the 6-week training, the CAI participants demonstrated a less everted ankle at HS during walking and running (-1.77°; -4.09° ~ 1.14° and -1.76°; -6.13° ~ 2.34°) compared to the previous ankle positions, but the change was not statistically significant (p = 0.050; p = 0.238, respectively). They also showed less ankle eversion at MS during walking and running (-5.14°; -6.12° ~ -0.59° and -4.19°; -6.49° ~ 0.77°) compared to the previous angles, and statistically significant differences were observed (p = 0.041; p = 0.033, respectively). Ankle orientation at TT during jump landing changed significantly compared to the previous angle and therefore demonstrated an inverted ankle position (4.11°; 2.30° ~ 7.25°, p = 0.003). At the 24-week follow-up, reduced ankle eversions were almost restored back to the former levels. Ankle position at HS during walking and running were -4.99° (-7.53° ~ -3.35°) and -6.92° (-9.34° ~ -2.62°), in which significant differences compared to the previous angles were observed (p = 0.012; p = 0.009, respectively). Returned ankle orientation was also demonstrated at MS during walking and running (-8.95°; -10.18° ~ -4.29° and -9.13°; -10.43° ~ -6.00°) (p = 0.012; p = 0.005, respectively). However, inverted ankle orientation at TT during jump landing did not change significantly at 24 weeks compared to the previous angle (3.05°; 1.27° ~ 8.73°, p = 0.346) (Figure 5).
Figure 5.
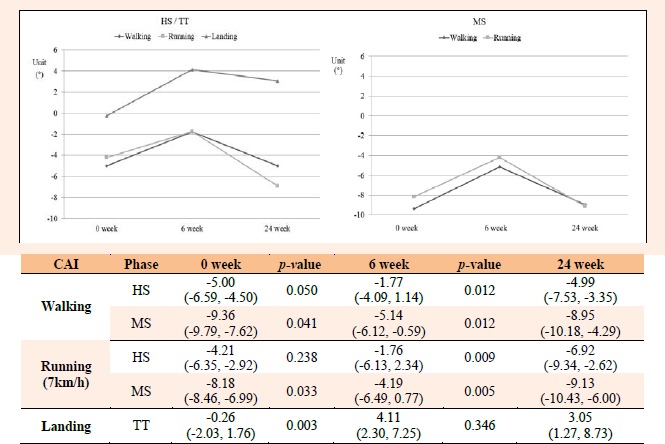
Ankle position at baseline and changes after 6-week neuromuscular training across assessment points. Values are presented as median (quartile 1, quartile 3), CAI; chronic ankle instability, HS; Heel strike, MS; Midstance, TT; Toe touch, +; inversion, -; eversion
Discussion
This study was intended to investigate ankle position in an active athletic population with CAI, to identify the changes in the ankle joint orientation that may be attributable to neuromuscular training effects, and to measure the persistence of these changes. The principle findings from this study were that athletes with unstable ankles had a relatively inverted ankle position compared to athletes with stable ankles in the initial contact and midstance phase of the gait cycle during walking at a self-regulated velocity and running, and that a 6-week regimen of neuromuscular training had an immediate effect on changing the ankle orientation towards a less everted (relatively more inverted) direction than before training during walking and running as well as jump landing. The changed ankle kinematics was restored back to the previous positions at 24 weeks except for jump landing, in which the changed ankle position was sustained to some degree.
We found the ankle positions of the CAI group were less everted by a magnitude of approximately 8° at HS, 9° at MS during walking, approximately 5° at HS, and 8° at MS during running compared to the control group. These findings are consistent with previous studies (Chinn et al., 2013; Delahunt et al., 2006A; Drewes et al., 2009; Monaghan et al., 2006) but the ranges of relatively inverted joint angles in the ankle instability group were different among the studies, in which the magnitude of the angular difference between groups during walking was 2° to 3° (Delahunt et al., 2006A; Drewes et al., 2009) or 6° to 7° (Monaghan et al., 2006) as in our results. These findings are likely to result in increased stress being applied to ankle joint structures during the HS and loading response of the gait cycle. This could result in repeated injury and consequent damage to ankle joint structures.
On the other hand, the CAI group did not show altered ankle positions in the frontal plane at touchdown during jump landing, which is also in agreement with previous studies (Imabayashi et al., 2013; Kipp and Palmieri-Smith, 2012; Monteleone et al., 2014; De Ridder et al., 2015). However, there are several studies that reported an increased inversion angle during jump landing in participants with ankle instability (Delahunt et al., 2006B; Delahunt et al., 2007). We believe that these conflicting findings are mostly due to different landing techniques (vertical, forward or mediolateral) and the periods of the landing phase during which the kinematic data were measured (prior to, at, or after landing). In general, when considering all available evidence on ankle kinematics during landing tasks, it seems difficult to generalize individual study results on ankle joint kinematics in CAI (De Ridder et al., 2015).
After completion of a 6-week neuromuscular training, athletes with unstable ankle demonstrated significant changes in ankle position during not only walking and running but also landing. Ankle orientations were more inverted than before the training, with a magnitude of approximately 3° at HS, 4° at MS during walking, approximately 2° at HS, 4° at MS during running, and approximately 4° at TT during jump landing. These findings are not consistent with a previous study (Coughlan and Caulfield, 2007; McKeon et al., 2009) in which a 4-week neuromuscular training program resulted in no significant changes in ankle position. One possible reason for the lack of significant changes in the previous study was that the participants consisted of a variety of individuals from recreationally active to elite-level athletes contrary to ours, in which the participants consisted of only female elite field hockey players. Additionally, the treatment group in the study included both athletes with healthy ankles and unstable ankles. In the present study, the participants were confined to elite field hockey players, among whom athletes who had reported functional instability were included in the CAI group and were involved in the training program and follow-up assessments. Another possible reason for the lack of changes in the prior study was the duration of the neuromuscular intervention. The previous study had a training period of only 4 weeks, but this duration of training may not have been sufficient to result in neuromuscular adaptation to influence changes in gait patterns. Most rehabilitation studies for acute and chronic ankle instability involved a 6 to 8-week training period (Mattacola and Dwyer, 2002). It seems possible that longer training periods of at least 6 weeks, as in our study, are more effective for achieving physiological adaptations although no study has systematically examined the influence of different training durations on recurrent injury rates after ankle sprains (Isakov and Mizrahi, 1997). In the present study, we believe that reeducation of the ankle muscles and retraining of proprioceptive feedback during dynamic movement results in a less everted ankle position. However, we are still not aware of which factors exactly contribute to the changes of the frontal plane kinematics of unstable ankles after training. Owing to the lack of similar studies investigating the effects of training on ankle joint kinematics and a consequent decrease in recurrent ankle sprain in athletes with CAI, it is difficult to compare our results with those of previous researchers or to determine the influence of the neuromuscular training on recurrent injury rates after ankle sprains.
At the 24-week follow-up, reduced ankle eversion during HS and MS after completion of the neuromuscular training was almost restored back to the former levels. However, with regard to TT during jump landing, ankle orientation stayed inverted consistently. It is important to know if immediate post-training effects are maintained in CAI and if there has been a developing need to examine the efficacy of rehabilitation training in the longer term. We are aware of only a few studies that have looked at recurrence rates of ankle sprain after an exercise program at 1 year of follow-up (Eils and Rosenbaum, 2001). A number of studies that have examined the effect of balance training (Akhbari et al., 2007; Michell et al., 2006; Tourné et al., 2010) reported an improvement in balance performance, but the effects of interventions in these studies were evaluated only after the 4 to 6 week programs with no longer term follow-ups. Furthermore, the exact mechanism behind these improvements could not be identified (Hale et al., 2007). To the best of our knowledge, we are not aware of any study that has performed long-term follow-up to evaluate changes in ankle kinematics after an exercise program. We also do not know whether changes in ankle position after the training in the present study would have any beneficial effect on reducing the risk of recurrent ankle sprain or not. However, we believe that improved dynamic ankle stability in terms of strength, balance, and proprioception after the neuromuscular training possibly contributed to an ankle position change during walking, running, and even jump landing. Our athletes with CAI showed a tendency towards a regression in ankle position during walking and running to a more everted position at the 24 week follow-up. These results may suggest that alterations in ankle orientation with neuromuscular training during walking and running does not tend to last long and therefore, if this change is ever proven to be protective against recurrent ankle sprains or giving way, continuous neuromuscular training might be necessary for athletes with CAI to maintain improved ankle position and therefore to contribute to a reduction in the risk of future ankle sprains.
The inverted ankle after the training seemed to stay in that position during jump landing for a longer period. Joint kinematics should be influential in the capability of modifying and absorbing impact forces during landing tasks and kinematic adaptations might be inefficient in CAI to deal with the rapid and very high loading forces, for example during jump landing, possibly increasing the susceptibility for injury (Zhang et al., 2000). In the present study, jump landing was the most demanding task for participants with CAI in comparison to walking at a comfortable normal speed or running at 7km/h. We speculate that our participants were more focused on the successful jump landing trials in a laboratory setting and the execution of this controlled landing task might have caused the persistence of the changed ankle position.
There have been a few recent investigations that reported the biomechanical differences existing in individuals with CAI during functional activities (Chinn et al., 2013; Coughlan and Caulfield, 2007; Delahunt et al., 2006A; Drewes et al., 2009; Monaghan et al., 2006; De Ridder et al., 2015). The principal findings from these investigations were that the CAI group had an increased inverted position of the ankle joint compared with a healthy control group during the terminal swing and early stance phases of the gait cycle, and the present results also support these findings.
Inappropriate positioning of the ankle joint before HS has been hypothesized as a potential mechanism contributing to the development of recurrent ankle sprain injury (Tropp, 2002). After HS, the line of action of the ground reaction force depends on the position of the foot in relation to the center of gravity and inertia (Tropp, 2002). If the ankle joint is held in a more inverted position when HS occurs, an external inversion load is placed on the ankle joint, thus increasing the potential for a hyper inversion injury. In addition, increased inversion of the ankle at HS places an excessive inversion load on the rear foot, and once weight bearing begins, the time taken to produce an effective recovery via the proprioceptive-neuromuscular complex is almost as long as the stance phase of running, and then it is most unlikely that a protective reflex will be able to respond in time to allow for dynamic stabilization of the ankle joint in this situation, which may also predispose an individual to injury (Tropp, 2002). These findings could explain the reason individuals with CAI experience repeated episodes of “giving way” of their ankle joints in situations with only slight or no external provocation (Delahunt et al., 2006A).
A previous study proposed that the disruption of the sensorimotor system associated with CAI could result in decreased detection of inversion movements or a delay in the motor response of the peroneal muscles (Hiller et al., 2004). Accordingly, the findings from the present study suggest that the ankle is already in an increased inversion position pre-HS and during the loading response. This may be due to decreased detection of the inverted position, thus rendering the ankle more vulnerable to turning on the lateral border (Konradsen et al., 1998). That is, the ankle is more inverted in the CAI subjects during an early stance possibly due to a change in pre-programmed motor control or lack of detection of the position and this is likely to result in repeated injury due to significant increases in stress on ankle joint structures (Monaghan et al., 2006).
Ankle training researches have been directed toward the development of exercise programs aimed at the prevention of recurrent ankle sprains. These researches have focused on proprioceptive (Eils and Rosenbaum, 2001), strengthening (Kaminski and Hartsell, 2002), balance (Osbourne et al., 2001), and coordination exercises (Bernier and Perrin, 1998). Neuromuscular training is used to describe a combination of functionally based exercises, including postural stability, proprioceptive and strength training, as part of a rehabilitation regimen, and exercises to improve neuromuscular control in individuals with CAI are advocated throughout the literature, yet there remains little unequivocal evidence regarding their effectiveness or optimal training methods (Lin et al., 2012). Furthermore, one aspect of ankle training research that has not even received attention is the persistence of the training effects on ankle movement control during functional daily activities such as walking, running, or landing. Thus, the present study focused on evaluating the effect of neuromuscular training on athletes with CAI and also focused on the study design examining the temporal changes of training effects.
The present study addressed functional instability from which athletes could experience one or more of the following: neuromuscular deficits, proprioceptive deficits, strength deficits, or impaired postural control, as these are readily amenable to neuromuscular training. The subjective method of determining functional ankle instability has been questioned in previous studies because it is often deduced from a history of ankle sprain despite evidence that these ankles are not necessarily functionally unstable (Hiller et al., 2006; Kaminski et al., 1999). In order to assess functional instability in this study, a CAIT questionnaire was used, which enables more homogenous groups of subjects for both control and ankle instability to be identified, objectively defined, and compared (Hiller et al., 2006). Athletes with a complete rupture of the lateral ankle ligaments implying severe mechanical instability on ultrasound examination were also excluded from this study. It is generally thought that most elite-level athletes with mild to moderate CAI continue to participate competitively in their sports. Therefore, the participants with CAI in the present study were all elite hockey players who, despite their instability, had continued to participate fully in their sports.
We have chosen a walking pace at their most comfortable and natural walking speed. This speed was chosen as to reduce variability of gait trials as it has been demonstrated that variability increases when healthy individuals walk faster or slower than their free selected pace (Oberg et al., 1993). It is advised to use multiple trials for analysis to represent the individuals gait pattern due to natural gait variability (Macellari et al., 1999), so we chose to use the average of 5 trials for analysis and comparisons between groups in this study. According to previous studies reporting the effects of lateral ankle trauma on balance of the involved and uninvolved limb following acute ankle injury and CAI, there is strong evidence that balance is bilaterally impaired after lateral ankle sprain (Holme et al., 1999; Wikstrom et al., 2010). Based on these studies, the uninvolved limb should not be used as a reference for normal gait or balance, and therefore athletes without CAI served as controls in this study, as opposed to using the uninjured contralateral limb of the participants with CAI.
In the present study, athletes with CAI had a less everted ankle (that is, relatively inverted compared to the healthy ankle) and neuromuscular training resulted in a temporary change of ankle kinematics into a more inverted orientation but not an absolutely inverted position at the early phase of gait cycle during walking and running as well as during the touchdown phase of jump landing, in which the ankle position was getting less everted with increasing gait speed as observed in the previous study (Drewes et al., 2009) and changed to an absolutely inverted angle when jump landing. It can be generally accepted that a more inverted ankle position may jeopardize the stability of the ankle, and the results of this study could be a dilemma to clinicians, therapists or trainers who make therapeutic decisions for individuals with ankle instability and advise prophylactic prevention. We do not know the mechanisms by which neuromuscular training changes ankle kinematics in individuals with CAI, and also do not know whether altered ankle kinematics can be of help to reduce the risk of recurrent ankle sprain, or even make the risk worse. Our findings raise a few issues regarding the implementation of neuromuscular training for rehabilitation of CAI. Therefore, we cannot draw any meaningful conclusions regarding the efficacy for neuromuscular training leading to changes in ankle joint kinematics, and there is certainly a need for more studies to examine the influence of neuromuscular training for athletes with CAI on immediate post-training changes in ankle joint kinematics, and whether or not these changes carry over to a long-term reduction in recurrent injury rates.
Although attempts were made to evaluate and determine the effects and persistence of the neuromuscular training on ankle kinematics in elite athletes with CAI who were fully engaged in their sports, the methods of this study may have several intrinsic limitations hindering the drawing of a relevant conclusion from the results. In the present study, hind foot varus, which is one of the predisposing factors of ankle instability, was not initially considered as exclusion criteria. There is also the possibility of undiagnosed subtalar instability or osteochondral lesions of the talar dome. All of these factors, if they really had existed, might have influenced the effects of the neuromuscular training program. The present study evaluated only ankle joint angles at defined events during dynamic tasks instead of considering the whole kinematic curve and did not evaluate the kinematics of proximal joints in which there should be interplay between proximal and distal segments during functional activities based on kinetic chain theories (Chuter and Janse de Jonge, 2012; Verrelst et al., 2014). These factors might result in a focus bias and obscure possibly relevant information. In addition, this study included only elite women’s field hockey players engaged in the sport at the national training center of the KOC, and therefore the study results should be interpreted cautiously, given that they describe a select group of female athletes of similar age, level of symptoms, and sporting ability. The present study was a case-control and prospective observational study design with a relatively small number of participants. Although several significant results were reported, these data need further verification by including athletes with CAI in addition to the controls who are measured at the same time (at 6 weeks and 24 weeks) but not subjected to neuromuscular training in a well-controlled study with a larger sample size. Furthermore, the present study did not include a follow-up assessment of athletes to determine whether the changes noted in ankle kinematics produced any meaningful functional consequence in terms of a reduction in the incidence of episodes of ankle sprain or sensations of the ankle “giving way”. Future studies conducting investigations with a similar design on larger various groups of CAI should, therefore, also include the implementation of functional outcomes with adequate sensitivity to detect the neuromuscular training effects.
Conclusion
The aims of this study were to investigate the ankle position and the changes and persistence of ankle kinematics after neuromuscular training in athletes with unstable ankle. They had a relatively inverted ankle position in the initial contact and midstance phase of the gait cycle during walking and running, and the 6-week neuromuscular training had an immediate effect on changing ankle orientation toward a less everted direction than before training during walking and running as well as jump landing. The changed ankle kinematics seemed to persist during jump landing but not during walking and running. Further research into the effects of neuromuscular training on preventing recurrent ankle sprains and the use of prophylactic ankle taping in addition to the training to improve joint proprioception or dynamic stability and the comparison of the effects between the taping and neuromuscular training could be very interesting with detailed investigation of ankle kinematics in athletes with unstable ankle.
Acknowledgment
This work was done with the sports promotion fund from Korea Institute of Sport Science, Korea Sports Promotion Foundation (KISS - 14 – A01001)
Biographies

Eunkuk KIM
Employment
Associate professor, Department of Physical Education, Korea National Sport University, Seoul, Republic of Korea
Degree
MD, PhD
Research interests
Rehabilitation of overuse sports injuries, diagnostic ultrasound on sports injuries.
eunkuk.kim@gmail.com

Hokyung CHOI
Employment
Ph.D. Doctoral course, Department of Physical Education Korea National Sport University
Degree
MSc
Research interests
Rehabilitation of overuse sports injuries
ghruddl82@gmail.com

Jung-Hoon CHA
Employment
Associate professor, Department of Community Sports, Korea National Sport University, Seoul, Republic of Korea
Degree
PhD
Research interests
Measurement and evaluation in physical education
jhcha8055@knsu.ac.kr

Jong-Chul PARK
Employment
Researcher, Department of Sport Science, Korea Institute of Sport Science, Seoul, Korea
Degree
PhD
Research interests
Kinetic and Kinematic analysis in sports
mori@sports.re.kr

Taegyu KIM
Employment
Physical therapist, Department of Sports Medicine and Science, Taereung National Training Center of the Korean Olympic Committee, Seoul, Republic of Korea
Degree
PhD
Research interests
Exercise and rehabilitation of sports injuries, evaluation of sports performance
ktk7718@gmail.com
References
- Akhbari B., Takamjani I.E., Salavati M., Sanjarib M.A. (2007) A 4-week Biodex stability exercise program improved ankle musculature onset, peak latency and balance measures in functionally unstable ankles. Physical Therapy in Sport 8(3), 117-129. [Google Scholar]
- Bernier J.N., Perrin D.H. (1998) Effect of coordination training on proprioception of the functionally unstable ankle. Journal of Orthopaedic & Sports Physical Therapy 27(4), 264-275. [DOI] [PubMed] [Google Scholar]
- Chinn L., Dicharry J., Hertel J. (2013) Ankle kinematics of individuals with chronic ankle instability while walking and jogging on a treadmill in shoes. Physical Therapy in Sport 14(4), 232-239. [DOI] [PubMed] [Google Scholar]
- Chuter V.H., Janse de Jonge X.A. (2012) Proximal and distal contributions to lower extremity injury: a review of the literature. Gait & Posture 36(1), 7-15. [DOI] [PubMed] [Google Scholar]
- Coughlan G., Caulfield B. (2007) A 4-week neuromuscular training program and gait patterns at the ankle joint. Journal of Athletic Training 42(1), 51-59. [PMC free article] [PubMed] [Google Scholar]
- Delahunt E., Monaghan K., Caulfield B. (2006A) Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. The American Journal of Sports Medicine 34(12), 1970-1976. [DOI] [PubMed] [Google Scholar]
- Delahunt E., Monaghan K., Caulfield B. (2006B) Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. Journal of Orthopaedic Research 24(10), 1991-2000. [DOI] [PubMed] [Google Scholar]
- Delahunt E., Monaghan K., Caulfield B. (2007) Ankle function during hopping in subjects with functional instability of the ankle joint. Scandinavian Journal of Medicine & Science in Sports 17(6), 641-648. [DOI] [PubMed] [Google Scholar]
- Drewes L.K., McKeon P.O., Paolini G., Riley P., Kerrigan D.C., Ingersoll C.D., Hertel J. (2007) Altered shank-rearfoot coupling during walking and jogging in those with chronic ankle instability. Medicine & Science in Sports & Exercise 39(5), S6. [Google Scholar]
- Drewes L.K., McKeon P.O., Paolini G., Riley P., Kerrigan D.C., Ingersoll C.D., Hertel J. (2009) Altered ankle kinematics and shank-rear-foot coupling in those with chronic ankle instability. Journal of Sport Rehabilitation 18(3), 375-388. [DOI] [PubMed] [Google Scholar]
- Eils E., Rosenbaum D. (2001) A multi-station proprioceptive exercise program in patients with ankle instability. Medicine & Science in Sports & Exercise 33(12), 1991-1998. [DOI] [PubMed] [Google Scholar]
- Gribble P.A., Delahunt E., Bleakley C.M., Caulfield B., Docherty C.L., Fong D.T., Fourchet F., Hertel J., Hiller C.E., Kaminski T.W., McKeon P.O., Refshauge K.M., van der Wees P., Vicenzino W., Wikstrom E.A. (2014) Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. Journal of Athletic Training 49(1), 121-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale S.A., Hertel J., Olmsted-Kramer L.C. (2007) The effect of a 4-week comprehensive rehabilitation Program on postural control and lower extremity function in Individuals with chronic ankle instability. Journal of Orthopaedic & Sports Physical Therapy 37(6), 303-311. [DOI] [PubMed] [Google Scholar]
- Henley J.R.J., Hudson D., Church C., Coleman S., Kerstetter L., Miller F. (2008) Reliability of a clinically practical multisegment foot marker set/model. Foot and ankle motion analysis: clinical treatment and technology SP. Eds: Harris GF, Marks RM. Boca Raton: CRC Press; 445-463. [Google Scholar]
- Hiller C.E., Refshauge K.M., Beard D.J. (2004) Sensorimotor control is impaired in dancers with functional ankle instability. The American Journal of Sports Medicine 32(1), 216-223. [DOI] [PubMed] [Google Scholar]
- Hiller C.E., Refshauge K.M., Bundy A.C., Herbert R.D., Kilbreath S.L. (2006) The cumberland ankle instability tool: a report of validity and reliability testing. Archives of Physical Medicine and Rehabilitation 87(9), 1235-1241. [DOI] [PubMed] [Google Scholar]
- Holme E., Magnusson S.P., Becher K., Bieler T., Aagaard P., Kjaer M. (1999) The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scandinavian Journal of Medicine & Science in Sports 9(2), 104-109. [DOI] [PubMed] [Google Scholar]
- Imabayashi E., Matsuda H., Tabira T., Arima K., Araki N., Ishii K., Yamashita F., Iwatsubo T. (2013) Comparison between brain CT and MRI for voxel-based morphometry of Alzheimer’s disease. Brain and Behavior 3(4), 487-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isakov E., Mizrahi J. (1997) Is balance impaired by recurrent sprained ankle? British Journal of Sports Medicine 31, 65-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminski T.W., Hartsell H.D. (2002) Factors contributing to chronic ankle instability: a strength perspective. Journal of Athletic Training 37(4), 394-405. [PMC free article] [PubMed] [Google Scholar]
- Kaminski T.W., Perrin D.H., Gansneder B.M. (1999) Eversion strength analysis of uninjured and functionally unstable ankles. Journal of Athletic Training 34(3), 239-245. [PMC free article] [PubMed] [Google Scholar]
- Kipp K., Palmieri-Smith R.M. (2012) Principal component based analysis of biomechanical inter-trial variability in individuals with chronic ankle instability. Clinical Biomechanics 27(7), 706-710. [DOI] [PubMed] [Google Scholar]
- Konradsen L., Olesen S., Hansen H.M. (1998) Ankle sensorimotor control and eversion strength after acute ankle inversion injuries. The American Journal of Sports Medicine 26(1), 72-77. [DOI] [PubMed] [Google Scholar]
- Konradsen L., Voigt M., Hojsgaard C. (1997) Ankle inversion injuries: the role of the dynamic defense mechanism. The American Journal of Sports Medicine 25(1), 54-58. [DOI] [PubMed] [Google Scholar]
- Lahde S., Putkonen M., Puranen J., Raatikainen T. (1998) Examination of the sprained ankle: anterior drawer test or arthrography? European Journal of Radiology 8(4), 255-257. [PubMed] [Google Scholar]
- Lin C.W., Delahunt E., King E. (2012) Neuromuscular training for chronic ankle instability. Physical Therapy 92(8), 987-991. [DOI] [PubMed] [Google Scholar]
- Macellari V., Giacomozzi C., Saggini R. (1999) Spatial–temporal parameters of gait: reference data and a statistical method for normality assessment. Gait & Posture 10(2), 171-181. [DOI] [PubMed] [Google Scholar]
- Mahmoudian A., Bruijn S.M., Yakhdani H.R., Meijer O.G., Verschueren S.M., van Dieen J.H. (2016) Phase-dependent changes in local dynamic stability during walking in elderly with and without knee osteoarthritis. Journal of Biomechanics 49(1), 80-86. [DOI] [PubMed] [Google Scholar]
- Mattacola C.G., Dwyer M.K. (2002) Rehabilitation of the ankle after acute sprain or chronic instability. Journal of Athletic Training 37, 413-429. [PMC free article] [PubMed] [Google Scholar]
- McKeon P.O., Paolini G., Ingersoll C.D., Kerrigan D.C., Saliba E.N., Bennett B.C., Hertel J. (2009) Effects of balance training on gait parameters in patients with chronic ankle instability: a randomized controlled trial. Clinical Rehabilitation 23(7), 609-621. [DOI] [PubMed] [Google Scholar]
- Michell T.B., Ross S.E., Blackburn J.T., Hirth C.J., Guskiewicz K.M. (2006) Functional balance training, with or without exercise sandals, for subjects with stable or unstable ankles. Journal of Athletic Training 41(4), 393-398. [PMC free article] [PubMed] [Google Scholar]
- Monaghan K., Delahunt E., Caulfield B. (2006) Ankle function during gait in patients with chronic ankle instability compared to controls. Clinical Biomechanics 21(2), 168-174. [DOI] [PubMed] [Google Scholar]
- Monteleone B.J., Ronsky J.L., Meeuwisse W.H., Zernicke R.F. (2014) Ankle kinematics and muscle activity in functional ankle instability. Clinical Journal of Sport Medicine 24(1), 62-68. [DOI] [PubMed] [Google Scholar]
- Oberg T., Karsnia A., Oberg K. (1993) Basic gait parameters: reference data for normal subjects, 10–79 years of age. Journal of Rehabilitation Research & Development 30(2), 210-223. [PubMed] [Google Scholar]
- Osbourne M.D., Chou L.S., Laskowski E.R., Smith J., Kaufman K.R. (2001) The effect of ankle disk training on muscle reaction time in subjects with a history of ankle sprain. The American Journal of Sports Medicine 29(5), 627-632. [DOI] [PubMed] [Google Scholar]
- Pfile K.R., Hart J.M., Herman D.C., Hertel J., Kerrigan C., Ingersoll C.D. (2013) Different exercise training interventions and drop landing biomechanics in high school female athletes. Journal of athletic training 48(4), 450-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Ridder R., Willems T., Vanrenterghem J., Robinson M.A., Roosen P. (2015) Lower limb landing biomechanics in subjects with chronic ankle instability. Medicine & Science in Sports & Exercise 47(6), 1225-1231. [DOI] [PubMed] [Google Scholar]
- Ryan L. (1994) Mechanical stability, muscle strength and proprioception in the functionally unstable ankle. Australian Journal of Physiotherapy 40, 41-47. [DOI] [PubMed] [Google Scholar]
- Seo S.G., Lee D.Y., Moon H.J., Kim S.J., Kim J., Lee K.M., Chung C.Y., Choi I.H. (2014) Repeatability of a multi-segment foot model with a 15-marker set in healthy adults. Journal of Foot and Ankle Research 22(7), 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanen L., Docherty C.L., Van Der Pol B., Simon J., Schrader J. (2014) Prevalence of chronic ankle instability in high school and division I athletes. Foot & Ankle Specialist 7(1), 37-44. [DOI] [PubMed] [Google Scholar]
- Tourné Y., Besse J.L., Mabit C. (2010) Chronic ankle instability. Which tests to assess the lesions? Which therapeutic options? Orthopaedics & Traumatology: Surgery & Research 96(4), 433-446. [DOI] [PubMed] [Google Scholar]
- Tropp H. (2002) Commentary: functional ankle instability revisited Journal of athletic training 37(4), 512-515. [PMC free article] [PubMed] [Google Scholar]
- Verrelst R., De Clercq D., Vanrenterghem J., Willems T., Palmans T., Witvrouw E. (2014) The role of proximal dynamic joint stability in the development of exertional medial tibial pain: a prospective study. British Journal of Sports Medicine 48(5), 388-393. [DOI] [PubMed] [Google Scholar]
- Wikstrom E.A., Naik S., Lodha N., Cauraugh J.H. (2010) Bilateral balance impairments after lateral ankle trauma: a systematic review and meta-analysis. Gait & Posture 31(4), 407-414. [DOI] [PubMed] [Google Scholar]
- Zech A., Hubscher M., Vogt L., Banzer W., Hansel F., Pfeifer K. (2009) Neuromuscular training for rehabilitation of sports injuries: a systematic review. Medicine & Science in Sports & Exercise 41(10), 1831-1841. [DOI] [PubMed] [Google Scholar]
- Zhang S.N., Bates B.T., Dufek J.S. (2000) Contributions of lower extremity joints to energy dissipation during landings. Medicine & Science in Sports & Exercise 32(4), 812-819. [DOI] [PubMed] [Google Scholar]


