Highlights
-
•
Eleven cases with a fracture of the anterior or anteromedial facet of the coronoid process were treated by coronoid fixation using a figure-eight suture loop.
-
•
All 11 fractures were united at final follow-up with no joint incongruity, dislocation, or subluxation of the injured elbow.
-
•
The figure-eight suture pattern technique is an easy and effective technique to fix anterior or anteromedial facet fractures of the coronoid process.
Keywords: Coronoid fractures, Elbow, Instability, Internal fixation
Abstract
Purpose
Sufficient fixation of an anterior or anteromedial facet fracture of the coronoid process in fracture-dislocation of elbow is important to maintain joint stability. The purpose of this study was to report our experience with 11 patients who were managed with an original fixation technique using a “figure-eight” suture loop.
Methods
From February 2010 to March 2011, 11 cases with a fracture of the anterior or anteromedial facet of the coronoid process were treated by coronoid fixation using a figure-eight suture loop. For cases with comminuted fractures, to prevent a suture from sliding into the fracture line, a 3- or 4-hole phalanx plate was enclosed in the suture loop to compress multiple fragments. Accompanying injuries, such as a radial head fracture or olecranon fracture, were fixed with repair of lateral collateral ligament injuries.
Results
On final evaluations at an average of 18 months after injury, the mean elbow arc of motion was 125.5° and the mean forearm rotation arc of 124.1°. All fractures were united with an average postoperative score according to the Mayo Elbow Performance Index of 91 points. All patients achieved satisfactory scores (seven excellent, four good). All 11 fractures were united at final follow-up with no joint incongruity, dislocation, or subluxation of the injured elbow.
Conclusions
The figure-eight suture loop technique is an easy and effective technique to fix anterior or anteromedial facet fractures of the coronoid process.
1. Introduction
The ulnar coronoid process is an anterior and medial extension of the proximal metaphysis, which is a critical structure to static elbow stability and plays an integral part in both the hinge and rotator components that function in trocho-ginglymus articulation of the elbow [1], [2]. Coronoid fractures are not usually isolated, but rather occur in more complex elbow trauma, such as the “terrible triad” injury, which involves posterolateral dislocation, radial head fracture, and fracture of the coronoid process. The importance of properly fixing coronoid fractures has been addressed in previous reports [3], [4], [5]. Inappropriate treatment of coronoid fractures will lead to a greater risk of a poor outcome, such as recurrent dislocation and instability. Because appropriate fixation is critical to good outcomes, different fixation methods have been established for different types of coronoid fractures, such as the suture lasso technique, Kirschner wire fixation, screw and plate fixation [6], the suture anchor technique [7], and the recently reported tension band wiring technique with steel wires [8]. However, each of these methods has features that may not be acceptable for all fractures. In this article, we report the use of a “figure-eight” suture loop and Kirschner wires to fix anterior and medial fragments of the coronoid process.
2. Patients and methods
This retrospective, single-center, non-consecutive, case series study of ulnar coronoid process fractures was approved by the Institutional Review Board of Shanghai Sixth People’s Hospital (approval no. 2015-KY-016 (K)) and performed in accordance with the PROCESS guidelines [9]. This work was registered at Research Registry (UIN: research registry 1769). From February 2010 to March 2011, 11 patients with a fracture of the ulnar coronoid process were treated by a single surgeon (JD) in the Orthopedic Department of Shanghai Sixth People’s Hospital. All patients were followed for a minimum of 1 year after surgery. At the emergency department, all fractures were evaluated by plain X-ray and three-dimensional computed tomography (CT). An orthopedic surgeon (JD) and a radiologist evaluated the radiographs to confirm the fracture classification according to the O’Driscoll classification system [10]. They also evaluated the fracture comminution by three-dimensional CT. Intraoperatively, the presence of a collateral ligament injury was confirmed by C-arm X-ray fluoroscopy.
2.1. Surgical technique
Under general anesthesia, the patient was placed in the supine position and the injured upper limb was placed on a radiolucent operating table. To expose the coronoid fracture, the elbow was approached through a medial incision and a medial skin flap was created. The ulnar nerve was identified and depressed proximally at the medial edge of the triceps and distally between the two heads of the flexor carpi ulnaris. Through an over-the-top exposure [11], a gap between the flexor-pronator muscles was developed by splitting the muscle mass. The anteromedial mass was elevated and reflected from the anterior part of the humerus and the elbow capsule. The brachialis was also reflected, more or less, depending on the size of the fracture fragments. The tip fragments and anteromedial fragments of the coronoid process were then clearly exposed.
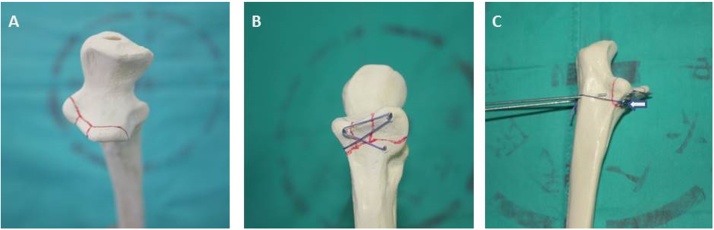
Direct reduction of the fragments was performed after first identifying the articular surface of the coronoid process by releasing part of the capsule and irrigating the area. In general, completing the reduction was not difficult. Two parallel Kirschner wires (1.5 mm) were used to fix the medial and lateral margins of the fragments in the anteroposterior direction, and then inserted into the ulna. By pulling the Kirschner wires from the dorsal side, no more than 3 mm of wire was left at the fixation site. At the distal end of the fragments, a 2-mm Kirschner wire was used to drill a hole in the anteroposterior direction on the lateral and medial side. A non-absorbable suture was then inserted into the hole on the dorsal side of the ulna. As is frequently done, a Keith needle was used to help pass the suture through the drill hole on the medial side of the ulna, just at the bottom of the sublime tubercle. For cases in which the edge of the fracture extended to the medial ulna, a hole was made only through the lateral side and the suture was directly passed through the medial side of the ulna. If the medial facet fragment was too small or thin to drill a hole, the suture was passed distally to the medial side of the ulna. A trocar inserted for lumbar puncture was placed closely to the bone to avoid ulnar nerve injury. In addition, the ulnar nerve was isolated distally until the first muscular branch. Then, the suture was passed by the two ends of the Kirschner wires to form a suture loop in the form of a figure-eight and then the suture was tightened and knotted on the dorsal side of the ulna. For cases with comminuted fractures, in order to avoid suture sliding into the fracture line, a 3- or 4-hole phalanx plate was enclosed in the suture loop to compress multiple fragments (Fig. 1). On the other hand, the suture plate also helped to extend the area under fixation. The ends of the Kirschner wires were bent and buried under the skin. Any accompanied fracture, such as a radial head fracture or olecranal fracture, were fixed with cannulated screws or plates. An anchor suture was used to repair injury to the lateral collateral ligament (LCL). For “terrible triad” injuries, an external fixator (Carewayer, Shanghai, China) was applied after fracture fixation and ligament repair, with the elbow at 90° flexion and forearm pronation.
Fig. 1.
Fracture model shows the “figure-eight” fixation method for repair of a coronoid fracture. (A) A type II coronoid fracture according to the O'Driscoll classification with anterior and medial fragments. (B) Two Kirschner wires and suture in a figure-eight pattern. (C) To prevent the sutures from sliding into the interfragmentary line, a small plate (white arrow) was looped in suture.
2.2. Postoperative care
Postoperatively, for “terrible triad” injuries, the external fixator was locked and the elbow was immobilized for 3–5 days. For injuries without external fixation, the elbow was immobilized using an adjustable orthosis (Össur Americas, Foothill Ranch, CA, USA) in 90° flexion and forearm pronation. On postoperative days 3–5, the external fixator or orthosis was unlocked and the patient performed passive range-of-motion exercises assisted by the healthy arm. As pain and swelling gradually subsided after one week, the patient was allowed to practice active elbow motion. However, abduction of the shoulder was strictly avoided [12]. The allowed range of active motion was gradually increased, so that the patient avoided extensive pain until the orthosis was removed. Patients received 100 mg of celecoxib (Celebrex; Pfizer, New York, NY, USA) twice daily for the first 3–4 weeks to prevent heterotopic ossification [13]. The external fixator and adjustable orthosis were removed at postoperative weeks 12 and 6, respectively.
2.3. Clinical evaluation
At the final follow-up, the elbow range of motion, including arc of motion (extension/flexion) and forearm rotation (pronation/supination), were measured with a goniometer by the author (JD) who performed all 11 surgeries. Radiographs were reviewed for signs of arthritis using the scale developed by Broberg and Morrey [10]. Postoperative score according to the Mayo Elbow Performance Index was evaluated at the final follow-up. A score of >90 was regarded as excellent, 75–89 as good, 60–74 as fair, and <60 as poor. Radiographic parameters of fracture union were recorded. The ability of each patient to return to work was recorded. The number of postoperative complications, including infection, neuropathy, joint incongruence, fracture nonunion, and implant failure, was tabulated.
3. Results
3.1. Demographic data of included patients
A total of 11 patients (one woman and 10 men; average age, 38.6 years) with elbow dislocation and anterior or anteriomedial coronoid fractures were included in this study. No patients were lost to follow-up. Of these 11 subjects, four had type I fractures and seven had type II fractures according to the O’Driscoll classification system [10] and all had LCL injuries. There were no open fractures. Three cases were combined with radial head fractures, which were fixed with cannulated screws. Two patients with “terrible triad” injuries underwent external fixation due to elbow instability. Osteosynthesis with plate and screw fixation was used for one patient to fix an olecranal fracture. For the four cases with comminuted fractures, contoured plates were enclosed in the suture loop, while fixation for the other seven cases was performed by placement of only figure-eight sutures without plates (Table 1).
Table 1.
Patient demographics. LCL: lateral collateral ligament.
| Patient no. | Gender | Age | Injuries | Surgical procedure | Final elbow arc of motion (extension/flexion) (°) | Final forearm rotation (pronation/supination) (°) | Mayo Elbow Performance Index |
|---|---|---|---|---|---|---|---|
| 1 | M | 24 | Coronoid fracture, elbow dislocation | “Figure 8 ” suture for coronoid, LCL repair, external fixation | 135 (115/20) | 120(65/55) | 85 |
| 2 | M | 31 | Varus posteromedial rotary instability | “Figure 8” suture plate for coronoid, LCL repair, | 130 (115/15) | 135(75/60) | 95 |
| 3 | M | 43 | Coronoid fracture, LUCL injury | “Figure 8” suture plate for coronoid, LCL repair | 120 (110/10) | 145(85/60) | 90 |
| 4 | F | 75 | Transolecranon fracture dislocation | “Figure 8” suture, LUCL repair, olecranon fixation with plate | 120 (90/30) | 150(85/65) | 95 |
| 5 | M | 38 | Terrible triad | “Figure 8” suture plate for coronoid, LCL and MCL repair, cannulated screw fixation for radial head | 125 (95/30) | 110 (55/55) | 85 |
| 6 | M | 29 | Coronoid fracture, LUCL injury | “Figure 8” suture plate for coronoid, LCL repair | 145 (130/15) | 140 (70/70) | 100 |
| 7 | M | 57 | Coronoid fracture, elbow dislocation | “Figure 8” suture for Coronoid, external fixation | 95 (65/35) | 95 (50/45) | 75 |
| 8 | M | 37 | Coronoid fracture, elbow dislocation | “Figure 8” suture plate for coronoid, LCL repair | 140 (125/15) | 130 (70/60) | 95 |
| 9 | M | 20 | Medial and lateral epicondyle avulsion, coronoid fracture, elbow dislocation | Cannulated screw fixation, Medial and lateral epicondyle avulsion, “Figure 8” suture for coronoid, LCL repair, external fixation | 125 (125/0) | 130 (70/60) | 100 |
| 10 | M | 43 | Coronoid fracture, elbow dislocation | Anchor suture failure and then “Figure 8” suture for coronoid, LCL repair, external fixation | 120 (85/35) | 110 (55/55) | 85 |
| 11 | M | 28 | Coronoid fracture, elbow dislocation | “Figure 8” suture for coronoid, LCL repair | 125 (95/35) | 100 (50/50) | 95 |
3.2. Clinical results
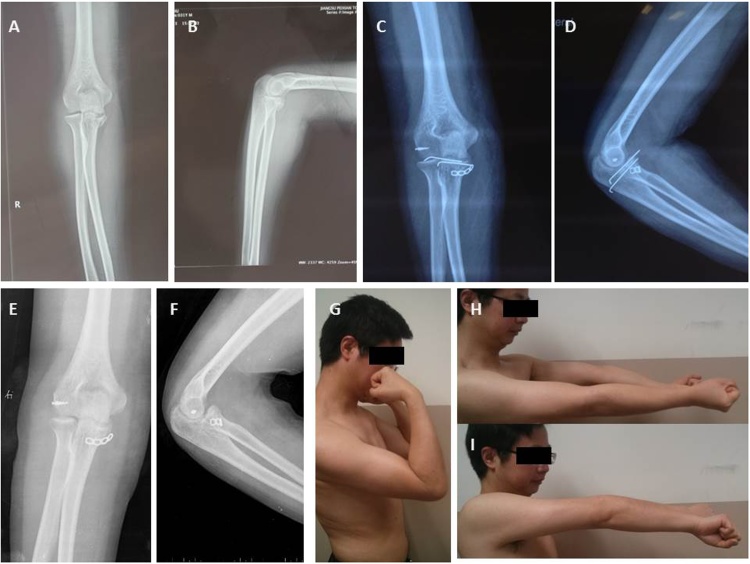
Of the 11 patients treated, the mean elbow arc of motion was 125.5° with a mean arc of extension of 104.5° and flexion of 21.8°. The mean forearm pronation was 66.4° and the mean supination was 57.7° with a mean forearm rotation arc of 124.1°. The average postoperative score according to the Mayo Elbow Performance Index was 91 points (range, 75–100 points) and all patients achieved satisfactory scores (seven excellent and four good). The elbow range of motion and Mayo Elbow Performance Index date are shown in Table 1. All 11 fractures were united by the time of the final follow-up and no joint incongruity, dislocation, or subluxation of the injured elbow was observed. All 11 patients who were employed at the time of injury returned to their original jobs. Two patients had small areas of heterotopic ossification on the final follow-up radiographs. One patient experienced transient paralysis of the ulnar nerve with reduced sensation in the hand associated with the distribution of the ulnar nerve, which recovered within 3 months. Additionally, one patient reported mild pain during repeated exertion and forceful use of the arm. None of the patients complained about elbow instability that required secondary surgery. No migration of the small contoured plates was observed in any of the four cases at final follow-up. No complications of infection, joint incongruency, fracture nonunion, or implant failure were reported. A typical case is shown in Fig. 2.
Fig. 2.
A 31-year-old man presented with a coronoid fracture and lateral collateral ligament (LCL) injury (A and B); The figure-eight fixation method with a 4-hole phalanx plate was used to fix the multiple fragments and an anchor suture was used to repair the LCL injury (C and D); Kirschner wires were removed after 6 months (E and D); good function was achieved at 2-year follow-up (G, H, and I).
4. Discussion
Because of the special anatomical and biomechanical features of the coronoid process, a fracture, especially combined with elbow dislocation, requires reliable fixation to allow for early rehabilitation. Otherwise, improper fixation may lead to elbow instability and poor outcomes. Even if such a fracture involves only 2.5 mm of the articular surface, it may increase internal rotation in the varus position when combined with avulsion of the lateral collateral ligament [14]. Although some fixation methods are appropriate for coronoid fractures, type II O’Driscoll fractures that involve the anterior and medial coronoid processes are still difficult to repair.
Each of the 11 patients included in our study had an LCL injury accompanied with an ulnar coronoid process fractures, which was similar to the cohort in the report by Park et al. [7]. Because such fractures have both anterior and medial fragments, the suture lasso technique and the Kirschner wire technique hardly provide sufficient fixation. The use of Kirschner wires alone is appropriate to fix articular fragments, but if distal fragments attached by a brachial muscle and the anterior band of the medial collateral ligament are present, they will be missed. In contrast, sutures alone cannot provide sufficient fixation for multifragment fractures, especially when the fragments are too thin to drill a hole through. For terrible triad injuries, coronoid fractures are usually Regan and Morrey type II coronoid fractures or type I O’Driscoll fractures [10]. For such tip fragments that are present on the anterior coronoid and attached to the anterior capsule, the suture lasso technique is generally recommended. Compared with this method, open reduction and internal fixation is associated with a greater risk of implant failure, while the use of suture anchors is associated with the threat of malunion and nonunion [15]. As for type II fractures, which are often related to varus posteromedial rotary instability, small fragments can be secured with a suture passed though the drilled holes. Coronoid plates are introduced to the majority of anteromedial facets with shearing fractures. This buttress plate can support and press larger fragments, and the small fragments can be simultaneously fixed with a suture [16], [17].
Compared with the buttress plate and suture technique, our experience using Kirschner wires and the figure-eight suture loop, with or without a plate, may induce less pressure on the anteromedial facet and our primary results indicate that this technique may also allow for early rehabilitation of the elbow. Our technique has its own advantages, as distal striping was not required for fixing the plate with distal screws, the brachial muscles were less interrupted, the figure-eight suture loop offered a greater area to apply pressure to multiple fragments, and the operative procedure was not complex. In addition, this procedure is relatively cheap and available to those with limited medical funds. The disadvantages of this method are as follows: a dorsal incision is required, a second surgery is needed to remove the subcutaneous ends of the Kirschner wires, and one patient complained of pain because the end of the Kirschner wire was too close to the olecranon. Consequently, the Kirschner wires should be placed from the anterior-proximal to the dorsal-distal direction of the ulna. Also, this method may be inappropriate to fix larger anteromedial fragments, such as with varus posteromedial rotary instability, which may require more buttressing support to protect against shearing [12]. As a result, cases with medial facet fragments in this series were advised to refrain from shoulder abduction for 6 weeks after surgery. Fortunately, rehabilitation was not negatively affected during this 6-week period.
Overall, these findings suggest that almost all LCL injuries were accompanied with anterior or anteromedial facet fractures. Fixation using a figure-eight suture loop is an easy and effective technique to fix anteromedial coronoid fractures.
Conflict of interest
The authors declare that they have no conflict of interests.
Funding
Funding was provided by the National Natural Science Foundation of China (81201440). http://www.nsfc.gov.cn/. This study was orally presented at the 37th SICOT Orthopedic World Congress, 2016, in Rome, Italy.
Ethical approval
This retrospective case series study of ulnar coronoid process fractures was approved by the Institutional Review Board of Shanghai Sixth People’s Hospital (approval no. 2015-KY-016 (K)).
Research registration Unique Identifying Number (UIN)
researchregistry1769.
Author contributions
Longxiang Shen; conceived and designed the study, analysed the data and wrote the paper.
Xingang Yu; analysed the data and wrote the paper.
Biao Zhong; analyzed the data and wrote the paper.
Jian Ding; conceived and designed the study, analysed the data and wrote the paper.
Guarantor
Jian Ding.
References
- 1.Pollock J.W., Pichora J., Brownhill J., Ferreira L.M., McDonald C.P. The influence of type II coronoid fractures, collateral ligament injuries, and surgical repair on the kinematics and stability of the elbow: an in vitro biomechanical study. J. Shoulder Elb. Surg. 2009;18:408–417. doi: 10.1016/j.jse.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Wells J., Ablove R.H. Coronoid fractures of the elbow. Clin. Med. Res. 2008;6:40–44. doi: 10.3121/cmr.2008.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Josefsson P.O., Gentz C.F., Johnell O., Wendeberg B. Dislocations of the elbow and intraarticular fractures. Clin. Orthop. Relat. 1989;Res:126–130. [PubMed] [Google Scholar]
- 4.Chemama B., Bonnevialle N., Peter O., Mansat P., Bonnevialle P. Terrible triad injury of the elbow: how to improve outcomes? Orthop. Traumatol. Surg. Res. 2010;96:147–154. doi: 10.1016/j.rcot.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 5.Sheehan S.E., Dyer G.S., Sodickson A.D., Patel K.I., Khurana B. Traumatic elbow injuries: what the orthopedic surgeon wants to know. Radiographics. 2013;33:869–888. doi: 10.1148/rg.333125176. [DOI] [PubMed] [Google Scholar]
- 6.Ring D., Horst T.A. Coronoid fractures. J. Orthop. Trauma. 2015;29:437–440. doi: 10.1097/BOT.0000000000000326. [DOI] [PubMed] [Google Scholar]
- 7.Park S.M., Lee J.S., Jung J.Y., Kim J.Y., Song K.S. How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O'Driscoll classification and ligament injury. J. Shoulder Elb. Surg. 2015;24:74–82. doi: 10.1016/j.jse.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 8.Mallard F., Hubert L., Steiger V., Cronier P. An original internal fixation technique by tension band wiring with steel wire in fractures of the coronoid process. Orthop. Traumatol. Surg. Res. 2015;101:S211–215. doi: 10.1016/j.otsr.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Fowler A.J., Rammohan S., Barai I., Orgill D.P., the PROCESS Group The PROCESS statement: preferred reporting of case series in surgery. Int. J. Surg. 2016;36:319–323. doi: 10.1016/j.ijsu.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 10.O'Driscoll S.W., Jupiter J.B., Cohen M.S., Ring D., McKee M.D. Difficult elbow fractures: pearls and pitfalls. Instructional Course Lect. 2003;52:113–134. [PubMed] [Google Scholar]
- 11.Hotchkiss R.N., Kasparyan G.N. The medial over the top approach to the elbow. Tech. Orthop. 2000;15:8. [Google Scholar]
- 12.Forthman C., Henket M., Ring D.C. Elbow dislocation with intra-articular fracture: the results of operative treatment without repair of the medial collateral ligament. J. Hand Surg. Am. 2007;32:1200–1209. doi: 10.1016/j.jhsa.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 13.Sun Y., Cai J., Li F., Liu S., Ruan H. The efficacy of celecoxib in preventing heterotopic ossification recurrence after open arthrolysis for post-traumatic elbow stiffness in adults. J. Shoulder Elb. Surg. 2015;24:1735–1740. doi: 10.1016/j.jse.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Pollock J.W., Brownhill J., Ferreira L., McDonald C.P., Johnson J. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J. Bone Jt. Surg. Am. 2009;91:1448–1458. doi: 10.2106/JBJS.H.00222. [DOI] [PubMed] [Google Scholar]
- 15.Garrigues G.E., Wray W.H., 3rd, Lindenhovius A.L., Ring D.C., Ruch D.S. Fixation of the coronoid process in elbow fracture-dislocations. J. Bone Jt. Surg. Am. 2011;93:1873–1881. doi: 10.2106/JBJS.I.01673. [DOI] [PubMed] [Google Scholar]
- 16.Ring D., Doornberg J.N. Fracture of the anteromedial facet of the coronoid process. Surgical technique. J Bone Jt. Surg. Am. 2007;89(Suppl. 2):267–283. doi: 10.2106/JBJS.G.00059. (Pt.2) [DOI] [PubMed] [Google Scholar]
- 17.Budoff J.E. Coronoid fractures. J. Hand Surg. Am. 2012;37:2418–2423. doi: 10.1016/j.jhsa.2012.09.002. [DOI] [PubMed] [Google Scholar]