Abstract
Objectives: Neuropathy and its associated pain pose great therapeutic challenges. While there has been a recent surge in acupuncture use and research, little remains known about its effects on nerve function. This review aims to assess the efficacy of acupuncture in the treatment of neuropathy of various etiologies.
Methods: The Medline, AMED, Cochrane, Scopus, CINAHL, and clintrials.gov databases were systematically searched from inception to July 2015. Randomized controlled trials (RCTs) assessing acupuncture's efficacy for poly- and mononeuropathy were reviewed. Parallel and crossover RCTs focused on acupuncture's efficacy were reviewed and screened for eligibility. The Scale for Assessing Scientific Quality of Investigations in Complementary and Alternative Medicine was used to assess RCT quality. RCTs with score of >9 and active control treatments such as sham acupuncture or medical therapy were included.
Results: Fifteen studies were included: 13 original RCTs, a long-term follow-up, and a re-analysis of a prior RCT. The selected RCTs studied acupuncture for neuropathy caused by diabetes, Bell's palsy, carpal tunnel syndrome, human immunodeficiency virus (HIV), and idiopathic conditions. Acupuncture regimens, control conditions, and outcome measures differed among studies, and various methodological issues were identified. Still, the majority of RCTs showed benefit for acupuncture over control in the treatment of diabetic neuropathy, Bell's palsy, and carpal tunnel syndrome. Acupuncture is probably effective in the treatment of HIV-related neuropathy, and there is insufficient evidence for its benefits in idiopathic neuropathy. Acupuncture appears to improve nerve conduction study parameters in both sensory and motor nerves. Meta-analyses were conducted on all diabetic neuropathy and Bell's palsy individual subject data (six RCTs; a total of 680 subjects) using a summary estimate random effects model, which showed combined odds ratio of 4.23 (95% confidence interval 2.3–7.8; p < 0.001) favoring acupuncture over control for neuropathic symptoms.
Conclusions: Acupuncture is beneficial in some peripheral neuropathies, but more rigorously designed studies using sham-acupuncture control are needed to characterize its effect and optimal use better.
Keywords: : neuropathic pain, neuropathy, acupuncture, integrative medicine
Introduction
Acupuncture has recently emerged as an important integrative medicine treatment, in both the hospital and clinic settings.1,2 In 1998, an National Institutes of Health Consensus Development Panel concluded that acupuncture is efficacious for postoperative and chemotherapy-induced nausea and vomiting, and helpful in other conditions, including stroke rehabilitation.3 Newer evidence-based reviews have shown the therapeutic benefits of acupuncture for chronic low-back pain,4,5 migraine and tension headache,6,7 chemotherapy-induced nausea and vomiting,8 and other pain conditions.9
Peripheral neuropathy (PN) is broadly defined as damage to the peripheral nervous system caused by a primary lesion or dysfunction,10 with polyneuropathy involving multiple nerves and mononeuropathy involving a single nerve. The most common causes of polyneuropathy are diabetes, thyroid disorders, vitamin B12 deficiency, alcohol abuse, chemotherapy, and human immunodeficiency virus (HIV) infection.10,11 In spite of exhaustive workups, no cause is identified in one third of PN cases, and they are considered idiopathic.11,12 The most common mononeuropathies are carpal tunnel syndrome (CTS), which is caused by demyelination of the median nerve at the wrist,10 and Bell's palsy, which involves the facial nerve and causes facial weakness.13 PN is often accompanied by painful paresthesias, which present a great therapeutic challenge.10,14 Integrative treatments such as acupuncture are used in pain clinics with increasing popularity and are gaining acceptance among the U.S. public and academic community.15,16 This acceptance of acupuncture has prompted growing research into integrative therapies for the challenging treatment of neuropathic pain. To the authors' knowledge, there has been no critical, systematic appraisal of the effects of acupuncture across all types of neuropathy, including both poly- and mononeuropathy.
Objectives
The objective of this review is to examine critically the evidence in the published literature for the safety and efficacy of acupuncture in the treatment of PN and associated symptoms compared to sham acupuncture or conventional medical therapy. Furthermore, acupuncture's effectiveness across various neuropathic conditions, as evidence permits, is also assessed.
Methods
Search strategy
The following electronic databases were searched from inception to July 2015: Medline, Cochrane Library, Scopus, AMED, CINAHL, and Clintrials.gov. The key search terms used were ([“acupuncture” OR “acup*” OR “laser acupuncture” OR “moxibustion” OR “electroacupuncture”] AND [“neuropathy” OR “peripheral neuropathy” OR “neuropathic pain” OR “neuralgia” OR “carpal tunnel syndrome” OR “Bell's palsy”]). Review papers were used to identify additional references. Language restrictions were set to English and subject restrictions to humans. Gray literature in clintrials.gov was reviewed for unpublished relevant data. Parallel and crossover RCTs were selected if their focus was acupuncture as an intervention for the treatment of PN, regardless of blinding. RCTs were selected if they included at least one group receiving acupuncture and one control group receiving sham acupuncture or another active treatment (e.g., medication).
Subject characteristics
Only adults (age >18 years) were included in the search parameters, as neuropathy, with the exception of Bell's palsy and hereditary neuropathies, is rare in children. The type of PN studied was further stratified by etiology as diabetic, chemotherapy-induced, HIV-induced, post-herpetic, idiopathic, or mononeuropathy such as CTS or Bell's palsy.
Intervention
Acupuncture was defined as the stimulation of acupuncture points by needles that pierce the skin, with or without electric stimulation, with or without moxibustion (heating with the mugwort herb). Methods of stimulating acupuncture points without needle insertion (laser, acupressure) were also searched. Controls needed to be active and included sham acupuncture or relevant medical treatments such as drugs or injections. Co-interventions were allowed only if they were given to both the intervention and the control group.
Outcome measures
One of the following outcome measures was required for inclusion: nerve conduction studies (NCS); validated questionnaires such as Symptom Severity Score, the Visual Analogue Scale, Global Symptom Score, or McGill Pain Questionnaire score; or clearly defined study-specific objective criteria distinguishing responders from non-responders.
Data extraction
The review team consisted of two neurologists with expertise in acupuncture, neuromuscular disorders, neurophysiology, and statistical methodology. Initially, an abstract review was performed to determine study eligibility. Studies were excluded if they were not RCTs or did not have acupuncture or PN as their focus. Other reasons for exclusion were the lack of a non-acupuncture control condition, such as comparing acupuncture with manual manipulation to acupuncture without manual manipulation or comparing acupuncture plus moxibustion to acupuncture alone. The remaining studies were reviewed in detail.
The Scale for Assessing Scientific Quality of Investigations in Complementary and Alternative Medicine Version (SAS-QI CAM), an instrument specifically designed to evaluate RCTs focused on integrative therapies,17 was utilized. It assesses methodological problems and sources of bias commonly encountered in integrative medicine research, such as allocation concealment, investigator and subject blinding, blinded outcome assessment, reproducibility of experimental procedures, and sound statistical analysis. The two reviewers assigned each paper a SAS-QI CAM score independently and in a blinded fashion. As the two reviewers were in agreement, there was no need to use a third reviewed as tiebreaker. Based on a recent study by D'Silva et al.,18 a SAS-QI CAM score of >9 (out of 21) served as the cutoff for inclusion based on RCT overall scientific quality.
Data synthesis plan
All included RCTs on acupuncture for diabetic peripheral neuropathy (DPN) and Bell's palsy used composite improvement scales such as “markedly relieved/improved/failed”19 or “marked effectiveness/effectiveness/failure,”20 reported at the level of the individual subject. These were converted to dichotomous “no improvement” and “improvement” variables and included in meta-analysis using standard pooling procedures based on odds ratios. Contingency tables were developed with acupuncture as the treatment marginal and improvement from baseline as the outcome marginal. Fisher's exact test was used to calculate the odds ratios as the primary endpoints. Weights for the studies were calculated based on reciprocal of the variance and normalized based on the total sum of the weights used in the meta-analyses. In addition to a standard fixed-effects Mantel–Haenszel model, a random effects meta-analysis was done due to the expected increase in heterogeneity resulting from combining Bell's palsy and DPN studies. Beyond the basal evaluation, a separate meta-analysis was conducted exclusively on the DPN subjects. All statistical analyses were conducted using R v3.0.221 with additional utility from the “rmeta” package.22
Results
Included studies
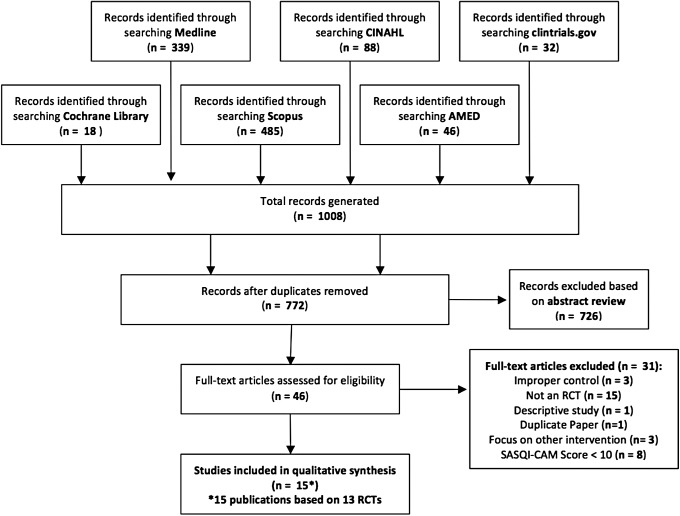
Initial searches generated 1008 records, and 772 remained after duplicate removal (Fig. 1). Of these, 726 studies were excluded after abstract review, leaving 46 to be reviewed in detail for eligibility. Initial searches identified studies with a focus on acupuncture for the treatment of DPN, chemotherapy-induced neuropathy, HIV-related neuropathy, idiopathic neuropathy, zoster neuralgia, traumatic peroneal neuropathy, and various cranial neuropathies such as Bell's palsy and trigeminal neuralgia. Of the 46 studies that underwent full review, 15 were excluded because they were not RCTs23–37: three for an improper control condition, including verum acupuncture38–40; three because they did not focus on acupuncture/involved multiple interventions41–43; one44 because it was identified as a duplicate to an included paper45; one because it was descriptive only46; and eight because of a low SAS-QI CAM score (<10).47–54
FIG. 1.
Database search flow diagram.
Following a detailed review, 15 papers met the final inclusion criteria (Table 1): 13 RCTs, a 13-month follow-up55 of an original RCT,56 and a re-analysis57 of a previously published paper.58 The selected studies focus on acupuncture for the treatment of neuropathy caused by Bell's palsy,45,59 CTS,55,56,60–62 diabetes,19,20,63,64 HIV,57,58,65 and a combination of diabetes and idiopathic causes.66 Of the included RCTs, nine studied manual acupuncture with or without moxibustion, three studied electroacupuncture, and one studied a combination of manual and electroacupuncture. Other active interventions included per os (P.O.) medications, intramuscular (i.m.)/intravenous (i.v.) injections, or splinting. As planned, all selected studies had an active control arm.
Table 1.
Study Quality Ratings Using the Scale for Assessing Scientific Quality of Investigations in Complementary and Alternative Medicine
| Study | Condition | SASQI-CAM | Intervention | Control |
|---|---|---|---|---|
| Li et al., 200445 | Bell's palsy | 13/21 | Acupuncture, moxibustion | 1. Acupuncture, moxibustion, meds P.O. and i.m. |
| 2. Meds P.O. and i.m.a | ||||
| Tong et al., 200959 | Bell's palsy | 14/21 | Acupuncture | 1. Prednisolone P.O. + pepcidine P.O.a |
| 2. Conservative Tx (non-medical) | ||||
| Khosrawi et al., 201260 | CTS | 19/21 | Acupuncture, splinting | Sham acupuncture, splinting, Vitamins B1 and B6 P.O. |
| Kumnerddee et al., 201061 | CTS | 14/21 | Electroacupuncture | Splinting |
| Yao et al., 201262 | CTS | 17/21 | Acupuncture, splinting | Sham acupuncture, splinting |
| Yang et al., 2009,56 201155 | CTS | 18/21 | Acupuncture | Prednisolone P.O. |
| Yu et al., 200119 | DM | 10/21 | Electroacupuncture | Meds P.O. and i.m. |
| Zhang et al., 201063 | DM | 11/21 | Acupuncture | Inositol P.O. |
| Zheng et al., 200464 | DM | 10/21 | Acupuncture, electroacupuncture, snow lotus i.m. injection | Mecobalamin P.O. |
| Zuo et al., 201020 | DM | 12/21 | Acupuncture, vitamin B12 i.v. | Vitamin B12 i.v. |
| Anastazi et al., 201365 | HIV | 18/21 | Acupuncture, moxibustion | Sham acupuncture, placebo moxibustion |
| Schiflett et al., 201157 | HIV | 15/21 | Acupuncture | Control (non-acupuncture) points |
| Shlay et al., 199858 | HIV | 19/21 | 1. Acupuncture 2. Acupuncture, amitriptyline |
1. Control (non-acupuncture) points |
| 3. Acupuncture, placebo P.O. | 2. Control points, amitriptyline | |||
| 3. Control points, placebo P.O. | ||||
| 4. Amitriptyline | ||||
| 5. Placebo P.O. | ||||
| Penza et al., 201166 | DM/IPN | 12/21 | Electroacupuncture | Sham electroacupuncture |
Control condition included in meta-analysis.
CTS, carpal tunnel syndrome; DM, diabetes mellitus; i.m., intramuscular; P.O., per os (oral); HIV, human immunodeficiency virus; i.v., intravenous; IPN, idiopathic peripheral neuropathy; Tx, treatment; SASQI-CAM, scale for assessing scientific quality of investigations in complementary and alternative medicine.
All included RCTs studied adult male and female outpatients, with the exception of Yu et al. who studied diabetic neuropathy in the hospital setting19 (Table 2). While most studies originated in China,19,20,45,56,59,63,64 others involved outpatients in Iran,60 Thailand,61 and the United States.58,62,65,66 Across studies, sample sizes ranged from 16 to 480 subjects, treatment courses ranged from 20 days to 3 months, and acupuncture frequency ranged from daily to weekly. There was significant variability in how neuropathy was diagnosed, including neurologic exam, symptom scales, NCS, and serologic testing. The same applied to outcome measures, which ranged from subjects' symptom ratings to validated clinical scales (Table 3), NCS (Table 4), serologic testing, and study-specific graded improvement scales.
Table 2.
Study Design, Population, Outcome Measures, and Results Summary
| Reference | Study design | Study population | Acupuncture intervention | Acupuncture course | Control intervention | Outcome measures | Reported findings |
|---|---|---|---|---|---|---|---|
| Li 200445 | 3-arm RCT |
n = 480 Bell's palsy China Outpatients |
Acupuncture, moxibustion | Treatment course: 5× per week for 4 weeks (20 total) | 1. Acupuncture, moxibustion, prednisone, vitamin B1, dibasole P.O., vitamin B12 i.m. 2. Prednisone, vitamin B1, dibasole P.O., vitamin B12 i.m. |
House–Brackmann Scale, FDIP, FDIS, Improvement Scalee |
Active intervention group vs. Control 2: Improvement Scale significantly better in active intervention (p < 0.05), “cured” (p = 0.013), “Obviously Improved” (p = 0.024); House–Brackmann (p = 0.005), FDIP (p = 0.009) Acupuncture Control 1 vs. Control 2 “Obviously Improved” (p = 0.014), House–Brackmann (p = 0.005), FDIP (p = 0.009) |
| Tong 200959 | 3-arm RCT |
n = 119 Bell's palsy China Outpatients |
Acupuncture, eye care, education | Treatment course: 3× per week until recovery or up to 3 months | 1. Prednisolone + pepcidine P.O., eye care, education 2. Eye care, home facial exercises, education |
House–Brackmann Scale |
Acupuncture vs. Control 1 vs. Control 2: No significant difference in rate of recovery among the three groups Overall improvement to Grade 3 or better: 96.4% acupuncture vs. 86.9% Control 1 vs. 89.5% Control 2 |
| Khosrawi 201260 | 2-arm RCT |
n = 64 CTS Iran Outpatients |
Acupuncture, nightly wrist splinting | Treatment course: 2× per week for 4 weeks (8 total) | Sham acupuncture, vitamins B1 and B6 P.O. | NCS including DML, DSL, SNCV, GSS |
Post vs. pre intervention: Acupuncture group GSS improvement (p < 0.001) Control group GSS unchanged (p = 0.17) Acupuncture group SNCV faster (p = 0.02) Acupuncture vs. control at 4-week follow-up: GSS improvement (p < 0.001) DSL improvement (p = 0.07) SNCV improvement (p = 0.02) |
| Kumnerddee 201061 | 2-arm RCT |
n = 61 CTS Thailand Outpatients |
Electroacupuncture | Treatment course: 2× per week for 5 weeks (10 total) | Nightly wrist splinting | BCTS including Symptom Severity Scale (SSS) and Functional Status Scale (FSS), VAS |
Post vs. pre intervention: Acupuncture group reduction in SSS, FSS, and VAS score (p < 0.05) Control group reduction in SSS (p = 0.008), no change in FSS and VAS Acupuncture vs. control: Greater VAS reduction in the acupuncture group (p = 0.028) |
| Yao 201262 | 2-arm RCT |
n = 41 CTS USA Outpatients |
Acupuncture, nightly wrist splinting | Treatment course: six weekly sessions | Sham acupuncture six weekly sessions, nightly wrist splinting | NCS including: DML, CMAP amplitude, CSI, CTSAQ Scale, key- and tip-pinch assessment |
Post vs. pre intervention CTSAQ: Acupuncture group (p < 0.05) Control group (p < 0.05) 3-month follow-up CTSAQ improvement: Acupuncture group (p = 0.17) Control group (p = 0.02) 3-month tip-pinch, key-pinch, CSI: No difference from baseline for either group Acupuncture vs. control: No difference in CTSAQ post intervention |
| Yang 200956 | 2-arm RCT |
n = 77 CTS China Outpatients |
Acupuncture | Treatment course: 2× per week for 4 weeks (8 total) | Prednisolone P.O. daily for 4 weeks | NCS including: DML, CMAP amplitude, MNCV, DSL, SNAP amplitude, W-P SNCV, GSS |
Post vs. pre intervention: GSS acupuncture group (p < 0.01) GSS control group (p < 0.01) NCS acupuncture group: decrease in DML, DSL, increase in W-P SNCV, SNAP amplitudes (p < 0.05) NCS control group: decrease in DML, DSL, Increase in W-P SNCV, SNAP amplitudes, APB CMAP amplitude (p < 0.05) Acupuncture vs. control at 4-week follow-up: GSS improvement post treatment (p = 0.15) Nocturnal awakening post treatment (p = 0.03) DML improvement (p = 0.012) |
| Yang 2011 (LTF)55 | Same | Same | Same | Same | Same | Same |
Post vs. pre intervention: 13-month acupuncture group NCS all different from baseline except for MNCV 13-month control group NCS no different from baseline except for MNCV, W-P CNCV (p < 0.01), DSL (p < 0.05) Acupuncture vs. control: Improved 7- and 13-month GSS (p < 0.01) Improved DML and MNCV at 13 months (p < 0.01) |
| Yu 200119 | 2-arm RCT |
n = 78 DM China Inpatients |
Electroacupuncture | Treatment course: 10 daily sessions × 3 Break: 3 days |
Thiamine P.O., vitamin B12 i.m.—same course | NCV, blood rheology, neurologic exam, symptomatic improvement, Improvement Scalea |
Acupuncture vs. control: Overall improvement (p < 0.01) NCV pre treatment (p > 0.05) NCV post treatment (p < 0.01) Post- vs. pre-intervention rheology: Acupuncture group (p < 0.01) Control group (p > 0.05) |
| Zhang 201063 | 2-arm RCT |
n = 65 DM China Outpatients |
Acupuncture | Treatment course: 14 daily sessions × 5 Break: 5 days |
Inositol P.O. daily for 3 months | Neurologic exam, symptomatic improvement, Improvement Scaleb |
Acupuncture vs. control: Overall improvement (p < 0.05) |
| Zheng 200464 | 2-arm RCT |
n = 104 DM China Outpatients |
Acupuncture, electroacupuncture, snow lotus i.v. | Treatment course: 10 every other day sessions × 2 | Mecobalamin P.O. daily × 2 months | Symptom score, clinical sign score, Improvement Scalec |
Post vs. pre intervention: Acupuncture group overall improvement (p < 0.01) Control group overall improvement (p < 0.01) Acupuncture vs. control: Overall improvement (p < 0.001) Symptom score (p < 0.05) Clinical sign score (p < 0.05) |
| Zuo 201020 | 2-arm RCT |
n = 75 DM China Outpatients |
Acupuncture, methylcobalamin i.v. | Treatment course: daily sessions for 4 weeks | Methylcobalamin i.v. daily for 4 weeks | NCV (MNCV, SNCV), Neurologic Exam Score, Improvement Scaled |
Acupuncture vs. control: Symptom score (p < 0.05) Neurologic Exam Score (p < 0.001) Post vs. pre intervention: Acupuncture group Neurologic Exam Score (p < 0.001) Acupuncture group median, peroneal MNCV and SNCV (p < 0.001) Control group median, peroneal SNCV (p < 0.001) |
| Anastasi 201365 | 2-arm RCT |
n = 50 HIV United States Outpatients |
Acupuncture, moxibustion | Treatment course: 2× per week for 6 weeks (12 total) | Sham acupuncture, placebo moxibustion | GPS, Subjective Peripheral Neuropathy Screen (SPNS) |
Acupuncture vs. control: GPS significantly better in acupuncture at 2-week follow-up (p < 0.05) Post vs. pre intervention: SPNS average score significantly improved in acupuncture at 2-week follow-up (p < 0.05) |
| Shlay 199858 | 8 groups |
n = 250 HIV United States Outpatients |
Acupuncture | Treatment course: 14 weeks: 2× per week for 6 weeks, followed by weekly for 8 weeks (20 total) | Sham acupuncture, amitriptyline, placebo pill | GPS, Global Pain Relief Score,f QOL questionnaire, Neurologic Summary Score |
Acupuncture vs. sham acupuncture: No difference in pain or quality of life at 6 or 14 weeks More patients in the acupuncture group reported moderate or more pain relief (p = 0.03), not significant after adjustment for multiple comparisons Amitriptyline vs. placebo: No difference in pain or quality of life at 6 or 14 weeks |
| Schiflett 2011 (reanalysis of Shlay 1998)57 | 2 × 2 table |
n = 125 HIV United States Outpatients |
Same | Same | Same | Same |
Covariate analysis using baseline pain with repeated measures at weeks 6 and 14: Baseline pain significant (p < 0.001), acupuncture + amitriptyline interaction significant (p < 0.017) ANCOVA with baseline pain as covariate: Acupuncture associated with significant global pain relief at weeks 6 and 14 |
| Penza 201166 | 2-arm RCT Crossover |
n = 16 DM/IPN United States Outpatients |
Electroacupuncture | Treatment course: six sessions every 5–7 days, 12-week break, crossover | Sham electroacupuncture | VAS, BDI, SF-36 QOL, Patient's Global Impression of Change (PGIC) |
Acupuncture vs. control: No significant difference after treatment Post vs. pre intervention: No significant difference compared to baseline in either group Crossover: No significant difference based on order of treatment |
Markedly relieved/improved/failed based on exam and symptoms.
Remarkable effectiveness/effectiveness/ineffectiveness based on symptom and clinical sign score.
Marked/some/none based on symptoms, exam, labs, NCVs.
Marked effectiveness/effectiveness/failure based on symptoms.
Cured/obviously improved/improved/no improvement based on House–Brackmann Scale and Facial Disability Index.
Global Pain Relief Score—complete/a lot/moderate/slight/none/worse.
BCTS, Boston Carpal Tunnel Score; BDI, Beck Depression Inventory; CMAP, Compound Muscle Action Potential; CSI, Combined Sensory Index; CTSAQ, Carpal Tunnel Self-Assessment Questionnaire; DML, distal motor latency, DSL, distal sensory latency; FDI, Facial Disability Index; FDIP, FDI Physical; FDIS, FDI Social; GPS, Gracely Pain Score; GSS, Global Symptom Scale; MNCV, motor nerve conduction velocities; NCS, nerve conduction studies; NCV, nerve conduction velocity; PN, peripheral neuropathy; QOL, quality of life; SNAP, sensory nerve action potential; SF-36 QOL, San Francisco-36 Quality of Life inventory; SNCV, sensory nerve conduction velocities; W-P SNCV, wrist–palmar sensory nerve conduction velocity; VAS, Visual Analog Scale.
Table 3.
Overview of Clinical Scales Used as Outcome Measures
| Validated scale used | Neuropathy-related condition | Study/condition | Post-acupuncture changes compared to baseline |
|---|---|---|---|
| BCTS including Symptom Severity | CTS | Kumnerddee 201061 | Improvement in SSS, FSS at 5 weeks (p < 0.05) |
| Scale (SSS) and Functional Status | |||
| Scale (FSS) | |||
| Carpal Tunnel Self-Assessment | CTS | Yao 201262 | Improved post acupuncture (p < 0.05) |
| Questionnaire (CTSAQ) | No difference from baseline at 3 months | ||
| Global Symptom Score (GSS) | CTS | Yang 200956 | Improved at 4 weeks (p < 0.01) |
| Yang 201155 | Improved at 7 and 13 months (p < 0.01) | ||
| Khosrawi 201260 | Improved at 4 weeks (p < 0.001) | ||
| Facial Disability Index (FDIP, FDIS) | Bell's palsy | Li 200445 | Improved FDIP compared to control at 4 weeks (p = 0.009) |
| House–Brackmann Scale | Bell's palsy | Li 2004 | Improved over medication control (p = 0.005) |
| Tong 200959 | 96.4% improvement to grade 3 or better | ||
| Gracely Pain Scale (GPS) | HIV | Anastasi 201365 | Improved at 2-week follow-up (p < 0.05) |
| HIV | Schiflett 201157 | N/A | |
| HIV | Shlay 199858 | Greater pain relief at 14 weeks (p = 0.03) | |
| Karnofsky Score | HIV | Schiflett 2011 | No difference at 6 or 14 weeks |
| Shlay 1998 | No difference at 6 or 14 weeks | ||
| Subjective Peripheral Neuropathy | HIV | Anastasi 2013 | Average score improved at 2 weeks (p < 0.05) |
| Screen (SPNS) | |||
| Visual Analog Scale (VAS) | HIV, DM, | Kumnerddee 2010 | Improved at 5 weeks (p < 0.05) |
| IPN | Penza 201166 | ||
| Beck Depression Inventory | DM/IPN | Penza 2011 | No difference after six treatments |
| SF-36 QOL | DM/IPN | Penza 2011 | No difference after six treatments |
Table 4.
Nerve Conduction Study Changes in Acupuncture and Control Groups
| Nerve conduction study parameter | Change from baseline in acupuncture group | Change from baseline in control group | Change in acupuncture vs. control |
|---|---|---|---|
| Motor NCS | |||
| Compound muscle action potential (CMAP) amplitude | |||
| Median nerve | ⇔ Yang 200956 | ↑ Yang 2009 | ⇔ Yang 2009 |
| ⇑⇑ Yang 201155 | ⇔ Yang 2011 | ⇔ Yang 2011 | |
| Distal motor latency (DML) | |||
| Median nerve | ⇔ Khosrawi 201260 | ⇔ Khosrawi 2012 | ⇔ Khosrawi 2012 |
| ↓ Yang 2009 | ↓ Yang 2009 | ↓ Yang 2009 | |
| ⇓⇓ Yang 2011 | ⇔ Yang 2011 | ⇓⇓ Yang 2011 | |
| Motor nerve conduction velocity (MNCV) | |||
| Ulnar, tibial nerve | ⇑⇑ Yu 200119 | ⇔ Yu 2001 | ⇑⇑ Yu 2001 |
| Median nerve | ⇔ Yang 2009 | ⇔ Yang 2009 | ⇔ Yang 2009 |
| ⇔ Yang 2011 | ⇑⇑ Yang 2011 | ⇑⇑ Yang 2011 | |
| ⇑⇑ Yu 2001 | ⇑⇑ Yu 2001 | ⇑⇑ Yu 2001 | |
| ⇑⇑ Zuo 201020 | ⇔ Zuo 2010 | ↑ Zuo 2010 | |
| Peroneal nerve | ⇑⇑ Zuo 2010 | ⇔ Zuo 2010 | ↑ Zuo 2010 |
| Sensory NCS | |||
| Sensory nerve action potential (SNAP) amplitude | |||
| Median nerve | ↑ Yang 2009 | ↑ Yang 2009 | ⇔ Yang 2009 |
| ⇑⇑ Yang 2011 | ⇑⇑ Yang 2011 | ⇔ Yang 2011 | |
| Distal sensory latency (DSL) | |||
| Median nerve | ⇔ Khosrawi 2012 | ⇔ Khosrawi 2012 | ⇔ (p = 0.07) Khosrawi 2012 |
| ↓ Yang 2009 | ↓ Yang 2009 | ⇔ Yang 2009 | |
| ⇓⇓ Yang 2011 | ↓ Yang 2011 | ⇔ Yang 2011 | |
| Sensory nerve conduction velocity (SNCV) | |||
| Median nerve | ↑ Khosrawi 2012 | ⇔ Khosrawi 2012 | ↑ Khosrawi 2012 |
| ↑ Yang 2009 | ↑ Yang 2009 | ⇔ Yang 2009 | |
| ⇑⇑ Yang 2011 | ⇔ Yang 2011 | ⇔ Yang 2011 | |
| ⇑⇑ Zuo 2010 | ⇑⇑ Zuo 2010 | ⇔ Zuo 2010 | |
| Peroneal nerve | ⇑⇑ Zuo 2010 | ⇑⇑ Zuo 2010 | ⇔ Zuo 2010 |
⇑⇑, increased (p < 0.01); ↑,increased (p < 0.05); ⇔, no significant change (p > 0.05); ↓, decreased (p < 0.05); ⇓⇓, decreased (p < 0.01).
DPN
Four RCTs met the eligibility criteria.19,20,63,64 These studies were conducted in China and used manual acupuncture20,63,64 or electroacupuncture19,64 in combination with snow lotus injection in acupuncture points64 and i.v. vitamin B12.20 All studies used P.O., i.m., or i.v. medication control (Table 2). Outcome measures included study-specific graded composite improvement scales based on symptoms,19,20,63,64 clinical signs,63 exam,19,63 labs,19 and NCS.19,20 The included studies reported significant improvement in acupuncture groups compared with control in neurologic exam,19,20,64 neuropathic symptoms,19,63,64 composite improvement scales,19,20,63,64 NCS,19,20 and blood rheology.19
HIV-related neuropathy
One included study of manual acupuncture for HIV-related neuropathy from the early-mid 1990s58 had enrollment difficulties and a 20–35% dropout rate due to significant HIV morbidity. This led to a complicated “factorial option” design with eight trial arms, which made a direct comparison of amitriptyline to acupuncture impossible. The study found significantly higher pain relief in the acupuncture group (p = 0.03). However, this was not true after adjustment for multiple comparisons. Shiflett et al.57 reanalyzed data from this trial using baseline pain as a covariate in a repeated-measures analysis of covariance and found that baseline pain intensity was significant (p < 0.001) and so was the interaction of acupuncture and amitriptyline over time (p < 0.017). Amitriptyline alone or acupuncture alone showed significant reduction in Gracely Pain Scale score at 6 weeks. However, only acupuncture sustained this effect at 14 weeks (Tables 2 and 3). When amitriptyline and acupuncture were combined, they did not differ from placebo.
Anastasi et al.65 also found significant reduction in Gracely Pain Scale following a 6-week course of manual acupuncture/moxibustion compared to sham acupuncture/placebo moxibustion control (Table 2). Additionally, the acupuncture group had significant improvement on the Subjective Peripheral Neuropathy Screen compared to its pretreatment baseline.
Idiopathic neuropathy
One RCT on electroacupuncture for idiopathic neuropathy was included.66 Four subjects with diabetic neuropathy and 12 with idiopathic neuropathy were enrolled in a double-blind crossover study comparing electroacupuncture to sham-electroacupuncture (eight subjects per group). There was no difference between acupuncture and control in any of the outcome measures used: Visual Analogue Scale, Patient's Global Impression of Change, Beck Depression Inventory, and the SF-36 Quality of Life Instrument (Table 3). Both groups showed no difference from baseline. The authors did not analyze data from the diabetic and idiopathic neuropathy subjects separately (Table 2).
CTS
All four RCTs56,60,61,62 used validated CTS-specific scales (Table 2) and reported significant improvement with manual acupuncture56,60,62 and electroacupuncture61 compared with baseline in the Global Symptom Score,56,60 Boston Carpal Tunnel Score,61 Carpal Tunnel Self-assessment Questionnaire,62 and Visual Analogue Scale61 (Table 3). Three of the four RCTs included showed significantly greater effectiveness of acupuncture compared with night splinting,61 sham acupuncture,60 oral vitamin B1 and B6,60 and oral prednisolone.56 In contrast, Yao et al.62 revealed no difference in CTS symptoms between acupuncture plus night splinting compared to sham acupuncture plus night splinting, with both groups improved from baseline. Most long-term follow-ups favored acupuncture at 4 weeks,56,60 5 weeks,61 7 months, and 13 months,55 with only a single study showing no difference between acupuncture and control at 3 months.62
Bell's palsy
Two RCTs with 48045 and 11959 subjects met the inclusion criteria (Table 2). Li et al.45 included an intermediate treatment group, “Control 1,” which received both acupuncture and medical therapy, and a medical therapy “Control 2” group. Tong et al.59 included an oral steroid group “Control 1” and a home exercises “Control 2” group (Table 2). Li et al.45 found significant improvement in the House–Brackmann Scale and Facial Disability Index in the acupuncture group compared with medical therapy and of the acupuncture plus medical therapy “Control 1” over the medical therapy “Control 2.” In contrast, Tong et al.59 found no significant difference on the House–Brackmann Scale, as all three groups had high improvement rates.
Acupuncture-induced changes in nerve conduction parameters
NCS were performed in included trials on DPN and CTS (Table 4). With respect to motor nerve function, acupuncture produced significant effects on median nerve compound muscle action potential (CMAP) amplitude, median nerve distal motor latency (DML), and motor nerve conduction velocity (NCV) of the median, ulnar, and peroneal nerves. Compared with medication control, acupuncture caused significantly greater improvement in DML and in median, ulnar, and motor NCV.
Sensory NCS revealed that acupuncture caused an increase in sensory nerve action potential (SNAP) amplitude in the median nerve, lowered median nerve distal sensory latency (DSL), and increased median and peroneal nerve NCV. However, compared to medication control, acupuncture showed significant improvement only in median nerve sensory NCV60 (Table 4).
With respect to longer-term NCS changes, acupuncture-treated groups had faster sensory NCV, a trend (p = 0.07) toward shorter DSL60 at 4 weeks, and shorter DML and motor NCV at 13 months.55
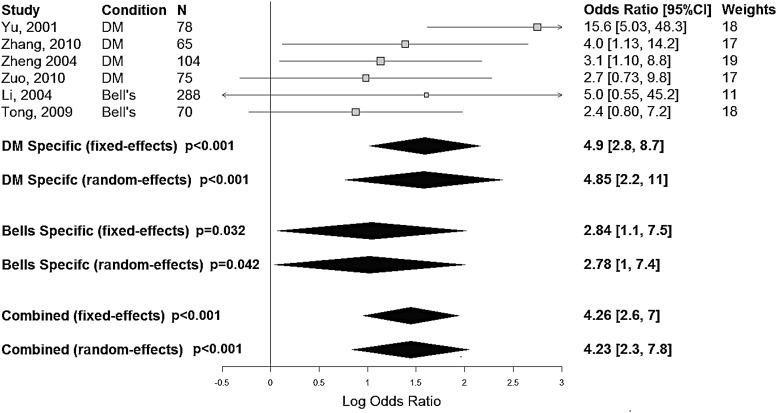
Meta-analysis on acupuncture for Bell's palsy and diabetic neuropathy
Outcomes from all included trials on DPN and Bell's palsy were reported on the individual subject level and included in this meta-analysis. All trials used medication control. Data from Li et al.'s45 “Control 1” were excluded because acupuncture was administered, and from Tong et al.'s59 “Control 2” because it was not an active control. The third arms of both trials were included in the data synthesis. A forest plot for acupuncture against control treatment was constructed using contingency tables of acupuncture against the control condition (Fig. 2). Meta-analysis on the DPN subjects showed an overall increased effect of acupuncture over control, which was still present (p < 0.001) when correcting for study heterogeneity (mean odds ratio [OR] = 4.85; 95% confidence interval [CI] 2.2–11). Meta-analysis on the Bell's palsy subjects also showed an increased effect of acupuncture over control (p = 0.042) when correcting for heterogeneity (mean OR = 2.78; 95% CI 1–7.4). Similarly, the pooled meta-analysis of all trials studying diabetic neuropathy and Bell's palsy, when adjusting for study heterogeneity, found a mean OR of 4.23 in favor of acupuncture over control (95% CI 2.3–7.8, p < 0.001).
FIG. 2.
Meta-analysis results for diabetes mellitus and Bell's palsy.
Acupuncture safety, adverse events
The included studies varied greatly in how adverse events were defined and monitored. Overall acupuncture treatment appeared safe, without serious adverse events, except in the early study on HIV-related neuropathy58 where both groups experienced significant morbidity. There was a trend toward lower rates of life-threatening events in the acupuncture group (3/58 subjects) compared with the control group (10/56; p = 0.06), with a high combined 2-year mortality rate (28.8%). The remaining studies reported no acupuncture-related serious adverse events. Minor adverse events included minor bruising with acupuncture,56,59,65 which in one study was as common as 20% of subjects61; local discomfort with needle insertion; pain following session; and uncomfortable paresthesias during acupuncture in 5% of subjects.56
Discussion
To date, no critical appraisal of acupuncture's effect on PN of various etiologies has been conducted. Prior systematic reviews were published in the areas of acupuncture for DPN, CTS, and Bell's palsy. The evidence is summarized below, along with the authors' perspective.
Acupuncture for DPN
The included RCTs involved manual acupuncture20,63 or electroacupuncture,19 which were superior to control conditions in DPN, as was the combination of both therapies.64 Further studies are needed to compare acupuncture to electroacupuncture in DPN.
By far the largest number of RCTs identified in preliminary searches dealt with acupuncture for DPN. However, only four RCTs met the inclusion criteria due to poor overall quality of the reviewed studies. In 2012, Bo et al.67 attempted a systematic review and identified 75 RCTs (73 in Chinese) on acupuncture for DPN. They concluded that the majority of those were of low-moderate methodological quality, while none of the trials met all of the CONSORT68 and STRICTA69 criteria. A systematic review was thus not conducted.
In 2013, Chen et al.70 reviewed 25 Chinese RCTs studying manual acupuncture for DPN. None of the included RCTs met all the CONSORT and STRICTA criteria, and there were no clear inclusion criteria. Meta-analysis on 23/25 RCTs suggested that acupuncture is more effective on a “global symptom improvement scale” than mecobalamin, vitamin B1 and B12, and no treatment. The authors identified multiple methodological problems and suggested that their findings were inconclusive. Neither study included the four English language trials on DPN identified in the present study.19,20,63,64
Similar conclusions were reached in this study to those of Chen et al.70 who found acupuncture to be superior to oral thiamine plus i.m. vitamin B12,19 i.v. vitamin B12,20 oral mecobalamin,64 and oral inositol.63 Similar to the above reviews, multiple methodological problems were encountered.
Acupuncture for Bell's palsy
The same six Chinese RCTs71–76 were included in two Cochrane reviews on Bell's palsy77,78 and in a systematic review79 published by the same group. Collectively, these six RCTs suggested that acupuncture leads to improved facial nerve recovery. However, the authors warned that the conclusions cannot be trusted due to multiple methodological flaws. Tong et al.59 was not referenced. Li et al.45 was excluded from the Cochrane reviews due to use of moxibustion. Moxibustion is the stimulation caused by burning the herb Artemisia vulgaris over an acupuncture point and is widely regarded as an acupuncture modality. Trials using moxibustion were included in the present review, as long as acupuncture was also used as active intervention.
In 2012, Kim et al.80 reviewed eight RCTs, among them Tong et al.,59 two studies included in the Cochrane reviews,72,74 and additional five Chinese language RCTs,81–85 all published prior to 2010, which were not included in the Cochrane 2010 review for unclear reasons. The authors excluded moxibustion, and this may be why Li et al.45 was not selected. The authors found that both acupuncture plus medication and acupuncture alone were more effective than medication alone. The authors concluded that acupuncture may be a useful adjunct or an alternative to drug therapy. However, they identified multiple methodological flaws.
The latest review on the subject included 14 RCTs86—all six RCTs from the Cochrane reviews, all RCTs reviewed by Kim et al., plus two additional Chinese language RCTs.87,88 The authors did not critically assess RCT quality except for rating them “high,” “low,” and “unclear.” Meta-analysis pooled data from 1541 individual subjects, using “effective rate” as the outcome. Acupuncture was found to be superior to control interventions (risk ratio [RR] = 1.14; 95% CI 1.04–1.25). The authors felt that their results were inconclusive due to various methodological flaws.
As the present search was limited to the English language, only two trials on manual acupuncture for Bell's palsy were included, with 599 subjects combined, which had different results. Li et al.45 found that acupuncture was more effective than a combination of acupuncture and medical therapy or medical therapy alone. Conversely, Tong et al.59 found no difference between acupuncture and the two control groups—oral steroids and home facial exercises—as all three groups had high rates of improvement from baseline. Studying episodic, self-limiting conditions such as Bell's palsy presents a challenge because the remission rate is 85% within the first 3 weeks and close to 100% within 6 months.89
Much has been written about the bias of acupuncture research coming from China. As early as 1998, Vickers et al.90 cautioned about publishing bias and the lack of negative trials. While this study is almost 20 years old, there are no negative RCTs in any of the selected reviews, which raises questions about continued publication bias.
Acupuncture for CTS
The present review found that manual acupuncture56,60 and electroacupuncture61 were more effective than control in three of the four included RCTs on CTS.56,60,61 Both acupuncture and sham-acupuncture groups improved significantly in the fourth included RCT.62 A possible explanation may be that CTS has a relatively high remission rate, ranging from 33% at 6 months91 to >50% at 1 year.92
All four included studies on CTS involved needle placement near the median nerve. Yang et al. found this effect to be sustained at 13 months.55 Further studies are needed on acupuncture's long-term effects. Similar to the present findings, Sim et al.93 reviewed six RCTs and found acupuncture to be more effective than control in five RCTs. The authors cautioned that the selected RCTs had multiple methodological flaws and were underpowered.
Acupuncture point selection
In addition to varied acupuncture treatment courses, the included RCTs used a wide variety of acupuncture points (Table 5). Point selection rationale was not justified in any RCTs, except for one.63
Table 5.
Acupuncture Point Selection
| Study | Condition | Acupuncture modality | Acupuncture point selection | Moxibustion point selection (if any) |
|---|---|---|---|---|
| Li 200445 | Bell's palsy | Acupuncture, moxibustion | Ipsilateral: ST4, ST6, ST7, LI4, GB14, SI17 Bilateral: LI4 |
Hanging moxibustion – 5 min at each point |
| Tong 200959 | Bell's palsy | Acupuncture | Ipsilateral: ST2, ST4, ST6, EX-HN7, GB14, TW17 Bilateral: LI4 |
N/A |
| Khosrawi 201260 | CTS | Acupuncture | Ipsilateral: PC6, PC7 | N/A |
| Kumnerddee 201061 | CTS | Electroacupuncture | Ipsilateral: LI4, LI11, PC7, PC8, 2 Ba-Xie points digits 2/3 and 3/4 | N/A |
| Yao 201262 | CTS | Acupuncture | Ipsilateral: PC6, PC7, SP6 Contralateral: TW5, LI4, LI11, GB34 | N/A |
| Yang 200956 | CTS | Acupuncture | Ipsilateral: PC6, PC7 | N/A |
| Yu 200119 | DM | Electroacupuncture | Bilateral: LI4, LI11, LI15, TW5, GB30, GB34, ST36, ST41, ST44 | N/A |
| Zhang 201063 | DM | Acupuncture | Bilateral: BL18, BL20, BL23, BL58, ST36, SP6, SP3, Yishu, ST40, GB 34; Also CV6, CV4 Custom points: Bilateral LI4, LI10, LI11, LI15, ST31, ST32, ST34, ST43, ST44, SP10, BL17—for blood stasis Bilateral SP8, SP9—for phlegm Bilateral Bafeng and Baxie—for severe numbness of the hands and feet |
N/A |
| Zheng 200464 | DM | Acupuncture, electroacupuncture, snow lotus i.m. injection | Manual acupuncture: bilateral T7Jiaji, BL23, GB30; Also CV4, CV6 Electroacupuncture: bilateral SP6 Injection of snow lotus herb bilaterally in T7 Jiaji and SP6 |
N/A |
| Zuo 201020 | DM | Acupuncture | Bilateral ST36, SP6, KI3, LI4, LI11, TW5, CV4, and CV6 | N/A |
| Anastazi 201365 | HIV | Acupuncture, Moxibustion | Not provided | Not provided |
| Shlay 199858 | HIV | Acupuncture | Bilateral SP6, SP7, SP9, Ba Feng, KI2, KI3 | N/A |
| Penza 201166 | DM/IPN | Electroacupuncture | Bilateral ST36, SP6, LR3, BL60 | N/A |
There was some consistency in point selection in the treatment of CTS and Bell's palsy. All included CTS trials involved points on the ipsilateral pericardium meridian: PC6,56,60,62 PC7,56,60–62 and PC8.61 Pericardium meridian points are commonly used in CTS treatment due to their close association with the median nerve, which is affected in CTS. Similarly, both of the included Bell's palsy trials used ipsilateral points on the stomach meridian—ST2,59 ST4,45,59 ST6,45,59 ST7,45 and GB1445,59—which are in close proximity to branches of the facial nerve. Both trials also included needling of bilateral LI4, which is one of the most commonly used points for facial pain.
The RCTs focused on acupuncture for diabetic, HIV-related, and idiopathic neuropathy used a greater variety of acupuncture points with little overlap. This may be because these conditions cause polyneuropathy with more complex symptoms compared with mononeuropathies.
Overview of statistical bias
Statistical bias within the larger meta-analysis was evaluated using assessments of study heterogeneity (I2) both within each of the disease subsets and in the pooled cohort. This combined approach was utilized to evaluate any discrepancy among the studies both within and across disease states. In all cases, the heterogeneity is not significant (Bell's: I2 = 6%, p = 0.55; diabetes mellitus [DM]: I2 = 47%, p = 0.12; combined: I2 = 28%, p = 0.22), indicating the effect of acupuncture intervention is appropriately similar among the studies. Even the comparatively high I2 value for DM is an indication of “moderate” heterogeneity according to the Cochrane criteria.94 The analysis of heterogeneity suggests that even in the absence of negative results, the effect of acupuncture treatment is moderately consistent within and across neuropathic conditions.
Suggested mechanism of action
While the selected trials employed varied acupuncture regimens, they all involved acupuncture points located near peripheral nerves, such as points close to the median nerve for CTS and close to the facial nerve for Bell's palsy (Table 5). It is possible that acupuncture needles exert direct effect on an underlying nerve and peri-neural tissues, either through manual manipulation or electric current. This could explain why acupuncture appears to have an effect not only on neuropathic symptoms, but also on NCS parameters (Table 4). These effects were sustained up to 13 months55 in CTS and were significantly different from the control condition. Further studies are needed before any definitive conclusions can be drawn about acupuncture's effect on NCS parameters in neuropathic conditions.
Methodological problems with standardization
One common problem in acupuncture research is the lack of standardization of point selection, number of needles used, needle retention time, needling depth, needle manipulation, use of moxibustion, and electroacupuncture. The 13 RCTs reviewed varied greatly in acupuncture point selection and in number of sessions: from six weekly sessions for DPN62 to 36 sessions in Bell's palsy.59 Consideration was given to calculating the amount of acupuncture delivered (in minutes or hours). However, there is no clear concept of an appropriate acupuncture dose and how much treatment is needed for a given condition.95 The relationship between number of needles and acupuncture effect is also unclear and probably not linear.
Lastly, isolating acupuncture's effect would be simpler in RCTs that study acupuncture alone as the intervention. Half of the included RCTs combined acupuncture with another intervention—moxibustion, medication or herbs, or splinting. This is further complicated by the use of various acupuncture modalities—manual acupuncture,20,45,56,58–60,62,63,65 electroacupuncture,19,61,66 or a combination of both.64 Manual and electroacupuncture may have different mechanisms of action and different effects on neuropathy and neuropathic pain. Unfortunately, not enough electroacupuncture trials were available to draw meaningful comparisons with manual acupuncture for each of the reviewed neuropathic conditions.
Methodological problems with sample size calculations
Only two of the included RCTs58,65 contained a sample size calculation. Therefore, it is possible that the majority of the included trials are underpowered (Table 6). In particular Penza et al.66 only enrolled eight subjects per group, and only 12 subjects had idiopathic neuropathy. There was no statistical rationalization for this sample size and this uneven split of patients with idiopathic and diabetic neuropathy.
Table 6.
Summary of Methodological Quality
| Reference | Additional active interventions? | Sham acupuncture as control? | Validated scales used? | Non-validated outcome measures used? | NCS used? | Subjects blinded? | Outcome assessors blinded? | Sample size calculation? | Statistical plan included in methods? |
|---|---|---|---|---|---|---|---|---|---|
| Li 200445 | Moxibustion | No | Yes | Improvement Scale,e symptomatic improvement | — | — | — | — | — |
| Tong 200959 | Eye care, education | No | Yes | — | — | — | — | — | Yes |
| Khosrawi 201260 | Nightly wrist splinting | YES plus P.O. meds | Yes | — | Yes | Yes | Yes | — | Yes |
| Kumnerddee 201061 | — | NO | Yes | — | — | — | — | — | Yes |
| Yao 201262 | Nightly wrist splinting | YES plus nightly wrist splinting | Yes | — | — | Yes | Yes | — | Yes |
| Yang 200956 | — | No | Yes | — | Yes | — | Yes | — | Yes |
| Yu 200119 | — | No | Yes | Improvement Scale,a symptomatic improvement | Yes | — | — | — | — |
| Zhang 201063 | — | No | No | Improvement Scale,b symptomatic improvement, neurologic exam | — | — | — | — | — |
| Zheng 200464 | Snow lotus injections | No | No | Symptom score, clinical sign score, Improvement Scalec | — | — | — | — | — |
| Zuo 201020 | Methylcobalamin i.v. | No | Yes | Neurologic Exam Score, Improvement Scaled | Yes | — | — | — | Yes |
| Anastasi 201365 | Moxibustion | YES plus placebo moxibustion | Yes | — | — | Yes | Yes | Yes | Yes |
| Shlay 199858 | — | YES plus P.O. meds, P.O. placebo | Yes | Global Pain Relief Score,f Neurologic Summary Score | — | Yes | Yes | Yes | Yes |
| Penza 201166 | — | YES | Yes | — | — | Yes | Yes | — | Yes |
Markedly relieved/improved/failed based on exam and symptoms.
Remarkable effectiveness/effectiveness/ineffectiveness based on symptom and clinical sign score.
Marked/some/none based on symptoms, exam, labs, NCVs.
Marked effectiveness/effectiveness/failure based on symptoms.
Cured/obviously improved/improved/no improvement based on House–Brackmann Scale and Facial Disability Index.
Global Pain Relief Score—complete/a lot/moderate/slight/none/worse.
—, no/none.
Methodological problems with improper control and blinding
In Traditional Chinese Medicine, there is a belief that a sensation called de qi is crucial to acupuncture's therapeutic benefit. De qi has been described as aching, soreness, heaviness, warmth, coolness, tingling, numbness at the site of the needle,96 or as radiating paresthesias.97 Because of this belief, many RCTs from China are designed to compare de qi elicited by needle manipulation to manipulation-free needling of an acupuncture point.39,40 Any studies that involved passive needle insertion in acupuncture point as control were excluded.
Lack of blinding of both subjects and investigators was a common methodological flaw of the selected studies. None of the studies originating in China19,20,45,56,59,63,64 used sham acupuncture, and the subjects were not blinded (Table 6). In 7 of the 13 included studies,19,20,45,56,59,63,64 the outcome assessors were not blinded to treatment assignment, which is source of investigator bias.
Methodological problems with placebo and expectancy
Most of the included RCTs carried out a greater number of visits or interventions in the acupuncture groups (Table 2), which may have affected subject expectancy. In many cases, the authors alluded to positive subject expectations from acupuncture, including higher dropout rates in the control condition and subjects seeking acupuncture independently.56,59 Subject expectations and the role of placebo in general were not addressed. It is well known that positive expectation amplifies acupuncture-induced analgesia in both subjective pain ratings and objective fMRI signal changes.98
Methodological problems with outcome measures
The 13 included RCTs contained a wide array of outcome measures, as should be expected with trials on various neuropathic conditions, involving both poly- and mononeuropathy. Overall, most trials assessed subject-reported measures of improvement, which are intrinsically subjective. Only four of the 13 RCTs used NCS for baseline and outcome measures (Table 4). More studies of neuropathy should use NCS or other objective measures of improvement such as somatosensory evoked potentials.
Several included studies used arbitrary, investigator-created scales of improvement (Table 6), such as “complete/a lot/moderate/slight/none/worse,”58 based on a combination of symptoms, neurologic exam, and improvement on disease-specific, validated scales. These could be a significant source of bias, particularly if the outcome assessors are not blinded to treatment assignment. With the exception of Zhang et al.,63 all RCTs using investigator-created scales of improvement also used validated outcome measures.
Conclusions
This systematic review suggests that acupuncture is effective in diabetic neuropathy, Bell's palsy, and CTS, under the conditions of the included studies. Acupuncture may be effective in HIV-related neuropathy. However, further studies are needed to explore its potential therapeutic role in this population. There is a need for future studies that address point selection, acupuncture modality, and frequency. Further studies should also aim to minimize methodological flaws by incorporating proper subject and investigator blinding, standardization of acupuncture intervention, use of validated, objective outcome assessments, a priori hypotheses with proper sample and effect size calculations, and appropriate statistical analyses.
Acknowledgments
This study is funded by the following grants: NIH K23 AT008405 (A.D.), NIH 5T32 AT002688 (B.O.). The authors wish to thank Prof. Marian McDonagh, PharmD, from OHSU's department of Medical Informatics and Clinical Epidemiology for her contribution to this manuscript.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Diehl DL, Kaplan G, Coulter I, et al. . Use of acupuncture by American physicians. J Altern Complement Med 1997;3:119–126 [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg DM, Kessler RC, Foster C, et al. . Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med 1993;328:246–252 [DOI] [PubMed] [Google Scholar]
- 3.NIH Consensus Conference. Acupuncture. JAMA 1998;280:1518–1524 [PubMed] [Google Scholar]
- 4.Manheimer E, White A, Berman B, et al. . Meta-analysis: Acupuncture for low back pain. Ann Intern Med 2005;142:651–663 [DOI] [PubMed] [Google Scholar]
- 5.Furlan AD, van Tulder M, Cherkin D, et al. . Acupuncture and dry-needling for low back pain: An updated systematic review within the framework of the cochrane collaboration. Spine (Phila Pa 1976) 2005;30:944–963 [DOI] [PubMed] [Google Scholar]
- 6.Linde K, Allais G, Brinkhaus B, et al. . Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev 2009;CD001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linde K, Allais G, Brinkhaus B, et al. . Acupuncture for tension-type headache. Cochrane Database Syst Rev 2009;CD007587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ezzo JM, Richardson MA, Vickers A, et al. . Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database Syst Rev 2006;CD002285. [DOI] [PubMed] [Google Scholar]
- 9.Vickers AJ, Cronin AM, Maschino AC, et al. . Acupuncture for chronic pain: Individual patient data meta-analysis. Arch Intern Med 2012;172:1444–1453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amato AA, Russell JA. Neuromuscular Disorders. New York: McGraw-Hill Medical, 2008 [Google Scholar]
- 11.Herskovitz S, Scelsa SN, Schaumburg HH. Peripheral Neuropathies in Clinical Practice. New York: Oxford University Press, 2010 [Google Scholar]
- 12.Gordon Smith A, Robinson Singleton J. Idiopathic neuropathy, prediabetes and the metabolic syndrome. J Neurol Sci 2006;242:9–14 [DOI] [PubMed] [Google Scholar]
- 13.Martyn CN, Hughes RA. Epidemiology of peripheral neuropathy. J Neurol Neurosurg Psychiatry 1997;62:310–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chong MS, Bajwa ZH. Diagnosis and treatment of neuropathic pain. J Pain Symptom Manage 2003;25:S4–S11 [DOI] [PubMed] [Google Scholar]
- 15.Vincent A, Kruk KM, Cha SS, et al. . Utilisation of acupuncture at an academic medical centre. Acupunct Med 2010;28:189–190 [DOI] [PubMed] [Google Scholar]
- 16.Barnes PM, Bloom B, Nahin RL; National Center for Health Statistics (U.S.). Complementary and Alternative Medicine Use Among Adults and Children: United States, 2007. Hyattsville, MD: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, 2008 [PubMed] [Google Scholar]
- 17.Jeste DV, Dunn LB, Folsom DP, et al. . Multimedia educational aids for improving consumer knowledge about illness management and treatment decisions: A review of randomized controlled trials. J Psychiatr Res 2008;42:1–21 [DOI] [PubMed] [Google Scholar]
- 18.D'Silva S, Poscablo C, Habousha R, et al. . Mind–body medicine therapies for a range of depression severity: A systematic review. Psychosomatics 2012;53:407–423 [DOI] [PubMed] [Google Scholar]
- 19.Yu J, Cui Z. Clinical study of diabetic peripheral neuropathy treated by acupuncture. Int J Clin Acupunct 2001;12:315–318 [Google Scholar]
- 20.Zuo L, Zhang L. Study on the effect of acupuncture plus methylcobalamin in treating diabetic peripheral neuropathy. J Acu Tuina Sci 2010;8:249–252 [Google Scholar]
- 21.R-Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing,; 2013. Online document at: www.R-project.org/, accessed November3, 2016 [Google Scholar]
- 22.Lumley T. rmeta: Meta-analysis. R package version 2.16. Online document at: http://cran.r-project.org/web/packages/rmeta/rmeta.pdf, accessed November3, 2016
- 23.Li Z. Mingmu dihuang tang combined with electro-acupuncture for treatment of diabetic oculomotor paralysis in 52 cases. J Tradit Chin Med 2007;27:37–38 [PubMed] [Google Scholar]
- 24.Man PL. Acupuncture analgesia for the treatment of trigeminal neuralgias: A series of forty-one cases. J Natl Med Assoc 1975;67:115–117 [PMC free article] [PubMed] [Google Scholar]
- 25.Hu J. Acupuncture treatment of herpes zoster. J Tradit Chin Med 2001;21:78–80 [PubMed] [Google Scholar]
- 26.Abuaisha BB, Costanzi JB, Boulton AJ. Acupuncture for the treatment of chronic painful peripheral diabetic neuropathy: A long-term study. Diabetes Res Clin Pract 1998;39:115–121 [DOI] [PubMed] [Google Scholar]
- 27.Green J, McClennon J. Acupuncture: An effective treatment for painful diabetic neuropathy. Diabet Foot J 2006;9(4):182–191 [Google Scholar]
- 28.Donald GK, Tobin I, Stringer J. Evaluation of acupuncture in the management of chemotherapy-induced peripheral neuropathy. Acupunct Med 2011;29:230–233 [DOI] [PubMed] [Google Scholar]
- 29.Lee S, Kim JH, Shin KM, et al. . Electroacupuncture to treat painful diabetic neuropathy: Study protocol for a three-armed, randomized, controlled pilot trial. Trials 2013;14:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galantino ML, Eke-Okoro ST, Findley TW, et al. . Use of noninvasive electroacupuncture for the treatment of HIV-related peripheral neuropathy: A pilot study. J Altern Complement Med 1999;5:135–142 [DOI] [PubMed] [Google Scholar]
- 31.Yongping J, Stefanovic J. The acupuncture treatment of peripheral neuropathy in HIV/AIDS. J Chin Med 2002;27–29 [Google Scholar]
- 32.Lu Z, Chen Z. Electroacupuncture for treatment of 12 cases of infantile peroneal nerve injury. J Tradit Chin Med 2000;20:130–131 [PubMed] [Google Scholar]
- 33.Branco K, Naeser MA. Carpal tunnel syndrome: Clinical outcome after low-level laser acupuncture, microamps transcutaneous electrical nerve stimulation, and other alternative therapies—an open protocol study. J Altern Complement Med 1999;5:5–26 [DOI] [PubMed] [Google Scholar]
- 34.Zhou Y, Garcia MK, Chang DZ, et al. . Multiple myeloma, painful neuropathy, acupuncture? Am J Clin Oncol 2009;32:319–325 [DOI] [PubMed] [Google Scholar]
- 35.Phillips KD, Skelton WD, Hand GA. Effect of acupuncture administered in a group setting on pain and subjective peripheral neuropathy in persons with human immunodeficiency virus disease. J Altern Complement Med 2004;10:449–455 [DOI] [PubMed] [Google Scholar]
- 36.Schroder S, Liepert J, Remppis A, et al. . Acupuncture treatment improves nerve conduction in peripheral neuropathy. Eur J Neurol 2007;14:276–281 [DOI] [PubMed] [Google Scholar]
- 37.Schroeder S, Meyer-Hamme G, Epplee S. Acupuncture for chemotherapy-induced peripheral neuropathy (CIPN): A pilot study using neurography. Acupunct Med 2012;30:4–7 [DOI] [PubMed] [Google Scholar]
- 38.Xie Z. 51 cases of occipital neuralgia treated with acupuncture. J Tradit Chin Med 1992;12:180–181 [PubMed] [Google Scholar]
- 39.Tong Y, Guo H, Han B. Fifteen-day acupuncture treatment relieves diabetic peripheral neuropathy. J Acupunct Meridian Stud 2010;3:95–103 [DOI] [PubMed] [Google Scholar]
- 40.Xu SB, Huang B, Zhang CY, et al. . Effectiveness of strengthened stimulation during acupuncture for the treatment of Bell palsy: A randomized controlled trial. CMAJ 2013;185:473–479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Napadow V, Liu J, Li M, et al. . Somatosensory cortical plasticity in carpal tunnel syndrome treated by acupuncture. Hum Brain Mapp 2007;28:159–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lun X. Treatment of diabetic peripheral neuropathy using Chinese herbs and acupuncture. Int J Clin Acupunct 1995;6:271–273 [Google Scholar]
- 43.Hui F, Boyle E, Vayda E, et al. . A randomized controlled trial of a multifaceted integrated complementary-alternative therapy for chronic herpes zoster-related pain. Altern Med Rev 2012;17:57–68 [PubMed] [Google Scholar]
- 44.Liang F, Li Y, Yu S, et al. . A multicentral randomized control study on clinical acupuncture treatment of Bell's palsy. J Tradit Chin Med 2006;26:307. [PubMed] [Google Scholar]
- 45.Li Y, Liang FR, Yu SG, et al. . Efficacy of acupuncture and moxibustion in treating Bell's palsy: A multicenter randomized controlled trial in China. Chin Med J (Engl) 2004;117:1502–1506 [PubMed] [Google Scholar]
- 46.Ahn AC, Bennani T, Freeman R, et al. . Two styles of acupuncture for treating painful diabetic neuropathy—a pilot randomised control trial. Acupunct Med 2007;25:11–17 [DOI] [PubMed] [Google Scholar]
- 47.Ursini T, Tontodonati M, Manzoli L, et al. . Acupuncture for the treatment of severe acute pain in herpes zoster: Results of a nested, open-label, randomized trial in the VZV Pain Study. BMC Complement Altern Med 2011;11:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lewith GT, Field J, Machin D. Acupuncture compared with placebo in post-herpetic pain. Pain 1983;17:361–368 [DOI] [PubMed] [Google Scholar]
- 49.Cai DF. Warm-needling plus Tuina relaxing for the treatment of carpal tunnel syndrome. J Tradit Chin Med 2010;30:23–24 [DOI] [PubMed] [Google Scholar]
- 50.Danciu A, Danciu E. The preference of acupuncture treatment in autonomic diabetic neuropathy. Am J Acupunct 1985;13:247–252 [Google Scholar]
- 51.Jiang H, Shi K, Li X, et al. . Clinical study on the wrist-ankle acupuncture treatment for 30 cases of diabetic peripheral neuritis. J Tradit Chin Med 2006;26:8–12 [PubMed] [Google Scholar]
- 52.Naeser MA, Hahn KA, Lieberman BE, et al. . Carpal tunnel syndrome pain treated with low-level laser and microamperes transcutaneous electric nerve stimulation: A controlled study. Arch Phys Med Rehabil 2002;83:978–988 [DOI] [PubMed] [Google Scholar]
- 53.Qian W, Qian H, Wu T, et al. . Clinical research on acupuncture treatment of diabetic peripheral neuropathy. J Acu Tuina Sci 2004;2:12–14 [Google Scholar]
- 54.Shao L. Observations on the curative effect of acupuncture on cardiac vegetative neuropathy of diabetes. J Acu Tuina Sci 2004;2:18–20 [Google Scholar]
- 55.Yang CP, Wang NH, Li TC, et al. . A randomized clinical trial of acupuncture versus oral steroids for carpal tunnel syndrome: A long-term follow-up. J Pain 2011;12:272–279 [DOI] [PubMed] [Google Scholar]
- 56.Yang CP, Hsieh CL, Wang NH, et al. . Acupuncture in patients with carpal tunnel syndrome: A randomized controlled trial. Clin J Pain 2009;25:327–333 [DOI] [PubMed] [Google Scholar]
- 57.Shiflett SC, Schwartz GE. Effects of acupuncture in reducing attrition and mortality in HIV-infected men with peripheral neuropathy. Explore (NY) 2011;7:148–154 [DOI] [PubMed] [Google Scholar]
- 58.Shlay JC, Chaloner K, Max MB, et al. . Acupuncture and amitriptyline for pain due to HIV-related peripheral neuropathy: A randomized controlled trial. Terry Beirn Community Programs for Clinical Research on AIDS. JAMA 1998;280:1590–1595 [DOI] [PubMed] [Google Scholar]
- 59.Tong FM, Chow SK, Chan PY, et al. . A prospective randomised controlled study on efficacies of acupuncture and steroid in treatment of idiopathic peripheral facial paralysis. Acupunct Med 2009;27:169–173 [DOI] [PubMed] [Google Scholar]
- 60.Khosrawi S, Moghtaderi A, Haghighat S. Acupuncture in treatment of carpal tunnel syndrome: A randomized controlled trial study. J Res Med Sci 2012;17:1–7 [PMC free article] [PubMed] [Google Scholar]
- 61.Kumnerddee W, Kaewtong A. Efficacy of acupuncture versus night splinting for carpal tunnel syndrome: A randomized clinical trial. J Med Assoc Thai 2010;93:1463–1469 [PubMed] [Google Scholar]
- 62.Yao E, Gerritz PK, Henricson E, et al. . Randomized controlled trial comparing acupuncture with placebo acupuncture for the treatment of carpal tunnel syndrome. PM R 2012;4:367–373 [DOI] [PubMed] [Google Scholar]
- 63.Zhang C, Ma YX, Yan Y. Clinical effects of acupuncture for diabetic peripheral neuropathy. J Tradit Chin Med 2010;30:13–14 [DOI] [PubMed] [Google Scholar]
- 64.Zheng HT, Li YF, Yuan SX. Observations on 52 patients with diabetic peripheral neuropathy treated by needling combined with drug. J Acu Tuina Sci 2004;2:24–26 [Google Scholar]
- 65.Anastasi JK, Capili B, McMahon DJ, et al. . Acu/Moxa for distal sensory peripheral neuropathy in HIV: A randomized control pilot study. J Assoc Nurses AIDS Care 2013;24:268–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Penza P, Bricchi M, Scola A, et al. . Electroacupuncture is not effective in chronic painful neuropathies. Pain Med 2011;12:1819–1823 [DOI] [PubMed] [Google Scholar]
- 67.Bo C, Xue Z, Yi G, et al. . Assessing the quality of reports about randomized controlled trials of acupuncture treatment on diabetic peripheral neuropathy. PLoS One 2012;7:e38461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.MacPherson H, Altman D, Hammerschlag R, et al. . Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. PLoS Med 2010;7:e1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen W, Yang GY, Liu B, et al. . Manual acupuncture for treatment of diabetic peripheral neuropathy: A systematic review of randomized controlled trials. PLOS ONE 2013;8:e73764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Li J. Comparison the efficacy between acupuncture and manipulation for Bell's palsy. Chin Clin Med Res 2005;11:1715–1716 [Google Scholar]
- 72.Liu M. Comparison of acupuncture and drug treatment for 130 patients with facial palsy. J Clin Acupunct 1996;12:56 [Google Scholar]
- 73.Ma Z. Clinical Observations on acupuncture and moxibustion treatment of HIV positive peripheral facial paralysis. Shanghai J of Acupunct Moxib 2004;23:19–20 [Google Scholar]
- 74.Shao S. Acupuncture and western medicine for 58 patients with peripheral facial palsy. New Chin Med 1999;30:14 [Google Scholar]
- 75.Yang G. Comparison of the efficacy between acupuncture and therapy apparatus for Bell's palsy. J Clin Acupunct Moxib 2001;17:28–29 [Google Scholar]
- 76.Yu Y. Analysis of acupuncture for peripheral facial palsy. Shanghai J Acupunct Moxib 1999;18:26 [Google Scholar]
- 77.He L, Zhou MK, Zhou D, et al. . Acupuncture for Bell's palsy. Cochrane Database Syst Rev 2007;CD002914. [DOI] [PubMed] [Google Scholar]
- 78.Chen N, Zhou M, He L, et al. . Acupuncture for Bell's palsy. Cochrane Database Syst Rev 2010;CD002914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zheng H, Li Y, Chen M. Evidence based acupuncture practice recommendations for peripheral facial paralysis. Am J Chin Med 2009;37:35–43 [DOI] [PubMed] [Google Scholar]
- 80.Kim JI, Lee MS, Choi TY, et al. . Acupuncture for Bell's palsy: A systematic review and meta-analysis. Chin J Integr Med 2012;18:48–55 [DOI] [PubMed] [Google Scholar]
- 81.Dai F, Zhang Y. Acupuncture point-penetrating method combined with glucocorticoids for 36 cases of Bell's palsy. Zhejiang J Tradit Chin Med 2009;44 [Google Scholar]
- 82.Wang L. Clinical observation on acupuncture combined medicine treatment for acute idiopathic facial paralysis. J Sichuan Tradit Chin Med 2007;25:109–110 [Google Scholar]
- 83.Xuan L, Wang L, Hou J, et al. . Study on shendao point of wild-horizontal needling for functional recovery of facial paralysis of facial muscles. Chin J Tradit Med Sci Technol 2007;14:6–7 [Google Scholar]
- 84.Yang C, Bao J, Zhang Z, et al. . Observations on the efficacy of combined acupuncture and medication for treating in 320 cases of facial paralysis. Sci Tech Info Gansu 2006;35:240–241 [Google Scholar]
- 85.Zhu L. Observations on the efficacy of combined acupuncture and medication for treating the acute stage of peripheral facial paralysis. Shanghai J Acupunct Moxibust 2006;25:17–18 [Google Scholar]
- 86.Li P, Qiu T, Qin C. Efficacy of acupuncture for Bell's palsy: A systematic review and meta-analysis of randomized controlled trials. PLoS One 2015;10:e0121880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhao Y, He L, Zhang Q. Effectiveness of three different treatments for peripheral facial paralysis. Chin J Clin Rehab 2005;29 41–43 [Google Scholar]
- 88.Zhu H, Jiang J, Feng L, et al. . Intractable facial paralysis treated with stellate ganglion block plus electric acupuncture. Chin J Pain Med 2004;5:263 [Google Scholar]
- 89.Peitersen E. The natural history of Bell's palsy. Am J Otol 1982;4:107–111 [PubMed] [Google Scholar]
- 90.Vickers A, Goyal N, Harland R, et al. . Do certain countries produce only positive results? A systematic review of controlled trials. Controlled Clin Trials 1998;19:159–166 [DOI] [PubMed] [Google Scholar]
- 91.Futami T, Kobayashi A, Ukita T, et al. . Carpal tunnel syndrome; its natural history. Hand Surg 1997;2:129–130 [Google Scholar]
- 92.Silverstein BA, Fan ZJ, Bonauto DK, et al. . The natural course of carpal tunnel syndrome in a working population. Scand J Work Environ Health 2010;36:384–393 [DOI] [PubMed] [Google Scholar]
- 93.Sim H, Shin BC, Lee MS, et al. . Acupuncture for carpal tunnel syndrome: A systematic review of randomized controlled trials. J Pain 2011;12:307–314 [DOI] [PubMed] [Google Scholar]
- 94.Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Online document at: www.handbook.cochrane.org, accessed November3, 2016 [Google Scholar]
- 95.White A, Cummings M, Barlas P, et al. . Defining an adequate dose of acupuncture using a neurophysiological approach—A narrative review of the literature. Acupunct Med 2008;26:111–120 [DOI] [PubMed] [Google Scholar]
- 96.Hui KK, Nixon EE, Vangel MG, et al. . Characterization of the “deqi” response in acupuncture. BMC Complement Altern Med 2007;7:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kou W, Gareus I, Bell JD, et al. . Quantification of DeQi sensation by visual analog scales in healthy humans after immunostimulating acupuncture treatment. Am J Chin Med 2007;35:753–765 [DOI] [PubMed] [Google Scholar]
- 98.Kong J, Kaptchuk TJ, Polich G, et al. . An fMRI study on the interaction and dissociation between expectation of pain relief and acupuncture treatment. Neuroimage 2009;47:1066–1076 [DOI] [PMC free article] [PubMed] [Google Scholar]