Abstract
Introduction
The electronic medical record (EMR) is standard in institutions. While there is not concern for legibility of notes and access to charts, there is an ease of copy and paste for daily notes. This may not lead to accurate portrayal of patient's status. Our purpose was to evaluate the use of copy and paste functions in daily notes of patients with injuries at high risk for complications.
Methods
IRB approval was obtained for a retrospective review. Inclusion criteria included patients aged 18 and older treated at our Level 1 Trauma Center after implementation of Epic Systems Corporation, Verona, WI, USA. Those who were surgically treated for bicondylar tibial plateau fracture, or open tibial shaft fracture type I or II were included. Manual comparison of daily progress to the previous day's note was carried out. Comparisons were made by evaluating the subjective, objective, and plan portions of the notes, coded nominally using 1 for a change 0 for remaining the same.
Results
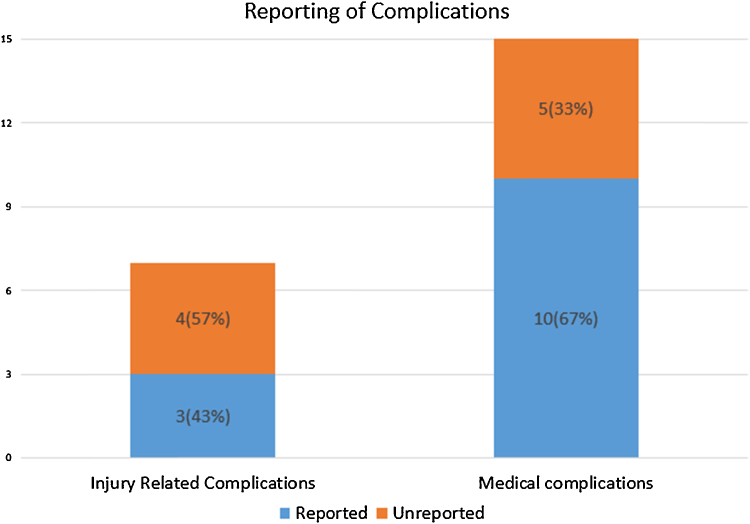
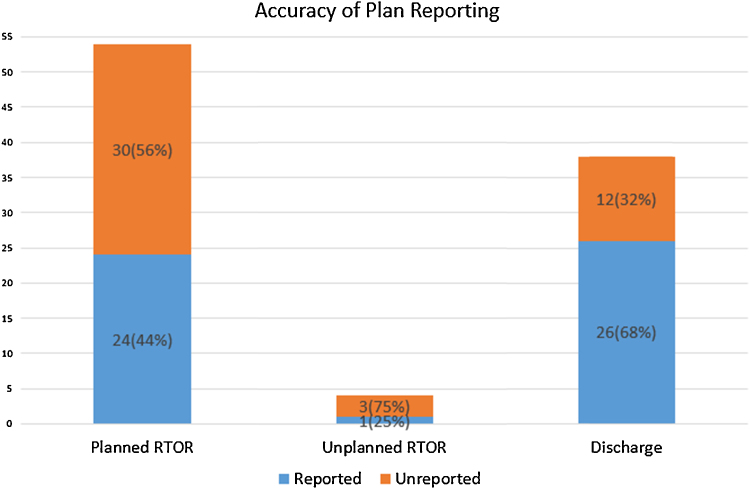
38 patients’ charts were reviewed during a 10-month (July 2012–April 2013) period, and the average length of stay was 12 days (range: 2–35). A total of 418 notes were compared. The overall average of copied data was 85% daily. In the subjective portion, 85–97% of the data was copied on a daily basis and 71–92% of the data was copied within the objective portion of the notes. There were 15 medical complications necessitating intervention. Of these medical complications, the note the day after the complication reflected the event in 10 out of 15, or 70%, of the complications. Thus 5, or 30%, of the patients did not have notes reflecting the complication (p < 0.05). There were 7 complications related to the injuries: 4 cases of compartment syndrome, 1 case of foot drop, representing a change in neurologic status, an amputation, and a wound infection treated with antibiotics. Four of the 7 complications (57%) were not reflected in the notes the following day after the complication (p < 0.05). There were 54 planned returns to the operating room for procedures, yet 30 of the 54 (56%) notes regarding planned surgical procedures notes did not accurately report the plan for surgery (p < 0.05). There were 4 patients with unplanned trips to the operating room and 3 of the notes (75%) did not reflect this (p < 0.05). Twelve patients (32%) did not have notes accurately reflecting discharge plans and/or destination (p < 0.05).
Discussion/conclusion
Our results demonstrated widespread use of copy and paste function. We encourage evaluation of the charts by comparing notes to check and a plan to minimize this practice. There needs to be consistent note writing guidelines and appropriate templates used. This will decrease the inaccuracies in the chart and provide a clear picture of the patient, their injuries, and current status.
Keywords: Orthopedic surgery, Trauma, Copy, Paste, Electronic medical record, EMR, Copy–paste
1. Introduction
As of January 1, 2014, the federal government mandated that all healthcare providers must have adopted some form of an electronic medical record (EMR). There are many commercially available EMR systems, including Cerner (Kansas City, Missouri) and Epic Systems Corporation (Verona, Wisconsin). EMR systems are designed to make medical documentation and patient care easier, more accurate, and accessible. This is accomplished by allowing multiple disciplines to communicate in a central location and manage prescriptions and documentation in one place. These electronic health records have proclaimed to improve the accessibility, legibility, and completeness of medical documentation while reducing medical errors and mortality rates.1, 2, 3, 4 However, there has been a noticeable and unexpected decline in the quality of documentation. This has been attributed to over-inclusion of data, or note clutter, and the inappropriate use of copy and paste.5, 6, 7, 8, 9, 10
The use of EMR for clinical notes carries with it the ease of the copy and paste function allowing providers to copy a note from the previous day in an effort to save time. The goal is to not re-write unchanged parts of the patient's record. The incorrect use of the copy and paste function may lead to errors and inaccuracies in day-to-day changes with patients. In this study, we sought to evaluate the prevalence of use of copy and paste functions and to assess its impact on the accuracy of documenting progress of patients in an orthopedic trauma service. We hypothesized that the daily progress notes by the orthopedic service would have less than 3 new points from the previous day and that the progress notes would not accurately portray a complication of a serious orthopedic injury.
The purpose of our study was to evaluate the use of copy and paste functions in daily progress notes of patients treated in a single institution, with injuries at a high risk for complications: bicondylar tibial plateau fractures and type I and II open tibial shaft fractures.
2. Methods
IRB approval was obtained from our institution to carry out a retrospective review of medical records. Inclusion criteria included patients aged 18 and older who were treated at Saint Louis University Hospital after the implementation of Epic Systems in July of 2012. Patients who were surgically treated for bicondylar tibial plateau fracture, or open tibial shaft fracture type I or type II were included. A search of ICD-9 codes was carried out to obtain a list of possibly eligible patients which were then either included or excluded using the above-mentioned inclusion criteria based on demographic data and operative reports describing fracture type and grade. Manual comparison of daily progress to the previous day's note was then completed. Comparisons were made using a standardized spreadsheet for the evaluation of subjective, objective, and plan portions of the notes, coded nominally, using 1 for a change 0 for remaining the same. The subjective data included: comparing pain, adverse reactions, activity, and overnight problems. The objective data included: sensory exam, splint exam, motor exam, circulation exam, wound evaluations, and dressing evaluations. Data from the plan section of the note included: complications, planned return to the operating room, unplanned return to the operating room, discharge plans and discharge destination, and whether the note reflected that plan.
Statistical analysis was then carried out using IBM's SPSS 20.0 (Chicago, Illinois). Descriptive data included frequency of each dichotomous variable for each individual patient and the percentage of occurrence, as well the overall frequency of each variable for all patients combined and percentages of variables that agreed or disagreed. For the plan section of the comparison, the McNemar test was used to compare the actual plan to what the notes reported.
3. Results
3.1. Demographics
There were 38 patients whose charts were reviewed during a 10-month period. There were 29 males and 9 females with an average age of 51 years old. Twenty-eight had tibial plateau fractures and 10 had open tibia fractures. The average length of stay for patients was 12 days (range: 2–35).
3.2. Progress notes
There were a total of 418 notes compared. The overall average of copied data was 85% on a daily basis. Vital signs were auto-updated, so they are not included in the overall copied material. In the subjective portion of the notes, 85–97% of the data was copied on a daily basis and 71–92% of the data was copied within the objective portion of the notes on a daily basis (Fig. 1, Fig. 2).
Fig. 1.
Complications reported versus unreported.
Fig. 2.
Accuracy of plan reported versus unreported.
3.3. Complications
There were a total of 15 medical complications necessitating intervention including 8 cases of anemia requiring transfusion, 4 cases mental status changes and/or cardiac issues, 2 cases of urinary tract infections, and 1 case of a fall delaying discharge (Table 1). Of these medical complications, the note the day after the complication reflected the event in 10 out of 15, or 70%, of the complications. Thus 5, or 30%, of the patients did not have notes reflecting the complication (p < 0.05). There were 7 complications related to the injuries: 4 cases of compartment syndrome, 1 case of foot drop representing a change in neurologic status, an amputation, and a wound infection treated with antibiotics (Table 2). Four of the 7 complications (57%) were not reflected in the notes the following day after the complication (p < 0.05). There were 54 planned returns to the operating room for procedures, yet 30 of the 54 (56%) notes regarding planned surgical procedures notes did not accurately report the plan for surgery (p < 0.05). There were 4 patients with unplanned trips to the operating room and three quarters of the notes (75%) did not reflect this (p < 0.05) (Table 3).
Table 1.
Subjective and objective data that was copied.
| # copied | % copied | |
|---|---|---|
| Subjective | ||
| Pain | 361 | 86.4 |
| Adverse reactions | 406 | 97.1 |
| Activity | 375 | 89.7 |
| Overnight problems | 356 | 85.2 |
| Objective | ||
| Sensory | 365 | 87.3 |
| Splint | 334 | 79.9 |
| Motor | 349 | 83.5 |
| Circulation | 386 | 92.3 |
| Wound | 298 | 71.3 |
| Dressing | 334 | 79.9 |
Table 2.
Medical complications.
| Type | Number |
|---|---|
| Anemia (requiring transfusion) | 8 |
| UTI | 2 |
| Altered mental status | 1 |
| Cardiac complication | 4 |
| Total | 15 |
Table 3.
Injury-related complications.
| Type | Number |
|---|---|
| Compartment syndrome | 4 |
| Foot drop | 1 |
| Amputation | 1 |
| Wound infection | 1 |
| Total | 7 |
3.4. Discharge
Twelve patients (32%) did not have notes accurately reflecting discharge plans and/or destination (p < 0.05).
4. Discussion
Our findings suggest that the copy and paste function is a detriment to the electronic medical record. This study found that the ease of this functionality causes inaccuracies in daily notes, which can lead to inappropriate patient care. We are not inferring that the EMR is inferior to hand written notes, as it provides many advantages and our study focuses on a single weakness. Some of the advantages include the ease of access to all of a patient's records within a hospital system, as well as a central location for communication and documentation of patient diagnoses, treatments, and progress. Other advantages as previously mentioned include legibility of notes, the EMR being a central location to house all of the information related to a patient. Another advantage is physician order entry being in the electronic medical record, which can eliminate medication dosage errors, as well as drug interactions. Despite these many advantages our study points to one weakness, the availability and ease of copy and paste functionality.
We chose surgically treated bicondylar tibial plateau fractures and open tibia fracture as the diagnoses for inclusion in this study as they may have a higher complication rate than other orthopedic trauma injuries and require monitoring of neurovascular status for compartment syndrome in both injuries and may have wound complications in the open tibia fracture patient. Orthopedic trauma patients were chosen as there are often multiple teams caring for these patients and accuracy of daily progress notes is important in patient care. A valid argument would be if other associated injuries could add to the inaccuracies in documentation. We chose to focus only on orthopedic injuries because the notes we were evaluating were written by the orthopedic trauma team. Therefore, we feel that this would not play a role in the accuracy or lack thereof in the documentation. The other injuries patients had would still be addressed and mentioned in each daily note. Furthermore, for returns to the OR, we did not include OR trips for other services as trips that needed to be accurately charted in the daily note.
Our study demonstrates that the EMR, while built to improve patient care and safety, can ironically not reflect a worsening of a patient's clinical course. The trustworthiness of EMRs has come into question due to the lengthy provider documentation, which contains redundant or extraneous information. Numerous quality of care concerns arise, as well as additional risks of malpractice liability and billing fraud and abuse. In academic health centers, these practices could also impact a trainee's educational experiences and even result in errors in data extraction in medical research.11 This extraneous information can lead providers to misinterpret the patient clinically.11 Excessively long documentation can lead to “reader fatigue” where providers scroll through redundant documentation, therefore increasing the risk that critical new information is overlooked.11
Although it seems harmless, copy and paste has become a common practice – 74–90% of physicians use the copy–paste function according to a September 2013 report by AHIMA.12 Physicians attitudes toward copy and paste function may be too relaxed. O’Donnell et al. demonstrated that the majority of physicians used copy and paste to write notes and did not perceive an overall negative impact on physician documentation or patient care.13 The overreliance of physicians on the copy and paste function, especially physicians in training such as residents, can decrease the critical thinking aspect of medicine. It can also insert diagnostic bias into a clinicians thinking due to the populated assessment and plans usurping a clinician's own experience and reasoning skills.14
Unfortunately, clinical documentation and reimbursement are intertwined and have resulted in the “more information is better” attitude. The required data elements needed to satisfy evaluation and management are complex which results in large amounts of supporting data being imported in. Hospitals push providers to comprehensively document the complexities of a patient's illness to meet coding and reimbursement requirements, and quality metrics and physicians attempt to safeguard themselves against fraud and abuse penalties.11 As described by Weis at al., “It seems very likely that physician use of content import technology will only continue to grow given the financial pressures in the health-care environment, unless there is a major reform in payment methodology”.11 As EMR documentation evolves, healthcare leadership must promote best practices that will improve care. This same argument is shared by Sheehy et al., who describe that the extent of documentation in the EMR is often directly related to how much physicians and hospitals are paid. Therefore, clinicians have incentive to err on the side of over-documentation whereas insurers have incentives to audit records to try and save money. If a different reimbursement process existed, the misuse of copy and paste could become obsolete. Since this does not appear on the horizon in the near future, physicians should use the EMR as it was intended – to improve patient care.15 Otherwise, the ease of copying can lead to documenting more treatment than actually occurred. The fraudulent practice, known as “upcoding,” costs the healthcare industry an estimated $11 billion annually.16 The common practice of cloning notes also makes it difficult to distinguish where clinical plagiarism ends and billing fraud begins.17
Residents are responsible for most of the daily progress notes in an academic practice with attending physician oversight. Thornton et al. looked at the prevalence of copied information by attending and residents in the critical care setting. They found that copying among attendings and residents was common in this ICU-based cohort, with residents copying more frequently and attendings copying more information per note.18 There have been attempts to improve resident note writing. There are many ways to fix this dilemma. First, each institution could eliminate copy and paste entirely as certain institutions have as listed by Weis et al.11 Dean et al. attempted to improve resident notes based on a multidisciplinary bundle approach which consisted of establishing note-writing guidelines, developing an aligned note template, and educating interns about the guidelines and using the template. They found a significant improvement in the total note score and in questions related to note clutter; however, there was no significant improvement seen for questions related to copy–paste.19 As noted by Shoolin et al., the primary goal of our profession is to spend as much time as possible listening to, understanding, and helping patients. Clinicians would use the EMR to make documentation easier, not harder. At the same time, there should be reasonable restrictions on the use of copy and paste to limit the growing challenge of ‘note bloat’. We must find the right balance between ease of use and thoughtless documentation.20 Some simple suggestions made by Shoolin at al. are first to document each encounter with the minimum data necessary. Second, collect the data and display it in a way that meets the varied needs of the following audiences for every note. Third, maintain supporting data integrity and quality. Finally, ensure privacy and security. We recommend that that note writing should be accurate without being made too cumbersome and time consuming for the physicians. There is a fine balance, which has to be reached so that physicians can devote their valuable time more on improving patient care rather than writing notes.
We recognize that there are some limitations to our study. Our small sample size is a limitation making the results of our study difficult to generalize. However, our results expose the pitfalls of using the copy and paste functions which opens the door for larger studies. Other sources of limitation in our study include the possibility of other injuries as a confounding variable. Other orthopedic injuries were included in the physical exam portion of the notes and compared day to day; this should not affect accuracy. Non-orthopedic injuries were followed by other services with the orthopedic team simply tracking them. Changes in other services plans should have been reflected in the orthopedic note. However, if the other service was not documenting accurately, this could be a confounder to the inaccuracies within the orthopedic notes. Other possible confounding variables that may have affected our results include incomplete examinations/evaluations of patients as well as poor discharge planning. Incomplete examination would lead to inaccurate portrayal of the patient, though this should not affect our analysis of the material that was copied from one day to the next. It is also possible the incomplete examinations themselves lead to increased use of copy and paste with the examiner assuming no changes to the exam. Poor discharge planning would lead to multiple changes in the disposition section of the note, which would have been reflected as changes, not inaccuracies. Inaccuracies were counted as such based on how well the final note reflected the final destination of the patient. Inaccuracies are therefore attributable to copying the discharge plan from day to day without reflecting changes to the plan. Another limitation of our study is that we did not compare hand written notes to the EMR. We cannot ascertain if the duplication of notes is due to the ease of EMR or healthcare providers themselves. What we know is the EMR provides an ease of function that allows copying and pasting notes.
This study demonstrates the importance of the quality of note writing in the electronic medical record. There is much more work to be done in improving the clinical narrative and the inappropriate use the copy and paste function.19 There needs to be consistent note writing guidelines and appropriate templates used. As billing and coding become more intertwined with documentation, there needs to be a standard method that eliminates note clutter and fraudulent practices. Providers need to maintain compliance, but most importantly, provide appropriate patient care. Residents should be educated early on the importance of accurate reflection of all aspects of the patient care and change the progress notes daily as it is highly unlikely each patient's complaints, exam, and plan remain the same. It is difficult for attendings who cosign each note to determine how much is copied and pasted without side by side comparison, which is not easily accomplished with the current EMR systems.
Conflicts of interest
The authors have none to declare.
References
- 1.Chaudhry B., Wang J., Wu S. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 2.Amarasingham R., Moore B.J., Tabak Y.P. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical record data. Med Care. 2010;48(11):981–988. doi: 10.1097/MLR.0b013e3181ef60d9. [DOI] [PubMed] [Google Scholar]
- 3.Makam A.N., Nguyen O.K., Moore B., Ma Y., Amarasingham R. Identifying patients with diabetes and the earliest date of diagnosis in real time: an electronic health record case-finding algorithm. BMC Med Inform Decis Mak. 2013;13:81. doi: 10.1186/1472-6947-13-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poon E.G., Wright A., Simon S.R. Relationship between use of electronic health record features and health care quality: results of a statewide survey. Med Care. 2010;48(3):203–209. doi: 10.1097/MLR.0b013e3181c16203. [DOI] [PubMed] [Google Scholar]
- 5.Hartzband P., Groopman J. Off the record – avoiding the pitfalls of going electronic. N Engl J Med. 2008;358(16):1656–1658. doi: 10.1056/NEJMp0802221. [DOI] [PubMed] [Google Scholar]
- 6.Hirschtick R.E. A piece of my mind. Copy-and-paste. JAMA. 2006;295(20):2335–2336. doi: 10.1001/jama.295.20.2335. [DOI] [PubMed] [Google Scholar]
- 7.Siegler E.L., Adelman R. Copy and paste: a remediable hazard of electronic health records. Am J Med. 2009;122(6):495–496. doi: 10.1016/j.amjmed.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 8.Siegler E.L. The evolving medical record. Ann Intern Med. 2010;153(10):671–677. doi: 10.7326/0003-4819-153-10-201011160-00012. [DOI] [PubMed] [Google Scholar]
- 9.Thielke S., Hammond K., Helbig S. Copying and pasting of examinations within the electronic medical record. Int J Med Inform. 2007;76(suppl 1):S122–S128. doi: 10.1016/j.ijmedinf.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Payne T.H., Patel R., Beahan S., Zehner J. The physical attractiveness of electronic physician notes. AMIA Annu Symp Proc 2010. 2010:622–626. [PMC free article] [PubMed] [Google Scholar]
- 11.Weis J.M., Levy P.C. Copy, paste, and cloned notes in electronic health records: prevalence, benefits, risks, and best practice recommendations. Chest. 2014;145(3):632–638. doi: 10.1378/chest.13-0886. [DOI] [PubMed] [Google Scholar]
- 12.Bowman S. Impact of electronic health record systems on information integrity: quality and safety implications. Perspect Health Inf Manag. 2013;10:1c. [PMC free article] [PubMed] [Google Scholar]
- 13.O’Donnell H.C., Kaushal R., Barrón Y., Callahan M.A., Adelman R.D., Siegler E.L. Physicians’ attitudes towards copy and pasting in electronic note writing. J Gen Intern Med. 2009;24(1):63–68. doi: 10.1007/s11606-008-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horsky J., Zhang J., Patel V.L. To err is not entirely human: complex technology and user cognition. J Biomed Inform. 2005;38(4):264–266. doi: 10.1016/j.jbi.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Sheehy A.M., Weissburg D.J., Dean S.M. The role of copy-and-paste in the hospital electronic health record. JAMA Intern Med. 2014;174(8):1217–1218. doi: 10.1001/jamainternmed.2014.2110. [DOI] [PubMed] [Google Scholar]
- 16.Haugen H. Overcoming the risks of copy and paste in EHRs. J AHIMA. 2014;85(6):54–55. [PubMed] [Google Scholar]
- 17.Vogel L. Cut-and-paste clinical notes confuse care, say US internists. CMAJ. 2013;185(18):E826. doi: 10.1503/cmaj.109-4656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thornton J.D., Schold J.D., Venkateshaiah L., Lander B. Prevalence of copied information by attendings and residents in critical care progress notes. Crit Care Med. 2013;41(2):382–388. doi: 10.1097/CCM.0b013e3182711a1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dean S.M., Eickhoff J.C., Bakel L.A. The effectiveness of a bundled intervention to improve resident progress notes in an electronic health record. J Hosp Med. 2015;10(2):104–107. doi: 10.1002/jhm.2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shoolin J., Ozeran L., Hamann C., Bria W., 2nd Association of Medical Directors of Information Systems consensus on inpatient electronic health record documentation. Appl Clin Inform. 2013;4(2):293–303. doi: 10.4338/ACI-2013-02-R-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]