Abstract
Background
For more than a decade, the Veterans Health Administration (VHA) has offered MOVE!, a comprehensive lifestyle intervention for weight management. However, there is limited knowledge to inform resource allocation decisions at the health system level—for example, the choice between reaching new veterans with weight management treatment, re-engaging veterans who have stopped attending, and/or increasing contact with current MOVE! participants.
Objective
To inform VHA policy and planning, this VHA-wide study examines the relationship between MOVE! participation and weight outcomes.
Design
A longitudinal observational study of veterans across VHA who participated in MOVE!.
Participants
Veterans who initiated their most recent episode of MOVE! care between 2004 and 2014.
Main Measures
Weight measurements were abstracted from VHA electronic health records. The primary outcome was the proportion of veterans with clinically relevant weight loss. The predictor of interest was number of MOVE! contacts during the 12 months following MOVE! initiation.
Key Results
The cohort consisted of 237,577 veterans (87.4% male; mean age 54.4 years), who had 5.3 contacts on average in the 12 months following initiation. Veterans with 2–5 contacts had the same odds of achieving clinically relevant weight loss as veterans with only one contact (adjusted OR: 1.00, 95% CI: 0.98–1.03). Veterans with 6–9, 10–13, 14–17, and 18 or more contacts had significantly higher odds of clinically relevant weight loss (adjusted OR: 1.17, 95% CI: 1.13–1.20; adjusted OR: 1.53, 95% CI: 1.47–1.59; adjusted OR: 1.84, 95% CI: 1.74–1.94; adjusted OR: 2.21, 95% CI: 2.12–2.31, respectively).
Conclusions
Veterans with ≥6 MOVE! contacts in the year following treatment initiation were significantly more likely to achieve clinically relevant weight loss than those with one contact, with greater participation further increasing the odds of clinically relevant weight loss. While further characterization of weight loss predictors is needed, the VHA should provide policy guidance that supports increasing participation among veterans who have initiated MOVE!.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-017-3992-3) contains supplementary material, which is available to authorized users.
KEY WORDS: weight management, behavioral science, veterans
INTRODUCTION
In recognition of the need to address the steadily increasing rates of overweight and obesity in veterans receiving care in the Veterans Health Administration (VHA), as well as active duty service members, in 2014 the Department of Veterans Affairs (VA) and Department of Defense (DoD) published an updated, evidence-based Clinical Practice Guideline for Screening of Management of Overweight and Obesity (VA-DoD CPG).1 Although the VA-DoD CPG included recommendations regarding which interventions should be offered, it did not specify how they should be implemented at the health system level.2 Moreover, there is limited knowledge informing resource allocation at the health system level. For example, it is unclear whether efforts should emphasize reaching new veterans with weight management treatment, re-engaging veterans who have stopped attending, or increasing contact with current participants.
Informed by other evidence-based recommendations,3 – 6 the VA-DoD CPG emphasizes comprehensive lifestyle interventions (CLI; combines dietary, physical activity, and behavioral strategies) as a key element of weight management for veterans who are obese or overweight with an obesity-associated condition. Based on findings that intensive, multicomponent lifestyle interventions were associated with significantly greater weight loss than less intensive interventions, the VA-DoD CPG recommends CLI with at least 12 contacts within 12 months.3 , 4
In the VHA, the VA-DoD CPG is operationalized through the MOVE! Weight Management Program for Veterans (MOVE!). Guided by national policy, MOVE! is an evidence-based CLI designed as a series of sessions with structured curricula. Delivery has ranged from 8 to 16 sessions per series.7 VHA facility-based MOVE! staff lead program activities and tailor programming to the veterans they serve. Veterans may choose to participate in the series of sessions individually or in a group format, and participation may be in person, by telephone, by video, or a combination thereof.
During the 10 years since national implementation, over 650,000 veterans have participated in MOVE!. However, a national evaluation of MOVE! through 2010 found that 42% of first-time participants never attend more than one MOVE! session.8 Far below the recommended 12 contacts, utilization patterns have indicated that first-time MOVE! participants attended 4.6 visits on average. While the VA-DoD CPG recommends CLI that include at least 12 contacts over 12 months based on evidence that the most effective interventions are of high intensity, i.e., 12 to 26 sessions in a year,3 , 4 , 6 it is unclear whether there is a threshold of visits or contacts below which no effect on weight loss is observed, and the nature of the dose–response relationship is not well understood.
Limited conclusions can be drawn from comparing published studies of MOVE! due to variability in how treatment intensity, weight change outcomes, and time parameters are defined. A study of one VHA region encompassing eight facilities found that intensive treatment, defined as six or more visits, was associated with greater mean weight loss at 12 months.9 Another VHA study of high-intensity MOVE! treatment, defined dichotomously as attending 14 or more sessions within the first 6 months, found that veterans were almost five times as likely to achieve 5% weight reduction at 6 months.10 In comparison, a study conducted at a different VHA facility categorized treatment participation into 0, 1–2, or ≥3 visits, and found that veterans with ≥3 visits had a larger mean percentage change in body weight.11 Moreover, several evaluations of MOVE! have been limited to single-site designs or a focus on special populations (e.g., veterans with specific diagnoses), and thus may lack the exposure contrast needed to assess how variation in participation is related to weight loss.10 – 19,
This VHA-wide study builds on findings from prior national evaluations of MOVE! programming7 , 16 by examining the relationship between MOVE! participation, categorized into various levels of contact, and weight outcomes. A greater understanding of the dose–response relationship will inform VHA policy and planning for optimizing resource allocation between reach (i.e., the number of people who participate in the intervention) and engagement (i.e., the extent to which people participate in the intervention).
METHODS
Cohort
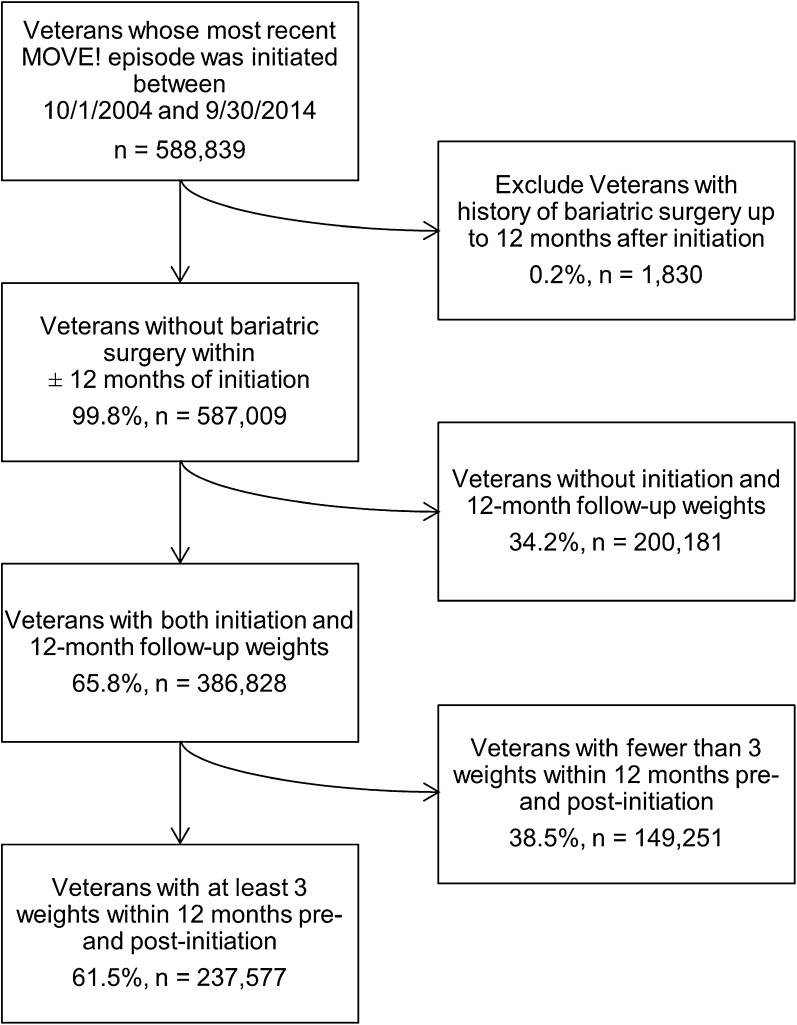
This nationwide study included all veterans receiving care in VHA who participated in at least one MOVE! session. Due to the episodic nature of weight management care, each veteran’s MOVE! participation was conceptualized into episodes that were separated by the absence of a MOVE! visit for ≥6 months, as applicable. In this study, we assessed veterans’ most recent MOVE! episodes that were initiated during the 10-year period from October 1, 2004, to September 30, 2014 (n = 588,839, Fig. 1).
Figure 1.
Cohort inclusion and exclusion flow chart. A total of 588,839 veterans initiated their most recent MOVE! episode of care during the 10-year period between October 1, 2004, and September 30, 2014. After excluding veterans with bariatric surgery and insufficient weight measurements, the final sample included 237,577 veterans.
A veteran’s most recent episode of MOVE! care was defined by the initiation date, i.e., the date of the first MOVE! visit or contact as identified in the electronic health record (EHR). We defined the 12 months prior to initiation as “pre-initiation” and the 12 months following initiation as “post-initiation.” A contact was defined as any clinical encounter between the veteran and a clinical professional in the EHR coded as “MOVE!” that was conducted in person, by telephone, or by video (Online Appendix A).
Veterans whose EHR indicated bariatric surgery (Current Procedural Terminology codes 43644, 43645, 43770, 43775, 43842, 43843, 43845, 43846, or 43847) anytime prior to the end of post-initiation were excluded from this study (n = 1830).
Data Sources
Predictor, covariate, and outcome data from the EHR were accessed through the VHA Corporate Data Warehouse, a repository of all EHRs for VHA facilities across the nation. Data on participation were available from every MOVE! program, as well as demographic information, weight measurements, medication use, and procedure coding.
Predictor
The primary predictor of interest was the number of MOVE! contacts post-initiation. These were categorized as follows: 1, 2–5, 6–9, 10–13, 14–17, and 18 or more, for a total of six categories.
For purposes of this study, episodes of MOVE! that continued longer than 12 months were truncated, and veterans with one contact during their most recent episode of care were used as the reference group.
Outcomes
Weight and height measurements taken during routine health care, including MOVE! participation, were obtained from the VHA’s EHR. Using a multi-step process, weight and height values that were identified as outliers were excluded (Online Appendix B).
The primary outcome was the proportion of veterans with clinically relevant weight loss (≥5% body weight loss) at 12 months following initiation.6 – 8 , 20 , 21 We assigned each veteran’s initiation weight as the weight taken closest to initiation up to 30 days prior to or 7 days after initiation. Similarly, we assigned each veteran’s post-initiation weight as the weight taken closest to 365 days after initiation, up to 60 days prior to and 60 days following the target date. Veterans who did not have weight values meeting the aforementioned time windows were excluded from the analysis (n = 200,181, Online Appendix C). The percentage body weight change was calculated as the difference between initiation weight and post-initiation weight divided by initiation weight.
The secondary outcome of interest was the mean change in weight trajectory from pre-initiation to post-initiation. Veterans with fewer than three weight measurements documented in the medical record during pre-initiation and three during post-initiation were also excluded from the analysis (n = 149,251), resulting in a sample of 237,577 veterans. The linear trends (i.e., slopes) of all weights available in the EHR separately during pre- and post-initiation were calculated in the percentage change in body weight from initiation per year. Change in weight trajectory was defined as the difference between pre-initiation and post-initiation weight trends, where a negative change in weight trajectory indicated that an individual reduced their slope from pre- to post-initiation (not necessarily that the individual lost weight). For example, a veteran who was gaining weight pre-initiation at a rate of +5% per year, and had since attenuated that gain to maintain a stable weight (which is a post-initiation weight trajectory of 0% per year), would experience a −5% change in weight trajectory per year (i.e. change in slope).
Covariates
A variety of demographic variables were available from the EHR, including age, gender, self-identified race, and marital status. Clinical variables were used to characterize the cohort, including body mass index (BMI; categorized into overweight: 25 to <30, obese class I: 30 to <35, obese class II: 35 to <40, and obese class III: ≥40), participation in TeleMOVE!22 (an 82-day disease management protocol for weight management delivered through home telehealth technologies, i.e., in-home messaging devices) during pre- or post-initiation, history of obesogenic23 medication use (at least a 30-day fill of amitriptyline, mirtazapine, olanzapine, quetiapine, risperidone, gabapentin, tolbutamide, pioglitazone, glimepiride, glyburide, glipizide, sitagliptin, or nateglinide) anytime before the end of post-initiation, and history of leptogenic medication use (at least a 30-day fill of sibutramine, orlistat, phentermine, phentermine/topiramate, or lorcaserin) anytime before the end of post-initiation. Naltrexone/bupropion and liraglutide, approved for the treatment of obesity near the end of our study period, were not included as leptogenic medications because no veterans in the cohort were prescribed them before the end of post-initiation.
Analysis
Analyses were conducted using SAS version 9.4 software (SAS Institute Inc., Cary, NC) with an alpha of 0.05. Primary analyses used logistic regression to estimate the odds of achieving clinically relevant weight loss at 1 year post-initiation, with unadjusted and adjusted analyses (with age, gender, marital status, participation in TeleMOVE!, history of obesogenic medication use, and history of leptogenic medication use). Secondary analyses involved estimating linear trends in pre-initiation and post-initiation weight trajectories, then assessing the difference from pre- to post-initiation as the change in weight trajectory per veteran.
RESULTS
The cohort of 237,577 veterans was, on average, 54.4 years old at initiation, i.e., the start of their most recent MOVE! episode (Table 1). The majority of the veterans were male (87.4%) and self-identified as racially white (72.9%), and half were married (50.6%). At initiation, veterans weighed 110.8 kg on average, and 81.9% were considered obese based on BMI. Within the cohort, 3.5% were concurrently enrolled in TeleMOVE!, 3.6% had leptogenic medication use, and 63.7% had obesogenic medication use. Veterans had on average 5.3 (SD = 7.8) MOVE! contacts post-initiation. The median number of contacts was 2, and 39.2% of veterans had only one contact post-initiation.
Table 1.
Cohort Demographics and Characteristics
| Cohort (n = 237,577) | |
|---|---|
| Demographic characteristics | |
| Age in years, mean (SD) | 54.4 (18.0) |
| Male, n (%) | 207,534 (87.4) |
| White, n (%) | 225,129 (72.9) |
| Married, n (%) | 120,051 (50.6) |
| Clinical characteristics | |
| Initiation weight in kg, mean (SD) | 110.8 (23.7) |
| Overweight, n (%) | 37,418 (15.8) |
| Obese – Class I, n (%) | 77,932 (32.8) |
| Obese – Class II, n (%) | 61,846 (26.0) |
| Obese – Class III, n (%) | 54,785 (23.1) |
| TeleMOVE! participation, n (%) | 8321 (3.5) |
| Leptogenic medication use, n (%) | 8562 (3.6) |
| Obesogenic medication use, n (%) | 151,371 (63.7%) |
Primary Analysis
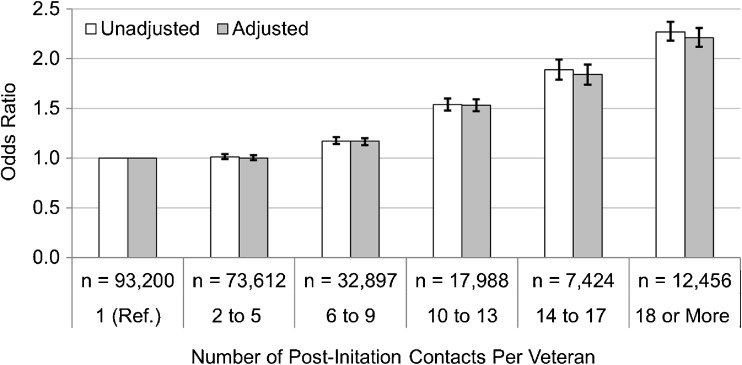
Among veterans with only one contact (used as the reference group), 18.7% achieved clinically relevant weight loss at 12 months post-initiation (Online Appendix D). Similarly, 18.8% of veterans with 2–5 contacts had clinically relevant weight loss and the same odds of achieving clinically relevant weight loss as veterans with only one contact (adjusted OR: 1.00, 95% CI: 0.98–1.03, Fig. 2). Examining categories of increasing MOVE! participation, veterans with 6–9 contacts had significantly higher odds of clinically relevant weight loss (adjusted OR: 1.17, 95% CI: 1.13–1.20), and each subsequent category of participation had significantly higher odds of clinically relevant weight loss. Adjusted models appear to have slightly attenuated effect sizes, but are very similar to the unadjusted estimates.
Figure 2.
Odds of achieving clinically relevant weight loss at 12 months post-initiation, comparing veterans in categories of increasing participation in MOVE! to those with one contact, are shown by the bars, with error bars representing 95% CI. Adjusted odds ratios included covariates for age, gender, race, marital status, TeleMOVE! participation, history of obesogenic medication use, and history of leptogenic medication use. Online Appendix D contains point estimates and 95% CI corresponding to this figure.
Secondary Analysis
Using all weights available in the EHR, we estimated each veteran’s pre- and post-initiation weight trajectory. More than half of veterans (53.8%) had pre-initiation trajectories characterized by weight gain of more than 1% per year (data not shown).
Table 2 shows the mean change in weight trajectory from pre-initiation to post-initiation for each category of participation. Veterans with one contact had a mean change in weight trajectory of −1.76% of body weight per year (95% CI: −1.96 to −1.55). In essence, these veterans “bent” their weight trajectory curves as they moved from pre-initiation to post-initiation by −1.76% body weight change per year on average. Veterans with 2–5 contacts experienced a significantly greater mean change in weight trajectory of −2.04 (95% CI: −2.23 to −1.85) compared to those with one contact. Veterans in additional categories of increasing participation had significantly greater mean change in weight trajectory compared to veterans with one contact.
Table 2.
Mean Change in Weight Trajectory from Pre- to Post-Initiation
| Number of post-initiation contacts per veteran | n | Mean (95% CI)* |
|---|---|---|
| 1 | 93,200 | −1.76 (−1.96 to −1.55) |
| 2–5 | 73,612 | −2.04 (−2.23 to −1.85) |
| 6–9 | 32,897 | −3.32 (−3.70 to −2.93) |
| 10–13 | 17,988 | −4.85 (−5.20 to −4.49) |
| 14–17 | 7424 | −6.45 (−7.00 to −5.90) |
| 18 or more | 12,456 | −7.10 (−7.56 to −6.64) |
* The unit for weight trajectory was estimated in % body weight change per year, such that a change from pre- to post-initiation is shown as the absolute difference in % body weight change per year
DISCUSSION
This study revealed that veterans with six or more MOVE! contacts in the year following treatment initiation were significantly more likely to achieve clinically relevant weight loss than those with one contact, with greater participation further increasing the odds of clinically relevant weight loss. In contrast, veterans with two to five contacts had the same odds of achieving clinically relevant weight loss as veterans with only one contact. While it is difficult to establish a minimum recommended dose for a clinically relevant effect, it appears that there may be a threshold around six contacts. Although some veterans in our cohort had >30 contacts per year, it is unclear whether there is an upper limit where the effect of increasing contacts on achieving clinically relevant weight loss plateaus. To our knowledge, no studies to date have explored this question, and further research is needed.
Our findings are consistent with other studies showing that increased participation is associated with increased weight loss. However, the magnitude of the effect was not well understood because of different definitions for predictors and outcomes. One study of eight VHA facilities found that intensive treatment (≥6 visits) was associated with greater weight loss at 12 months than non-participation.9 Similarly, a recent study reported that veterans who attended ≥14 sessions within 6 months were found to have increased odds of achieving ≥5% weight loss at 6 months compared to participants with fewer visits, while controlling for age, gender, and race (OR: 4.74, 95% CI: 1.3–17.2).10 Using a continuous predictor, another VHA study found increased odds of achieving ≥5% weight loss per additional group visit (OR: 1.05, 95% CI: 1.01–1.08).24 In addition, few studies have assessed MOVE! across multiple VHA facilities, which limits generalizability. Our nationwide study allowed for multiple levels of the predictor with exposure contrast, and assessed outcomes across all MOVE! programs.
Our findings on changes in weight trajectory involved a novel approach that sought to characterize participants by pre-initiation weight trajectory and to identify changes in post-initiation. To our knowledge, this has been done in only one other published MOVE! study, an interrupted time series analysis at a single VHA facility.13 The study found that MOVE! participants were gaining 2 kg/year on average before enrolling in MOVE!, but were losing an average of 1.6 kg/year following participation in 10 weekly group sessions. Our weight trajectory analysis found that over half of the study population had weight gain trajectories pre- initiation. Additional research on weight trends before participation in weight management is needed, because it is possible that changing one’s weight trajectory may be considered clinically meaningful in the absence of a 5% body weight loss. Change in weight trajectory may be an important outcome that demonstrates treatment effect before weight loss is observed.
Several aspects of this study are noteworthy, including the availability of weight values collected through routine health care, allowing for examination of weight outcomes for veterans who did not complete the traditional MOVE! series as designed. Other strengths of the study include the national cohort of veterans participating in MOVE! across all VHA facilities, the large sample size, variability in the number of contacts across veterans, accounting for medication use, and the cohort of primarily older men (compared to many commercial weight loss evaluations that report mostly on women).25
However, there were several limitations to the study, one of which was the lack of a comparison group of individuals without MOVE! contacts. Additionally, our study may have introduced bias by excluding veterans with an insufficient number of weight measurements in the EHR (Online Appendix C), limiting findings to participants who remained engaged in the VHA care for at least 1 year post-initiation. Although extensive effort was made to identify outlier weight values from the EHR (Online Appendix B), the relatively high frequency of inaccurate weights suggests that erroneous values may have been included and potential non-differential misclassification of outcomes.
The primary outcome of interest, weight change 1 year post-initiation of treatment, was chosen specifically to allow for equal follow-up time after treatment initiation. This choice may have inflated the relative effects of longer versus shorter treatment duration (i.e., more vs. fewer MOVE! contacts), because weight change has been shown to be greatest at the end of treatment, often followed by weight regain.26 – 28 This study did not examine how veterans’ short-term weight change may impact longer-term weight change.
We also did not evaluate how veteran characteristics that promoted engagement differed across the categories of contacts. Because this study assessed the number of contacts per veteran regardless of intervention delivery modality, it is unclear how participation in a single modality (e.g., in-person visits, telephone care, video) or a combination of modalities is related to weight outcomes. Similarly, while participation in TeleMOVE! was accounted for, it was not possible to identify concurrent adjunctive weight management program participation (e.g., commercial weight management programs), and therefore their respective contributions to reported weight changes cannot be assessed.
There are several policy implications of our findings. The VHA should provide policy guidance that supports increasing participation of veterans who have initiated MOVE!. For example, an initiative to provide MOVE! staff with training in patient-centered health communication strategies could enhance the skills that impact patient engagement. In addition, future MOVE! programming could involve offerings that vary by intensity—e.g., 6-session series, 12-session series—so that veterans may choose, up front, what they are willing to commit to. At the patient level, results from this study could be used by providers as they engage in shared decision-making with veterans who are considering initiating, continuing, or discontinuing participation in MOVE!. While not all veterans may be ready or able to attend 12 or more sessions over the course of a year, a veteran who has attended six sessions, for example, may be encouraged to know that attendance at a few more sessions could have added benefit.
Overall, many veterans participating in the VHA’s MOVE! program have achieved clinically relevant weight loss, and this proportion differs by level of program engagement. Further characterization of key predictors of weight loss is needed to understand how participation may modify weight change and its implications for increasing engagement.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOCX 20 kb)
Acknowledgements
This work was funded by the VHA National Center for Health Promotion and Disease Prevention as part of ongoing evaluation of the National MOVE! Weight Management Program.
Compliance with Ethical Standards
Conflict of Interest
Ms. Chan and Dr. Raffa are employees of the Department of Veterans Affairs, and have no additional conflicts of interest to declare.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans of Affairs or the United States government.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-017-3992-3) contains supplementary material, which is available to authorized users.
REFERENCES
- 1.VA/DoD 2014 Clinical Practice Guideline for the Screening and Management of Overweight and Obesity. Available at: http://www.healthquality.va.gov/guidelines/CD/obesity/CPGManagementOfOverweightAndObesityFINAL041315.pdf. Accessed 18 July 2016.
- 2.Raffa SD, Maciejewski ML, Zimmerman LE, et al. A system-level approach to overweight and obesity in the Veterans Health Administration. J Gen Intern Med. This issue. [DOI] [PMC free article] [PubMed]
- 3.LeBlanc E, O’Connor E, Whitlock EP, Patnode C, Kapka T. Screening for and Management of Obesity and Overweight in Adults. Evidence Report No. 89. AHRQ Publication No. 11-05159-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 4.LeBlanc ES, O’Connor E, Whitlock EP, Patnode CD, Kapka T. Effectiveness of primary care-relevant treatments for obesity in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155:434–47. doi: 10.7326/0003-4819-155-7-201110040-00006. [DOI] [PubMed] [Google Scholar]
- 5.Moyer VA, on behalf of the U.S. Preventive Services Task Force Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:373–78. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- 6.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Kinsinger LS, Jones KR, Kahwati L, et al. Design and dissemination of the MOVE! Weight-management program for veterans. Prev Chronic Dis. 2009;6:A98. [PMC free article] [PubMed] [Google Scholar]
- 8.Kahwati LC, Lance TX, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration’s MOVE! Weight management program. Transl Behav Med. 2011;1:551–60. doi: 10.1007/s13142-011-0077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Littman AJ, Boyko EJ, McDonnel MB, Fihn SD. Evaluation of a weight management program for Veterans. Prev Chronic Dis. 2012;9:110267. doi: 10.5888/pcd9.110267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garvin JT. Weight reduction goal achievement with high-intensity MOVE!® treatment. Public Health Nurs. 2015;32:232–6. doi: 10.1111/phn.12194. [DOI] [PubMed] [Google Scholar]
- 11.Braun K, Erickson M, Utech A, List R, Garcia JM. Evaluation of Veterans MOVE! program or weight loss. J Nutr Educ Behav. 2016;48:299–303. doi: 10.1016/j.jneb.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 12.Romanova M, Liang LJ, Deng ML, et al. Effectiveness of the MOVE! Multidisciplinary weight loss program for veterans in Los Angeles. Prev Chronic Dis. 2014;10:E112. doi: 10.5888/pcd10.120325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dahn JR, Fitzpatrick SL, Llabre MM, et al. Weight management for veterans: examining change in weight before and after MOVE! Obesity (Silver Spring) 2011;19:977–981. doi: 10.1038/oby.2010.273. [DOI] [PubMed] [Google Scholar]
- 14.Hoerster KD, Lai Z, Goodrich DE, et al. Weight loss after participation in a national VA weight management program among veterans with or without PTSD. Psychiatr Serv. 2014;65:1385–1388. doi: 10.1176/appi.ps.201300404. [DOI] [PubMed] [Google Scholar]
- 15.Janney CA, Kilbourne AM, Germain A, et al. The influence of sleep disordered breathing on weight loss in a national weight management program. Sleep. 2015;39:59–65. doi: 10.5665/sleep.5318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Littman AJ, Damschroder LJ, Verchinina L, et al. National evaluation of obesity screening and treatment among veterans with and without mental health disorders. Gen Hosp Psychiatry. 2015;37:7–13. doi: 10.1016/j.genhosppsych.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 17.Taft T, Payvar S, Wool L. Effectiveness of the MOVE! program among African American veterans: weight loss and quality of life. Federal Pract. 2011;17–24.
- 18.Goldberg RW, Reeves G, Tapscott S, et al. MOVE! Outcomes of a weight loss program modified for veterans with serious mental illness. Psychiatr Serv. 2013;64:737–744. doi: 10.1176/appi.ps.201200314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masheb R, Lutes L, Kim H, et al. Weight loss outcomes in patients with pain. Clin Trials Investig. 2015;23:1778–1784. doi: 10.1002/oby.21160. [DOI] [PubMed] [Google Scholar]
- 20.Ackerman ET, Liss DT, Finch EA, et al. A randomized comparative effectiveness trial for preventing type 2 diabetes. Am J Public Health. 2015;105:2328–34. doi: 10.2105/AJPH.2015.302641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–6. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skoyen JA, Rutledge T, Wiese JA, Woods GN. Evaluation of TeleMOVE: a weight reduction intervention for Veterans with obesity. Ann Behav Med. 2015;49:628–33. doi: 10.1007/s12160-015-9690-7. [DOI] [PubMed] [Google Scholar]
- 23.Domecq JP, Prutsky G, Leppin A, et al. Drugs commonly associated with weight change: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100:363–70. doi: 10.1210/jc.2014-3421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garvin JT, Marion LN, Narsavage GL, Finnegan L. Characteristics influencing weight reduction among Veterans in the MOVE! program. West J Nurs Res. 2015;34:50–65. doi: 10.1177/0193945914534323. [DOI] [PubMed] [Google Scholar]
- 25.Gudzune KA, Doshi RS, Mehta AK, et al. Efficacy of commercial weight-loss programs: an updated systematic review. Ann Intern Med. 2015;162:501–12. doi: 10.7326/M14-2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Look AHEAD Research Group. Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145–54. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neiberg RH, Wing R, Bray GA, et al. Patterns of weight change associated with long-term weight change and cardiovascular disease risk factors in the Look AHEAD Study. Obesity (Silver Spring) 2012;20:2048–56. doi: 10.1038/oby.2012.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 20 kb)