Abstract
Sedatives are commonly used for mechanically ventilated patients in intensive care units (ICU). However, a variety of sedatives are available and their efficacy and safety have been compared in numerous trials with inconsistent results. To resolve uncertainties regarding usefulness of these sedatives, we performed a systematic review and network meta-analysis. Randomized controlled trials comparing sedatives in mechanically ventilated ICU patients were included. Graph-theoretical methods were employed for network meta-analysis. A total of 51 citations comprising 52 RCTs were included in our analysis. Dexmedetomidine showed shorter MV duration than lorazepam (mean difference (MD): 68.7; 95% CI: 18.2–119.3 hours), midazolam (MD: 10.2; 95% CI: 7.7–12.7 hours) and propofol (MD: 3.4; 95% CI: 0.9–5.9 hours). Compared with dexmedetomidine, midazolam was associated with significantly increased risk of delirium (OR: 2.47; 95% CI: 1.17–5.19). Our study shows that dexmedetomidine has potential benefits in reducing duration of MV and lowering the risk of delirium.
The management of critically ill patients often requires invasive and uncomfortable procedures such as tracheal intubation and physical restraint. Furthermore, the intensive care unit (ICU) environment is filled with noise, which greatly exaggerates the stress and anxiety of conscious patients1. There is evidence that stress and anxiety have adverse effects on clinical outcomes, and prevention of exposure to environmental noise can help to improve outcome2,3. An alternative but important modality is the use of sedatives to prevent critically ill patients from being exposed to hazardous physical and psychological stimulus4.
Mechanical ventilation (MV) is among the most commonly used techniques in the ICU. Because of its invasiveness, MV usually brings stressful, uncomfortable and even painful experience to ICU patients5,6. MV patients are at increased risk of developing delirium7. Therefore, international guideline recommends routine use of sedation to fully prevent patients from exposure to these adverse stimuli. However, there is a variety of sedatives that are available for clinical use, including midazolam, dexmedetomidine, propofol and lorazepam8. They have different advantages and limitations in clinical use, due to their distinct pharmacological properties. In clinical practice, clinicians usually face with the choice between multiple alternative sedatives. The choice may become difficult when investigators have undertaken head-to-head comparisons of only some of available sedatives. Network meta-analysis allows for simultaneous comparisons of multiple sedatives against each other, providing direct evidence on the choice among multiple sedatives. In this study we performed a systematic review and network meta-analysis of the efficacy and safety of these sedatives, in the hope that it will provide updated and unbiased evidence for clinical practice.
Methods
Study population and registration
The study population was critically ill adult patients who required MV. Critically ill patients were defined as those treated in the ICU and were defined as per the original studies. MV included both invasive and non-invasive modes. Pediatric patients (younger than 12 years old) were excluded. Patients included medical patients requiring long-term MV and patients underwent major operation that were transferred to ICU. The study was registered at PROSPERO (CRD42016041920).
Interventions
Sedatives of any types were deemed suitable for inclusion. However, studies investigating sedation protocol but the types of sedatives are not distinguishable were excluded. Sedatives included midazolam, dexmedetomidine, propofol, clonidine and lorazepam. Studies with one arm involving these sedatives were included. The other arms can be atypical sedatives such as haloperidol, morphine and combination of two types of sedatives. Dexmedetomidine was employed as the base comparator, and other sedatives were compared to it.
Outcomes
The primary outcome was the duration of MV. Other outcomes included Richmond Agitation Sedation Scale (RASS), Ramsay Sedation Scale (RSS), ICU and hospital length of stay (LOS).
Search strategy and data extraction
Electronic databases including Pubmed, SCOPUS, ISI web of science, and EMBASE were searched from inception to April 2016. There was no language restriction. Search items included core terms related to critical care, mechanical ventilation, outcomes and sedatives. Examples of searching strategy in PubMed and SCOPUS, as well as the number of extracted citations were provided in supplemental file. Reference lists of relevant articles were screened by hand for potential eligible studies.
Custom-made form was employed to extract data from included trials. Characteristics of studies included the name of the first author, publication year, type of study population, sample size, comparator in each arm and study outcomes. Numerical data on the number of participants in each arm, names of comparators, number of events in each arm, and mean (standard error) were extracted. Two authors (X.Z. and H.F.) independently extracted data, and disagreement was settled by a third opinion (Z.Z.). If the original article reported median and interquartile range, its distribution was assumed to be normal. Data on mean and standard error can be derived according to normal distribution rules. Some continuous outcomes were reported in median and range. They were converted to mean (standard error) according to the equations proposed by Hozo and coauthors9.
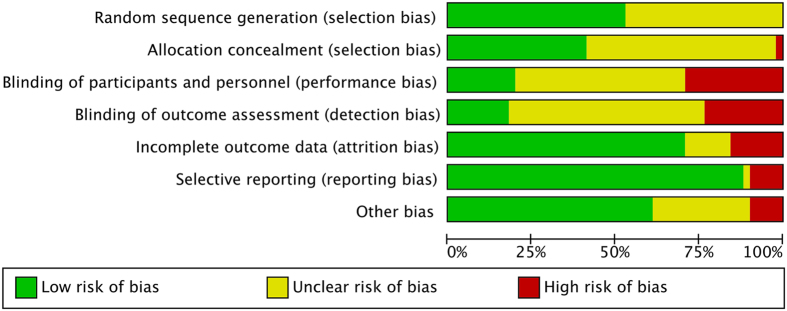
Quality assessment of component trials
Only randomized controlled trials were included in our study. Therefore, the qualities of trials were assessed in six aspects: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessor (5) incomplete data outcome, (6) selective reporting, and (7) other bias. These items were adapted from the Cochrane Collaboration’s tool for assessing risk of bias10.
Statistical analysis
There were two types of outcome data: continuous and binary outcomes. The former included ICU and hospital LOS, and duration of MV. RASS and RSS were ordinal variables. Binary outcomes included mortality, atrial fibrillation and delirium. Mean difference (MD) was reported for the comparison of continuous outcomes between interventions, and odds ratio (OR) was reported for binary outcomes.
Graph-theoretical methods, which have been routinely applied to electrical networks, were employed for network meta-analysis11. Direct comparisons between sedatives were derived from each of the two-arm trials, and were represented by edges in a network plot. Effect sizes from component trials were weighted by the inverse of the observed variance of the treatment effect. For a meta-analytic network, the node corresponds to a treatment strategy, and the edge represents the existing comparisons between treatments. Each two-arm study (e.g. randomized controlled trial) contributes to one comparison. The thickness of the edge is proportional to inverse standard error of random effects model comparing two treatments. Additionally, we employed net heat plot to highlight hot spots of inconsistency between specific direct and indirect evidence in the whole network12. The area of a gray square displays the contribution of the direct estimate of one design in the column to a network estimate in a row. The colors are associated with the change in inconsistency between direct and indirect evidence in row design after detaching the effect of column design. Forest plots were employed to show the effect size of each drug, by setting dexmedetomidine as the reference. Effect sizes and corresponding 95% confidence intervals were reported in the forest plots. All statistical analyses were performed using R (version 3.2.3)13.
Results
Included studies and characteristics
The initial search identified 598 citations. Another 9 studies were added from the references of relevant articles (Fig. 1). After removing duplicates, a total of 203 citations remained for further screening. The titles and abstracts were screened by hand and 125 were excluded because 18 were related to anesthesia, one was animal study, 57 were irrelevant studies, 12 were observational studies, 11 involved pediatric patients, and 26 were reviews. The full-text articles of the remaining 78 citations were screened. Twenty-seven articles were excluded because 20 investigated sedation protocol that the type of sedative drugs could not be identified, 4 studies were secondary analysis of previous reports, and 3 were study protocols. As a result, a total of 51 citations comprising 52 RCTs were included in our analysis14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64. The article by Jakob and colleagues comprised two RCTs38. Characteristics of component trials are shown in Table 1. These articles were published between the year 1989 and 2016. Study populations included patients underwent major operations requiring ICU admission, and those requiring long-term MV. The sample sizes in included trials ranged from 20 to 500. Most of the trials were two-arm trials, and there were five three-arm trials20,35,42,63,64. Study endpoints included duration of MV, Richmond Agitation Sedation Scale (RASS), Ramsay Sedation Scale (RSS), ICU and hospital length of stay (LOS). Adverse events included bradycardia, hypotension and death.
Figure 1. PRISMA flow diagram for study inclusion.
Table 1. Characteristics of included studies.
| Studies | Study population or setting | Sample size | Comparators | Outcomes |
|---|---|---|---|---|
| Abd Aziz14 | Cardiac surgery | 28 | DEX; morphine | Sedation scores; pain; HR; ABP; extubation time |
| Aghdaii15 | CABG | 50 | Propofol; Midazolam | BP; HR; extubation time; ICU LOS |
| Aitkenhead16 | MV > 12 H | 101 | Propofol; Midazolam | MV duration; BP; HR; biochemistry profile |
| Aydogan17 | Scoliosis surgery | 32 | DEX; Midazolam | Adverse events; MV duration; ICU LOS |
| Balkanay18 | CABG | 90 | Placebo; DEX | Renal injury; hospital and ICU stay |
| Barrientos-Vega19 | MV > 24 h | 108 | Propofol; Midazolam | Cost; extubation time; mortality; |
| Carrasco20 | CABG | 75 | Propofol; Midazolam; Propofol + Midazolam | HR; BP; extubation time |
| Carson21 | Medical ICU; MV > 48 hours | 132 | Lorazepam; propofol | Ventilator days; 28-day ventilator-free survival, ICU and hospital LOS, and hospital mortality. |
| Cernaianu22 | MV | 95 | Lorazepam; Midazolam | HR; MAP; hemodynamic parameters; |
| Chamorro23 | MV > 48 h | 98 | Propofol; Midazolam | Sedation efficacy; hypotension; |
| Corbett24 | CABG | 89 | DEX; propofol | Perception of ICU experience |
| Djaiani25 | Cardiac surgery | 183 | DEX; propofol | Delirium; extubation time; |
| Abdulatif26 | MV | 40 | DEX; propofol | |
| Elbaradie27 | Postoperative MV | 60 | DEX; propofol | RSS; BIS; extubation time |
| Eremenko28 | Cardiac surgery | 55 | DEX; propofol | Duration of MV; adverse events; |
| Esmaoglu29 | Eclampsia | 40 | Midazolam; DEX | Heart rate, blood pressure, RSS; ICU LOS; |
| Gupta30 | Postabdominal surgery MV > 24 h | 40 | Midazolam; DEX | Heart rate; ICU LOS; duration of MV |
| Hall31 | MV | 99 | Midazolam; propofol | ICU LOS; duration of MV |
| Hellström32 | Cardiac surgery | 99 | Sevoflurane; propofol | ICU and hospital LOS; duration of MV; agitation |
| Herr33 | CABG | 295 | DEX; propofol | Adverse events; extubation time |
| Higgins34 | CABG | 84 | Propofol; midazolam | HR; BP; cardiac output |
| Hu35 | ICU MV > 24 h | 76 | DEX; propofol; midazolam | extubation time; delirium; adverse events; |
| Huang36 | Non-invasive MV | 62 | DEX; midazolam | Delirium; ICU LOS; duration of MV; adverse events |
| Huang37 | Major surgery MV | 108 | DEX; propofol | Adverse events; ICU LOS; duration of MV |
| Jakob38 | Prolonged MV | 500 + 498 | DEX; propofol; midazolam | ICU LOS; RASS; duration of MV |
| Jalonen39 | CABG | 80 | DEX; placebo | Hemodynamics; myocardial function; |
| Kim40 | CABG | 153 | DEX; placebo | ICU and hospital LOS; mortality; cardiac function |
| MacLaren41 | Mixed ICU; MV > 12 h | 23 | DEX; midazolam | Duration of MV; ICU LOS |
| Maldonado42 | Cardiac surgery | 90 | DEX; midazolam; propofol | Duration of MV; ICU and hospital LOS |
| Memis43 | Septic shock | 40 | DEX; propofol | Hemodynamics, ICU LOS; mortality |
| Pandharipande44 | Mixed ICU; MV > 120 h | 103 | DEX; lorazepam | Duration of MV; ICU LOS; mortality; efficacy of sedation |
| Reade45 | Delirious MV | 20 | Haloperidol; DEX | MV duration; adjunct propofol; ICU LOS |
| Reade46 | Agitated delirium | 71 | DEX; placebo | duration of MV; ICU and hospital LOS; mortality |
| Ren47 | CABG | 162 | DEX; placebo | BP; HR; other arrhythmia |
| Riker48 | MV > 3 d | 366 | DEX; midazolam; | duration of MV; ICU LOS; mortality; delirium |
| Roekaerts49 | Coronary artery surgery | 30 | Midazolam; propofol | BP; HR; extubation time; |
| Rubino50 | Surgery for type-A aortic dissection | 30 | Clonidine; placebo | Delirium; duration of MV; ICU LOS; |
| Ruokonen64 | MV requiring long-term sedation | 85 | DEX; midazolam; propofol | duration of MV; ICU LOS; delirium |
| Sakarya51 | CABG | 40 | midazolam; propofol | Adverse events; MV duration |
| Shah52 | Postoperative MV | 30 | DEX; propofol | Safety and efficacy; |
| Shehabi53 | MV > 12 h | 37 | DEX-based EGDS; standard care | ICU and hospital LOS; mortality; delirium; MV duration |
| Shehabi54 | Cardiac surgery | 299 | DEX; morphine | Delirium; ICU and hospital LOS; mortality; adverse events |
| Song55 | ICU MV > 3d | 90 | DEX; midazolam | Delirium; ICU LOS; |
| Soro56 | CABG | 73 | Sevoflurane; propofol | ICU and hospital LOS; mortality; adverse events |
| Srivastava57 | MV > 12 h | 70 | Clonidine; DEX | MV duration; hypotension; bradycardia |
| Tasdogan58 | Severe sepsis | 40 | DEX; propofol | Mortality; IAP; MV duration; ICU LOS |
| Venn59 | Postoperative MV > 8 h | 20 | DEX; propofol | RSS; BIS; MV duration; ICU LOS |
| Wan60 | SICU | 200 | DEX; midazolam | Delirium; MV duration; ICU LOS |
| Weinbroum61 | MV | 67 | Midazolam; propofol | Hypotension; agitation; |
| Yapici62 | Cardiac surgery | 72 | DEX; midazolam | MV duration; RASS; |
| Zhang63 | COPD MV > 48 h | 162 | Midazolam; propofol;control | Vital signs; extubation time; |
CABG: coronary artery bypass grafting; DEX: Dexmedetomidine; MV; mechanical ventilation; RSS: Ramsay sedation score; BIS: bispectral index; ICU: intensive care unit; LOS: length of stay; EGDS: early-goal directed sedation; IAP: intra-abdominal pressure; SICU: surgical ICU.
Risk of bias
Random sequence generation was adequately described in approximately half of included trials (Fig. 2). In the remaining trials, they did not specifically describe the method of sequence generation. Allocation concealment was properly done in about 21 of the 52 trials. Blinding was difficult to perform because propfol was distinctive in appearance. Attrition bias and reporting bias were generally well performed in included trials. Risk of bias assessment of each trial is present in Supplemental Fig. 1.
Figure 2. Summary of risk of bias for included trials.
Network graph for the duration of MV is shown in Fig. 3. Collectively, there were 8 sedatives being compared. They were midazolam, dexmedetomidine, propofol, clonidine, morphine, haloperidol, clonidine and lorazepam. The placebo meant that no sedative was given in that group. Two studies employed propofol and midazolam in combination as the control arm, and we denoted it as the standard20,53. The thickness of the edge is proportional to inverse standard error of random effects model comparing two treatments. For example, the dex-propofol comparison appears to be thick, indicating a small standard error for the effect size of the comparison (Fig. 3). Multi-arm studies were highlighted with blue color.
Figure 3. Network of comparators.

The nodes in the graph correspond to sedatives and edges display the observed treatment comparisons. The thickness of the edge is proportional to inverse standard error of random effects model comparing two treatments. For example, the dex-propofol comparison appears to be thick, indicating a small standard error for the effect size. Multi-arm studies were highlighted with blue color. For example, there is a study with three arms comprising midazolam, propofol and placebo. The triangle involving these three alternative treatments is filled with blue color.
Clinical outcomes
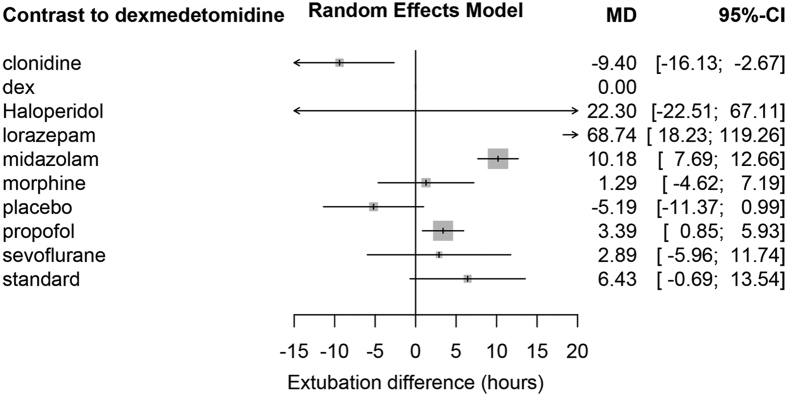
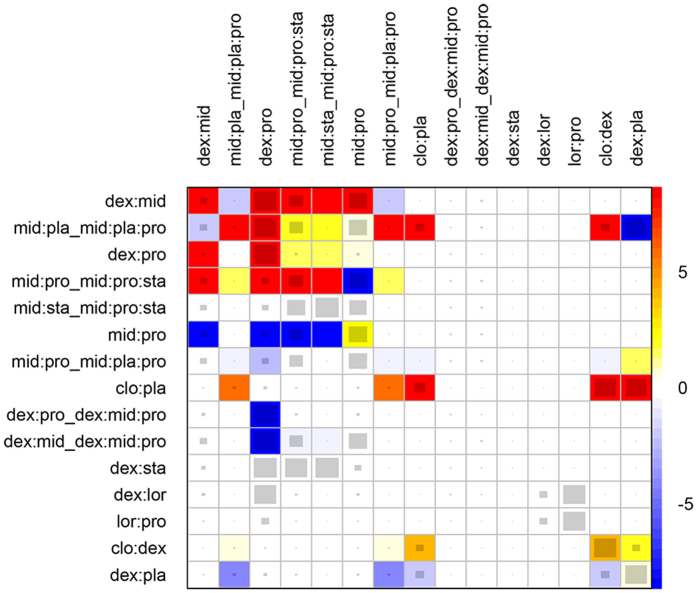
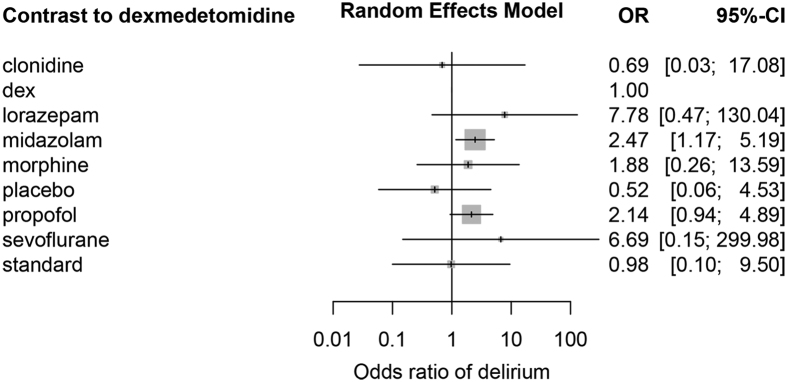
MV duration was reported in most studies. Random effects model was employed to combine the results. Dexmedetomidine showed shorter MV duration than lorazepam (MD: 68.74; 95% CI: 18.2–119.3 hours), midazolam (MD: 10.2; 95% CI: 7.7–12.7 hours) and propofol (MD: 3.4; 95% CI: 0.9–5.9 hours). However, MV duration in dexmedetomidine group was longer than clonidine (MD: −9.4; 95% CI: −16.1–-2.7 hours) and placebo (MD: −5.2 95% CI: −11.4–0.99 hours). There were no significant differences for MV duration in dexmedetomidine group as compared to that in haloperidol, morphine, sevoflurane and standard groups (Fig. 4). There were large changes in inconsistency between direct and indirect evidence in design dex:pro (shown in the row) after detaching the effect of corresponding column design (Fig. 5). As compared to dexmedetomidine, midazolam was associated with significantly increased risk of delirium (OR: 2.47; 95% CI: 1.17–5.19). Propofol was associated with increased risk of delirium with marginal statistical significance (OR: 2.14; 95% CI: 0.94–4.89). There was no difference in the risk of delirium in other comparisons (Fig. 6). There was no difference in the ICU LOS in all comparisons (Suppl. Fig. 2), except that haloperidol was associated with longer ICU stay (MD: 5; 95% CI: 1.8–8.2 days). Dexmedetomidine was associated with shorter LOS in hospital than propofol (MD: 4.6; 95% CI: 1.2–8.1 days, Suppl. Fig. 3). There is no difference in mortality between dexmedetomidine and other sedatives (Suppl. Fig. 4). There were no differences in RSS, RASS or atrial fibrillation between dexmedetomidine and other comparators (Suppl. Figs 5 to 7).
Figure 4. Difference in duration of mechanical ventilation between comparators.
Dexmedetomidine was used as the reference.
Figure 5. Net heat plot highlights the inconsistency between specific direct and indirect evidence in the whole network.
The effect estimates in the row represents pooled effect of direct and indirect effects, and the effects in the column corresponds to the direct effect. There are gray squares in some cells, and the area size is proportional to the contribution of one design in a column that is estimated from direct comparison to an overall network estimate in a row. Also note there are different colors in the cells. After detaching the effect of column design, there will be a change in the inconsistency between direct and indirect estimates. Blue colors indicate an increase in the inconsistency between direct and indirect estimates, and warm colors indicate the opposite (the intensity of the color is proportional to the magnitude of change). The pairwise contrasts corresponding to designs of three-arm studies are marked by the symbol ‘_’ following the treatments of the design.
Figure 6. Odds of delirium in each sedative, as compared to that in dexmedetomidine group.
Discussion
The present study showed that dexmedetomidine was able to reduce MV duration in critically ill patients, as compared to conventional sedatives such as lorazepam, midazolam and propofol. In addition, dexmedetomidine was associated with lower risk of delirium than that of midazolam and propofol. Dexmedetomidine was also associated with shorter hospital LOS than propofol. Propofol showed a shorter MV duration when compared to midazolam, and it has similar risk of delirium to midazolam. There were no significant differences between sedatives in other important outcomes such as mortality, ICU and hospital LOS.
Several meta-analyses of sedatives in critically ill patients have been conducted before our study65,66,67. Fraser’s study included only 6 trials comparing Benzodiazepine versus nonbenzodiazepine-based sedation for the mechanically ventilated patients. Numerous studies in this area have been published since that time, and the evidence needs to be updated. In our study, we included 51 citations that were far more than that included in Fraser’s study. Furthermore, previous studies did not perform meta-analysis in network framework. By using conventional pairwise meta-analysis, many types of sedatives had to be combined as the control group, ignoring the fact that these sedatives were different in their pharmacological properties. In clinical practice, clinicians usually face with the choice between multiple alternative sedatives. The choice may become difficult when investigators have undertaken head-to-head comparisons of only some of available sedatives. Chen’s study highlighted dexmedetomidine, and other sedatives were used as the controls. Cruickshank’s study also had the same limitation. We believe that all other sedatives are different in their efficacy and safety profiles. In this situation, network meta-analysis is more appropriate because it allows for simultaneous comparisons of multiple interventions against each other. With respect to searching database, SCOPUS was not searched in Cruickshank’s study. In the present study, many publications in non-English language were retrieved from SCOPUS. Missing these citations may result in biased estimates of pooled results, also known as publication bias. Although there are significant differences in included trials, some aspects of our findings are consistent with previous meta-analyses. For example, Cruickshank’s study found that dexmedetomidine was effective in reducing time to extubation in the ICU patients, and risk of bradycardia but not of overall mortality is higher among patients treated with dexmedetomidine67. However, Fraser’s study found a similar prevalence of delirium between patients treated with benzodiazepine versus nonbenzodiazepine sedatives65. This discrepancy can be partly explained by the limited number of component trials and the combination of different types of sedatives as the control group.
Several limitations in our study need to be acknowledged. First, the study population involved critically ill patients that were heterogeneous in nature. Patients after major operation and medical ICU patients requiring long-term MV were enrolled. However, the common feature was that they all needed MV, and sedatives were used for the same purpose for them. Second, there were significant risks of bias in most of enrolled trials. For example, blinding to participants and investigators was not performed due to the appearance of propofol. Also, specific methods to generate random sequence were not explicitly reported in nearly half of the trials. Third, more than two thirds of component trials had a sample size of less than 100, which were typically small studies. As a result, the systematic review may be subject to small study effect bias68.
In conclusion, our study showed that dexmedetomidine had potential benefits in reducing duration of MV and lowering the risk of delirium. Propofol is considered superior to midazolam in terms of MV duration. Adverse events of hypotension and bradycardia should be closely monitored when sedatives are used for MV patients.
Additional Information
How to cite this article: Zhang, Z. et al. Sedation of mechanically ventilated adults in intensive care unit: a network meta-analysis. Sci. Rep. 7, 44979; doi: 10.1038/srep44979 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Footnotes
The authors declare no competing financial interests.
Author Contributions Z.Z. conceived the idea and drafted the manuscript; K.C. and H.N. searched the electronic databases and helped statistical analysis; X.Z., and H.F. designed the forms for data extraction and extracted relevant data.
References
- Czaplik M. et al. Psychoacoustic analysis of noise and the application of earplugs in an ICU: A randomised controlled clinical trial. Eur J Anaesthesiol 33, 14–21 (2016). [DOI] [PubMed] [Google Scholar]
- Van Rompaey B., Elseviers M. M., Van Drom W., Fromont V. & Jorens P. G. The effect of earplugs during the night on the onset of delirium and sleep perception: a randomized controlled trial in intensive care patients. Crit Care 16, R73 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu R.-F., Jiang X.-Y., Hegadoren K. M. & Zhang Y.-H. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. Crit Care 19, 115 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sneyers B., Laterre P.-F., Perreault M. M., Wouters D. & Spinewine A. Current practices and barriers impairing physicians‘ and nurses’ adherence to analgo-sedation recommendations in the intensive care unit--a national survey. Crit Care 18, 655 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime D. et al. Patient experiences during awake mechanical ventilation. J Community Hosp Intern Med Perspect 6, 30426 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink R. M., Makic M. B. F., Poteet A. W. & Oman K. S. The Ventilated Patient’s Experience. Dimens Crit Care Nurs 34, 301–308 (2015). [DOI] [PubMed] [Google Scholar]
- Mehta S. et al. Prevalence, risk factors, and outcomes of delirium in mechanically ventilated adults. Critical Care Medicine 43, 557–566 (2015). [DOI] [PubMed] [Google Scholar]
- Shehabi Y., Bellomo R., Mehta S., Riker R. & Takala J. Intensive care sedation: the past, present and the future. Crit Care 17, 322 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hozo S. P., Djulbegovic B. & Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5, 13 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane Handbook for Systematic Reviews of Interventions. 1–649 (John Wiley & Sons, Ltd, doi: 10.1002/9780470712184 (2008). [DOI] [Google Scholar]
- Rücker G. Network meta-analysis, electrical networks and graph theory. Res Synth Methods 3, 312–324 (2012). [DOI] [PubMed] [Google Scholar]
- Krahn U., Binder H. & König J. A graphical tool for locating inconsistency in network meta-analyses. BMC Med Res Methodol 13, 35 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neupane B., Richer D., Bonner A. J., Kibret T. & Beyene J. Network Meta-Analysis Using R: A Review of Currently Available Automated Packages. PLoS ONE 9, e115065 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abd Aziz N. et al. Efficacy and safety of dexmedetomidine versus morphine in post-operative cardiac surgery patients. Int J Clin Pharm 33, 150–154 (2011). [DOI] [PubMed] [Google Scholar]
- Aghdaii N., Yazdanian F. & Faritus S. Z. Sedative Efficacy of Propofol in Patients Intubated/Ventilated after Coronary Artery Bypass Graft Surgery. Anesth Pain Med 3 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aitkenhead A. R. et al. Comparison of propofol and midazolam for sedation in critically ill patients. Lancet 2, 704–709 (1989). [DOI] [PubMed] [Google Scholar]
- Aydogan M. S. et al. Pain, fentanyl consumption, and delirium in adolescents after scoliosis surgery: dexmedetomidine vs midazolam. Paediatr Anaesth 23, 446–452 (2013). [DOI] [PubMed] [Google Scholar]
- Balkanay O. O., Goksedef D., Omeroglu S. N. & Ipek G. The dose-related effects of Dexmedetomidine on renal functions and serum neutrophil gelatinase-associated lipocalin values after coronary artery bypass grafting: a randomized, triple-blind, placebo-controlled study. Interactive CardioVascular and Thoracic Surgery 20, 209–214 (2015). [DOI] [PubMed] [Google Scholar]
- Barrientos-Vega R. et al. Prolonged sedation of critically ill patients with midazolam or propofol: impact on weaning and costs. Critical Care Medicine 25, 33–40 (1997). [DOI] [PubMed] [Google Scholar]
- Carrasco G. et al. Synergistic sedation with propofol and midazolam in intensive care patients after coronary artery bypass grafting. Critical Care Medicine 26, 844–851 (1998). [DOI] [PubMed] [Google Scholar]
- Carson S. S. et al. A randomized trial of intermittent lorazepam versus propofol with daily interruption in mechanically ventilated patients*. Critical Care Medicine 34, 1326–1332 (2006). [DOI] [PubMed] [Google Scholar]
- Cernaianu A. C. et al. Lorazepam and midazolam in the intensive care unit: a randomized, prospective, multicenter study of hemodynamics, oxygen transport, efficacy, and cost. Critical Care Medicine 24, 222–228 (1996). [DOI] [PubMed] [Google Scholar]
- Chamorro C. et al. Comparative study of propofol versus midazolam in the sedation of critically ill patients: results of a prospective, randomized, multicenter trial. Critical Care Medicine 24, 932–939 (1996). [DOI] [PubMed] [Google Scholar]
- Corbett S. M. et al. Dexmedetomidine does not improve patient satisfaction when compared with propofol during mechanical ventilation. Critical Care Medicine 33, 940–945 (2005). [DOI] [PubMed] [Google Scholar]
- Djaiani G. et al. Dexmedetomidine versus Propofol Sedation Reduces Delirium after Cardiac Surgery: A Randomized Controlled Trial. Anesthesiology 124, 362–368 (2016). [DOI] [PubMed] [Google Scholar]
- Abdulatif M. A comparative study of the use of dexmedetomidine and propofol as sedatives for mechanically ventilated patients in ICU. Egyptian Journal of Anaesthesia 20, 437–442 (2004). [Google Scholar]
- Elbaradie S., Mahalawy El, F. H. & Solyman A. H. Dexmedetomidine vs. propofol for short-term sedation of postoperative mechanically ventilated patients. J Egypt Natl Canc Inst 16, 153–158 (2004). [PubMed] [Google Scholar]
- Eremenko A. [Comparison of dexmedetomidine and propofol for short-term sedation in early postoperative period after cardiac surgery]. Anesteziologiia i reanimatologiia 37–41 (2014). [PubMed] [Google Scholar]
- Esmaoglu A., Ulgey A., Akin A. & Boyaci A. Comparison between dexmedetomidine and midazolam for sedation of eclampsia patients in the intensive care unit. Journal of Critical Care 24, 551–555 (2009). [DOI] [PubMed] [Google Scholar]
- Gupta S., Singh D., Sood D. & Kathuria S. Role of dexmedetomidine in early extubation of the intensive care unit patients. J Anaesthesiol Clin Pharmacol 31, 92–98 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall R. I. et al. Propofol vs midazolam for ICU sedation: a Canadian multicenter randomized trial. Chest 119, 1151–1159 (2001). [DOI] [PubMed] [Google Scholar]
- Hellström J., Öwall A. & Sackey P. V. Wake-up times following sedation with sevoflurane versus propofol after cardiac surgery. Scand. Cardiovasc. J. 46, 262–268 (2012). [DOI] [PubMed] [Google Scholar]
- Herr D. L., Sum-Ping S. T. J. & England M. ICU sedation after coronary artery bypass graft surgery: dexmedetomidine-based versus propofol-based sedation regimens. J. Cardiothorac. Vasc. Anesth. 17, 576–584 (2003). [DOI] [PubMed] [Google Scholar]
- Higgins T. L. et al. Propofol versus midazolam for intensive care unit sedation after coronary artery bypass grafting. Critical Care Medicine 22, 1415–1423 (1994). [DOI] [PubMed] [Google Scholar]
- Hu Z. The use of dexmedetomidine combined with propofol in mechanically ventilated patients. Medical Journal of Chinese People’s Liberation Army 40, 479–483 (2015). [Google Scholar]
- Huang Z., Chen Y.-S., Yang Z.-L. & Liu J.-Y. Dexmedetomidine Versus Midazolam for the Sedation of Patients with Non-invasive Ventilation Failure. Intern. Med. 51, 2299–2305 (2012). [DOI] [PubMed] [Google Scholar]
- Huang F. Sedative effects of dexmedetomidine in post-operative elder patients on mechanical ventilation. Zhonghua yi xue za zhi 94, 3211–3215 (2014). [PubMed] [Google Scholar]
- Jakob S. M. et al. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA 307, 1151–1160 (2012). [DOI] [PubMed] [Google Scholar]
- Jalonen J. et al. Dexmedetomidine as an anesthetic adjunct in coronary artery bypass grafting. Anesthesiology 86, 331–345 (1997). [DOI] [PubMed] [Google Scholar]
- Kim H.-J. et al. A comparison among infusion of lidocaine and dexmedetomidine alone and in combination in subjects undergoing coronary artery bypass graft: a randomized trial. Contemp Clin Trials 39, 303–309 (2014). [DOI] [PubMed] [Google Scholar]
- MacLaren R. et al. A Randomized, Double-Blind Pilot Study of Dexmedetomidine Versus Midazolam for Intensive Care Unit Sedation: Patient Recall of Their Experiences and Short-Term Psychological Outcomes. Journal of Intensive Care Medicine 30, 167–175 (2015). [DOI] [PubMed] [Google Scholar]
- Maldonado J. R. et al. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics 50, 206–217 (2009). [DOI] [PubMed] [Google Scholar]
- Memiş D., Kargi M. & Sut N. Effects of propofol and dexmedetomidine on indocyanine green elimination assessed with LİMON to patients with early septic shock: A pilot study. Journal of Critical Care 24, 603–608 (2009). [DOI] [PubMed] [Google Scholar]
- Pandharipande P. P. et al. Effect of Sedation With Dexmedetomidine vs Lorazepam on Acute Brain Dysfunction in Mechanically Ventilated Patients. JAMA 298, 2644–2653 (2007). [DOI] [PubMed] [Google Scholar]
- Reade M. C. et al. Dexmedetomidine vs. haloperidol in delirious, agitated, intubated patients: a randomised open-label trial. Crit Care 13, R75 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reade M. C. et al. Effect of Dexmedetomidine Added to Standard Care on Ventilator-Free Time in Patients With Agitated Delirium: A Randomized Clinical Trial. JAMA 315, 1460–1468 (2016). [DOI] [PubMed] [Google Scholar]
- Ren J. et al. Protective effect of dexmedetomidine in coronary artery bypass grafting surgery. Exp Ther Med 6, 497–502 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riker R. R. Dexmedetomidine vs Midazolam for Sedation of Critically Ill Patients <subtitle> A Randomized Trial </subtitle>. JAMA 301, 489–499 (2009). [DOI] [PubMed] [Google Scholar]
- Roekaerts P. M., Huygen F. J. & de Lange S. Infusion of propofol versus midazolam for sedation in the intensive care unit following coronary artery surgery. J. Cardiothorac. Vasc. Anesth. 7, 142–147 (1993). [DOI] [PubMed] [Google Scholar]
- Rubino A. S. et al. Impact of clonidine administration on delirium and related respiratory weaning after surgical correction of acute type-A aortic dissection: results of a pilot study. Interactive CardioVascular and Thoracic Surgery 10, 58–62 (2010). [DOI] [PubMed] [Google Scholar]
- Sakarya M. Propofol or midazolam infusion for sedation following myocardial revascularization | Miyokard revaskularizasyonu sonrasi propofol ve midazolam ile sedasyon. Turk Anesteziyoloji ve Reanimasyon 27, 171–176 (1999). [Google Scholar]
- Shah P. et al. Comparison of post-operative ICU sedation between dexmedetomidine and propofol in Indian population. Indian J Crit Care Med 18, 291 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehabi Y. et al. Early Goal-Directed Sedation Versus Standard Sedation in Mechanically Ventilated Critically Ill Patients. Critical Care Medicine 41, 1983–1991 (2013). [DOI] [PubMed] [Google Scholar]
- Shehabi Y. et al. Prevalence of delirium with dexmedetomidine compared with morphine based therapy after cardiac surgery: a randomized controlled trial (DEXmedetomidine COmpared to Morphine-DEXCOM Study). Anesthesiology 111, 1075–1084 (2009). [DOI] [PubMed] [Google Scholar]
- Song R. A study of using dexmedetomidine in ventilator bundle treatment in an ICU. Chinese Critical Care Medicine 27, 836–840 (2015). [PubMed] [Google Scholar]
- Soro M. et al. Cardioprotective effect of sevoflurane and propofol during anaesthesia and the postoperative period in coronary bypass graft surgery: a double-blind randomised study. Eur J Anaesthesiol 29, 561–569 (2012). [DOI] [PubMed] [Google Scholar]
- Srivastava U. et al. Comparison of clonidine and dexmedetomidine for short-term sedation of intensive care unit patients. Indian J Crit Care Med 18, 431–436 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasdogan M., Memiş D., Sut N. & Yuksel M. Results of a pilot study on the effects of propofol and dexmedetomidine on inflammatory responses and intraabdominal pressure in severe sepsis. Journal of Clinical Anesthesia 21, 394–400 (2009). [DOI] [PubMed] [Google Scholar]
- Venn R. M. & Grounds R. M. Comparison between dexmedetomidine and propofol for sedation in the intensive care unit: patient and clinician perceptions. Br J Anaesth 87, 684–690 (2001). [DOI] [PubMed] [Google Scholar]
- Wan L. Comparison of sedative effect of dexmedetomidine and midazolam for post-operative patients undergoing mechanical ventilation in surgical intensive care unit. Chinese Critical Care Medicine 23, 543–546 (2011). [PubMed] [Google Scholar]
- Weinbroum A. A. et al. Midazolam versus propofol for long-term sedation in the ICU: a randomized prospective comparison. Intensive Care Medicine 23, 1258–1263 (1997). [DOI] [PubMed] [Google Scholar]
- Yapici N. et al. Dexmedetomidine in cardiac surgery patients who fail extubation and present with a delirium state. The Heart Surgery Forum 14, E93–8 (2011). [DOI] [PubMed] [Google Scholar]
- Zhang C. Clinical study of different types of sedation and analgesia in patients with mechanical ventilation in icu. Medical Journal of Wuhan University 37, 322–326 (2016). [Google Scholar]
- Ruokonen E. et al. Dexmedetomidine versus propofol/midazolam for long-term sedation during mechanical ventilation. Intensive Care Medicine 35, 282–290 (2009). [DOI] [PubMed] [Google Scholar]
- Fraser G. L. et al. Benzodiazepine versus nonbenzodiazepine-based sedation for mechanically ventilated, critically ill adults: a systematic review and meta-analysis of randomized trials. Critical Care Medicine 41, S30–8 (2013). [DOI] [PubMed] [Google Scholar]
- Chen K. et al. Alpha-2 agonists for long-term sedation during mechanical ventilation in critically ill patients. Cochrane Database Syst Rev 1, CD010269 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruickshank M. et al. Alpha-2 agonists for sedation of mechanically ventilated adults in intensive care units: a systematic review. Health Technology Assessment 20, 1–118 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Xu X. & Ni H. Small studies may overestimate the effect sizes in critical care meta-analyses: a meta-epidemiological study. Crit Care 17, R2 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.