Highlights
-
•
Solid pseudopapillary neoplasm is a rare pancreatic tumor.
-
•
Most patients are female and within the second or third decade of life.
-
•
The radiologic features are crucial for an accurate diagnosis.
-
•
Tumor size has not been shown to be a predictor of resectability.
-
•
Surgical resection is the treatment of choice with an excellent long-term prognosis.
Keywords: Solid pseudopapillary neoplasm, Frantz's tumor, Pancreatic tumor, Case report
Abstract
Introduction
Solid pseudopapillary neoplasm (SPN) is a rare pancreatic tumor. Most patients are female within the second or third decade of life with only a small minority concerning children. Frequently described as low malignant potential tumors, surgical resection remains the main treatment.
Presentation of case
The authors present a case of a SPN diagnosed in a 17-year-old Caucasian girl with vomiting and abdominal pain localized to the right upper quadrant. CT scans and MRI scans showed the presence of a well-defined tumor arising from the pancreatic head with 14 cm of greater diameter. Pylorus-preserving pancreatoduodenectomy was performed and histopathology confirmed a SPN with complete resection and no evidence of malignancy.
Discussion
SPN are usually found incidentally hence the importance of an accurate radiologic diagnosis. Symptoms may be present such as abdominal pain or vomiting due to compression, namely in large tumors. A surgical approach is usually indicated aiming complete resection, with tumor size not predicting resectability.
Conclusion
Solid pseudopapillary tumors of the pancreas are extremely rare and usually have an excellent long-term prognosis after surgical resection.
1. Introduction
Solid pseudopapillary neoplasm (Frantz’s tumor) is a rare disease, accounting for 0, 2 to 2, 7% of all pancreatic tumors [1], [2], [3], [4]. Most patients are female within the second or third decade of life with only a small minority concerning children [1], [5], [6].
Frequently they are found incidentally, presenting as a slowly growing abdominal mass with nonspecific symptoms, such as abdominal pain.
Considered to be a low-grade malignant tumor, with an incidence of malignant transformation of around 15%, surgical resection is the treatment of choice with an excellent long-term prognosis [2], [7], [8], [9].
2. Presentation of case
A 17-year-old Caucasian girl, with no relevant past medical or surgical history, presented to our emergency department with vomiting and abdominal pain localized to the right upper quadrant. She denied weight loss or diarrhea and had no jaundice. On physical examination, a mass was present on the right hypochondrial region.
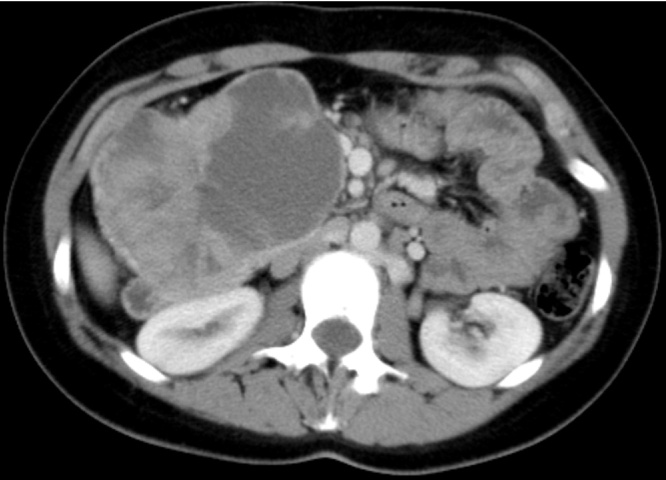
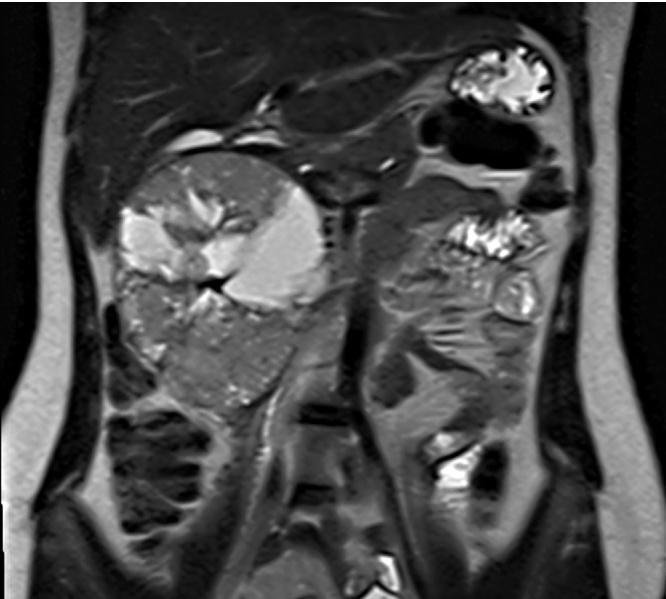
Computed tomography (CT) scan showed the presence of a well-defined tumor arising from de pancreatic head with 14 cm of greater diameter, heterogeneous and with solid and cystic component. In attempt to clarify the diagnosis the patient had a magnetic resonance imaging (MRI) scan confirming this findings and suggesting a solid pseudopapillary neoplasm (SPN) (Fig 1, Fig. 2).
Fig 1.
CT scan showed a well-defined pancreatic tumor.
Fig. 2.
MRI scan showed a heterogeneous pancreatic tumor with solid and cystic component.
No evidence was found of pancreatic insufficiency, abnormal liver function, cholestasis or elevated pancreatic enzymes. Tumor markers carcinoembryonic antigen (CEA), carbohydrate antigen (CA19-9), and alpha-fetoprotein (AFP) were all within normal range.
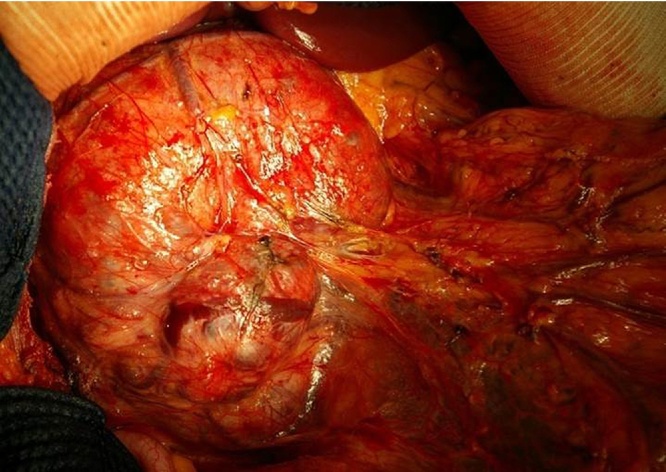
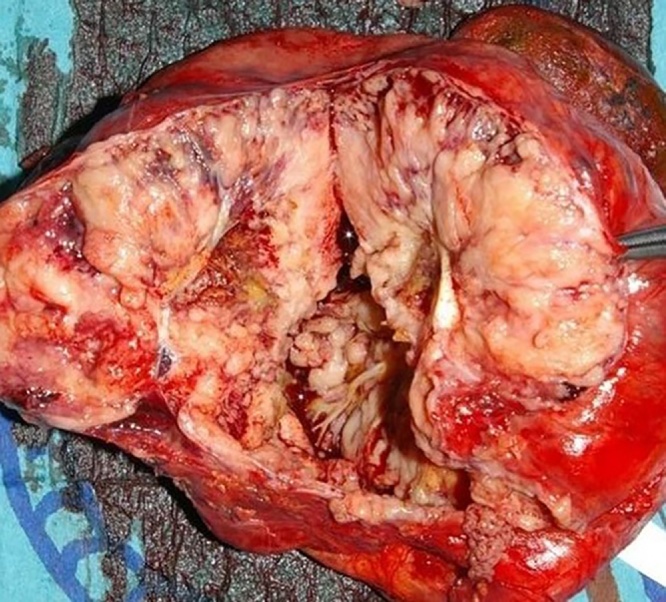
Approximately two weeks later the patient underwent an elective surgery revealing a tick-walled encapsulated mass found in the pancreatic head, without evidence of metastatic disease, and a pylorus-preserving pancreatoduodenectomy was performed (Fig. 3, Fig. 4). Histopathology showed a well circumscribed tumor with a fibrous pseudocapsule, composed of sheets of polygonal cells with pseudopapillary formations, confirming a SPN with complete resection and no evidence of malignancy. Immunochemistry profile revealed positivity for vimentin, CD-10, progesterone receptor and neuron-specific enolase. Focal positivity was found for α-1 antitrypsin, chromogranin A and estrogen receptor.
Fig. 3.
Tumor approximately 14 cm in diameter located in the head of the pancreas.
Fig. 4.
Pancreatoduodenectomy specimen with a macroscopic examination of the tumor.
Postoperative course was uneventful and no additional therapy was administered. After 5 years of follow-up neither signs of tumor recurrence neither endocrine nor exocrine pancreatic insufficiency are present.
3. Discussion
Solid pseudopapillary tumor of the pancreas is extremely rare, mostly occurring in young women within the second or third decade of life, and occasionally diagnosed in children. Usually found incidentally on radiologic examination, SPN is most frequently localized in the head or tail of the pancreas [2]. Extrapancreatic cases have also been reported namely in the retroperitoneum, mesentery and left adrenal gland [5], [8], [10], [11].
Nonspecific symptoms may be present such as abdominal discomfort or pain (36, 8%) and a palpable abdominal mass is present in 12, 3% [10]. Symptoms due to compression such as vomiting are a possibility, as reported in our patient [5]. Bloods tests are usually within normal range and no specific tumor markers are known [5], [8].
An accurate diagnosis is crucial hence the importance of the radiologic features [1]. Other major pancreatic cystic neoplasms should be taken into consideration, such as cystadenocarcinoma or intraductal papillary mucinous neoplasms. SPN appear as a solid well-defined tumor, usually heterogeneous and with solid and cystic component. A pseudocapsule may be present and evidenced by peripheral contrast enhancement [2], [3], [5]. Endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) can help clarify the diagnosis. Biopsy and fine needle aspiration cytology are controversial and rarely performed [8].
Described as low malignant potential tumor, surgery is usually indicated with an improved prognosis and overall survival rate of more than 95% [9], [12]. Radical resection is commonly performed, namely a pancreatoduodenectomy for pancreatic head tumor and a distal pancreatectomy with or without splenectomy for pancreatic body or tail tumor. Pancreatic parenchyma sparing operations such as local resection or enucleation can be an option if a curative complete resection is achievable [5], [9], [13], [14]. Despite the possibility of large sizes due to delayed diagnosis, as reported in our case, tumor size has not been shown to be a predictor of resectability [5], [13], [14]. The presence of metastasis or vascular invasion is not a contraindication for surgical resection, with long survival time shown in patients who underwent vascular resection and reconstruction [8].
On histological evaluation, a typical solid and pseudopapillary structure is present. According to the WHO criteria SPNs are considered malignant in the presence of pancreatic parenchyma, perineural and/or angiovascular invasion, none of which were found in our case [15]. As previously reported immunochemistry profile may reveal positivity for α-1 antitrypsin (>90%), vimentin (>90%), neuron-specific enolase (>80%), chromogranin A, cytokeratin, synaptophysin, progesterone and estrogen receptors [8].
There is no relation between the biological behavior and malignant potential of SPN with known clinical factors or histological criteria [4], [5], [11]. Positive immunoreactivity for Ki-67 may predict the malignant potential and poor outcome of SPNs [16]. Genetic studies are supported by recent reports to better understand the pathogenesis of these tumors [17].
Follow-up is essential due to the potential of local recurrence and appearance of metastasis, most commonly at the liver, regional lymph nodes, mesentery, omentum and peritoneum [5], [10], [18]. Surgery is still the treatment of choice for these situations, with no clear role for systemic therapy or radiotherapy in case of malignancy, inoperable tumors or relapse [5], [13], [14]. Some authors advocate a possible role of an hormonal treatment due to the expression of estrogen receptors in these tumors [20].
4. Conclusion
Solid pseudopapillary tumors of the pancreas are extremely rare and usually have an excellent long-term prognosis after surgical resection. This case report has been written in line with the SCARE criteria [19].
Conflicts of interest
Nothing to declare.
Funding
Nothing to declare.
Ethical approval
No ethical approval has been applied for this case report study.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
S Vilaça: Management of this patient; Study concept; Final revision.
J Falcão: Management of this patient; Study concept; Final revision.
C Branco: Data collection; Writing the article.
Registration of research studies
Not applicable.
Guarantor
C Branco.
References
- 1.Słowik-Moczydłowska Z., Gogolewski M., Yaqoub S. Solid pseudopapillary tumor of the pancreas (Frantz’s tumor): two case reports and a review of the literature. J. Med. Case Rep. 2015;9:268. doi: 10.1186/s13256-015-0752-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Papavramidis T., Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in the English literature. J. Am. Coll. Surg. 2005;2:965–972. doi: 10.1016/j.jamcollsurg.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Cai H., Zhou M., Hu Y. Solid-pseudopapillary neoplasms of the pancreas: clinical and pathological features of 33 cases. Surg. Today. 2013;43:148–154. doi: 10.1007/s00595-012-0260-3. [DOI] [PubMed] [Google Scholar]
- 4.Yang F., Jin C., Long J. Solid pseudopapillary tumor of the pancreas: a case series of 26 consecutive patients. Am. J. Surg. 2009;198:210–215. doi: 10.1016/j.amjsurg.2008.07.062. [DOI] [PubMed] [Google Scholar]
- 5.Guo N., Zhou Q.B., Chen R.F. Diagnosis and surgical treatment of solid pseudopapillary neoplasm of the pancreas: analysis of 24 cases. Can. J. Surg. 2011;54:368–374. doi: 10.1503/cjs.011810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van den Akker M., Angelini P., Taylor G. Malignant pancreatic tumors in children: a single-institution series. J. Pediatr. Surg. 2012;47:681–687. doi: 10.1016/j.jpedsurg.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 7.Tipton S.G., Smyrk T.C., Sarr M.G. Malignant potential of solid pseudopapillary neoplasm of the pancreas. Br. J. Surg. 2006;93:733–737. doi: 10.1002/bjs.5334. [DOI] [PubMed] [Google Scholar]
- 8.Yu P.F., Hu Z.H., Wang X.B. Solid pseudopapillary tumor of the pancreas: a review of 553 cases in Chinese literature. World J. Gastroenterol. 2010;16:1209–1214. doi: 10.3748/wjg.v16.i10.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Law J.K., Ahmed A., Singh V.K. A systematic review of solid-pseudopapillary neoplasms: are these rare lesions? Pancreas. 2014;43:331–337. doi: 10.1097/MPA.0000000000000061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang H.L., Shih S.C., Shang W.H. Solid-pseudopapillary tumor of the pancreas: clinical experience and literature review. World J. Gastroenterol. 2005;11:1403–1409. doi: 10.3748/wjg.v11.i9.1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salvia R., Bassi C., Festa L. Clinical and biological behavior of pancreatic solid pseudopapillary tumors: report on 31 consecutive patients. J. Surg. Oncol. 2007;95:304. doi: 10.1002/jso.20685. [DOI] [PubMed] [Google Scholar]
- 12.Campanile M., Nicolas A., LeBel S. Frantz’s tumor: is mutilating surgery always justified in young patients? Surg. Oncol. 2011;20:121–125. doi: 10.1016/j.suronc.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Gedaly R., Toledano A., Millan G. Treatment of liver metastases from a solid pseudopapillary tumor of the pancreas. J. Hepatobiliary Pancreat. Surg. 2006;13:587–590. doi: 10.1007/s00534-006-1122-4. [DOI] [PubMed] [Google Scholar]
- 14.Vollmer C.M., Dixon E., Grant D. Management of a solid pseudopapillary tumor of the pancreas with liver metastases. HPB (Oxford) 2003;5:264–267. doi: 10.1080/13651820310001397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marchegiani G., Andrianello S., Massignani M. Solid pseudopapillary tumors of the pancreas: specific pathological features predict the likelihood of postoperative recurrence. J. Surg. Oncol. 2016;114:597–601. doi: 10.1002/jso.24380. [DOI] [PubMed] [Google Scholar]
- 16.Yu P., Cheng X., Du Y. Solid pseudopapillary neoplasms of the pancreas: a 19-year multicenter experience in China. J. Gastrointest. Surg. 2015;19:1433–1440. doi: 10.1007/s11605-015-2862-8. [DOI] [PubMed] [Google Scholar]
- 17.Hallas C., Phillipp J., Domanowsky L. BCL9L expression in pancreatic neoplasia with a focus on SPN: a possible explanation for the enigma of the benign neoplasia. BMC Cancer. 2016;16:648. doi: 10.1186/s12885-016-2707-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sperti C., Berselli M., Pasquali C. Aggressive behaviour of solid-pseudopapillary tumor of the pancreas in adults: a case report and review of the literature. World J. Gastroenterol. 2008;14:960–965. doi: 10.3748/wjg.14.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agha R.A., Fowler A.J., Saetta A. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 20.Tognarini I., Tonelli F., Nesi G. In vitro effects of oestrogens, antioestrogens and SERMs on pancreatic solid pseudopapillary neoplasm-derived primary cell culture. Cell. Oncol. 2010;32:331–343. doi: 10.3233/CLO-2010-0522. [DOI] [PMC free article] [PubMed] [Google Scholar]