Abstract
OBJECTIVES
To describe the prevalence and secular trends of high weight-for-length among infants (ages, 3–23 months) in the biennial US Department of Agriculture Women, Infants, and Children Program and Participants Characteristic (WIC-PC) Survey from 2000 through 2014 (n = 16 927 120).
METHODS
Weight-for-length was considered to be “high” if it was ≥2 SDs above the sex-and age-specific median in the World Health Organization growth standards. Poisson regression was used to calculate adjusted prevalence ratios.
RESULTS
The overall prevalence of high weight-for-length increased from 13.4% in 2000 to 14.5% in 2004, remained constant until 2010, and then decreased by >2 percentage points (to 12.3%) through 2014. The prevalence of high weight-for-length was associated with sex (higher among boys), race-ethnicity (highest among American Indians/Alaskan Natives), and with both age (positive) and family income (inverse). The secular trends, however, were fairly similar within categories of these variables. From 2010 to 2014, the prevalence of high weight-for-length decreased in 40 states and 3 (of 5) US territories, with the largest decreases seen in Puerto Rico (−9 percentage points) and Kentucky (−7 percentage points), and the largest increase (+2 percentage points) seen in West Virginia.
CONCLUSIONS
Although the current results cannot be considered representative of infants in the populations, the prevalence of a high weight-for-length has decreased among infants in WIC-PC since 2010. These decreases were similar across categories of most characteristics, but there were substantial differences across jurisdictions, possibly reflecting differences in policy and local programs that target maternal and infant health.
Since the early 1970s, the prevalence of obesity has increased by more than threefold among 6- to 19-year-olds.1, 2 Somewhat similar increases have been seen among 2- to 5-year-olds, with the prevalence increasing from ~5% (1971–1974) to 14% in 2003 to 2004.1–3 The prevalence of obesity among these younger children, however, has decreased by ~5 percentage points since 2003 to 2004.2–4
Despite these well-documented trends, there is relatively little information on trends in high levels of relative weight among infants, which is most frequently assessed by weight-for-length.5 Data from the National Health and Examination Survey (NHANES) indicate that prevalence of a high weight-for-length (≥95th percentile of the Centers for Disease Control and Prevention [CDC] growth charts) among infants (6 to 23 months of age) increased from 7.2% in 1976 to 1980 (SE = 1.0) to 11.6% (1.9) in 1999 to 2000.1 Although there was no consistent trend among infants from 1999–2000 through 2013–2014,6 the small sample sizes (<850 in each 2-year cycle) result in very imprecise estimates. Based on the SE of 1.9% for the 1999–2000 estimated prevalence of high weight-for-length,1 for example, the 95% confidence interval (CI) ranges from 8% to 15%. The small numbers and imprecise estimates in NHANES make it very difficult to identify recent secular trends.
Because several reviews7–9 have concluded that infants with a high weight-for-length are at increased risk for subsequent obesity, it is important to further document trends in this age group. In addition, information on state-specific trends is needed for the development of state-level policies aimed at obesity prevention.8 The objectives of the current study of 3- to 23-month-olds were to describe1 characteristics associated with weight-for-length and2 secular trends in high weight-for-length from 2000 through 2014. We used data from ~17 million infants who were examined in biennial censuses in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Program.
METHODS
Description of the WIC Participants Characteristic Survey
Established in 1972, the WIC program provides supplemental foods, nutrition education, and referrals for health care services to pregnant, postpartum, and breastfeeding women, infants, and children up to their fifth birthday who meet various criteria, including nutritional risk and income eligibility.10 Approximately 83% of all WIC-eligible infants participate in the program during the first year of life,10 and approximately one-half of all infants in the United States are enrolled in WIC.
WIC is administered in each state or territory by state health departments and eligibility is generally based on a family income ≤185% of the federal income-poverty level.11 For a family of 4 in the 48 contiguous states in 2014–2015, the income cutoff would be ≤$44 122. Households with higher incomes may be eligible to receive benefits if a family member is in various federal programs such as the Supplemental Nutrition Assistance Program or Medicaid.
The WIC Participant Characteristics (WIC-PC) Survey is a biennial census of participants who are certified to receive benefits in April of the census year. In each cycle, every state WIC agency submits standardized data on persons enrolled at local agencies.12 The current analyses include data from 8 censuses (2000 to 2014), and is based on data from 50 states, the District of Columbia, and 5 territories. Of the 17 million infants in the current analyses, 2.5% were from a US territory, primarily Puerto Rico.
Infant Characteristics
Children’s anthropometric measurements were taken by trained WIC professionals during certification (or recertification) visits.13 Weight was measured to the nearest one-quarter pound, and length to the nearest one-eighth inch by using an infant measuring board according to CDC surveillance standards.12, 14 We refer to the 3- to 23-month-olds in the current study as “infants,” whereas the term refers to the first year of life in the WIC program.
Race-ethnicity was classified into 5 categories: non-Hispanic white (white), non-Hispanic black (black), Hispanic, American Indian/Alaskan Native, or Asian/Pacific Islander. Race-ethnicity was unknown for ~163 000 children, and these children were excluded from analyses that focused on (or adjusted for) race. Relative income was calculated as 100 times the annual family income divided by the poverty level for a family of the specified size. Approximately 10% of subjects were missing information on relative income.
Classification of High Weight-for-Length and Exclusions
CDC recommends the use of the World Health Organization (WHO) growth standards,15 rather than the CDC growth charts, for infants <24 months of age.16 The WHO standards are based on data from various international communities and are thought to describe the growth of healthy children under optimal conditions.17 We calculated sex- and age-specific z scores for each child18 and considered a weight-for-length ≥2 SDs to be “high”; this cutpoint has proposed for the identification of “abnormal or unhealthy growth.”16 Infants who have a high (defined by various ways) level of weight, BMI, or weight-for-length, as well as those who exhibit rapid growth, are at increased risk of subsequent obesity in childhood and early adulthood.7–9 Although weight-for-length rather than BMI has been recommended for use among infants,16, 19 the 2 measures of relative weight were highly correlated (Spearman r = 0.98) in the current study.
There were 17 239 260 children 3 to 23 months old examined in the 8 censuses who had a recorded date for the weight and length measurements. Of these, we excluded 129 126 (0.8%) who were missing information on sex, weight, or length, as well as 12 156 (0.8%) who had a length outside the range (45–110 cm) in the WHO growth standards and 145 455 (0.9%) who had a measurement considered to be implausible.*20
Statistical Analyses
Analyses were performed in R (R Foundation for Statistical Computing, Vienna, Austria; www.r-project.org/).21 Initial analyses indicated that some of the annual prevalences of high weight-for-length for a state differed substantially from adjacent estimates, and this was further assessed in a robust regression model (“rlm” function).22 Regression models were fit for each state that predicted annual prevalence from year (modeled using splines). Based on a residual >10 percentage points from the fitted line, we excluded the 2002 and 2004 data (n = 25 503) for Hawaii. The sample size for all analyses was 16 927 120.
We first assessed possible knots in the trend in high weight-for-length prevalence over the 8 censuses by using JoinPoint Trend Analysis Software (Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute, Calverton, MD).23 This identified 2004 and 2010 as knots, and several analyses therefore focused on 3 periods, 2000 to 2004, 2004 to 2010, and 2010 to 2014.
We describe participant characteristics, such as the prevalence of high weight-for-length and the distribution of relative income. To calculate the adjusted (for sex, age, and race-ethnicity) change in the prevalence of high weight-for-length in each of these 3 time periods, we used Poisson regression models to estimate prevalence ratios (PRs).24 These PRs were then used to obtain the adjusted change in prevalence during the period. For example, if the initial prevalence was 14% and the adjusted PR (final versus initial prevalence) was 0.90, the adjusted prevalence would have decreased by 1.4 percentage points. Because of the very large n, statistical significance was assessed only in state-specific analyses.
RESULTS
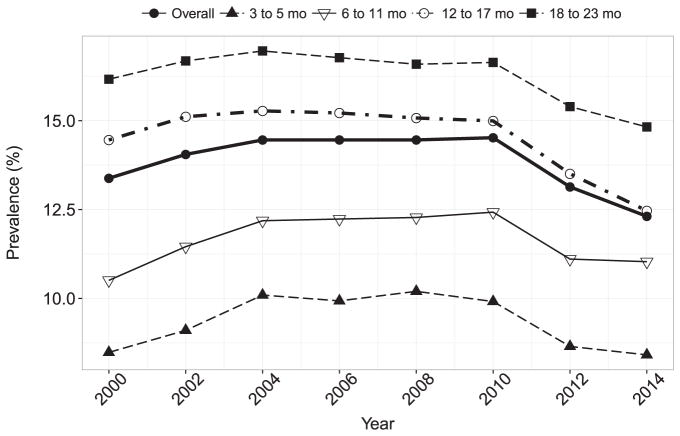
The prevalence of high weight-for-length increased from 13.4% in 2000 to 14.5% in 2004, remained fairly stable from through 2010, and then decreased to 12.3% in 2014 ( Table 1, Fig 1). There were changes in other characteristics over time ( Table 1), with the percentage of Hispanic infants increasing from 35% to 41%, and the percentage of white children decreasing from 38% to 31%. Further, the percentage of infants from families with relative incomes <50% increased from 26% to 35% over the 14 years. As seen in Fig 1, the prevalence of high weight-for-length increased with age, but there was little difference in the age-specific trends over the study period.
TABLE 1.
Characteristics of Infants in the WIC-PC Survey in Selected Years
| 2000 | 2004 | 2010 | 2014 | |
|---|---|---|---|---|
| n | 1 847 324 | 2 018 235 | 2 319 712 | 2 340 611 |
| High weight-for-length, %a | 13.4 | 14.5 | 14.5 | 12.3 |
| Weight-for length z-score | 0.76 | 0.83 | 0.86 | 0.76 |
| Age, mo | 13.7 | 13.6 | 14.2 | 13.5 |
| Girls, % | 49.4 | 49.7 | 49.3 | 49.2 |
| Race-ethnicity, %b | ||||
| White | 38.3 | 35.3 | 32.3 | 31.2 |
| Black | 21.1 | 19.4 | 20.0 | 21.5 |
| Hispanic | 35.4 | 39.7 | 41.8 | 41.4 |
| Asian/Pacific Islander | 3.5 | 3.4 | 3.8 | 4.5 |
| American Indian/Alaskan Native | 0.9 | 1.0 | 1.2 | 1.2 |
| Unknown | 0.8 | 1.2 | 0.9 | 0.1 |
| Relative income, %c | ||||
| <50 | 26.2 | 28.6 | 31.1 | 34.5 |
| 50–99 | 29.7 | 28.6 | 32.4 | 33.0 |
| 100–134 | 16.1 | 14.9 | 14.3 | 13.1 |
| ≥135 | 15.5 | 14.7 | 14.8 | 11.3 |
| Unknown | 12.5 | 13.2 | 7.3 | 8.0 |
High weight-for-length is defined as ≥2 SDs above the median in the WHO growth charts.
Values for race-ethnicity and relative income represent column percentages.
For a family of 4 in the contiguous 48 states, the relative income (expressed as a percentage of the poverty level) cutpoints correspond to incomes of $11 925 (50%), $23 850 (100%), and $32 197 (135%).
FIGURE 1.
Prevalence of high weight-for-length among infants in the WIC-PC survey by year. The overall and age group–specific estimates are shown.
Table 2 shows the prevalence of high weight-for-length within categories of sex, age, race-ethnicity, and relative income. There were substantial differences across race-ethnicity groups, with the 2014 prevalence higher among American Indian (15.6%) and Hispanic (13.8%) infants than among black (11.9%), white (11.0%), and Asian/Pacific Islander (8.5%) infants. The prevalence of high weight-for-length was inversely associated with the relative income of the family.
TABLE 2.
Prevalence of High Weight-for-Length by Various Characteristics Among Infants in WIC-PC, 2000 Through 2014
| Overall | Annual Prevalences | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| n | Prevalence | 2000 | 2004 | 2010 | 2014 | |
| Overall | 16 927 120 | 13.8 | 13.4 | 14.5 | 14.5 | 12.3 |
| Sex | ||||||
| Boys | 8 575 038 | 14.8 | 14.2 | 15.4 | 15.5 | 13.2 |
| Girls | 8 352 082 | 12.9 | 12.5 | 13.5 | 13.5 | 11.4 |
| Age, mo | ||||||
| 3–5 | 1 526 561 | 9.4 | 8.5 | 10.1 | 9.9 | 8.4 |
| 6–11 | 4 110 587 | 11.6 | 10.5 | 12.2 | 12.4 | 11.0 |
| 12–17 | 6 358 680 | 14.4 | 14.5 | 15.3 | 15.0 | 12.5 |
| 18–23 | 4 931 292 | 16.3 | 16.2 | 17.0 | 16.6 | 14.8 |
| Race-ethnicity | ||||||
| Hispanic | 6 832 729 | 16.0 | 15.9 | 16.6 | 17.0 | 13.8 |
| White | 5 684 671 | 11.8 | 11.3 | 12.4 | 12.1 | 11.0 |
| Black | 3 423 061 | 13.4 | 13.3 | 14.5 | 13.9 | 11.9 |
| Asian/Pacific Islander | 638 358 | 9.8 | 9.7 | 10.2 | 10.6 | 8.5 |
| American Indian/Alaskan Native | 185 374 | 18.4 | 19.4 | 20.4 | 18.7 | 15.6 |
| Unknown | 162 927 | 13.8 | 12.5 | 13.2 | 14.0 | 12.9 |
| Relative incomea | ||||||
| 0–49 | 5 086 404 | 14.3 | 14.1 | 15.0 | 15.1 | 12.8 |
| 50–99 | 5 212 089 | 14.2 | 13.8 | 15.0 | 14.8 | 12.4 |
| 100–150 | 3 283 148 | 13.1 | 12.6 | 13.8 | 13.6 | 11.4 |
| ≥150 | 1 625 796 | 12.1 | 11.7 | 12.7 | 12.6 | 10.7 |
| Unknown | 1 719 683 | 14.4 | 13.7 | 14.4 | 15.6 | 12.9 |
| Jurisdiction | ||||||
| State | 16 471 769 | 13.8 | 13.2 | 14.5 | 14.4 | 12.3 |
| Territory | 455 351 | 15.3 | 18.3 | 13.6 | 18.4 | 10.7 |
Relative income expresses a family’s annual income as a percentage of the poverty level.
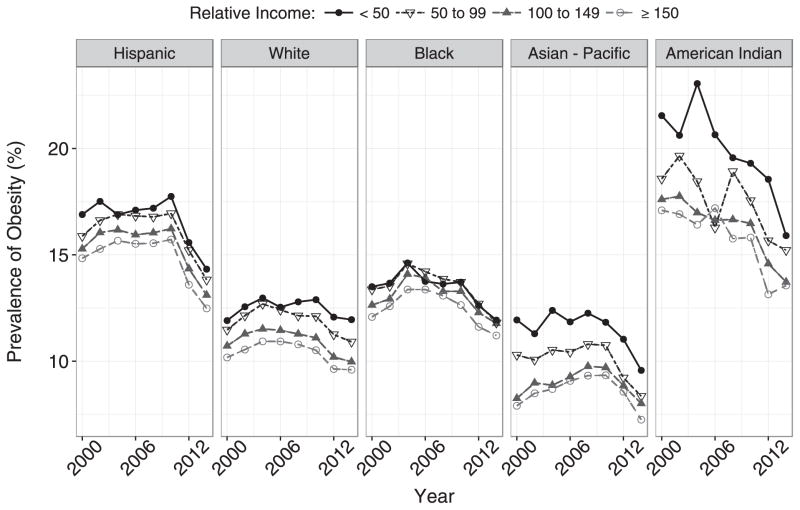
Although race-ethnicity and relative income were correlated, with black infants more likely to have a lower relative family income, and whites and Asian/Pacific Islanders more likely to have higher relative incomes, these characteristics were independently associated with weight-for-length ( Fig 2). At every income level, American Indian infants had the highest prevalence of high weight-for-length, whereas the prevalence was lowest among Asian/Pacific Islander infants. Further, within each race-ethnicity group, the prevalence of high weight-for-length was highest among infants from families below the poverty level. Between 2010 and 2014, all 20 combinations of race-ethnicity and income showed decreases in the prevalence of high weight-for-length. The magnitudes of these decreases, however, were largest among American Indian and Hispanic infants, and smallest among white infants.
FIGURE 2.
Prevalence of high weight-for-length among infants in the WIC-PC survey by race-ethnicity and percent of poverty. Children who were missing information on relative income or race-ethnicity have been excluded.
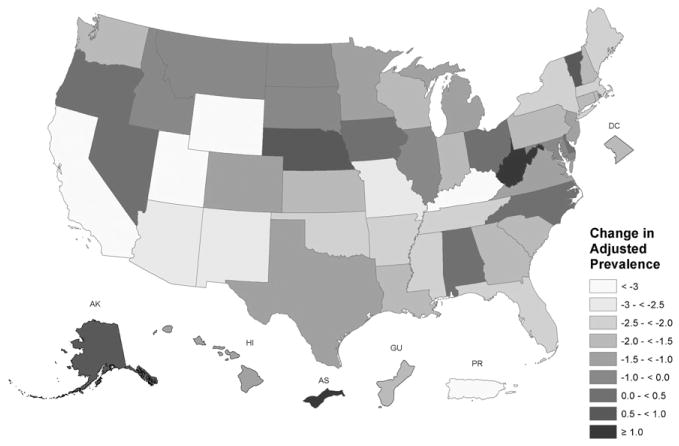
The adjusted change in prevalence between 2010 and 2014 for each of the 50 states (and the District of Columbia) and selected territories are shown in Fig 3. In 2014, the prevalence of high weight-for-length varied by fourfold across the states, ranging from 5.5% in Wyoming (n = 3767) to 22.6% (Virginia, n = 40 505). Among the states, the largest decreases in high weight-for-length between 2010 and 2014 were seen in Kentucky (−7 percentage points) and Utah (−4 points), whereas the largest increase (+2 points) was seen in West Virginia. (Information on the prevalence changes for each of the individual jurisdictions is shown in Supplemental Table 3.) Between 2010 and 2014, 40 states showed a decrease in high weight-for-length, with the change being statistically significant (<0.05) in 36. In contrast, only West Virginia and North Carolina showed statistically significant increases in the prevalence of high weight-for-length. Of the 5 territories, Puerto Rico showed the largest decrease in prevalence (−9 percentage points), whereas the largest increase (+6 points) was seen in America Samoa.
FIGURE 3.
Adjusted (for race, sex, and age) changes in the prevalence of high weight-for-length from 2010 through 2014, by state or territory, among infants in the WIC-PC survey. AS, American Samoa; GU, Guam; PR, Puerto Rico.
DISCUSSION
Our findings indicate that the prevalence of high weight-for-length among WIC-enrolled infants (ages 3 to 23 months) decreased by 2.3 percentage points from 2010 through 2014. This decrease contrasts with the increase in prevalence observed between 2000 and 2004, as well as the lack of change from 2004 to 2010. The 2010 to 2014 decreases were evident in all categories of sex, race-ethnicity, age, and family income, but were largest among American Indian/Alaskan Native and Hispanic infants. The magnitude of the decreases also varied substantially across states, with the largest decrease seen in Kentucky (−7 percentage points) and the largest increase (+2 percentage points) in West Virginia. Analyses (not shown) also indicated that only a very small proportion of these changes could be attributed to demographic changes between 2000 and 2014.
Despite the importance of this age range for the subsequent development of obesity,7–9 there have been few studies of secular trends in high weight-for-length among infants. National US data indicate that among 6- to 23-month-olds, the prevalence of a weight-for-length ≥95th percentile in the CDC growth charts increased from ~7% (1976–1980) to 12% (1999–2000).1 Although 2-year estimates for infants in NHANES should be interpreted cautiously because of the small samples, the prevalence in 2011–2012 (CDC ≥95th percentile) was 8% (95% CI 6–11).3 However, it should be realized that estimates of prevalences and secular trends in WIC, which focuses on low-income families, might differ from national estimates. For example, the prevalence that we observed, based on the WHO growth charts, was approximately twofold higher than in NHANES 2011–2012.3 The race-ethnicity differences that we observed in high weight-for-length, however, agree with those in a large, multisite pediatric practice in Massachusetts.25
Despite the recent reductions in high weight-for-length in WIC, ~12% of the infants in 2014 had a level that was ≥2 SDs above the median. The first few years of a child’s life, in which dietary and lifestyle patterns are established, may be a critical time for the subsequent development of obesity,26 and several reviews7–9 concluded that infants with a high weight-for-length are at increased risk for subsequent obesity. Recent reviews of risk factors8 and interventions27 in early life for subsequent obesity have identified several maternal factors, such as excess gestational weight gain, higher prepregnancy BMI, and smoking that are associated with increased risk. Among infants, characteristics such as rapid weight gain and lower socioeconomic status also are associated with the risk for subsequent obesity. A limitation of the current study is that there was little information in WIC-PC on other characteristics that have been associated with high weight-for-length and child obesity.
There are various factors that could have contributed to the decreases in the prevalence of high weight-for-length that we observed between 2010 and 2014. There has been increased awareness of the high prevalence of childhood obesity among US families, society, and government, and there have been increases in the prevalence of breastfeeding.28, 29 (It should be noted, however, that the prevalence of breastfeeding also increased between 2000 and 2004, a period in which the prevalence of high weight-for-length increased.) There also have been national initiatives, such as Let’s Move, along with recommendations concerning maternal, infant, child, and perinatal health from various national organizations.30–32 Parents, early care and education providers, and health care providers, along with state and local officials, have been identified as groups able to address child obesity.30, 33, 34 The WIC food allocation package also has been aligned with the Dietary Guidelines for Americans35 and the infant feeding guidelines of the American Academy of Pediatrics.36 This has resulted in increased access to a variety of healthy foods and changes in food labeling, as well as increases in the consumption of fruits, vegetables, and whole grains.37–40 It is likely that some of these program changes in WIC, such as the increased availability of healthy foods, have benefited the wider community.37
As has been noted in other studies that have examined state-specific prevalences of obesity,41, 42 we found substantial differences across states. From 2010 to 2014, 40 states showed a decrease in the prevalence of high weight-for-length. However, as the largest decrease and largest increase were seen in neighboring states (Kentucky and West Virginia), these patterns may reflect differences in policies targeted at infant nutrition. It is difficult to identify the causes of these interstate differences, but our findings may reflect a combination of factors, such as initiatives that focus on the implementation of nutrition and physical activity standards for early care and education programs, along with efforts to improve healthier food options and physical activity offerings in communities.43 It is also possible that the revised WIC food allocation package may have been implemented differently across states.
There are several limitations to our study that should be considered when interpreting our results. We defined a high weight-for-length as being ≥2 SDs in the WHO growth standards, and this cutpoint, as well as the 95th percentile, is somewhat arbitrary, because it is based on a statistical distribution rather than biological endpoint. As has been noted by others,3, 16 this classification resulted in fewer (~15% in the current study) infants having a high weight-for-length than does the CDC 95th percentile. There was, however, a very strong association between the WHO and CDC classifications (a κ statistic of 0.9,44 data not shown). Additional analyses also indicated that the secular trends in high weight-for-length were almost identical for the 2 classification systems and did not depend on whether 2 SDs or the 95th percentile was used as the cutpoint.
In addition, our findings apply only to infants who were enrolled in WIC and cannot be extrapolated to all infants. Although this program covers more than 80% of infants in the first year of life,10 the prevalences that we observed differ from those based on limited national data.6 Further, although the analyses excluded 2 years of data from Hawaii that were inconsistent with prevalence estimates for other years, it is possible that other data errors were included. In addition, WIC expanded the set of nutritional risks for certification45 in 2011 to include high weight-for-length, but this may have primarily shifted infants across certification categories. If additional infants were enrolled in 2012 and 2014 based solely on a high weight-for-length, we may have underestimated the extent of the true secular decrease. Although other changes in the eligibility criteria for WIC also may have influenced the prevalence of high weight-for-length among infants over time, there is some evidence to indicate that nearly all eligible families who applied for WIC in recent years have been able to participate.10 Further, we observed decreases in the prevalence of high weight-for-length in all 20 combinations of race-ethnicity and income (Fig 2), indicating that the decreases were independent of these demographic characteristics.
As documented in several reviews,7–9 infants with a high weight-for-length are at increased risk for subsequent obesity, and we found that although the prevalence of high weight-for-length among infants in WIC is high, it decreased by more than 2 percentage points from 2010 to 2014. The documentation of these secular trends in weight-for-length may aid states in the development of obesity-prevention policies8 aimed at further reductions in obesity in early life.
Supplementary Material
WHAT’S KNOWN ON THIS SUBJECT
Trends in obesity among 2- to 19-year-olds in the United States have been well-documented; however, there is little information on trends in high levels of relative weight among infants, which is most frequently assessed by weight-for-length.
WHAT THIS STUDY ADDS
Among 17 million children examined in the Special Supplemental Nutrition Program for Women, Infants, and Children, we found that the prevalence of high weight-for-length increased from 13.4% in 2000 to 14.5% in 2004, remained constant until 2010, and then decreased to 12.3% through 2014.
Acknowledgments
We thank Tricia Brindley (CDC), Lisa McGuire (CDC), and Jinee Burdg (US Department of Agriculture) for help in data management.
FUNDING: No external funding.
ABBREVIATIONS
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- NHANES
National Health and Nutrition Examination Survey
- PR
prevalence ratios
- WHO
World Health Organization
- WIC
Special Supplemental Nutrition Program for Women, Infants, and Children
- WIC-PC
WIC Participant and Program Characteristic Survey
Footnotes
Based on WHO growth standards cutpoints,20 we considered the following values to be implausible: weight-for-age < −6 or >5 SDs, length-for-age < −6 or >6, and weight-for-length < −5 or >5.
Dr Freedman performed most analyses, drafted the initial manuscript, and revised the manuscript; Drs Sharma, Hammer, Panzera, and Blanck critically reviewed and revised the manuscript; Dr Pan and Mr Smith performed some analyses, managed the data, and reviewed the manuscript; and all authors approved the final manuscript as submitted.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of either the Centers for Disease Control and Prevention or the US Department of Agriculture.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief. 2015;(219):1–8. [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cattaneo A, Monasta L, Stamatakis E, et al. Overweight and obesity in infants and pre-school children in the European Union: a review of existing data. Obes Rev. 2010;11(5):389–398. doi: 10.1111/j.1467-789X.2009.00639.x. [DOI] [PubMed] [Google Scholar]
- 6.National Center for Health Statistics. [Accessed November 15, 2016];Prevalence of high weight-for-recumbent length among infants and toddlers from birth to 24 months of age: United States, 1971–1974 through 2013–2014. Available at: www.cdc.gov/nchs/data/hestat/high_weight_recumbent_2013-14/high_weight_recumbent_length_2013_14.htm.
- 7.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;331:929. doi: 10.1136/bmj.38586.411273.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1, 000 days: a systematic review. Am J Prev Med. 2016;50(6):761–779. doi: 10.1016/j.amepre.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Monteiro POA, Victora CG. Rapid growth in infancy and childhood and obesity in later life—a systematic review. Obes Rev. 2005;6(2):143–154. doi: 10.1111/j.1467-789X.2005.00183.x. [DOI] [PubMed] [Google Scholar]
- 10.Oliveira V, Frazao E. The WIC Program: Background, Trends, and Economic Issues. Washington, DC: Economic Research Service, US Department of Agriculture; 2015. 2015 edition. [Google Scholar]
- 11.USDA. Food and Nutrition Service. WIC income eligibility guidelines. Food and Nutrition Service; 2015. [Accessed March 18, 2016]. Available at: www.fns.usda.gov/wic/wic-income-eligibility-guidelines. [Google Scholar]
- 12.Abt Associates. Codebook and Documentation: WIC Participant and Program Characteristics (PC 2010). Prepared for the Office of Research and Analysis. Cambridge, MA: Food and Nutrition Service, US Department of Agriculture; 2012. [Google Scholar]
- 13.Thorn B, Tadler C, Huret N, et al. WIC Participant and Program Characteristics 2014. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service; 2015. [Google Scholar]
- 14.Pennsylvania Department of Health. Anthropometric training manual. Division of Women, Infants and Children; 2010. [Accessed November 15, 2016]. Available at: https://wicworks.fns.usda.gov/wicworks/Sharing_Center/PA/Anthro/lib/pdf/Anthropometric_Training_Manual.pdf. [Google Scholar]
- 15.de Onis M, Garza C, Onyango AW, Borghi E. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr. 2007;137(1):144–148. doi: 10.1093/jn/137.1.144. [DOI] [PubMed] [Google Scholar]
- 16.Grummer-Strawn LM, Reinold C, Krebs NF Centers for Disease Control and Prevention (CDC) Use of World Health Organization and CDC growth charts for children aged 0–59 months in the United States. MMWR Recomm Rep. 2010;59(RR-9):1–15. [PubMed] [Google Scholar]
- 17.de Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food Nutr Bull. 2004;25(suppl 1):S15–S26. doi: 10.1177/15648265040251S103. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC) [Accessed March 28, 2016];A SAS program for the WHO growth charts (ages 0 to <2 years) Available at: www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas-who.htm.
- 19.SACN/RCPCH Expert Group on Growth Standards. Application of WHO Growth Standards in the UK. Norwich, England: The Stationery Office; 2007. [Google Scholar]
- 20.World Health Organization. WHO child growth standards. [Accessed March 18, 2016];SAS igrowup package. Available at: www.who.int/childgrowth/software/readme_sas.pdf.
- 21.Dowle M, Short T, Lianoglou S, Srinivasan A. [Accessed November 15, 2016];data.table: extension of data.frame. Available at: http://cran.rproject.org/web/packages/data.table/index.html.
- 22.Venables W, Ripley B. MASS: support functions and datasets for Venables and Ripley’s MASS. [Accessed March 15, 2016];Comprehensive R Archive Network (CRAN) Available at: https://cran.r-project.org/web/packages/MASS/index.html.
- 23.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 24.Lumley T, Kronmal R. Relative risk regression in medical research: models, contrasts, estimators, and algorithms. [Accessed November 15, 2016];UW Biostatistics Working Paper Series. 2006 Available at: http://biostats.bepress.com/uwbiostat/paper293.
- 25.Wen X, Gillman MW, Rifas-Shiman SL, Sherry B, Kleinman K, Taveras EM. Decreasing prevalence of obesity among young children in Massachusetts from 2004 to 2008. Pediatrics. 2012;129(5):823–831. doi: 10.1542/peds.2011-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Birch LL, Doub AE. Learning to eat: birth to age 2 y. Am J Clin Nutr. 2014;99(3):723S–728S. doi: 10.3945/ajcn.113.069047. [DOI] [PubMed] [Google Scholar]
- 27.Blake-Lamb TL, Locks LM, Perkins ME, Woo Baidal JA, Cheng ER, Taveras EM. Interventions for childhood obesity in the first 1, 000 days: a systematic review. Am J Prev Med. 2016;50(6):780–789. doi: 10.1016/j.amepre.2015.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ryan AS, Wenjun Z, Acosta A. Breastfeeding continues to increase into the new millennium. Pediatrics. 2002;110(6):1103–1109. doi: 10.1542/peds.110.6.1103. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Breastfeeding among U.S. Children Born 2002–2012. [Accessed March 29, 2016];National Immunization Surveys. Available at: www.cdc.gov/breastfeeding/data/NIS_data/index.htm.
- 30.Institute of Medicine. Local Government Actions to Prevent Childhood Obesity. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 31.Daniels SR, Hassink SG Committee on Nutrition. The role of the pediatrician in primary prevention of obesity. Pediatrics. 2015;136(1) doi: 10.1542/peds.2015-1558. Available at: www.pediatrics.org/cgi/content/full/136/1/e275. [DOI] [PubMed] [Google Scholar]
- 32.White House Task Force on Childhood Obesity. [Accessed November 15, 2016];White House Task Force on Childhood Obesity Report to the President. Available at: www.letsmove.gov/white-house-task-force-childhood-obesity-report-president.
- 33.Khan LK, Sobush K, Keener D, et al. Centers for Disease Control and Prevention. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm Rep. 2009;58(RR-7):1–26. [PubMed] [Google Scholar]
- 34.Institute of Medicine. [Accessed June 3, 2016];Early childhood obesity prevention policies. 2011 Available at: www.nationalacademies.org/hmd/Reports/2011/Early-Childhood-Obesity-Prevention-Policies.aspx.
- 35.USDA. Food and Nutrition Service. [Accessed November 15, 2016];Women, Infants, and Children (WIC) background: revisions to the WIC Food Package. Available at: www.fns.usda.gov/wic/background-revisions-wicfood-package.
- 36.American Academy of Pediatrics. [Accessed April 7, 2016];Infant food and feeding. Available at: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/HALF-Implementation-Guide/Age-Specific-Content/Pages/Infant-Food-and-Feeding.aspx.
- 37.Andreyeva T, Luedicke J, Middleton AE, Long MW, Schwartz MB. Positive influence of the revised Special Supplemental Nutrition Program for Women, Infants, and Children food packages on access to healthy foods. J Acad Nutr Diet. 2012;112(6):850–858. doi: 10.1016/j.jand.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 38.Lu W, McKyer ELJ, Dowdy D, et al. Evaluating the influence of the Revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food allocation package on healthy food availability, accessibility, and affordability in Texas. J Acad Nutr Diet. 2016;116(2):292–301. doi: 10.1016/j.jand.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 39.Hillier A, McLaughlin J, Cannuscio CC, Chilton M, Krasny S, Karpyn A. The impact of WIC food package changes on access to healthful food in 2 low-income urban neighborhoods. J Nutr Educ Behav. 2012;44(3):210–216. doi: 10.1016/j.jneb.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 40.Chiasson MA, Findley SE, Sekhobo JP, et al. Changing WIC changes what children eat. Obesity (Silver Spring) 2013;21(7):1423–1429. doi: 10.1002/oby.20295. [DOI] [PubMed] [Google Scholar]
- 41.Singh GK, Kogan MD, van Dyck PC. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Arch Pediatr Adolesc Med. 2010;164(7):598–607. doi: 10.1001/archpediatrics.2010.84. [DOI] [PubMed] [Google Scholar]
- 42.Kann L, Kinchen S, Shanklin SL, et al. Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance—United States, 2013. MMWR Suppl. 2014;63(4):1–168. [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention (CDC) [Accessed June 2, 2016];Overweight and obesity reports. Available at: www.cdc.gov/obesity/resources/reports.html.
- 44.Chmura Kraemer H, Periyakoil VS, Noda A. Kappa coefficients in medical research. Stat Med. 2002;21(14):2109–2129. doi: 10.1002/sim.1180. [DOI] [PubMed] [Google Scholar]
- 45.The Committee on Dietary Risk Assessment in the WIC Program; Food and Nutrition Board; Institute of Medicine. Dietary Risk Assessment in the WIC Program. Washington, DC: National Academies Press; 2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.