Abstract
Early initiation of breastfeeding (EIBF) within 1 hour of birth can decrease neonatal death. However, the prevalence of EIBF is approximately 50% in many developing countries, and data remains unavailable for some countries. We conducted a secondary analysis using the WHO Global Survey on Maternal and Perinatal Health to identify factors hampering EIBF. We described the coverage of EIBF among 373 health facilities for singleton neonates for whom breastfeeding was initiated after birth. Maternal and facility characteristics of EIBF were compared to those of breastfeeding >1 hour after birth, and multiple logistic regression analysis was performed. In total, 244,569 singleton live births without severe adverse outcomes were analysed. The EIBF prevalence varied widely among countries and ranged from 17.7% to 98.4% (average, 57.6%). There was less intra-country variation for BFI <24 hours. After adjustment, EIBF was significantly lower among women with complications during pregnancy and caesarean delivery. Globally, EIBF varied considerably across countries. Maternal complications during pregnancy, caesarean delivery and absence of postnatal/neonatal care guidelines at hospitals may affect EIBF. Our findings suggest that to better promote EIBF, special support for breastfeeding promotion is needed for women with complications during pregnancy and those who deliver by caesarean section.
Despite a significant reduction in child mortality from 12.7 million in 1990 to 5.9 million in 2015, neonatal mortality has been decreasing more slowly and constitutes a larger proportion of under-5 mortality1. Globally, neonatal mortality represented approximately 45% of under-5 deaths in 20152. The World Health Organization (WHO) has recommended a package of interventions including breastfeeding to reduce neonatal mortality3. Breastfeeding is a unique, valuable feeding practice in infancy that is associated with lower neonatal mortality and which alleviates inequities in child mortality and prevents morbidities such as diarrhoea, pneumonia, neonatal sepsis and may reduce obesity and diabetes later in life4,5,6,7. An estimated 11.6% of infant deaths and 21.9 million disability-adjusted years could be prevented by large-scale breastfeeding promotion programmes8. The global breastfeeding recommendations are to place all newborns in skin-to-skin contact with their mothers immediately after birth, to support the initiation of breastfeeding (BFI) within 1 hour after birth (defined as early initiation of breast feeding or EIBF) and to exclusively breastfeed the child until 6 months of age7,9.
EIBF stimulates breast milk production, produces antibody protection for the newborn and reduces postpartum maternal haemorrhage, and its practice determines the successful establishment and longer duration of breastfeeding10,11,12. Several studies have shown that EIBF is associated with a lower risk of neonatal mortality13,14,15,16.
Despite the known health benefits of EIBF, in many countries, a considerable proportion of newborns are not breastfed within 1 hour after birth in accordance with the WHO recommendation. The prevalence of EIBF ranges from 14% to 95% with an average of 64% in 128 countries, and one-half of these countries have a prevalence of less than 50%17. Furthermore, existing studies were conducted in a single country or focused on individual factors only10. A recent systematic review of the literature on EIBF in South Asia, which included 25 studies from 7 countries, revealed that EIBF is predominately associated with socio-economic, health-related and individual factors, and it highlighted the limited evidence on the health care system in relation to EIBF18.
To address these gaps and promote EIBF, we need to acquire both data on EIBF coverage and a better understanding of the factors associated with delayed breastfeeding, for which little is known, especially in low- and middle income countries.
In this analysis, we aimed to determine the coverage of EIBF and individual and health facility factors associated with delayed EIBF taking advantage of the WHO Global Survey on Maternal and Perinatal Health (WHO GS) that was implemented concurrently in health facilities across 24 countries using a standardised questionnaire.
Methods
We conducted a secondary data analysis of the WHO GS dataset. The methodological details of this survey were described previously19,20. The survey was implemented in 373 health facilities of 24 countries using a stratified multistage cluster sampling design. The countries included in the survey were from three continents: Africa (Algeria, Angola, Democratic Republic of Congo, Niger, Nigeria, Kenya and Uganda), Latin America (Argentina, Brazil, Cuba, Ecuador, Mexico, Nicaragua, Paraguay and Peru) and Asia (Cambodia, China, India, Japan, Nepal, Philippines, Sri Lanka, Thailand and Vietnam). For each country, two provinces were randomly selected with probability proportional to population size and were included in the sample along with the capital city of the country. From each of these selected areas, up to seven health facilities that had at least 1,000 deliveries per year and the capability to perform caesarean section were randomly selected with probability proportional to the number of births per year. The survey was conducted between 2004 and 2005 in Africa and Latin America and between 2007 and 2008 in Asia.
Trained medical staffs extracted data from patient records for all women who were admitted for delivery at the participating facilities during a 2- to 3-month period. Individual data were collected at hospital discharge, 8 days postpartum or at maternal death, whichever occurred first, and included demographics and reproductive characteristics, medical conditions during pregnancy, mode of delivery, birth outcomes, maternal and perinatal complications, received interventions and time of BFI.
In addition to individual data, facility information was collected on a standard form by the hospital coordinators in consultation with the facility director or the head of obstetrics, as described previously20. Data encompassed maternal and perinatal care characteristics, including the availability of laboratory tests, anaesthesiology resources, intrapartum care services, delivery and care of the newborn infant, and the availability of basic emergency medical and obstetric care facilities, intensive care units (ICUs) and human training resources.
Study population
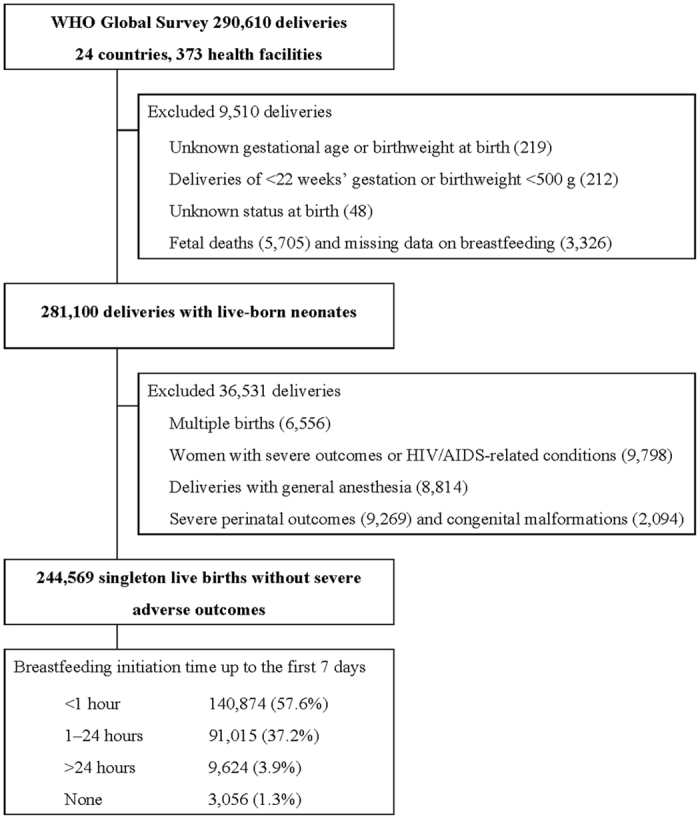
In the WHO GS dataset, individual data were available for all mothers and neonates, including first-born neonates in the case of multiple births. We initially selected all live births excluding deliveries at <22 weeks’ gestational age, birth weight <500 g, stillbirths and deliveries with missing data on BFI. The study population was restricted to neonates and mothers considered able to initiate breastfeeding and excluded those with multiple births and deliveries with certain maternal and perinatal complications, including congenital malformation, neonatal near-miss cases21 at gestational age <33 weeks, birth weight <1750 g or Apgar score at 5 minutes <7, women with severe maternal outcomes22 defined as the presence of any of the following conditions: eclampsia, blood transfusion, hysterectomy, admission to ICU and maternal death, women with any conditions suggesting HIV/AIDS and deliveries with general anaesthesia (Fig. 1).
Figure 1. Flow chart of the study population.
Variables
EIBF was the main outcome (variable of interest of this analysis) of this study, and this outcome was designated as ‘Yes’ and all others were designated as ‘No’. Additionally, to describe the time to BFI in the participating facilities and countries, we used the following four categories: EIBF (<1 hour), BFI within 1–24 hours, BFI after the first day (>24 hours) and breastfeeding not initiated by the time of discharge or by 7 days after birth.
The following maternal and obstetric characteristics were considered as factors associated with EIBF: maternal age, marital status, education, parity, number of antenatal care visits, mode of delivery, gestational age at delivery and complications during pregnancy (defined as the presence of any of the following: pregnancy-induced hypertension, chronic hypertension, cardiac/renal diseases, chronic respiratory conditions, diabetes, severe anaemia [haemoglobin <7 g/dl], pyelonephritis or urinary tract infections and other health conditions). Also, health facility characteristics such as location, ownership, capacity and availability of postnatal and/or neonatal care were examined. Facility capacity was used to reflect the facilities’ medical and obstetric care service level and summarise the services available in each facility. Total scores were determined (range: 3–63) and categorised into three groups: low (<51), medium (51–60) and high (>61)23.
Statistical analysis
We analysed the occurrence of BFI among 373 health facilities in 24 countries in singleton neonates who could breastfeed soon after birth. The prevalence of EIBF and BFI within 1–24 hours after birth was examined among participating health facilities. Maternal and facility characteristics of EIBF were compared to those of BFI at >1 hour after birth, and multiple logistic regression analysis was performed to determine odds ratios (OR) and adjusted OR (AOR). All missing variables were excluded from the analysis of association estimates. Analysis was conducted to account for the complexity of the study design in which health facilities were considered as sampling units and countries as strata. Statistical analysis was conducted using Stata/MP version 13·0 (Stata Corp LP, College Station, TX), and a P value of <0·05 was considered to indicate statistical significance.
Role of the funding source
The funders had no role in the study design, data collection and analysis, decision to publish or preparation of this manuscript.
Ethical approval
The WHO GS was approved by the WHO Ethical Review Committee and the relevant ethical clearance bodies in the participating countries and facilities. Informed consent was formally waived by the WHO Ethical Review committee. Thus, written consent from individual women was not needed because there was no contact between the data collectors (who extracted routine medical records data) and the individual women.
Results
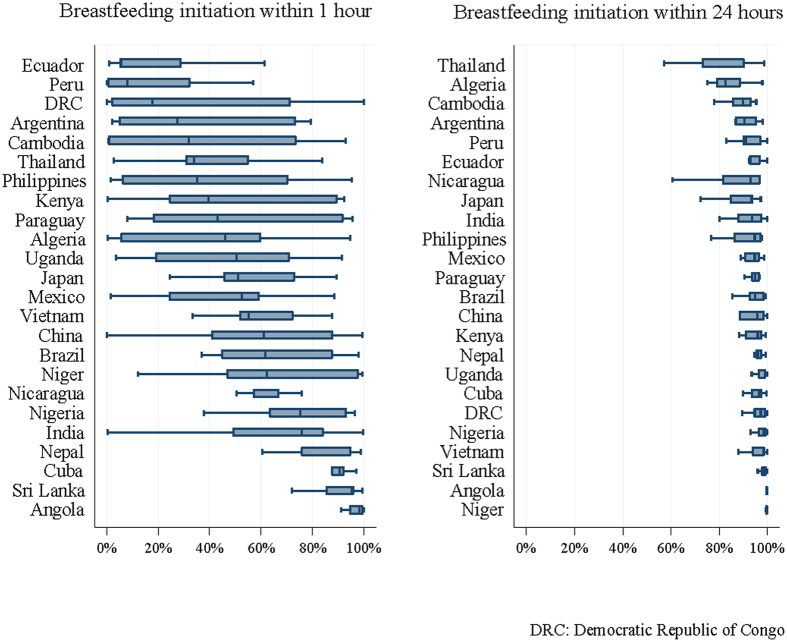
Data from 290,610 deliveries were collected from 373 health facilities in the 24 countries in the WHO GS. BFI data were available for 281,100 deliveries with liveborn neonates. Of these, 244,569 singleton live births were included in this analysis after applying the exclusion criteria (Fig. 1). BFI practice in the study population is shown in Table 1. Overall, breastfeeding was initiated for 57.6% and 37.2% of neonates within the first hour after birth and from 1–24 hours after birth, respectively. The proportion of EIBF among all live births ranged from 17.7% to 98.4% with the lowest percentages found in Peru (17.7%), Ecuador (20.1%) and the Philippines (39.9%) and the highest in Angola (98.4%), Cuba (89.2%) and Sri Lanka (88.5%). We observed wide variation in EIBF both within and between countries. However, the variation in BFI within the first 24 hours after birth was narrower than that for EIBF (Fig. 2).
Table 1. Breastfeeding initiation practice by hospital discharge in participating countries.
| Region | Country | Health facilities | Live births | Breastfeeding initiation n, % |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤1 hour | >1 to ≤24 hours | >24 hours | None | ||||||||
| Africa | Algeria | 18 | 12,391 | 5,532 | 44.7 | 6,343 | 51.2 | 301 | 2.4 | 215 | 1.7 |
| Angola | 20 | 5,198 | 5,112 | 98.4 | 80 | 1.5 | 6 | 0.1 | 0 | 0.0 | |
| DRC | 21 | 6,942 | 3,000 | 43.2 | 3,753 | 54.1 | 174 | 2.5 | 15 | 0.2 | |
| Kenya | 20 | 13,532 | 7,946 | 58.7 | 5,335 | 39.4 | 179 | 1.3 | 72 | 0.5 | |
| Niger | 11 | 7,070 | 4,734 | 67.0 | 2,335 | 33.0 | 1 | 0.0 | 0 | 0.0 | |
| Nigeria | 21 | 6,525 | 5,107 | 78.3 | 1,349 | 20.7 | 44 | 0.7 | 25 | 0.4 | |
| Uganda | 20 | 11,236 | 6,190 | 55.1 | 4,925 | 43.8 | 61 | 0.5 | 60 | 0.5 | |
| Asia | Cambodia | 5 | 4,407 | 2,463 | 55.9 | 1,742 | 39.5 | 152 | 3.5 | 50 | 1.1 |
| China | 21 | 13,867 | 8,300 | 59.9 | 4,312 | 31.1 | 511 | 3.7 | 744 | 5.4 | |
| India | 20 | 20,608 | 13,550 | 65.8 | 4,626 | 22.5 | 2,399 | 11.6 | 33 | 0.2 | |
| Japan | 10 | 2,972 | 1,809 | 60.9 | 939 | 31.6 | 197 | 6.6 | 27 | 0.9 | |
| Nepal | 8 | 7,321 | 6,329 | 86.5 | 907 | 12.4 | 75 | 1.0 | 10 | 0.1 | |
| Philippines | 17 | 11,907 | 4,754 | 39.9 | 6,380 | 53.6 | 551 | 4.6 | 222 | 1.9 | |
| Sri Lanka | 14 | 14,061 | 12,438 | 88.5 | 1,512 | 10.8 | 106 | 0.8 | 5 | 0.0 | |
| Thailand | 12 | 7,202 | 3,787 | 52.6 | 2,570 | 35.7 | 713 | 9.9 | 132 | 1.8 | |
| Vietnam | 15 | 12,202 | 7,798 | 63.9 | 4,072 | 33.4 | 283 | 2.3 | 49 | 0.4 | |
| Latin America | Argentina | 14 | 9,720 | 4,153 | 42.7 | 5,028 | 51.7 | 396 | 4.1 | 143 | 1.5 |
| Brazil | 19 | 13,437 | 9,373 | 69.8 | 3,724 | 27.7 | 289 | 2.2 | 51 | 0.4 | |
| Cuba | 17 | 11,383 | 10,153 | 89.2 | 912 | 8.0 | 284 | 2.5 | 34 | 0.3 | |
| Ecuador | 18 | 11,080 | 2,221 | 20.1 | 8,040 | 72.6 | 719 | 6.5 | 100 | 0.9 | |
| Mexico | 21 | 18,707 | 8,520 | 45.5 | 8,188 | 43.8 | 1,024 | 5.5 | 975 | 5.2 | |
| Nicaragua | 8 | 5,046 | 3,476 | 68.9 | 1,070 | 21.2 | 492 | 9.8 | 8 | 0.2 | |
| Paraguay | 6 | 3,091 | 1,531 | 49.5 | 1,482 | 48.0 | 64 | 2.1 | 14 | 0.5 | |
| Peru | 17 | 14,664 | 2,598 | 17.7 | 11,391 | 77.7 | 603 | 4.1 | 72 | 0.5 | |
| Overall | 373 | 244,569 | 140,874 | 57.6 | 91,015 | 37.2 | 9,624 | 3.9 | 3,056 | 1.3 | |
Figure 2. Variation in the initiation of breastfeeding practices at participating health facilities by country (median ranges and 25th and 75th percentiles).
Characteristics of the study population are shown in Table 2. The majority of mothers were aged 20–34 years (76.9%), married (86.9%), had made at least four antenatal care visits (67.5%) and delivered vaginally (78.3%) at 37–41 weeks’ gestation (89.7%). Furthermore, most deliveries took place at a public facility in an urban setting.
Table 2. Characteristics of the study population.
| |
Breastfeeding initiation |
|||||
|---|---|---|---|---|---|---|
| Total | ≤1 hour | >1 hour | ||||
| Number of neonates | 244,569 | 140,874 | 57.6 | 103,695 | 42.4 | |
| Maternal age (years) | ||||||
| <20 | 30,675 | 12.5 | 17,699 | 12.6 | 12,976 | 12.5 |
| 20–34 | 187,983 | 76.9 | 109,221 | 77.5 | 78,762 | 76 |
| >35 | 25,483 | 10.4 | 13,625 | 9.7 | 11,858 | 11.4 |
| Missing | 428 | 0.2 | 329 | 0.2 | 99 | 0.1 |
| Marital status | ||||||
| Single | 31,318 | 12.8 | 17,730 | 12.6 | 13,588 | 13.1 |
| Married/cohabiting | 212,579 | 86.9 | 122,667 | 87.1 | 89,912 | 86.7 |
| Missing | 672 | 0.3 | 477 | 0.3 | 195 | 0.2 |
| Education (years) | ||||||
| None or primary (<6) | 64,870 | 26.5 | 40,109 | 28.5 | 24,761 | 23.9 |
| Secondary (7–12) | 135,850 | 55.6 | 76,580 | 54.4 | 59,270 | 57.2 |
| Higher ( >12) | 32,593 | 13.3 | 17,713 | 12.5 | 14,880 | 14.3 |
| Missing | 11,256 | 4.6 | 6,472 | 4.6 | 4,784 | 4.6 |
| Parity | ||||||
| Nullipara | 104,715 | 42.8 | 59,902 | 42.5 | 44,813 | 43.2 |
| Multipara | 139,153 | 56.9 | 80,483 | 57.1 | 58,670 | 56.6 |
| Missing | 701 | 0.3 | 489 | 0.4 | 212 | 0.2 |
| Antenatal care visits | ||||||
| None | 9,851 | 4.0 | 5,909 | 4.2 | 3,942 | 3.8 |
| 1–3 | 58,498 | 23.9 | 34,341 | 24.4 | 24,157 | 23.3 |
| >4 | 164,995 | 67.5 | 94,989 | 67.4 | 70,006 | 67.5 |
| Missing | 11,225 | 4.6 | 5,635 | 4.0 | 5,590 | 5.4 |
| Maternal complications during pregnancy† | ||||||
| Yes | 67,106 | 27.4 | 33,015 | 23.4 | 34,091 | 32.9 |
| No | 176,958 | 72.4 | 107,731 | 76.5 | 69,227 | 66.8 |
| Missing | 505 | 0.2 | 128 | 0.1 | 377 | 0.3 |
| Gestational age (weeks) | ||||||
| <36 | 16,670 | 6.8 | 9,185 | 6.5 | 7,485 | 7.2 |
| 37–41 | 219,349 | 89.7 | 126,747 | 90 | 92,602 | 89.3 |
| >42 | 5,910 | 2.4 | 3,245 | 2.3 | 2,665 | 2.6 |
| Missing | 2,640 | 1.1 | 1,697 | 1.2 | 943 | 0.9 |
| Mode of delivery | ||||||
| Vaginal delivery | 191,390 | 78.3 | 122,828 | 87.2 | 68,562 | 66.1 |
| Caesarean delivery | 53,147 | 21.7 | 18,030 | 12.8 | 35,117 | 33.9 |
| Missing | 32 | 0.0 | 16 | 0.0 | 16 | 0.0 |
| Facility location | ||||||
| Urban | 208,315 | 85.2 | 116,894 | 83 | 91,421 | 88.1 |
| Peri-urban | 16,152 | 6.6 | 10,860 | 7.7 | 5,292 | 5.1 |
| Rural | 19,439 | 7.9 | 12,834 | 9.1 | 6,605 | 6.4 |
| Missing | 663 | 0.3 | 286 | 0.2 | 377 | 0.4 |
| Capacity | ||||||
| Low | 59,291 | 24.2 | 36,919 | 26.2 | 22,372 | 21.6 |
| Medium | 100,896 | 41.3 | 58,101 | 41.2 | 42,795 | 41.3 |
| High | 84,382 | 34.5 | 45,493 | 32.6 | 38,528 | 37.1 |
| Ownership | ||||||
| Public | 202,665 | 82.9 | 121,538 | 86.3 | 81,127 | 78.2 |
| Private | 7,388 | 3 | 2,972 | 2.1 | 4,416 | 4.3 |
| Others | 30,613 | 12.5 | 14,558 | 10.3 | 16,055 | 15.5 |
| Missing | 3,903 | 1.6 | 1,806 | 1.3 | 2,097 | 2 |
| Average number of beds in use | ||||||
| <50 | 105,217 | 43 | 58,981 | 41.9 | 46,236 | 44.6 |
| 50–100 | 58,462 | 23.9 | 34,042 | 24.1 | 24,420 | 23.5 |
| >100 | 78,137 | 32 | 46,647 | 33.1 | 31,490 | 30.4 |
| Missing | 2,753 | 1.1 | 1,204 | 0.9 | 1,549 | 1.5 |
| Protocols/guidelines for postnatal and/or neonatal care | ||||||
| None | 33,125 | 13.5 | 16,992 | 12.1 | 16,133 | 15.5 |
| Available | 211,071 | 86.3 | 123,795 | 87.8 | 87,276 | 84.2 |
| Missing | 373 | 0.2 | 373 | 0.1 | 286 | 0.3 |
| Region | ||||||
| Africa | 62,894 | 25.7 | 37,621 | 26.7 | 25,273 | 24.4 |
| Latin America | 87,128 | 35.6 | 42,025 | 29.8 | 45,103 | 43.5 |
| Asia | 94,547 | 38.7 | 61,228 | 43.5 | 33,319 | 32.1 |
†Medical conditions during pregnancy included chronic hypertension, pregnancy-induced hypertension, diabetes mellitus, cardiac and renal disorders, chronic respiratory conditions, pyelonephritis or urinary infections and other medical conditions.
Table 3 shows ORs and AORs for the estimated effects of individual and facility characteristics for EIBF. The crude OR for EIBF was significantly lower among women aged >35 years (OR 0.85; 95% CI 0.73–0.96) and having a secondary (OR 0.83; 95% CI 0.70–0.99) or higher education (OR 0.76; 95% CI 0.59–0.97) compared to women aged 20–34 years and having a primary or lower education, respectively. Odds of EIBF were significantly lower in Latin America (OR 0.63; 95% CI 0.41–0.99) than in Africa. However, after adjustment for potential confounders, these lower odds were no longer significant.
Table 3. Odds ratios for breastfeeding initiation within 1 hour after birth.
| OR (95% CI) | AOR (95% CI) | |||
|---|---|---|---|---|
| Maternal age (years) | ||||
| 20–34 | 1 | 1 | ||
| <20 | 0.96 | (0.81–1.12) | 1.05 | (0.92–1.19) |
| ≥35 | 0.85 | (0.73–0.96)** | 0.91 | (0.83–1.01) |
| Marital status | ||||
| Married/cohabiting | 1 | 1 | ||
| Single | 0.94 | (0.74–1.19) | 1.08 | (0.84–1.39) |
| Education (years) | ||||
| None or primary (<6) | 1 | 1 | ||
| Secondary (7–12) | 0.83 | (0.70–0.99)* | 0.86 | (0.73–1.02) |
| Higher (>12) | 0.76 | (0.59–0.97)* | 0.83 | (0.66–1.07) |
| Parity | ||||
| Multipara | 1 | 1 | ||
| Nullipara | 0.99 | (0.91–1.07) | 0.95 | (0.88–1.04) |
| Antenatal care visits | ||||
| >4 | 1 | 1 | ||
| None | 1.09 | (0.87–1.37) | 0.84 | (0.67–1.04) |
| 1–3 | 1.04 | (0.82–1.32) | 0.82 | (0.62–1.01) |
| Maternal complications during pregnancy† | ||||
| No | 1 | 1 | ||
| Yes | 0.62 | (0.52–0.73)*** | 0.76 | (0.65–0.88)*** |
| Gestational age (weeks) | ||||
| 37–41 | 1 | 1 | ||
| ≤36 | 0.87 | (0.65–1.17) | 0.81 | (0.60–1.10) |
| ≥42 | 0.87 | (0.72–1.05) | 0.95 | (0.78–1.14) |
| Mode of delivery | ||||
| Vaginal delivery | 1 | 1 | ||
| Caesarean delivery | 0.29 | (0.22–0.38)*** | 0.28 | (0.22–0.37)*** |
| Health facility location | ||||
| Urban | 1 | 1 | ||
| Peri-urban | 1.44 | (0.75–2.74) | 1.13 | (0.57–2.24) |
| Rural | 1.54 | (0.79–2.97) | 1.34 | (0.60–3.00) |
| Health facility capacity | ||||
| Low | 1 | 1 | ||
| Medium | 0.86 | (0.54–1.36) | 0.97 | (0.57–1.63) |
| High | 0.80 | (0.49–1.32) | 0.88 | (0.60–1.56) |
| Ownership | ||||
| Public | 1 | 1 | ||
| Private | 0.64 | (0.26–1.58) | 0.58 | (0.21–1.62) |
| Others | 0.62 | (0.30–1.26) | 0.60 | (0.31–1.15) |
| Average number of beds in use | ||||
| <50 | 1 | |||
| 50–100 | 1.06 | (0.70–1.62) | 1.21 | (0.79–1.88) |
| >100 | 1.10 | (0.67–1.78) | 1.40 | (0.79–2.49) |
| Guidelines for postnatal/neonatal care | ||||
| No | 1 | |||
| Available | 1.35 | (0.93–2.62) | 2.05 | (1.07–3.92)* |
| Region | ||||
| Africa | 1 | 1 | 1 | |
| Latin America | 0.63 | (0.41–0.99)* | 0.85 | (0.51–1.41) |
| Asia | 1.36 | (0.89–2.08) | 1.54 | (0.87–2.74) |
(N = 213,908 deliveries at 352 health facilities). OR: odds ratio; CI: confidence interval; AOR: adjusted odds ratio. †Medical conditions during pregnancy included chronic hypertension, pregnancy-induced hypertension, diabetes mellitus, cardiac and renal disorders, chronic respiratory conditions, pyelonephritis or urinary infections and other medical conditions.
*p < 0.05, **p < 0.01, ***p < 0.001.
EIBF was significantly lower among women who had complications during pregnancy (AOR 0.76; 95% CI 0.65–0.88) and those who delivered by caesarean section (AOR 0.28; 95% CI 0.22–0.37). Deliveries at facilities with available postnatal and/or neonatal guidelines/protocols were more likely to be associated with EIBF (AOR 2.05; 95% CI 1.07–3.92) than those at facilities with no guidelines.
Discussion
In this study, we investigated EIBF among women and their singleton neonates without maternal and perinatal severe adverse outcomes. We found that maternal complications during pregnancy, caesarean delivery (CD) and absence of postnatal/neonatal care guidelines at hospitals were negatively associated with EIBF. Maternal socio-demographic characteristics were not found to be factors associated with EIBF.
As we noted in the Introduction, there is a research gap relating to EIBF promotion, especially considering the substantial evidence indicating that EIBF is suitable for practical intervention. Research in developed countries suggests that health education and peer support interventions24, the duration of labour25, having a professional occupation26 and maternal overweight27 are associated with the initiation of breastfeeding. However, the duration of labour or having a professional occupation are not modifiable factors, and the generalisability and relevance of these findings to low- and middle- income countries is questionable. Comparatively little evidence is available relating to the determinants of BF in low- and middle-income countries. In a cohort study of exclusive breastfeeding practices in eight countries, Patil et al. found that primiparity, the provisioning of prelacteal foods and the withholding of colostrum are all associated with delay in the initiation of breastfeeding28. On the basis of these facts and keeping our findings in mind, we discuss feasible policy implications for the promotion of EIBF such as special support for mothers with CD and maternal complications.
Overall 57.6% of mothers in our study initiated breastfeeding within 1 hour after birth. This result was similar to recent data on breastfeeding indicators from 153 countries that showed the prevalence of EIBF to range from 30% to 60% in low-, middle- and high-income countries7.
The proportions of EIBF practiced at health facilities varied widely within (0–100%) and between (17.7–98.4%) the participating countries of the WHO GS. These were variations likely due to factors such as cultural and economic characteristics29, prelacteal feeding28 and violation of the 1981 International Code of Marketing for Breastmilk Substitutes30 and health institutional practices and policies31.
Our results showed that CD was one of the factors contributing to the delay in the initiation of breastfeeding, which is consistent with previous studies32,33. A recent systematic review provided evidence that CD is significantly negatively associated with EIBF. The authors suggested that maternal and foetal indications for CD and postoperative care disrupt bonding and mother-newborn interaction and delay BFI. The study also found greater risk of delayed BFI in elective, pre-labour CD and suggested a possible relation between maternal preference for CD and the decision not to breastfeed34. However, another meta-analysis suggested that CD is not a risk factor of EIBF in the presence of adequate support, but the details were not discussed31. Considering the increasing rates of CD globally, it is crucial to encourage and support EIBF in all women regardless of the mode of delivery and to inform all prospective mothers and health staff of the negative effects of CD on breastfeeding and the well-being of the newborn.
In this study, complications during pregnancy were associated with delayed EIBF, and it is possible that complications are more likely to cause intrapartum and early postpartum morbidities requiring immediate interventions for mothers or neonates that delay the mother-newborn interaction. Prevention of pregnancy complications and special support for mothers with complications, which are linked with postnatal care after hospital discharge, are essential to promoting EIBF. Although WHO recommends only 24 hours of care for mothers and neonates discharged from hospitals35, reflecting the positive evidence of postnatal care given in the communities in low- and middle-income countries36, the implementation of Birth Preparedness and Complication Readiness (BPCR) should be considered to reduce maternal and neonatal health risks37,38. A systematic review of BPCR by Soubeiga et al. found that the BPCR interventions associated with increased use of early newborn care included EIBF in low-resource settings37. We expect that the promotion of BPCR in the community works as a function of postnatal care. A feasible approach would be to integrate EIBF into primary health care (PHC) activities because PHC activities may entrench EIBF behaviours1,39,40. Strong evidence shows that lay health workers, who are key actors in PHC, aim to achieve BFI and a reduction in neonatal mortality through interventions by providing special support to women with caesarean section and complications during pregnancy41,42. We expect that a PHC programme that makes greater use of women’s groups and community health workers will be of benefit to low-income populations43,44,45.
The presence of guidelines for postnatal or neonatal care at health facilities was associated with a two times higher rate of EIBF, whereas maternal socio-demographic characteristics such as age, education and parity were not. Although an association with the presence of guidelines was found, it may be due to underlying associations between the availability of guidelines and the overall quality of care. The pursuit of contents of care may be an interesting pathway of investigation, and it can be our future challenge.
With further exploration of the data, we found that 95% of mothers initiated breastfeeding within the 1st day of birth. Although some evidence exists of the association between the workloads of health care staff and breastfeeding promotion, considering that the workload of nurses affects patient safety46,47, we assume that another contributing factor to delayed EIBF is possibly related to health facility practices or to high workload and a shortage of human resources to support and promote EIBF in women immediately after birth because the WHO GS was conducted in relatively larger health facilities from mainly low- and middle-income countries. Our assumption can be supported by the past research, which implies that heavy workload may cause possible failure to provide appropriate advice for deliveries48. However, it is difficult to prove our assumption based on the available data. Thus, it may be interesting to explore the real situations of facility practices and staff workloads using the workload indicators for staffing need developed by WHO49, especially in the facilities studied in this survey. There are findings supportive of our assumption of greater hospital influence on EIBF practices regardless of the study setting or outcome duration50,51,52. Several studies found higher proportions of EIBF and longer durations of breastfeeding among mothers delivered at Baby Friendly Hospital Initiative (BFHI)-accredited hospitals and a positive association between the number of BFHI steps in place and breastfeeding outcomes52,53.
In spite of the existence of WHO and UNICEF recommendations and the BFHI since 1989, recently, only about half of newborns have begun breastfeeding within 1 hour of birth globally7. Therefore, expansion, monitoring and reaccreditation of BFHI, and adherence of clinical care standards would increase breastfeeding outcomes including EIBF, exclusive breastfeeding and a longer duration of breastfeeding.
A key strength of this study is the uniqueness of the dataset. The study data were collected concurrently during the same time period using standardised record forms right before discharge of the women from hospital at a large number of facilities in multiple countries. This allowed a comparison of EIBF practices, which is one of the steps of the BFHI, between countries and facilities.
This study also has several limitations. Because it is a cross-sectional study, we could not examine the causal relation of exposure and outcome variables22. Our study findings are not necessarily generalisable to community settings or smaller facilities. In addition, not all participating countries had high coverage of institutional delivery. In the WHO-GS data, information on cultural factors, maternal knowledge and intention to breastfeed, prelacteal feeding and the availability of facility-level breastfeeding policies and their compliance was not available.
Finally, BFI timing data was collected in four categories (<1 hour, 1–24 hours, >24 hours and breastfeeding not initiated before hospital discharge or by the 7th day after birth) instead of at exact hours of initiation, which may have an important effect on showing how close to or far facilities are from improving EIBF coverage. However, despite these limitations, the WHO GS is a large, multi-country study that collected data in a standardised fashion.
In conclusion, our findings suggest that CD, maternal complications during pregnancy and the absence of postnatal/neonatal care guidelines were negatively associated with the rate of EIBF. To better promote EIBF, special support for the promotion of breastfeeding is needed for women with complications during pregnancy and those who deliver by caesarean section.
Additional Information
How to cite this article: Takahashi, K. et al. Prevalence of early initiation of breastfeeding and determinants of delayed initiation of breastfeeding: secondary analysis of the WHO Global Survey. Sci. Rep. 7, 44868; doi: 10.1038/srep44868 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgments
The authors thank all members of the WHO Global Survey on Maternal and Perinatal Health Research Network, including regional and country coordinators, data collection coordinators, facility coordinators, data collectors and all staff of the participating facilities who made the surveys possible. The views expressed in this article represent the views of the named authors only and not the views of their institutions or organisations. The WHO Global Survey on Maternal and Perinatal Health was funded by the Governments of China, India and Japan and the United States Agency for International Development (USAID). In addition, this secondary analysis is partially supported by the Health Labour Sciences Research Grant (Nos 26260101, 26200101) from the Ministry of Health, Labour and Welfare, Japan, and from the Japan Agency for Medical Research and Development (AMED). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Footnotes
The authors declare no competing financial interests.
Author Contributions R.M. and E.O. acquired funding and obtained ethical clearance from the WHO. K.T. and T.G. made significant contributions to the writing of the manuscript. T.G. conducted the data analysis. J.P.V. and M.L. advised about interpretation of the data. C.P.C., K.J., P.L., R.M., E.O., J.P.V., E.O.P. and J.P.S. advised about details of the contents. All authors read and approved the final draft of the manuscript.
References
- Black R. E. et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375, 1969–1987 (2010). [DOI] [PubMed] [Google Scholar]
- WHO. Global Health Observatory data http://www.who.int/gho/child_health/mortality/neonatal/en/ (2015).
- Lassi Z. S. & Bhutta Z. A. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Sys Rev 3, Cd007754 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones G., Steketee R. W., Black R. E., Bhutta Z. A. & Morris S. S. How many child deaths can we prevent this year? Lancet 362, 65–71 (2003). [DOI] [PubMed] [Google Scholar]
- Edmond K. M. et al. Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics 117, e380–e386 (2006). [DOI] [PubMed] [Google Scholar]
- Gilmour S. & Shibuya K. Simple steps to equity in child survival. BMC Med 11, 261 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora C. G. et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet 387, 475–490 (2016). [DOI] [PubMed] [Google Scholar]
- Doherty T. et al. Early cessation of breastfeeding amongst women in South Africa: an area needing urgent attention to improve child health. BMC Pediatr 12, 105 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO et al. Indicators for assessing infant and young child feeding practices. (WHO, 2008). [Google Scholar]
- Clemens J. et al. Early initiation of breastfeeding and the risk of infant diarrhea in rural Egypt. Pediatrics 104, e3 (1999). [DOI] [PubMed] [Google Scholar]
- Brandtzaeg P. Mucosal immunity: integration between mother and the breast-fed infant. Vaccine 21, 3382–3388 (2003). [DOI] [PubMed] [Google Scholar]
- Goldman A. S. Modulation of the gastrointestinal tract of infants by human milk. Interfaces and interactions. An evolutionary perspective. J Nutr 130, 426s–431s (2000). [DOI] [PubMed] [Google Scholar]
- Debes A. K., Kohli A., Walker N., Edmond K. & Mullany L. C. Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. BMC Public Health 13 Suppl 3, S19 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berde A. S. & Yalcin S. S. Determinants of early initiation of breastfeeding in Nigeria: a population-based study using the 2013 demograhic and health survey data. BMC Pregnancy Childbirth 16, 32 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- NEOVITA Study Group. Timing of initiation, patterns of breastfeeding, and infant survival: prospective analysis of pooled data from three randomised trials. Lancet Glob health 4, e266–275 (2016). [DOI] [PubMed] [Google Scholar]
- Lassi Z. S., Middleton P. F., Crowther C. & Bhutta Z. A. Interventions to improve neonatal health and later survival: an overview of systematic reviews. EBioMedicine 2, 985–1000 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF. The state of the world’s children 2015 (UNICEF, 2015).
- Sharma I. K. & Byrne A. Early initiation of breastfeeding: a systematic literature review of factors and barriers in South Asia. Int Breastfeed J 11, 17 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah A. et al. Methodological considerations in implementing the WHO Global Survey for Monitoring Maternal and Perinatal Health. Bull World Health Organ 86, 126–131 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumbiganon P. et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet 375, 490–499 (2010). [DOI] [PubMed] [Google Scholar]
- Pileggi-Castro C. et al. Development of criteria for identifying neonatal near-miss cases: analysis of two WHO multicountry cross-sectional studies. BJOG 121 Suppl 1, 110–118 (2014). [DOI] [PubMed] [Google Scholar]
- Souza J. P. et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004–2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med 8, 71 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsen S. et al. The relationship between maternal education and mortality among women giving birth in health care institutions: Analysis of the cross sectional WHO Global Survey on Maternal and Perinatal Health. BMC Public Health 11, 606 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyson L., McCormick F. & Renfrew M. J. Interventions for promoting the initiation of breastfeeding. Cochrane Database Syst Rev 2, CD001688 (2005). [DOI] [PubMed] [Google Scholar]
- Chen D. C., Nommsen-Rivers L., Dewey K. G. & Lonnerdal B. Stress during labor and delivery and early lactation performance. Am J Clin Nutr 68, 335–344 (1998). [DOI] [PubMed] [Google Scholar]
- Dagher R. K., McGovern P. M., Schold J. D. & Randall X. J. Determinants of breastfeeding initiation and cessation among employed mothers: a prospective cohort study. BMC Pregnancy Childbirth 16, 194 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen K. M., Hilson J. A. & Kjolhede C. L. Obesity may impair lactogenesis II. J Nutr 131, 3009s–3011s (2001). [DOI] [PubMed] [Google Scholar]
- Patil C. L. et al. Early interruption of exclusive breastfeeding: results from the eight-country MAL-ED study. J Health Popul Nutr 34, 10 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts T. J., Carnahan E. & Gakidou E. Can breastfeeding promote child health equity? A comprehensive analysis of breastfeeding patterns across the developing world and what we can learn from them. BMC Med 11, 254 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. International code of marketing of breast-milk substitutes. (WHO, 1981). [PubMed] [Google Scholar]
- Rollins N. C. et al. Why invest, and what it will take to improve breastfeeding practices? Lancet 387, 491–504 (2016). [DOI] [PubMed] [Google Scholar]
- Karlstrom A., Lindgren H. & Hildingsson I. Maternal and infant outcome after caesarean section without recorded medical indication: findings from a Swedish case-control study. BJOG 120, 479–486, discussion 486 (2013). [DOI] [PubMed] [Google Scholar]
- Bodner K., Wierrani F., Grunberger W. & Bodner-Adler B. Influence of the mode of delivery on maternal and neonatal outcomes: a comparison between elective cesarean section and planned vaginal delivery in a low-risk obstetric population. Arch Gynecol Obstet 283, 1193–1198 (2011). [DOI] [PubMed] [Google Scholar]
- Prior E. et al. Breastfeeding after cesarean delivery: a systematic review and meta-analysis of world literature. Am J Clin Nutr 95, 1113–1135 (2012). [DOI] [PubMed] [Google Scholar]
- WHO. WHO recommendations on Postnatal care of the mother and newborn. (WHO, 2013). [PubMed] [Google Scholar]
- Kikuchi K. et al. Effective linkages of continuum of care for improving neonatal, perinatal, and maternal mortality: a systematic review and meta-analysis. PloS One 10, e0139288 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soubeiga D., Gauvin L., Hatem M. A. & Johri M. Birth Preparedness and Complication Readiness (BPCR) interventions to reduce maternal and neonatal mortality in developing countries: systematic review and meta-analysis. BMC Pregnancy Childbirth 14, 129 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markos D. & Bogale D. Birth preparedness and complication readiness among women of child bearing age group in Goba woreda, Oromia region, Ethiopia. BMC Pregnancy Childbirth 14, 282 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson K. E. et al. Every Newborn: health-systems bottlenecks and strategies to accelerate scale-up in countries. Lancet 384, 438–454 (2014). [DOI] [PubMed] [Google Scholar]
- Rohde J. et al. 30 years after Alma-Ata: has primary health care worked in countries? Lancet 372, 950–961 (2008). [DOI] [PubMed] [Google Scholar]
- Lewin S. et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Sys Rev 3, CD004015 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines A. et al. Achieving child survival goals: potential contribution of community health workers. Lancet 369, 2121–2131 (2007). [DOI] [PubMed] [Google Scholar]
- Houweling T. A. et al. How to reach every newborn: three key messages. Lancet Glob Health 2, e436–437 (2014). [DOI] [PubMed] [Google Scholar]
- Mullan Z. Moving the needle on neonatal and child health. Lancet Glob Health 2, e431 (2014). [DOI] [PubMed] [Google Scholar]
- Bhutta Z. A. Seeing the unseen: targeting neonatal mortality in rural Vietnam. Glob Health Action 4 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P. & Gurses A. P. Nursing workload and patient safety—a human factors engineering perspective in Patient Safety and Quality: An Evidence-Based Handbook for Nurses(ed. Hughes R. G.) 2–203–2–16 (Agency for Healthcare Research and Quality, 2008). [PubMed] [Google Scholar]
- Oliveira A. C., Garcia P. C. & Nogueira L. S. Nursing workload and occurrence of adverse events in intensive care: a systematic review. Rev Esc Enferm USP 50, 683–694 (2016). [DOI] [PubMed] [Google Scholar]
- Bohren M. A. et al. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reprod Health 11, 71 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Workload Indicators of Staffing Need (WISN) User’s manual. (WHO, 2015). [Google Scholar]
- Patel A. et al. Rates and determinants of early initiation of breastfeeding and exclusive breast feeding at 42 days postnatal in six low and middle-income countries: A prospective cohort study. Reprod Health 12, S10 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse L., Denk C. E., Feldman-Winter L. & Rotondo F. M. Comparing sociodemographic and hospital influences on breastfeeding initiation. Birth 32, 81–85 (2005). [DOI] [PubMed] [Google Scholar]
- Forster D. A. & McLachlan H. L. Breastfeeding initiation and birth setting practices: a review of the literature. J Midwifery Womens Health 52, 273–280 (2007). [DOI] [PubMed] [Google Scholar]
- Venancio S. I., Saldiva S. R., Escuder M. M. & Giugliani E. R. The Baby-Friendly Hospital Initiative shows positive effects on breastfeeding indicators in Brazil. J Epidemiol Community Health 66, 914–918 (2012). [DOI] [PubMed] [Google Scholar]