Abstract
Flibanserin (Addyi) for female sexual interest/arousal disorder in premenopausal women
INTRODUCTION
Female sexual interest/arousal disorder (FSIAD) is a newly defined clinical diagnosis that appears in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5).1 The diagnosis was previously listed as hypoactive sexual desire disorder (HSDD) in DSM-4 and as inhibited sexual desire disorder in DSM-3. References to the condition prior to 2013 (and even afterward), including research studies, often refer to the condition as HSDD.
FSIAD is characterized by significantly reduced or lack of sexual interest or arousal in women.1 To meet the criteria for diagnosis, patients must exhibit an absence or reduction in three of the following items for a minimum of six months: interest in sexual activity; sexual or erotic thoughts and fantasies; initiation of sexual activity and being unreceptive to a partner’s attempts to initiate; sexual excitement or pleasure during sexual activity; sexual interest/arousal in response to sexual or erotic cues; and genital or nongenital sensations during sexual activity. The presenting symptoms must cause clinically significant distress in the individual and cannot be better explained by a nonsexual mental disorder or as a consequence of severe relationship distress or another significant stressor.1
Based on epidemiologic studies, the prevalence of FSIAD is not well known, and sexual desire among women can be greatly influenced by hormonal changes, ethnicity, medical comorbidities, medications, and psychological distress. Prevalence estimates vary, especially with changes in terminology and definitions, with studies reporting estimates of 6% to 46% in premenopausal women, with desire disorders likely being approximately 10% and possibly higher in post-menopausal women.2–5 Asian ethnicities, including Chinese and Japanese women, reported higher rates of low sexual desire.6 Cardiovascular disease, diabetes mellitus, urological and gynecological disorders, and psychotropic medications can all reduce levels of sexual desire and libido.3,5 Because sexual dysfunction is often multifactorial, the true prevalence of sexual desire disorders unrelated to psychological or other medical conditions is difficult to capture in epidemiologic studies. Epidemiologic studies based on DSM-5 criteria are not yet available.
Prior to 2015, no Food and Drug Administration (FDA)-approved treatments were available to address sexual desire disorders in women in the United States. The transdermal testosterone patch, Intrinsa (Warner Chilcott UK Ltd.), was the only commercially approved product available for the disorder in the European Union, but its marketing authorization was withdrawn in 2012.7 Some off-label treatments used for FSIAD include: androgens, such as testosterone or antiprogesterone compounds; bupropion; and the phosphodiesterase inhibitor sildenafil. Sildenafil and bupropion have limited utility in treating sexual desire in women due to lack of efficacy, and testosterone supplementation is controversial due to the risks associated with hormone replacement and the lack of data to support use.4,5,8
Flibanserin (Addyi, Sprout Pharmaceuticals) is a multimodal serotonergic agent that was originally developed by Boehringer Ingelheim for the treatment of major depressive disorder. Flibanserin was unsuccessful in clinical trials for treating depression, but was reported to have the side effect of increased libido in female patients. Boehringer Ingelheim filed a new drug application (NDA) with the FDA for the use of flibanserin in the treatment of female HSDD in 2009, but approval was denied due to the failure of two clinical trials to show statistical improvement in the coprimary endpoint of sexual desire. Sprout Pharmaceuticals subsequently purchased the rights to flibanserin and again filed an NDA in 2013. The FDA did not approve the application, citing safety concerns, and requested additional studies, including a trial examining the effects of the drug on driving ability due to its potential to cause severe drowsiness and a study to determine if cytochrome P450 (CYP) enzymes are involved in the drug’s metabolism. Sprout Pharmaceuticals completed the required studies and submitted another NDA in February 2015. In August 2015, the FDA approved flibanserin as the first drug for treating female sexual interest/arousal disorder of any severity.9
INDICATION
Flibanserin is indicated for acquired generalized FSIAD of any severity, from mild to severe, in premenopausal women. It is not approved for decreased libido or other sexual dysfunction secondary to antidepressant use. The disorder is characterized by low sexual desire that causes marked distress or interpersonal difficulty and is not secondary to relationship issues, substance- or drug-induced causes, or a comorbid medical or psychiatric condition that could influence sexual desire.9
CHEMICAL PROPERTIES
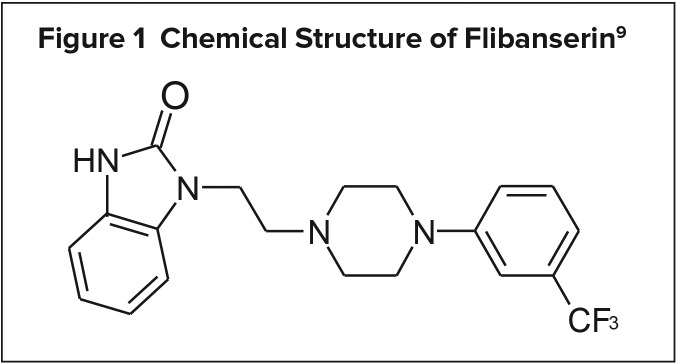
Flibanserin is a 5-hydroxytryptamine 1A (5-HT1A) agonist/5-HT2A antagonist that also exhibits weak to moderate antagonism at 5-HT2B, 5-HT2C, and dopamine D4 receptors. Its chemical and empirical formula are 2H-benzimidazol-2-one, 1, 3-dihydro-1-[2-[4-[3-(trifluoromethyl) phenyl]-1-piperazinyl]ethyl] and C20H21F3N4O, respectively. Its structural formula is illustrated in Figure 1.9
Figure 1.
Chemical Structure of Flibanserin9
PHARMACOLOGY AND MECHANISM OF ACTION
Although the mechanism of action of flibanserin is not well elucidated in FSIAD, flibanserin exerts regional selectivity for serotonin receptors in the central nervous system, having high affinity for 5-HT1A receptors in the hippocampus and the prefrontal cortex, with no activation present in the dorsal raphe. In addition, flibanserin exerts greater selectivity for postsynaptic 5-HT1A receptors. Agonist activity at 5-HT1A postsynaptic receptors has downstream effects in altering levels of other monoamines, including dopamine.9–11 Combined with 5-HT2A antagonism, chronic treatment with flibanserin boosts levels of dopamine in the mesocortical area of the prefrontal cortex from ventral tegmental projections.10,11 Flibanserin also produces a net increase in norepinephrine concentrations selectively in the prefrontal cortex through disinhibition of locus coeruleus noradrenergic neurons.10–12
Both dopamine and norepinephrine play a critical role in sexual excitation, with norepinephrine playing a stimulating role in sexual arousal and dopamine playing a role in boosting desire.12,13 Flibanserin does not alter dopamine neurotransmission within the nucleus accumbens, thus no abusive properties are seen with flibanserin.10 In addition, flibanserin reduces concentrations of serotonin in the prefrontal cortex with chronic administration. Like other monoamines, serotonin modulates sexual activity in an inhibitory fashion through downstream decreases in dopamine release in the prefrontal cortex. By modulating these monoamines in patients with FSIAD, flibanserin could theoretically improve sexual desire and arousal. In addition to activity at the 5-HT1A and 5-HT2A receptors, flibanserin has weak antagonistic activity at 5-HT2C, 5-HT2B, and dopamine D4 receptors. Flibanserin’s therapeutic activity has yet to be fully linked to activity at these receptors.10,11
PHARMACOKINETICS
Flibanserin has an absolute bio-availability of 33% following oral administration. Flibanserin displays linear pharmacokinetics in doses ranging from 100 mg to 250 mg in healthy women and reaches maximal concentrations 0.75 hours after administration (maximal concentration = 419 ng/mL). Administration with food slows the rate of absorption and increases the extent of absorption up to 56%. Flibanserin is highly protein bound (98%) to serum proteins, primarily albumin. Flibanserin undergoes extensive first-pass metabolism and is primarily metabolized to inactive metabolites by the hepatic isoenzymes CYP3A4 and, to a lesser extent, CYP2C19.9
The average terminal half-life of flibanserin is 11 hours, and steady-state concentrations are achieved after three days of administration. The half-life is increased to 26 hours and the area under the curve is increased 4.5-fold in patients with mild hepatic impairment. Due to marked elevations in concentrations in patients with hepatic insufficiency, flibanserin should not be used in patients with hepatic impairment.9 Flibanserin concentrations are slightly increased in mild-to-moderate renal impairment by 1.1-fold and in severe renal impairment by 1.2-fold. Flibanserin metabolites are primarily eliminated in the urine (44%) and feces (51%).8
DOSAGE AND ADMINISTRATION
The starting and recommended maximum dose for flibanserin is 100 mg at bedtime. Flibanserin can be administered with or without food; however, food increases systemic absorption. Flibanserin should not be taken during daytime hours because this increases the risk of hypotension, somnolence, and syncope. An adequate treatment trial of flibanserin is eight weeks, and if no improvements in sexual desire are observed or experienced by week 8, then flibanserin should be discontinued.9
CLINICAL TRIALS
Efficacy
The efficacy and safety of flibanserin have been studied extensively in phase2 and phase 3 trials for the treatment of FSIAD in premenopausal women. The FDA approval of flibanserin was based on three phase 3, 24-week, randomized, placebo-controlled trials in premenopausal women in North America (the BEGONIA, DAISY, and VIOLET studies).14–16 All three trials utilized the DSM-4 criteria for HSDD. The three studies included only premenopausal women 18 years of age or older diagnosed with acquired generalized HSDD for a duration of 24 weeks or more prior to the study. Participants were required to score at least 15 on the Female Sexual Distress Scale–Revised (FSDS–R) and to score 0 or 1 on the Sexual Interest and Desire Inventory–Female scale (indicating a lack of receptivity to a partner’s sexual approach). In addition, the women were required to be in a monogamous heterosexual relationship of at least one year.14–16 Exclusion criteria included diagnoses of sexual dysfunction other than HSDD, psychiatric disorders that may impact sexual function, major depressive disorder within the past six months, and substance abuse or any other ongoing clinical disorder. Participants were also deemed ineligible if they were using hormone therapy (except contraceptives), antiarrhythmics, beta blockers, central nervous system stimulants, anticoagulants, dopamine agonists, muscle relaxants, benzodiazepines, sedative hypnotics, antidepressants, anti-psychotics, antiepileptic drugs, mood stabilizers, St. John’s wort, yohimbine, metoclopramide, narcotics, or triptans. Women were also excluded if they had received psychotherapeutic treatment within 12 weeks of the study or if they had experienced a recent major life stressor.14–16
The BEGONIA trial examined the coprimary endpoints of change in the number of satisfying sexual encounters (SSEs) over 28 days and Female Sexual Function Index (FSFI) score. The SSEs were reported using a daily electronic diary, while FSFI was determined through a two-question test on which participants rated their sexual desire on a scale of 1–5 every fourweeks. Secondary outcomes were defined as change from baseline in FSFI total score, FSDS–R total score, and FSDS-R item 13 score (“bothered by low sexual desire”).14
Premenopausal women were randomized to receive either placebo (n = 545) or flibanserin 100 mg (n = 542) daily at bedtime for 24 weeks. Flibanserin improved the number of SSEs (2.5 versus 1.5; P ≤ 0.0001) and sexual desire score based on the FSFI (5.3 versus 3.5; P ≤ 0.0001) compared with placebo.14 Primary and relevant secondary outcomes are listed in Table 1.
Table 1.
Flibanserin 100 mg in Phase 3 Clinical Trials: Mean Change in Effiacy Parameters at 24 Weeks9
| BEGONIA14 | DAISY15 | VIOLET16 | ||||
|---|---|---|---|---|---|---|
| Placebo (n = 545) | Flibanserin (n = 542) | Placebo (n = 398) | Flibanserin (n = 395) | Placebo (n = 295) | Flibanserin (n = 290) | |
| Number of SSEs, mean (SD)* | 1.5 (4.5) | 2.5 (4.6) (P < 0.001) | 1.1 (0.2) | 1.9 (0.3) (P < 0.001) | 0.8 (0.2) | 1.6 (0.23) P < 0.01 |
| SFI desire domain score, mean (SE) | 0.7 (0.1) | 1.0 (0.1) (P < 0.001) | 0.6 (0.1) | 0.9 (0.1) (P < 0.001) | 0.5 (0.1) | 0.9 (0.1) (P < 0.001) |
| FSFI total score, mean (SE) | 3.5 (0.3) | 5.3 (0.3) (P < 0.001) | 2.6 (0.3) | 4.1 (0.3) (P < 0.001) | 2.4 (0.4) | 5.0 (0.4) (P < 0.001) |
| FSDS–R item 13 score, mean (SE) | −0.7 (0.1) | −1.0 (0.1) (P < 0.001) | −0.5 (0.1) | −0.7 (0.1) (P < 0.001) | −0.5 (0.1) | −0.8 (0.1) (P < 0.001) |
| FSDS–R total score, mean (SE) | −6.1 (0.6) | −9.4 (0.6) (P < 0.001) | −5.2 (0.5) | −7.8 (0.5) (P < 0.001) | −4.9 (0.7) | −8.9 (0.7) (P < 0.001) |
standardized to 28-day period.
FSDS–R = Female Sexual Distress Scale–Revised; FSFI = Female Sexual Function Index; item 13 = “bothered by low sexual desire;” SD = standard deviation; SE = standard error; SSEs = satisfying sexual encounters.
The DAISY trial examined two coprimary endpoints in placebo (n = 398) versus three flibanserin arms: 25 mg twice daily (n = 396), 50 mg twice daily (n = 392), and 100 mg once daily at bedtime (n = 395). Coprimary endpoints were defined as changes in the number of SSEs and sexual desire score from baseline at 24 weeks. Reports of both endpoints were recorded using a daily electronic diary. Secondary endpoints included change in FSDS–R total score and FSDS–R item 13 score at week 24. Only the 100-mg flibanserin treatment showed a statistically significant increase in SSEs (1.9 versus 1.1; P < 0.01). Sexual desire based on the FSFI scale increased statistically with all dosage forms of flibanserin, with the greatest increase seen in the 100-mg group versus placebo (0.9 versus 0.6, respectively; P < 0.0001).15 Primary and relevant secondary outcomes are listed in Table 1.
The VIOLET trial randomized patients to placebo (n = 295), flibanserin 50 mg (n = 295), or flibanserin 100 mg once daily at bedtime (n = 290). Coprimary and secondary endpoints were the same as the DAISY trial and measured changes from baseline to week 24. Both coprimary endpoints were recorded using an electronic diary. Both the flibanserin 50-mg and 100-mg treatment groups showed a statistically significant increase in SSEs (1.4, P< 0.05; 1.6, P < 0.01, respectively) compared with placebo (0.8). Sexual desire based on FSFI was significantly higher at the conclusion of the trial for flibanserin 50 mg once a day (0.8; P< 0.05) and flibanserin 100 mg once a day (0.9; P < 0.0001) compared with placebo (0.5).16 Primary and relevant secondary outcomes are listed in Table 1.
Supportive responder analyses were conducted by both the FDA and the investigators to determine treatment response in the three trials. Using the Patient Global Impression–Improvement scale, responders were classified as either “very much improved” or “much improved.” From eight to 24 weeks, patients treated with flibanserin had a placebo-adjusted response rate of approximately 10% reporting “much improved” or “very much improved” status (e.g., 9.9% versus 21.1%; P < 0.01, at 24 weeks). 17
Although it is not FDA-approved for treatment of sexual dysfunction in post-menopausal women, the safety and efficacy of flibanserin was assessed in this population in the SNOWDROP trial, in which the patients received placebo (n= 481) or flibanserin 100 mg (n = 468) daily at bedtime over a test period of 24 weeks. Similar to the studies performed in premenopausal women, the coprimary endpoints were change in SSEs over a 28-day period and change in FSFI desire domain score. The number of SSEs reported was statistically significantly greater in the flibanserin group (+1.0) versus the placebo group (+0.6; P= 0.004). FSFI desire domain scores also increased in the flibanserin group (+0.7) compared with placebo (+0.4; P < 0.001).18 These positive findings have yet to be duplicated in a second clinical study.
Safety
A total of 2,997 women were treated with flibanserin 100 mg in clinical trials; of these patients, 1,672 were treated for at least six months, 850 received treatment for at least 12 months, and 88 were treated for at least 18 months. The most commonly reported adverse event in the phase 3 clinical trials in premenopausal women was dizziness.9,14–16 Common adverse effects reported were headache, dizziness, fatigue, somnolence, and nausea. Flibanserin appears to have a dose-dependent sedative effect, likely due to its 5-HT2A antagonism. Dosing the drug at bedtime can decrease, but not completely ameliorate, this effect. Somnolence recorded in the DAISY study varied by frequency of administration: 16.3% with flibanserin 50 mg twice daily and 11.9% with 100 mg once daily at bedtime.15 Hypotension and syncope occurred in 0.2% of flibanserin-treated patients compared with less than 0.1% of placebo-treated patients in clinical trials. Taking more than the recommended maximum dose and taking flibanserin during daytime hours increase this risk. A statistically small dose-related increase in malignant mammary tumors was noted in mice when flibanserin was used at three to 10 times the recommended maximum dose over a two-year period. The clinical significance of this increase has not been demonstrated in human studies, yet it is included in the warnings section in the package labeling.9 There were no elevated prolactin levels noted in the clinical trials.17 Also, no increase in QT-prolongation was observed in clinical trials.17 Common adverse effects associated with flibanserin from the North American trials are reported in Table 2.
Table 2.
Flibanserin 100 mg Safety in Phase 3 Clinical Trials: Frequency of Adverse Effects9
| BEGONIA14 | DAISY15 | VIOLET16 | ||||
|---|---|---|---|---|---|---|
| Placebo (n = 545) (%) | Flibanserin (n = 542) (%) | Placebo (n = 398) (%) | Flibanserin (n = 395) (%) | Placebo (n = 295) (%) | Flibanserin (n = 290) (%) | |
| Any AE | 275 (50.5) | 337 (62.2) | 234 (58.8) | 274 (69.4) | 175 (59.3) | 193 (66.6) |
| Somnolence | 19 (3.5) | 78 (14.4) | 14 (3.5) | 47 (11.9) | 9 (3.1) | 32 (11.0) |
| Dizziness | 6 (1.1) | 56 (10.3) | 8 (2.0) | 48 (12.2) | 5 (1.7) | 26 (9.0) |
| Nausea | 12 (2.2) | 41 (7.6) | 16 (4.0) | 47 (11.9) | 12 (4.1) | 33 (11.4) |
| Fatigue | 18 (3.3) | 31 (5.7) | 27 (6.8) | 38 (9.6) | 8 (2.7) | 18 (6.2) |
| URTI | 13 (2.4) | 28 (5.2) | 20 (5.0) | 25 (6.3) | 15 (5.1) | 13 (4.5) |
AE = adverse effect; URTI = upper respiratory tract infection
WARNINGS AND PRECAUTIONS
Flibanserin carries a boxed warning for hypotension and syncope in certain settings, including with the concurrent use of alcohol and/or moderate or strong CYP3A4 inhibitors, and for patients with hepatic impairment.9
A risk evaluation and mitigation strategy (REMS) program has been established for flibanserin specifically due to the risk of hypotension and syncope associated with concomitant alcohol use. Prescribers must complete certification training before being able to prescribe flibanserin and must document that they counseled the patient on avoiding alcohol use with flibanserin treatment. Pharmacies must be certified with the REMS program and can only dispense flibanserin to patients after they have verified that the prescriber is certified.9
DRUG INTERACTIONS
Flibanserin exerts agonist and antagonist action at various serotonin receptors, making pharmacodynamic interactions possible with medications that alter or are involved in serotonergic neurotransmission in both the central and peripheral nervous systems. The phase 3 clinical trials conducted with flibanserin excluded patients who took serotonergic antidepressants, triptans, and other serotonergic compounds.9
Flibanserin was studied with paroxetine for 10 days to determine pharmacokinetic drug interactions. Flibanserin exposure decreased by 4% when combined with paroxetine compared with flibanserin alone.9 Animal trials utilizing flibanserin with other serotonergic antidepressants, fluoxetine and imipramine, revealed no significant increase in serotonin toxicity when combined and at supratherapeutic dosages in rats.19 Although human data are lacking regarding pharmacodynamic interactions with serotonergic compounds, based on flibanserin’s ability to decrease serotonin neurotransmission in various areas of the central nervous system, the theoretical risk of serotonin syndrome should be low. Nevertheless, given the seriousness of serotonin syndrome, caution and vigilance is warranted when combining flibanserin with other serotonergic agents due to the paucity of data and limited clinical experience to date.
Compounds that interfere with or reduce sexual desire may decrease the effectiveness of flibanserin. Pharmacodynamic interaction studies are lacking; however, drugs known to cause sexual dysfunction, such as selective-serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, anti-psychotics, tricyclic antidepressants, anticholinergics, antihistamines, anti-androgenic progesterones, various anti-hypertensives, and diuretics, may have negative effects on sexual function and limit the utility of flibanserin.4,5,20
Clinical safety data reveal that flibanserin treatment may commonly cause somnolence and is thus recommended only at bedtime. Due to this somnolence, the concomitant use of flibanserin with central nervous system depressants, including opioids, benzodiazepines, and sedating antihistamines, should be observed cautiously as the combination of these classes of medications with flibanserin could increase the risk of central nervous system depression.9
Flibanserin is primarily metabolized by CYP3A4 and is subject to pharmacokinetic interactions mediated by CYP3A4 inhibition and induction. Flibanserin is contraindicated with moderate and strong CYP3A4 inhibitors due to marked increases in peak plasma levels of flibanserin, leading to hypotension and syncope. Strong CYP3A4 inducers limit the utility of flibanserin, as rifampin decreased concentrations of flibanserin by 95%. Although not contraindicated, strong CYP2C19 inhibitors should be used cautiously with flibanserin, as they could theoretically lead to higher levels of and adverse effects associated with flibanserin.9
COST
The average wholesale price of a 30-day supply of 100-mg tablets is $960.21
P&T COMMITTEE CONSIDERATIONS
Flibanserin is the first drug in its class to treat FSIAD in premenopausal women. Based on clinical trials in North America, flibanserin demonstrated modest efficacy for increasing SSEs and FSFI sexual desire scores.14 Based on the research, flibanserin treatment may lead to an additional one-half SSE per month.14–16 Although flibanserin appears to offer a small but statistically significant benefit to premenopausal women with FSIAD, the required REMS program adherence and the possibility of hypotension and syncope with use provide a disincentive to prescribe or utilize this medication. Costs and continuous treatment, along with the required avoidance of alcohol while using flibanserin, will hinder the clinical utility of the drug. There is cause for concern that the study examining the combination of alcohol and flibanserin included mostly male test subjects, though women may experience faster onset and greater effects of alcohol than their male counterparts. With somnolence, dizziness, and fatigue reported in approximately 10% to 20% of treated patients and a REMS system in place to reduce the risk of hypotension and syncope, undue adverse effects are possible with flibanserin.
The long-term clinical utility of flibanserin is unknown at this time, and additional safety and drug interaction studies are needed to determine its legitimacy for routine clinical use. In many cases, the safety risks of using flibanserin will outweigh the small net benefits in improving sexual desire. The best candidates for treatment with flibanserin are women with FSIAD who have not had success with psychosocial interventions, are willing to accept the risks associated with continued use, and are capable of abstaining from alcohol during the entire course of treatment. Recognizing the disparity of agents available to women for FSIAD, sexual dysfunction, or low libido compared to those available to men, flibanserin represents some progress, though limited, as a treatment option that may improve sexual function and outcomes for some women.
Footnotes
Disclosures: The authors report no financial or commercial relationships in regard to this article.
REFERENCES
- 1.American Psychiatric Association; DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- 2.West SL, D’Aloisio AA, Agans RP, et al. Prevalence of low sexual desire and hypoactive sexual desire disorder in a nationally representative sample of U.S. women. Arch Intern Med. 2008;168(13):1441–1449. doi: 10.1001/archinte.168.13.1441. [DOI] [PubMed] [Google Scholar]
- 3.Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35–39. doi: 10.1111/j.1743-6109.2004.10106.x. [DOI] [PubMed] [Google Scholar]
- 4.Simons JS, Carey MP. Prevalence of sexual dysfunctions: results from a decade of research. Arch Sex Behav. 2001;30(2):177–219. doi: 10.1023/a:1002729318254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frank JE, Mistretta P, Will J. Diagnosis and treatment of female sexual dysfunction. Amer Fam Phys. 2008;77(5):635–642. [PubMed] [Google Scholar]
- 6.Cain VS, Johannes CB, Avis NE, et al. Sexual functioning and practices in a multiethnic study of midlife women: baseline results from SWAN. J Sex Res. 2003;40(3):266–276. doi: 10.1080/00224490309552191. [DOI] [PubMed] [Google Scholar]
- 7.European Medicines Agency. Intrinsa (testosterone): withdrawal of the marketing authorisation in the European Union. Jul 11, 2012. [Accessed February 2, 2017]. Available at: www.ema.europa.eu/docs/en_GB/document_library/Public_state-ment/2012/06/WC500128837.pdf.
- 8.Lodise NM. Hypoactive sexual desire disorder in women: treatment options beyond testosterone and approaches to communicating with patients on sexual health. Pharmacotherapy. 2013;33(4):411–421. doi: 10.1002/phar.1209. [DOI] [PubMed] [Google Scholar]
- 9.Addyi (flibanserin) prescribing information. Raleigh, North Carolina: Sprout Pharmaceuticals, Inc.; Aug, 2015. [Google Scholar]
- 10.Stahl SM, Sommer B, Allers KA. Multi-functional pharmacology of flibanserin: possible mechanism of therapeutic action in hypoactive sexual desire disorder. J Sex Med. 2011;8(1):15–27. doi: 10.1111/j.1743-6109.2010.02032.x. [DOI] [PubMed] [Google Scholar]
- 11.Stahl SM. Mechanism of action of flibanserin, a multifunctional serotonin agonist and antagonist (MSAA), in hypoactive sexual desire disorder. CNS Spectr. 2015;20(1):1–6. doi: 10.1017/S1092852914000832. [DOI] [PubMed] [Google Scholar]
- 12.Stahl SM. Circuits of sexual desire in hypoactive sexual desire disorder. J Clin Psychiatry. 2010;71(5):518–519. doi: 10.4088/JCP.10bs06115whi. [DOI] [PubMed] [Google Scholar]
- 13.Pfaus JG. Pathways of sexual desire. J Sex Med. 2009;6(6):1506–1533. doi: 10.1111/j.1743-6109.2009.01309.x. [DOI] [PubMed] [Google Scholar]
- 14.Katz M, DeRogatis LR, Ackerman R, et al. Efficacy of flibanserin in women with hypoactive sexual desire disorder: results from the BEGONIA trial. J Sex Med. 2013;10(7):1807–1815. doi: 10.1111/jsm.12189. [DOI] [PubMed] [Google Scholar]
- 15.Thorp J, Simon J, Dattani D, et al. Treatment of hypoactive sexual desire disorder in premenopausal women: efficacy of flibanserin in the DAISY study. J Sex Med. 2012;9(3):793–804. doi: 10.1111/j.1743-6109.2011.02595.x. [DOI] [PubMed] [Google Scholar]
- 16.Derogatis LR, Komer L, Katz M, et al. Treatment of hypoactive sexual desire disorder in premenopausal women: efficacy of flibanserin in the VIOLET study. J Sex Med. 2012;9(4):1074–1085. doi: 10.1111/j.1743-6109.2011.02626.x. [DOI] [PubMed] [Google Scholar]
- 17.Food and Drug Administration. Summary review: application number 022526Orig1s000. Center for Drug Evaluation and Research; Aug 18, 2015. [Accessed October 25, 2015]. Available at: www.access-data.fda.gov/drugsatfda_docs/nda/2015/022526Orig1s000SumRedt.pdf. [Google Scholar]
- 18.Simon JA, Kingsberg SA, Shumel B, et al. Efficacy and safety of flibanserin in postmenopausal women with hypoactive sexual desire disorder: results of the SNOWDROP trial. Menopause. 2014;21(6):633–640. doi: 10.1097/GME.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 19.Borsini F, Brambilla A, Cesana R, Grippa N. Lack of interaction between flibanserin and antidepressants in inducing serotonergic syndrome in rats. Int J Neuropsychopharmacol. 2001;4(1):9–15. doi: 10.1017/S1461145701002206. [DOI] [PubMed] [Google Scholar]
- 20.Wright JJ, O’Connor KM. Female sexual dysfunction. Med Clin North Am. 2015;99(3):607–628. doi: 10.1016/j.mcna.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Red Book Online. Ann Arbor, Michigan: Truven Health Analytics; [Accessed February 2, 2017]. [Google Scholar]