Abstract
Advance care planning is relevant for homeless individuals because they experience high rates of morbidity and mortality. The impact of advance directive interventions on hospital care of homeless individuals has not been studied. The objective of this study was to determine if homeless individuals who complete an advance directive through a shelter-based intervention are more likely to have information from their advance directive documented and used during subsequent hospitalizations. The advance directive included preferences for life-sustaining treatments, resuscitation, and substitute decision maker(s). A total of 205 homeless men from a homeless shelter for men in Toronto, Canada, were enrolled in the study and offered an opportunity to complete an advance directive with the guidance of a trained counselor from April to June 2013. One hundred and three participants chose to complete an advance directive, and 102 participants chose to not complete an advance directive. Participants were provided copies of their advance directives. In addition, advance directives were electronically stored, and hospitals within a 1.0-mile radius of the shelter were provided access to the database. A prospective cohort study was performed using chart reviews to ascertain the documentation, availability, and use of advance directives, end-of-life care preferences, and medical treatments during hospitalizations over a 1-year follow-up period (April 2013 to June 2014) after the shelter-based advance directive intervention. Chart reviewers were blinded as to whether participants had completed an advance directive. The primary outcome was documentation or use of an advance directive during any hospitalization. The secondary outcome was documentation of end-of-life care preferences, without reference to an advance directive, during any hospitalization. After unblinding, charts were studied to determine whether advance directives were available, hospital care was consistent with patient preferences as documented in advance directives, and hospital resource utilization during admission. During the 1-year follow-up period, 38 participants who completed an advance directive and 37 participants who did not complete an advance directive had at least one hospitalization (36.9 vs. 36.2 %, p = 0.93). Participants who completed an advance directive were significantly more likely to have documentation or use of an advance directive in hospital, compared to participants who did not complete an advance directive (9.7 vs. 2.9 %, p = 0.047). Without reference to an advance directive, documentation of end-of-life care preferences occurred in 30.1 vs. 30.4 % of participants, respectively (p = 0.96), most often due to documentation of code status. There were no significant differences in resource utilization between admitted patients who completed and did not complete an advance directive. In conclusion, homeless men who complete an advance directive through a shelter-based intervention are more likely to have their detailed care preferences documented or used during subsequent hospitalizations.
Electronic supplementary material
The online version of this article (doi:10.1007/s11524-016-0105-2) contains supplementary material, which is available to authorized users.
Keywords: Advance directives, Homeless, End-of-life care
Introduction
Homelessness is a serious social problem that affects an estimated 3.5 million people in the USA [1], 4.1 million people in Europe [2], and 235,000 people in Canada in any given year [3]. People experiencing homelessness suffer from high levels of excess morbidity and are much more likely to be hospitalized than individuals in the general population [4–8]. They have standardized mortality ratios ranging from two to five times higher than the general population [7], and due to social isolation, they are less likely to have substitute decision makers identified or available in end-of-life care situations [9, 10]. Advance directives have been proposed to improve end-of-life care for homeless people [9, 11, 12].
Studies have shown that most homeless people are interested in discussing end-of-life care but rarely have the opportunity to complete an advance directive [10, 13]. In a randomized controlled trial involving a community-based sample of homeless people in Minneapolis, Minnesota, and a cohort study involving chronically homeless people in Toronto, Ontario, a one-on-one counselor-guided intervention led to advance directive completion rates of 37.9 and 50.2 %, respectively [14, 15]. However, neither study examined whether completed advance directives were useful in guiding future health care decisions. In addition, among the few end-of-life studies that have examined the impact of advance directive interventions on patient care outcomes, none have focused on individuals who were homeless or socially marginalized [16–18].
The primary objective of this study was to determine if chronically homeless individuals who chose to complete an advance directive through a shelter-based intervention were more likely to have an advance directive documented or explicitly affect processes of care during hospitalizations over a 1-year follow-up period, compared to homeless individuals who chose to not complete an advance directive. The secondary objective was to compare rates of documentation of end-of-life care preferences that did not explicitly reference an advance directive. Lastly, this study assessed whether hospital care was consistent with patient preferences as documented in advance directives, and whether there were differences in health resource utilization between admitted patients who completed and did not complete an advance directive.
Methods
Participants
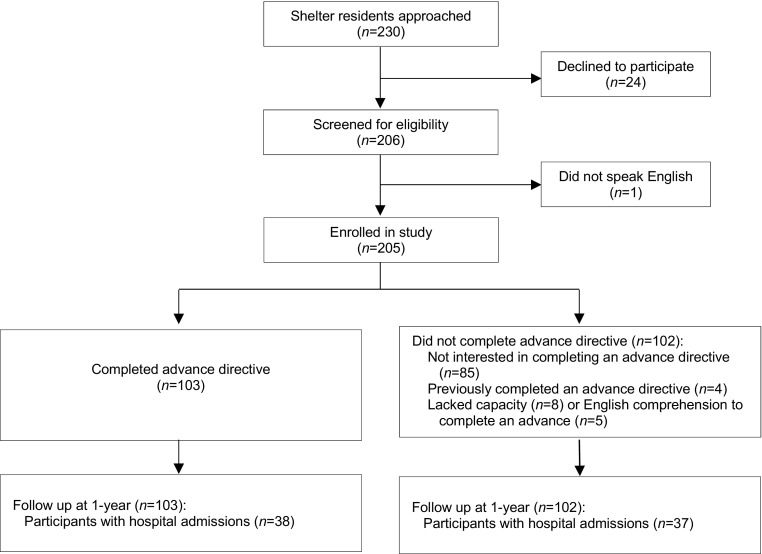
Details of the study design have been described previously [15]. Briefly, participants were recruited in the long-term programs of a large homeless shelter for men in Toronto, Canada, between April to June 2013. Long-term programs were targeted because among homeless individuals, those who are chronically homeless have higher levels of medical comorbidities, utilization of hospital services, and mortality [19]. Of 253 individuals residing in long-term programs at the shelter during the recruitment period, 230 were located and approached, and 205 (81.0 % of all residents and 89.1 % of those approached) gave written informed consent to participate in the study (Fig. 1).
Fig. 1.
Study recruitment and participants
Participants were invited to complete a written advance directive with a counselor. A group of three medical students and two non-specialist physicians served as counselors on advance directive completion. Each member was trained in end-of-life care planning, which involved a review of literature on advance directives and the unique end-of-life care needs of homeless persons [15]. The advance directive document included elements necessary for a legal advance directive or Power of Attorney for Personal Care in Ontario [20]. The advance directive was comprised of general decision aids to address the specific needs of homeless persons, a section to appoint a substitute decision maker (also known as an Attorney for Personal Care), and a tool that allowed individuals to decide which life-preserving treatments they would want to receive or forgo in the event of a life-threatening illness, if there was a possibility of returning to their current state of health [15]. The advance directive document used with study participants is provided (Supplemental file 1); a revised and refined version of the advance directive document, prepared after completion of the study, is provided (Supplemental file 2).
Availability of Advance Directives
Participants were provided with a copy of their completed advance directive and a wallet card with contact information about how their advance directive could be accessed if required. Copies of the completed advance directive were provided to the shelter, the primary health care team at the shelter, and/or the participant’s family physician, if the participant gave written consent to do so. All participants who completed an advance directive gave permission for the document to be made available to their health care providers in the event of future hospitalization.
At the end of the study recruitment period, physicians and staff in the divisions of Emergency Medicine, General Internal Medicine, and Critical Care at the three acute care hospitals closest to the shelter (hospitals A, B, and C, all located within a 1.0 mile radius from the shelter) were informed that if they were providing care to a shelter resident, they could contact the research team or the primary health care team at the shelter to obtain the patient’s advance directive if one had been completed. At hospital A, which is closest to the shelter and provides the majority of emergency and inpatient care for shelter residents, electronic copies of completed advance directives were placed on a secure hospital server that was accessible only to attending staff physicians and social workers in the divisions of Emergency Medicine, General Internal Medicine, and Critical Care. If a staff physician or social worker was providing care for a study participant who had completed an advance directive, they were able to access the document directly from the secure server.
Outcomes
The pre-specified primary outcome was direct evidence that a participant’s advance directive had been made available to health care providers or had affected processes of care in the hospital. The pre-specified secondary outcome was documentation of the participant’s end-of-life care preferences or efforts by health care providers to ascertain these preferences, without any explicit reference to an advance directive.
The primary outcome was deemed to have occurred if any of the following pre-specified criteria were met: presence of a copy of an advance directive document in the hospital chart; documentation of the existence of an advance directive in medical notes or nursing admission intake forms; documentation explicitly citing the use of an advance directive to guide treatment decisions or ascertain the patient’s treatment preferences; identification of and/or efforts to contact a substitute decision maker with explicit reference to the use of an advance directive to identify the substitute decision maker; ethics consultation or legal intervention specifically due to the existence of an advance directive; or documentation of the existence of an advance directive that was non-operative or revoked before or during the hospitalization. The secondary outcome was deemed to have occurred if any of the following pre-specified criteria were met, in the absence of any explicit reference to an advance directive: documentation of the participant’s end-of-life care preferences; documentation of a discussion with the participant regarding end-of-life care preferences; identification of and/or efforts to contact a substitute decision maker; documentation of discussions with the participant’s family member regarding the patient’s end-of-life care preferences; documentation of the existence of and/or identification of an Attorney for Personal Care; or documentation of code status. The outcomes were selected based on a review of literature and our clinical experience of collecting such information in our setting [21–25]. If a participant had multiple hospitalizations, data were extracted separately for each hospitalization, and the individual was then classified as having or not having the primary outcome at least once during any of their hospitalizations. The same procedure was used for secondary outcomes.
Two approaches were used to assess whether hospital care was consistent with preferences documented in advance directives. First, hospitalizations during which an advance directive was explicitly used to guide the participant’s medical treatment were reviewed in detail. Second, when a substitute decision maker was mentioned in the hospital chart, it was determined if this person corresponded to the person named as the participant’s substitute decision maker in his advance directive.
A standardized form was used to collect the occurrence of primary and secondary outcomes. In addition, the forms collected background information on each hospital admission. This included hospital and ICU length of stay, diagnosis, discharge disposition, level of consciousness during admission, and whether life-sustaining treatments were received during admission. We focused on life-sustaining treatments that study participants who completed an advance directive through our counselor-guided intervention would have had an opportunity to state a preference (Supplementary file 1).
Identification of Hospitalizations and Chart Review
A search of electronic medical records was conducted using an online system to identify participants’ admissions at the three acute care general hospitals closest to the shelter (hospitals A, B, and C) and three additional hospitals located within a 7.5-mile radius of the homeless shelter. This was conducted at 1 year after the participant was enrolled in our study. This search of hospital records was based on the following personal identifiers: first name, last name, date of birth, and Ontario health card number.
Two researchers, blinded as to whether participants had completed an advance directive at the time of enrollment, independently reviewed the medical record for each hospitalization. A standardized data collection form was used to obtain information on utilization of health care services, clinical events, documentation of and use of advance directives during the hospitalization, identification of and efforts to contact substitute decision makers, and documentation of end-of-life care preferences. After two reviewers completed independent data collection for each participant, they met to identify any discrepancies in the data. Discrepancies were resolved by discussion between the reviewers or by arbitration with a third reviewer when necessary.
Statistical Analyses
Characteristics of participants who did and did not complete an advance directive were compared using chi-square tests for categorical variables and t tests for continuous variables. The chi-square test was used to compare the proportion of participants in each group who had the primary outcome. The same procedure was used for the secondary outcome. Because outcomes could only occur in individuals who were hospitalized at least once during the follow-up period, differences between the two groups could potentially be attributed to differences in the prevalence of hospitalization. We therefore compared the proportion of individuals who had at least one hospitalization among those who did and did not complete an advance directive. An additional analysis examined the proportion of individuals with the primary outcome and secondary outcome among the subset of participants with at least one hospitalization. The level of significance used for all tests was p = 0.05. Analyses were performed using SPSS version 20.0 (IBM Corp., Armonk, NY, USA).
Results
There were 205 participants in our study. From the participants, 103 individuals completed an advance directive through the counselor-guided intervention. The mean age of participants was 54 years. The majority of participants were chronically homeless, with 147 (72.8 %) reporting that their current episode of homelessness had lasted 12 months or longer. Of 205 study participants, 103 (50.2 %) completed an advance directive, and 102 (49.8 %) participants declined to complete an advance directive or lacked the capacity or English comprehension to complete an advance directive (Fig. 1). A total of four (2.0 %) participants reported that they had previously completed an advance directive. These individuals declined to participate in our intervention and update their advance directive and were included in the group of 102 participants who did not complete an advance directive through the study intervention. There were no significant differences in sociodemographic characteristics, self-reported health status, or self-reported use of health care services between the participants who did and did not complete an advance directive (Table 1).
Table 1.
Baseline characteristics of study participants
| Characteristic | Completed advance directive | Did not complete advance directive | p value |
|---|---|---|---|
| (n = 103) | (n = 102) | ||
| N (%) | N (%) | ||
| Age, mean (SD) | 55.8 (9.6) | 55.0 (10.9) | 0.54 |
| Ethnicity | |||
| White | 72 (69.9) | 72 (70.6) | 0.87 |
| Black | 10 (9.7) | 8 (7.8) | |
| First nations/aboriginal | 7 (6.8) | 7 (6.9) | |
| Asian | 10 (9.7) | 13 (12.7) | |
| Other | 4 (3.9) | 2 (2.0) | |
| Born in Canada | 69 (67.0) | 68 (66.7) | 0.96 |
| Marital status | |||
| Never married | 46 (44.7) | 45 (44.1) | 0.85 |
| Divorced | 49 (47.6) | 51 (50.0) | |
| Married/common law | 8 (7.8) | 6 (5.9) | |
| Education | |||
| 8th grade or lower | 9 (8.7) | 16 (15.7) | 0.34 |
| Some high school | 37 (35.9) | 41 (40.2) | |
| High school diploma | 23 (22.3) | 21 (20.6) | |
| Some college/university | 18 (17.5) | 15 (14.7) | |
| College/university degree | 16 (15.5) | 9 (8.8) | |
| Duration of current episode of homelessness, n (%)a | |||
| <12 months | 29 (28.2) | 26 (26.3) | 0.16 |
| 12–59 months | 47 (45.6) | 35 (35.4) | |
| ≥60 months | 27 (26.2) | 38 (38.4) | |
| Self-reported health statusb | |||
| Excellent | 8 (7.8) | 8 (7.9) | 0.18 |
| Very good | 18 (17.5) | 14 (13.9) | |
| Good | 27 (26.2) | 40 (39.6) | |
| Fair | 26 (25.2) | 26 (25.7) | |
| Poor | 24 (23.3) | 13 (12.9) | |
| Self-reported mental illnessb | 42 (40.8) | 37 (36.6) | 0.54 |
| Self-reported alcohol or drug addiction | 49 (47.6) | 41 (40.6) | 0.32 |
| Count of self-reported chronic conditionsb, c | |||
| 0 | 48 (46.6) | 52 (51.5) | 0.70 |
| 1 | 29 (28.2) | 30 (29.7) | |
| 2 | 18 (17.5) | 12 (11.9) | |
| ≥3 | 8 (7.8) | 7 (6.9) | |
| Past or current smokerd | 65 (69.1) | 64 (68.8) | 0.96 |
| Visited emergency department in past yearb | 78 (75.7) | 70 (69.3) | 0.30 |
| Admitted to hospital in past yearb | 62 (60.2) | 52 (51.5) | 0.21 |
| Has a family doctorb | 83 (80.6) | 77 (76.2) | 0.45 |
| Has any childrenb | 56 (54.4) | 42 (41.6) | 0.07 |
| Had any contact with children in past yeare | 32 (58.2) | 23 (59.0) | 0.94 |
| Had any contact with relatives in past yearf | 68 (67.3) | 61 (62.2) | 0.45 |
aData missing for three participants
bData missing for one participant
cChronic conditions were as follows: heart disease, lung disease, liver disease, diabetes, HIV/AIDS, and stroke
dData missing for 18 participants
eData missing for 4 of 98 participants who had children
fData missing for five participants
Of 205 participants, 75 (36.6 %) were admitted to hospital at least once during the 1-year follow-up period. These individuals had a total of 184 hospital admissions, with the most common diagnoses being chronic obstructive pulmonary disease exacerbation (n = 26), seizures (n = 15), pneumonia (n = 12), sepsis (n = 9), gastrointestinal bleeding (n = 9), alcohol withdrawal or intoxication (n = 9), and cirrhosis or liver failure (n = 9). There were no significant differences for reasons for admission between those who completed and did not complete an advance directive. There were 126 admissions (68 %) at hospital A, 29 admissions (16 %) at hospital B, 21 admissions (11 %) at hospital C (11 %), and 8 admissions (5 %) at two other hospitals. A total of seven participants (3.4 %) died in hospital.
As shown in Table 2, participants who completed an advance directive through the shelter-based intervention were significantly more likely to have explicit evidence that an advance directive had been made available to health care providers or had affected processes of care in the hospital (9.7 vs. 2.9 %, p = 0.047). This occurred in three participants who did not complete an advance directive through the shelter-based intervention; these individuals completed an advance directive after study enrollment but prior to or during a hospitalization. There was no significant difference in the proportion of participants with the secondary outcome among those who did and did not complete an advance directive through the shelter-based intervention (30.1 vs. 30.4 %, p = 0.96). This finding was largely due to the high rate of documentation of code status among all participants who were admitted to hospital (Table 2).
Table 2.
Outcomes among study participants
| Completed advance directive | Did not complete advance directive | p value | |
|---|---|---|---|
| (n = 103) | (n = 102) | ||
| N (%) | N (%) | ||
| Primary outcome | 10 (9.7) | 3 (2.9) | 0.047 |
| AD present in chart | 5 (4.9) | 1 (1.0) | |
| Existence of AD documented in medical notes, but AD not present in chart | 4 (3.9) | 1 (1.0) | |
| Existence of AD noted on admission intake form | 4 (3.9) | 1 (1.0) | |
| AD explicitly used to guide treatment decisions, as documented in medical notes | 2 (1.9) | 0 (0) | |
| Patient’s treatment preferences documented, with explicit reference to AD | 2 (1.9) | 0 (0) | |
| SDM identified, with explicit reference to use of AD to identify SDM | 3 (2.9) | 0 (0) | |
| SDM contacted or attempt made to contact SDM, with explicit reference to use of AD to identify SDM | 1 (1.0) | 0 (0) | |
| Ethics consultation or legal intervention due to existence of AD | 0 (0) | 0 (0) | |
| Existence of non-operative AD documented | 1 (1.0) | 0 (0) | |
| Secondary outcome | 31 (30.1) | 31 (30.4) | 0.96 |
| Patient’s EOL preferences documented, without explicit mention of AD | 3 (2.9) | 4 (3.9) | |
| Discussion with patient regarding EOL preferences documented, without explicit mention of AD | 4 (3.9) | 7 (6.9) | |
| SDM identified, without explicit mention of use of AD to identify SDM | 3 (2.9) | 10 (9.8) | |
| SDM contacted or attempt made to contact SDM, without explicit mention of use of AD to identify SDM | 4 (3.9) | 5 (4.9) | |
| Discussion with patient’s family member regarding patient’s EOL wishes, without explicit mention of AD or family member’s status as SDM | 2 (1.9) | 3 (2.9) | |
| Existence of Attorney for Personal Care noted on admission intake form, without explicit mention of AD | 1 (1.0) | 3 (2.9) | |
| Identity of Attorney for Personal Care documented, without explicit mention of AD | 3 (2.9) | 3 (2.9) | |
| Code status (e.g., full code, no CPR) documented, without explicit mention of AD | 31 (30.1) | 30 (29.4) |
AD advance directive, SDM substitute decision maker, EOL end-of-life
The proportion of participants with at least one hospital admission was almost identical among participants who did and did not complete an advance directive at the time of recruitment (36.9 vs. 36.3 %, p = 0.93). In analyses restricted to the subset of 75 participants who had at least one admission, the proportion of participants with the primary outcome was again significantly higher among participants who completed an advance directive through the shelter-based intervention than those who did not (26.3 vs. 8.1 %, p = 0.04). The proportion of participants with the secondary outcome was not significantly different in the two groups (81.6 vs. 83.8 %, p = 0.80).
Clinical events and interventions among study participants who were hospitalized are shown in Table 3. More than two thirds of participants had a decreased level of consciousness while in hospital, and an assessment of capacity was documented in about one-quarter of participants. Twenty participants (9.8 % of all participants and 26.7 % of those who were hospitalized) were admitted to the ICU at least once. Comparing those who did and did not complete an advance directive at the time of recruitment, there were no significant differences in the proportion admitted to ICU, proportion receiving specific interventions and procedures, total days in hospital, total days in ICU, or deaths in hospital (Table 3).
Table 3.
Clinical events and interventions among study participants who were hospitalized
| Completed advance directive | Did not complete advance directive | p value | |
|---|---|---|---|
| n = 38 | n = 37 | ||
| N (%) | N (%) | ||
| Decreased level of consciousness | 26 (68.4) | 26 (70.3) | 0.53 |
| Capacity assessment | 13 (34.2) | 8 (21.6) | 0.17 |
| ICU admission | 10 (26.3) | 10 (27.0) | 0.94 |
| Rapid response team | 4 (10.5) | 7 (18.9) | 0.30 |
| CPR | 1 (2.6) | 2 (5.4) | 0.54 |
| Mechanical ventilation | 4 (10.5) | 9 (24.3) | 0.12 |
| Non-invasive positive pressure ventilation | 2 (5.3) | 2 (5.4) | 0.98 |
| Dialysis | 0 (0) | 1 (2.7) | 0.31 |
| Tube feeding | 4 (10.5) | 6 (16.2) | 0.47 |
| Surgery | 6 (15.8) | 5 (13.5) | 0.78 |
| Blood transfusion | 6 (15.8) | 11 (29.7) | 0.15 |
| Number of admissions, mean (SD) | 2.2 (1.7) | 2.7 (3.4) | 0.33 |
| Total days in hospital, mean (SD) | 15.4 (18.0) | 24.4 (35.6) | 0.69 |
| Total days in ICU, mean (SD) | 8.4 (9.8) | 17.2 (9.0) | 0.09 |
| Death in hospital | 4 (10.5) | 3 (8.1) | 0.72 |
The advance directive was explicitly used to guide treatment decisions for two participants (1.9 % of all participants who completed an advance directive and 5.3 % of those who were hospitalized). One participant indicated a willingness to receive blood transfusions but no other life-sustaining treatments. These wishes were confirmed and respected during subsequent hospitalizations, and the patient died in hospital while receiving supportive care. Another participant stated in his advance directive that he did not want his life to be prolonged through the use of life support machines. During the follow-up period, the participant experienced a cardiac arrest and was resuscitated. Subsequent treatment decisions by the individual’s substitute decision maker and physicians were informed by the advance directive, and the individual ultimately died in hospital.
Among the 38 participants who completed an advance directive through the shelter-based intervention and were subsequently hospitalized, 5 participants had a substitute decision maker mentioned in their hospital charts. In 4 of these cases, the name of the substitute decision maker corresponded with the substitute decision maker specified in the participant’s advance directive. In the remaining case, the name of the substitute decision maker was not specified in the hospital record.
Discussion
In this study, 103 out of 205 homeless individuals completed an advance directive through a shelter-based counselor-guided intervention. These individuals were significantly more likely to have an advance directive made available to health care providers and affect processes of care during subsequent hospitalizations. Over a 1-year follow-up period, the advance directive was explicitly referenced in the chart of 9.7 % of participants (26 % of those who were hospitalized) and had a direct impact on treatment decisions in 1.9 % of the participants (5.3 % of those who were hospitalized). Our findings demonstrate that when homeless persons have the opportunity to prepare advance directives and identify preferred substitute decision makers, health care professionals can use these in providing patient-centered care.
The urgent need for advance directive interventions for chronically homeless individuals is highlighted by the fact that over the course of a single year, 37 % of all study participants were admitted to hospital, and nearly 70 % of those admitted suffered from a decreased level of consciousness, where informed consent would be problematic. Furthermore, 10 % were admitted to ICU, and more than 3 % died. Indeed, given the high rates of morbidity and mortality within our study population, we were originally aiming to achieve higher rates of advance directive completion through our counselor-guided intervention.
This study substantially expands upon current knowledge on interventions for advance care planning, especially for homeless and other disadvantaged populations. Very few studies have evaluated the ability of end-of-life care decision aids and advance directives to improve decision making [18, 26, 27]. One study has prospectively evaluated the ability of an advance care planning intervention for in-hospital elderly patients to increase the likelihood of the patient’s wishes being honored during hospitalization [23]. These investigators found that 86.2 % of patients who completed the intervention and subsequently died had their end-of-life wishes known and followed. The intervention involved multiple meetings with the patient and discussions with family members; in contrast, our intervention involved a single encounter with a highly disadvantaged population in a community setting.
Previous research has found a significant association between written advance directives and decreased resource utilization [28]. In our study, individuals who completed an advance directive had lower mean ICU length of stay, rates of CPR, and mechanical ventilation. Although not statistically significant, the differences may be related to the aggressive care patients often receive by default in the absence of advance directives. In addition, the costs involved with costly interventions like mechanical ventilation, CPR, and hospitalization appear to make these findings clinically and socially significant [29]. The clinically applicability of these findings are underscored by the higher proportion of individuals in our study requiring ICU admission, rapid response teams, and life-sustaining interventions in comparison to the average population [30, 31]. Similarly, previous studies have shown that documenting preferences against resuscitation at end-of-life was associated with improved quality of care [23, 32]. This included a reduction in hospital length of stays [32, 33], lower incidence of death in an acute care setting, and increased utilization of hospice care services [32–35].
One of the major challenges to improving end-of-life care through advance directives is ensuring that hospital-based health care providers are aware of and have timely access to their patients’ advance directives; very few studies exist that demonstrate the link between advance directives and care given, especially in vulnerable populations [36–42]. In our study, only 26 % of individuals who completed an advance directive and were hospitalized within 1 year had definitive evidence in their hospital chart that their health care providers were aware of their advance directive. This low level of awareness occurred despite the creation of an in-hospital electronic database for advance directives and a concerted effort to inform health care professionals at nearby hospitals about the advance directive intervention. These findings highlight the need to make advance directives more readily available to hospital-based clinicians through systematic approaches such as automatic alerts within electronic medical record systems and secure online advance directive repositories. Documentation of end-of-life care preferences alone, however, is unlikely to improve patient outcomes [23]. For homeless persons, advance directive interventions should be linked to improved access to appropriate primary care, specialized services, and palliative care.
This study has limitations. This was a non-randomized study. Participants were recruited at a single shelter for homeless men, and our results may not be generalizable to other homeless populations and settings. Our findings reflect the effectiveness of our efforts to make completed advance directives available to hospital-based clinicians; results obtained in other settings could vary widely depending on the structure of the hospital system and the strategies used to make advance directives available. We did not adjust for potential confounders. This includes the possibility that the degree to which ADs were documented or utilized could be from institutional differences. Accordingly, we were unable to infer causality from our study. Our predefined primary and secondary outcomes were not based on a previously validated instrument for assessing the impact of advance directives on hospital care; however, to our knowledge, no such instrument exists. Outcomes were ascertained through chart reviews and were therefore dependent on the completeness of written documentation in hospital charts. Participants may have received care at hospitals other than the six hospitals where records were searched; however, our study findings and previous clinical experience suggest that the number of such hospitalizations is likely very small. Finally, the small number of primary outcomes, and borderline significant p values, limit the applicability of our findings and indicate the need for future studies on this topic.
This study demonstrates that a shelter-based advance directive intervention for homeless individuals can increase the likelihood that health care providers have access to specific information on patient preferences to guide health care decisions during subsequent hospitalizations. Future research should focus on refining strategies to improve access to advance care planning for homeless and other marginalized populations and to increase the accessibility and utilization of advance directives by substitute decision makers and health care providers.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 113 kb)
(PDF 393 kb)
Acknowledgments
The authors wish to thank the staff of the Seaton House for their collaboration and the residents of the Seaton House for their participation in this study.
Authors’ Contributions
Dr. Hwang had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Leung, Song, Hwang.
Acquisition, analysis, or interpretation of data: All authors.
Draft of the manuscript: Leung, To, Luong.
Critical revision of the manuscript for important intellectual content: All authors.
Study supervision: Hwang.
Author Information
Dr. Hwang holds the Chair in Homelessness, Housing, and Health at St. Michael’s Hospital and the University of Toronto. This study received no external funding.
Compliance with Ethical Standards
All participants provided informed and written consent to participate in the study. The Research Ethics Board at St. Michael’s Hospital and administrators at the shelter reviewed and approved the study protocol (reference number REB 12-375C).
References
- 1.National Coalition for the Homeless. How many people experience homelessness? http://www.nationalhomeless.org/publications/facts/How_Many.pdf (2007, Accessed 1 Sept 2014).
- 2.Employment Social Affairs and Inclusion. Staff working document: confronting homelessness in the European Union. Report no. SWD(2013) 42 final, 20 February 2013. Brussels, Belgium: European Commission.
- 3.Gaetz S, Gulliver T, Richter T. The state of homelessness in Canada 2014. http://homelesshub.ca/sites/default/files/SOHC2014.pdf (2014, Accessed 23 Aug 2016).
- 4.Larimer ME, Malone DK, Garner MD, et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–1357. doi: 10.1001/jama.2009.414. [DOI] [PubMed] [Google Scholar]
- 5.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 6.Baggett TP, Hwang SW, O’Connell JJ, et al. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med. 2013;173(3):189–195. doi: 10.1001/jamainternmed.2013.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–1540. doi: 10.1016/S0140-6736(14)61132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hwang SW, Wilkins R, Tjepkema M, et al. Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ. 2009;339:b4036. doi: 10.1136/bmj.b4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Norris WM, Nielsen EL, Engelberg RA, et al. Treatment preferences for resuscitation and critical care among homeless persons. Chest. 2005;127(6):2180–2187. doi: 10.1378/chest.127.6.2180. [DOI] [PubMed] [Google Scholar]
- 10.Song J, Ratner ER, Bartels DM, et al. Experiences with and attitudes toward death and dying among homeless persons. J Gen Intern Med. 2007;22(4):427–434. doi: 10.1007/s11606-006-0045-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Song J, Bartels DM, Ratner ER, et al. Dying on the streets: homeless persons’ concerns and desires about end of life care. J Gen Intern Med. 2007;22(4):435–441. doi: 10.1007/s11606-006-0046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song J, Wall MM, Ratner ER, et al. Engaging homeless persons in end of life preparations. J Gen Intern Med. 2008;23(12):2031–2036. doi: 10.1007/s11606-008-0771-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McNeil R, Guirguis-Younger M, Dilley LB. Recommendations for improving the end-of-life care system for homeless populations: a qualitative study of the views of Canadian health and social services professionals. BMC Palliat Care. 2012;11:14. doi: 10.1186/1472-684X-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song J, Ratner ER, Wall MM, et al. Effect of an end-of-life planning Intervention on the completion of advance directives in homeless persons: a randomized trial. Ann Intern Med. 2010;153(2):76–84. doi: 10.7326/0003-4819-153-2-201007200-00003. [DOI] [PubMed] [Google Scholar]
- 15.Leung AK, Nayyar D, Sachdeva M, et al. Chronically homeless persons’ participation in an advance directive intervention: a cohort study. Palliat Med. 2015;29(8):746–755. doi: 10.1177/0269216315575679. [DOI] [PubMed] [Google Scholar]
- 16.Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28(8):1000–1025. doi: 10.1177/0269216314526272. [DOI] [PubMed] [Google Scholar]
- 17.Houben CHM, Spruit MA, Groenen MTJ, et al. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Dir Assoc. 2014;15:477–489. doi: 10.1016/j.jamda.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 18.Butler M, Ratner E, McCreedy E, et al. Decision aids for advance care planning: an overview of the state of the science. Ann Intern Med. 2014;161(6):408–418. doi: 10.7326/M14-0644. [DOI] [PubMed] [Google Scholar]
- 19.Toward understanding homelessness: the 2007 National Symposium on Homelessness Research. Washington (DC): National Symposium on Homelessness Research, http://aspe.hhs.gov/hsp/homelessness/symposium07/ (2007, Accessed Feb 6 2015).
- 20.Power of Attorney and “Living Wills”: questions and answers. Toronto (ON): Office of the Public Guardian and Trustee. http://www.attorneygeneral.jus.gov.on.ca/english/family/pgt/livingwillqa.pdf. (Accessed 23 July 2013).
- 21.Kish Wallace S, Martin CG, Shaw AD, et al. Influence of an advance directive on the initiation of life support technology in critically ill cancer patients. Crit Care Med. 2001;29(12):2294–2298. doi: 10.1097/00003246-200112000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Danis M, Southerland LI, Garrett JM, et al. A prospective study of advance directives for life-sustaining care. N Engl J Med. 1991;324(13):882–888. doi: 10.1056/NEJM199103283241304. [DOI] [PubMed] [Google Scholar]
- 23.Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hartog CS, Peschel I, Schwarzkopf D, et al. Are written advance directives helpful to guide end-of-life therapy in the intensivecare unit? A retrospective matched-cohort study. J Crit Care. 2014; 29(1): 128–133. [DOI] [PubMed]
- 25.Hammes BJ, Rooney BL, Gundrum JD, et al. The POLST Program: a retrospective review of the demographics of use and outcomes in one community where advance directives are prevalent. J Palliat Med. 2012; 15(1): 77–85. [DOI] [PubMed]
- 26.Ditto PH, Danks JH, Smucker WD, et al. Advance directives as acts of communication: a randomized controlled trial. Arch Intern Med. 2001;161(3):421–430. doi: 10.1001/archinte.161.3.421. [DOI] [PubMed] [Google Scholar]
- 27.Song MK, Kirchhoff KT, Douglas J, et al. A randomized, controlled trial to improve advance care planning among patients undergoing cardiac surgery. Med Care. 2005;43(10):1049–1053. doi: 10.1097/01.mlr.0000178192.10283.b4. [DOI] [PubMed] [Google Scholar]
- 28.Teno JM, Gruneir A, Schwartz Z, et al. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc. 2007;55(2):189–194. doi: 10.1111/j.1532-5415.2007.01045.x. [DOI] [PubMed] [Google Scholar]
- 29.Dasta JF, McLaughlin TP, Mody SH, et al. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266–1271. doi: 10.1097/01.CCM.0000164543.14619.00. [DOI] [PubMed] [Google Scholar]
- 30.Hill AD, Fan E, Stewart TE, et al. Critical care services in Ontario: a survey-based assessment of current and future resource needs. Can J Anaesth. 2009;56(4):2105–297. doi: 10.1007/s12630-009-9055-4. [DOI] [PubMed] [Google Scholar]
- 31.University of Manitoba Faculty of Medicine. The use of intensive care units in Manitoba. Manitoba Centre for Health Policy, http://mchp-appserv.cpe.umanitoba.ca/reference/ICU_4Pager_final_(20120416).pdf (2012, Accessed 10 Aug 2015)
- 32.Bischoff KE, Sudore R, Miao Y, et al. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc. 2013;61(2):209–214. doi: 10.1111/jgs.12105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chapman M, Johnston N, Lovell C, et al. Avoiding costly hospitalisation at end of life: findings from a specialist palliative care pilot in residential care for older adults. BMJ Support Palliat Care. 2016. doi:10.1136/bmjspcare-2015-001071 [DOI] [PubMed]
- 34.Baidoobonso S. Patient care planning discussions for patients at the end of life: an evidence-based analysis. Ont Health Technol Assess Ser. 2014;14(19):1–72. [PMC free article] [PubMed] [Google Scholar]
- 35.Schellinger S, Sidebottom A, Briggs L. Disease specific advance care planning for heart failure patients: implementation in a large health system. J Palliat Med. 2011;14(11):1224–1230. doi: 10.1089/jpm.2011.0105. [DOI] [PubMed] [Google Scholar]
- 36.The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT) JAMA. 1995;274(20):15105–1598. [PubMed] [Google Scholar]
- 37.Fagerlin A, Schneider CE. Enough. The failure of the living will. Hastings Cent Rep. 2004;34(2):30–42. doi: 10.2307/3527683. [DOI] [PubMed] [Google Scholar]
- 38.Holley JL, Hines SC, Glover JJ, et al. Failure of advance care planning to elicit patients’ preferences for withdrawal from dialysis. Am J Kidney Dis. 1999;33(4):688–693. doi: 10.1016/S0272-6386(99)70220-9. [DOI] [PubMed] [Google Scholar]
- 39.Levi BH, Green MJ. Too soon to give up: re-examining the value of advance directives. Am J Bioeth. 2010;10(4):3–22. doi: 10.1080/15265161003599691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lynn J, Goldstein NE. Advance care planning for fatal chronic illness: avoiding commonplace errors and unwarranted suffering. Ann Intern Med. 2003;138(10):812–818. doi: 10.7326/0003-4819-138-10-200305200-00009. [DOI] [PubMed] [Google Scholar]
- 41.Teno JM, Licks S, Lynn J, et al. Do advance directives provide instructions that direct care? SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. J Am Geriatr Soc. 1997;45(4):508–512. doi: 10.1111/j.1532-5415.1997.tb05179.x. [DOI] [PubMed] [Google Scholar]
- 42.Visser M, Deliens L, Houttekier D. Physician-related barriers to communication and patient- and family-centred decision-making towards the end of life in intensive care: a systematic review. Crit Care. 2014;18(6):604. doi: 10.1186/s13054-014-0604-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 113 kb)
(PDF 393 kb)