Abstract
Urban populations disproportionately experience poor sexual outcomes, including high rates of teenage pregnancy and sexually transmitted infections. However, the contribution of substance use across adolescence to poor sexual outcomes in young adulthood has not been investigated in depth, despite offering opportunities for more targeted prevention. This study aimed to estimate joint trajectories of adolescent alcohol and marijuana use to determine if they relate differently to four sexual outcomes: multiple sexual partners, sex without a condom, teenage pregnancy, and contraction of a sexually transmitted infection in young adulthood (by age 25). Data came from a longitudinal study of urban youth followed from age 6 to age 25, with annual assessments during adolescence and young adulthood (n = 608). The sample showed high levels of sexual risk, with young adults on average having sex without a condom once in the past month, 28.5% having multiple sexual partners in the past month, one quarter having contracted a sexually transmitted infection, and over 60% of the women being pregnant as a teenager and 36% of the men having gotten a partner pregnant. Applying longitudinal latent profile analysis to estimate joint trajectories of alcohol and marijuana use from grades 8–12, we identified four classes representing high dual use, moderate alcohol use, moderate alcohol use with increasing marijuana use, and non-use. Class membership differently predicted all four outcomes investigated with high dual users having the highest level of teenage pregnancy and the increasing marijuana trajectory having the highest risk of engaging with multiple sexual partners in the past month. Results suggest implications for both sexual risk and substance use prevention for urban youth.
Keywords: African Americans, Blacks, Cannabis, HIV/AIDS, Latent profile analysis, Longitudinal patterns, Substance use effects
Background
African Americans disproportionately experience negative sexual outcomes, particularly in young adulthood. They suffer from high rates of HIV/AIDS and other sexually transmitted infections (STIs) and disproportionately experience teenage pregnancies [5, 39, 50]. The morbidity and mortality associated with early parenting and STIs contribute greatly to racial disparities in health [10, 16, 17, 39].
Those in urban centers are especially at risk of negative sexual outcomes for multiple reasons, including greater exposure to STIs [1, 39]. Among urban youth, teenage pregnancy is more normative due to its higher rates [28]. These negative outcomes are further compounded in metropolitan areas by elevated rates of poverty, incarceration, dense sexual networks, discrimination, racial segregation, and lack of health insurance and regular sources of care [1, 9, 22, 50].
Numerous studies have examined the contribution of substance use to sexual health and have shown event-level causal effects as a result of impaired decision-making and disinhibition [33, 40, 42]. The research base has often focused on a single substance, typically alcohol, or substance use in general with little attention to common patterns of substance use among youth. Studies have shown that immediately after consuming alcohol, the likelihood of risky sexual activity increases, as alcohol is thought to decrease an individual’s ability to consider negative consequences [56]. Adolescent drinkers have been found to be more likely to report multiple sexual partners, inconsistent condom use, sexually transmitted infections, and unplanned pregnancy [8, 12, 34].
Studies have also demonstrated a longer-term association [46, 49]. For example, Stueve and O’Donnell [47] in a study of urban minority adolescents found that early adolescent drinking was associated with mid-adolescent sexual risk-taking. Those who initiated alcohol use by seventh grade were more likely to engage in unprotected sexual intercourse, have multiple sexual partners, be intoxicated or high during sexual intercourse, and become pregnant through mid-adolescence. Strachman and colleagues, [46] in a sample of Midwestern youth, demonstrated an association between early drinking and number of sexual partners 10 years later. These longitudinal associations suggest that early substance use may set an individual on a trajectory of disadvantage. In line with the life course perspective’s notion of cumulative disadvantage, [11, 14, 15] early substance use, particularly heavy use, can accentuate existing adversities and lead to hardship that accumulates over time. Thus, for at-risk urban youth, significant involvement with alcohol and marijuana may have broad, long-lasting consequences.
Early substance use has been shown to interfere with cognitive and social development, which may explain the later impact on sexual risk behavior [38, 53]. Alcohol and marijuana use also exposes adolescents to different social and sexual norms and networks, which may be particularly risky [18, 51]. The impact of these networks on sexual health outcomes may be especially salient in socially disadvantaged communities where there are fewer available male partners resulting from high mortality and incarceration rates [19].
Despite an increasing prevalence of marijuana use among Black youth that is not seen among White youth, [26, 32] the empirical base linking marijuana use with sexual risk behaviors and outcomes over time has not been studied as extensively as alcohol. Recent work suggests that marijuana too is associated with later sexual risk behaviors and outcomes, including inconsistent condom use, multiple sexual partners, and STI diagnoses [6, 7, 21]. The limited knowledge base shows inconsistent findings, particularly among Blacks, perhaps because marijuana’s interrelationship with alcohol is rarely considered. For example, Berger et al. [6] analyzed data from two waves of the National Longitudinal Study of Adolescent Health and found a consistent association between adolescent marijuana use and later self-reported STI risk among Whites but a weaker and non-significant association among Blacks.
Recently, researchers have begun to consider both marijuana and alcohol use’s association with sexual risk, estimating and reporting their individual contribution; however, these studies have concentrated on short-term effects and more advantaged populations (e.g., college students) [29, 41, 54], with less attention to urban adolescents, long-term effects, or joint patterns of use. Co-use may be particularly important to consider as use of alcohol together with marijuana may have a multiplicative effect on elevating risk [35, 48]. Guo et al., [21] in one of the few longitudinal studies of urban youth, provide insight into the association of separate trajectories of alcohol and marijuana with sexual risk outcomes. Analyzing data from a prospective cohort study, Guo et al. identified how four trajectories of adolescent marijuana use and four distinct trajectories of adolescent binge drinking predicted sexual risk behavior at age 21. They found early binge-drinking trajectories were related to the number of sexual partners at age 21 after controlling for marijuana use while adolescent marijuana use trajectories were significantly associated with both the number of sexual partners and inconsistent condoms use at age 21 after controlling for binge drinking. This finding suggests independent contributions of alcohol and marijuana patterns over time, but did not test joint effects. Swartzendruber et al., [48] in a rare examination of the interaction of alcohol and marijuana use, demonstrated the additional risk of co-use of alcohol and marijuana. In a sample of African American female adolescents, they found that those who used both alcohol and marijuana had an increased risk of pregnancy 18 months later compared to those who used marijuana or alcohol alone. Further, those who used both alcohol and marijuana also had an increased risk of acquiring a STI compared to those who used marijuana only.
Despite the demonstrated association between substance use and later sexual risk behavior for youth, significant gaps remain. For one, our understanding of the association of adolescent substance use and sexual risk behavior is less extensive for urban minority youth, who have disproportionately negative sexual outcomes. Second, much of our understanding relies on cross-sectional studies, or those that follow individuals over a relatively short portion of the life course. Identifying patterns of substance use across adolescence, and their association with later sexual risk behaviors and outcomes would allow for a more complete understanding of the developmental process by which substance use trajectories contributes to sexual risk, and this information is critical for prevention efforts. Third, much of this research has focused on a single substance (e.g., alcohol) or substance use in general and not considered patterns of dual use, despite alcohol and marijuana being commonly used together, and previous work suggesting patterns of dual use relate differentially to long-term outcomes [20, 48]. Fourth, in estimating long-term associations, studies have struggled to adequately take selection effects into account.
To address these gaps, the purpose of the current study is to identify the developmental relationship between patterns of alcohol and marijuana use during adolescence and sexual risk behaviors and outcomes in young adulthood among a sample of predominantly Black urban youth followed prospectively from ages 6 to 25. We test whether joint patterns of alcohol and marijuana use during grades 8 to 12 relate to four distinct outcomes: multiple sexual partners, inconsistent condom use, sexually transmitted infections, and teenage pregnancy, after taking into account early risk factors. We hypothesize that all substance use trajectories have worse sexual outcomes compared to nonuse with dual use and increasing patterns having the worst outcomes. We explore whether classes with marijuana use have worse outcomes than classes with alcohol only as our previous work with this cohort found marijuana combined with alcohol to be associated with worse substance use and crime outcomes than alcohol alone [20].
Methods
Sample
This study utilized data from an intervention trial that began in 1993 in an effort to improve academic performance and decrease aggressive behavior among children. (For more information on intervention effects, see [23, 24, 36, 55]). The initial sample of 678 children was representative of students entering first grade in one of nine Baltimore City public schools in the fall of 1993. Three classrooms in each of the nine schools were randomly assigned to one of the intervention conditions, and teachers and students were randomly assigned to classrooms. Youth were followed-up mostly annually until age 25; youth were not assessed in grades 3 and 4.
The analytic sample for the current study included 608 of the 678 children (90%) who had sufficient data over time for analysis. Both intervention and control students are included in the analysis. These individuals had (1) first grade teacher ratings of behaviors and academic achievement, (2) at least one annual report of past year frequency of marijuana and alcohol use during grades 8–12, and (3) at least one assessment of outcomes during the 7-year period following high school (approximately ages 19–25). Most of the sample (65.5%) participated in all five annual assessments in grades 8–12, whereas 63.5% participated in all seven assessments post high school graduation. Participants in the analytic sample (n = 608) did not differ from those excluded (n = 70) in terms of gender, intervention status, free or reduced-price school meals, or age in first grade.
The sample was relatively evenly split by gender (46.3% female), and the vast majority were Black (87.4%). Most (70.1%) were low income, as evidenced by receiving free or reduced price meals in first grade. This research was approved by the Institutional Review Board of the Johns Hopkins Bloomberg School of Public Health. Prior to age 18, signed consent was obtained from parents, while youth provided assent. After age 17, signed consent was obtained from each participant for each interview.
Measures
Adolescent substance use: Substance use data were collected using an audio-computer assisted interview in an effort to reduce social desirability bias and increase accuracy. Substance use was measured using items adapted from the Monitoring the Future survey [27]. Past-year frequency of use of alcohol and marijuana for grades 8–12 was collected on a 7-point scale (0 = none, 1 = once, 2 = twice, 3 = 3–4 times, 4 = 5–9 times, 5 = 10–19 times, 6 = 20–39 times, 7 = 40 or more times).
Sex without a condom: At each of the age 19–25 interviews, participants were asked how often in the past month, they had had sex without a condom. A mean was calculated across the interviews.
Multiple sexual partners: In each interview post-high school, participants reported on their number of sexual partners in the past month, including main partners, one time partners, acquaintance partners, friend partners, and unknown partners. These items were summed to create an overall total number of partners for each past month period. Those with any values greater than 1 were considered to have multiple sexual partners.
Sexually transmitted infections: Participants also reported any lifetime sexually transmitted infections (STIs). Any yes response between ages 19 and 25 was coded as having had a sexually transmitted infection post-high school.
Teenage pregnancies: Teenage pregnancies were based on a single question asked annually asking the participant’s age the first time they got someone pregnant or became pregnant. Ages less than 20 were considered a teen pregnancy.
Covariates: Models included gender, race, intervention status, free/reduced price meal status (an indicator of family economic status), and four teacher ratings of student academic performance and behavior in first grade based on the Teacher Observation of Classroom Adaptation Scale (TOCA-R, [57]). Academic progress was based on a single item in which first grade teachers rated students on a 6-point scale (1–6) with higher scores indicating better performance. Aggressive/disruptive behavior, attention/concentration problems, and hyperactivity were based on multiple questions and measured on the same 6-point scale with lower scored indicating better adaptation. The coefficient alphas for the three TOCA-R subscales included were 0.108 (aggressive/disruptive behavior), 0.97 (attention/concentration problems), and 0.80 (hyperactivity).
Analysis
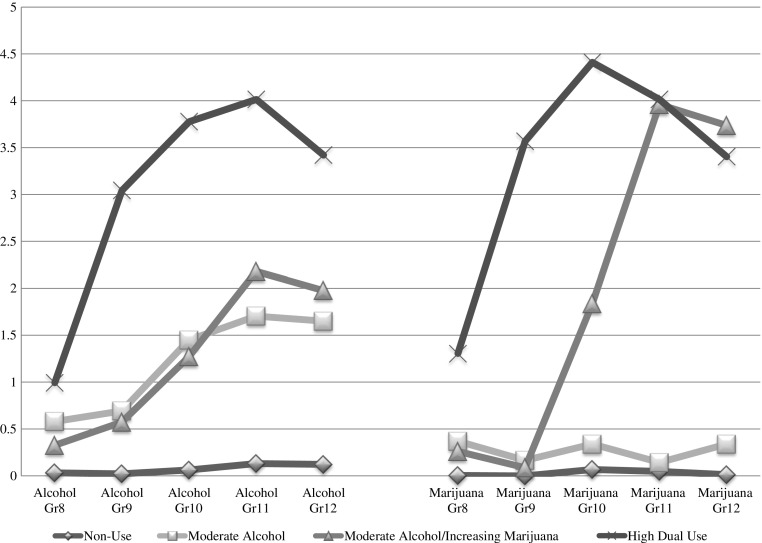
First, we conducted a longitudinal latent profile analysis to model the joint frequency of alcohol and marijuana use from grades 8 to 12 using Mplus Version 7.11 [37] in order to describe the patterns of annual marijuana and alcohol use over time. This approach assumes that individuals can be grouped into distinct classes based on their marijuana and alcohol use patterns over the five time points. To determine the number of latent classes, we compared goodness of fit indices, including the Bayesian Information Criterion, the Vuong Lo-Mendell-Rubin, and the Bootstrapped Loglikelihood Ratio Test, as well as compared the entropy for one through five-class models (see Table 1). A four-class solution was chosen based on the BIC and the Lo-Mendell-Rubin test, as well as class size and interpretability. This resulted in a “Non-Use” class (45.3%), a “Moderate Alcohol” class (29.4%), a “Moderate Alcohol/Increasing Marijuana” class (13.0%), and a “High Dual Use” class (12.3%) as shown in Fig. 1. The “Non-Use” class had little use of alcohol or marijuana from grades 8 to 12; the “Moderate Alcohol” class had moderate and increasing levels of alcohol use, and little to no marijuana use during this time. The “Moderate Alcohol/Increasing Marijuana” class had increasing levels of marijuana use across grades 10 through 12 and similar levels of alcohol to the “Moderate Alcohol” class. The “High Dual Use” class showed high levels of alcohol and marijuana use across high school.
Table 1.
Class enumeration test statistics
| Bayesian information criteria | Vuong-Lo-Mendel-Rubin Likelihood Ratio Test | Parametric Bootstrapped Loglikelihood Ratio Test | Entropy | ||||
|---|---|---|---|---|---|---|---|
| Number of classes | Statistic | Statistic | P value | Statistic | P value | ||
| 1 | 16881.27 | ||||||
| 2 | 12.559.71 | 1 vs 2 | 4392.07 | <0.001 | 4392.07 | <0.001 | 0.1088 |
| 3 | 11798.65 | 2 vs 3 | 841.58 | 0.003 | 841.58 | <0.001 | 0.892 |
| 4 | 11471.10 | 3 vs 4 | 388.06 | 0.046 | 402.24 | <0.001 | 0.893 |
| 5 | 11245.452 | 4 vs 5 | 296.42 | 0.072 | 296.96 | <0.001 | 0.887 |
Fig. 1.
Latent classes of substance use based on frequency of past year alcohol use and marijuana use from grades 8 through 12
This model was run without covariates in order to obtain the BCH weights that are used in the second step (i.e., models with distal outcomes and covariates); this weighted multiple group model avoids the class shifting that can occur in other three-step approaches [3, 4, 52]. These weights reflect the measurement error in the latent class variable, which leads to a significant reduction in bias as compared to hard classification approaches. This approach is the gold standard, performing particularly well when the variance of the auxiliary variable differs significantly across classes [3].
In a second model, utilizing the BCH weights, we tested for overall differences in the prevalence of distal outcomes across the alcohol and marijuana classes using a Wald Test and based pairwise comparisons on z-tests. These models control for the influence of covariates on both the latent class variable and also the outcomes of interest. The full information maximum likelihood estimation as implemented in Mplus 7.11 was used to adjust parameter estimates of to reflect missingness. This missing data approach is considered the appropriate method for handling data that can reasonably be assumed to be missing at random. Models were initially run separately for men and women in order to explore gender moderation. The final model included both genders, with gender as a covariate as no appreciable gender differences were observed in the association between latent class membership and distal outcomes when analyzed separately for men and women, which is consistent with previous work [13].
Results
As shown in Table 2 on average women had sex without a condom once during the past month (ages 18–25), while men engaged in condomless sex less often. Over 32% of the men and 24% of the women reported having multiple sexual partners in the past month during this young adult period. Over one third of women had contracted a sexually transmitted infection by age 25 compared with 16.8% of the men. Teenage pregnancy was high with over 61% of the women having become pregnant by age 19, and 36% of the men having impregnated a woman by age 19.
Table 2.
Young adults sexual risk by gender, ages 18–25
| Males (n = 327) |
Females (n = 281) |
Total (n = 608) |
|
|---|---|---|---|
| Mean frequency of sex without a condom in the past month | 0.85 | 1.17 | 1.01 |
| Multiple sexual partners past month (%) | 32.3 | 24.2 | 28.5 |
| Sexually transmitted infection (%) | 16.8 | 34.7 | 25.2 |
| Teenage pregnancy (%) | 36.0 | 60.7 | 47.6 |
Table 3 describes the classes on background variables. The “Moderate Alcohol/Increasing Marijuana” class is comprised of a greater percentage of boys (75.1%) compared to the others classes, which range from 46.0–51.4% male. The “High Dual Use” class has the lowest percentage of black youth (78.3%) and the greatest percentage of youth receiving free/reduced priced school meals (77.9%). Teacher ratings of behavior and academic performance are similar across the developmental trajectories of alcohol and marijuana use.
Table 3.
Description of alcohol and marijuana classes (n = 608)
| Non-use class (45.3%) | Moderate alcohol class (29.4%) | Moderate alcohol /increasing marijuana class (13.0%) | Dual use class (12.3%) | |
|---|---|---|---|---|
| Gender (% male) | 51.4 | 46.0 | 75.1 | 49.1 |
| Ethnicity (% Black) | 88.6 | 88.0 | 90.5 | 78.3 |
| Intervention status (% in intervention condition) | 69.4 | 68.6 | 54.0 | 72.7 |
| Free/reduced priced school meals (%) | 67.7 | 70.1 | 71.0 | 77.9 |
| Academic performance (mean) | 4.17 | 4.20 | 4.12 | 4.24 |
| Aggressive/disruptive behavior (mean) | 1.65 | 1.58 | 1.62 | 1.67 |
| Attention/concentration problems (mean) | 2.87 | 2.84 | 2.108 | 2.81 |
| Impulsivity (mean) | 2.25 | 2.32 | 2.28 | 2.39 |
Next, as shown in Table 4, we examined the association of the latent classes of adolescent alcohol and marijuana use with sexual risk outcomes. The overall chi-square indicated a statistically significant difference in mean past month frequency of sex without a condom across alcohol/marijuana classes (χ 2 = 16.815, p = 0.0008). The “Moderate Alcohol/Increasing Marijuana” (1.24) and the “Moderate Alcohol” (1.16) classes were significantly higher than the “Non-Use” Class (0.81).
Table 4.
Distal outcomes across four latent classes of alcohol and marijuana use in adjusted analyses: overall model statistics and pairwise comparisons
| Proportion | Standard error | Significant pairwise comparisons | |
|---|---|---|---|
| Past month frequency of sex without a condom, χ 2 = 16.815, p = 0.0008 | |||
| High dual use | 1.11 | 0.15 | |
| Moderate alcohol/increasing marijuana | 1.24 | 0.14 | Increasing marijuana vs. non-use, p < .001 |
| Moderate alcohol | 1.16 | 0.10 | Moderate alcohol vs. non-use, p = .007 |
| Non-use | 0.81 | 0.06 | |
| Multiple sexual partners, χ 2 = 18.388, p = 0.0004 | |||
| High dual use | 0.39 | 0.06 | Dual vs. non-use, p = .001 |
| Moderate alcohol/increasing marijuana | 0.46 | 0.06 | Increasing marijuana vs. non-use, p < .001 Increasing marijuana vs. moderate alcohol, p = .070 |
| Moderate alcohol | 0.29 | 0.04 | Moderate alcohol vs. non-use, p = .061 |
| Non-use | 0.20 | 0.03 | |
| Sexually transmitted infection, χ 2 = 20.267, p = 0.0001 | |||
| High dual use | 0.30 | 0.06 | Dual use vs. non-use, p < .001 |
| Moderate alcohol/increasing marijuana | 0.24 | 0.05 | Increasing marijuana vs. non-use, p = .002 |
| Moderate alcohol | 0.22 | 0.03 | Moderate alcohol vs. non-use, p = .002 |
| Non-use | 0.11 | 0.02 | |
| Teenage pregnancy, χ 2 = 35.153 p = 0.0001 | |||
| High dual use | 0.71 | 0.06 | Dual use vs. non-use, p < .001 Dual use vs. moderate alcohol, p = .011 |
| Moderate alcohol/increasing marijuana | 0.55 | 0.06 | Increasing marijuana vs. non-use, p < .001 |
| Moderate alcohol | 0.53 | 0.04 | Moderate alcohol vs. non-use, p = .002 |
| Non-use | 0.36 | 0.03 | |
Note: Models adjust for gender, intervention status, free/reduced price lunch, as well as academic performance, aggressive/disruptive behavior, attention/concentration problems, shy behavior, impulsivity, hyperactivity, and likeability/rejection as rated by first grade teachers
Similarly, having multiple sexual partners in the past month significantly differed across the four latent classes (χ 2 = 18.388, p = 0.0004). A lower percentage of the “Non-Use” class had sexual relationships with multiple partners in the past month than all three substance-using classes. That is, an estimated 20% of the “Non-Use” class had multiple sexual partners compared to 39% of the “High Dual Use” class, 46% of the “Moderate Alcohol/Increasing Marijuana” class, and 29% of the “Moderate Alcohol” class. Further, a greater percentage of the “Moderate Alcohol/Increasing Marijuana” class had multiple sexual partners in the past month compared to the “Moderate Alcohol” class (46 vs. 29%, p = .070).
The statistically significant overall chi-square also indicated differences across the substance use latent classes for sexually transmitted infections (χ 2 = 20.267, p = 0.0001), with the “Non-Use” class having significantly less STIs than all three substance use classes. Specifically, an estimated 30% of participants in the “High Dual Use” class, 24% of participants in the “Moderate Alcohol/Increasing Marijuana” class and 22% of participants in the “Moderate Alcohol” class had a sexually transmitted infection between ages 19 and 25 compared to 11% of participants in the “Non-Use” class.
Finally, teenage pregnancy also differed significantly across the latent classes (χ 2 = 35.153 p = 0.001) with all three substance use classes having higher levels of teenage pregnancy than the “Non-Use” class. In particular, an estimated 71% of the “High Dual Use” class, 55% of the “Moderate Alcohol/Increasing Marijuana” class, and 53% of the “Moderate Alcohol” class became pregnant as a teenager compared to an estimated 36% of the “Non-Use” class. Teenage pregnancy in the “High Dual Use” class was also significantly higher than in the “Moderate Alcohol” class.
Discussion
Previous studies have demonstrated a link between adolescent substance use and sexual risk behavior; however, few studies have focused on the dual use of alcohol and marijuana over time, estimated associations prospectively over a significant proportion of the life course in an urban sample or compared a variety of sexual risk outcomes, all the while controlling for earlier risk factors. Examining the association of four young adult sexual risk behaviors/outcomes with various patterns of adolescent marijuana and alcohol use among a predominantly Black, urban sample of youth, we found high levels of sexual risk behaviors compared to national statistics [31, 44]. Participants, on average, engaged in sex without a condom monthly from ages 18–25; 28.5% had multiple sexual partners in the past month during this young adult time period. Over one quarter had a sexually transmitted infection by age 25 and almost half had been pregnant or had gotten someone pregnant as a teenager. These pregnancy levels in this urban sample, in particular, are markedly higher than those found nationally and point out the urgency of preventive interventions with at-risk urban populations. National data estimate teenage pregnancy rates at about 5.7% among girls, [31] while the level in this sample was 60.7%. Clearly, regardless of substance use patterns, all at-risk urban youth would benefit from preventive interventions that focus on sexual risk behaviors.
As hypothesized, for just about all comparisons, the three substance use classes had poorer outcomes than the non-use class, including engaging in sex without a condom more frequently, having 1.5–2 times higher level of multiple sexual partners, two to three times the level of sexually transmitted infection, and higher levels of teenage pregnancy. Thus, developmental trajectories involving substance use across adolescence in general seem to be associated with differential sexual risk among urban young adults, consistent with previous work identifying longitudinal associations between adolescent substance use and later sexual outcomes [13, 21, 30, 46].
Our analyses, though, also allowed for a more nuanced look at specific dual use patterns that differentiated risk. One unique finding is that the “Moderate Alcohol/Increasing Marijuana” class was almost twice likely as the “Moderate Alcohol” class to report having multiple sexual partners in the past month during at least one of their young adult interviews. These classes are comparable on alcohol use across adolescents but differ on marijuana use with the “Moderate Alcohol/Increasing Marijuana” use class showing rapid increases from grades 10 to 11 and significant marijuana involvement in grades 11 and 12, suggesting a potential role of escalating marijuana use in uniquely increasing risk for sex with multiple partners. Similar results were found by Lowry and colleagues [33] in a nationally representative cross-sectional sample whereby high school students who used marijuana were four times more likely to report having four or more sexual partners compared to those who reported only alcohol or tobacco use in adjusted analyses. The mechanisms by which youth who use marijuana may have a greater risk of engaging in sex with multiple partners clearly needs further exploration and may have to do with unconventional attitudes, sensation seeking, social and sexual norms among urban marijuana using youth, or marijuana related sexual expectancies related to long-term use. More research is needed, in particular, to understand the characteristics of drug-using networks to better understand their potential role in elevated sexual risks, as these may be particularly relevant for Black adults [6].
Early, heavy dual use of marijuana and alcohol was associated with teenage pregnancy with an estimated 71% of those in the “High Dual Use” class either becoming pregnant (females) or impregnating a partner (males) compared to 55% of those in the “Moderate Alcohol/Increasing Marijuana” class and 53% of those in the “Moderate Alcohol” class. Nationally, Salas-Wright and colleagues [43] showed that pregnant teens were significantly more likely than non-pregnant adolescents to have met criteria for alcohol and cannabis disorders, which is often a result of heavier use. Their work suggests that substance use often continues during pregnancy; those findings combined with our findings of particularly high rates of pregnancy among alcohol and marijuana using youth suggest that importance of screening and joint intervention efforts that focus both on substance use and pregnancy prevention. Future research is needed to tease out potential reciprocal relationships, as substance use may contribute to and result from teenage pregnancies. In this study, the substance use trajectories and teenage pregnancy overlapped in time.
While the study had multiple strengths (e.g., longitudinal study spanning 20 years with annual assessments, a representative urban sample, focus on frequency of alcohol and marijuana, consideration of dual use patterns, examination of multiple sexual risk outcomes), a number of limitations are worth reviewing. For one, this is an observational study so causal conclusions are inappropriate; the causal nature of these associations require further study. Second, while this sample represented students entering Baltimore public schools in the fall of 1993, it is unclear how well these findings translate to other urban settings or more contemporary cohorts. Finally, because both substance use frequency and sexual risk outcomes were self-reported, we may have underestimated prevalence and associations.
Overall, findings suggest that specific patterns of alcohol and marijuana use during adolescence are associated with a higher risk of sexual risk behaviors and adverse sexual outcomes in young adulthood, including having sex without a condom, engaging in sex with multiple partners, and contracting a sexually transmitted infection post-high school compared to a nonuser class. These associations extend from adolescence into young adulthood, suggesting that developmental trajectories of substance use may impact poor sexual outcomes over time. We also found more serious substance use patterns among girls who became pregnant or boys who got a partner pregnant as a teenager.
Singer [45] describes substance abuse and sexually transmitted infections as “closely linked” and “interdependent threats to health and well being” that “constitute a major syndemic that already has taken a devastating toll on the lives of the urban poor” (p. 99). Thus, it is critical to reduce this link and provide prevention intervention for those urban youth at greatest risk of poor outcomes in adulthood. If associations prove to be causally related, substance use prevention efforts have the potential to decrease the burden of teenage parenting and sexually transmitted infections in at-risk urban communities. Therefore, it is important that substance use prevention programs monitor their impact on sexual risk behavior as Jackson and colleagues [25] found that few interventions have evaluated their impact on both substance use and sexual risk behavior.
Because of the strong link between substance use trajectory and a variety of sexual risk, a broader focus on shared risk and protective factors and joint programming is clearly needed. This study provides evidence that interventions for urban youth aimed at reducing sexual risk behaviors and outcomes clearly should consider the various patterns of adolescent alcohol and marijuana use as certain patterns of use may put urban youth at greatest risk of specific, adverse sexual outcomes.
Acknowledgments
Funding for this study was provided by the National Insitute on Drug Abuse (NIDA) R01-DA032550. The original data collection was funded by R01-DA11796 and R01-MH57005. Dr. Johnson’s work was supported by K01-DA31738. Dr. Matson’s work was supported by K01-DA035387.
References
- 1.Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005;191:S115–22. doi: 10.1086/425280. [DOI] [PubMed] [Google Scholar]
- 2.Andrade LF, Carroll KM, Petry NM. Marijuana use is associated with risky sexual behaviors in treatment-seeking polysubstance abusers. Am J Drug Alcohol Abuse. 2013;39(4):266–71. doi: 10.3109/00952990.2013.803112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: three-step approaches using Mplus. Struct Equ Model Multidiscip J. 2014;21:329–341. doi: 10.1080/10705511.2014.915181. [DOI] [Google Scholar]
- 4.Bakk Z, Tekle FB, Vermunt JK. Estimating the association between latent class membership and external variables using bias adjusted three-step approaches. In: Liao TF, editor. Sociological methodology. Thousand Oake, CA: SAGE publications; 2013. [Google Scholar]
- 5.Barrow RY, Newman LM, Douglas JM. Taking positive steps to address STD disparities for African-American communities. Sex Transm Dis. 2008;35(12Suppl):S1–S3. doi: 10.1097/OLQ.0b013e31818fbc92. [DOI] [PubMed] [Google Scholar]
- 6.Berger AT, Khan MR, Hemberg JL. Race differences in longitudinal associations between personal and peer marijuana use and adulthood sexually transmitted infection risk. J Addict Dis. 2012;31:130–142. doi: 10.1080/10550887.2012.665691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: trajectories, risk factors, and event-level relationships. Dev Psychol. 2012;48(5):1429–42. doi: 10.1037/a0027547. [DOI] [PubMed] [Google Scholar]
- 8.Bryant KJ. Expanding research on the role of alcohol consumption and related risks in the prevention and treatment of HIV/AIDS. Subst Use Misuse. 2006;41:1465–1507. doi: 10.1080/10826080600846250. [DOI] [PubMed] [Google Scholar]
- 9.Bunnell RE, Dahlberg L, Rolfs R, et al. High prevalence and incidence of sexually transmitted diseases in urban adolescent females despite moderate risk behaviors. J Infect Dis. 1999;180:1624–31. doi: 10.1086/315080. [DOI] [PubMed] [Google Scholar]
- 10.Center for Disease Control and Prevention Update to racial/ethnic disparities in diagnoses of HIV/AIDS – 33 states, 2001–2004. MMWR. 2007;56(09):189–193. [Google Scholar]
- 11.Dannefer D. Aging as intracohort differentiation: accentuation, the Matthew Effect, and the life course. Sociol Forum. 1987;2:211–36. doi: 10.1007/BF01124164. [DOI] [Google Scholar]
- 12.Dermen KH, Cooper ML, Agocha VB. Sex-related alcohol expectancies as moderators of the relationships between alcohol use and risky sex in adolescents. J Stud Alcohol. 1998;59:71–77. doi: 10.15288/jsa.1998.59.71. [DOI] [PubMed] [Google Scholar]
- 13.Duncan SC, Strycker LA, Duncan TE. Exploring associations in developmental trends of adolescent substance use and risky sexual behavior in a high-risk population. J Behav Med. 1999;22:21–34. doi: 10.1023/A:1018795417956. [DOI] [PubMed] [Google Scholar]
- 14.Elder GH. Life course dynamics: trajectories and transitions 1968–1980. Ithaca: Cornell: Cornell University Press; 1985. [Google Scholar]
- 15.Elder GH. The life course as developmental theory. Child Dev. 1998;69:1–12. doi: 10.1111/j.1467-8624.1998.tb06128.x. [DOI] [PubMed] [Google Scholar]
- 16.Fergusson DM, Woodward LJ. Maternal age and educational and psychosocial outcomes in early adulthood. J Child Psychol Psychiatry. 1999;40:479–89. doi: 10.1111/1469-7610.00464. [DOI] [PubMed] [Google Scholar]
- 17.Fraser AM, Brockert JE, Ward RH. Association of young maternal age with adverse reproductive outcomes. N Engl J Med. 1995;332:1113–17. doi: 10.1056/NEJM199504273321701. [DOI] [PubMed] [Google Scholar]
- 18.Galea S, Nandi A, Vlahov D. The social ecology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 19.Geronimus AT, Bound J, Waidmann TA, Hillemeier MM, Burns PB. Excess mortality among Blacks and Whites in the United States. NEJM. 1996;335:1552–1558. doi: 10.1056/NEJM199611213352102. [DOI] [PubMed] [Google Scholar]
- 20.Green KM, Musci RJ, Johnson RM, Matson PA, Reboussin BA, Ialongo NS. Outcomes associated with adolescent marijuana and alcohol use among urban young adults: a prospective study. Addict Behav. 2016;53:155–160. doi: 10.1016/j.addbeh.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guo J, Chung I, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. J Adoles Health. 2002;31:354–62. doi: 10.1016/S1054-139X(02)00402-0. [DOI] [PubMed] [Google Scholar]
- 22.Hallfors DD, Iritani BJ, Miller WC, Bauer DJ. Sexual and drug behavior patterns and HIV and STD racial disparities: the need for new directions. Am J Public Health. 2007;97:125–32. doi: 10.2105/AJPH.2005.075747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ialongo NS, Werthamer L, Kellam SG, Brown CH, Wang S, Lin Y. Proximal impact of two first-grade prevention interventions on the early risk behaviors for later substance abuse, depression and antisocial behavior. Am J Commun Psychol. 1999;27(5):599–641. doi: 10.1023/A:1022137920532. [DOI] [PubMed] [Google Scholar]
- 24.Ialongo NS, Poduska J, Werthamer L, Kellam S. The distal impact of two first-grade prevention interventions on conduct problems and disorder in early adolescence. J Emot Behav Disord. 2001;9(3):146–160. doi: 10.1177/106342660100900301. [DOI] [Google Scholar]
- 25.Jackson CA, Henderson M, Frank JW, Haw SJ. An overview of prevention of multiple risk behavior in adolescence and young adulthood. J Public Health. 2012;34(Supplement 1):i31–i40. doi: 10.1093/pubmed/fdr113. [DOI] [PubMed] [Google Scholar]
- 26.Johnson RM, Fairman B, Gilreath T, Xuan Z, Rothman EF, Parnham T, Furr-Holden CDM. Past 15 year trends in adolescent marijuana use: differences by race/ethnicity and sex. Drug Alc Depend. 2015;155:8–15. doi: 10.1016/j.drugalcdep.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnston LD, Bachman JG, O’Malley PM. Monitoring the future: questionnaire responses from the nation’s high school seniors, 1993. Ann Arbor, MI: Institute for Social Research, University of Michigan; 1995. [Google Scholar]
- 28.Kearney MS, Levine PB. Why is the teen birth rate in the United States so high and why does it matter? J Econ Perspect. 2012;26(2):141–66. doi: 10.1257/jep.26.2.141. [DOI] [PubMed] [Google Scholar]
- 29.Kerr DCR, Washburn IJ, Morris MK, Lewis KAG, Tiberio SS. Event-level associations of marijuana and heavy alcohol use with intercourse and condom use. J Stud Alcohol Drugs. 2015;76(5):733–737. doi: 10.15288/jsad.2015.76.733. [DOI] [PubMed] [Google Scholar]
- 30.Khan MR, Berger AT, Wells BE, Cleland CM. Longitudinal associations between adolescent alcohol use and adulthood sexual risk behavior and sexually transmitted infections in the United States: assessment of differences by race. Am J Public Health. 2012;102:867–76. doi: 10.2105/AJPH.2011.300373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kost K, Henshaw S. U.S. teenage pregnancies, births and abortions, 2010: National trends by age, race and ethnicity: Guttmacher Institute; 2014. Retrieved May 4, 2016, from http://www.guttmacher.org/pubs/USTPtrends10.pdf.
- 32.Lanza ST, Vasilenko SA, Dziak JJ, Butera NM. Trends among U.S. high school seniors in recent marijuana use and associations with other substances: 1976–2013. J Adolesc Health. 2015;57(2):198–204. doi: 10.1016/j.jadohealth.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lowry R, Holtzman D, Truman BI, Kann L, Collins JL, Kolbe LJ. Substance use and HIV-related sexual behaviors among US high school students: are they related? Am J Public Health. 1994;84(7):1116–20. doi: 10.2105/AJPH.84.7.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McEwan RT, McCallum A, Bhopal RS, Madhok R. Sex and the risk of HIV infection: the role of alcohol. British J Addict. 1992;87:577–84. doi: 10.1111/j.1360-0443.1992.tb01959.x. [DOI] [PubMed] [Google Scholar]
- 35.Metrik J, Cawell AJ, Magill M, Monti PM, Kahler CW. Sexual risk behavior and heavy drinking among weekly marijuana users. J Stud Alcohol Drugs. 2016;77(1):104–12. doi: 10.15288/jsad.2016.77.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Musci RJ, Bradshaw CP, Maher B, Uhl GR, Kellam SG, Ialongo NS. Reducing aggression and impulsivity through school-based prevention programs: a gene by intervention interaction. Prev Sci. 2014;15(6):831–40. doi: 10.1007/s11121-013-0441-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- 38.Newcomb MD, Bentler PM. Impact of adolescent drug use and social support on problems of young adults: a longitudinal study. J Abnorm Psychol. 1988;97(1):64–75. doi: 10.1037/0021-843X.97.1.64. [DOI] [PubMed] [Google Scholar]
- 39.Newman LM, Berman SM. Epidemiology of STD disparities in African American communities. Sex Transm Dis. 2008;35(12):S4–S12. doi: 10.1097/OLQ.0b013e31818eb90e. [DOI] [PubMed] [Google Scholar]
- 40.Poulin C, Graham L. The association between substance use, unplanned sexual intercourse and other sexual behaviours among adolescent students. Addiction. 2001;96(4):607–621. doi: 10.1046/j.1360-0443.2001.9646079.x. [DOI] [PubMed] [Google Scholar]
- 41.Ritchwood TD, DeCoster J, Metzger IW, Bolland JM, Danielson CK. Does it really matter which drug you choose? An examination of the influence of type of drug on type of risky sexual behavior. Addict Behav. 2016;60:97–102. doi: 10.1016/j.addbeh.2016.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rolf J, Nanda J, Baldwin J, Chandra A, Thompson L. Substance misuse and HIV/AIDS risks among delinquents: a prevention challenge. Int J Addict. 1990–1991; 25(4-A):533–559. [DOI] [PubMed]
- 43.Salas-Wright CP, Vaughn MG, Ugalde J, Todic J. Substance use and teen pregnancy in the United States: evidence from the NSDUH 2002–2012. Addict Behav. 2015;45:218–25. doi: 10.1016/j.addbeh.2015.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40(3):187–93. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- 45.Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inquiry Creative Sociol. 1996;24(2):99–110. [Google Scholar]
- 46.Strachman A, Impett EA, Henson JM, Pentz MA. Early adolescent alcohol use and sexual experience by emerging adulthood: a 10-year longitudinal investigation. J Adolesc Health. 2009;45:478–482. doi: 10.1016/j.jadohealth.2009.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stueve A, O’Donnell LN. Early alcohol initiation and subsequent sexual and alcohol risk behaviors among urban youths. Am J Public Health. 2005;95:887–893. doi: 10.2105/AJPH.2003.026567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Swartzendruber A, Sales JM, Brown JL, DiClemente RJ, Rose ES. Comparison of substance use typologies as predictors of sexual risk outcomes in African American females. Arch Sex Behav. 2016;45(1):63–72. doi: 10.1007/s10508-015-0518-0. [DOI] [PubMed] [Google Scholar]
- 49.Tapert SF, Aarons GA, Sedlar GR, Brown SA. Adolescent substance use and sexual risk-taking behavior. J Adoles Health. 2001;28(3):181–189. doi: 10.1016/S1054-139X(00)00169-5. [DOI] [PubMed] [Google Scholar]
- 50.Valentine JA. Impact of attitudes and beliefs regarding African American sexual behavior on STD prevention and control in African American communities: unintended consequences. Sex Transm Dis. 2008;35(12Suppl):S23–S29. doi: 10.1097/OLQ.0b013e31818d3cc7. [DOI] [PubMed] [Google Scholar]
- 51.Valente TW, Gallaher P, Mouttapa M. Using social networks to understand and prevent substance use: a transdisciplinary perspective. Subst Use Misuse. 2004;39(10–12):1685–1712. doi: 10.1081/JA-200033210. [DOI] [PubMed] [Google Scholar]
- 52.Vermunt JK. Latent class modeling with covariates: two improved three-step approaches. Polit Anal. 2010;18:450–469. doi: 10.1093/pan/mpq025. [DOI] [Google Scholar]
- 53.Volkow ND, Baker RD, Compton WM, Weiss SRB. Adverse health effects of marijuana. NEJM. 2014;370:2219–2227. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Walsh JL, Fielder RL, Carey KB, Carey MP. Do alcohol and marijuana use decrease the probability of condom use for college women? J Sex Res. 2014;51:145–158. doi: 10.1080/00224499.2013.821442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang Y, Storr CL, Green KM, Zhu S, Stuart EA, Lynne-Landsman S, Clemans K, Petras H, Kellam S, Ialongo N. The effect of two elementary school-based prevention interventions on being offered tobacco and the transition to smoking. Drug Alcohol Depend. 2012;120:202–208. doi: 10.1016/j.drugalcdep.2011.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–157. [PMC free article] [PubMed] [Google Scholar]
- 57.Werthamer-Larsson L, Kellam SG, Wheeler L. Effect of first-grade classroom environment on child shy behavior, aggressive behavior, and concentration problems. Am J Commun Psychol. 1991;19:585–602. doi: 10.1007/BF00937993. [DOI] [PubMed] [Google Scholar]