Abstract
Study Objectives:
To examine caffeine consumption from various dietary sources in a cohort of Australian children and the relationship between caffeine consumption, sleep, and daytime behavior.
Methods:
Children aged 8 to 12 years and their parents/guardians completed a battery of questionnaires. Children completed a caffeine questionnaire while parents completed questionnaires regarding demographics, sleep, and behavior.
Results:
The final sample consisted of 309 children (mean ± standard deviation [SD] age 10.6 ± 1.3 years, male = 48%) and corresponding parent reports. On average a mean ± SD 10.2 ± 17.4 mg/day of caffeine was consumed with a range of zero to 151 mg/day. Of the children who consumed caffeine (87% of the sample), the largest contributor was coffee and tea; making up 41% of total caffeine intake, and sodas (soft drinks) contributed to 40% of caffeine intake. Total caffeine consumption was significantly associated with sleep routine (r = 0.152); morning tiredness (r = 0.129); restless sleep (r = 0.113); and internalizing behavioral problems (r = 0.128). Using path analysis, caffeine consumption was positively associated with morning tiredness (β = 0.111, P = .050) which was positively associated with internalizing behaviors (β = 0.432, P < .001). The addition of sleep routine and restless sleep to the model led to a complete mediation of caffeine consumption on morning tiredness, as well as a partial mediation of the association between morning tiredness and internal behaviors.
Conclusions:
In 8- to 12-year-olds the primary sources of caffeine are coffee/tea and sodas. Overall mean caffeine consumption is small by adult standards but has an effect on behavior and sleep in children. The effect on behavior is mediated by disrupted sleep, indicating that caffeine is a contributor to sleep problems and related behavior in children.
Citation:
Watson EJ, Banks S, Coates AM, Kohler MJ. The relationship between caffeine, sleep and behavior in children. J Clin Sleep Med. 2017;13(4):533–543.
Keywords: behavior, caffeine, internalizing behaviors, morning tiredness, path analysis, restless sleep, school-aged children, sleep, sleep routine
INTRODUCTION
Caffeine is commonly found in chocolate, soda, energy drinks, coffee, and tea; of these products many are marketed toward children and adolescents using enticing slogans and branding.1,2 The 2007 Australian National Children's Nutrition and Physical Activity Survey collected data on 4,487 children aged 2 to 18 years and found that children aged 4 to 13 years consumed 7 to 47 mg of caffeine per day.3 More recently, the Australian Bureau of Statistics (ABS) reported that children aged 4 to 18 years in 2011–2012 consumed 6 to 52 mg of caffeine per day.4 This amount of caffeine consumption is within the suggested guidelines provided by other countries such as Canada5; however, even a modest amount of caffeine has been shown to affect sleep in children aged 13 years,6 and therefore could affect child behavior, academic performance, and well-being as a result.7
Few studies have intended to explore the relationship between caffeine and sleep in children younger than 12 years with the majority of studies focusing on adolescents or adults.8 Unlike adults and adolescents, school-aged children (5 to 12 years) may not drink caffeinated beverages to purposefully stay awake, but rather the consumption of caffeine may disturb their sleep, leading children to become sleepy during the day.9 In school-aged children, studies have found that higher caffeine consumption is associated with shorter total sleep time (TST)9–11 and a greater frequency of sleep problems.12 However, other studies have found that caffeine has no effect on TST,13 daytime sleepiness,14 or sleep problems.10 Other domains of sleep quality such as bedtime anxiety, morning tiredness, night arousals, sleep-disordered breathing, and bedtime routine have not previously been linked with caffeine consumption. These studies in children have not directly aimed to determine the association between caffeine and sleep, and many have used nonvalidated measures of caffeine.
BRIEF SUMMARY
Current Knowledge/Study Rationale: There are limited data available regarding caffeine intake and the relationship with sleep and behavior in children. Current data in the Australian child population suggests caffeine is being consumed in children under the age of 12 years.
Study Impact: In the current study a large portion of children reported caffeine intake, with soda, coffee, and tea being primary sources and caffeine intake was associated with reduced sleep quality, which was in turn related to internalizing behavior symptoms in children aged 8 to 12 years. This study is important for clinicians who manage children reporting sleep and/or behavioral problems.
In previous studies a range of methods have been used to collect caffeine data, for example, personal interviews,10 phone interviews,9 or a food frequency questionnaire.13 Some of these approaches may have underreported caffeine consumption as they have limited the range of products asked about,9,13,15 have focused on caffeine consumption only after 6:00 PM,11 or not included a clear description of methods used to measure caffeine intake.14
Sleep has a well-documented relationship with behavior in children with reduced or disrupted sleep predictive of cognitive and behavioral problems such as decreased attention, decreased memory, decreased school performance, decreased executive function, increased hyperactivity, increased aggression, increased sick days, increased symptoms of depression, and increased mood problems.16,17 Whether caffeine consumption has a similar effect on a child's behavior is unclear. Higher caffeine consumption, specifically coffee and soda, has been shown to be significantly associated with an increase in depressive symptoms (internalizing behaviors) in children aged 14 years.18 Additionally, girls in grades 6 through 10 who report high caffeine consumption are 1.4 times more likely to complain of headaches, stomachaches, and backaches (somatic complaints) compared with those who consumed lower levels of caffeine.19 Furthermore, increased caffeine consumption has been shown to be related to increased aggression in children aged 14 to 15 years,15,20 and is strongly related to increased violent behaviors and conduct disorder (externalizing behaviors) in children 10 to 12 years of age.21
To date, only one study has reported a three-way interaction between aspects of sleep, caffeine consumption, and behavior in children. Kristjansson et al.15 conducted structural equation modelling to investigate the direct effect of caffeine on aggressive behavior and the indirect effect with sleepiness and licit substance (cigarettes and alcohol) use in children aged 14 to 15 years. The study found that sleepiness was partly responsible for a relationship between caffeine and anger, suggesting 43% to 48% of the association between caffeine and anger was due to mediation by sleepiness and licit substance use. The unique contribution of sleepiness was not reported. Also, no study has investigated this relationship across a broader range of sleep factors or with the use of a validated assessment of caffeine consumption, sleep, and behavior in children.
The aims of this study were to determine (1) the amount and source of caffeine in 8- to 12-year-old Australian children, (2) the relationship between caffeine consumption and sleep time and sleep quality, (3) caffeine consumption and behavior, and (4) in an attempt to understand the interrelationship between the variables use structural equation modelling to determine if sleep acts as a mediator between caffeine consumption and behavior.
METHODS
Participants
Children were 8 to 12 years old and fluent in both reading and writing of English. They were excluded if they had diabetes or had been clinically diagnosed with, or were currently experiencing, an abnormality in diet, behavior or sleep (eg, attention deficit disorder, or diagnosed sleep disorders).
Measures
This study required both a parent and child to complete a questionnaire battery reflecting on the child's caffeine intake, behavior, and sleep. Questionnaires were collected on one occasion and took approximately 45 minutes for parents/guardians to complete and 10 minutes for the child to complete.
Parent Questionnaires
DEMOGRAPHIC: Parents or guardians were asked to provide information on postcode, their child's sex, date of birth, body mass, and height. Socioeconomic status (SES) was determined by postcode, using the deciles of the Socio-Economic Indexes for Areas (SEIFA), 2011.22 A SEIFA score is created using information variables such as household income, education, occupation, employment, and housing.23 This score is standardized against a national mean of 1,000 with a standard deviation of 100, which is then divided into decile rankings. A lower decile ranking indicates lower SES. Body mass index (BMI) z-scores for children and adolescents were calculated using Centers for Disease Control and Prevention criteria.24 A BMI z-score of 0.0 indicates the child is at the 50th percentile, a score greater than 1.0 is classified as overweight, and a score greater than 2.0 is classified as obese.
CHILD BEHAVIOR CHECKLIST FOR AGES 6 TO 18 YEARS (CBCL): The CBCL was used to measure each child's typical behavior.25 The CBCL consists of 113 questions and asks parents or guardians to consider their child's behavior over the past 6 months and rate each item as 0 = not true, 1 = somewhat or sometimes true, or 2 = often true or very often true of their child. The CBCL can be used to assess a range of behavior domains, which can be further condensed into the broad domains of (1) internalizing behaviors and (2) externalizing behaviors. Internalizing behaviors is a measure of emotional problems (Anxious/Depressed, Withdrawn/Depressed and Somatic Problems; problems that are mainly within the self). Externalizing behaviors is a measure of behavioral problems (Rule Breaking Behavior and Aggressive Behavior; problems that mainly inflict conflicts with other people and with their expectations for their child). Total behavior problems is a combination of both measures.
The current study used 109 items from the CBCL and excluded 4 items that were deemed problematic in this study and not essential for the described aims. The items were automatically assigned a 0; the excluded items were numbers 59 (plays with own genitalia in public), 60 (plays with own genitalia too much), 73 (sexual problems), and 96 (thinks about sex too much). Removed items 59 and 60 were associated with thought problems (Internalizing problems) and items 73 and 96 were associated with rule-breaking behavior (Externalizing behavior). A total problem score was computed by summing all 109 items answered. A high score on the scale (a t score greater than or equal to 70) indicates a clinical problem. The CBCL is reported to have test-retest reliability across all scales ranging from r = 0.80–0.94), as well as moderate to strong internal consistency (alpha = 0.72–0.97).25
PEDIATRIC SLEEP PROBLEM SURVEY INSTRUMENT (PSPSI): The PSPSI is a validated questionnaire that assesses sleep problems in school-aged children.26 It contains a total of 30 items and parents are asked to retrospectively report on their child's sleep behaviors over the past “typical” 7-day week. Items are rated on a four-point Likert scale of “never,” “rarely (once per week),” “sometimes (two to four times per week),” and “usually (five to seven times per week).” The sleep domains include: sleep routine (a regular and consistent pattern of activities before bed; 6 items), bedtime anxiety (fear of going to bed; 4 items), morning tiredness (being less alert in the morning; 4 items), night arousals (amount of times the child wakes during the night; 4 items), sleep-disordered breathing (snoring during the night; 4 items) and restless sleep (movement during sleep; 4 items). Within each scale a higher score indicates greater symptoms. The PSPSI is a validated tool in school-aged children,26 with internal consistency for each scale domain ranging between 0.63–0.80.26 Reported t scores were used in analyses, with a t score of 70 or higher indicating a score above the 95th percentile. Finally, an additional 2 sleep questions were added asking about the child's TST and sleep onset latency (SOL). Categorical data were collected for TST and SOL on Likert scales; TST: 9 to 11 hours, 8 to 9 hours, 7 to 8 hours, 5 to 7 hours, and less than 5 hours; SOL: less than 15 minutes, 15 to 30 minutes, 30 to 45 minutes, 45 to 60 minutes, and over 60 minutes. Test-retest reliability of the PSPSI is reported as moderate to strong (0.36–0.90), with moderate to strong internal consistency (alpha 0.6–0.8).26
PUBERTY CATEGORY SCORES QUESTIONNAIRE: Puberty category scores (PCS)27 were calculated to determine the level of pubertal development of each child. This questionnaire has 5 items relating to symptoms of puberty; for example, hair growth and pimples, which were assessed on a 4-point Likert scale (1 = not started, 2 = barely started, 3 = definitely started, 4 = seems complete). For girls the fifth question asks if they have started menarche, which required a “yes,” “no,” or “I don't know” response. A PCS of 2 to 3 indicates prepubertal growth and development; a PCS of 4 to 11 indicates the progression of puberty; and a PCS of 12 indicates sexual maturation has been completed. The measure has established validity and reliability27 and parent ratings are strongly correlated with child and pediatrician ratings of Tanner stages.27 It was left to each parent to determine whether the parent or the child completed the questionnaire. Internal consistency of the PCS shows reasonable reliability for both the self (α = 0.67–0.70) and parent (α = 0.68–0.78) versions. Correlations between PCS Tanner ratings and paediatrician assessments were considered strong.27
Child Questionnaire
CAFFEINE FOOD FREQUENCY QUESTIONNAIRE (C-FFQ): The C-FFQ is a self-report questionnaire designed to assess the average daily caffeine consumption over the previous week. The C-FFQ was specifically designed to capture caffeine intake from beverages and foods available in Adelaide, South Australia (location of study) between 2013 and 2015. The questions on the C-FFQ ask about the different beverages (eg, energy drinks, soft drinks (soda), both hot and cold coffee and tea, and chocolate-flavored milk) and foods (eg, chocolate) consumed in the previous 7 days. Caffeine content was obtained using Nutrient Tables for use in Australia28 and specific food manufacturer websites. Medications, supplements, and other sources of caffeine that are not diet-related were not included. The questionnaire requires participants to select the beverage or foods they consumed based on images of currently available products in Australia, indicating the specific brand, size, and the number of times over the past week each was consumed. The C-FFQ has been validated in Australian adults29 with successful piloting in a small group of children prior to this study. The C-FFQ calculates caffeine values, in mg/day, for total caffeine and the four subcategories of beverages and foods by calculating total caffeine consumption over the previous week and dividing by seven. Amount consumed on specific individual days is not determined. A Bland-Altman plot was used to determine validity and indicated fair agreement overall and for values below 300 mg of caffeine per day, the agreement improved. Test-retest reliability was strong for total caffeine (r = 0.90, P < .001) and for the four individual categories (r = 0.94–1.00, P < .001). Cohen κ showed reasonable agreement between the C-FFQ1 and C-FFQ2, κ = 0.65 (95%; CI: 0.52, 0.78), P < .001.29
Procedure
This was a cross-sectional study conducted in South Australia between October 2013 and July 2015. The study was approved by the Human Research Ethics Committees of the University of South Australia (Adelaide, Australia; HREC number: 30885), the Department for Education and Child Development, and the Catholic Education Office. Written informed consent was obtained from parents/guardians of all children prior to commencement. As children were 8 to 12 years old they did not provide their own consent; however, they were free to withdraw at any time. Recruitment of participants was completed through the community and schools.
Community Approach
Community recruitment was through fliers placed in the Adelaide metropolitan area. Locations included universities, hospitals, public libraries, community noticeboards, medical centers, and entertainment facilities. Interested participants either emailed or called for further information. Potential participants were then sent an information sheet and consent form, and all questionnaires with completed information returned in a postage-paid envelope that was provideed. Seventy-two questionnaire packets were distributed among the community and 53 complete packets were returned (a 74% acceptability rate).
School Approach
South Australian public and private schools were also approached from a variety of socioeconomic areas. Socioeconomic areas for South Australian public schools were determined using the 2012 Index of Educational Disadvantage released by the Department for Education and Child Development. If an individual school wanted to take part in the study, a member from the research team presented the study to the children and teachers and the school then distributed information sheets, consent forms, and parent questionnaires to all children aged 8 to 12 years. When questionnaires and consent forms were returned, the researcher returned to the school to supervise the children during class while they completed their questionnaires. Questionnaire packs were distributed across 17 schools; however, it is not possible to ascertain the exact number of questionnaire packs that were distributed across schools.
Statistical Analyses
For the C-FFQ, PSPSI, and CBCL a selection of N/A or a non-response resulted in an item score of zero to underestimate rather than overestimate problems in the sample. All data were checked for normality, and caffeine variables and some sleep variables (sleep routine, bedtime anxiety, night arousals, and sleep-disordered breathing) were found to be positively skewed. Total caffeine intake was log transformed and sleep routine was inversely transformed to correct to a normal distribution for parametric testing. However, caffeine intake data from individual beverage and food categories were skewed such that they could not be transformed into a normal distribution.
Mean, standard deviation, median, interquartile range, and range were calculated to describe the population and to show where the differences between populations occurred. Independent samples t tests were used to determine differences between groups and sex differences in caffeine consumption. To determine if there were differences in total caffeine consumption across each response category of TST and SOL, one-way analysis of variance was used.
Spearman correlations were used to assess relationships between caffeine, sleep, and behavior variables. A path analysis was also undertaken to determine if sleep factors mediated the relationship between caffeine intake and behavior. A path analysis allows reporting on direct and indirect pathways and provides estimates of explained variance between variables. The path analysis was conducted using Analysis of Moment Structures (AMOS, version 23.0, Amos Development Corp., Crawford, Florida, United States). The path analysis was guided by the Spearman correlation variables calculated. Bootstrap maximum likelihood estimation was used (1,000 samples). There were three missing values for SES, which was replaced by the sample mean. Modification indices were examined post hoc to ascertain if any potentially relevant pathways were omitted from the model. Significance was set at P < .05.
RESULTS
Study Participants
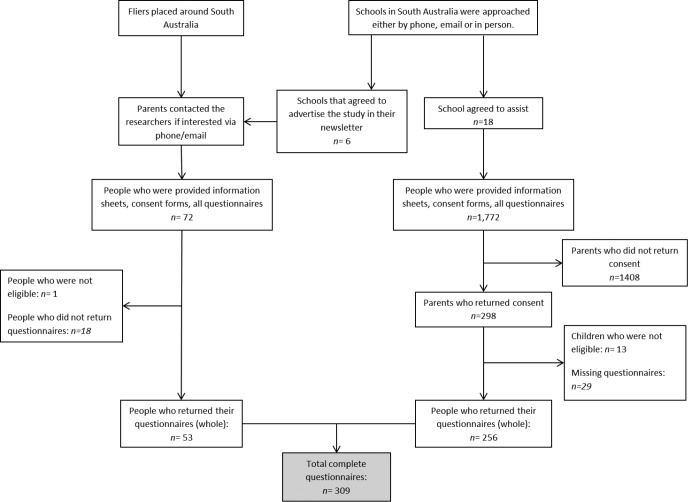
The majority of participants were recruited by approaching schools and children completed questionnaires under supervision during class. A total of 309 participants (Figure 1) were included in the final analysis, with an average age of 10.6 ± 1.3 years (mean ± standard deviation) and 47.9% male. Average puberty score was 5.2 ± 2.4 in females and 3.8 ± 1.3 in males; this was significantly different t299 = −6.317, P < .001. Caffeine consumption did not differ between boys and girls (P = .844). The average socioeconomic status rating was 6.9 ± 2.6 and on average participants were in the healthy BMI range (BMI z-score = 0.22 ± 1.63 kg/m2). Total caffeine intake was on average 10.2 ± 17.4 mg per day, which is equal to a 50-g solid milk chocolate bar or 30 mL of Red Bull. When considering only participants who consumed caffeine, the average increased to 11.8 ± 18.1 mg per day. A majority of the participants did not wet the bed (95%); sleep walk (90%), experience hyperhidrosis (97%), or report bruxism (91%). Furthermore, of the sample, 64.7% achieved 9 to 11 hours of sleep per night but only 20.7% required less than 15 minutes to fall asleep. Additional participant descriptive details are reported in (Table 1). Highest level of parental education was also reported, indicating all mothers completed high school, with 49.3% of the mothers completing a university degree and 27.2% completing a technical and further education degree. In contrast 1.3% of the fathers only completed primary school and the remaining fathers completed high school with 49.2% of fathers completing a university degree and 19.7% a technical and further education degree.
Figure 1. Description of recruitment strategies and participant flow from each source.
Table 1.
Caffeine variables, sleep variables, and behavior variables calculated from the Caffeine Food Frequency Questionnaire, Pediatric Sleep Problem Survey Instrument, and Child Behavior Checklist.
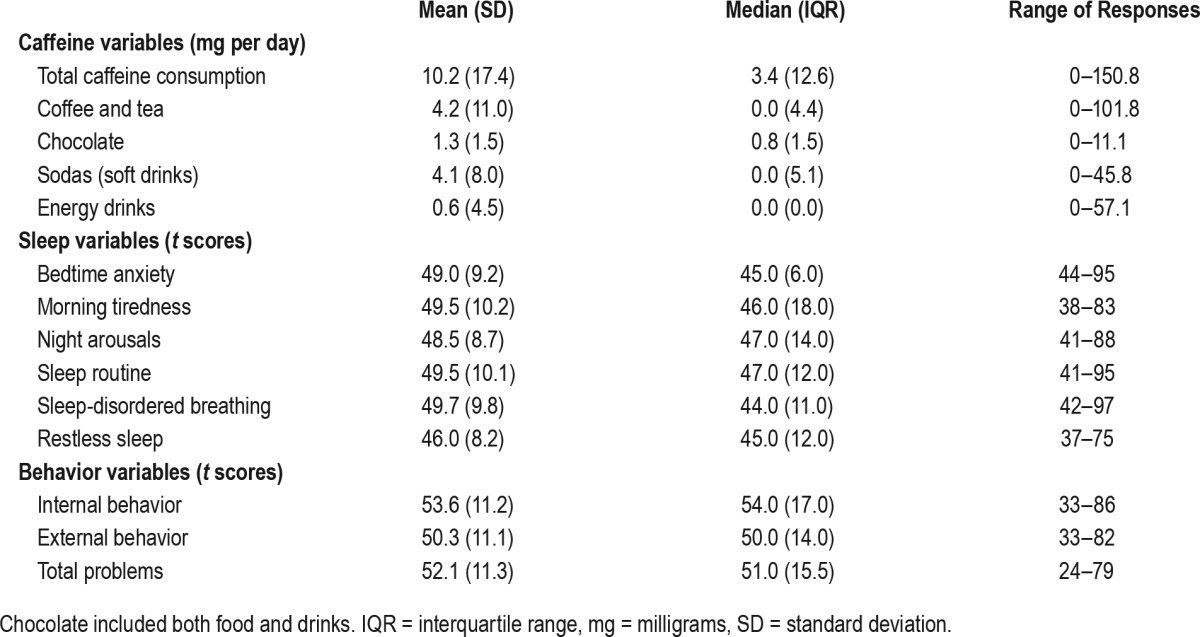
Caffeine Description
Overall, 87% of the sample consumed caffeine during the week before testing. Of the children who consumed caffeine, the largest contributor to caffeine consumption was coffee and tea; making up 41% of total caffeine intake. However, only 84 children (27.4%) reported having coffee and tea over the past week. Sodas (soft drinks) contributed to 40% of caffeine in-take, with 116 participants (37.8%) consuming this beverage type over the previous week. Only 8 participants consumed energy drinks, contributing to 13% of the caffeine intake. Foods and drinks containing chocolate were consumed by 245 participants (79% of sample); however, this contributed to only 6% of caffeine intake.
Caffeine consumption differed by amount of sleep, F3,305 = 7.55, P < .001. Post hoc analyses showed children who slept 9 to 11 h consumed significantly less caffeine compared to children who slept 7 to 8 hours per night (P < .001). There were no differences in caffeine consumption across SOL categories.
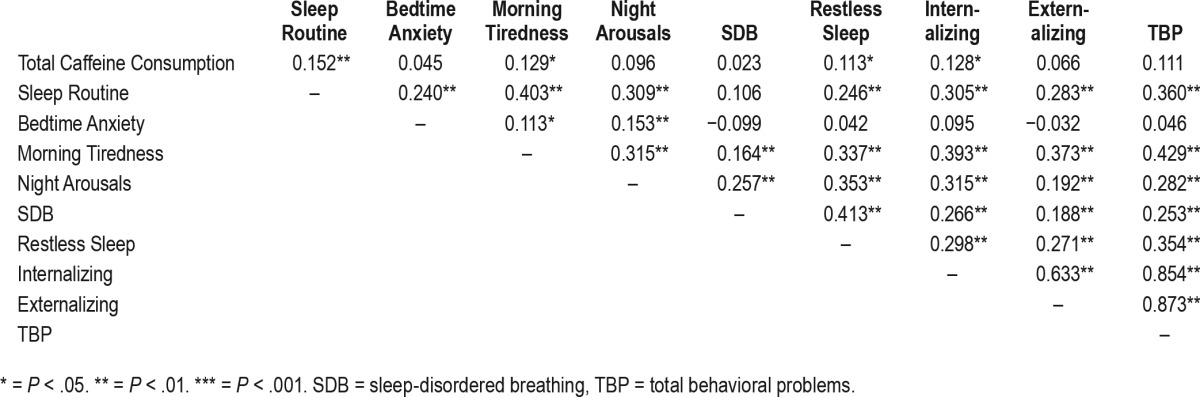
Correlations
Age, puberty, and SES were correlated with total caffeine, sleep, and behavioral variables. Increased age, higher puberty scores, and higher morning tiredness values were correlated with increased total caffeine consumption (r = 0.166, P = .004; r = 0.582, P < .001; r = 0.126, P = .027, respectively). Higher SES was correlated with decreased total caffeine consumption (r = −0.162, P = .004) and better internalizing (r = −0.119, P = .048), externalizing (r = −0.159, P = .007), and total behavioral problems (r = 0.167, P = .005). The results indicated that BMI Z-score was not correlated with any variables.
Higher caffeine consumption was significantly associated with worse scores in sleep routine (r = 0.152, P = .007), morning tiredness (r = 0.129, P = .023), and restless sleep (r = 0.113, P = .047). Caffeine consumption was not associated with night arousals (P = .092) and sleep-disordered breathing (P = .694). Regarding daytime behavior, higher total caffeine consumption was associated with worse internalizing behavioral problems (r = 0.128, P = .024), but not externalizing (P = .244) or total problems (P = .052; Table 2).
Table 2.
Spearman correlation values for all relationships between variables.
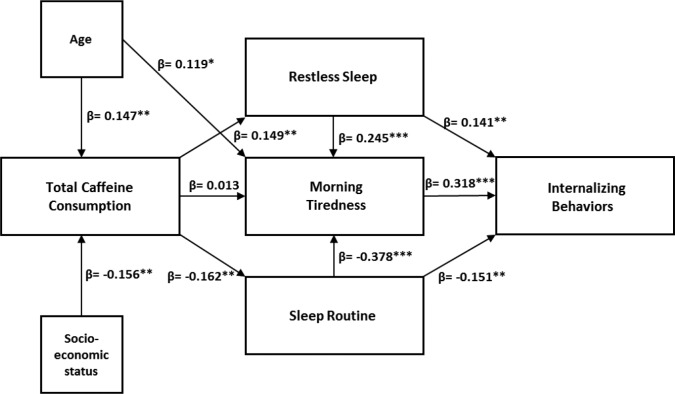
Path Analysis
A path analysis investigated the effect of caffeine intake on internalizing behaviors through its effect on sleep. Initially a model that included only a direct path from caffeine consumption to morning tiredness and morning tiredness to internalizing behavior was evaluated (Figure 2). As expected, total caffeine intake was positively associated with morning tiredness (β = 0.111, P = .050), which was positively associated with internalizing behavior (β = 0.432, P < .001).
Figure 2. Initial model.
Direct pathway analysis with beta (β) values between the controlled variables (age and socioeconomic status) and between total caffeine consumption, morning tiredness, and internalizing behaviors. * = P < .05. ** = P < .01. *** = P < .001.
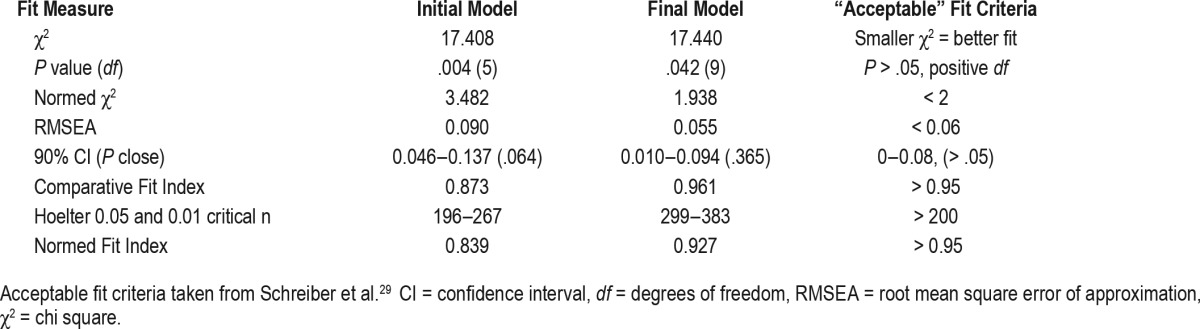
When the additional sleep variables associated with caffeine consumption (sleep routine [inverse] and restless sleep) were included in the model, the direct relationship between caffeine consumption and morning tiredness was no longer significant (β = 0.013, P = .794; Figure 3). However, significant paths from caffeine consumption to restless sleep (β = 0.149, P = .008) and sleep routine [inverse] (β = −0.162, P = .004) emerged. Both sleep routine and restless sleep were significantly related to morning tiredness (β = −0.378, P < .001; and β = 0.245, P < .001, respectively) and internalizing behavior (β = −0.151, P = .007; and β = 0.141, P = .008, respectively; Table 3), indicating mediation. It is important to note that the relationship between morning tiredness and internalizing behaviors also decreased when sleep routine and restless sleep were added to the model, indicating partial mediation for this aspect of the overall model. Measure of fit was determined by Schreiber et al.30 and the path analysis showed good overall fit (Table 4).
Figure 3. Final model.
Indirect pathway analysis with beta (β) values between the controlled variables (age and socioeconomic status) and between total caffeine consumption, sleep routine, restless sleep, morning tiredness and internalizing behaviors. A straight arrow represents a hypothesized effect. * = P < .05. ** = P < .01. *** = P < .001.
Table 3.
A pathway analysis summary, with standardized and unstandardized regression weights for the model.
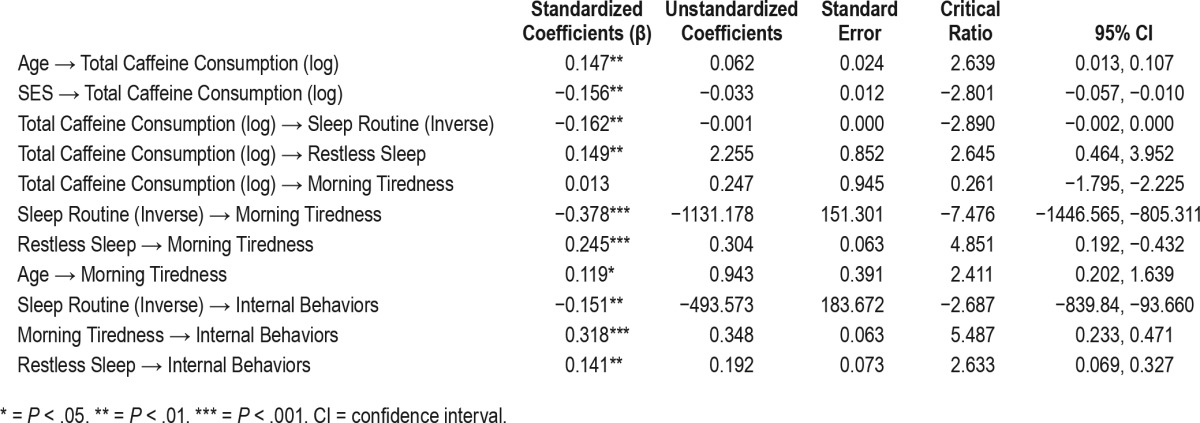
Table 4.
Summary of the Model fit indices.
DISCUSSION
Overall, this study found that most children in this cohort were consuming caffeine, and consumption ranged between zero to 151 mg per day, which is equivalent to 750 g of milk chocolate or 500 mL of Red Bull. Although coffee and tea contributed the greatest amount of caffeine per serving, the most commonly consumed caffeine source was chocolate. Caffeine consumption did not differ between sexes, but there were significant associations between caffeine consumption and age, SES, and puberty status. This is similar to results from previous studies that have needed to control for SES and age on caffeine consumption and adjusted for each in statistical tests.11,15,31–33 Furthermore, caffeine consumption was significantly associated with morning tiredness, sleep routine, and restless sleep, as well as problematic internalizing daytime behavior. Modelling of the associations between these factors indicated that sleep variables completely mediated the relationship between caffeine and behavior.
The first aim of the study was to determine the average caffeine intake and the sources of the caffeine consumption. Of the children who consumed caffeine, 41% of caffeine came from coffee and tea, 40% from sodas (soft drinks), 13% from chocolate food and drinks, and 6% from energy drinks. These findings were similar to previous Australian national data, which showed that for children aged 9 to 13 years 9% of caffeine intake was derived from chocolate, 38% from sodas (soft drinks), 5% from coffee, 19% from tea, and only 1% from energy drinks.4 Icelandic data15 assessing 7,348 subjects aged 14 to 15 years reported 76.3% of their sample consumed caffeine (as a beverage) and of the 4 beverages surveyed (soft drink, energy drink, coffee, and tea) the most consumed was soft drinks, followed by energy drinks. When considering beverages only in our sample, sodas (soft drinks) were also the most consumed; however, energy drinks were the least consumed.
The second aim was to determine if there was a relationship between caffeine consumption, sleep, and daytime behavior. Caffeine consumption was significantly related to sleep routine, morning tiredness, and restless sleep in children, with increasing caffeine consumption correlated with increasing sleep problems. There was also significant between-group differences in TST, but not SOL. Less TST as caffeine consumption increased is consistent with other literature in children9–11; similarly, no relationship with SOL was found in a sample of adolescents.34 With regard to broader sleep problems, sleep routine and restless sleep, specifically in relation to caffeine intake, have not been investigated previously in any age group. Li and colleagues32 found an increase in the number of nocturnal awakenings when children aged 5 to 12 years consumed caffeine after 6:00 PM. Pollak and Bright35 found that increased total caffeine consumption (including beverages, condiments and medications) increased wake after sleep onset in children aged 12 to 14 years. Similar to the results of the present study, Orbeta et al.33 showed that caffeine consumption increased the risk of morning tiredness by 1.8 times in older children and adolescents in grades 6 through 10; however, caffeine intake comprised only soda and coffee.
Finally, caffeine was significantly associated with internalizing behavior. Internalizing behavior is defined as an over-control of emotions that includes social withdrawal, demand for attention, feelings of worthlessness or inferiority, and dependency.36,37 Symptoms commonly classified as internalizing type include anxiety, depression, and psychosomatization. Previous studies have reported similar findings with increases in somatic complaints among caffeine consumers in grades 6 through 10.19 Furthermore, Fulkerson et al.18 indicated that increased caffeine consumption, specifically coffee and sodas, was significantly associated with an increase in depressive symptoms.18
No relationship was found with caffeine and externalizing problems in our sample, which is in contrast to study results by Kim20 and Kristjansson et al.15 who found that aggression in children was significantly related to total caffeine intake. The differing results could be due to different cultural approaches to anger, as the two previous studies were in Iceland15 and Korea20 whereas the current study was conducted in Australia.38,39 Furthermore, the way in which caffeine was measured varied across studies. The current study used a C-FFQ, which analyzed caffeine intake over the past 7 days and included caffeine from both beverages and foods. The C-FFQ provides the child with a list of all caffeinated products and sizes to assist in reporting and relying less on memory and previous knowledge. Kim20 asked participants whether they drank caffeine daily, requiring a simple “yes” or “no” response. Kristjansson et al.15 collected more detail and asked participants to report their daily caffeine consumption (beverages only) as the number of glasses or cups of coffee, tea, cola drinks, or energy drinks that contain caffeine. There were seven response options from “never” through to “six glasses/cups or more,” which therefore relied on the child knowing which beverages contained caffeine; data from this study were reported as the mean Likert scale response.
The final aim of this study was to determine if sleep mediates the relationship between caffeine and behavior. Sleep routine is determined by measuring the consistency of bedtime and sleep patterns26 and can be defined as behavioral practices that promote good sleep quality, adequate sleep duration, and full daytime alertness.40 Previously good sleep routine has been shown to have a positive effect on sleep quality.41 This model indicated that sleep routine and restless sleep completely mediate the relationship between caffeine consumption and morning tiredness but only partially mediated the relationship between morning tiredness and internalizing behaviors. This is important because it gives further insight into the importance of sleep and further understanding of the effect of caffeine on the relationship between sleep and behavior in children.
Overall, relatively little is known about the short-term and long-term health effects of caffeine in the pediatric population, and this study extends our knowledge to how caffeine plays a role in children's day-to-day sleep and behavior. The clinical implications extend to a growing need to consider caffeine in-take for children presenting with sleep and/or behavior issues. The C-FFQ29 used in this study provides a simple and effective means to estimate caffeine consumption in children in the clinical setting. Further study is required using objective measures of sleep and caffeine to further understand the mechanistic relationship between caffeine and sleep.
When interpreting these results it is important to consider other ingredients of popular caffeinated beverages and chocolate such as sugar, guarana, food additives, and theobromine, and their additional effects on sleep and behavior. Higher in-takes of added sugar have also been associated with shorter sleep duration42,43 in children aged 8 to 11 years. Further, research looking specifically at an association between sugar-sweetened beverages and sleep in children shows increased sugar-sweetened beverage consumption is associated with decreased sleep duration,43–45 and most consistently in males.46–48 The studies indicate further research on the short-term and long-term effect of sugar on sleep and sleepiness is required in children. Guarana contains large amounts of caffeine and could provide further caffeine-related effects on sleep and behavior that have not been measured in this study. The typical beverages that contain guarana were not consumed by many of this sample of participants and therefore are unlikely to contribute significantly to the results.
The foods and beverages that contain caffeine also contain a variety of food additives and other compounds. Food additives have been found to have a relationship with sleep disturbances previously. Rowe49 reported that food colors increased sleep disturbance and Kaplan et al.50 found that removing food additives from the diet of hyperactive children causes a reduction in sleep disturbance and shorter SOL. However, it is difficult to associate these changes with food additives specifically because many other aspects of the diet was changed. Finally, the chemical compound theobromine is primarily found in chocolate and has shown mixed results regarding its effect on sleep. Grandner et al. reported theobromine to increase daytime sleepiness.51 However, theobromine was consumed more by people sleeping for 7 to 8 hours than those sleeping more than 9 hours, with longer sleep time a potential indication of increased sleepiness.52
The strengths of this study include a sufficiently large sample size, naturalistic setting, and strong associations between valid and reliable measures. However, there are limitations that should be considered. First, one consideration is that the current study utilizes self-report and parental report surveys. Although previous research and survey validation show that self-reported caffeine use and sleep behavior can provide reliable estimates, it would be ideal to obtain an objective measure of both caffeine intake and sleep to substantiate the findings. Second, the timing of caffeine intake was not reported. This is important because the half-life of caffeine is estimated to be 4 to 5 hours based on reports in adults53 and therefore, theoretically, children consuming caffeine after school could be at increased risk for disturbed sleep compared with children having caffeine during or before school. Adult studies have investigated the effect of caffeine intake in the morning54 and evening,55 and although both have shown that caffeine intake negatively affects sleep, evening intake has the largest effect. Similar studies have not been conducted in children and it would be beneficial to be aware of the effect of caffeine consumption at different times of the day on sleep and behavior. Third, this study did not capture other factors such as physical activity that may influence sleepiness and energy intake in children.
Overall, this study has shown that caffeine intake in children aged 8 to 12 years is associated with reduced sleep quality, which in turn increases internalizing behavior symptoms. This is especially important with such high numbers of children in this age group who reportedly consume caffeine. In our sample it appears energy drink consumption is not the main contributor to caffeine intake, but it is important to be aware of the high numbers of children consuming soft drinks, coffee, and tea. This is likely to be an important consideration for clinicians dealing with children presenting with sleep and/or behavioral problems, as caffeine consumption could be playing a role in the presented problems. Furthermore, parents may be purchasing caffeinated drinks such as energy drinks, iced tea, or caffeinated sodas (soft drinks) without realizing the effect on sleep and behavior.
DISCLOSURE STATEMENT
Institution where the study was completed: Centre for Sleep Research, School of Psychology, University of South Australia, GPO Box 2471, Adelaide, South Australia 5001, Australia. E.W. received funding through a University of South Australia Post Graduate Award. This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank all of the families who participated and made this research possible and all the schools that assisted us. Furthermore, we thank the students who assisted on this study: Lee Priestley, Marie Georgopoulos, Susan Ward, Stephanie Cheng, Susan Pfeiffer, and Karen Hislop. Author contributions: E.W. developed the project, carried out the study, collected data, undertook analysis, and prepared the first draft of the manuscript. S.B., A.C., and M.K. assisted in developing the project, analysis, and revising the manuscript as well as supervising the study.
ABBREVIATIONS
- ABS
Australian Bureau of Statistics
- AMOS
Analysis of Moment Structures
- BMI
body mass index
- CBCL
Child Behavior Checklist
- C-FFQ
caffeine food frequency questionnaire
- NUTTAB
Nutrient Tables for use in Australia
- PCS
puberty category scores
- PSPSI
Pediatric Sleep Problem Survey Instrument
- SEIFA
Socio-Economic Indexes for Areas
- SES
socioeconomic status
- SOL
sleep onset latency
- TST
total sleep time
REFERENCES
- 1.Bramstedt KA. Caffeine use by children: the quest for enhancement. Subst Use Misuse. 2007;42(8):1237–1251. doi: 10.1080/10826080701208962. [DOI] [PubMed] [Google Scholar]
- 2.Warner M. A Jolt of Caffeine, by the Can. New York Times website. [Accessed January 3, 2017]. http://www.nytimes.com/2005/11/23/business/a-jolt-of-caffeine-by-the-can.html. Published November 23, 2005.
- 3.2007 Australian National Children's Nutrition and Physical Activity Survey - Main Findings. Australian Government Department of Health website. [Accessed January 3, 2017]. http://www.health.gov.au/internet/main/publishing.nsf/content/phd-nutrition-childrens-survey. Updated 2007.
- 4.4364.0.55.007 - Australian Health Survey: Nutrition First Results - Foods and Nutrients, 2011-12. Australian Bureau of Statistics website. [Accessed January 3, 2017]. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.007main+features12011-12. Published September 5, 2014. Updated December 21, 2015.
- 5.Food and Nutrition: Caffeine in Food. Health Canada website. [Accessed January 3, 2017]. http://www.hcsc.gc.ca/fn-an/securit/addit/caf/food-caf-aliments-eng.php. Updated February 16, 2012.
- 6.Lodato F, Araujo J, Barros H, et al. Caffeine intake reduces sleep duration in adolescents. Nutr Res. 2013;33(9):726–732. doi: 10.1016/j.nutres.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Owens JA, Mindell J, Baylor A. Effect of energy drink and caffeinated beverage consumption on sleep, mood, and performance in children and adolescents. Nutr Rev. 2014;72(Suppl 1):65–71. doi: 10.1111/nure.12150. [DOI] [PubMed] [Google Scholar]
- 8.Clark I, Landolt HP. Coffee, caffeine, and sleep: a systematic review of epidemiological studies and randomized controlled trials. Sleep Med Rev. 2016 Jan 30; doi: 10.1016/j.smrv.2016.01.006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Calamaro CJ, Yang K, Ratcliffe S, Chasens ER. Wired at a young age: the effect of caffeine and technology on sleep duration and body mass index in school-aged children. J Pediatr Health Care. 2012;26(4):276–282. doi: 10.1016/j.pedhc.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 10.Warzak WJ, Evans S, Floress MT, Gross AC, Stoolman S. Caffeine consumption in young children. J Pediatr. 2011;158(3):508–509. doi: 10.1016/j.jpeds.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 11.Li S, Zhu S, Jin X, et al. Risk factors associated with short sleep duration among Chinese school-aged children. Sleep Med. 2010;11(9):907–916. doi: 10.1016/j.sleep.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 12.Kristjansson AL, Sigfusdottir ID, Mann MJ, James JE. Caffeinated sugar-sweetened beverages and common physical complaints in Icelandic children aged 10-12 years. Prev Med. 2014;58:40–44. [PubMed] [Google Scholar]
- 13.Drescher AA, Goodwin JL, Silva GE, Quan SF. Caffeine and screen time in adolescence: associations with short sleep and obesity. J Clin Sleep Med. 2011;7(4):337–342. doi: 10.5664/JCSM.1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Calhoun SL, Vgontzas AN, Fernandez-Mendoza J, et al. Prevalence and risk factors of excessive daytime sleepiness in a community sample of young children: the role of obesity, asthma, anxiety/depression, and sleep. Sleep. 2011;34(4):503–507. doi: 10.1093/sleep/34.4.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kristjansson AL, Sigfusdottir ID, Allegrante JP, James JE. Adolescent caffeine consumption, daytime sleepiness, and anger. J Caffeine Res. 2011;1:75–82. [Google Scholar]
- 16.Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011;58(3):649–665. doi: 10.1016/j.pcl.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blunden SL, Beebe DW. The contribution of intermittent hypoxia, sleep debt and sleep disruption to daytime performance deficits in children: consideration of respiratory and non-respiratory sleep disorders. Sleep Med Rev. 2006;10(2):109–118. doi: 10.1016/j.smrv.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Fulkerson JA, Sherwood NE, Perry CL, Neumark-Sztainer D, Story M. Depressive symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Prev Med. 2004;38(6):865–875. doi: 10.1016/j.ypmed.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 19.Ghandour RM, Overpeck MD, Huang ZJ, Kogan MD, Scheidt PC. Headache, stomachache, backache, and morning fatigue among adolescent girls in the United States: associations with behavioral, sociodemographic, and environmental factors. Arch Pediatr Adolesc Med. 2004;158(8):797–803. doi: 10.1001/archpedi.158.8.797. [DOI] [PubMed] [Google Scholar]
- 20.Kim K. Association between Internet overuse and aggression in Korean adolescents. Pediatr Int. 2013;55(6):703–709. doi: 10.1111/ped.12171. [DOI] [PubMed] [Google Scholar]
- 21.Kristjansson AL, Sigfusdottir ID, Frost SS, James JE. Adolescent caffeine consumption and self-reported violence and conduct disorder. J Youth Adolesc. 2013;42(7):1053–1062. doi: 10.1007/s10964-013-9917-5. [DOI] [PubMed] [Google Scholar]
- 22.SEIFA by Postal Area Code (POA) Australian Bureau of Statistics website. [Accessed January 3, 2017]. http://stat.data.abs.gov.au/Index.aspx?DataSetCode=SEIFA_POA.
- 23.2033.0.55.001 - Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2011. Technical Paper. Australian Bureau of Statistics website. [Accessed January 3, 2017]. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/203 3.0.55.001main+features52011. Updated November 11, 2014.
- 24.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190. [PubMed] [Google Scholar]
- 25.Achenbach TM, Rescorla L. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: ASEBA; 2001. [Google Scholar]
- 26.Biggs S, Kennedy J, Martin A, van den Heuvel C, Lushington K. Psychometric properties of an omnibus sleep problems questionnaire for school-aged children. Sleep Med. 2012;13(4):390–395. doi: 10.1016/j.sleep.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 27.Carskadon MA, Acebo C. A self-administered rating scale for pubertal development. J Adolesc Health. 1993;14(3):190–195. doi: 10.1016/1054-139x(93)90004-9. [DOI] [PubMed] [Google Scholar]
- 28.NUTTAB 2010 Online Searchable Database. Food Standards Australia New Zealand website. [Accessed January 12, 2017]. http://www.foodstandards.gov.au/science/monitoringnutrients/nutrientables/nuttab/Pages/default.aspx.
- 29.Watson EJ, Kohler M, Banks S, Coates AM. Validation and reproducibility of an Australian caffeine food frequency questionnaire. Int J Food Sci Nutr. 2017 Jan 5; doi: 10.1080/09637486.2016.1268102. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 30.Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res. 2006;99(6):323–338. [Google Scholar]
- 31.James JE, Kristjansson AL, Sigfusdottir ID. Adolescent substance use, sleep, and academic achievement: evidence of harm due to caffeine. J Adolesc. 2011;34(4):665–673. doi: 10.1016/j.adolescence.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 32.Li L, Ren J, Shi L, et al. Frequent nocturnal awakening in children: prevalence, risk factors, and associations with subjective sleep perception and daytime sleepiness. BMC Psychiatry. 2014;14:204. doi: 10.1186/1471-244X-14-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Orbeta RL, Overpeck MD, Ramcharran D, Kogan MD, Ledsky R. High caffeine intake in adolescents: associations with difficulty sleeping and feeling tired in the morning. J Adolesc Health. 2006;38(4):451–453. doi: 10.1016/j.jadohealth.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 34.Astill RG, Verhoeven D, Vijzelaar RL, Someren EJ. Chronic stress undermines the compensatory sleep efficiency increase in response to sleep restriction in adolescents. J Sleep Res. 2013;22(4):373–379. doi: 10.1111/jsr.12032. [DOI] [PubMed] [Google Scholar]
- 35.Pollak CP, Bright D. Caffeine consumption and weekly sleep patterns in US seventh-, eighth-, and ninth-graders. Pediatrics. 2003;111(1):42–46. doi: 10.1542/peds.111.1.42. [DOI] [PubMed] [Google Scholar]
- 36.Achenbach TM, Edelbrock CS. The classification of child psychopathology: a review and analysis of empirical efforts. Psychol Bull. 1978;85(6):1275–1301. [PubMed] [Google Scholar]
- 37.McCulloch A, Wiggins RD, Joshi HE, Sachdev D. Internalising and externalising children's behaviour problems in Britain and the US: relationships to family resources. Child Soc. 2000;14(5):368–383. [Google Scholar]
- 38.Maxwell JP, Sukhodolsky DG, Chow CC, Wong CF. Anger rumination in Hong Kong and Great Britain: validation of the scale and a cross-cultural comparison. Pers Individ Dif. 2005;39:1147–1157. [Google Scholar]
- 39.Ramírez JM, Fujihara T, Goozen SV. Cultural and gender differences in anger and aggression: a comparison between Japanese, Dutch, and Spanish students. J Soc Psychol. 2001;141(1):119–121. doi: 10.1080/00224540109600528. [DOI] [PubMed] [Google Scholar]
- 40.American Sleep Disorders Association. International Classification of Sleep Disorders: Diagnostic and Coding Manual. 1st ed. Rochester, MN: American Sleep Disorders Association; 1990. [Google Scholar]
- 41.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115(1 Suppl):257–265. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kjeldsen JS, Hjorth MF, Andersen R, et al. Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in Danish school children. Int J Obes (Lond) 2014;38(1):32–39. doi: 10.1038/ijo.2013.147. [DOI] [PubMed] [Google Scholar]
- 43.Hjorth M, Quist J, Andersen R, et al. Change in sleep duration and proposed dietary risk factors for obesity in Danish school children. Pediatr Obes. 2014;9(6):e156–e159. doi: 10.1111/ijpo.264. [DOI] [PubMed] [Google Scholar]
- 44.Al-Hazzaa H, Musaiger A, Abahussain N, Al-Sobayel H, Qahwaji D. Lifestyle correlates of self-reported sleep duration among Saudi adolescents: a multicentre school-based cross-sectional study. Child Care Health Devel. 2014;40(4):533–542. doi: 10.1111/cch.12051. [DOI] [PubMed] [Google Scholar]
- 45.Franckle RL, Falbe J, Gortmaker S, et al. Insufficient sleep among elementary and middle school students is linked with elevated soda consumption and other unhealthy dietary behaviors. Prev Med. 2015;74:36–41. doi: 10.1016/j.ypmed.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al-Haifi AA, AlMajed HT, Al-Hazzaa HM, Musaiger AO, Arab MA, Hasan RA. Relative contribution of obesity, sedentary behaviors and dietary habits to sleep duration among Kuwaiti adolescents. Glob J Health Sci. 2016;8(1):107–117. doi: 10.5539/gjhs.v8n1p107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Collison KS, Zaidi MZ, Subhani SN, Al-Rubeaan K, Shoukri M, Al-Mohanna FA. Sugar-sweetened carbonated beverage consumption correlates with BMI, waist circumference, and poor dietary choices in school children. BMC Public Health. 2010;10:234. doi: 10.1186/1471-2458-10-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hitze B, Bosy-Westphal A, Bielfeldt F, et al. Determinants and impact of sleep duration in children and adolescents: data of the Kiel Obesity Prevention Study. Eur J Clin Nutr. 2009;63(6):739–746. doi: 10.1038/ejcn.2008.41. [DOI] [PubMed] [Google Scholar]
- 49.Rowe KS. Synthetic food colourings and ‘hyperactivity’: a double-blind crossover study. Aust Paediatr J. 1988;24(2):143–147. doi: 10.1111/j.1440-1754.1988.tb00307.x. [DOI] [PubMed] [Google Scholar]
- 50.Kaplan BJ, McNicol J, Conte RA, Moghadam H. Dietary replacement in preschool-aged hyperactive boys. Pediatrics. 1989;83(1):7–17. [PubMed] [Google Scholar]
- 51.Grandner MA, Jackson N, Gerstner JR, Knutson KL. Sleep symptoms associated with intake of specific dietary nutrients. J Sleep Res. 2014;23(1):22–34. doi: 10.1111/jsr.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grandner MA, Jackson N, Gerstner JR, Knutson KL. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite. 2013;64:71–80. doi: 10.1016/j.appet.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kaplan GB, Greenblatt DJ, Ehrenberg BL, et al. Dose-dependent pharmacokinetics and psychomotor effects of caffeine in humans. J Clin Pharmacol. 1997;37(8):693–703. doi: 10.1002/j.1552-4604.1997.tb04356.x. [DOI] [PubMed] [Google Scholar]
- 54.Landolt HP, Werth E, Borbély AA, Dijk D-J. Caffeine intake (200 mg) in the morning affects human sleep and EEG power spectra at night. Brain Res. 1995;675(1-2):67–74. doi: 10.1016/0006-8993(95)00040-w. [DOI] [PubMed] [Google Scholar]
- 55.Drapeau C, Hamel-Hebert I, Robillard R, Selmaoui B, Filipini D, Carrier J. Challenging sleep in aging: the effects of 200 mg of caffeine during the evening in young and middle-aged moderate caffeine consumers. J Sleep Res. 2006;15(2):133–141. doi: 10.1111/j.1365-2869.2006.00518.x. [DOI] [PubMed] [Google Scholar]