Abstract
Background
To compare the short and mid-term results of intraarticular triamcinolone hexacetonide and hyaluronic acid (HA) in knee osteoarthritis.
Methods
A prospective randomized study including 40 patients in steroid and 42 patients in HA group. The outcome was evaluated with Knee Society Score (KSS) and Visual Analog Scale (VAS).
Result
On KSS function and VAS score, there was no difference till four weeks. On KSS pain there was no difference till 12 weeks (P > 0.05) after that score of steroid group deteriorated rapidly. At six months HA was significantly better than a steroid.
Conclusion
The HA seems to be better for pain relief and functionality in the short and mid-term periods.
Keywords: Osteoarthritis, Intra-articular, Steroid, Hyaluronic acid, Knee Society Score
1. Introduction
Osteoarthritis (OA) is the most common cause of knee pain and a leading cause of disability globally. It is a progressive disorder caused by gradual loss of articular cartilage. Many mechanical and biochemical factors have been suggested as the responsible causes for cartilage destruction leading to OA. Cytokines and various growth factors (GF) may also play a role in the regulation of catabolic and anabolic process in the pathophysiology of knee OA. The catabolic process is mainly mediated by Interleukin-1 and tumor necrosis factor-β that activate proteolytic digestion of articular cartilage. Various GF as tissue GF-β and insulin GF-1 may help body's attempt to repair the degenerated cartilage.
Various conservative treatment modalities including both pharmacological and the non-pharmacological modalities are recommended in clinical guidelines.1, 2 However, if these are ineffective then intraarticular (IA) injections (corticosteroids, viscosupplements, blood-derived products) are considered as the second line of the non-operative modality of treatment.3
We compared the outcomes of the two most commonly used intra-articular therapy of steroids and hyaluronic acid (HA) in a prospective, randomized cohort study, in adults with the moderate degree of knee OA (Kellgren grade II and III).
2. Material and method
All the patients with moderate OA knee, Kellgren–Lawrence (KL) grade II and III were enrolled in the study. Patient with systemic disorders such as diabetes and thyroid disorder, inflammatory arthritis, major axial deviation at knee joint (varus >5, valgus >5), hematological diseases, e.g. coagulopathy, severe cardiovascular diseases, any infective foci anywhere in the body, immunosuppression, malignancy, age > 80 years, case with history of previous IA injection were excluded from study. A total of 82 patients (142 knees) of both the sexes with a unilateral or bilateral knee pain of more than three months were selected for this study. All of these patients were randomized by computer generated random number table and were given steroid or HA accordingly. Our bilateral knee pain cases were symptomatic for both knee from beginning of study and both knee was injected simultaneously. Forty patients (68 knees) were included in the steroid group. The patients of this group were given IA 40 mg triamcinolone hexa acetate (THA). Forty-two patients (72 knees) were included in HA group and were given IA 6 ml (48 mg) HA (Synvisc-one™, Sanofi, Genzyme). Synvisc (Hylan polymer A and B, G-F 20) contains high molecular weight (HMW) elastoviscous fluid with long chain polymer chemically cross-linked. All the injections were given after aspiration of synovial fluid, under sterile conditions.
Evaluation of pain and function – all patients were examined and data collected as per Knee Society Score (KSS) pain and function score, and Visual Analog Scale (VAS) before injection and at subsequent follow-ups at 1, 4, 12, and 24 weeks.4 All the data was compared both within the group as well as with one another at different follow-up time. Bilateral knee pain case was considered as one patient, because it is difficult to calculate function of individual knee in these patients. Wilcoxon sign rank test is used to compare data within a group. Wilcoxon rank sum test was used to compare data between two separate groups.
3. Results
In both the groups, the patients were matched similar (Table 1). None of the patients, in either group, had any significant complication. However, in steroid group, one patient developed a mild infection, which responded to antibiotic therapy and three patients had a transient rise in blood sugar levels. In HA group, one patient had an acute inflammatory reaction at the site of injection, which settled down in 5 days with ice therapy, anti-inflammatory drugs, and rest.
Table 1.
Baseline demographic and clinical parameters.
| Steroid group | HA group | |
|---|---|---|
| No. of cases (%age) | No. of cases (%age) | |
| Male | 15 (37.5%) | 13 (31%) |
| Female | 25 (62.5%) | 29 (69%) |
| Unilateral | 11 (27.5%) | 11 (26%) |
| Bilateral | 29 (72.5%) | 31 (74%) |
| KL grade II | 22 (55%) | 18 (43%) |
| KL grade III | 18 (45%) | 24 (57%) |
3.1. KSS and VAS in different groups
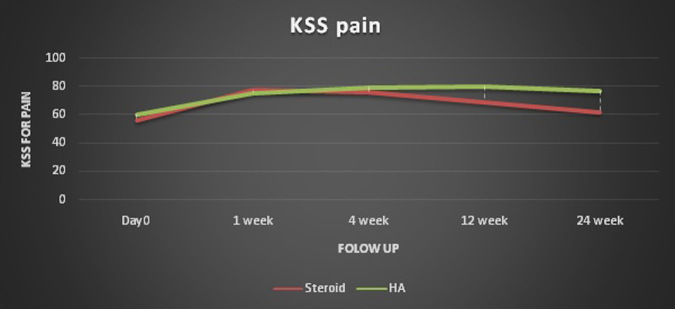
With the improvement in knee pain, the mean of KSS pain and function score increased while VAS decreased, in both groups (Table 2). All the three variables (KSS pain, KSS function, and VAS) had similar trends of improvement. In both the groups, the scores at 24th weeks were significantly better than the baseline data, and the scores of HA group were significantly better compared to steroid group. Baseline data of KSS for function showed statistically no difference (p-value 0.14) between the groups. At one week follow-up, similar improvement was seen on KSS for pain in both the groups with statistically no difference (p-value 0.47), in further follow-up from the fourth week till the end of study KSS for knee pain of HA group was statistically better than steroid group (p-value <0.01) (Fig. 1).
Table 2.
KSS pain, KSS function and VAS score in steroid and HA group.
| KSS pain score |
KSS function score |
VAS score |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Steroid | HA | p-value | Steroid | HA | p-value | Steroid | HA | p-value | |
| Baseline | 55.92 | 60.14 | 0.14 | 50.62 | 52.92 | 0.12 | 4.82 | 5.19 | 0.09 |
| 1st week | 77.30 | 75.56 | 0.47 | 73.25 | 83.41 | 0.16 | 1.75 | 1.87 | 0.34 |
| 4thweek | 75.35 | 79.56 | 0.01 | 71.50 | 73.17 | 0.22 | 2.07 | 1.95 | 0.26 |
| 12th week | 68.82 | 80.24 | <0.01 | 65.25 | 73.90 | <0.01 | 2.8 | 2.34 | <0.01 |
| 24th week | 61.75 | 76.80 | <0.01 | 57.50 | 70.60 | <0.01 | 3.6 | 3.14 | 0.03 |
Fig. 1.
Graph showing KSS pain of steroid and HA at different follow-up period.
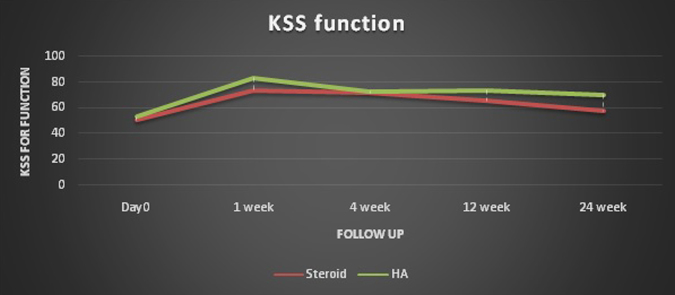
Baseline data of KSS for function showed statistically no difference (p-value 0.47) between the groups. Initial improvement in both groups was similar, though the score of HA group was more but statistically there was no difference in score till four weeks (p-value 0.22) of follow-up. At 12 week follow-up and after that till the end of study HA was statistically better than steroid group (p-value <0.01) (Fig. 2).
Fig. 2.
Graph showing KSS function of steroid and HA at different follow-up period.
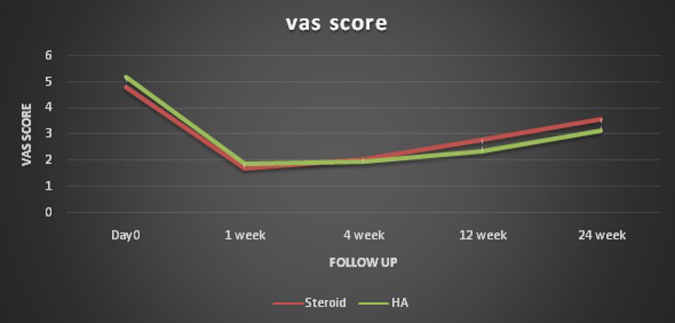
Baseline data of VAS pain score of both groups had statistically no difference (p-value 0.09). Initial improvement in both groups was similar and had no statistical difference till four weeks of follow-up. At 12 week follow-up and after that until the end of study HA was statistically better than steroid group (p-value 0.03) (Fig. 3).
Fig. 3.
Graph showing VAS score of steroid and HA at different follow-up period.
4. Discussion
Five different steroids are approved by Food and Drug Administration that can be given in OA knee. These are triamcinolone hexacetonide (THA), methylprednisolone acetate, betamethasone acetate, triamcinolone acetate, betamethasone sodium phosphate, and dexamethasone. There is some published study that compares the result of different steroids in knee OA but could not document any conclusive results or recommendations. Steroids have both anti-inflammatory and immunosuppressive effects. These agents act on nuclear steroid receptors and interrupt the inflammatory and immune cascade at several steps. Thus, it decreases vascular permeability and inhibits the accumulation of inflammatory cells, phagocytosis, metalloprotease, production of neutrophil superoxide, and prevents the synthesis and secretion of several inflammatory mediators such as prostaglandin and leukotrienes. Clinically it decreases erythema, heat, swelling, and tenderness of the inflamed joints and it also increases the relative viscosity of joint fluid.5 Steroid injections are usually used to treat acute and chronic inflammatory conditions. It decreases acute episodes of pain and increases joint mobility during the flare of knee OA.6 The reported side effects of steroid injection include cortisone flare reaction, softening of the cartilage, the increase in blood sugar level, infection, and development of Cushing syndrome, usually seen after frequent injections.
Valtonen7 in a comparative study (42 patients) between THA and betamethasone found that THA gives pronounced effect and longer duration of pain relief than betamethasone. Five patients in their THA group and 12 patients from betamethasone group needed new treatment after 12 weeks. Jüni et al. 8 in a prospective, randomized, controlled study, compared the effect of methylprednisolone, betamethasone, and triamcinolone and found that the positive effect of all three injection decreases by 12 week time. Methylprednisolone acetate was found to be a statistically more effective analgesic as compared to the other agents until the sixth weeks. We preferred to us THA because of its highest potency, long duration of action and rare flare reaction compared to other steroids.
Hyaluronic acid (HA) is being used in different preparations for viscosupplementation. In a body, HA remains in the form of sodium hyaluronate instead of proton donor acid form. In our study, we have used term HA to represent sodium hyaluronate. Hyaluronic acid is present in dermis and epidermis. It is also present in hyaline cartilage where it organizes the extracellular matrix by creating specific interactions with aggrecan. High molecular weight (HMW) HA is a major component of synovial fluid. It is synthesized and secreted by type B synoviocytes of lining fibroblastic cells of the joint capsule.9 It is about 3–4 ml in each knee and provides lubrication to joint and nutrients to the hyaline cartilage. HA remains in the dynamic state in joint; its half-life is about 12 h.10 Through peroxidative cleavage, HA is removed from joint, and it also helps in maintaining the hypoxic environment in the joint, which is required for normal synovial function and joint homeostasis.11 It is synthesized by three different synthases enzymes known as hyaluronic acid synthase. High molecular weight HA has anti-angiogenic, anti-inflammatory and anti-immunogenic properties.12 The high viscosity of HMW HA grants viscoelastic properties to the fluid that is needed for low friction on the joint surface.13 In a study on an animal model, it had been seen that HA had many different properties like immune-suppressive, anti-inflammatory, antiangiogenic, anti-fibrotic effects, and anti-apoptotic, chondroprotection and normalization of endogenous HA synthesis. It binds to a variety of cell membrane receptors known as hyaladherins; CD44 a commonly expressed hyaladherins.
High-molecular-weight or cross-linked formulations achieved both significant and clinically important pain reductions. Although subgroups are often exploratory, these findings appeared to support further exploration of the specific hyaluronic acid formulation and relying less on the overall class of viscosupplementation effect.
The American Association of Orthopedic Surgery (AAOS) reversed from their earlier position statement that effect of intraarticular HA has the inconclusive result (2008) to strong rating against based on new evidence. Despite significant benefits of hyaluronic acid, these effects did not reach the minimal clinically important difference cut-offs. The previous study failed to account adequately for the placebo additive effect associated with intraarticular knee injections.14, 15
Zavan et al.,16 showed in an experiment the activity of HA on the opioid receptor and beside other action described previously it has analgesic activity through this opioid receptor. This is because of similarity in conformational structures of HA with morphine. It also increases pain threshold. At present, HA preparations are available in different molecular weight. Low molecular weight (LMW) preparations (0.5–1.5 million Dalton) have enhanced diffusion through the extracellular matrix (ECM) of the synovium and interact with synovial cells.17 High molecular weight HA preparation (6–7 million Dalton) because of its hydrophilic property it can retain the high amount of water in joint space. It also decreases migration of inflammatory cell leads and reduced prostaglandin and bradykinin concentration and ultimately anti-inflammatory effect.18
Jones et al.,19 in a randomized study showed that at six months follow-up in inflammatory arthritis HA was superior to THA. He enrolls total 63 patients for study from which 43 were withdrawn before six months because of worsening of the symptoms. Outcomes assessment in that report was done on the Visual Analog Scale.
Leardini et al. in a comparative study between methylprednisolone and HA on 40 patients they found that HA had prolonged action than prednisolone.20 They said that HA would bring the therapeutic breakthrough in the treatment of knee OA. That was a short duration study of only two months, and VAS score was used to measure the outcomes.
Heyworth et al.,21 did a prospective, randomized, double-blinded clinical study of HA, steroid, and placebo. They found that the both steroid and placebo groups showed significant pain relief for ten weeks and its effect disappeared by 12 weeks. While patients of HA group continue to have pain relief until 26 weeks after that, it was not statistically significant.
Merolla et al.,22 used steroid and HA injections in the OA of shoulder and found similar results as of knee OA. The effect of steroid decreased after 1month, but HA remains up to 6 months.
Campbell et al.,23 did a review study of meta-analysis comparing the treatment of knee OA with intra-articular HA versus NSAIDs, IA-corticosteroids, IA-platelet rich plasma (PRP), or IA-placebo to determine which meta-analyses provide the best current evidence and identify potential causes of discordance. They included 14 meta-analysis with total 20,049 patients and found the highest level of evidence suggests that IA-HA is a viable option for knee OA. Compression between HA and PRP, PRP shows more robust result than HA. Like our study, it shows pain and function improvement was significant up to 26 weeks.
Askari et al.,24 compared IA-HA with IA-steroid in 140 cases, in a randomized study. Western Ontario and McMaster University Osteoarthritis Index (WOMAC), Knee Injury and Osteoarthritis Outcome Score (KOOS), and the visual analog pain scale were used in accessing the result. Similar to our study they also found superior results was seen in HA group than the steroid.
The present study demonstrated that both the THA and HA are safe and effective in relieving OA pain temporarily and are effective palliative agents and are not curative therapy. Steroid given IA can give pain relief for about 12 weeks while HA provides significant pain relief until six months after the injection.
Conflict of interest
The authors have none to declare.
Contributor Information
Raju Vaishya, Email: raju.vaishya@gmail.com.
Ramsagar Pandit, Email: ramsagarpandit7@gmail.com.
Amit Kumar Agarwal, Email: amitorthopgi@yahoo.co.in.
Vipul Vijay, Email: dr_vipulvijay@yahoo.com.
References
- 1.Zhang W., Nuki G., Moskowitz R.W. OARSI recommendations for the management of hip and knee osteoarthritis. Part III. Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18:46–499. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 2.Vaishya R., Pariyo G.B., Agarwal A.K., Vijay V. Non-operative management of osteoarthritis of the knee joint. J Clin Orthop Trauma. 2016;7(3):170–176. doi: 10.1016/j.jcot.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kon E., Filardo G., Drobnic M. Non-surgical management of early knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):436–449. doi: 10.1007/s00167-011-1713-8. [DOI] [PubMed] [Google Scholar]
- 4.Insall J.N., Dorr L.D., Scott R.D. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 5.Ostergaard M., Halberg P. Intra-articular corticosteroids in arthritic disease: a guide to treatment. BioDrugs. 1998;9(2):95–103. doi: 10.2165/00063030-199809020-00002. [DOI] [PubMed] [Google Scholar]
- 6.Rozental T.D., Sculco T.P. Intra-articular corticosteroids: an updated overview. Am J Orthop (Belle Mead NJ) 2000;29(1):18–23. [PubMed] [Google Scholar]
- 7.Valtonen E.J. Clinical comparison of THA and betamethasone in the treatment of osteoarthrosis of the knee-joint. Scand J Rheumatol Suppl. 1981;41:1–7. [PubMed] [Google Scholar]
- 8.Jüni P., Hari R., Rutjes A.W. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev. 2015;(10):CD005328. doi: 10.1002/14651858.CD005328.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reitinger S., Lepperdinger G. Hyaluronan, a ready choice to fuel regeneration: a mini review. Gerontology. 2013;59:71–76. doi: 10.1159/000342200. [DOI] [PubMed] [Google Scholar]
- 10.Fraser J.R., Laurent T.C., Laurent U.B. Hyaluronan: its nature, distribution, functions and turnover. J Intern Med. 1997;242(1):27–33. doi: 10.1046/j.1365-2796.1997.00170.x. [DOI] [PubMed] [Google Scholar]
- 11.Juranek I., Stern R., Soltes L. Hyaluronan peroxidation is required for normal synovial function: a hypothesis. Med Hypotheses. 2014;82(6):662–666. doi: 10.1016/j.mehy.2014.02.024. [DOI] [PubMed] [Google Scholar]
- 12.Zhang F.J., Luo W., Gao S.G. Expression of CD44 in articular cartilage is associated with disease severity in knee OA. Mod Rheumatol. 2013;23(6):1186–1191. doi: 10.1007/s10165-012-0818-3. [DOI] [PubMed] [Google Scholar]
- 13.Musumeci G., Loreto C., Carnazza M.L. Acute injury affects lubricin expression in knee menisci: an immunohistochemical study. Ann Anat. 2013;195(2):151–158. doi: 10.1016/j.aanat.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 14.Jevsevar D., Donnelly P., Brown G.A. Viscosupplementation for osteoarthritis of the knee: a systematic review of the evidence. J Bone Joint Surg Am. 2015;97(24):2047–2060. doi: 10.2106/JBJS.N.00743. [DOI] [PubMed] [Google Scholar]
- 15.Zhang W., Robertson J., Jones A.C., Dieppe P.A., Doherty M. The placebo effect and its determinants in osteoarthritis: a meta-analysis of randomized controlled trials. Ann Rheum Dis. 2008;67(12):1716–1723. doi: 10.1136/ard.2008.092015. [DOI] [PubMed] [Google Scholar]
- 16.Zavan B., Ferroni L., Giorgi C. HA induces activation of the κ-opioid receptor. PLOS ONE. 2013;8(1):e55510. doi: 10.1371/journal.pone.0055510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bagga H., Burkhardt D., Sambrook P., March L. Long-term effects of IA hyaluronan on synovial fluid in osteoarthritis of the knee. J Rheumatol. 2006;33(5):946–950. [PubMed] [Google Scholar]
- 18.Migliore A., Giovannangeli F., Granata M., Laganà B. Hylan G-F20: review of its safety and efficacy in the management of joint pain in OA. Clin Med Insights Arthritis Musculoskelet Disord. 2010;3:55–68. [PMC free article] [PubMed] [Google Scholar]
- 19.Jones A.C., Pattrick M., Doherty S., Doherty M. Intra-articular HA compared to intra-articular THA in inflammatory knee OA. Osteoarthritis Cartilage. 1995;3(4):269–273. doi: 10.1016/s1063-4584(05)80018-4. [DOI] [PubMed] [Google Scholar]
- 20.Leardini G., Mattara L., Franceschini M., Perbellini A. Intra-articular treatment of knee OA. A comparative study between hyaluronic acid and 6-methyl prednisolone acetate. Clin Exp Rheumatol. 1991;9(4):375–381. [PubMed] [Google Scholar]
- 21.Heyworth B.E., Lee J.H., Kim P.D., Lipton C.B., Strauch R.J., Rosenwasser M.P. Hylan versus corticosteroid versus placebo for treatment of basal joint arthritis: a prospective, randomized, double-blinded clinical trial. J Hand Surg Am. 2008;33(1):40–48. doi: 10.1016/j.jhsa.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Merolla G., Sperling J.W., Paladini P., Porcellini G. Efficacy of Hylan G-F 20 versus 6-methylprednisolone acetate in painful shoulder OA: a retrospective controlled trial. Musculoskelet Surg. 2011;95(3):215–224. doi: 10.1007/s12306-011-0138-3. [DOI] [PubMed] [Google Scholar]
- 23.Campbell K.A., Erickson B.J., Saltzman B.M. Is local viscosupplementation injection clinically superior to other therapies in the treatment of OA of the knee: a systematic review of overlapping meta-analyses. Arthroscopy. 2015;31(10) doi: 10.1016/j.arthro.2015.03.030. 2036–45.e14. [DOI] [PubMed] [Google Scholar]
- 24.Askari A., Gholami T., NaghiZadeh M.M., Farjam M., Kouhpayeh S.A., Shahabfard Z. Hyaluronic acid compared with corticosteroid injections for the treatment of osteoarthritis of the knee: a randomized control trail. Springerplus. 2016;5:442. doi: 10.1186/s40064-016-2020-0. [DOI] [PMC free article] [PubMed] [Google Scholar]