Abstract
Objectives
Our objective was to perform a systematic review of the literature and conduct a meta-analysis to investigate the effect of initial varus or valgus displacement of proximal humerus on the outcomes of patients with proximal humerus fractures treated with open reduction and internal fixation.
Methods
In accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement standards, we performed a systematic review. Electronic databases MEDLINE, EMBASE, CINAHL and the Cochrane Central Register of Controlled Trials (CENTRAL) were searched to identify randomised and non-randomised studies comparing postoperative outcomes associated with initial varus versus initial valgus displacement of proximal humerus fracture. The Newcastle–Ottawa scale was used to assess the methodological quality and risk of bias of the selected studies. Fixed-effect or random-effects models were applied to calculate pooled outcome data.
Results
We identified two retrospective cohort studies and one retrospective analysis of a prospective database, enrolling a total of 243 patients with proximal humerus fractures. Our analysis showed that initial varus displacement was associated with a higher risk of overall complication (RR 2.28, 95% CI 1.12–4.64, P = 0.02), screw penetration (RR 2.30, 95% CI 1.06–5.02, P = 0.04), varus displacement (RR 4.38, 95% CI 2.22–8.65, P < 0.0001), and reoperation (RR 3.01, 95% CI 1.80–5.03, P < 0.0001) compared to valgus displacement. There was no significant difference in avascular necrosis (RR 1.43, 95% CI 0.62–3.27, P = 0.40), infection (RR 1.49, 95% CI 0.46–4.84, P = 0.51), and non-union or malunion (RR 1.37, 95% CI 0.37–5.04, P = 0.64).
Conclusions
The best available evidence demonstrates that initial varus displacement of proximal humerus fractures is associated with higher risk of overall complication, screw penetration, varus displacement, and reoperation compared to initial valgus displacement. The best available evidence is not adequately robust to make definitive conclusions. Further high quality studies, that are adequately powered, are required to investigate the outcomes of initial varus and valgus displacement in specific fracture types.
Level of evidence
Level II.
Keywords: Varus, Valgus, Humerus fracture, Open reduction and internal fixation
1. Introduction
Humerus fractures have a substantial impact on personal function and well-being.1, 2, 3 Proximal humerus fractures account for 50% of humerus fractures and commonly occur in patients with osteoporosis.4 The incidence of proximal humerus fractures has increased in elderly patients over the past two decades.5
Management of proximal humerus fracture depends on the patient's characteristics, the type of the fracture, technical difficulties in surgical treatment, and the surgeon's circumstances. In addition to the increasing incidence of these fractures, the use of open reduction and internal fixation in surgical management of proximal humerus fractures has increased over the past decade.5 The advent of locked plating has allowed surgeons to treat a greater percentage of proximal humerus fractures with open reduction and internal fixation and retention of the native humeral head technology.6 However, use of locked plating for management of proximal humerus fractures has been associated with a high complication rate according to the literature.7 The most common complications include avascular necrosis, screw penetration, and varus displacement. The patient-specific factors contributing to the complications following surgical management of proximal humerus fractures have not been investigated adequately.
Our objective was to perform a systematic review of the literature and conduct a meta-analysis to investigate the effect of initial varus or valgus displacement of proximal humerus on the outcomes of patients with proximal humerus fractures treated with open reduction and internal fixation. The robustness and quality of the available evidence was evaluated in a systematic and explicit approach with consideration of consistency and generalisability of the results.
2. Methods
This systematic review was performed according to an agreed predefined protocol. The review was conducted and presented according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement standards.8
2.1. Eligibility criteria
We planned to include all randomised controlled trials (RCTs) and observational studies including patients with proximal humerus fractures treated with open reduction and internal fixation, and comparing the postoperative outcomes of fractures with initial varus displacement with those with initial valgus displacement.
2.2. Outcome measures
Overall complication was considered as primary outcome measure. The secondary outcome measures included avascular necrosis, screw penetration, infection, varus displacement, nonunion or malunion, reoperation rate, Constant–Murley (CM) score, and the Disabilities of the Arm, Shoulder and Hand (DASH) Score.
2.3. Literature search strategy
Two authors independently searched the following electronic databases: MEDLINE, EMBASE, CINAHL and the Cochrane Central Register of Controlled Trials (CENTRAL). The last search was run on 01 May 2016. The details of the search strategy, which was adapted according to thesaurus headings, search operators and limits in each of the above databases, are appended in Appendix A. In addition, the following trial databases were searched for details of ongoing and unpublished studies: World Health Organization International Clinical Trials Registry http://apps.who.int/trialsearch/, ClinicalTrials.gov http://clinicaltrials.gov/, ISRCTN Register http://www.isrctn.com/. We searched the bibliographic lists of relevant articles and reviews for further potentially eligible trials. No language restrictions were applied in our search strategies.
2.4. Study selection
Two authors independently assessed the title and abstract of articles identified from the literature searches. The full-texts of relevant reports were retrieved and those articles that met the eligibility criteria of our review were selected. We resolved any discrepancies in study selection by discussion between the authors. An independent third author was consulted in the event of disagreement.
2.5. Data collection
We created an electronic data extraction spreadsheet in line with the Cochrane's data collection form for intervention reviews. We pilot-tested the spreadsheet in randomly selected articles and adjusted it accordingly. Our data extraction spreadsheet included: study-related data (first author, year of publication, country of origin of the corresponding author, journal in which the study was published, study design, and study size); baseline demographic and clinical information of the study populations (age, gender, clinical presentation of the study participants, fracture type, surgical procedure, and duration of follow up); and primary and secondary outcome measures data.
Two authors independently collected and recorded data and resolved disagreements by discussion. If no agreement could be reached, a third author was consulted.
2.6. Methodological quality and risk of bias assessment
The methodological quality and risk of bias of the included articles were assessed independently by two authors. We planned to use the Cochrane's tool9 and the Newcastle–Ottawa scale (NOS)10 for assessing the risk of bias of randomised trials and observational studies, respectively. The Cochrane's tool assesses domains including selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias and, for each individual domain, classifies studies into low, unclear, and high risk of bias. The NOS uses a star system with a maximum of nine stars to evaluate a study in three domains (8 items): the selection of the study groups, the comparability of the groups, and the ascertainment of outcome of interest. For each item of the scale, we judged each study as low risk (one star awarded) or high risk (no star awarded). We determined studies that received a score of nine stars to be of low risk of bias, studies that scored seven or eight stars to be of moderate risk, and those that scored six or less to be of high risk of bias. Disagreements were resolved by discussion between the two reviewers. If no agreement could be reached, a third author acted as an adjudicator. A risk of bias graph was constructed to present the results.
2.7. Data synthesis and statistical analyses
For dichotomous outcome variables (overall complication rate, avascular necrosis, screw penetration, infection, varus displacement, nonunion or malunion, and reoperation rate), we calculated the risk ratio (RR). The RR is the risk of an event in the varus group compared to the valgus group. An RR of less than one would favour varus stent and an RR of more than one would favour the valgus group. For continuous parameters (CM score and DASH score) we planned to calculate the mean difference (MD) between the two groups.
We used the individual patient as the unit of analysis. Information about dropouts, withdrawals and other missing data were recorded and, if not reported, we contacted the study authors where possible. The final analysis was based on intention-to-treat data from the individual clinical studies.
The Review Manager 5.3 software was used for data synthesis. Extracted data were entered into Review Manager by the first independent author and checked by the second independent author. We used random effects or fixed effect modelling as appropriate, for analysis. We applied random effects models if considerable heterogeneity among the studies, as defined by Higgins et al., was identified. The results were reported in a forest plot with 95% confidence intervals (CIs).
Heterogeneity among the studies was assessed using the Cochran Q test (χ2). We quantified inconsistency by calculating I2 and interpreted it using the following guide: 0–25% may present low heterogeneity; 25–75% may represent moderate heterogeneity; and 75–100% may represent high heterogeneity. We planned to construct funnel plots and evaluate their symmetry to visually assess publication bias, as long as a sufficient number of studies (more than 10) were available.
2.8. Sensitivity and sub-group analyses
In order to explore potential sources of heterogeneity and assess the robustness of our results, we planned to perform additional analyses for outcomes that were reported by at least four studies. For each outcome, we planned to repeat the primary analysis using random effects models and fixed effect models. In addition, we planned to calculate both OR and RD for each dichotomous variable. We planned to assess the effect of each study on the overall effect size and heterogeneity by repeating the analysis after removing one study at a time. Also, we planned to perform separate analyses for studies with low, moderate, or high risk of bias to assess the change in direction of the effect size. We also planned to perform sub-group analyses including studies that were RCT.
3. Results
3.1. Literature search results
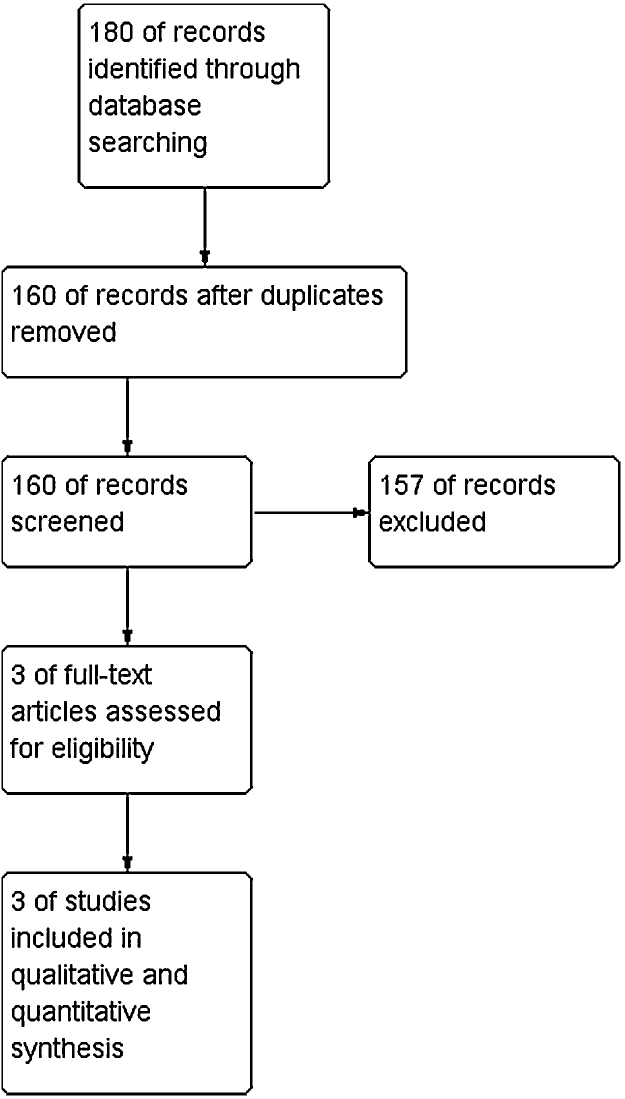
Searches of electronic databases identified 160 articles of which three11, 12, 13 were eligible for this review (Fig. 1). These included two retrospective cohort studies11, 12 and one retrospective analysis of a prospective database,13 enrolling a total of 243 patients with proximal humerus fractures. Overall, 103 patients had fractures with varus displacement and 140 patients had fractures with valgus displacement. All patients underwent open reduction and internal fixation with proximal humeral locked plate. The mean duration of follow up was 16 months. The characteristics of the included studies are presented in Table 1.
Fig. 1.
Study flow diagram.
Table 1.
Baseline characteristics of the included studies.
| Author | Year | Country | Journal | Type of study | Clinical presentation | Fracture type | Procedure | Follow up | Sample size | Age (mean) | Male (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Capriccioso | 2016 | USA | Injury | Retrospective cohort | Proximal humerus fractures | OTA A, B, C | Locked plating (Synthes/Exatech) | 12 months | 101 | Varus: 59.3 Valgus: 62.4 |
Varus: 31.9% Valgus: 38.9% |
| Little | 2014 | USA | J Orthop Trauma | Retrospective data analysis | Isolated proximal humerus fractures | Neer 2, 3, 4 | Locked plating (Endosteal allograft) | 19 months | 72 | All: 62 | NR |
| Solberg | 2009 | USA | J Orthop Trauma | Retrospective cohort | Low energy proximal humerus fractures | Neer 3, 4 | Locked plating (Synthes/Stryker/Zimmer) | 18 months | 70 | Varus: 65.6 Valgus: 67.4 |
Varus: 29.2% Valgus: 19.6% |
OTA: Orthopedic Trauma Association; NR: not reported.
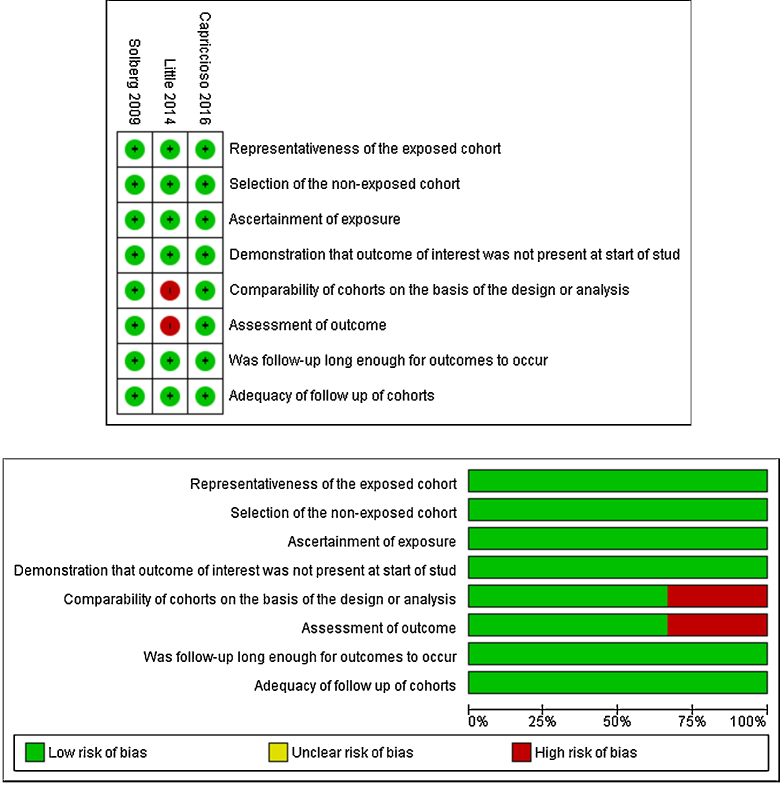
3.2. Methodological quality and risk of bias
Two studies11, 12 were judged to be of low risk of bias and one study13 was judged to be of moderate risk of bias. Lack of comparability of cohorts on the basis of the design or analysis was found to be the source of bias in Little et al.13 The summary and results of methodological quality assessment are demonstrated graphically in Fig. 2.
Fig. 2.
Risk of bias summary and graph showing authors’ judgements about each Newcastle–Ottawa scale item for each included study.
3.3. Outcome synthesis
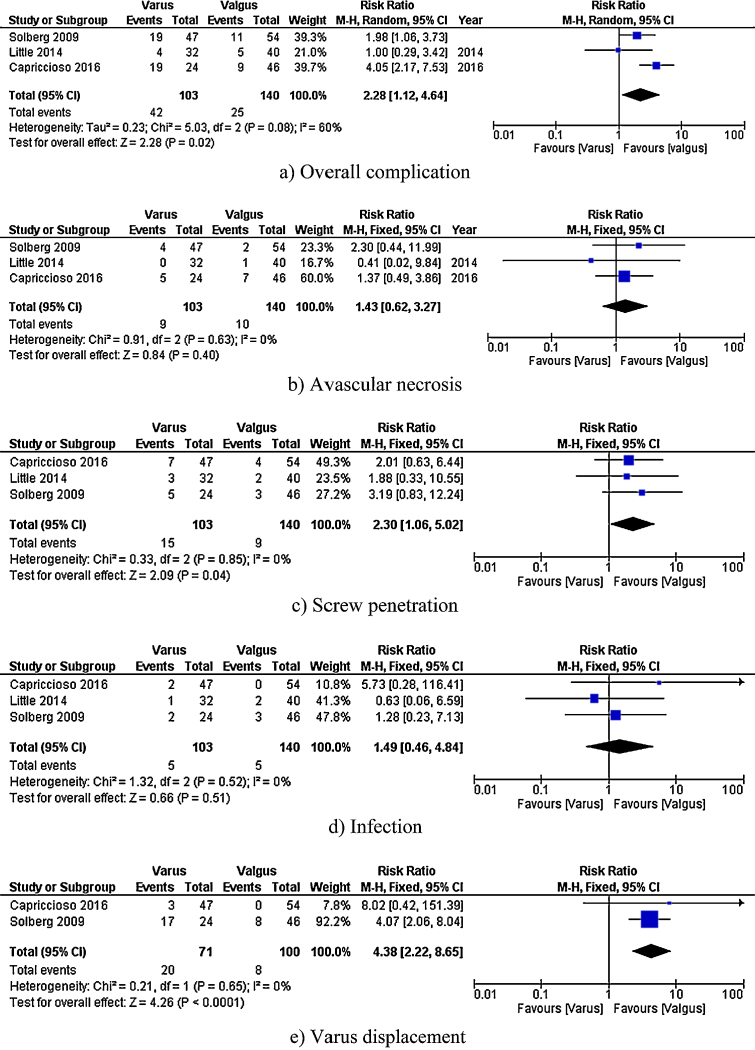
3.3.1. Overall complication
Overall complication was reported in three studies,11, 12, 13 including 243 patients (Fig. 3). The risk of overall complication was significantly higher in the varus group than the valgus group (RR 2.28, 95% CI 1.12–4.64, P = 0.02). A moderate level of heterogeneity among the studies existed (I2 = 60%, P = 0.08).
Fig. 3.
Forest plots of the comparisons: (a) overall complication, (b) avascular necrosis, (c) screw penetration, (d) infection, (e) varus displacement, (f) Malunion or nonunion, and (g) reoperation. The solid squares denote the risk ratios (RRs), the horizontal lines represent the 95% confidence intervals (CIs), and the diamond denotes the pooled RR. M–H, Mantel–Haenszel test.
3.3.2. Avascular necrosis
Avascular necrosis was reported in three studies,11, 12, 13 including 243 patients (Fig. 3). There was no significant difference in avascular necrosis between the varus and valgus groups (RR 1.43, 95% CI 0.62–3.27, P = 0.40). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.63).
3.3.3. Screw penetration
Screw penetration was reported in three studies,11, 12, 13 including 243 patients (Fig. 3). The risk of screw penetration was significantly higher in the varus group than the valgus group (RR 2.30, 95% CI 1.06–5.02, P = 0.04). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.85).
3.3.4. Infection
Infection was reported in three studies,11, 12, 13 including 243 patients (Fig. 3). There was no significant difference in the risk of infection between the varus and valgus groups (RR 1.49, 95% CI 0.46–4.84, P = 0.51). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.52).
3.3.5. Varus displacement
Varus displacement was reported in two studies,11, 12 including 171 patients (Fig. 3). The risk of varus displacement was significantly higher in the varus group than the valgus group (RR 4.38, 95% CI 2.22–8.65, P < 0.0001). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.65).
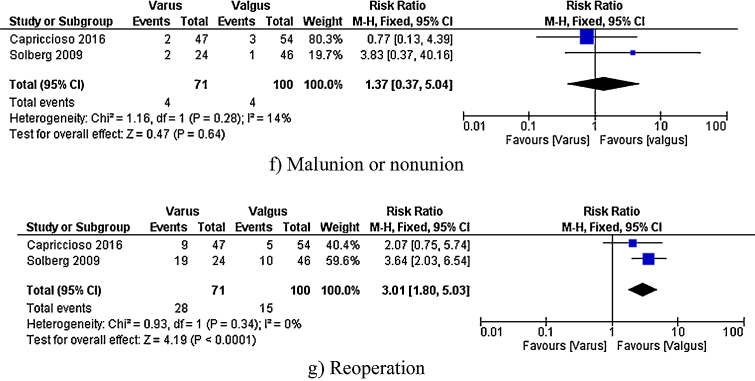
3.3.6. Nonunion or malunion
Nonunion or malunion reported in two studies,11, 12 including 171 patients (Fig. 3). There was no significant difference in the risk of nonunion or malunion between the varus and valgus groups (RR 1.37, 95% CI 0.37–5.04, P = 0.64). A low level of heterogeneity among the studies existed (I2 = 14%, P = 0.28).
3.3.7. Reoperation rate
Reoperation rate was reported in two studies,11, 12 including 171 patients (Fig. 3). The risk of reoperation was significantly higher in the varus group than the valgus group (RR 3.01, 95% CI 1.80–5.03, P < 0.0001). A low level of heterogeneity among the studies existed (I2 = 0%, P = 0.34).
3.3.8. CM score
CM score was reported in two studies,12, 13 including 142 patients. The available data did not allow us to calculate pooled MD for this outcome. Little et al.13 reported that there is no significant difference in the mean CM score between the varus and valgus groups (85.2 versus 88.7, respectively). Solberg et al.12 reported that mean CM score was significantly higher in the valgus group (63.3 versus 71.2, P < 0.01).
3.3.9. DASH score
DASH score was reported in two studies,11, 13 including 173 patients. The available data did not allow us to calculate pooled MD for this outcome. Capriccioso et al.11 and Little et al.13 did not find a significant difference in the mean DASH score between the varus and valgus groups (29 versus 21 in Capriccioso et al.,11 and 21.4 versus 13.9 in Little et al.13).
3.4. Sensitivity analyses
In our protocol we planned to perform additional analyses for the outcomes that were reported by at least four studies. Considering the limited number of included studies, we were not able to perform sensitivity or subgroup analyses for any of the outcomes.
4. Discussion
We conducted a systematic review of the literature and meta-analysis of reported outcomes to evaluate the effect of initial varus or valgus displacement of proximal humerus on the outcomes of patients with proximal humerus fractures treated with open reduction and internal fixation. We included three retrospective studies,11, 12, 13 enrolling a total of 243 patients with proximal humerus fractures. Our analysis showed that initial varus displacement was associated with a higher risk of overall complication, screw penetration, varus displacement, and reoperation compared to valgus displacement. There was no significant difference in avascular necrosis, infection, and non-union or malunion. The available evidence did not allow us to reach a conclusion regarding CM or DASH scores. The between-study heterogeneity was moderate for overall complication but it was low for other outcomes. The available evidence is derived from a very small number of studies with generally small sample sizes; therefore, the best available evidence is not adequately robust to make definitive conclusions.
There is no published systematic review and meta-analysis investigating the effect of initial varus or valgus displacement of proximal humerus on the outcomes of patients with proximal humerus fractures treated with open reduction and internal fixation. The overall complication rate of 48.8% following locking plate fixation of proximal humerus fractures has been reported in the literature.7 The overall complication rate in our study was 40.8% in the varus group and 17.9% in the valgus group. Therefore, initial varus displacement was associated with a higher complication rate. The association between initial angulation of proximal humerus fractures and complications of locking plate fixation has not been investigated adequately in the literature. Some authors14 reported higher complication or failure rate following locking plate fixation in fractures with initial varus displacement while others15 have not found any associations between initial varus angulation and fixation failure.
Although the best available evidence suggests that initial varus deformity of proximal humerus fracture is associated with poorer postoperative outcomes compared to initial valgus deformity, the quality of the available evidence is low. The available evidence is derived from retrospective studies that are inevitably subject to selection bias. All the outcomes were reported by a very limited number of studies; therefore, few participants and few events may have led to imprecise effects estimates, reflected by wide confidence intervals for the calculated RRs.
Varus-angulated fractures are an important, but poorly defined subgroup of fractures of the proximal humerus.16, 17 They have a wide range of severity, with considerable variation in the degree of varus deformity, displacement of the humeral head and involvement of the tuberosities.18 The treatment of these injuries is technically challenging when there is disruption of the medial cortical buttress.18 This may explain the higher complication rate in the varus group in our study.
The reported outcomes of our review and analysis should be viewed and interpreted in the context of inherent limitations. We identified a limited number of eligible studies reporting a relatively small number of patients. None of the included studies were prospective. As discussed above, our results are subject to selection bias and imprecise effects estimates. Finally, the available data did not allow us to perform subgroup analysis based on parameters such as specific Orthopaedic Trauma Association (OTA) or Neer fracture types, or other patient-specific factors.
5. Conclusions
The best available evidence demonstrates that initial varus displacement of proximal humerus fractures is associated with higher risk of overall complication, screw penetration, varus displacement, and reoperation compared to initial valgus displacement following open reduction and fixation with locking plate. The best available evidence is not adequately robust to make definitive conclusions. Further high quality studies, that are adequately powered, are required to investigate the outcomes of initial varus and valgus displacement in specific fracture types. Moreover, further studies are required to recognise the other parameters contributing to the complications following surgical management of proximal humerus fractures.
Author contributions
Project lead: Shahab H.
Design: Shahab H.
Literature search and study selection: MC, Shahab H.
Data collection: MC, Shahab H.
Statistical analysis: Shahab H, Shahin H.
Writing the article: MC, Shahab H.
Critical revision of the article: MC, Shahin H, Shahab H.
Final approval of the article: MC, Shahin H, Shahab H.
Conflicts of interest
The authors have none to declare.
Ethical approval
Not required.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Appendix A.
| Search no. | Search strategya |
|---|---|
| #1 | varus: TI,AB,KW |
| #2 | varus deformity: TI,AB,KW |
| #3 | varus angulation: TI,AB,KW |
| #4 | valgus: TI,AB,KW |
| #5 | valgus deformity: TI,AB,KW |
| #6 | valgus angulation: TI,AB,KW |
| #7 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 |
| #8 | MeSH descriptor: [bone fracture] explode all trees |
| #9 | fractur*: TI,AB,KW |
| #10 | #8 OR #9 |
| #11 | humer*: TI,AB,KW |
| #12 | humer* near2 fractur* TI,AB,KW |
| #13 | #11 OR #12 |
| #9 | #7 AND #10 AND #13 |
This search strategy was adopted for following databases: MEDLINE, EMBASE, CINAHL and the Cochrane Central Register of Controlled Trials (CENTRAL)
References
- 1.Piirtola M., Vahlberg T., Lopponen M., Raiha I., Isoaho R., Kivela S.L. Fractures as predictors of excess mortality in the aged: a population-based study with a 12-year follow-up. Eur J Epidemiol. 2008;23:747–755. doi: 10.1007/s10654-008-9289-4. [DOI] [PubMed] [Google Scholar]
- 2.Johnell O., Kanis J.A., Oden A. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38–42. doi: 10.1007/s00198-003-1490-4. [DOI] [PubMed] [Google Scholar]
- 3.Olsson C., Nordquist A., Petersson C.J. Long-term outcome of a proximal humerus fracture predicted after 1 year: a 13-year prospective population-based follow-up study of 47 patients. Acta Orthop. 2005;76:397–402. [PubMed] [Google Scholar]
- 4.Kim S.H., Szabo R.M., Marder R.A. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken) 2012;64(3):407–414. doi: 10.1002/acr.21563. [DOI] [PubMed] [Google Scholar]
- 5.Khatib O., Onyekwelu I., Zuckerman J.D. The incidence of proximal humeral fractures in New York State from 1990 through 2010 with an emphasis on operative management in patients aged 65 years or older. J Should Elbow Surg. 2014;23(9):1356–1362. doi: 10.1016/j.jse.2013.12.034. [DOI] [PubMed] [Google Scholar]
- 6.Vallier H.A. Treatment of proximal humerus fractures. J Orthop Trauma. 2007;21:469–476. doi: 10.1097/BOT.0b013e318133479c. [DOI] [PubMed] [Google Scholar]
- 7.Sproul R.C., Iyengar J.J., Devcic Z., Feeley B.T. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42:408–413. doi: 10.1016/j.injury.2010.11.058. [DOI] [PubMed] [Google Scholar]
- 8.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins J.P., Altman D.G., Higgins J.P., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.1. 2014. Chapter 8: assessing risk of bias in included studies. [Updated September 2008]. Available at: http://hiv.cochrane.org/sites/hiv.cochrane.org/files/uploads/Ch08_Bias.pdf Accessed May 15. [Google Scholar]
- 10.Wells G.A., Shea B., O’Connell D. 2014. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Accessed May 15. [Google Scholar]
- 11.Capriccioso C.E., Zuckerman J.D., Egol K.A. Initial varus displacement of proximal humerus fractures results in similar function but higher complication rates. Injury. 2016 doi: 10.1016/j.injury.2016.01.021. S0020-1383(16)00023-1. [DOI] [PubMed] [Google Scholar]
- 12.Solberg B.D., Moon C.N., Franco D.P., Paiement G.D. Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009;23:113–119. doi: 10.1097/BOT.0b013e31819344bf. [DOI] [PubMed] [Google Scholar]
- 13.Little M.T., Berkes M.B., Schottel P.C. The impact of preoperative coronal plane deformity on proximal humerus fixation with endosteal augmentation. J Orthop Trauma. 2014;28(6):338–347. doi: 10.1097/BOT.0000000000000012. [DOI] [PubMed] [Google Scholar]
- 14.Hardeman F., Bollars P., Donnelly M., Bellemans J., Nijs S. Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury. 2012;43:153–158. doi: 10.1016/j.injury.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 15.Krappinger D., Bizzotto N., Riedmann S., Kammerlander C., Hengg C., Kralinger F.S. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42:1283–1288. doi: 10.1016/j.injury.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 16.Court-Brown C.M., McQueen M.M. The impacted varus (A2.2) proximal humeral fracture: prediction of outcome and results of nonoperative treatment in 99 patients. Acta Orthop Scand. 2004;75:736–740. doi: 10.1080/00016470410004111. [DOI] [PubMed] [Google Scholar]
- 17.Edelson G., Kelly I., Vigder F., Reis N.D. A three-dimensional classification for fractures of the proximal humerus. J Bone Joint Surg [Br] 2004;86-B:413–425. doi: 10.1302/0301-620x.86b3.14428. [DOI] [PubMed] [Google Scholar]
- 18.Robinson C.M., Wylie J.R., Ray A.G. Proximal humeral fractures with a severe varus deformity treated by fixation with a locking plate. J Bone Joint Surg Br. 2010;92(5):672–678. doi: 10.1302/0301-620X.92B5.22849. [DOI] [PubMed] [Google Scholar]