Abstract
Peak oxygen uptake (VO2peak) is an indicator of cardiovascular health and a useful tool for risk stratification. Direct measurement of VO2peak is resource-demanding and may be contraindicated. There exist several non-exercise models to estimate VO2peak that utilize easily obtainable health parameters, but none of them includes lung function measures or hemoglobin concentrations. We aimed to test whether addition of these parameters could improve prediction of VO2peak compared to an established model that includes age, waist circumference, self-reported physical activity and resting heart rate. We included 1431 subjects aged 69-77 years that completed a laboratory test of VO2peak, spirometry, and a gas diffusion test. Prediction models for VO2peak were developed with multiple linear regression, and goodness of fit was evaluated. Forced expiratory volume in one second (FEV1), diffusing capacity of the lung for carbon monoxide and blood hemoglobin concentration significantly improved the ability of the established model to predict VO2peak. The explained variance of the model increased from 31% to 48% for men and from 32% to 38% for women (p<0.001). FEV1, diffusing capacity of the lungs for carbon monoxide and hemoglobin concentration substantially improved the accuracy of VO2peak prediction when added to an established model in an elderly population.
Introduction
Cardiorespiratory fitness is an indicator of cardiovascular health and is a good predictor of all-cause mortality [1]. Measurement of peak oxygen uptake (VO2peak) during an incremental work test is considered the best measure of cardiorespiratory fitness [2, 3]. Measured VO2peak is a useful tool for risk stratification and is of interest when planning and evaluating medical treatment, surgery or rehabilitation [4, 5]. However, incremental work tests are not routinely used in most healthcare settings as they are time-consuming, costly and require trained personnel and expensive equipment, and are also contraindicated in some patients.
To avoid the disadvantages with incremental work tests, several non-exercise models to estimate VO2peak have been developed [6–12]. The models have included easily obtainable measures such as sex, age, self-reported physical activity, resting heart rate, smoking history, BMI, waist circumference and body composition. Models of non-exercise estimation of VO2peak have been shown to predict cardiovascular and all-cause mortality [13, 14].
VO2peak is an important predictor of morbidity and mortality [15], and an indicator of functional decline in elderly [16]. With increasing age the mortality and morbidity of most diseases increase. Tools for prediction of VO2peak without the need of an exercise test could be particularly useful for both clinical and research purposes in this age group.
VO2peak reflects the maximal rate the body can take up oxygen from the surrounding air and utilize it to produce energy-rich substrate for biological functions. This process comprises several steps: air inspiration, diffusion of O2 over the alveolocapillary membrane, binding to blood hemoglobin, transport through the cardiovascular system and diffusion of oxygen from the blood into the muscle cells, and finally utilization of oxygen by the mitochondrial enzymes. While it is not possible to measure the functional capacity of the cardiovascular system without exercise testing, several of the other steps of the oxygen uptake and transport are easily measurable at rest. Spirometry measures the capacity of the respiratory system to transport air into and out of the lungs. Diffusion capacity testing measures the conductance of gas from the alveoli across the alveolocapillary membrane until binding to the hemoglobin in the erythrocytes. Spirometry data and blood hemoglobin concentration are usually available or easily obtainable in a general practice setting, while CO-diffusion data are frequently available in hospital settings. To our knowledge, measurements of pulmonary function have not previously been evaluated in non-exercise estimation models of VO2peak. Based on the physiological connection between oxygen uptake and these parameters, we hypothesize that they can improve a non-exercise estimation model of VO2peak.
We have previously shown that forced expiratory volume in 1 second (FEV1) and diffusing capacity of the lungs divided by alveolar volume (DLCO/VA) are associated with VO2peak [17] in elderly. It is therefore relevant to include lung function indices as predictors in non-exercise estimation models of VO2peak in elderly.
In a mostly healthy elderly population aged 69–77 years, we included spirometry data, hemoglobin values and lung diffusing capacity data in a previously validated non-exercise prediction model of VO2peak developed by Nes et al [7]. We hypothesized that addition of these lung function indices would improve the prediction of VO2peak in this population.
Methods
Study subjects were obtained from the Generation 100 study with clinicaltrials.gov identifier NCT01666340. This is a randomized controlled study on the effects of an exercise intervention in elderly, previously described in detail [17, 18]. All participants gave written informed consent. Briefly, all persons born from 1st January 1936 to 31st December 1942 who were registered inhabitants of Trondheim municipality by the 1st January 2012 (n = 6966) were invited to participate in a randomized, controlled trial aiming to study the effect of an exercise intervention on morbidity and mortality. Subjects with conditions or test results indicating that high intensity exercise could be unsafe were excluded. The present study uses baseline, pre-randomization data from the Generation 100 study. Baseline testing were performed as previously described and included symptom-limited test of VO2peak; spirometry (pre-bronchodilator values), lung diffusion capacity (Sensormedics Vmax22 Encore, CareFusion, San Diego, USA) in accordance with the ATS/ERS standardized procedures[19, 20]. VO2peak was measured by an incremental work test on a treadmill using the gas analyzer Oxycon Pro (Erich Jaeger, Hoechberg, Germany, n = 67) or Cortex MetaMax II (Leipzig, Germany, n = 1364). After a warm-up period, the work load was increased by 1 km/h or 2% inclination every 1 to 2 minutes until exhaustion. Tests were aborted if subjects reported to have chest pain, nausea or dizziness. Subjects previously having aborted testing due to such symptoms and also those with previously diagnosed heart disease were supervised by a trained physician during testing with monitoring of blood pressure and ECG as recommended [21]. Every 10 seconds the gas analyzers reported average values from the last 30 seconds, and VO2peak was calculated as the average of the three highest consecutive VO2-values. Ventilation, respiratory exchange ratio, heart rate and rated perceived exertion at peak work were registered, but not used as criterions for defining VO2peak. Physical activity index (PAI) was calculated from self-reported physical activity as previously described [7]. Peripheral capillary oxygen saturation (SpO2) at rest was measured (Nonin 8500 Pulse oximeter, Nonin Medical Inc., Plymouth, MN, USA) and blood samples were analyzed for hemoglobin concentration. The Generation 100 Study and the present sub-study were approved by the Regional Committee for Medical Research Ethics (REK 2012/381 B) and all participants gave written informed consents.
Statistical analysis
Predicted values for gas diffusion and spirometry data were calculated from relevant reference equations [22, 23]. Breathing reserve (BR) was calculated as BR = 1-(minute volume at peak exercise/(FEV1x40))[24]. Multiple linear regression analyses with VO2peak (mL·kg-1·min-1) as the dependent variable were performed separately for men and women. In the first model, the previously used predictors age (rounded to nearest year), PAI, resting heart rate (RHR) and waist circumference (WC) [7] were included, whilst in two further models hemoglobin and FEV1, and DLCO/VA were added. DLCO/VA was not corrected for hemoglobin. Forced vital capacity (FVC), FEV1/FVC, SpO2 and DLCO and VA as separate variables were also tested as predictors, but were not included in the final model. Model assumptions were tested using residuals vs fitted values plots. Due to concerns about heteroscedasticity robust estimation of standard errors was used. Collinearity between the variables was assessed by tolerance and variance inflation factor. Due to concerns about non-normal distributions and to assess the internal validity of the models bootstrapping was performed with 10000 randomly drawn samples with replacement and n equal to the total sex-specific cases. This was used to calculate bootstrapped 95% bias-corrected and accelerated confidence intervals for the regression coefficients. The ability of the model to predict a VO2peak in the lower tertile of measured values was evaluated by ROC curves with SigmaPlot 12.0 (Systat, San Jose, CA, USA). All other analyses were performed with IBM SPSS Statistics 23 (New York, USA) or Stata 13.1 (StataCorp, Texas, USA).
Results
Valid VO2peak measurements were obtained from 1520 participants. Of these 43, 37, 4 and 5 individuals were excluded due to missing data on spirometry or DLCO-tests, self-reported physical activity, waist circumference and hemoglobin, respectively, giving 1431 cases eligible for analysis, see flowchart (Fig 1). About 8% of both men and women were current smokers whereas 50% of men and 37% of women were former smokers (Table 1). Mean FEV1 and FVC were respectively 94% and 103% of predicted values for men and 103% and 111% for women. In the never-smoking sub-sample the corresponding percentages were 97% and 104% for men and 105% and 112% for women. Mean peripheral saturation was 97% percent for both men and women. Plots showing distribution of VO2peak and added predictors are shown in S1 File.
Fig 1. Flowchart showing participant excluded due to various missing data.

Table 1. Descriptive statistics for participants.
| Men (n = 722) | Women (n = 709) | |
|---|---|---|
| Age (years) | 72.8±2.0 | 72.9±2.1 |
| Height (cm) | 176.9±5.8 | 163.4±5.2 |
| Weight (kg) | 82.7±11.5 | 68.1±10.8 |
| Body mass index (kg/m2) | 26.4±3.3 | 25.5±3.7 |
| Waist circumference (cm) | 98.2±9.6 | 89.9±10.8 |
| Smoking status (n) | ||
| Current smoker | 58 (8.1%) | 60 (8.6%) |
| Former smoker | 361 (50.3%) | 257 (36.8%) |
| Never smoker | 299 (41.6%) | 382 (54.6%) |
| Resting heart rate (bpm) | 62.8±11.2 | 66.9±9.9 |
| FEV1 | ||
| (liters) | 3.13±0.61 | 2.24±0.36 |
| (% of predicted) | 93.7±16.8 | 102.6±15.8 |
| <80% of predicted (n) | 123 (17.0%) | 52 (7.3%) |
| FVC | ||
| (liters) | 4.35±0.73 | 3.06±0.46 |
| (% of predicted) | 103.2±15.1 | 111.0±15.3 |
| FEV1/FVC | ||
| (%) | 72.0±8.1 | 73.5±6.6 |
| ratio<0.7 (n) | 228 (31.6%) | 176 (24.8%) |
| DLCO | ||
| (mmol·min-1·kPa-1) | 8.99±1.74 | 6.71±1.14 |
| (% of predicted) | 93.1±16.7 | 86.1±13.5 |
| VA | ||
| (liters) | 6.60±0.94 | 4.82±0.64 |
| (% of predicted) | 101.1±12.2 | 98.9±12.0 |
| DLCO/VA | ||
| (mmol·min-1·kPa-1·L-1) | 1.37±0.23 | 1.40±0.20 |
| (% of predicted) | 93.6±18.7 | 84.8±12.0 |
| <75% of predicted (n) | 110 (15.2%) | 131 (18.5%) |
| Resting SpO2 (%) | 96.8±1.4 | 97.1±1.4 |
| Hemoglobin (g/dL) | 15.0±1.1 | 13.9±0.9 |
| Measurements obtained during exercise tests: | ||
| VO2peak(mL·kg-1·min-1) | 31.3±6.8 | 26.3±4.9 |
| Peak heart rate (bpm) | 157±18 | 157±15 |
| Max treadmill speed (km/h) | 6.0±1.3 | 5.2±0.9 |
| Max treadmill inclination (%) | 12.4±4.1 | 11.7±3.3 |
| RER (ratio) | 1.14±0.09 | 1.10±0.09 |
| Breathing reserve (%) | 21.9±16.7 | 30.8±13.2 |
| Breathing reserve<15% (n) | 211 (29.5%) | 79 (11.3%) |
Abbreviations: VO2peak – peak oxygen uptake, FEV1 – forced expiratory volume in 1 second, FVC – forced vital capacity, DLCO – diffusing capacity of the lung for carbon monoxide, VA – alveolar volume, SpO2 – peripheral capillary oxygen saturation, RER – respiratory exchange ratio at peak exercise. Values given as mean±standard deviation or n (column percentage).
Compared to the basic model with age, PAI, WC and RHR, additional inclusion of FEV1 and hemoglobin increased the explained variance (adjusted R2) of measured VO2peak from 31% to 41% for men and from 32% to 34% for women (Table 2). Further addition of DLCO/VA increased the explained variance to 48% and 38% for men and women, respectively. Basic models expanded with only one predictor (FEV1, DLCO/VA or hemoglobin) are shown in S2 File. The prediction equations (Table 3) had tolerance > 0.8 and variance inflation factor < 1.2 indicating no multicollinearity issues. FVC, FEV1/FVC and DLCO and VA as separate variables were also tested in the model, but their additional contributions to explained variance of VO2peak were negligible and did also introduce multicollinearity problems. SpO2 did not improve prediction. Comparison of the results from the bootstrap analyses with that of the normal regression analyses revealed only marginal differences. Bootstrapped confidence intervals and standard deviations and the same statistics from the normal regression analyses yielded the same conclusions attesting to the generalizability of the model to similar populations.
Table 2. Summary of multiple linear regressions models predicting VO2peak.
| Men | Women | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model | Predictors | R | Adj.R2 | R2 change | SEE | R | Adj.R2 | R2 change | SEE |
| 1 | Age, PAI, WC, RHR | 0.56 | 0.31 | 5.61 | 0.57 | 0.32 | 4.04 | ||
| 2 | Age, PAI, WC, RHR, FEV1, Hb | 0.64 | 0.41 | 0.10*** | 5.21 | 0.59 | 0.34 | 0.03*** | 3.97 |
| 3 | Age, PAI, WC, RHR, FEV1, Hb, DLCO/VA | 0.70 | 0.48 | 0.07*** | 4.87 | 0.62 | 0.38 | 0.03*** | 3.87 |
Abbreviations: R – multiple correlation coefficient, SEE – standard error of estimate, PAI – Physical activity index calculated from Nes et al. [7], WC – waist circumference, PAI – Physical activity index, RHR – resting heart rate, FEV1 – forced expiratory volume in 1 second, Hb – blood hemoglobin concentration, DLCO/VA – diffusing capacity divided by alveolar volume.
*** p<0.001 (F-test) compared to previous step.
Table 3. Description of prediction models.
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Variable | β | Bootstrapped 95%CI for β | β | Bootstrapped 95%CI for β | ||
| Model 1 predictors: Age, PAI, WC and RHR | ||||||
| Intercept | 97.825*** | (80.6, 115.0) | 70.108*** | (58.9, 80.9) | ||
| Age | -0.458*** | (-0.646, -0.269) | -0.306*** | (-0.436, -0.164) | ||
| PAI | 0.172*** | (0.125, 0.220) | 0.123*** | (0.092, 0.157) | ||
| WC | -0.322*** | (-0.368, -0.280) | -0.200*** | (-0.228, -0.172) | ||
| RHR | -0.050* | (-0.090, -0.007) | -0.068*** | (-0.097, -0.039) | ||
| Model 2 predictors: Age, PAI, WC, RHR, Hb and FEV1 | ||||||
| Intercept | 64.893*** | (46.5, 83.0) | 56.205*** | (44.2, 68.7) | ||
| Age | -0.331*** | (-0.518, -0.143) | -0.251*** | (-0.391, -0.107) | ||
| PAI | 0.150*** | (0.107, 0.194) | 0.120*** | (0.090, 0.154) | ||
| WC | -0.320*** | (-0.361, -0.284) | -0.199*** | (-0.229, -0.169) | ||
| RHR | -0.056** | (-0.094, -0.016) | -0.069*** | (-0.097, -0.041) | ||
| FEV1 | 2.967*** | (2.289, 3.681) | 2.041*** | (1.199, 2.814) | ||
| Hb | 0.989*** | (0.615, 1.382) | 0.385* | (0.044, 0.728) | ||
| Model 3 predictors: Age, PAI, WC, RHR, Hb, FEV1 and DLCO/VA | ||||||
| Intercept | 47.886*** | (30.8, 65.3) | 45.847*** | (34.0, 58.4) | ||
| Age | -0.177* | (-0.353, -0.009) | -0.178* | (-0.321, -0.038) | ||
| PAI | 0.131*** | (0.092, 0.171) | 0.114*** | (0.084, 0.148) | ||
| WC | -0.342*** | (-0.379, -0.310) | -0.211*** | (-0.240, -0.183) | ||
| RHR | -0.055*** | (-0.090, -0.021) | -0.068*** | (-0.095, -0.040) | ||
| FEV1 | 3.266*** | (2.639, 3.888) | 2.447*** | (1.624, 3.233) | ||
| Hb | 0.693*** | (0.305, 1.066) | 0.287 | (-0.057, 0.638) | ||
| DLCO/VA | 8.485*** | (6.723, 10.190) | 4.635*** | (3.101, 6.156) | ||
Abbreviations: β – regression coefficient, β-weights – standardized coefficient, PAI – Physical activity index calculated from Nes et al. [7], WC – waist circumference, PAI – Physical activity index, RHR – resting heart rate, FEV1 – forced expiratory volume in 1 second, Hb – blood hemoglobin concentration, DLCO/VA – diffusing capacity divided by alveolar volume.
*p<0.05
**p<0.01
***p<0.001 (non-bootstrapped).
Description of prediction models with regression coefficients and bootstrapped confidence intervals. VO2peak is dependent variable.
Bland-Altman plots (Fig 2) show that VO2peak is overestimated for low levels of VO2peak, and underestimated for high levels. This over- and underestimation is attenuated when lung function and hemoglobin are added to the models. This attenuation is evident by the reduction in the slope of the trend lines in the Bland-Altman plots as these parameters are added in the models.
Fig 2. Bland-Altman plots for predictions models.
Difference between predicted and measured VO2peak is plotted against the average of the predicted and measured VO2peak. A line of best fit is plotted to show trends. Slope and 95% confidence interval for slope for this line is given. Shaded areas represent 95% limits of agreement.
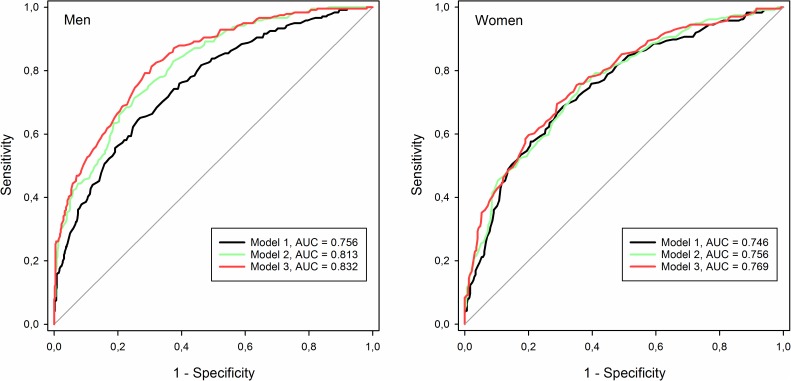
To better visualize how adding parameters to the models change their predictive performance, the ability of the models to correctly identify subjects in the lower tertile of measured VO2peak was illustrated using Receiver Operating Characteristic (ROC) curves. Adding hemoglobin and lung function improved the ability of the models to identify men in the lower tertile of VO2peak, as is shown by increased area under the ROC curve, but little effect was seen for women (Fig 3).
Fig 3. Performance of models identifying subjects with VO2peak in lower tertile.
ROC curves for detecting subjects in the lower tertile of measured VO2peak (<28.1 ml·kg-1·min-1 for men, <23.9 ml·kg-1·min-1 for women). Significance of change in area under curve (AUC) for men: model 1 vs. model 2 p<0.001, model 1 vs. model 3 p<0.001, model 2 vs. model 3 p = 0.052; women: model 1 vs. model 2 p = 0.108, model 1 vs. model 3 p = 0.009, model 2 vs. model 3 p = 0.052 (chi-square test).
Discussion
In this study we found that hemoglobin and lung function measurements can be used to improve a previously developed non-exercise model of VO2peak prediction in elderly individuals. A new prediction model containing FEV1, hemoglobin and DLCO/VA have been developed in this large study sample aged 69–77 years.
The explained variances (adjusted R2) estimated by the present prediction models (0.48 for men and 0.38 for women) are low compared with other comparable studies that have reported values in the range of 0.56–0.74 [7–11]. This can largely be explained by the relatively homogenous study group in general and especially the narrow age span with corresponding less contribution of age to the explained variance. The accuracy of the predictions evaluated with standard error of the estimate for VO2peak (SEE) in our model show equivalent or better predictions (4.87 for men and 3.87 for women) compared to other models that have reported error values in the range of 4.7–5.7 [7–11].
The clinical usefulness of VO2peak prediction models is much dependent on their ability to identify individuals with low fitness. Those with low fitness have not only increased risk for disease and death, but also the greatest potential for improvements in their fitness level from exercise interventions. Our results suggest that the ability of non-exercise estimation models of VO2peak to correctly identify elderly subject with low fitness can be improved by adding measurements of lung function and hemoglobin to the prediction models.
Our models show that FEV1 and DLCO/VA are, at least for men, potent determinants for VO2peak. Pulmonary function has to our knowledge not previously been evaluated in non-exercise prediction models of VO2peak, maybe due to a conception that the lungs have a spare capacity and are not limiting exercise capacity in healthy subjects.
There are few studies on lung diffusing capacity in the elderly, and to our knowledge, the present data constitute the largest data set gathered. Compared with predicted values from equations developed in a healthy never-smoking Spanish population aged 65–85 [22], measured mean DLCO and DLCO/VA were about 7% lower than predicted for men and 15% lower than predicted for women. For the never-smoking sub-sample corresponding figures were 2% and 13% lower in men and women, respectively. Measured mean for VA were very close to the predicted mean.
The increase in the explained variance from adding lung function measurements and hemoglobin to the prediction models is greater for men than for women. The improvements in prediction for men are also evident from the ROC curves in Fig 3, but for women the effects of adding these variables are marginal. One of the possible explanations for this sex-difference is that a larger proportion of the men seem to be ventilatory limited during exercise. Reaching minute ventilation constituting more than 85% of the maximal voluntary ventilation during exercise is regarded as a sign of ventilatory limitation. Among our study subjects almost three times as many men as women reached this threshold indicating that they might have their maximal exercise capacity limited by a relatively low ventilatory function. The distribution of measured lung function is also different between the sexes. Men have considerably higher standard deviations for all measured pulmonary function parameters compared to women. The higher spread in lung function for men gives lung function a higher potential for explaining variance of VO2peak in men than in women.
The strengths of this study are the population-based design and the extensive testing of pulmonary function and directly measured VO2peak in a large sample of elderly. No other non-exercise VO2peak prediction model have been developed or validated in a larger population of elderly. Bootstrapped confidence intervals and standard deviations and the same statistics from the normal regression analyses yielded the same conclusions, attesting to the generalizability of the model to similar populations. Few of the study subjects had severe cardiopulmonary restrictions, so the models cannot be assumed to apply to such individuals. The study subjects were invited to participate in an exercise intervention study and it is possible that this have led to selection bias favoring fit individuals or those with a special interest for exercise. Ventilatory function and gas diffusing capacity is reduced with age, and while reduced lung function may limit maximal oxygen uptake in elderly, this may not be the case for younger subjects. The prediction models were developed in a relatively fit and healthy population aged 69–77 years. Before the models are applied beyond this age span or for less active individuals, or for individuals with various health conditions, they should be validated against such groups.
Conclusions
We have shown that a validated prediction model of VO2peak can be significantly improved by adding hemoglobin, pre-bronchodilator FEV1 and DLCO/VA measurements in an elderly population. Especially in men, the lung function parameters are shown to be important predictors of cardiovascular fitness. The developed prediction equations may be useful in some clinical or research settings where incremental exercise tests are considered impractical or too resource demanding. Although these models give a rough estimate of cardiorespiratory fitness, it must be emphasized that direct measurement of oxygen uptake during an exercise test is still a far superior method.
Supporting information
(PDF)
(PDF)
Acknowledgments
The authors would like to acknowledge Solfrid Løwensprung for her considerable contribution in obtaining pulmonary function measurements.
Data Availability
Due to ethical restrictions involving participant consent, third party data used from the Generation 100 study in research projects will when reasonably requested by others be made available on request to generasjon100@medisin.ntnu.no.
Funding Statement
Erlend Hassel received a Ph.D.-grant from Norwegian Health Association (www.nasjonalforeningen.no, grant number N/A). K.G. Jebsen Center for Exercise in Medicine was funded by The Kristian Gerhard Jebsen Foundation (www.stiftkgj.no, grant number N/A). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA. 2009;301(19):2024–35. 10.1001/jama.2009.681 [DOI] [PubMed] [Google Scholar]
- 2.Struthers R, Erasmus P, Holmes K, Warman P, Collingwood A, Sneyd JR. Assessing fitness for surgery: a comparison of questionnaire, incremental shuttle walk, and cardiopulmonary exercise testing in general surgical patients. Br J Anaesth. 2008;101(6):774–80. 10.1093/bja/aen310 [DOI] [PubMed] [Google Scholar]
- 3.Vanhees L, Lefevre J, Philippaerts R, Martens M, Huygens W, Troosters T, et al. How to assess physical activity? How to assess physical fitness? Eur J Cardiovasc Prev Rehabil. 2005;12(2):102–14. [DOI] [PubMed] [Google Scholar]
- 4.Kavanagh T, Mertens DJ, Hamm LF, Beyene J, Kennedy J, Corey P, et al. Prediction of long-term prognosis in 12 169 men referred for cardiac rehabilitation. Circulation. 2002;106(6):666–71. [DOI] [PubMed] [Google Scholar]
- 5.Loewen GM, Watson D, Kohman L, Herndon JE 2nd, Shennib H, Kernstine K, et al. Preoperative exercise Vo2 measurement for lung resection candidates: results of Cancer and Leukemia Group B Protocol 9238. J Thorac Oncol. 2007;2(7):619–25. 10.1097/JTO.0b013e318074bba7 [DOI] [PubMed] [Google Scholar]
- 6.George JD, Stone WJ, Burkett LN. Non-exercise VO2max estimation for physically active college students. Med Sci Sports Exerc. 1997;29(3):415–23. [DOI] [PubMed] [Google Scholar]
- 7.Nes BM, Janszky I, Vatten LJ, Nilsen TI, Aspenes ST, Wisloff U. Estimating V.O 2peak from a nonexercise prediction model: the HUNT Study, Norway. Med Sci Sports Exerc. 2011;43(11):2024–30. 10.1249/MSS.0b013e31821d3f6f [DOI] [PubMed] [Google Scholar]
- 8.Jackson AS, Blair SN, Mahar MT, Wier LT, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc. 1990;22(6):863–70. [DOI] [PubMed] [Google Scholar]
- 9.Jurca R, Jackson AS, LaMonte MJ, Morrow JR Jr., Blair SN, Wareham NJ, et al. Assessing cardiorespiratory fitness without performing exercise testing. Am J Prev Med. 2005;29(3):185–93. 10.1016/j.amepre.2005.06.004 [DOI] [PubMed] [Google Scholar]
- 10.Matthews CE, Heil DP, Freedson PS, Pastides H. Classification of cardiorespiratory fitness without exercise testing. Med Sci Sports Exerc. 1999;31(3):486–93. [DOI] [PubMed] [Google Scholar]
- 11.Wier LT, Jackson AS, Ayers GW, Arenare B. Nonexercise models for estimating VO2max with waist girth, percent fat, or BMI. Med Sci Sports Exerc. 2006;38(3):555–61. 10.1249/01.mss.0000193561.64152 [DOI] [PubMed] [Google Scholar]
- 12.Mailey EL, White SM, Wojcicki TR, Szabo AN, Kramer AF, McAuley E. Construct validation of a non-exercise measure of cardiorespiratory fitness in older adults. BMC Public Health. 2010;10:59 10.1186/1471-2458-10-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nes BM, Vatten LJ, Nauman J, Janszky I, Wisloff U. A simple nonexercise model of cardiorespiratory fitness predicts long-term mortality. Med Sci Sports Exerc. 2014;46(6):1159–65. 10.1249/MSS.0000000000000219 [DOI] [PubMed] [Google Scholar]
- 14.Stamatakis E, Hamer M, O'Donovan G, Batty GD, Kivimaki M. A non-exercise testing method for estimating cardiorespiratory fitness: associations with all-cause and cardiovascular mortality in a pooled analysis of eight population-based cohorts. Eur Heart J. 2013;34(10):750–8. 10.1093/eurheartj/ehs097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee DC, Sui X, Ortega FB, Kim YS, Church TS, Winett RA, et al. Comparisons of leisure-time physical activity and cardiorespiratory fitness as predictors of all-cause mortality in men and women. Br J Sports Med. 2011;45(6):504–10. 10.1136/bjsm.2009.066209 [DOI] [PubMed] [Google Scholar]
- 16.Morey MC, Pieper CF, Cornoni-Huntley J. Physical fitness and functional limitations in community-dwelling older adults. Med Sci Sports Exerc. 1998;30(5):715–23. [DOI] [PubMed] [Google Scholar]
- 17.Hassel E, Stensvold D, Halvorsen T, Wisloff U, Langhammer A, Steinshamn S. Association between pulmonary function and peak oxygen uptake in elderly: the Generation 100 study. Respir Res. 2015;16:156 10.1186/s12931-015-0317-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stensvold D, Viken H, Rognmo O, Skogvoll E, Steinshamn S, Vatten LJ, et al. A randomised controlled study of the long-term effects of exercise training on mortality in elderly people: study protocol for the Generation 100 study. BMJ Open. 2015;5(2):e007519 10.1136/bmjopen-2014-007519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38. 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 20.Macintyre N, Crapo RO, Viegi G, Johnson DC, van der Grinten CP, Brusasco V, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26(4):720–35. 10.1183/09031936.05.00034905 [DOI] [PubMed] [Google Scholar]
- 21.Gibbons RJ, Balady GJ, Beasley JW, Bricker JT, Duvernoy WF, Froelicher VF, et al. ACC/AHA Guidelines for Exercise Testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). J Am Coll Cardiol. 1997;30(1):260–311. [DOI] [PubMed] [Google Scholar]
- 22.Langhammer A, Johnsen R, Gulsvik A, Holmen TL, Bjermer L. Forced spirometry reference values for Norwegian adults: the Bronchial Obstruction in Nord-Trondelag Study. Eur Respir J. 2001;18(5):770–9. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Rio F, Dorgham A, Galera R, Casitas R, Martinez E, Alvarez-Sala R, et al. Prediction equations for single-breath diffusing capacity in subjects aged 65 to 85 years. Chest. 2012;142(1):175–84. 10.1378/chest.11-2021 [DOI] [PubMed] [Google Scholar]
- 24.Wasserman K, Hansen JE, Sue DY, Stringer WW, Sietsema KE, Sun X, et al. Ventilatory Limitation during Exercise In: Exercise Testing and Interpretation. 5th ed. Phildelphia: Lippincott Williams & Wilkins; 2012. pp. 165–167. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Data Availability Statement
Due to ethical restrictions involving participant consent, third party data used from the Generation 100 study in research projects will when reasonably requested by others be made available on request to generasjon100@medisin.ntnu.no.