ABSTRACT
Technologies to differentiate human pluripotent stem cells into three-dimensional organized structures that resemble in vivo organs are pushing the frontiers of human disease modeling and drug development. In response to the global health emergency posed by the Zika virus (ZIKV) outbreak, brain organoids engineered to mimic the developing human fetal brain have been employed to model ZIKV-induced microcephaly. Here, we discuss the advantages of brain organoids over other model systems to study development and highlight recent advances in understanding ZIKV pathophysiology and its underlying pathogenesis mechanisms. We further discuss perspectives on overcoming limitations of current organoid systems for their future use in ZIKV research.
KEY WORDS: Zika, Cortex, iPSC, Microcephaly, Organoids
Summary: This Spotlight article summarises the latest advances in using cerebral organoids to model Zika virus infection and the resulting pathology.
Introduction
The rapidly advancing field of stem cell biology continually provides new insights into basic biology and human disorders, as well as innovative approaches to develop new patient treatment strategies. In the past 10 years, human pluripotent stem cells (hPSCs) have emerged as an invaluable tool in modeling human disorders, especially those with complex genetic origins that are challenging to model in animals (Takahashi et al., 2007; Wen et al., 2016). Significant progress has been made in the targeted differentiation of hPSCs into various cell types with high purity in order to study human cell biology and develop cell replacement therapies. A new frontier of stem cell research is the generation of three-dimensional (3D) tissue structures to model organogenesis and developmental disorders. Human brain organoids are stem cell-derived 3D tissues that self-assemble into organized structures that resemble the developing human brain (Jo et al., 2016; Kadoshima et al., 2013; Lancaster et al., 2013; Mariani et al., 2015; Paşca et al., 2015; Qian et al., 2016). The ability to engineer brain organoids from genetically tractable patient stem cells holds tremendous potential to transform our understanding of human neural development, which is otherwise inaccessible to manipulation and detailed analyses. In this Spotlight article, we highlight the use of brain organoids to study Zika virus (ZIKV) infection, identify advantages and limitations of brain organoids as a model system, and discuss perspectives for future studies.
The ZIKV pandemic
ZIKV, a mosquito-borne flavivirus, has reportedly spread in over 70 countries and territories globally (Box 1) (CDC, 2016; Heukelbach et al., 2016). While ZIKV infection in adults usually results in mild symptoms, much attention has been drawn towards the co-occurrence of ZIKV outbreaks and an increased incidence of newborns with microcephaly, a condition in which infants are born with an abnormally small head. Since the declaration of ZIKV as a global health emergency by the World Health Organization (WHO), clinical examinations of microcephalic fetal tissues have shown the presence of ZIKV in damaged fetal brains (Heymann et al., 2016; Mlakar et al., 2016; Ventura et al., 2016). More recently, the United States Centers for Disease Control and Prevention (CDC) evaluated existing evidence and concluded that ZIKV causes microcephaly and other severe fetal brain defects (CDC, 2016). Live infected human fetal tissues are not accessible and postmortem tissues are variable in their quality and genetic backgrounds, and clinical studies alone cannot provide sufficient insights for understanding how ZIKV causes this damage. Therefore, researchers have adopted brain organoid models to study the cellular tropism and pathogenesis mechanisms of ZIKV in controlled settings (Ming et al., 2016).
Box 1. Timeline of major events in ZIKV history.
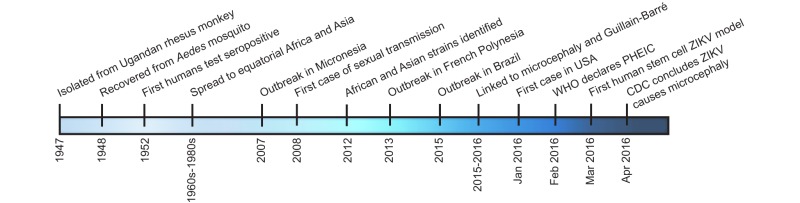
ZIKV was first isolated in April 1947 in the blood of a rhesus monkey found in Uganda's Ziika (or Zika) Forest (Dick et al., 1952). The virus was later recovered from the Aedes africanus mosquito in 1948 and the first human in 1952, establishing a vector for transmission (Dick et al., 1952). Between the 1960s and 1980s, only sporadic cases of benign illness were reported in Africa (Simpson, 1964). The virus continued to spread across the globe to equatorial Africa and Asia during the period from 1969 to 1983, the Pacific Islands from 2013 to 2014, and then the outbreak in the Americas from 2015 to 2016 with hundreds of thousands of confirmed and suspected cases of ZIKV infection (Fauci and Morens, 2016). While infected individuals can often be asymptomatic or have only mild symptoms, of mounting concern are reports linking ZIKV infection to fetal and newborn microcephaly and serious neurologic complications, such as Guillain-Barré syndrome (Petersen et al., 2016). The WHO declared a public health emergency of international concern (PHEIC) on February 1st, 2016, in part due to the uncertainty surrounding increased reports of microcephaly and other disorders coinciding with clusters of ZIKV outbreaks (Heymann et al., 2016). Soon after, the first human stem cell-based model of ZIKV infection was reported (Tang et al., 2016), which provided evidence of a plausible link between ZIKV and microcephaly. This and clinical evidence of the presence of ZIKV in the amniotic fluid of fetuses diagnosed with microcephaly and microcephalic brain tissue (Calvet et al., 2016; Mlakar et al., 2016) led the CDC to declare that ZIKV causes microcephaly on April 13th, 2016 (CDC, 2016).
Why use brain organoids?
Brain organoids include at least two categories, namely cerebral organoids and brain region-specific organoids (Kelava and Lancaster, 2016). The cerebral organoid system utilizes the intrinsic signaling of hPSCs to allow spontaneous differentiation into neural tissues that resemble features of different brain regions (Lancaster et al., 2013). The cerebral organoid offers an opportunity to model whole brain development and interactions among different brain regions. Brain region-specific organoids, by contrast, use patterning factors to induce the differentiation of hPSCs into specific lineages, such as cerebral cortex (Kadoshima et al., 2013; Mariani et al., 2015; Paşca et al., 2015; Qian et al., 2016), midbrain (Jo et al., 2016; Qian et al., 2016) and hypothalamus (Merkle et al., 2015; Qian et al., 2016; Sakaguchi et al., 2015; Wang et al., 2015). Compared with cerebral organoids, brain region-specific organoids model individual brain regions of interest and generally result in more uniform and reproducible tissue, providing a platform for quantitative characterization.
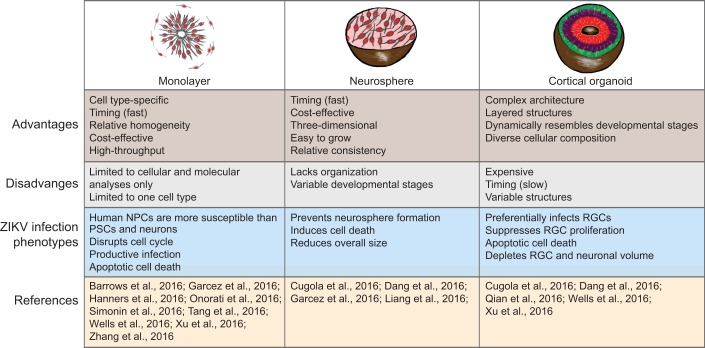
Despite the different methodologies, a common characteristic that distinguishes brain organoids from other in vitro models, such as monolayer and neurosphere cultures, is that, in addition to producing the relevant cell types, brain organoids are capable of recapitulating much of the architecture of the fetal brain (Fig. 1). For example, cortical organoids contain well-organized neural progenitor cell (NPC) layers and neuronal layers, resembling the laminated structure found in the cerebral cortex (Kadoshima et al., 2013; Paşca et al., 2015). This provides a unique opportunity for direct investigation of structural phenotypes, such as the relationship between ZIKV infection and cortical layer thickness. Embryonic primate and human brains exhibit a well-defined outer subventricular zone (oSVZ) layer containing outer radial glial cells (oRGCs), the major progenitors believed to be responsible for primate and human cortical expansion (Lui et al., 2011; Nowakowski et al., 2016b). One forebrain organoid model recapitulates the progenitor zone organization with an oSVZ layer formed by specialized NPCs displaying the distinct molecular signature of human oRGCs (Qian et al., 2016). oRGCs are few in number and do not form a discrete layer in rodents, highlighting the potential of brain organoids to recapitulate human-specific developmental features that cannot be studied in animal models. Forebrain organoids also exhibit functional cortical neuron subtypes found in all six cortical layers, as well as diverse interneuron subtypes (Qian et al., 2016). In addition, astrocytes are present in brain organoids (Paşca et al., 2015; Qian et al., 2016).
Fig. 1.
Comparison of brain cortical organoids with other human stem cell-based models, and summary of key ZIKV-related findings obtained from each system.
Compared with monolayer and neurosphere cultures, which usually contain relatively pure populations of one or a few cell types, brain organoids better recapitulate the composition, diversity and organization of cell types found in the developing human brain (Fig. 1). By exposing the whole organoid to ZIKV, it is possible to analyze and compare the efficiency with which ZIKV infects different cell types, layers and regions within the same organoids, as well as to investigate potential non-cell-autonomous effects. In addition, compared with 2D differentiation protocols, brain organoids of different stages can more accurately mimic the developing trajectory of fetal brain within the first and second trimesters of pregnancy. Because these spatiotemporal transitions take place as a continuous process, researchers can examine brain organoids at any time point of interest to gain insight into both short- and long-term effects of viral infection over the course of fetal brain development. Therefore, in the context of a global health emergency, such as the ZIKV outbreak, brain organoid systems can provide direct insight into human neural development and expedite therapeutic progress.
Using brain organoids to study ZIKV-induced microcephaly
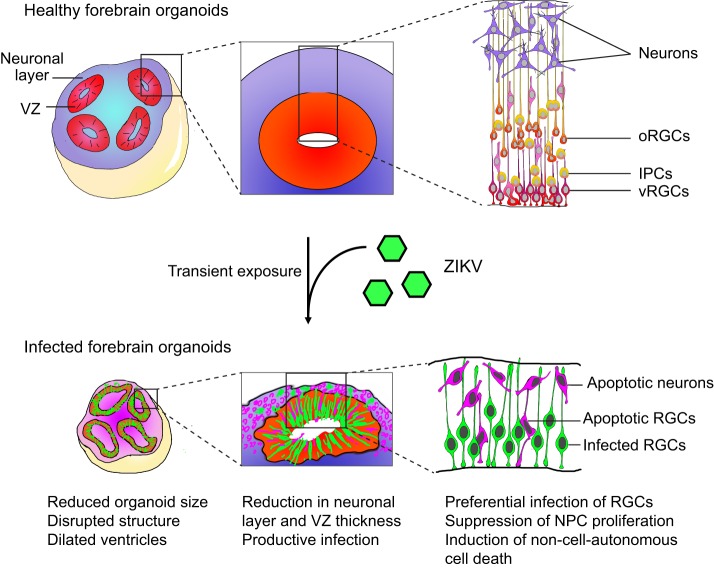
The first study to model ZIKV infection during human brain development used monolayer cultures of forebrain-specific NPCs, which provided the initial hint that ZIKV more efficiently infects NPCs over hPSCs or immature neurons (Tang et al., 2016). A number of studies have since modeled ZIKV infection using human NPC monolayer and neurosphere cultures, acute fetal brain slices, and brain organoids (Barrows et al., 2016; Cugola et al., 2016; Dang et al., 2016; Garcez et al., 2016; Hanners et al., 2016; Liang et al., 2016; Onorati et al., 2016; Qian et al., 2016; Retallack et al., 2016; Simonin et al., 2016; Wells et al., 2016) (Fig. 1). An in-depth analysis of forebrain organoids transiently exposed to ZIKV at different developmental stages showed that ZIKV exhibits tropism towards NPCs, including ventricular RGCs and oRGCs, over intermediate neural progenitors or immature neurons (Fig. 2) (Qian et al., 2016). This finding was later confirmed in studies of fetal human brain slices in vitro (Onorati et al., 2016; Retallack et al., 2016) and embryonic mouse brains in vivo (Li et al., 2016; Nguyen et al., 2016). Infected NPCs become viral factories to produce more infectious viral particles, leading to an increasing number of infected cells over time (Qian et al., 2016). In addition to the reduced overall size of forebrain organoids, quantitative analysis revealed that ZIKV infection caused depletion of NPCs by at least two means: suppression of NPC proliferation and increased cell death of both infected NPCs and uninfected neurons. This resulted in a decrease in volume of both NPC and neuronal layers, resembling microcephaly (Fig. 2). Notably, ZIKV infection-induced NPC death was much more dramatic in forebrain organoids than in monolayer cultures (Qian et al., 2016; Tang et al., 2016).
Fig. 2.
Phenotypes of ZIKV-infected forebrain organoids. Schematics of healthy and ZIKV-infected forebrain organoids illustrate the virus-induced phenotypes observed at different levels. ZIKV-infected cells are in green; apoptotic cells are in purple. NPC, neural progenitor cell; VZ, ventricular zone; oRGC, outer radial glial cell; vRGC, ventricular radial glial cell; IPC, intermediate progenitor cell.
Infection of human neurospheres and cerebral organoids with ZIKV and dengue virus 2 (DENV2) showed that ZIKV, but not DENV2, attenuates NPC growth, suggesting that the detrimental consequence of ZIKV infection is not a general feature of the flavivirus family (Garcez et al., 2016). Indeed, a recent transcriptome analysis of infected monolayer NPCs showed that ZIKV has a more selective and substantial impact on the expression of genes involved in DNA replication and repair, in contrast to the robust global transcriptome changes induced by DENV (Zhang et al., 2016). Transcriptome analysis of ZIKV infection in human cerebral organoids and mouse neurospheres also identified upregulation of toll-like receptor 3 (TLR3), an innate immune receptor (Dang et al., 2016). Analysis of gene expression changes highlighted TLR3-mediated downregulation of neurogenesis and upregulation of pro-apoptotic pathways. Functionally, a TLR3 inhibitor partially rescued the reduced size of ZIKV-infected neurospheres and organoids, and it will be interesting to further determine whether cell viability and organoid structures are also rescued.
Initial studies in the field used the only available strain at the time, the original African strain of ZIKV (ZIKVM), which shares 87-90% RNA sequence identity with the Asian strain (ZIKVC) and recent clinical isolates from Brazil (ZIKVB) and Puerto Rico (ZIKVP) (Faria et al., 2016). One study combined mouse models and cerebral organoids to compare the effect of infection by different ZIKV strains. Compared with ZIKVM, ZIKVB appeared to exhibit stronger deleterious effects in cerebral organoids and in embryonic mice, including more severe effects on NPC depletion and neuronal layer disruption (Cugola et al., 2016). Transcriptome analysis of monolayer NPCs infected with different ZIKV strains showed similar overall expression profiles, yet ZIKVC, but not ZIKVM, induced upregulation of viral response genes and TP53 (Zhang et al., 2016). Functionally, TP53 inhibitors can block the apoptosis induced by both ZIKVC and ZIKVM in human NPCs, with higher potency against ZIKVC-induced apoptosis. It should be noted that any strain-specific phenotypes in experimental models need to be considered in the context of the passage histories of the strains. For example, ZIKVC has been passaged extensively in suckling mouse brain and then in vitro, whereas ZIKVB and ZIKVP have only been passaged a limited number of times in the laboratory.
Limitations of current brain organoid systems for ZIKV research
Within a short period of time, brain organoids have been applied in multiple laboratories to investigate ZIKV infection (Ming et al., 2016). Consistent results from these studies have consolidated the causal link between fetal ZIKV infection and birth defects. Despite these advances, it is important to acknowledge challenges when applying current organoid technologies to ZIKV research. The first challenge is the limited accessibility of organoid technologies. Methodologies for generating monolayer NPCs and neurospheres are well-established and commercially available, but culturing organoids requires specialized expertise and it would take extensive training and resources for a laboratory specializing in virology to adopt organoid technology. Although commercialization of organoid technology is unlikely to fulfill the urgent need for addressing the current ZIKV emergency, researchers world-wide have overcome this challenge by establishing extensive collaborations outside of their own discipline, as the majority of studies published so far on ZIKV organoid modeling are collaborative efforts involving multiple laboratories that would not normally overlap in their topics of research.
The second challenge is the heterogeneity that accompanies the structural complexity and cell type diversity offered by brain organoids over simpler models, such as neurospheres (Kelava and Lancaster, 2016). In cerebral organoids, spontaneous differentiation of PSCs determines composition and properties, leading to considerable sample-to-sample, batch-to-batch and cell line-dependent variations. These variations present obstacles for quantitative analysis and reproducibility of results. Moreover, owing to the long-term nature of organoid culturing, small perturbations in culture conditions could potentially change the outcome significantly. While efforts have been made to generate brain region-specific organoids under defined conditions, it is important to establish common standards of organoid quality by carefully characterizing multiple aspects, including lineage specificity, proportion of different cell types and, in the case of cortical organoids, the relative size of each layer.
A third challenge in applying organoid technology to ZIKV research is the low-throughput nature of culturing and analyzing organoids. This represents a major obstacle to conducting drug screening and other high-throughput applications. Although technologies such as miniaturized bioreactors offer promise for scaling up organoid cultures with reduced cost and increased throughput (Qian et al., 2016), current methods for structural and cellular characterization have relied on labor-intensive procedures, including cryosectioning, immunostaining and image collection. For large-scale screening involving hundreds of conditions, new methods are needed to process these organoids in batches and to automate readouts to obtain quantitative data.
A final and perhaps most difficult challenge in brain organoid research is their simplistic nature compared with the actual developing human fetal brain. All current reported studies evaluate direct exposure of ZIKV to brain organoids in the absence of immune and vascular systems, which might skew the actual effects of ZIKV infection in humans. In the future, new and more sophisticated models, which might involve the addition of endothelial cells or microglial cells to organoids, or that add blood-derived components to the medium, might provide more physiologically relevant features for modeling ZIKV infection during fetal human brain development.
Using brain organoids for ZIKV research: the next phase
Most published studies have so far focused on characterizing the pathological impact of ZIKV infection. Brain organoids can be easily manipulated, both genetically and chemically, offering a valuable platform for the next phase of ZIKV-related research. There are at least two major directions: (1) to delve into the underlying molecular and cellular mechanisms responsible for ZIKV-induced damage; and (2) to use organoids as a screening and validation tool for therapeutic development.
Genetic manipulation of brain organoids can be achieved via stable genome editing of hPSCs, or transiently via electroporation or retrovirus/lentivirus/adeno-associated virus infection of organoids directly. Therefore, it is possible to examine how an individual or combination of ZIKV-encoded proteins, or ZIKV-derived noncoding RNAs, affects brain organoid development (Liang et al., 2016). Insights into downstream molecular events will enhance our understanding of how ZIKV interacts with the host machinery to suppress NPC proliferation and induce cell death, as well as help to identify genes and pathways necessary for ZIKV replication (Ming et al., 2016). These studies will not only provide potential therapeutic targets against ZIKV, but might also enhance our general knowledge of human brain development.
Although current brain organoid systems have yet to meet the demand for full-scale screening of hundreds to thousands of conditions, they provide a relevant platform for testing specific hypotheses and for validation of therapeutic candidates. For example, the observation that the AXL receptor tyrosine kinase protein is highly expressed in human RGCs and oRGCs has led to the hypothesis that it could function as a ZIKV entry receptor in NPCs (Nowakowski et al., 2016a). To test this hypothesis, AXL was deleted via genome editing in hPSCs and the resulting cerebral organoids showed no difference in ZIKV infection and pathophysiology, suggesting that AXL is dispensable for ZIKV infection in human NPCs (Wells et al., 2016). In another example, a recent study screened over 6000 drug candidates and approved drugs using monolayer NPC cultures and identified a number of hits that were then applied to forebrain organoids to test drug efficacy and to evaluate potential toxicity (Xu et al., 2016). The same principle applies to validating antibodies against ZIKV for vaccine development. Whereas most screens are conducted by measuring one or two specific parameters, characterization of brain organoids can provide comprehensive insights into the effectiveness of therapeutic candidates to rescue the effects of ZIKV at molecular, cellular and structural levels.
Conclusions
Studies using brain organoids derived from hPSCs have contributed substantially to a growing body of knowledge on the effects of ZIKV infection on fetal brain development (Ming et al., 2016). Brain organoids have proven to be an invaluable model system for studying human cortical development and diseases in general. With future improvements, the brain organoid system presents a unique and comprehensive platform to investigate human-specific developmental features as a continuous process in a highly relevant context, and holds great promise for therapeutic development.
Acknowledgements
We thank Dr. Kimberly M. Christian for comments.
Footnotes
Competing interests
H.N.N., H.S. and G.-l.M. are co-founders of 3Dnamics.
Funding
Work in the authors' laboratories was supported by the National Institutes of Health (R01MH105128 and R35NS097370 to G.-l.M.; R37NS047344, U19MH106434 and P01NS097206 to H.S.; T32MH015330 to H.N.N.), Maryland Stem Cell Research Fund (to G.-l.M. and H.S.), Simons Foundation Autism Research Initiative (SFARI) (to G.-l.M. and H.S.), Foundation for Prader-Willi Research (to G.-l.M.) and Dr. Miriam and Sheldon G. Adelson Medical Research Foundation (to G.-l.M.). Deposited in PMC for release after 12 months.
References
- Barrows N. J., Campos R. K., Powell S. T., Prasanth K. R., Schott-Lerner G., Soto-Acosta R., Galarza-Muñoz G., McGrath E. L., Urrabaz-Garza R., Gao J. et al. (2016). A screen of FDA-approved drugs for inhibitors of Zika virus infection. Cell Host Microbe 20, 259-270. 10.1016/j.chom.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvet G., Aguiar R. S., Melo A. S. O., Sampaio S. A., de Filippis I., Fabri A., Araujo E. S. M., de Sequeira P. C., de Mendonça M. C. L., de Oliveira L. et al. (2016). Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect. Dis. 16, 653-660. 10.1016/S1473-3099(16)00095-5 [DOI] [PubMed] [Google Scholar]
- CDC (2016). Zika virus. Atlanta, GA: US Department of Health and Human Services, United States Centers for Disease Control and Prevention; https://www.cdc.gov/zika/index.html. [Google Scholar]
- Cugola F. R., Fernandes I. R., Russo F. B., Freitas B. C., Dias J. L., Guimaraes K. P., Benazzato C., Almeida N., Pignatari G. C., Romero S. et al. (2016). The Brazilian Zika virus strain causes birth defects in experimental models. Nature 534, 267-271. 10.1038/nature18296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang J., Tiwari S. K., Lichinchi G., Qin Y., Patil V. S., Eroshkin A. M. and Rana T. M.(2016). Zika virus depletes neural progenitors in human cerebral organoids through activation of the innate immune receptor TLR3. Cell Stem Cell 19, 258-265. 10.1016/j.stem.2016.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick G. W. A., Kitchen S. F. and Haddow A. J.(1952). Zika virus (I). Isolations and serological specificity. Trans. R. Soc. Trop. Med. Hyg. 46, 509-520. 10.1016/0035-9203(52)90042-4 [DOI] [PubMed] [Google Scholar]
- Faria N. R., Azevedo Rdo S. S., Kraemer M. U. G., Souza R., Cunha M. S., Hill S. C., Theze J., Bonsall M. B., Bowden T. A., Rissanen I. et al. (2016). Zika virus in the Americas: early epidemiological and genetic findings. Science 352, 345-349. 10.1126/science.aaf5036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauci A. S. and Morens D. M.(2016). Zika virus in the Americas--yet another arbovirus threat. N. Engl. J. Med. 374, 601-604. 10.1056/NEJMp1600297 [DOI] [PubMed] [Google Scholar]
- Garcez P. P., Loiola E. C., Madeiro da Costa R., Higa L. M., Trindade P., Delvecchio R., Nascimento J. M., Brindeiro R., Tanuri A. and Rehen S. K.(2016). Zika virus impairs growth in human neurospheres and brain organoids. Science 352, 816-818. 10.1126/science.aaf6116 [DOI] [PubMed] [Google Scholar]
- Hanners N. W., Eitson J. L., Usui N., Richardson R. B., Wexler E. M., Konopka G. and Schoggins J. W.(2016). Western Zika virus in human fetal neural progenitors persists long term with partial cytopathic and limited immunogenic effects. Cell Rep. 15, 2315-2322. 10.1016/j.celrep.2016.05.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heukelbach J., Alencar C. H., Kelvin A. A., De Oliveira W. K. and Pamplona de Góes Cavalcanti L.(2016). Zika virus outbreak in Brazil. J. Infect. Dev. Ctries 10, 116-120. 10.3855/jidc.8217 [DOI] [PubMed] [Google Scholar]
- Heymann D. L., Hodgson A., Sall A. A., Freedman D. O., Staples J. E., Althabe F., Baruah K., Mahmud G., Kandun N., Vasconcelos P. F. C. et al. (2016). Zika virus and microcephaly: why is this situation a PHEIC? Lancet 387, 719-721. 10.1016/S0140-6736(16)00320-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo J., Xiao Y., Sun A. X., Cukuroglu E., Tran H.-D., Göke J., Tan Z. Y., Saw T. Y., Tan C.-P., Lokman H. et al. (2016). Midbrain-like organoids from human pluripotent stem cells contain functional dopaminergic and neuromelanin-producing neurons. Cell Stem Cell 19, 248-257. 10.1016/j.stem.2016.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadoshima T., Sakaguchi H., Nakano T., Soen M., Ando S., Eiraku M. and Sasai Y.(2013). Self-organization of axial polarity, inside-out layer pattern, and species-specific progenitor dynamics in human ES cell-derived neocortex. Proc. Natl. Acad. Sci. USA 110, 20284-20289. 10.1073/pnas.1315710110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelava I. and Lancaster M. A.(2016). Stem cell models of human brain development. Cell Stem Cell 18, 736-748. 10.1016/j.stem.2016.05.022 [DOI] [PubMed] [Google Scholar]
- Lancaster M. A., Renner M., Martin C.-A., Wenzel D., Bicknell L. S., Hurles M. E., Homfray T., Penninger J. M., Jackson A. P. and Knoblich J. A.(2013). Cerebral organoids model human brain development and microcephaly. Nature 501, 373-379. 10.1038/nature12517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Xu D., Ye Q., Hong S., Jiang Y., Liu X., Zhang N., Shi L., Qin C.-F. and Xu Z.(2016). Zika virus disrupts neural progenitor development and leads to microcephaly in mice. Cell Stem Cell 19, 120-126. 10.1016/j.stem.2016.04.017 [DOI] [PubMed] [Google Scholar]
- Liang Q., Luo Z., Zeng J., Chen W., Foo S.-S., Lee S.-A., Ge J., Wang S., Goldman S. A., Zlokovic B. V. et al. (2016). Zika virus NS4A and NS4B proteins deregulate Akt-mTOR signaling in human fetal neural stem cells to inhibit neurogenesis and induce autophagy. Cell Stem Cell 19, 663-671. 10.1016/j.stem.2016.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lui J. H., Hansen D. V. and Kriegstein A. R.(2011). Development and evolution of the human neocortex. Cell 146, 18-36. 10.1016/j.cell.2011.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariani J., Coppola G., Zhang P., Abyzov A., Provini L., Tomasini L., Amenduni M., Szekely A., Palejev D., Wilson M. et al. (2015). FOXG1-dependent dysregulation of GABA/glutamate neuron differentiation in autism spectrum disorders. Cell 162, 375-390. 10.1016/j.cell.2015.06.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merkle F. T., Maroof A., Wataya T., Sasai Y., Studer L., Eggan K. and Schier A. F.(2015). Generation of neuropeptidergic hypothalamic neurons from human pluripotent stem cells. Development 142, 633-643. 10.1242/dev.117978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ming G.-l., Tang H. and Song H.(2016). Advances in Zika virus research: stem cell models, challenges, and opportunities. Cell Stem Cell 19, 690-702. 10.1016/j.stem.2016.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mlakar J., Korva M., Tul N., Popović M., Poljšak-Prijatelj M., Mraz J., Kolenc M., Resman Rus K., Vesnaver Vipotnik T., Fabjan Vodusek V. et al. (2016). Zika virus associated with microcephaly. N. Engl. J. Med. 374, 951-958. 10.1056/NEJMoa1600651 [DOI] [PubMed] [Google Scholar]
- Nguyen H. N., Qian X., Song H. and Ming G.-l.(2016). Neural stem cells attacked by Zika virus. Cell Res. 26, 753-754. 10.1038/cr.2016.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowakowski T. J., Pollen A. A., Di Lullo E., Sandoval-Espinosa C., Bershteyn M. and Kriegstein A. R.(2016a). Expression analysis highlights AXL as a candidate Zika virus entry receptor in neural stem cells. Cell Stem Cell 18, 591-596. 10.1016/j.stem.2016.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowakowski T. J., Pollen A. A., Sandoval-Espinosa C. and Kriegstein A. R.(2016b). Transformation of the radial glia scaffold demarcates two stages of human cerebral cortex development. Neuron 91, 1219-1227. 10.1016/j.neuron.2016.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onorati M., Li Z., Liu F., Sousa A. M., Nakagawa N., Li M., Dell'Anno M. T., Gulden F. O., Pochareddy S., Tebbenkamp A. T. et al. (2016). Zika virus disrupts phospho-TBK1 localization and mitosis in human neuroepithelial stem cells and radial glia. Cell Rep. 16, 2576-2592. 10.1016/j.celrep.2016.08.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paşca A. M., Sloan S. A., Clarke L. E., Tian Y., Makinson C. D., Huber N., Kim C. H., Park J.-Y., O'Rourke N. A., Nguyen K. D. et al. (2015). Functional cortical neurons and astrocytes from human pluripotent stem cells in 3D culture. Nat. Methods 12, 671-678. 10.1038/nmeth.3415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen E., Wilson M. E., Touch S., McCloskey B., Mwaba P., Bates M., Dar O., Mattes F., Kidd M., Ippolito G. et al. (2016). Rapid spread of Zika virus in the Americas-implications for public health preparedness for mass gatherings at the 2016 Brazil Olympic Games. Int. J. Infect. Dis. 44, 11-15. 10.1016/j.ijid.2016.02.001 [DOI] [PubMed] [Google Scholar]
- Qian X., Nguyen H. N., Song M. M., Hadiono C., Ogden S. C., Hammack C., Yao B., Hamersky G. R., Jacob F., Zhong C. et al. (2016). Brain-region-specific organoids using mini-bioreactors for modeling ZIKV exposure. Cell 165, 1238-1254. 10.1016/j.cell.2016.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retallack H., Di Lullo E., Arias C., Knopp K. A., Laurie M. T., Sandoval-Espinosa C., Mancia Leon W. R., Krencik R., Ullian E. M., Spatazza J. et al. (2016). Zika virus cell tropism in the developing human brain and inhibition by azithromycin. Proc. Natl. Acad. Sci. USA 113, 14408-14413. 10.1073/pnas.1618029113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakaguchi H., Kadoshima T., Soen M., Narii N., Ishida Y., Ohgushi M., Takahashi J., Eiraku M. and Sasai Y.(2015). Generation of functional hippocampal neurons from self-organizing human embryonic stem cell-derived dorsomedial telencephalic tissue. Nat. Commun. 6, 8896 10.1038/ncomms9896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonin Y., Loustalot F., Desmetz C., Foulongne V., Constant O., Fournier-Wirth C., Leon F., Molès J.-P., Goubaud A., Lemaitre J.-M. et al. (2016). Zika virus strains potentially display different infectious profiles in human neural cells. EBioMedicine 12, 161-169. 10.1016/j.ebiom.2016.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson D. I. H.(1964). Zika virus infection in man. Trans. R. Soc. Trop. Med. Hyg. 58, 335-338. 10.1016/0035-9203(64)90201-9 [DOI] [PubMed] [Google Scholar]
- Takahashi K., Tanabe K., Ohnuki M., Narita M., Ichisaka T., Tomoda K. and Yamanaka S.(2007). Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131, 861-872. 10.1016/j.cell.2007.11.019 [DOI] [PubMed] [Google Scholar]
- Tang H., Hammack C., Ogden S. C., Wen Z., Qian X., Li Y., Yao B., Shin J., Zhang F., Lee E. M. et al. (2016). Zika virus infects human cortical neural progenitors and attenuates their growth. Cell Stem Cell 18, 587-590. 10.1016/j.stem.2016.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura C. V., Maia M., Bravo-Filho V., Gois A. L. and Belfort R. Jr.(2016). Zika virus in Brazil and macular atrophy in a child with microcephaly. Lancet 387, 228 10.1016/S0140-6736(16)00006-4 [DOI] [PubMed] [Google Scholar]
- Wang L., Meece K., Williams D. J., Lo K. A., Zimmer M., Heinrich G., Martin Carli J., Leduc C. A., Sun L., Zeltser L. M. et al. (2015). Differentiation of hypothalamic-like neurons from human pluripotent stem cells. J. Clin. Invest. 125, 796-808. 10.1172/JCI79220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells M. F., Salick M. R., Wiskow O., Ho D. J., Worringer K. A., Ihry R. J., Kommineni S., Bilican B., Klim J. R., Hill E. J. et al. (2016). Genetic ablation of AXL does not protect human neural progenitor cells and cerebral organoids from Zika virus infection. Cell Stem Cell 19, 703-708. 10.1016/j.stem.2016.11.011 [DOI] [PubMed] [Google Scholar]
- Wen Z., Christian K. M., Song H. and Ming G.-l.(2016). Modeling psychiatric disorders with patient-derived iPSCs. Curr. Opin. Neurobiol. 36, 118-127. 10.1016/j.conb.2015.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu M., Lee E. M., Wen Z., Cheng Y., Huang W.-K., Qian X., Tcw J., Kouznetsova J., Ogden S. C., Hammack C. et al. (2016). Identification of small-molecule inhibitors of Zika virus infection and induced neural cell death via a drug repurposing screen. Nat. Med. 22, 1101-1107. 10.1038/nm.4184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang F., Hammack C., Ogden S. C., Cheng Y., Lee E. M., Wen Z., Qian X., Nguyen H. N., Li Y., Yao B. et al. (2016). Molecular signatures associated with ZIKV exposure in human cortical neural progenitors. Nucleic Acids Res. 44, 8610-8620. 10.1093/nar/gkw765 [DOI] [PMC free article] [PubMed] [Google Scholar]