Abstract
Background
Intramedullary and extramedullary strategies of pertrochanteric fracture fixation are still controversial, but new percutaneous devices may give advantages regarding operative time, blood loss and rate of cardiovascular complications. We retrospectively analyze our cases regarding Anteversa® plate (Intrauma, Turin, Italy) fixation of pertrochanteric femoral fractures, focusing on the correlation between two radiographical parameters (tip-apex distance “TAD” and calcar referenced tip-apex distance “CalTAD”) and the occurrence of cut-out. The purpose of this study was to determine if these predicting factors of cut-out are reliable in the treatment of proximal femoral fractures with the Anteversa plate.
Methods
A series of 77 patients with 53 31-A1 fracture types and 24-A2 fractures completed a 12-month-follow-up. Clinical outcomes were evaluated according to Parker-Palmer Mobility Score at the final follow-up. TAD and CalTAD were considered to determine their correlation with cut-out events.
Results
The mean Parker-Palmer Score was 6.94 in A1 group and 7.41 in A2 group (p = 0.47). Mean value of TAD index was 29.58, 29.81 in the A1 group and 29.08 in the A2 group, and mean value of CalTAD index was 30.87, 31.03 in the A1 group and 30.50 in the A2 group. We observed 3 cases of implant cut-out. We shared our sample in two groups, one group with TAD and CalTAD indices lower than 25 mm and another group higher than 25 mm to evaluate how the Palmer Parker score changed and no statistical differences were found between the two groups.
Conclusions
Taking into consideration that good clinical results were obtained for TAD and CalTAD values superior to 25 mm, the prognostic value of 25 mm of TAD and CalTAD indices might not be appropriate to this new percutaneous plate.
Keywords: Pertrocahanteric fracture, Extramedullary devices, Cut-out, Tip-apex distance (TAD), Calcar referenced tip-apex distance (CalTAD)
1. Introduction
Proximal femoral fractures (PFF), place a heavy demand on orthopaedic departments worldwide, and annual volume of this type of injury is growing up every year.1
There is a considerable controversy regarding which the optimal implant is for fixing extracapsular fractures. Options for treating trochanteric fractures include extramedullary fixation and intramedullary fixation. Stable fractures (AO classification 31-A1 and 31-A2) are conventionally treated using a sliding hip screw (SHS) or a dynamic hip screw (DHS), rather than intramedullary nailing, due to similar functional outcomes and advantageous cost-benefit ratio.2, 3 Percutaneous plate fixation adds advantages regarding reduction of operative time, blood loss and cardiovascular events.4, 5, 6, 7 Literature reported a correlation between major complications, such as cut-out of the implant, and values of the tip-apex distance (TAD)8 and calcar referenced tip-apex distance (CalTAD)9 parameters. The question is whether these parameters preserve their reproducibility and validity with new fixation devices, which have different mechanical properties.
The aim of our study is to determine if these predicting factors of cut-out are reliable in the treatment of proximal femoral fractures with the Anteversa® plate fixation device (Intrauma, Turin, Italy), considering clinical and radiographic outcomes, and postoperative complications.
2. Methods
We reviewed retrospectively patients admitted to our Unit from January 2012 to February 2015 with a diagnosis of intertrochanteric femoral fracture and surgically treated with Anteversa® plate. The Anteversa® plate is an extramedullary device with a cephalic screw and cephalic anti-rotational pin (cervico-diaphyseal angle of 130° and anteversion angle of 8°) and two distal locking screws. The plate can be positioned on the lateral surface of the proximal femoral diaphysis, thus allowing the screw and pin to pass through the centre of the neck of the femur. The diameter of lag cephalic screw is 8 mm in the core and 11 mm in the threaded portion, anti-rotational pin is 5 mm of diameter. The implant is made of steel AISI 316LVM-ISO 5832-1 to allow MRI. Implant design allows a minimally invasive approach using lesser trochanter as a radiographic landmark with a skin incision of about 5 cm (Fig. 1).
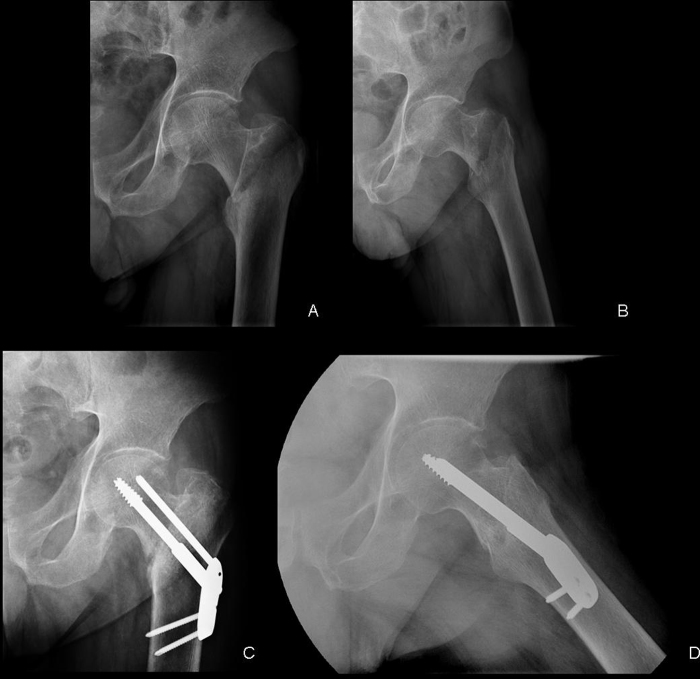
Fig. 1.
A patient with pertrochanteric fractures 31-A2 (A, B) treated with Anteversa® plate, anteroposterior view (C) and lateral view (D).
Data regarding general information, history, clinical and radiological findings, surgery and follow-up of the patients were collected from our hospital electronical database (SAP) clinical records. The fractures were classified by the senior author (L.M.) according to the AO classification10 and The Orthopaedic Trauma Association Classification of Fractures.11 We included pertrocanteric femoral fractures, 31-A1 and 31-A2 types according to AO-OTA classification. We excluded patients with a minimum follow-up inferior to 12 months and those cases with inadequate radiographic imaging. Patients were followed-up for one year minimum; patients who died within one year since the date of the surgery were excluded. The fracture classification, quality of fracture reduction, position of the Lag screw, tip apex distance (TAD)10 and the calcar referenced tip-apex distance (CalTAD)11 were determined with the use of preoperative and postoperative anteroposterior and lateral digital radiographs (Fig. 2). All specifications were measured with the Picture Archiving and Communication System (PACS). An earlier study showed that the PACS is suitable for measuring the tip-apex distance.12 The postoperative quality of fracture reduction was described as good, acceptable, or poor, according to the definitions of the three-grade classification system proposed by Baumgaertner.13 A good reduction is classified as normal or slight valgus alignment on the anteroposterior radiograph, <20° of angulation on the lateral radiograph, and ≤4 mm of displacement of any fragment. An acceptable reduction has to meet the criteria for a good reduction, but for either the alignment or the displacement, not for both. A poor reduction meets none of the criteria. Immediate weight-bearing was allowed after the evaluation of postoperative X-rays, when the quality of reduction and the position of the implant were considered good ones by the senior author (L.M.). Furthermore, we measured TAD and CalTAD indices, which have been proved to be predictors of lag screw cut-out.10, 11, 15
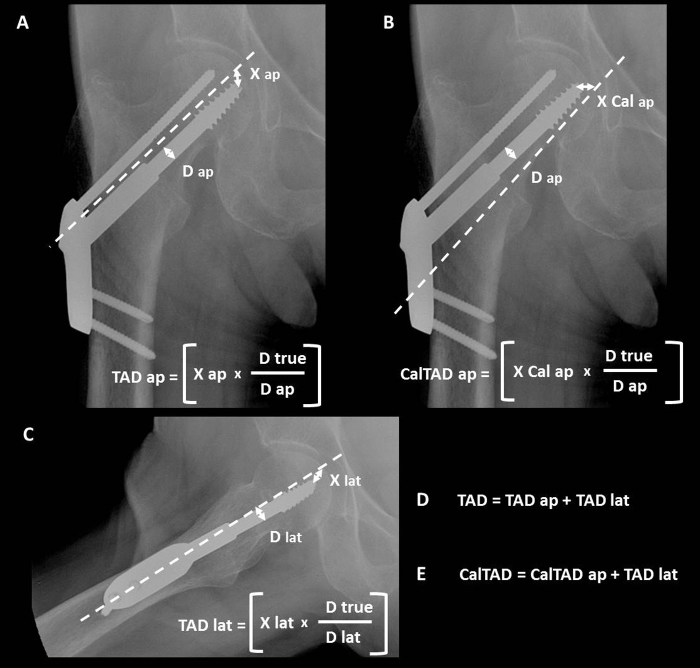
Fig. 2.
(A) Tip-apex distance calculated on anteroposterior radiograph (TAD ap); (B) Tip-apex distance as referenced to the calcar calculated on the anteroposterior radiograph (CalTAD ap); (C) Tip-apex distance calculated on the lateral radiograph (TAD lat); (D) Tip-apex distance (TAD); (E) Calcar referenced tip-apex distance (CalTAD). D true is the known diameter of the lag screw (8 mm). D ap is the calculated diameter of the lag screw on the anteroposterior radiograph. D lat is the calculated diameter of the lag screw on the lateral radiograph.
Observer-blinded functional assessment was carried out by the unit research physiotherapist using the Parker-Palmer score16 at 12 months after surgery. The Parker-Palmer score was classified as excellent (8–9 points), good (6–7 points), fair (4–5 points) and poor (<3 points).
The incidence of any postoperative complication was recorded. Among major complications we took into consideration implant cut-out. On the other hand minor complications included mobilization of the anti-rotational pin and surgical wound healing problems.
2.1. Statistical analysis
We used the software Stata to run regressions to assess whether the Tad Index and the CalTad Index have a significant impact on the Palmer score. In particular, we regressed the Palmer score on the Tad Index; its coefficient is not significant. We obtained the same result regressing the Palmer score on the CalTad Index. We assumed 5% to be the relevant level of significance, but even at 10% the outcome is the same. These findings suggest that these two indices are not good measures to determine the success of surgery. However, our sample is quite small and further analysis should be conducted to confirm our findings.
2.2. Ethics
This study was approved by the ethics committee of Ferrara (AOU Ferrara Italy). Written informed consent to participate and to share data anonymously were obtained from all participants.
3. Results
90 patients with intertrochanteric hip fractures treated with Anteversa® plate were identified. No bilateral fractures were observed. 2 patients, who did not undergo a complete follow-up at 12 months postoperatively, were excluded. 8 patients died within a year after surgery and were excluded too. The quality of 3 of the postoperative radiographs was too poor to check the femoral head properly, thus these patients were excluded. Therefore, according to our inclusion and exclusion criteria, 77 patients were suitable for our study.
There were 50 women (65%) and 27 men (35%) with a mean age (and standard deviation) of 81.27 ± 9.37 years. Fracture pattern was AO A1 in 53 patients (69%) and A2 in 24 (31%) as shown in Table 1.
Table 1.
Patient data.
| Variables | Value | Percentage (%) |
|---|---|---|
| Number of patients | 77 | |
| Mean age | 81 | |
| Gender | ||
| Male | 27 | 35 |
| Female | 50 | 65 |
| AO fracture types | ||
| A1 | 53 | 69 |
| A2 | 24 | 31 |
Post-operative reduction was considered good or acceptable in 71 patients (92%) and immediate weight-bearing was allowed post-operatively in this group. In the remaining 6 patients reduction was poor and weight-bearing was postponed until the first radiological follow-up examination as outpatients (35 days). Mean time of fracture healing was 13.6 ± 2.3 weeks.
The mean Palmer-Parker score was 7.09 ± 2.15 points; 6.94 ± 2.38 points in the group of A1 fracture type, 7.41 ± 1.55 in the group of A2 fracture type. The Palmer-Parker Score was not significantly different in the two fracture patterns (p = 0.47) as shown in Table 2.
Table 2.
Outcomes in relation with AO fracture types.
| A1 | A2 | p value | |
|---|---|---|---|
| Number of patients | 53 | 24 | |
| Mean time to bone healing (week) | 14 | 12 | |
| Mean Parker-Palmer score (point) | 6.94 | 7.41 | 0.47 |
| Mean TAD | 29.81 | 29.08 | 0.72 |
| Mean CalTAD | 31.03 | 30.50 | 0.53 |
Among minor complications, incorrect positioning and mobilization of the anti-rotational pin were found in 9.43% (n = 5) of the A1 fracture pattern, in 4.16% (n = 1) of the A2 fracture pattern. Considering major complications, we observed 3 cases of implant cut-out (1 case in the group of the A1 type and 2 cases in the group of the A2 type) with mean TAD value of 40.27 and mean CalTAD value of 42.47; their characteristics are illustrated in Table 3.
Table 3.
Characteristics of 3 cases of implant cut-outs.
| Case of cut-outs | Type of fracture | Age | Gender | TAD | CalTAD |
|---|---|---|---|---|---|
| 1 | A1 | 83 | F | 37.6 | 43.59 |
| 2 | A2 | 88 | F | 46.23 | 47.64 |
| 3 | A2 | 74 | M | 37.0 | 36.2 |
Mean value of TAD index is 29.58 ± 9.24, 29.81 ± 9.31 in the A1 group and 29.08 ± 9.26 in the A2 group. Mean value of CalTAD index is 30.87 ± 8.70, 31.03 ± 8.68 in the A1 group and 30.50 ± 8.91 in the A2 group.
Taking into account mean values of TAD and CalTAD, among our different groups of fractures, no statistically significant difference was shown with p-values of 0.72 and 0.53 respectively (Table 2).
4. Discussion
In literature there is an ongoing controversy about the optimal treatment strategy for different fracture types of the proximal femur. Intramedullary and extramedullary strategies were analyzed by biomechanical and functional aspects as well as the incidence of mechanical failure. In our study, we reviewed a fixation device, which is mainly indicated for intertrochanteric fractures with intact lateral wall (AO type 31.A1, 31.A2) taking advantage of providing rotational stability, obtained by anti-rotational pin in the femoral neck. A central-posterior placement of the implanted hip screw in the lateral radiographic view and a central-inferior position in the anteroposterior view are recommended.14, 15, 16, 17
Regarding TAD and CalTAD indices, some authors identified the prognostic value with a maximum of 25 mm to prevent post-operative complications such as implant cut-out.13
Cut-out failure has been found as one of the most important mechanical complications after intra-medullary and extra-medullary treatments with an incidence between 1.4% and 19% depending on fracture type and implants used.18, 19, 20
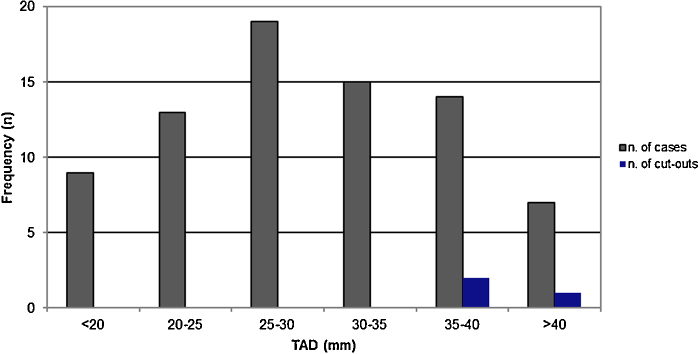
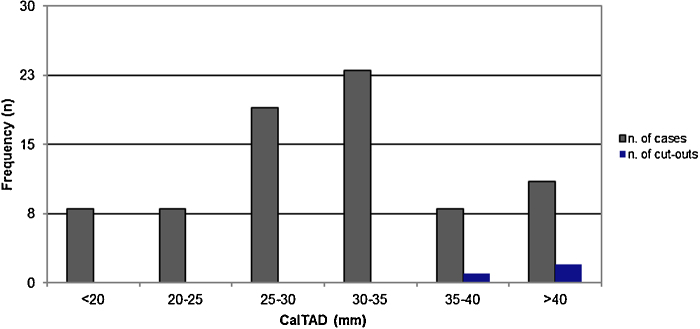
Regarding our good clinical outcomes (mean Palmer value of 7.09 ± 2.15), we would have expected that most values of TAD and CalTAD indices were inferior to the prognostic value of 25 mm. Instead, most values (n TAD = 55; n CalTAD = 61) were superior to this prognostic value, as shown in the charts in Fig. 3, Fig. 4.
Fig. 3.
Chart showing the distribution of TAD values and frequencies of cut-outs.
Fig. 4.
Chart showing the distribution of CalTAD values and frequencies of cut-outs.
We shared our sample in two groups, one group with TAD and CalTAD indices lower than 25 mm and another group higher than 25 mm to evaluate how the Palmer Score changed. Mean values of Palmer score were 7.5 and 6.98 respectively in the groups with CalTAD lower than 25 mm and higher than 25 mm. Meanwhile, mean values of Palmer score were 7.54 and 6.90 respectively in the groups with TAD lower than 25 mm and higher than 25 mm. No statistical differences were found between the two groups (p TAD = 0.63; p CalTAD = 0.51), as shown in Table 4.
Table 4.
Mean values of Palmer Score among groups with TAD value and CalTad value lesser or higher than thresold of 25 mm.
| TAD value < 25 mm | Tad value > 25 mm | p value | |
|---|---|---|---|
| Palmer | 7.54 | 6.90 | 0.63 |
| CalTAD value < 25 mm | CalTad value > 25 mm | p value | |
|---|---|---|---|
| Palmer | 7.50 | 6.98 | 0.51 |
Despite small sample size limitations, we could assume that those indices do not seem to have a considerable influence on the clinical outcomes in patients treated with Anteversa plate. Notwithstanding the most values were superior to 25 mm, we observed only 3 cases of cut-out. Perhaps the prognostic value of 25 mm could not be reliable for this new fixation device.
Studies in literature which have identified the value of 25 mm as a cut-off were done using fixation devices with structural and biomechanical properties different from Anteversa plate.
Taking into consideration that good clinical results were obtained even for TAD and CalTAD values superior to 25 mm, we do believe that further clinical studies on this new fixation device should be performed to measure again these indices.
In our experience with Anteversa® we analyzed both TAD and CalTAD values, due to the lower placement of the cephalic screw for this implant, but neither of them have shown a threshold, able to predict the cut-out. Previous reported values do not seem to be applicable to our court of patients; there might be other factors involved in the development of this type of complication. As far as we are concerned, the prognostic value of 25 mm of TAD and CalTAD indices might not be appropriate to this new percutaneous plate. New prospective randomized trials could be useful to find a more suitable cut-off value for this new fixation device.
Conflicts of interest
The authors have none to declare.
References
- 1.White S.M., Griffiths R. Projected incidence of proximal femoral fracture in England: a report from the NHS Hip Fracture Anaesthesia Network (HIPFAN) Injury. 2011;42(11):1230–1233. doi: 10.1016/j.injury.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Swart E., Makhni E.C., Macaulay W., Rosenwasser M.P., Bozic K.J. Cost-effectiveness analysis of fixation options for intertrochanteric hip fractures. J Bone Jt Surg Am. 2014;96:1612–1620. doi: 10.2106/JBJS.M.00603. [DOI] [PubMed] [Google Scholar]
- 3.Parker M.J., Handoll H.H. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2010;(September (9)):CD000093. doi: 10.1002/14651858.CD000093.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Ma J., Xing D., Ma X. The percutaneous compression plate versus the dynamic hip screw for treatment of intertrochanteric hip fractures: a systematic review and meta-analysis of comparative studies. Orthop Traumatol Surg Res. 2012;98:773–783. doi: 10.1016/j.otsr.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Zhou Z., Zhang X., Tian S., Wu Y. Minimally invasive versus conventional dynamic hip screw for the treatment of intertrochanteric fractures in older patients. Orthopedics. 2012;35(February (2)):e244–e249. doi: 10.3928/01477447-20120123-42. [DOI] [PubMed] [Google Scholar]
- 6.Zakaria M., Benoit O., Desrousseaux J.F., Rakotonarivo M., Polveche G., Cordonnier D. Percutaneous compression plate for pertrochanteric fixation of hip fractures: surgical technique and first results. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(September (5)):465–469. doi: 10.1016/s0035-1040(05)84364-8. French. [DOI] [PubMed] [Google Scholar]
- 7.Gotfried Y. Percutaneous compression plating of intertrochanteric hip fractures. J Orthop Trauma. 2000;14(September–October (7)):490–495. doi: 10.1097/00005131-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 8.De Bruijn K., den Hartog D., Tuinebreijer W., Roukema G. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J Bone Jt Surg Am. 2012;94(July (14)):1266–1272. doi: 10.2106/JBJS.K.00357. [DOI] [PubMed] [Google Scholar]
- 9.Kashigar A., Vincent A., Gunton M.J., Backstein D., Safir O., Kuzyk P.R. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Jt J. 2014;96-B(August (8)):1029–1034. doi: 10.1302/0301-620X.96B8.33644. [DOI] [PubMed] [Google Scholar]
- 10.Meling T., Harboe K., Enoksen C.H., Aarflot M., Arthursson A.J., Søreide K. How reliable and accurate is the AO/OTA comprehensive classification for adult long bone fractures? J Trauma Acute Care Surg. 2012;73(July (1)):224–231. doi: 10.1097/TA.0b013e31824cf0ab. [DOI] [PubMed] [Google Scholar]
- 11.Marsh J.L., Slongo T.F., Agel J. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(November–December (10 Suppl.)):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 12.Johnson L.J., Cope M.R., Shahrokhi S., Tamblyn P. Measuring tip-apex distance using a picture archiving and communication system (PACS) Injury. 2008;39:786–790. doi: 10.1016/j.injury.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 13.Baumgaertner M.R., Curtin S.L., Lindskog D.M., Keggi J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Jt Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Parker M.J., Palmer C.R. A new mobility score for predicting mortality after hip fracture. J Bone Jt Surg Br. 1993;75(September (5)):797–798. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 15.Lobo-Escolar A., Joven E., Iglesias D., Herrera A. Predictive factors for cutting-out in femoral intramedullary nailing. Injury. 2010;41(12):1312–1316. doi: 10.1016/j.injury.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 16.Guven M., Yavuz U., Kadioglu B. Importance of screw position in intertrochanteric femoral fractures treated by dynamic hip screw. Orthop Traumatol Surg Res. 2010;96(1):21–27. doi: 10.1016/j.rcot.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Hsueh K.K., Fang C.K., Chen C.M., Su Y.P., Wu H.F., Chiu F.Y. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: an evaluation of 937 patients. Int Orthop. 2010;34(8):1273–1276. doi: 10.1007/s00264-009-0866-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bojan A.J., Beimel C., Speitling A., Taglang G., Ekholm C., Jonsson A. 3066 consecutive gamma nails. 12 years experience at a single centre. BMC Musculoskelet Disord. 2010;11:133. doi: 10.1186/1471-2474-11-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mereddy P., Kamath S., Ramakrishnan M., Malik H., Donnachie N. The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury. 2009;40(4):428–432. doi: 10.1016/j.injury.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Verhofstad M.H., van der Werken C. DHS osteosynthesis for stable pertrochanteric femur fractures with a two-hole side plate. Injury. 2004;35(10):999–1002. doi: 10.1016/j.injury.2003.10.030. [DOI] [PubMed] [Google Scholar]