Abstract
Football is currently the most popular sporting activity in the world. Multiple reports have shown that a high incidence of osteoarthritis is found in football players. Evidence clearly shows that traumatic injury significantly predisposes players for such pathophysiology. Injuries are frequent in amateur as well as professional football players, with knee and ankle accounting for the most severe injuries. Many professional athletes lose playing time due to injuries and many are forced into early retirement. Posttraumatic osteoarthritis is a common finding among ex-football players with numbers well above the normal population. Today’s surgical techniques are advanced and capable of restoring the joint to a certain extent. However, a restitution ad integrum is reached only in very rare cases. Professional football players that return to play after serious injuries perform their extremely strenuous activity on morphologically compromised joints. Incomplete rehabilitation and pressure to return to play after an injurious event clearly put the athlete at an even higher risk for joint degeneration. Prevention strategies, improved surgical management, strict rehabilitation, as well as future aspects such as early suppression of inflammation, personalized medicine, and predictive genomics DNA profiling are needed to reduce incidence and improve the health perspectives of football players.
Keywords: osteoarthritis, diagnosis, football, soccer, cartilage, knee, joint involved
Introduction
Football is the most popular sport in the world with over 300 million active players.1 There are more than 200,000 professional football players, with 80% of those being of male gender. Hundreds of thousands of games at all levels are organized and played each weekend. Football requires performance of dynamic, fast-paced tasks including running, jumping, dueling with the opponent, and dribbling with the ball. None of these activities are necessarily connected to the development of osteoarthritis (OA).2 However, the prevalence rate of OA among retired football players is well above that of the normal population.3,4 Most likely injuries predispose joints for development of early-onset OA within this collective population. The lower extremity is usually affected during football-related trauma,5 and there is a large body of literature reporting a correlation between posttraumatic OA of the knee joint and previous injury.6,7 The aim of this review is to give an overview of current mechanisms and pathophysiology resulting in such early degeneration. For greatest impact, this article will concentrate on the knee joint and its connection to football-related OA.
Football
Participation in sports is generally viewed as having great health benefits. Football, however, has undergone many changes over recent years. The physical demands on the athlete have increased and players are forced to perform close to their maximum capacity. National league games, international league competition, national team play, as well as charity games are an enormous physical and mental load for a player. The performance profile of each player or team can be influenced by constraints related to both biological and environmental factors. Football performance depends on a countless number of factors. The current and globally accepted index of physiological demands on players is represented by the total distance covered in a game. Typical activities during a football match are composed of running and jumping without the ball with repetitive acceleration, deceleration, as well as cutting maneuvers; dribbling with the ball; tackling; shooting of the ball; and duels with and without the ball. The actual physical activity is strongly dependent on player position, score, team strategy, level of performance, leg dominance, type of competition, player age and gender, fitness level, motivation, and finally joint anatomy.8 The major task during a football game can be defined by running, followed by kicking of the ball. The typical distribution of activity during a match is approximately 5% standing, 50% walking, 30% jogging, 7% running, 6% high-speed running, and finally 0.3% sprinting. Contact with the ball has been reported to occur in only 3% to 5% of playing time.9 Clemente and colleagues have closely analyzed the distance covered as well as activity profile of professional football players during the 2010 FIFA World Cup. Of the 443 players analyzed, there were 35 goalkeepers, 84 external defenders, 77 central defenders, 182 midfielders, and 65 forwards. While goalkeepers had the lowest distance covered/minute with 45.69 m/min per game, all the remaining player positions ran on average over 100 m/min per game (just over 10 km per game). Midfield players, in line with previous reports, covered the largest distance per game. The tactical positions of the players and their specific tasks, however, does significantly influence the activity profile and physical demands during a match.10 The activity of running without opponent contact and without existing risk factors has not been shown to be associated with a higher risk of OA.2,11,12 Indeed, the combination of improved muscle strength and proprioception, and reduced body mass index (BMI) have been even declared to be joint protective. Furthermore, articular cartilage can adapt to biomechanical loading.13 When such loading is lost, as described by Hinterwimmer and colleagues in a partial weight-bearing ankle-fracture model, the articular cartilage undergoes atrophy already after 7 weeks. This raises the question whether cartilage is mechanically less competent and particularly vulnerable after states of partial or complete immobilization.14 Among adult subjects there are no further significant changes in cartilage volume after strenuous activity. It has been shown using magnetic resonance imaging (MRI) that high-impact forces during long-distance running are well tolerated even in marathon beginners and do not lead to clinically relevant cartilage loss.15 In contrast, Arokoski showed softening of the lateral condyle articular cartilage in the canine knee joint after long distance (up to 40 km/day) running training lasting 1 year.16 Such data have not been reproduced among human subjects. In football, kicking is the main offensive action during the game, and the team with more kicks on target has the better chances to score and thus potentially win a game. The kicking motion is achieved by a combination of muscle moments and motion-dependent moments. Muscle moments are the result of high activation patterns of several muscles whereas some muscle activity serves to stabilize the involved joints and segments in order to achieve a fine coordinated movement.17 The football kick per se is linked to an only mildly elevated injury rate (5% of all injuries) according to the available evidence.5 Yet groin-associated pathology (sports hernia), which can be defined a classical football player problem or overuse injury, has been described to be connected to the typical football instep kick.18 The motion of kicking a ball has not been described to be associated with a higher risk of OA, while it has been proposed that the knee is somewhat susceptible to injury during kicking. It is presumably related to the fact that the player which is currently holding or trying to kick the ball will be attacked by at least one player of the opposing team. Such duels, played at maximum intensity, can be declared one of the or the most dangerous part of football, resulting in the majority of contact-related injuries.19
Injury
Animal and human studies have shown no evidence of increased risk of hip or knee OA with moderate exercise, and in the absence of traumatic injury, sporting activity has a protective effect. Engebretsen and coworkers have reported that football players do not necessarily carry an intrinsic increased risk for injury.20 However, element of sports-related contact and noncontact injury can be regarded as one major influencing factor when development of early OA among professional athletes is concerned. The injury rate among football players is clearly elevated over the normal population. The incidence of football-related injuries is estimated to be over 2 injuries per player/year or 10 to 42 injuries per 1,000 playing hours in adult male players.5,21-25 The injury rate is often higher among younger and less skilled players. Trauma-related injuries account for 80% of all injuries, while the rest is attributed to overuse injuries. But clearly it is speculation where one can truly differentiate between trauma and overuse injuries. Contact injuries (two thirds of the total) are more frequent when compared to noncontact injuries (one third of the total). Typically, contact injuries are related to foul play in one third of cases with a referee sanction in approximately two thirds of cases. Approximately 60% to 80% of severe injuries occur in the lower extremities, most commonly in the knee or ankle. There is a clear difference between male and female football-related injuries, with female football players having at least twice the risk of anterior cruciate ligament (ACL) and meniscus injury compared with their male counterparts. Males, on the other hand, are more likely to have groin-associated pathology such as sports hernia symptoms or hamstring injuries.26 In a current analysis of the 2014 FIFA World Cup in Brazil, Junge and Dvorak documented 1.6 injuries/match or 104 in total. Sixty-four (63.4%) injuries were caused by direct contact with another player. The injuries most frequently affected the lower extremity (68; 65.4%) followed by the head/neck (19; 18.3%), upper extremity (10; 9.6%), and the trunk (7; 6.7%). A total of 0.97 injuries per match did result in absence from training or match. Eight injuries were classified as severe with a resulting absence longer than 28 days. There were 12 knee joint injuries in total, 3 of which were declared as severe. The overall incidence of match injuries in the 2014 FIFA World Cup (1.6) was significantly lower (minus 37%) than the average of the 4 preceding FIFA World Cups, both for injuries (2.34) and time loss due to injuries.27
It should be noted that not every posttraumatic pathology is clearly existent directly after the incident. Selected athletes may continue to play despite symptoms following an injury. Direct or indirect trauma to the knee joint such as severe axial compression, distortion, or subluxation can result in the initial diagnostic finding of a sprain or bruise without morphological changes as seen on current imaging methods. Often ill-defined subchondral bone marrow signal intensities (bone marrow edema or lesion) occur in relation to such previous mechanical impact.28 In particular, within previously injured or surgically treated joints. In most cases such bone marrow lesions do heal spontaneously and without MRI would not even be detected. However, it has been shown that bone lesions can secondarily predispose cartilage to defect formation when the support of the subchondral bone is at least temporarily compromised.29 In this way bone marrow lesions can directly predispose football players to early-onset OA. In particular, nonresolving and chronically symptomatic lesions pose a significant problem to the treating physician and result in longer absences from play.30,31 Finally, a postinjury painful joint may result in less use of the joint, with associated secondary muscle atrophy and weakness. Quadriceps weakness occurs in both acute and chronic knee injury and has been shown to predate the symptoms of OA.32 It may further accelerate the process of degradation, due to reduced joint stability. Due to career considerations, peer pressure, and the lack of alternatives many football players continue training and competition despite pain and impaired functionality. During another analysis of the FIFA World Cups between 2002 and 2014, it was found that 69% of adult male players reported using medication, with more than half using nonsteroidal anti-inflammatory drugs (NSAIDs). Up to one third of all players used NSAIDs prior to every match, regardless of whether they played or not.33 In professional or elite athletes involved in contact sports, there is a higher incidence of significant joint injuries and a greater pressure to continue playing despite pain, potentially adding further insult to the joint. It has been reported that 47% of professional football players retire due to injury.
ACL, Meniscus, Cartilage, Lower Extremity Malalignment
The knee joint has a complex anatomy that allows 6 degrees of freedom movement. This flexibility in movement, however, renders the joint fundamentally more unstable, and stability is provided primarily by soft tissue. As in all diarthrodial joints, knee cartilage has a very limited healing capacity when morphological defects set in. This is particularly true at postpuberty since it has been shown that joint tissues of children and adolescents contain a greater intrinsic healing potential and regenerate better following biological surgery.34 Typical severe football injuries include rupture of the ACL ( Fig. 1 ), torn or displaced meniscus ( Fig. 2 ), cartilage defects ( Fig. 3 ), injury to the medial collateral ligament or combinations thereof. Highly frequent medial collateral ligament sprains or partial ruptures among football players are conservatively treated and only require surgical intervention in very select cases. No correlation or predisposition for early OA has been reported in these cases. The same however is not true for the highly frequent rupture of the ACL in active football players.35 Current evidence for ACL management has reported that post-ACL rupture OA will set in irrespective of whether the treatment is surgical or conservative.36,37 However, ACL reconstruction gives back joint stability among noncopers and appears to decrease the rates of subsequent meniscal and cartilage injuries in young healthy adults as well as in children and adolescents.38,39 Given that, ACL surgery may decrease the rate of posttraumatic OA.40 When ACL surgery is applied, current techniques can until today not completely restore the original functional anatomy ( Fig. 4 ). In particular, the natural large ACL footprints, complex bundle structure, biomechanical properties, and proprioception cannot be fully restored. Multiple techniques are available to the surgeon, though current evidence has not identified a gold standard that results in an optimal outcome for patients in general and for the professional football player in particular.41-44 Pain-free stability with full function are required to return the athlete to play. Not every subject does return to play while ACL surgery can be plagued by several and also severe complications.45 Ardern and colleagues have reported in a systematic review and meta-analysis of 69 articles with 7,556 participants following ACL replacement that on average 81% of subjects returned to any sport, 65% returned to their pre-injury level of sport, and 55% returned to competitive-level sport. It was further described that the contextual factors of younger age (d = −0.3), male gender (odds ratio [OR] = 1.4), playing elite sport (OR = 2.5), and having a positive psychological response (d = 0.3) favored return to pre-injury level sport. Receiving a hamstring tendon autograft favored returning to competitive level sport (OR = 2.4), whereas receiving a patellar tendon autograft favored returning to the preinjury level sport (OR = 1.2).46,47 Meniscus damage does frequently appear simultaneously with a rupture of the ACL, but as well as an isolated finding. Multiple rupture morphology patterns can occur, while in many cases the surgeon is significantly limited by the surgical options available. In general, meniscus surgery is a subject of medical and political debate.48 The poor intrinsic healing capacity is related to the limited blood supply as well as regionally different healing capacities of the meniscus.49 Often partial resection is the sole solution. Displaced tears such as bucket handle tears have been reported to rerupture in up to 25% of cases after surgery.50 Meniscal root tears confront the surgeon with a demanding pathology.51 In any case, loss of meniscus tissue is acknowledged to be a pre-arthritic condition since multiple functions are lost and the articular cartilage is subjected to an increased biomechanical exposure.52,53 Nawabi et al. have analyzed 92 football players of which 42 had a lateral meniscectomy and 48 had a medial meniscectomy. The median time to return to play was 7 (5-18) weeks for the lateral and 5 (3-6) weeks for the medial meniscectomies. At all time points after surgery, the cumulative probability of returning to play was 5.99 times greater after medial meniscectomy. Lateral meniscectomy cases showed higher adverse events related to pain/swelling (−29 [69%] vs. 4 [8%]; P < 0.001) and more often required a second arthroscopy (3 [7%] vs. 0). Lateral meniscectomy is also associated with a significantly lower rate of return to play.54 In selected cases of severe meniscal tissue loss, meniscal substitute ( Fig. 5 ) allografts can be implanted to restore anatomical joint function. Marcacci and colleagues have reported a 75% return to play rate among professional football players following such procedures.55
Figure 1.
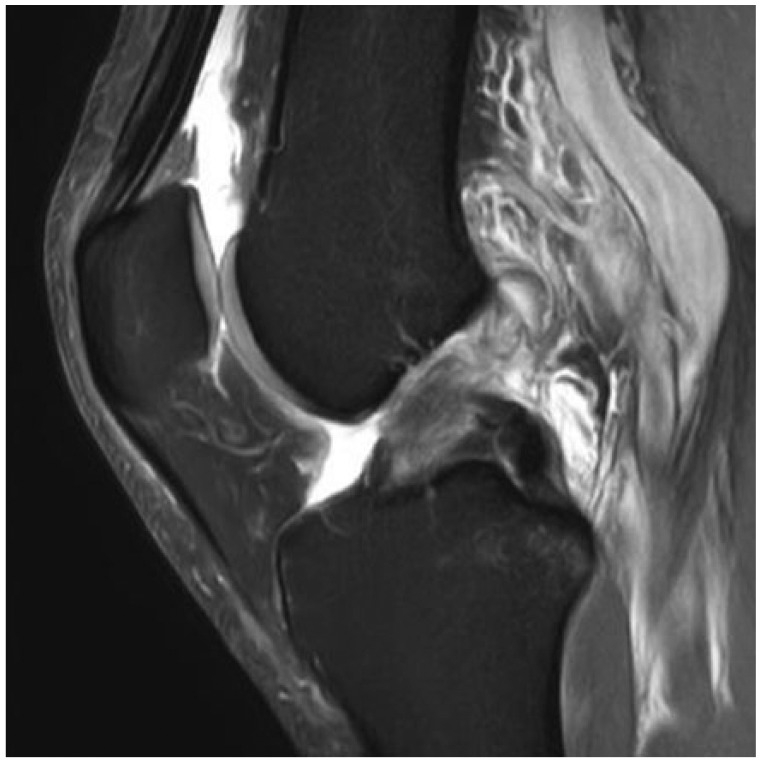
T2-weighted sagittal image illustrating fresh and complete anterior cruciate ligament rupture with typical bone marrow edema at the posterior tibia plateau.
Figure 2.

Intraoperative arthroscopic image constituting a radial split tear at the dorsolateral meniscus mostly in the white zone peripheral from the meniscus root. According to the West classification, grade 1 lesion is indicated for partial resection.
Figure 3.

Intraoperative arthroscopic image in display of severe cartilage defect at the medial femoral condyle, which is grade 3 and thus indicated for repair.
Figure 4.

T2-weighted sagittal image illustrating 6-month postoperative anterior cruciate ligament reconstruction using autologous hamstring tendons and interference screw fixation.
Figure 5.

Intraoperative arthroscopic image depicting meniscus substitute sewed to meniscus remnants in order to replace previously partially resected lateral meniscus pars intermedia.
Cartilage damage is the typical pathological progressive outcome of meniscal tissue loss and/or chronic ACL deficiency.56 Cartilage defects represent a dramatic health risk for professional football players.57 The prevalence of defective cartilage as seen during routine arthroscopy is alarmingly high.58 Flanigan and coworkers in 2010 reported, in an analysis of 931 athletes, a cartilage defect prevalence rate of 36%, which is much higher than that of the normal population (16%).59 Cartilage defects of postpuberty patients do not heal and instead undergo a pathological progression, which commonly results in an increased size of the lesion and an increase in clinical symptoms, though outcome varies from patient to patient.60,61 Currently, multiple surgical options are available to the treating surgeon with conflicting scientific and clinical evidence.62-65 Novel products are pushed on the market and seem to disappear as quickly when there is no clear superiority over standard microfracturing.66 Autologous chondrocyte implantation (ACI) ( Fig. 6 ) is regarded as standard of care for treatment of large-diameter cartilage defects.67 Mithoefer and coworkers have reported 72% good to excellent results with significant overall improvement of knee function and activity scores following ACI among professional football players. The return to play was 83% in competitive players but lower in recreational players. Return to sport was better for younger, competitive players with shorter intervals between injury and ACI.68 ACI long-term data, however, could not demonstrate a halt of whole knee joint degeneration with incomplete recovery with regard to clinical and morphological outcome.69-71 Yet no study to date has compared untreated and surgically treated cartilage defects with midterm or long-term follow-up.
Figure 6.

Intraoperative image showing third-generation autologous chondrocyte implantation product in place to cover trochlear cartilage defect.
The role of joint anatomy in OA predisposition is controversial. It is hypothesized that particularly varus malalignment is a frequent entity among football players.72 Yet Thijs and colleagues have reported that practicing load bearing sports in general is associated with the same knee varus alignment in adolescent boys as previously has been indicated in intense football-playing adolescents.73 Sauerschnig and coworkers have shown by use of quantitative imaging that leg malalignment is not associated with an abnormal cartilage signal within the overloaded compartment in adult active subjects.74 However, frontal plane knee mechanical axis malalignment is considered as an independent risk factor for the progression of OA.75
Any severe knee joint structural pathology does clearly predispose the patient for early OA. It is likely that optimal surgical technique, material and time point, joint circumstances such as stability and alignment, rehabilitation, and compliance will postpone and/or reduce the impound OA rate—an arrest will never set in. Spahn and coworkers have analyzed the relative risk (odds ratio) of posttraumatic OA among certain knee joint injuries in a 2011 meta-analysis. The relative risk of posttraumatic OA following ACL rupture has been reported to be increased 2.5 times, following meniscus rupture 1.8 times and 4.4 times when these pathologies appeared at the same time.76
Osteoarthritis
Osteoarthritis is a slowly developing chronic disease with multifactorial origin and is the most common joint disease in the world. OA generally affects single organs (i.e., knee joint) with damaged cartilage and synovial inflammation being hallmark characteristics.77 The current worldwide prevalence has been reported to be as high as 27%, with more patients suffering in the developed countries. Up to 50% of those over 65 years of age are affected, whereof 80% are limited in natural movement. Against the fact of the significant socioeconomic impact, until today, the complete etiology is unknown. OA remains incurable and treatment for advanced stage OA is restricted to management of its symptoms. Theories for such pathogenesis are the classical wear and tear theory (the more strain a joint is exposed to the more it will wear down).78 Recent evidence suggests a strong inflammatory component. In either case, a healthy joint <40 years of age is not the subject of pathologic wear,11,12 a fact that is also true for the typical professional football player. On the contrary, certain professions have been accepted as an occupational illness to predispose for early OA. To kneel for many thousands of hours in one’s profession is an accepted occupational risk for early-onset OA with an increased relative risk of up to 13.0 times higher when comparing to the normal collective.79 Currently, the molecular pathophysiologic etiologies for primary OA are chondrocyte senescence, a reduced sensitivity to growth factors during repair processes, mitochondrial dysfunction, and increased oxidative stress. These processes can result in articular cartilage degradation due to activity of catabolic and pro-inflammatory proteins. Finally fragmentation of the cartilage extracellular matrix and resultant fissuring with potential breakdown of the articular surface can occur.80 Also, an acute injury results in an immediate imbalance of the intraarticular joint homeostasis, which delineates a disadvantageous condition for the joint potentially initiating long-term sequelae.81-83 A solitary hemarthrosis clearly circumscribes a pathological intraarticular condition, as it has been previously described in a dog model where 2 acute joint bleeds lead to prolonged cartilage damage independent of the level of synovial inflammation.84 The majority of knee joint injuries do finally result in OA with a strong heterogeneity in initiation time point and expression. The Clearwater Osteoarthritis Study has reported in a prospective cohort with a sample size of 1.436 subjects that any history of knee injury is associated with a 7.4 times higher likelihood to develop knee OA compared to those individuals who did not have a history of knee injury.85 Multiple factors do play a role in such processes. One can distinguish between early and late onset, as well as primary and secondary OA. Primary OA has also been described as idiopathic since the etiology is unknown. Yet advanced age and female gender have been declared the 2 major risk factors, in particular in postmenopausal women. Degeneration is a physiological process that affects the whole human body. The joints, mostly those that are subjected to advanced biomechanical impact (lower extremities), are consequently as well affected by such degeneration processes.
Genetics in OA
Although the multifactorial nature of OA is well recognized, genetic factors have been found to be strong determinants of this disease. Evidence of a genetic influence of OA comes from a number of sources, including epidemiological studies of family history and family clustering, adoption studies, twin studies, and exploration of rare genetic disorders related to OA, such as chondrodysplasias. A certain genetic predisposition increases the risk for primary and/or early OA development. Genome-wide linkage analyses have identified selected chromosomal loci that are associated with a significantly elevated predisposition for primary OA—osteoarthritis susceptibility genes. Siblings of patients undergoing hip and knee replacement surgery have a 2 to 3 times increased risk of OA with the heritability rate of severe OA of 27%.86 Identified genes that contribute to the prevalence and progression of the disease include those which belong to the bone morphogenetic protein (BMP) and the wingless-type (WNT) signaling pathways. Most often it will not be one defective gene that results in OA, but a combination of genetic disposition and environmental factors. To date, the lack of a clear genetic linkage for most families suggests a multifactorial etiology with primary OA in rare cases without evidence of direct linkage. Along this line, predictive genomic DNA profiling has been declared a measure for sports performance. It can be used to aid in sport selection and elaboration of personalized training and nutrition programs. It does not detect or determine superior athletic performance, but can predict abilities and weaknesses associated with sports performance, and detect low penetrance sequence variation not proven to be causative, but probably contributing, in a cumulative fashion, to the relevant phenotypic manifestations. However, gene therapy, as it has clearly proven to be effective in vitro and in vivo,87,88 will probably never reach clinical application for treatment of non–life-threatening diseases.
Risk Factors for OA
Other unmodifiable risk factors for idiopathic OA are ethnic origin, with subjects of Caucasian origin being at an elevated risk. Vitamin D deficiency or supplementation was not shown to be of effect as shown in a randomized controlled trial by Jin and coworkers. Among patients with symptomatic knee OA and low serum 25-hydroxyvitamin D levels, vitamin D supplementation, compared with placebo, did not result in significant differences in change in MRI-measured tibial cartilage volume or Western Ontario and McMaster Universities Arthritis Index (WOMAC) knee pain score over 2 years. The authors concluded that the findings were not in support of the use of vitamin D supplementation for preventing tibial cartilage loss or improving WOMAC knee pain in patients with knee OA.89 The most important exogenous risk factors for developing secondary OA are injury-related macrotrauma (e.g., meniscus root tear),6 repetitive microtrauma (e.g., ACL deficiency), increased BMI, previous surgery, and certain lifestyle factors such as smoking and alcohol abuse.90 It is clear that among the reported risk factors macrotrauma and repetitive microtrauma do represent the most important ones in football. Microtrauma can occur for example in ACL-deficient knee joints, or as overload within meniscus-deficient knee joints. Whittaker and coworkers examined the association between sport-related knee injury and outcomes related to development of OA 3 to 10 years postinjury in one hundred 15 to 26 year olds, where 50 had a history of previous injury and 50 age- and sex-matched cohorts did not. The outcome measures were Knee Injury and Osteoarthritis Outcome Score (KOOS), BMI, hip abductor/adductor and knee extensor/flexor strength, estimated aerobic capacity (VO2max), and performance scores on 3 dynamic balance tests. Injured participants demonstrated poorer KOOS outcomes, quality of life, and sport/recreation levels. The injured were 3.75 times more likely to be overweight/obese and had lower triple single leg hop scores compared to controls.
OA among Retired Football Players
The OA prevalence among retired football players has been reported to be well above the normal population. Kuijt et al. have found in a systematic review a prevalence rate of knee OA between 60% and 80% among a collective of retired football players. Arliani and coworkers directly compared 27 former male professional football players and 30 male volunteers from different nonsporting professions using MRI (both knee joints) and clinical analysis. Both cohorts had no previous surgery. Both the clinical and magnetic resonance evaluations and the group comparisons performed in this study revealed that former football players have a worse quality of life than that of a control group with regard to physical aspects related to the knee; these aspects include greater pain, increased symptoms, and substantial changes in radiographic and magnetic resonance images of the knee.4 This evidence has been reported by numerous previous authors as well.3-5,91-98
Football and OA
It has been a matter of debate if playing football necessarily results in unphysiological OA development. Consequently, Spahn and coworkers in 2015 analyzed if the sporting activity of football without injury is linked to a significantly increased risk for the development of OA. One major aim was to answer the question if football can be declared as an occupational illness. For that a total 4.649 papers underwent a “Title-Abstract-Review” and finally 6 publications were included for the subsequent systematic review and meta-analysis. It was found that football players without injury have an only very slightly increased risk for knee OA: relative risk 1.3 (95% confidence interval = 1.0-1.7). The authors concluded that football should not be regarded as an occupational illness for OA development. In contrast, among studies without differentiation between injured and noninjured knees, the relative risk for OA was significantly increased: 2.9 (95% confidence interval = 2.0-4.1).99 Consequently, exogenous, contact-related trauma to the lower extremity with potential surgical consequences can be declared as the major predisposing factor for the generation of early OA among football players. Not every injury results in a clear morphological pathology. Sprains, contusions, and bruises occur with high frequency in every football match. It is hypothesized that any biomechanical impact to the joint above a certain individual threshold might have an initially silent and invisible impact on the joint, yet causing damage on a molecular level.100 The athlete will remain asymptomatic and continue the sporting activity, but is unwittingly prone to early OA when ageing. If such biomechanical joint impact is being paired with a significant morphological pathology such as an ACL rupture and surgery will be commenced to repair the torn ligament, chances of developing OA are multiplied.101
Conclusion
The sport of football does not predispose players for early-onset OA, when there is no injury, the players are healthy and less 40 years of age, and when no risk factors or genetic predisposition exists. Football has undergone many changes over recent years with constantly increasing physical demands placed on the players. The characteristics of football are strongly connected to a significantly increased risk of injury compared to the normal population. In particular, trauma-related injury to the lower extremities such as knee and ankle predispose players to early-onset OA, often with consecutive requirement for surgical treatment to restore joint anatomy and kinematics. The trauma to the joint itself induces several molecular pathologic cascades with the physiological internal aim to rest and repair (inflammation). The inherent well-balanced intraarticular homeostasis of a healthy joint is altered.102 Potentially irreversible anti-autoimmune processes are initiated, and once started are difficult to abort. It is speculated today that such initial incidence represents a major risk factor for secondary OA at a certain interval following the trauma. Furthermore, our current operative methods to address existing joint defects are imperfect and do not restore the joint ad integrum. Return to play is significantly limited.103 The players that do return to full competition are (declared) posttraumatic, which is a highly significant predisposition for early OA. A possible postoperative status is increasing such risk related to a nonnormal joint. Rehabilitation with continued muscle imbalance or decreased proprioception may be incomplete. Continuation of strenuous activity such as professional football performance exposes the joint to an unphysiological load/overload. Potential symptoms are initially absent, neglected, or suppressed by the use of medication.33 Peer pressure on the football player often has no further beneficial effects on perfect pain/injury management. Playing with fatigue, previous injury, or muscle imbalance predisposes players to overuse, re-injury, and thus early OA.32,104,105 In order to decrease the probability of injury and early OA among football players, prevention programs such as the FIFA 11+ have been introduced. These have been clearly shown to significantly reduce the injury rate among football players.106 More strict refereeing as well as fair play have been shown to be effective as well. Future methods may more effectively treat joint inflammation by addressing early time points in order to shorten the timely interval of such negative exposure. Personalized medicine with aid of biomarkers may support such management.107,108 Certainly, improved surgical methods to better restore joint anatomy close to integrum are required. And finally rehabilitation protocols need to be improved with room for player to player individualization and functional/morphological monitoring.
Footnotes
Acknowledgments and Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: This article does not require ethical approval.
References
- 1. Dvorak J, Graf-Baumann T, Peterson L, Junge A. Football, or soccer, as it is called in North America, is the most popular sport worldwide. Am J Sports Med. 2000;28:S1-S2. [PubMed] [Google Scholar]
- 2. Gantz S, Schindel R, Schneider S, Schiltenwolf M, Bolm-Audorff U, Eberth F, et al. Laufsport-Führt Laufsport zu vorzeitigen degenerativen Veränderungen am Kniegelenk? Trauma Berufskrankh. 2012;14:446-51. doi: 10.1007/s10039-012-1873-x. [DOI] [Google Scholar]
- 3. Anderson CL. High rate of osteoarthritis of the knee in former soccer players. Med Sci Sports Exerc. 1986;18:141. [PubMed] [Google Scholar]
- 4. Arliani GG, Astur DC, Yamada RK, Yamada AF, Miyashita GK, Mandelbaum B, et al. Early osteoarthritis and reduced quality of life after retirement in former professional soccer players. Clinics. 2014;69:589-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wong P, Hong Y. Soccer injury in the lower extremities. Br J Sports Med. 2005;39:473-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thelin N, Holmberg S, Thelin A. Knee injuries account for the sports-related increased risk of knee osteoarthritis. Scand J Med Sci Sports. 2006;16:329-33. [DOI] [PubMed] [Google Scholar]
- 7. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756-69. [DOI] [PubMed] [Google Scholar]
- 8. Goncalves BV, Figueira BE, Macas V, Sampaio J. Effect of player position on movement behaviour, physical and physiological performances during an 11-a-side football game. J Sports Sci. 2014;32:191-9. [DOI] [PubMed] [Google Scholar]
- 9. Di Salvo V, Baron R, Gonzalez-Haro C, Gormasz C, Pigozzi F, Bachl N. Sprinting analysis of elite soccer players during European Champions League and UEFA Cup matches. J Sports Sci. 2010;28:1489-94. [DOI] [PubMed] [Google Scholar]
- 10. Clemente FM, Couceiro MS, Martins FM, Ivanova MO, Mendes R. Activity profiles of soccer players during the 2010 world cup. J Hum Kinet. 2013;38:201-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Panush RS, Hanson CS, Caldwell JR, Longley S, Stork J, Thoburn R. Is running associated with osteoarthritis? An eight-year follow-up study. J Clin Rheumatol. 1995;1:35-9. [DOI] [PubMed] [Google Scholar]
- 12. Chakravarty EF, Hubert HB, Lingala VB, Zatarain E, Fries JF. Long distance running and knee osteoarthritis. A prospective study. Am J Prev Med. 2008;35:133-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jones G, Bennell K, Cicuttini FM. Effect of physical activity on cartilage development in healthy kids. Br J Sports Med. 2003;37:382-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hinterwimmer S, Krammer M, Krotz M, Glaser C, Baumgart R, Reiser M, et al. Cartilage atrophy in the knees of patients after seven weeks of partial load bearing. Arthritis Rheum. 2004;50:2516-20. [DOI] [PubMed] [Google Scholar]
- 15. Hinterwimmer S, Feucht MJ, Steinbrech C, Graichen H, von Eisenhart-Rothe R. The effect of a six-month training program followed by a marathon run on knee joint cartilage volume and thickness in marathon beginners. Knee Surg Sports Traumatol Arthrosc. 2014;22:1353-9. [DOI] [PubMed] [Google Scholar]
- 16. Arokoski J, Jurvelin J, Kiviranta I, Tammi M, Helminen HJ. Softening of the lateral condyle articular cartilage in the canine knee joint after long distance (up to 40 km/day) running training lasting one year. Int J Sports Med. 1994;15:254-60. [DOI] [PubMed] [Google Scholar]
- 17. Lees A, Asai T, Andersen TB, Nunome H, Sterzing T. The biomechanics of kicking in soccer: a review. J Sports Sci. 2010;28:805-17. [DOI] [PubMed] [Google Scholar]
- 18. Brophy RH, Backus S, Kraszewski AP, Steele BC, Ma Y, Osei D, et al. Differences between sexes in lower extremity alignment and muscle activation during soccer kick. J Bone Joint Surg Am. 2010;92:2050-8. [DOI] [PubMed] [Google Scholar]
- 19. Ryynanen J, Junge A, Dvorak J, Peterson L, Kautiainen H, Karlsson J, et al. Foul play is associated with injury incidence: an epidemiological study of three FIFA World Cups (2002-2010). Br J Sports Med. 2013;47:986-91. [DOI] [PubMed] [Google Scholar]
- 20. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for acute knee injuries among male football players: a prospective cohort study. Scand J Med Sci Sports. 2011;21:645-52. [DOI] [PubMed] [Google Scholar]
- 21. Hammes D, Aus Der Funten K, Kaiser S, Frisen E, Dvorak J, Meyer T. Injuries of veteran football (soccer) players in Germany. Res Sports Med. 2015;23:215-26. [DOI] [PubMed] [Google Scholar]
- 22. Faude O, Junge A, Kindermann W, Dvorak J. Risk factors for injuries in elite female soccer players. Br J Sports Med. 2006;40:785-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Faude O, Junge A, Kindermann W, Dvorak J. Injuries in female soccer players: a prospective study in the German national league. Am J Sports Med. 2005;33:1694-700. [DOI] [PubMed] [Google Scholar]
- 24. Junge A, Dvorak J. Soccer injuries: a review on incidence and prevention. Sports Med. 2004;34:929-38. [DOI] [PubMed] [Google Scholar]
- 25. Junge A, Cheung K, Edwards T, Dvorak J. Injuries in youth amateur soccer and rugby players–comparison of incidence and characteristics. Br J Sports Med. 2004;38:168-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Junge A, Grimm K, Feddermann N, Dvorak J. Precompetition orthopedic assessment of international elite football players. Clin J Sport Med. 2009;19:326-8. [DOI] [PubMed] [Google Scholar]
- 27. Junge A, Dvorak J. Football injuries during the 2014 FIFA World Cup. Br J Sports Med. 2015;49:599-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Roemer FW, Frobell R, Hunter DJ, Crema MD, Fischer W, Bohndorf K, et al. MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthritis Cartilage. 2009;17:1115-31. [DOI] [PubMed] [Google Scholar]
- 29. Mrosek EH, Lahm A, Erggelet C, Uhl M, Kurz H, Eissner B, et al. Subchondral bone trauma causes cartilage matrix degeneration: an immunohistochemical analysis in a canine model. Osteoarthritis Cartilage. 2006;14:171-8. [DOI] [PubMed] [Google Scholar]
- 30. Simon MJ, Barvencik F, Luttke M, Amling M, Mueller-Wohlfahrt HW, Ueblacker P. Intravenous bisphosphonates and vitamin D in the treatment of bone marrow oedema in professional athletes. Injury. 2014;45:981-7. [DOI] [PubMed] [Google Scholar]
- 31. Soder RB, Simoes JD, Soder JB, Baldisserotto M. MRI of the knee joint in asymptomatic adolescent soccer players: a controlled study. AJR Am J Roentgenol. 2011;196:W61-5. [DOI] [PubMed] [Google Scholar]
- 32. Oiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:171-7. [DOI] [PubMed] [Google Scholar]
- 33. Tscholl PM, Vaso M, Weber A, Dvorak J. High prevalence of medication use in professional football tournaments including the World Cups between 2002 and 2014: a narrative review with a focus on NSAIDs. Br J Sports Med. 2015;49:580-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Salzmann GM, Sah BR, Schmal H, Niemeyer P, Sudkamp NP. Microfracture for treatment of knee cartilage defects in children and adolescents. Pediatr Rep. 2012;4:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among U.S. high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45:462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Delince P, Ghafil D. Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc. 2012;20:48-61. [DOI] [PubMed] [Google Scholar]
- 37. Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42:1049-57. [DOI] [PubMed] [Google Scholar]
- 38. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:275-81. [DOI] [PubMed] [Google Scholar]
- 39. Kennedy J, Jackson MP, O’Kelly P, Moran R. Timing of reconstruction of the anterior cruciate ligament in athletes and the incidence of secondary pathology within the knee. J Bone Joint Surg Br. 2010;92:362-6. [DOI] [PubMed] [Google Scholar]
- 40. Karahan M. Role of anterior cruciate ligament reconstruction in preventing osteoarthritis. Arthroscopy. 2012;28:1750. [DOI] [PubMed] [Google Scholar]
- 41. Mascarenhas R, Cvetanovich GL, Sayegh ET, Verma NN, Cole BJ, Bush-Joseph C, et al. Does double-bundle anterior cruciate ligament reconstruction improve postoperative knee stability compared with single-bundle techniques? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:1185-96. [DOI] [PubMed] [Google Scholar]
- 42. Mascarenhas R, Erickson BJ, Sayegh ET, Verma NN, Cole BJ, Bush-Joseph C, et al. Is there a higher failure rate of allografts compared with autografts in anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:364-72. [DOI] [PubMed] [Google Scholar]
- 43. Mascarenhas R, Saltzman BM, Sayegh ET, Verma NN, Cole BJ, Bush-Joseph C, et al. Bioabsorbable versus metallic interference screws in anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:561-8. [DOI] [PubMed] [Google Scholar]
- 44. Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22:100-10. [DOI] [PubMed] [Google Scholar]
- 45. Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish Registry for Knee Ligament Reconstructions. Am J Sports Med. 2012;40:1551-7. [DOI] [PubMed] [Google Scholar]
- 46. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543-52. [DOI] [PubMed] [Google Scholar]
- 47. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596-606. [DOI] [PubMed] [Google Scholar]
- 48. Khan M, Evaniew N, Bedi A, Ayeni OR, Bhandari M. Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ. 2014;186:1057-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011;32:7411-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Espejo-Reina A, Serrano-Fernandez JM, Martin-Castilla B, Estades-Rubio FJ, Briggs KK, Espejo-Baena A. Outcomes after repair of chronic bucket-handle tears of medial meniscus. Arthroscopy. 2014;30:492-6. [DOI] [PubMed] [Google Scholar]
- 51. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42:3016-30. [DOI] [PubMed] [Google Scholar]
- 52. Freutel M, Seitz AM, Ignatius A, Durselen L. Influence of partial meniscectomy on attachment forces, superficial strain and contact mechanics in porcine knee joints. Knee Surg Sports Traumatol Arthrosc. 2015;23:74-82. [DOI] [PubMed] [Google Scholar]
- 53. Papalia R, Del Buono A, Osti L, Denaro V, Maffulli N. Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull. 2011;99:89-106. [DOI] [PubMed] [Google Scholar]
- 54. Nawabi DH, Cro S, Hamid IP, Williams A. Return to play after lateral meniscectomy compared with medial meniscectomy in elite professional soccer players. Am J Sports Med. 2014;42:2193-8. [DOI] [PubMed] [Google Scholar]
- 55. Marcacci M, Marcheggiani Muccioli GM, Grassi A, Ricci M, Tsapralis K, Nanni G, et al. Arthroscopic meniscus allograft transplantation in male professional soccer players: a 36-month follow-up study. Am J Sports Med. 2014;42:382-8. [DOI] [PubMed] [Google Scholar]
- 56. Van Ginckel A, Verdonk P, Victor J, Witvrouw E. Cartilage status in relation to return to sports after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:550-9. [DOI] [PubMed] [Google Scholar]
- 57. Mithoefer K, Peterson L, Zenobi-Wong M, Mandelbaum BR. Cartilage issues in football-today’s problems and tomorrow’s solutions. Br J Sports Med. 2015;49:590-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Widuchowski W, Widuchowski J, Trzaska T. Articular cartilage defects: study of 25,124 knee arthroscopies. Knee. 2007;14:177-82. [DOI] [PubMed] [Google Scholar]
- 59. Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH. Prevalence of chondral defects in athletes’ knees: a systematic review. Med Sci Sports Exerc. 2010;42:1795-801. [DOI] [PubMed] [Google Scholar]
- 60. Buckwalter JA. Articular cartilage injuries. Clin Orthop Relat Res. 2002;(402):21-37. [DOI] [PubMed] [Google Scholar]
- 61. Buckwalter JA, Mankin HJ, Grodzinsky AJ. Articular cartilage and osteoarthritis. Instr Course Lect. 2005;54:465-80. [PubMed] [Google Scholar]
- 62. Kon E, Roffi A, Filardo G, Tesei G, Marcacci M. Scaffold-based cartilage treatments: with or without cells? A systematic review of preclinical and clinical evidence. Arthroscopy. 2015;31:767-75. [DOI] [PubMed] [Google Scholar]
- 63. Oussedik S, Tsitskaris K, Parker D. Treatment of articular cartilage lesions of the knee by microfracture or autologous chondrocyte implantation: a systematic review. Arthroscopy. 2015;31:732-44. [DOI] [PubMed] [Google Scholar]
- 64. Hunziker EB, Lippuner K, Keel MJ, Shintani N. An educational review of cartilage repair: precepts & practice—myths & misconceptions—progress & prospects. Osteoarthritis Cartilage. 2015;23:334-50. [DOI] [PubMed] [Google Scholar]
- 65. Li Z, Zhu T, Fan W. Osteochondral autograft transplantation or autologous chondrocyte implantation for large cartilage defects of the knee: a meta-analysis. Cell Tissue Bank. 2016;17:59-67. [DOI] [PubMed] [Google Scholar]
- 66. Shive MS, Stanish WD, McCormack R, Forriol F, Mohtadi N, Pelet S, et al. BST-CarGel(R) treatment maintains cartilage repair superiority over microfracture at 5 years in a multicenter randomized controlled trial. Cartilage. 2015;6:62-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Niemeyer P, Andereya S, Angele P, Ateschrang A, Aurich M, Baumann M, et al. Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: a guideline by the working group “Tissue Regeneration” of the German Society of Orthopaedic Surgery and Traumatology (DGOU). Z Orthop Unfall. 2013;151:38-47. [DOI] [PubMed] [Google Scholar]
- 68. Mithoefer K, Peterson L, Saris DB, Mandelbaum BR. Evolution and current role of autologous chondrocyte implantation for treatment of articular cartilage defects in the football (soccer) player. Cartilage. 2012;3:31S-36S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Niemeyer P, Porichis S, Steinwachs M, Erggelet C, Kreuz PC, Schmal H, et al. Long-term outcomes after first-generation autologous chondrocyte implantation for cartilage defects of the knee. Am J Sports Med. 2014;42:150-7. [DOI] [PubMed] [Google Scholar]
- 70. Salzmann GM, Erdle B, Porichis S, Uhl M, Ghanem N, Schmal H, et al. Long-term T2 and qualitative MRI morphology after first-generation knee autologous chondrocyte implantation: cartilage ultrastructure is not correlated to clinical or qualitative MRI outcome. Am J Sports Med. 2014;42:1832-40. [DOI] [PubMed] [Google Scholar]
- 71. Loken S, Heir S, Holme I, Engebretsen L, Aroen A. 6-year follow-up of 84 patients with cartilage defects in the knee. Knee scores improved but recovery was incomplete. Acta Orthop. 2010;81:611-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Witvrouw E, Danneels L, Thijs Y, Cambier D, Bellemans J. Does soccer participation lead to genu varum? Knee Surg Sports Traumatol Arthrosc. 2009;17:422-7. [DOI] [PubMed] [Google Scholar]
- 73. Thijs Y, Bellemans J, Rombaut L, Witvrouw E. Is high-impact sports participation associated with bowlegs in adolescent boys? Med Sci Sports Exerc. 2012;44:993-8. [DOI] [PubMed] [Google Scholar]
- 74. Sauerschnig M, Bauer JS, Kohn L, Hinterwimmer S, Landwehr S, Woertler K, et al. Alignment does not influence cartilage T2 in asymptomatic knee joints. Knee Surg Sports Traumatol Arthrosc. 2014;22:1396-403. [DOI] [PubMed] [Google Scholar]
- 75. Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum. 2009;61:459-67. [DOI] [PubMed] [Google Scholar]
- 76. Spahn G, Schiele R, Hofmann GO, Schiltenwolf M, Grifka J, Vaitl T, et al. The relative risk of knee osteoarthritis after knee injuries: results of a metaanalysis. Phys Med Rehab Kuror. 2011;21:269-79. [Google Scholar]
- 77. Berenbaum F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthritis Cartilage. 2013;21:16-21. [DOI] [PubMed] [Google Scholar]
- 78. Mandelbaum B, Waddell D. Etiology and pathophysiology of osteoarthritis. Orthopedics. 2005;28:S207-14. [DOI] [PubMed] [Google Scholar]
- 79. Rossignol M, Leclerc A, Hilliquin P, Allaert FA, Rozenberg S, Valat JP, et al. Primary osteoarthritis and occupations: a national cross sectional survey of 10 412 symptomatic patients. Occup Environ Med. 2003;60:882-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Sauerschnig M, Stolberg-Stolberg J, Schulze A, Salzmann GM, Perka C, Dynybil CJ. Diverse expression of selected cytokines and proteinases in synovial fluid obtained from osteoarthritic and healthy human knee joints. Eur J Med Res. 2014;19:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Schmal H, Salzmann GM, Niemeyer P, Langenmair E, Guo R, Schneider C, et al. Early intra-articular complement activation in ankle fractures. BioMed Res Int. 2014;2014:426893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Schmal H, Salzmann GM, Langenmair ER, Henkelmann R, Sudkamp NP, Niemeyer P. Biochemical characterization of early osteoarthritis in the ankle. ScientificWorldJournal. 2014;2014:434802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Schmal H, Henkelmann R, Mehlhorn AT, Reising K, Bode G, Sudkamp NP, et al. Synovial cytokine expression in ankle osteoarthritis depends on age and stage. Knee Surg Sports Traumatol Arthrosc. 2015;23:1359-67. [DOI] [PubMed] [Google Scholar]
- 84. van Meegeren ME, Roosendaal G, Jansen NW, Lafeber FP, Mastbergen SC. Blood-induced joint damage: the devastating effects of acute joint bleeds versus micro-bleeds. Cartilage. 2013;4:313-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Wilder FV, Hall BJ, Barrett JP, Jr, Lemrow NB. History of acute knee injury and osteoarthritis of the knee: a prospective epidemiological assessment. The Clearwater Osteoarthritis Study. Osteoarthritis Cartilage. 2002;10:611-6. [DOI] [PubMed] [Google Scholar]
- 86. Chitnavis J, Sinsheimer JS, Clipsham K, Loughlin J, Sykes B, Burge PD, et al. Genetic influences in end-stage osteoarthritis. Sibling risks of hip and knee replacement for idiopathic osteoarthritis. J Bone Joint Surg Br. 1997;79:660-4. [DOI] [PubMed] [Google Scholar]
- 87. Salzmann GM, Nuernberger B, Schmitz P, Anton M, Stoddart MJ, Grad S, et al. Physicobiochemical synergism through gene therapy and functional tissue engineering for in vitro chondrogenesis. Tissue Eng A. 2009;15:2513-24. [DOI] [PubMed] [Google Scholar]
- 88. Vogt S, Wexel G, Tischer T, Schillinger U, Ueblacker P, Wagner B, et al. The influence of the stable expression of BMP2 in fibrin clots on the remodelling and repair of osteochondral defects. Biomaterials. 2009;30:2385-92. [DOI] [PubMed] [Google Scholar]
- 89. Jin X, Jones G, Cicuttini F, Wluka A, Zhu Z, Han W, et al. Effect of vitamin D supplementation on tibial cartilage volume and knee pain among patients with symptomatic knee osteoarthritis: a randomized clinical trial. JAMA. 2016;315:1005-13. [DOI] [PubMed] [Google Scholar]
- 90. Musumeci G, Aiello FC, Szychlinska MA, Di Rosa M, Castrogiovanni P, Mobasheri A. Osteoarthritis in the XXIst century: risk factors and behaviours that influence disease onset and progression. Int J Mol Sci. 2015;16:6093-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Arliani GG, Lara PS, Astur DC, Cohen M, Goncalves JP, Ferretti M. Impact of sports on health of former professional soccer players in Brazil. Acta Ortop Bras. 2014;22:188-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Armenis E, Pefanis N, Tsiganos G, Karagounis P, Baltopoulos P. Osteoarthritis of the ankle and foot complex in former Greek soccer players. Foot Ankle Spec. 2011;4:338-43. [DOI] [PubMed] [Google Scholar]
- 93. Chantraine A. Knee joint in soccer players: osteoarthritis and axis deviation. Med Sci Sports Exerc. 1985;17:434-9. [DOI] [PubMed] [Google Scholar]
- 94. Drawer S, Fuller CW. Propensity for osteoarthritis and lower limb joint pain in retired professional soccer players. Br J Sports Med. 2001;35:402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Elleuch MH, Guermazi M, Mezghanni M, Ghroubi S, Fki H, Mefteh S, et al. Knee osteoarthritis in 50 former top-level soccer players: a comparative study. Ann Readapt Med Phys. 2008;51:174-8. [DOI] [PubMed] [Google Scholar]
- 96. Kujala UM, Kettunen J, Paananen H, Aalto T, Battie MC, Impivaara O, et al. Knee osteoarthritis in former runners, soccer players, weight lifters, and shooters. Arthritis Rheum. 1995;38:539-46. [DOI] [PubMed] [Google Scholar]
- 97. Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145-52. [DOI] [PubMed] [Google Scholar]
- 98. von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Spahn G, Grosser V, Schiltenwolf M, Schroter F, Grifka J. Football as risk factor for a non-injury-related knee osteoarthritis - results from a systematic review and meta-analysis [in German]. Sportverletz Sportschaden. 2015;29:27-39. [DOI] [PubMed] [Google Scholar]
- 100. Ding L, Guo D, Homandberg GA, Buckwalter JA, Martin JA. A single blunt impact on cartilage promotes fibronectin fragmentation and upregulates cartilage degrading stromelysin-1/matrix metalloproteinase-3 in a bovine ex vivo model. J Orthop Res. 2014;32:811-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Simon D, Mascarenhas R, Saltzman BM, Rollins M, Bach BR, Jr, MacDonald P. The relationship between anterior cruciate ligament injury and osteoarthritis of the knee. Adv Orthop. 2015;2015:928301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Saris DB, Dhert WJ, Verbout AJ. Joint homeostasis. The discrepancy between old and fresh defects in cartilage repair. J Bone Joint Surg Br. 2003;85:1067-76. [DOI] [PubMed] [Google Scholar]
- 103. Bizzini M, Silvers HJ. Return to competitive football after major knee surgery: more questions than answers? J Sports Sci. 2014;32:1209-16. [DOI] [PubMed] [Google Scholar]
- 104. McCall A, Carling C, Davison M, Nedelec M, Le Gall F, Berthoin S, et al. Injury risk factors, screening tests and preventative strategies: a systematic review of the evidence that underpins the perceptions and practices of 44 football (soccer) teams from various premier leagues. Br J Sports Med. 2015;49:583-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Shrier I. Muscle dysfunction versus wear and tear as a cause of exercise related osteoarthritis: an epidemiological update. Br J Sports Med. 2004;38:526-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Bizzini M, Dvorak J. FIFA 11+: an effective programme to prevent football injuries in various player groups worldwide-a narrative review. Br J Sports Med. 2015;49:577-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Tonge DP, Pearson MJ, Jones SW. The hallmarks of osteoarthritis and the potential to develop personalised disease-modifying pharmacological therapeutics. Osteoarthritis Cartilage. 2014;22:609-21. [DOI] [PubMed] [Google Scholar]
- 108. Lafeber FP, van Spil WE. Osteoarthritis year 2013 in review: biomarkers; reflecting before moving forward, one step at a time. Osteoarthritis Cartilage. 2013;21:1452-64. [DOI] [PubMed] [Google Scholar]


