Abstract
Introduction: Telepathology evolved from video microscopy (i.e., “television microscopy”) research in the early 1950s to video microscopy used in basic research in the biological sciences to a basic diagnostic tool in telemedicine clinical applications. Its genesis can be traced to pioneering feasibility studies regarding the importance of color and other image-based parameters for rendering diagnoses and a series of studies assessing concordance of virtual slide and light microscopy diagnoses. This article documents the empirical foundations of telepathology.
Methods: A selective review of the research literature during the past decade (2005–2016) was conducted using robust research design and adequate sample size as criteria for inclusion.
Conclusions: The evidence regarding feasibility/acceptance of telepathology and related information technology applications has been well documented for several decades. The majority of evidentiary studies focused on intermediate outcomes, as indicated by comparability between telepathology and conventional light microscopy. A consistent trend of concordance between the two modalities was observed in terms of diagnostic accuracy and reliability. Additional benefits include use of telepathology and whole slide imaging for teaching, research, and outreach to resource-limited countries. Challenges still exist, however, in terms of use of telepathology as an effective diagnostic modality in clinical practice.
Keywords: : telepathology, virtual microscopy, digital pathology, whole slide imaging, cost, telemedicine
Introduction and Background
This is the seventh in a series of articles assessing the empirical foundations for telemedicine interventions as supported by the scientific research literature. The goal in all the articles has been to establish the scientific evidence on feasibility/acceptance and effects of telemedicine as a modality of healthcare delivery. In this article, we focus on telepathology. Much like teleradiology,1 telepathology evolved from advances in technology. High-quality video microscopy (i.e., “television microscopy”) research initiated in the early 1950s mounted a television camera on a compound light microscope (LM) at the RCA David Sarnoff Laboratory.2 Video microscopy was soon adapted for basic research in the biological sciences. By 1960, the Woods Hole Marine Biological Laboratory (MBL) had a cluster of high-profile neuroscience laboratories using video microscopy on a daily basis. The MBL emerged as an epicenter for video microscopy research and training, supported by the National Library of Medicine (NLM) for decades.
Video microscopy migrated to the Boston-area research universities and teaching hospitals and was adopted by the Massachusetts General Hospital (MGH) for telemedicine clinical applications after pioneering studies on the importance of color for rendering teledermatology and television microscopy diagnosis. By 1968, video microscopy was used almost daily, serving patients at a walk-in clinic at Boston's Logan International Airport linking them to physicians at MGH. More than 1,000 television microscopy cases were examined on a black-and-white video monitor.
The term “telepathology” was introduced into the literature in 1986,3–7 and by 2016, there were more than 1,000 peer-reviewed articles and 137 U.S. patents for telepathology.8,9 Telepathology was differentiated from its predecessor “video microscopy” by the fact that with telepathology, the diagnosing telepathologist maintained direct control over the selection of histopathology fields and magnifications for methodical examination of glass slides (GSs) at a distance.3,4,10–13 Using such technologies, telepathology services have been successfully used since 1989 in Europe and since 1996 in the United States, based on evidentiary support from numerous diagnostic studies.14–19
Organization of Pathology Departments
Hospital laboratory services at larger U.S. academic medical centers and commercial reference laboratories are divided into sections (e.g., surgical pathology, chemistry, and clinical microbiology) based on categories of laboratory tests and the requisite professional expertise. Although it is anticipated that most sections will eventually incorporate digital images in their daily practices, most telepathology services have been carried out in just two areas, surgical pathology and cytopathology.17,20–23 As a frame of reference, academic pathology departments are typically organized into two service divisions: (1) anatomic pathology that includes surgical pathology, cytopathology, and autopsy pathology and (2) clinical pathology that includes chemistry, clinical microbiology, hematology, cytogenetics, genomics, and toxicology.24,25
Subspecialty Pathology
To date, the greatest interest in telepathology has come from subspecialty surgical pathologists and their clients. Globally, access to subspecialty surgical pathology services is highly variable. In the United States, the surgical pathology section at an academic medical center may have as many as 20 or more organ-based pathology subsections ranging from cardiology to neuropathology. In much of the rest of the world, there is a dearth of general surgical pathologists, let alone subspecialists. To put the abundance of surgical pathologists in the United States into perspective, one recent estimate had 40,000–50,000 pathologists worldwide. Of these, ∼20,000 (∼40%) were located in the United States, serving just 3% of the world's population.26–28
Practicing surgical pathologists differ widely with respect to their perceived need for subspecialty second opinions. If second opinions on surgical pathology diagnoses were required in the United States for either peer-to-peer reviews or to provide expert second opinions for all new cases of cancer, then the number of telepathologists would have to increase substantially to meet these needs.28–30 In several provinces in Canada, primary diagnoses and second opinions are obtained by telepathology at rural and urban hospitals.31
Telepathology may prove to be highly useful in hematopathology in the future, but it is currently limited because of high LM resolution requirements and dependence on a 100× oil immersion lens to render many diagnoses. Remote management of the cleaning of oil immersion lenses has been technically challenging. Several start-up companies (e.g., Cellavision, Fraunhofer, Clemex, Tissuegnostics, and MEDCO) include oil immersion lens as an option.18
At some institutions, challenging or complicated surgical pathology cases are routinely diagnosed by organ-specific subspecialty pathologists. In smaller “general pathology practices,” most cases are diagnosed by “general pathologists.” Indeed, the use of subspecialty pathologists is highly variable because there are no standardized requirements. Community hospital laboratories often mail out GSs to reference laboratories to obtain second opinions from expert pathologists. “Meaningful uses” of subspecialty pathologist services are determined locally and are variable. For example, many small pathology practices may send out most renal biopsies, but fewer gastrointestinal (GI) pathology cases.
The past two decades have witnessed a remarkable growth in reference laboratory businesses that market outsourcing of services to medical centers and office practices of all sizes. Pathologists employed by reference laboratories work in free-standing buildings, often miles or states away from their clients. Typically, histopathology GSs are mailed by Federal Express or other carriers from the site of origin of the case where the patient is located to a consulting subspecialty pathologist located elsewhere. Needless to say, this does not count as telepathology.
Conventional Light Microscopy as the Standard for Comparison of Telepathology Systems
For well more than a century, light microscopy diagnosis has been the “gold standard” for medical diagnoses and the underpinning of medical education coursework as well. A LM (Fig. 1) uses visible light and magnifying lenses to examine small objects not visible to the naked eye, or in finer detail than the naked eye allows. Issues such as magnification and focus have an impact on diagnostic light microscopy and telepathology.
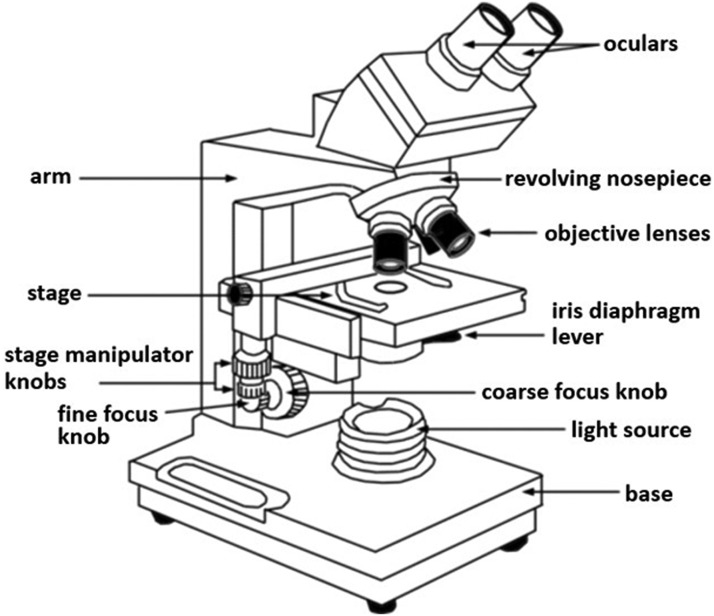
Fig. 1.
Conventional light microscope with its key component labeled. Focusing on a histopathology section on a slide is done by manually using the “coarse” and “fine” focus adjustment knobs.
Most LMs have the same structural components. The principal components include ocular lenses (eyepieces); objective lenses, mounted on a revolving turret; coarse and fine focus knobs (mechanically linked to the stage); a stage; a light condenser; and a light source. A camera is optional. The ocular lenses bring the image into focus. There is a set of objective lenses that collect light from the sample at the lower end of a compound optical microscope. Objective lenses (4–6) are characterized by two parameters: magnification (typically ranges from 2× to 100× ) and numerical aperture (ranges from 0.14 to 0.7). The stage (below the objective lens) supports the 1′′ × 3′′ GSs. In the center of the stage is a hole through which light passes to illuminate the specimen. A mechanical stage allows for small movements of the GS through control knobs that reposition the slide according to the desired x and y coordinates. The stage moves up and down for focus. This will be important in later discussions regarding telepathology systems.
The condenser is a lens designed to focus light from the illumination source onto the sample. For illumination techniques such as dark field, additional optical components precisely align the light path. An autofocus digital camera may be mounted on the microscope. For dynamic robotic microscopy, the moving parts of a conventional LM, including the focus knobs, are motorized and controllable remotely from a distance, using signals delivered over a telecommunication system. Whole slide imaging (WSI) telepathology systems are GS digital image scanners that house motorized microscopy components very similar to those in dynamic robotic microscopy systems.26
Telepathology Nomenclature
For all practical purposes, “telepathology” is synonymous with conducting light microscopy at a distance. “Digital pathology” and “WSI” are used in the literature as being synonymous with “telepathology,” but this can be confusing. “Digital pathology” is an umbrella term covering an assortment of areas in the much larger field of pathology informatics.32 Some industry leaders prefer “digital pathology” over “telepathology” because they anticipate bundling multiple forms on medical imaging into consolidated digital imaging medical product lines in the future.33,34 With regard to use of the competing terms, there have been more than 20,000 published articles on “telemedicine.” Of those on pathology listed in PubMed as of November 2016, there are 965 under “telepathology,” 395 under “digital pathology,” and 232 under “whole slide imaging.”35 It may take years for “whole slide imaging” to surpass “telepathology.”36
Telepathology Imaging Modalities
In contrast to teleradiology companies that provide diagnostic services for distinctly different imaging modalities (e.g., X-rays, CT, MRI, and PET), telepathology currently involves a single modality—viewing light microscopy images at a distance. Nonetheless, dark field and immunofluorescence microscopies are being used increasingly. At present, the primary aim of telepathology system innovators is to equalize, using electronic imaging, what ordinarily can be seen with human eyes looking at histopathology or cytopathology slides directly through the eyepieces of a conventional LM. This seemingly modest aim has proven to be somewhat elusive despite substantial investments of hundreds of millions of dollars by telepathology companies around the world.8,23
Technology Innovations
Early “clinical microscopy” specimens consisted mostly of blood smears, urinalysis specimens, and gram stains for microorganisms. Before opening the MGH television microscopy service, Robert E. Scully examined 100 clinical microscopy specimens by black-and-white television, and he concluded that color was not necessary to render a diagnosis in most cases. He also noted that when color information was needed, he could obtain the information over the telephone from the nurse site manager at the Medical Station, Logan International Airport, who was responsible for making and mounting the slides on the video microscope's stage. The nurse looked through the microscope eyepieces and described what she saw, while the remote physician told her how to focus and reposition the GSs.36 Of course, numerous technological innovations in telepathology have been made since these 1950s television-based initiatives (Table 1).26,37
Table 1.
Innovations in Telepathology System Designs
| HISTOPATHOLOGY AND CYTOPATHOLOGY GLASS SLIDE IMAGING SYSTEM | YEAR OF INNOVATIONa |
|---|---|
| Television microscopyb | |
| System assembly and testingc | 1952 |
| Research applications | 1955 |
| Clinical applications | 1968 |
| Static imaged telepathology | 1985 |
| Dynamic RT | 1986 |
| Static RT | 1989 |
| Hybrid dynamic RT/static image telepathologye | 1989 |
| Automated WSI telepathology | 1991 |
| Integrated automated and operator-directed VS processor telepathology | 1994 |
| Dual dynamic RT/WSI telepathologyf | 2011 |
| Mobile telepathology | 2007g, 2012h,i |
Dates are approximations based on publications, lectures, announcements, corporate annual reports, oral histories, or other sources of information.
Television microscopy systems lacked remote controls for microscope by a distant telepathologist. Microscope controls were operated by an on-site technician or nurse.
RCA/David Sarnoff Research Laboratories, Princeton, NJ.
Used low-cost PC-based image grabber boards.
“Hybrid” indicates system houses two independent imaging modes, dynamic RT and static image telepathology. These are viewed separately compared with simultaneous viewing on displays with “dual imaging” systems.
“Dual” indicates simultaneous use of multiple imaging modes, for example, using WSI telepathology and dynamic RT, in different layers, even toggling back-and-forth among layers, in a single diagnostic session. System operator can jump back-and-forth between the whole slide image modality and the dynamic RT modality, with shared x, and y coordinates. As the operator views images on a remote monitor, the whole slide image and underlying dynamic robotic image are linked and registered.
Ref. 39.
Ref. 40.
Ref. 41.
RT, robotic telepathology; VSs, virtual slides; WSI, whole slide imaging.
Classes of Telepathology Systems
Five classes of telepathology systems are listed in Table 2. The first four have been used in diagnostic assessment studies. As a practical matter, it is important for researchers to identify the class of telepathology system under consideration (including year of purchase, optional accessories, and serial number) and explain, where possible, how specific features may have affected outcomes, as they could impact use in actual clinical practice.38 Comparisons of human performance should be made within and among classes. The features listed in Table 2 should also be considered by consumers when selecting a telepathology system.23,38,39
Table 2.
Comparison of the Features of Telepathology Systems
| CLASSES OF TELEPATHOLOGY EQUIPMENT | IMAGE SYSTEM | REMOTE CONTROL | IMAGES/CASE | IMAGE SELECTION | AVERAGE TIME TO REVIEW | IMAGE RESOLUTION | BANDWIDTH REQUIREMENT | COST |
|---|---|---|---|---|---|---|---|---|
| Static imaging | Still | No | Limited | Host | Variable | Good to high | Low | Low |
| Dynamic imaging | Live | Yes | Unlimited | TP | Short | Good | Medium to high | High |
| Hybrid/dynamic static imaging | Live | Yes | Unlimited | TP | Short | High | High | High |
| WSI | Still | No | Unlimited | TP | Short | Good to high | Low to high | Moderate to high |
| Dual dynamic—WSI | Live/still | Yes | Unlimited | TP | Short | Good to high | High | High |
Modified with permission.5
TP, telepathologist; WSI, whole slide imaging.
Drivers for Telepathology
Telepathology can be used in a variety of clinical applications, including but not limited to primary diagnosis, intraoperative consultations (IOCs) (frozen section [FS] diagnosis), rapid cytology, secondary consultation (peer-to-peer case review or expert opinion), special studies (e.g., immunochemistry), archival review, quality assurance (QA), multidisciplinary interactions (e.g., tumor boards), and patient consultations.40 The U.S. Food and Drug Administration (FDA) has not yet approved telepathology for primary diagnosis, but is likely to do so in the near future.
Currently, there are important drivers for the deployment of telepathology in the United States. First, there is the need to have a surgical pathologist “on site,” or immediately available by telepathology, to render intraoperative FS diagnoses for certain surgical procedures (e.g., breast biopsies). Telepathology-based intraoperative FS diagnostic services have been in continuous use for decades and have rendered diagnoses on thousands of surgical cases.14,15 Second, telepathology provides timely second opinions on surgical pathology cases as pioneered at the Armed Forces Institute of Pathology (AFIP), and used at The University of Arizona and internationally.41,42 There are two types of surgical pathology second opinions: peer-to-peer surgical pathology case reviews43,44 and subspecialty pathologist's second opinions on either “routine” or challenging cases.45–48
Implementations of Telepathology Systems
At a multinational telepathology conference in Venice, Italy, in 2011, Vincente Della Mea noted that the conference marked the 25th anniversary of the publication of the first telepathology article (an editorial) in 1986.3,8,12 Twenty imaging companies demonstrated a wide variety of digital slide imaging devices, but none were interoperable with their competitors. At this multinational conference, telepathology standards were either nonexistent or at an early stage of development. Since then, more than 400 laboratories in 32 countries have published articles on telepathology, yet relatively few actually use telepathology in their practices beyond rendering occasional intraoperative FS diagnosis or second opinions on problematic surgical pathology.8
Issues Related to Telepathology Acceptance: The “Up-and-Down” Focus Question
The WSI telepathology equivalent of the manual focusing feature of light microscopy is a critical issue (Fig. 1). Some WSI vendors have chosen to bypass this issue, and in so doing they have potentially compromised the extent of sampling of tissue mounted on histopathology GSs. It is now incumbent on WSI manufacturers to demonstrate that the minimized extent of tissue sampling does not compromise diagnostic accuracy.17,23,26
The up-and-down focusing of LMs during surgical pathology and cytopathology specimen examination is generally regarded as the standard-of-care by surgical pathologists and cytopathologists. It is hard to imagine a surgical pathologist using a traditional LM without its focusing knobs for signing out surgical pathology cases on a routine basis. Historically, this gave rise to the original dynamic robotic telepathology (RT) systems that offered complete robotic remote control of up-and-down focusing on histopathology slides.3,12,13 There are no published diagnostic accuracy studies showing specifically that up-and-down focusing of conventional LMs is either a noncontributor to diagnostic accuracy in surgical pathology or an outdated, dispensable feature. In this regard, it should be emphasized that the autofocus feature of many commercial WSI systems is, in reality, an incomplete solution. Substituting a single optical plane representation of a histopathology slide, the commonest extent of viewing with current WSI instruments, provides only a partial imaging solution for some challenging surgical pathology and cytopathology cases.23 Given the WSI relatively shallow depth of focus operating with a 40 × lens, more than 80% of the volume of a tissue section on a GS might be inadvertently excluded from viewing using a single optical plane imaging system. In the process, critically important diagnostic information could be missed.26 Admittedly, this would not be a problem for many surgical cases for which the majority of the essential information contained in a histopathology slide is highly redundant, thus minimizing the tissue sampling issues.
Substituting WSI for conventional light microscopy (CLM) has yet to be embraced by the pathology community at large. This traces back to the introduction of static image pathology in the mid 1980s, which was oversold as a tool for obtaining second opinions.45 Ironically, 95% diagnostic accuracy was achievable with static imaging systems, but getting accuracy to 97%, the gold standard for light microscopy surgical pathology diagnosis, proved to be out of reach using a single optical plane imaging system.42 Might the absence of an up-and-down focusing feature contribute to the 2% diagnostic accuracy gap comparing CLM with WSI telepathology? Our hypothesis is that this could be the case.
Why is the up-down focusing on tissue sections so important in surgical pathology practice? To further explain, tissue sections are actually three-dimensional (3D) objects varying from 3 to 10 μm in thickness. An optical imaging system's “depth of field” is the distance between the nearest and the farthest objects appearing in focus within a scene. It can be less than 10% of the section thickness, increasing the likelihood that significant pathological structures might be missed in a single WSI. Furthermore, the depth of field varies with the focal length of the objective lens, its numerical aperture, and the wavelength of light, thus influencing what pathologists observe. Experienced pathologists know that extensive up-and-down focusing can be very important for rendering some LM diagnoses, and that critical diagnostic features could be overlooked any time they view a single WSI in isolation.20
In recent years, some manufacturers of WSI telepathology equipment have added a robotic imaging module to enable a remote system operator to manipulate images in three dimensions. Although dynamic robotic/static image-enhanced WSI first appeared in 2011 in Europe, such systems were not sold in the United States until 2014 because of potential patent infringement issues.9,26 According to the most recently published survey, four companies, Lieca/Aperio, Philips, Omnyx, and Ventana, do not offer a Z-stack (up-and-down focus) feature.39 This should raise a flag because it could reflect the conceding of an incremental increase of 1–5% in error rates. Four companies (Leica, Motic, Olympus, and Zeiss) market a WSI system with a live robotic microscopy module that could be a satisfactory solution to the up-and-down focusing issue for now, although an expensive alternative.
There are some remaining questions regarding the up-and-down focusing capabilities of current WSI instruments. There is limited information on the optimal Z-plane height intervals (0.1, 0.5, 1.0 μm, etc.). It has yet to be shown that viewing of Z-stacks or Z-planes would be actually equivalent to diagnostic performance using either a conventional hands-on light microscopy or a telepathologist using a robotic dynamic system offering unlimited “up-and-down” focusing capability.12,15,17 There are a number of diagnostic situations in which the absence of up-and-down focusing with WSI tend to limit the rendering of an accurate diagnosis. For example, the challenges of identifying and classifying certain microorganisms is tissue sections (e.g., bacteria, fungi, and parasites, especially in which speciation is required, as in malaria) using CLM may be compounded in telepathology. With respect to tumors, quantifying mitotic figures, identifying abnormal mitotic figures, and differentiating benign tissue from cancerous tissue can all be problematic. Also, quantitating tumor budding (TB) and “single file” cancer cell infiltration can be challenging. Examples of difficult cytology cases include body fluids because of the tendency of cells to aggregate into balls that are incompletely observed in a single optical plane.39 Fine needle aspirates present an analogous challenge.49 These types of situations should be represented in the case study sets to be used for the independent evaluations of various brands of telepathology systems.17
Additional Barriers
During the 1980s, some companies decided to keep things simple by incorporating only a single objective lens (e.g., 10 × or 20 × ) in their optics package. This eliminated the possibility of rendering diagnoses in cases requiring higher magnification necessary for the identification of certain bacteria. Other companies offered robotic motorized microscopy products that provided the full range of traditional LM magnifications (1.5 × –100 × high-dry objectives), but they were cumbersome to operate remotely and impractical for use in high-volume telepathology practices.31
In the United States, the rendering of primary diagnoses by telepathology has not been approved by the FDA, despite high levels of involvement of major medical imaging companies in the approval process.50–52 In other countries with active telemedicine programs, such as Canada, their FDAs have not presented major barriers to implementation. In the United States, the cumulative effect of these equipment issues and regulatory barriers to implementation was the creation of a high baseline of skepticism for telepathology within the U.S. pathology community.
Telepathology Evidence: Feasibility and Acceptance
The empirical studies on telepathology have focused mostly on the feasibility of various forms of telepathology technologies, diagnostic accuracy, and reliability as compared with CLM. We identified a total of 77 feasibility studies conducted in 27 countries and two multinational consortia between 2005 and 2016 (Table 3). These were based on a variety of applications, including virtual microscopy (VM), online platforms, dynamic/robotic systems, histopathology, and cytology; they were conducted in a variety of settings including academic medical centers, and regional and multinational consortia. Nearly all the studies were observational in nature, typically based on simple comparative designs, except where noted. Because the focus in this part of the article is on feasibility rather than effects, we ignored sample size as a criterion for inclusion. Nonetheless, sample sizes of feasibility studies in this review ranged from a low of 11 cases to a high of 650. The total number of cases for all reported studies was 4,920.
Table 3.
Summary List of Empirical Evidence in Telepathology Intermediate Outcomes
| REFERENCE | YEAR | COUNTRY | STUDY DESIGN | SAMPLE SIZE | INTERVENTION | FINDINGS | COMMENTS |
|---|---|---|---|---|---|---|---|
| Hitchcock and Hitchcock132 | 2005 | The United States | Comparative analysis | 524 | Excisional and aspirate biopsies/breast cancer | Sensitivity = 81.6%; specificity = 94%; accuracy = 94% | Malignant tumors: positive predictive value = 100%; negative = 94% |
| Burthem et al.133 | 2005 | The United Kingdom | Observational | 166 | Hematologic morphology | Navigation easy = 92%; image and field size adequate = 82% and 76% | In assessing malaria, only 51% found field size adequate |
| Hutarew et al.134 | 2006 | Austria | Prospective | 343 | Intraoperative FSs diagnosis in teleneuropathology | Average time for diagnosis = 26.1 min. 83% diagnosed in 15–20 min. Reliability = 100%. Accuracy = 97.9% | Smear slides take 16 times longer than light microscopy |
| Leinweber et al.135 | 2006 | Austria | Case control | 560 | Robotic microscope: histopathology | Concordance = 90.4–96% | Median time = 22 s; higher for melanoma |
| Odze et al.136 | 2006 | Germany–the United States | Comparative analysis | 152 | Diagnosis of dysplasia in ulcerative colitis | Interobserver agreement (κ = 0.32) | Lowest agreement in negative and high-grade dysplasia |
| McLemore et al.137 | 2006 | The United States | Comparative analysis | 202 | Intrapathology decision-making | 78% of residents exposed to FS vs. 80% in telepathology | No significant differences in exposure |
| Glatz et al.138 | 2006 | Switzerland | Comparative analysis | 246 | Urinary specimen/cytological diagnosis | High-grade cancers correctly diagnosed = 76%; low grade = 33.9% | Diagnosis by viewing static images not equivalent to real slide |
| Horbinski et al.139 | 2007 | The United States | Comparative analysis | 1,629 | Intraoperative neuropathological consults | Overall concordance = 85–87%. Average deferral rates: conventional = 10.6%; telepathology = 19.7% | Remote consultations require sophisticated technology, planning, communication and training |
| Butnor et al.140 | 2007 | The United States | Comparative analysis | 103 participants: 22 countries | Histological features: nonsmall cell cancer | Interobserver agreement: 36.9–93.2% | Considerable disagreement from 22 countries |
| Li et al.141 | 2007 | China | Comparative analysis | 400 | Intraoperative accuracy in surgical pathology consults | Accuracy = 97.25–95.5% for A and 96.25–94.75% for B | No significant differences between telepathology and glass slides |
| Bhele et al.142 | 2007 | India | Observational | 346 | Deferral reasons in static telepathology consults | Need for ancillary studies = 87%; clinical detail = 11%; poor quality image = 2% | Probable diagnosis matched final diagnosis 47% |
| Eichhorn et al.143 | 2008 | The United States | Record review | 191 | Gynecological cytology through Internet | Agreement on correct diagnosis: atypical squamous cell = 83%; high-grade lesion not excluded 100%; low-grade squamous 83%; high grade 94%; atypical glandular cells 40%. | Further accuracy may be achieved with training and experience |
| Li et al.144 | 2008 | China–The United States | Comparative analysis | 600 | Diagnostic accuracy of dynamic telepathology | Diagnostic accuracy ranged from 91.6% to 97% | Majority of cases diagnosed in 15–40 min; average = 17 min |
| Graham et al.43 | 2009 | The United States | Prospective comparison | 329 | Accuracy of telepathology in surgical pathology | Diagnostic concordance = 91.8% | Only 1.5% significant discrepancies. Improved job satisfaction |
| Horbinski and Wiley145 | 2009 | The United States | Comparative analysis | 1,321 | Intraoperative consultations in neuropathology | Diagnostic concordance in both light microscopy and telepathology = 70–72% | Differences in types of surgery and cancer must be considered |
| Dunn et al.146 | 2009 | The United States | Observational | 11,553 | Teleconsultations using robotic microscopy | Overall discordant diagnostic rate = 0.35%. Deferral rates = 2.5–28.7% | No relationship between deferral rates and discordance |
| Lopez et al.34 | 2009 | The United States | Observational | 154 | VSs for quality assurance | Concurrence with primary diagnosis = 90.3%; 2.3% major and 1.9% minor discrepancies | Small number of significant diagnostic discrepancies. |
| Evans et al.31 | 2009 | Canada | Comparative analysis | 790 | Accuracy and efficiency of robotic microscopy in a network | Diagnostic accuracy 98% in both modalities. Turnaround time in 88%: 19.98 and 15.68 min. 9.65 min to review slide | Deferral rate = 7.7%. Availability of service improved satisfaction |
| Wienert et al.147 | 2009 | Germany | Observational | 257 | VM in routine diagnosis | 95% of diagnostic paths would not result in deletion of any entries | Images parts stored after JPEG compression |
| Slodkowska et al.148 | 2009 | Poland | Comparative analysis | 304 | Intraoperative diagnosis in thoracic/pulmonary pathology | Diagnostic concordance = 87.5–100% | 100% agreement between telepathology and conventional slides |
| Alsharif et al.149 | 2010 | The United States | Comparative analysis | 792 | Telecytology of FNA (pancreas, gastrointestinal-tract, liver) | Telepathology adequate in 90.4% vs. 97.7% in conventional on-site review | Telepathology is adequate and accurate |
| Kldiashvili and Schrader150 | 2010 | Republic of Georgia | Comparative analysis | 420 | Accuracy of digital images in gynecological telecytology | 94% concordance in sharpness and quality | Digital images of adequate quality |
| Risio et al.151 | 2010 | Italy | Comparative analysis | 457 | Effectiveness of VM in colo-rectal cancer screening | Intraobserver and interobserver agreement = κ = 0.66 & 0.52 | VM effective in diagnosis of colorectal cancer |
| Zembowicz et al.152. | 2011 | The United States | Observational | 1,229 | Effectiveness of dermato-pathology consults | Same day turn-around time = 82% | Reduces cost and barriers to second opinion |
| Jukic et al.153 | 2011 | The United States | Observational | 606 | Intrapathologists diagnostic certainty | No discrepancies between two modalities | No significant differences |
| Nassar et al.154 | 2011 | The United States | Comparative analysis | 520 | Virtual immune histochemical slides of breast tissue | No discrepancies between two modalities in two sites: 91.3% and 99.0% | Reading slides on computer monitor was equivalent to conventional light microscopy |
| Georgoulakis et al.155 | 2011 | Greece | Comparative analysis | 270 | Diagnostic concordance of digital images of FNA of the thyroid | Interobserver agreement: κ = 0.869 and 0.939; intraobserver agreement: κ = 1.0 and 0.967 | No significant differences in accuracy between initial and subsequent reviews |
| Pagni et al.156 | 2011 | Zambia | Observational | 322 | Virtual pathology in a developing country: cervical cancer | No major changes made in diagnosis in 12.3% of cases | Telepathology enabled local clinicians to receive diagnosis and provide appropriate treatment |
| Schettini et al.157 | 2011 | Brazil | Comparative analysis | 135 | Histopathological second opinion in skin diseases | Agreement between two consultants = 88.1% and 80.7%; κ = 98.6% and 91.3% | Micrography is viable for second opinion consultation in dermatopathology |
| Campbell et al.158 | 2012 | The United States | Comparative analysis | 251 | Concordance between WSI and LM | Diagnostic concordance +97.7%; only two discordant cases were clinically significant | Technical difficulties encountered in 13% and associated with inability to observe microscopic organisms |
| Krupinski et al.159 | 2012 | The United States | Comparative analysis | 250 | Observer performance in virtual pathology | No significant differences in observer performance | Slight advantage for properly calibrated and color in workflow |
| Marotti et al.160 | 2012 | The United States | Observational | 240 | Efficiency of telecytology in endoscopic ultrasound FNA | Procedure time for conventional = 0.74 h; telecytology = 0.2 h | Telecytology improved system efficiency |
| Santiago et al.161 | 2012 | The United States | Comparative analysis | 127 | Pediatric oncology for developing countries | Concordance between telepathology and original diagnosis = 90.6% | Static and dynamic telepathology equally effective; training improves accuracy |
| Ayad and Yagi.162 | 2012 | Egypt, Italy, the United Kingdom, the United States | Observational/qualitative | 250 | WSI for e-education and telepathology | Saved time and money | Telepathology useful in developing countries |
| Tsilalis et al.163 | 2012 | Greece | Comparative analysis | 404 | Accuracy of telecytology for cervical smears | Interobserver agreement κ = 0.76 and 1.0 VSs comparable with conventional microscopy | Digital images can be used for rapid and accurate diagnosis |
| Shaw et al.164 | 2012 | Australia | Prospective analysis | 316 | Accuracy of VSs for assessing morphological characteristics of breast cancer | VSs comparable with conventional microscopy (vascular invasion, necrosis, and central scar) (κ = 0.37–0.78) | VSs acceptable and obviate travel and post |
| Fonyad et al.165 | 2012 | Hungary | Comparative analysis | 306 | Accuracy of VSs in routine histopathology | Good to excellent quality in 96%; consensus in 88.2% | Competency of pathologist more important than quality of images |
| Khurana et al.166 | 2013 | The United States | Comparative analysis | 200 | Accuracy of telecytology for malignancy | Concordance between preliminary and final diagnoses = 96% in telecytology and 93% in conventional microscopy | Discordant cases because of difficulty distinguishing small-cell and reactive lymph nodes |
| Gage et al.167 | 2013 | The United States | Comparative analysis | 500 | Accuracy of digitized vs. conventional images in cervical cancer surveillance | Intrareader and Inter-reader κ = 0.7–0.8 and 0.6–0.7 | Diagnosis of cervical cancer did not differ in the two modalities |
| Francissen et al.168 | 2013 | The Netherlands | Retrospective analysis | 628 | Accuracy of intraoperative FSs in breast cancer | FS predicted axillary status 83.6%. True positive = 12.4%; false positive = 0.3%; FN = 16.1% | High FN rate, and telepathology increased it |
| Rao et al.170 | 2013 | Italy | Comparative analysis | 334 | Accuracy of remote RCM in tumors | Sensitivity ≤90%; specificity ≤60% | RCM may be limited in classification of epithelial tumors |
| Tawfik et al.171 | 2014 | The United States | Comparative analysis | 335 | WSI in cervical cancer detection in screening | Evaluation of cell blocks feasible and of high quality; reliable and timely | Robotic imaging obviated the need for multiple focusing |
| Buck et al.172 | 2014 | The United States | Comparative analysis | 300 | WSI in surgical pathology | Discordance of 3.3–13.3% in traditional microscopy vs. 2.1–10.1% in WSI | No statistically significant differences between two modalities |
| Bauer and Slaw173 | 2014 | The United States | Comparative analysis | 217 | WSI in surgical pathology | Only two major and eight minor discrepancies | Safety and ethics of WSI for surgical pathology |
| Khurana et al.174 | 2014 | The United States | Comparative analysis | 217 | Nondiagnostic rate of EUS-FNA of pancreatic lesions | Nondiagnostic rate for Groups 1 and 2 = 3.7% and 25.6% | Telecytology reduced nondiagnostic rate in solid lesions |
| McMahon et al.176 | 2014 | The United States | Comparative analysis | 298 | Image resolution | Concordance index = 0.943 | No significant differences in concordance in number of passes for adequate telepathology |
| Mpunga et al.177 | 2014 | Rwanda–the United States | Observational | 437 | Efficiency of anatomic pathology in rural areas | Median time for receipt of report = 32 days. 55.8% of cases confirmed malignant, 37.3% benign, 6.4% inconclusive | Model serves as road map for pathology service in resource-limited countries |
| Tetu et al.178 | 2014 | Canada | Observational | 7,490 | Intraoperative consults, expert opinion, urgent analysis and supervision | Concordance = 98%; expert opinion rendered within 72 h in 85% of cases | Network provided rapid and high-quality pathology in large region |
| Chen et al.179 | 2014 | China | Observational | 16,247 | Accuracy of WSI in national consultation program | Agreement between initial diagnosis and expert = 59.8%; disagreement = 24.2%; no preliminary diagnosis = 16% | Program could solve uneven distribution of resources and quality control in China |
| Ribback et al.180 | 2014 | Germany | Comparative analysis | 1,204 | Accuracy of VS telepathology in intraoperative FSs in urology, GYN, and derm | Accurate diagnosis = 98.59%; discrepant = 1.41% | Quality is highly acceptable and investment is lower than robotic microscopy |
| Carey et al.181 | 2014 | Malawi/the United Kingdom | Observational | 197 | Timely diagnosis in resource-limited country | Diagnosis made in 52%: 23.35% discordant results; 19.3% local provider unable to make diagnosis. Reports by distant team made within 24 h | Project had a positive impact on clinical management |
| Silveira et al.182 | 2014 | Brazil | Comparative analysis | 2,592 | Accuracy of digital images in skin cancer screening | Agreement between two oncologists: 85.8% and 93.5%; sensitivity 89.3%; specificity 38.5% and 25% | Overall accuracies of two oncologists: 85.3% and 87.3% |
| Thrall et al.183 | 2015 | The United States | Observational | 1,000 | Validation of WSI | Interobserver agreement = 79%; major discrepancies = 1.8%. Concern for neoplasia: κ = 0.878 | Scans of × 20 magnification may be insufficient for small focal findings |
| Jones et al.184 | 2015 | The United States | Comparative analysis | 477 | Evaluation of WSI in multi-institutional setting | During training (correlation 94.6%, 4.6%, and 0.8% minor and major discrepancies. During clinical trial 5.4% major discrepancies) | Potential issues: IT collaboration, work flow, and division of labor |
| Zhao et al.185 | 2015 | China/the United States | Observational | 1,561 | International collaboration in telepathology | Average turnaround time = 5.4 days. Final diagnosis identical in 25.6%. Diagnosis modified significantly in 50.8% | International telepathology consultation improves patient care |
| Papathomas et al.186 | 2015 | International | Observational | 351 | VM in adrenal cancer | Agreement among reviewers (κ = 0.7338 in two-tiered classification and 0.6543 in three-tiered classification) | Immunochemistry is a reliable tool to identify patients with mutations |
EUS, endoscopic ultrasound; FN, false negative; FNA, fine needle aspiration; FS, frozen section; GI, gastrointestinal; IT, information technology; RCM, reflectance confocal microscopy; VM, virtual microscopy; VS, virtual slide.
Starting in 2005, seven studies met the selection criteria, two each from the United Kingdom and the United States, and one each from Ireland, Finland, and Hungary. The first U.K. study was based on a survey (n = 500, response rate = 47%) of U.K. histopathologists, and it collected information regarding the availability of infrastructure for telepathology, as well as training for and attitudes toward digital pathology.53 Nearly two-thirds (64%) of the respondents reported having a digital camera mounted on the microscope in their clinics, but only 12% had any of the requisite equipment for transmission or receipt of images; 59% received no training in digital imaging; and 58% indicated that legal issues constituted a significant barrier to the practice of telepathology in the United Kingdom. The authors suggested that the limited use of telepathology was probably because of the lack of appropriate training. A majority (69%) of the respondents expressed interest in using videoconferencing for remote attendance at professional meetings, not necessarily patient care. However, the low response rate precludes drawing any definitive conclusions from the survey findings.
The second U.K. study investigated the safety and effectiveness of sending still digital images through e-mail during neurosurgery.54 A sample (n = 48) of neurosurgical smear specimens was digitized, compressed, and sent by e-mail for remote reading by a consultant. The original “permanent section” diagnosis served as the gold standard. Average time for image selection and digitization was 9.51 min. Overall diagnostic accuracy with digital images was 85.4% (sensitivity 100%, specificity 85.4%), but accuracy was 100% for historical smears. “Most inaccuracies were in grading and caused by problems with field selection and familiarity with the technique.” Based on their findings, the authors concluded that static digital images were reliable and safe for interpreting tissue during neurosurgical procedures.
The first U.S. study in 2005 (n = 110) investigated the feasibility of dynamic telepathology in Mohs surgery.55 The most common reason for requesting a surgical pathology consultation in this procedure was to distinguish between basal cell carcinomas and benign histological lesions on FSs. The sample consisted of 50 fixed-tissue slides of basal and squamous cells, 40 FS slides for presence or absence of tumor, and 20 FS slides for IOC. Subsequently, all slides were randomly reviewed by the same dermatopathologist using CLM. The authors concluded that “Overall, the use of telepathology in this Mohs surgery practice enhanced the quality of patient care by providing immediate consultation in a convenient manner.” The system obviated the need for further excisions, whereas it “offered” a unique educational and collaborative opportunity between the dermatopathologist and the Mohs surgeon.
The second U.S. study (n = 32) investigated the feasibility of VM as an automated screening and interpretation process for cervical cytology through an Internet connection with low-resolution images.56 Screening for cervical carcinoma accounts for the phenomenal 70% decline in mortality from this disease since widespread screening was started in the 1950s. Today, the majority of deaths from cervical carcinoma occur in under-screened populations. In this study, masked reviews by two telepathologists resulted in 37.5% false negative (FN) and 8.3% false positive (FP) rates, and an overall concordance of 84% (specificity of 92% and sensitivity of 63%). The high FN rate compares unfavorably with the current standard of ≤10%. However, ongoing use of the system improved sensitivity. The results supported the hypothesis that “Internet transmission of images derived from automated screening devices for interpretation at remote locations has the potential to provide an effective screening program for countries that lack a trained cytology infrastructure, and to provide a more efficient, economic and centralized way of triaging patient samples.” The system of image selection, digital storage, electronic transmission, and remote interpretation worked reasonably well.
From Ireland, a study (n = 70 pathologists, reviewing 10 breast biopsies) evaluated the performance of an online pathology platform (ReplaySuite) for needle core breast biopsies, and it provided pathologists' opinions regarding its potential for training and QA.57 The intervention used a virtual double-headed microscope. Of 70 invited pathologists, 9 agreed to participate. Seven of nine indicated that ReplaySuite was “of some or great benefit in pathology training and quality assurance.” The authors indicated that “further work is planned to determine whether use of ReplaySuite can result in improved diagnostic ability.”
From Finland, a study (n = 62 biopsies) investigated the validity of Web-based VM in terms of interobserver diagnostic agreement of a comprehensive set of prostatic needle biopsies.58 The study used Gleason grading scores (widely used for grading prostatic adenocarcinoma, which entails a significant degree of interobserver variability) for comparison with scores given by expert uropathologists. The Web-based VM offered the “possibility to view the entire specimens, that is, any part of the whole slide at any magnification.” The study concluded that this intervention was “…an effective method to the evaluation of inter-observer variability, and that it is a promising new tool for teaching and standardizing Gleason grading.”
Finally in 2005, the Hungarian experience with telepathology was described, including several projects implemented with support from the European Union.59 “Electronic fixation of the images and their transmission by telephone line (Integrated Services Digital Network [ISDN]) is easily available and an important feature of the multimedia system applied to telepathology.” Typically, 5–10% of yearly 600–700 thousand histopathological diagnoses involve a second opinion, mostly from other European tumor experts. “The telepathology system provided an opportunity to discuss difficult cases, and this consultation led to improved diagnosis in several cases.” However, no specific findings were reported.
Four studies met the selection criteria in 2006, one each from the United States, India, Iran, and a European consortium. The U.S. study (n = 20 breast core biopsies) involved an analysis of human factors that affected the proficiency of pathologists using CLM.60 The authors pointed out that VM removed the barrier to access for the operator's eyes and opened the door for studies on human factors and visual search strategies. Their analysis revealed that when “a virtual slide reader initially looks at a virtual slide, his or her eyes are very quickly attracted to regions of interest,” which are likely to contain pertinent diagnostic information. These types of human factor studies are important because the digitized WSIs are very large, and even the best viewing interfaces are slower and more cumbersome than the traditional LM. Increased acceptance of telepathology may depend significantly on solving these human factor challenges.
An Indian study (record review, n = 46) assessed diagnostic concordance between GSs and telecytology using the Internet.61 The sample consisted of cytology cases from two rural hospitals located about 500 km away from each other. The cases were submitted for second opinion using static store-and-forward telecytology. The average number of images per patient was 15. Eighty-nine percent of the requests received a report within 3 days, and 54% within 1 day. “A clinically useful diagnosis was rendered in 91% of the cases, with 74% complete concordance. Eleven percent were deferred for glass slide review.” The authors concluded that “…telecytology using the Internet is a rapid and effective method of providing expert diagnosis…”
Also based on record review (n = 161), a report described the findings from the first experience with static telepathology in Iran.62 This project involved two academic cancer centers, one in Iran and the other in Switzerland, and the report was based on data for the initial 32 months. Definite diagnosis was achieved in 54.7% of the cases, recommendations for further evaluation were made in 26%, and discrepancies were noted in 19%. One-in-four consultations were completed within 1 day. The rate of arriving at a final diagnosis was higher in histology than in cytology, possibly because of (1) inappropriate sampling and (2) problematic cases “…that a definite diagnosis could not be made for them even in primary consultation.”
Finally, we include a special report from a European consortium (including seven countries) concerning VM in virtual tumor banking.63 Although this was not an empirical study, it demonstrated the high level of interest in telepathology through the Internet in Europe as a substitute for GSs. The images were stored on a server that enabled the user to choose magnification on any segment in the scan. “This offers new opportunities in histology review, overcoming the necessity of the dynamic telepathology systems to have compatible software systems and microscopes…” Users had ready access to this bio repository (The European Human Frozen Tumor Tissue Bank) simply by having Internet access and a computer with a high-quality monitor.
In 2007, three studies met the selection criteria, one each from the United States, Iran, and a multinational consortium. The U.S. study (prospective analysis, n = 100) assessed a telepathology system using an ultraportable computer, a wireless local area network (LAN), and a wide area network (WAN) in terms of concordance with original FS diagnosis rendered by other staff pathologists.64 Diagnostic agreement was achieved in 95% of the cases. The 5% discordant cases “…were deemed to be errors in the original frozen-section diagnosis; 1 was not clinically important; and 2 were believed to have potential clinical implications.” The average response time (from a faculty consultant back to chief resident) was 1 min and 42 s for wireless WAN and 51 s for wireless LAN. The authors concluded that this system was “…useful for frozen-section consultation between an experienced resident and a faculty member in pathology.”
A feasibility study (n = 50) of telepathology diagnosis in pleural cytology was conducted in Iran. The project connected an academic medical center in Iran with two academic medical centers in the United States that provided the consultations remotely.65 The sample consisted of 50 (randomly selected) pleural effusion smears that normally require a cytological examination of the pleural fluid to ascertain malignancy. The slides were initially diagnosed as 23 benign, 7 suspicious of malignancy, and 20 malignant (2 mesotheliomas, 5 ductal carcinomas of the breast, 5 adenocarcinomas of the lung, 4 adenocarcinomas of the stomach, 2 adenocarcinomas of the ovary, and 2 small cell carcinomas of the lung). Concordance of diagnosis between telecytology and GSs between the two U.S. centers and the original diagnoses were 86% and 84% respectively; 14% and 16% were discordant. The remote diagnosis was correct in 76% and 82% of the cases, respectively, at the two institutions, whereas the correct diagnosis of GSs review in Iran was 82%. The authors suggested that “…telecytology consultation may be useful in minimizing the risk of loss, breakage or non-return of limited cytology material, that the greatest benefit is the ease of sharing images, and the more efficient use of scarce cytopathologist resources and expertise.”
A multinational consortium of researchers (Austria, Italy, Iran, Japan, the United States, Sweden, and Slovenia) investigated the feasibility and diagnostic agreement of a virtual slide system (VSS) in teledermatopathology.66 This study (n = 46) was based on diagnostic reports made by 12 teleconsultants from six different countries who reviewed virtual slides (VSs) of inflammatory skin disease, and their diagnoses were compared with the gold standard of conventional slide viewing. “Telediagnosis agreed with the gold standard and conventional diagnosis with an average of 73% and 74% respectively.” Complete concordance was observed in 20% of the cases. Among cases with incomplete clinical data, the level of agreement decreased to 65% and 66%, respectively. “Only 3 of the 4 cases of inflammatory skin diseases were correctly diagnosed remotely with the VSS.” The authors concluded that the Web-based application they used was not “completely feasible for teledermatopathology of inflammatory skin disease.” The main obstacles were incomplete clinical data and the intrinsic difficulty of diagnosing inflammatory skin disease.
In 2008, six studies met the selection criteria, one each from the United States, Poland, Taiwan, Japan, the United Kingdom, and South Africa. We also include two descriptive reports from Egypt and Italy that shed light on the importance of telepathology for developing countries and the design of an assessment system in telepathology.
The U.S. study (n = 100) evaluated the effectiveness of a telepathology system for consultations between residents and faculty using fine needle aspiration (FNA) specimen to ascertain malignancy.67 The study assessed diagnostic adequacy, preliminary interpretation, and final diagnosis in telepathology. The initial 50 cases were transmitted through Internet to remote cytopathologists who responded by telephone. Diagnostic concordance was 97% and accuracy was 99%. Screening time ranged from 41 s to 30.19 min. Viewing times were shorter, ranging from 10 s to 12.5 min. The authors concluded that the “telepathology system is efficient and accurate for initial assessment and preliminary diagnosis of FNA specimens, but we recommend its use by more senior and experienced trainees.”
The Polish study (n = 20) investigated the efficacy and usability of VSs in an interactive microscope emulator system (which allows one computer behave like another computer).68 A sample of 20 high-quality VSs was evaluated initially through the Internet and subsequently by CLM. Overall concordance was 85%, and the 15% discordant cases were attributed to “… poor quality of tissue sample or insufficient immunostaining…” Pathologists who participated in the study found the download speed of VSs to be adequate. In addition, the study demonstrated that experience in telepathology was associated with reduced time for rendering VS diagnosis.
From Taiwan, a low-cost telepathology system for intraoperative FS consultation was evaluated in terms of diagnostic accuracy.69 The study (n = 50) assessed the concordance between the diagnosis made by the pathologist on duty and that of a subspecialist or senior telepathologist who served as a consultant. The tissues were derived from 10 organ systems (majority were from brain/spinal cord). The results indicated a high level of agreement (κ = 0.97) between the pathologist on duty and the remote consultant. However, in two cases (or 4%), histopathology GSs were deemed to be slightly superior to VSs. For example, a breast cancer with a small focus of stromal invasion was not recognized by the telepathologist, and the decision on an inflamed tissue mass with few atypical cells was deferred in telepathology. However, neither case had a clinically significant negative impact. The time for telepathology averaged 4.5 min, and there was “no record of complaint related to problems with the computer system.” The authors observed that telepathology was a “…good tool for FS consultation and imposes little additional cost.”
A small Japanese study (n = 15) investigated the effectiveness of VS telepathology in judging negative or positive surgical margins in intraoperative remote diagnosis.70 Telepathology took about 10 min using a 10 × objective when the specimen measured less than 20 mm in the maximal dimension. The rendering of diagnosis by telepathology was completed within 5 min, and all diagnoses were correct. However, these findings are only suggestive in view of the small sample.
A U.K. study (n = 104 pathologists) assessed interobserver agreement in grading 20 colorectal cancers in a nationwide Web-based survey of histopathologists.71 Of 1,347 U.K. consultant histopathologists asked to participate, 80 declined because of lack of subspecialization or retirement, and only 104 completed the questionnaire. The overall response rate was only 8%, but the respondents represented 32% of U.K. Trusts. At any rate, interobserver agreement was generally low as measured by κ values. Grading results were 0.351 and 0.358 for low- and high-grade tumors, respectively. The individual scores for grades “well, moderate, and poorly differentiated” were 0.467, 0.259, and 0.358, respectively. Hence, overall agreement in both grading systems was only fair.
A feasibility study (n = 60) of a dynamic telepathology system delivered over a national service network was conducted in South Africa.72 Digital microscopes with Internet connections were installed in national laboratories, thereby allowing real-time viewing of full slides any time of the day. Usefulness was tested with 60 cases to ascertain how the network can help small histopathology departments lacking expertise in specialty areas, such as dermatopathology, oncology, and hematopathology. The initial results were positive, and the quality of the images was judged to be “very good,” but no empirical findings were reported.
Finally, we include two descriptive reports of international telepathology projects as examples of (1) telepathology serving low-resource countries and (2) the feasibility of low-cost architecture for telepathology in this setting. An Egyptian report described a telepathology pilot project linking two hospitals in Egypt and Italy,73 employing WSI to transmit images from the Egyptian to the Italian hospital. The authors concluded that they “…saved a lot of time and money and succeeded in providing our patients with a better medical service.” However, they did not quantify these benefits. An Italian report described the design of a telepathology system using VSs as well as its acceptance.74 Here again, the results were stated in qualitative terms. “Preliminary results indicate a high degree of acceptance from the expert pathologists.”
In 2009, only two studies met the selection criteria, and they were conducted in Greece and the Republic of Georgia. In addition to presenting findings from these two studies, we provide brief reviews of three descriptive reports.
The Greek study (n = 106) identified the minimum requirements for remote grading of astrocytomas (a brain cancer) in terms of histological characteristics. A histopathologist examined tissue samples of low- and high-grade astrocytomas.75 The accuracy of VSs was compared with that of conventional GSs, in addition to using a custom-designed decision support system. The use of the decision support system resulted in an overall improved accuracy of 91.8% in telepathology. The authors concluded that their findings “…suggest that a telepathology system might be valuable for accurate grade diagnosis of astrocytomas…. This could significantly reduce the overall time and cost of diagnosis.”
The Republic of Georgia report described the implementation of telepathology and the results of the initial experience in telepathology consultations.76 Data were based on 140 cases in general pathology. The average number of consultants per case was three, and the remote diagnosis was rendered in less than 12 h. Primary diagnosis was confirmed in 65.7% of the cases, corrected in 17.8%, additional laboratory tests suggested in 7.1%, and in 9.3% the images were of poor quality
Three U.S. descriptive reports focused on (1) digital pathology in drug discovery,77 (2) Internet-based interpretive information for laboratory tests,78 and (3) the design, implementation, and maintenance of an effective telepathology service for neuropathologists.79 The first report suggested that “…digital pathology is transforming global pharmaceutical research by enabling data sharing… around the world.” Somewhat similar and complementary conclusions were reached by the second report in terms of the benefits of using the Internet for sharing laboratory test results in patient care. The third report discussed the benefits of telepathology in IOCs in terms increasing workflow efficiency, enhancing QA/quality control, and integration into other informatics modalities.
In 2010, only three feasibility studies met the selection criteria, one each from Denmark, Germany, and Italy. The Danish study (n = 96) evaluated the validity and diagnostic performance of VM in routine histological diagnosis of skin tumors, more specifically “…whether conventional microscopy of skin tumors can be replaced by virtual microscopy.”80 Diagnoses rendered on 4 of 96 VSs were compared with those of CLM slides, and this was repeated at least 3 weeks later. Slides that were difficult to interpret were evaluated to assess the reasons for the difficulty. The accuracy of VM was 89.2% compared with 92.7% for CLM. The κ coefficient for intraobserver agreement for both groups was 0.93. The diagnostic accuracies for “benign, premalignant, and malignant” comparing VM versus CLM were 90.0% versus 92.9%; 57.5% versus 75.0%; and 100% versus 100%, respectively, for each diagnostic category. VM of actinic keratosis (premalignant) resulted in lower accuracy. However, re-evaluation of the slides showed that diagnostic difficulty occurred in both VM and CLM. In addition, the authors explained that the observed differences may be attributed to “…the pathologists' lack of experience using the virtual microscope.”
The German study (n = 26) investigated the feasibility of “telemicroscopic conferences” for children with suspected or proven malignant solid tumors in the Perm Territory (Russian Federation).81 A microscope and a video camera in Perm captured the images, which were subsequently transmitted to four cooperating institutions in Germany through Internet at low bandwidth (54 kilobits per second capacity). This international cooperative project demonstrated “… proof of principle to obtain second opinions in short time over far distances for seldom [rare] diseases on a scientific level.” Supportive evidence was also provided by an Italian pilot study that demonstrated the feasibility of integrating digital cytometry in telemedicine for second opinion.82
A total of 13 studies met the selection criteria in 2011: 4 from the United States, and 1 each from Poland, Germany, Italy, Egypt, Austria, Georgia, The Netherlands, the United Kingdom, and a European consortium. Some of these studies were conducted by international collaboratives involving two or more countries.
The first U.S. study (n = 79) evaluated telepathology for rapid diagnosis of ultrasound-guided FNA of thyroid nodules.83 Real-time images of thyroid nodules were captured by a digital camera attached to a microscope and transmitted to a pathologist through an Ethernet connection for a preliminary diagnosis. Oral communication with the on-site cytotechnologist was done by telephone. Preliminary diagnoses of “…benign, suspicious/malignant, and unsatisfactory” were 72%, 7%, and 21%, respectively. “The accuracy rate between the final cytology and preliminary telecytology diagnosis was 94%.” The main reason for the discrepancy between the two modalities was the presence of additional material on the slides and cellblock section. The authors concluded that telecytology “…is highly accurate… and it allows pathologists to use their time more efficiently…”
The second U.S. study (n = 78) examined interobserver variability in diagnostically challenging endometrial biopsies using the Internet.84 Eighteen cases were selected from a pool of gynecological consultations illustrating common diagnostic dilemmas and subsequently presented as quiz cases. Participants from 13 countries (60% from the United States) were presented with endometrial biopsies and were asked to choose one of four diagnoses: “(1) polyp, (2) benign endometrium, (3) tubal metaplasia, or (4) adenocarcinoma.” Agreement ranged from 17% to 100%, with averages of 88% in (1), 87% in (2), and 75% in (3). The overall average agreement for endometrial hyperplasia was 63%. This international online quiz demonstrated general problems in diagnosing endometrial neoplasia, which are likely to require consensus review.
The third U.S. study (record review, n = 126) investigated the feasibility of IOCs for specialty neurosurgery.85 Slides were mounted on a robotic microscope for remote viewing using a virtual private network. The system also provided access to pertinent radiological images as needed. The average time for rendering diagnosis was 11 and 20 min from initial notification. This time interval was shorter than the usual in-person consultations. Hence, the authors concluded, “the result was an effective means of distributing neuropathological expertise…”
The fourth U.S. study (record review, n = 72) assessed the use of a mobile high-resolution device for assessing remote FS of WSI.86 Available clinical information and gross descriptions of images were included in the linked files. All FS slides were cut and stained by trained histotechnologists or pathology assistants, and categorized by case type, tissue of origin, and nature of question to the consultant. The average scan time per slide was 1 min and 20 s. Diagnostic accuracy was 89%, minor discrepancies were noted in 8%, and clinically significant discrepancies were noted in 3%. Overall κ statistic was 0.85. Five of the six consultants reported having some difficulty using the software. The authors concluded that although it is possible to obtain acceptable results in remote diagnosis, the main obstacle was slide navigation at high magnification.
As indicated earlier, in 2012 there were eight additional studies that met the inclusion criteria. The first was a Polish study (n = 28) that examined the accuracy of a remote quantitative image analysis of tumors of the central nervous system using WSI.87 The study assessed the accuracy and reliability of remote assessment of morphological features and the Ki-67 LI labeling index (an expression of nuclear antigen or cell proliferation) with computerized analysis of medical images (CAMI). The authors concluded that the results demonstrated that “…the remote automated Ki-67 LI analysis performed with the CAMI algorithm on the whole slide images of meningiomas and oligodendrogliomas could be successfully used as an alternative method to manual reading as well as to digital images quantitation with CAMI software.” They also suggested that specialized training for this system would be necessary.
An international study (n = 96) evaluated the feasibility and diagnostic accuracy of Internet-based dynamic telepathology between Uganda and Germany.88 It compared the performance of robotic telemicroscopy—using e-mail and Skype—to CLM in terms of exchanging clinical and diagnostic information. “It took approximately 30 min for a pathologist to learn to use the telepathology system and 4–25 min to read a case remotely.” The pathologists at the two locations agreed on the diagnosis in 97% of the cases. Discordant diagnoses were related to difficult cases, including soft tissue sarcomas and primitive tumors.
The performance of a binational (Slovenia and Italy) telepathology consultation program was assessed in terms of feasibility, diagnostic quality of images, and communication reliability.89 Sixty histology and cytology cases were used to assess image quality, time needed for diagnosis, and system compatibility with standard videoconferencing software. The results did not reveal any discrepancies between local and remote diagnosis. Once the systems were established and fully operational, the time needed for most operations was similar.
The results of a similar binational consultation project between Egypt and Italy were reported in 2011.90 Although the project ran for 7 years, no empirical data were reported. The authors reported that consultations were completed “…on many problematic pathological cases… and we saved a lot of time and money and succeeded in providing our patients with a better medical service.”
A study (n = 45) in Austria assessed the feasibility of dynamic telecytological evaluation of CT-guided lung biopsies.91 The microscope was operated by a radiologist and a technician, and the cytological samples were diagnosed by a cytologist as “benign, malignant, atypical cells, or non-diagnosis.” The gold standard was based on a consensus reading by two independent cytologists. Diagnostic accuracy was 100% when the radiologist operated the microscope and 95.6% when the technician did. The report concluded that “…telecytological evaluation of imprint samples from CT-guided lung biopsies is feasible because it can be performed with high diagnostic accuracy if personnel from the radiology department operate the microscope.”
A Republic of Georgia study (randomized controlled study [RCT], n = 50) analyzed diagnostic accuracy and interobserver agreement of telecytology diagnosis of cervical smears in a QA program.92 Digital images (2048 × 1536 pixels) of a mixed set of cervical smears were transmitted by e-mail, and the diagnosis of GSs (after 3 months) and digital images was made independently by three cytologists in a double-blind manner. The results showed “…good inter-observer agreement for the first (correlation coefficient of 0.82) and second (0.68) GS diagnoses, and the first (0.80) and second (0.66) digital image diagnoses.” It was concluded that “digital images are suitable substitutes for glass slides; telecytology can be used as an alternative method for the cytologic diagnosis of cervical smears, particularly in a quality assurance program.”
An evaluation of digital images as a substitute for GSs was conducted in the United Kingdom in a national prostate QA scheme.93 The sample consisted of 51 pathologists who participated in an external QA scheme for evaluating prostatic biopsies. Their responses for GSs were compared with those of 24 pathologists who reviewed VSs. “Levels of agreement for diagnostic categories using virtual slides were moderate to substantial, comparable to those found using glass slides.” A higher level of agreement was observed for higher grades of cancer than for lower grades (using Gleason grading).
Finally, in 2011, a multinational (Denmark, the United Kingdom, Germany, Italy, Switzerland, France, and Turkey) study (n = 20) assessed reliability of biopsy diagnoses of cardiac allograft rejection made by different pathologists in a European telepathology system.94 Twenty sets of endomyocardial biopsies, preselected by 2 pathologists and digitized, were viewed over the Internet by 18 pathologists from 16 transplant centers in Europe. “The combined kappa value for all grades of acute cellular rejection (ACR) diagnosed by all 18 pathologists was 0.317 for the 1990 grading system and 0.3923 for the 2004 system.” As noted, agreement was higher when using the more recent classification scheme. However, the authors indicated that although these results should be considered preliminary, “…virtual microscopy is feasible as a tool for international collaboration and standardization in this challenging area of biopsy diagnosis.”
In 2012, 15 studies met the selection criteria: 5 from the United States, 3 from Canada, 2 from Japan, and 1 each from Australia, the United Kingdom, The Netherlands, Kenya, and a multinational consortium.
A U.S. comparative study (n = 110) evaluated the reliability of endoscopic ultrasound-guided FNA of pancreatic masses in two modalities, dynamic telecytopathology and CLM.95 The preliminary diagnoses of “benign, atypical/suspicious, and positive” for malignancy were 69%, 7%, and 24% in telecytology (n = 55), and 60%, 9%, and 31% in CLM evaluation (also n = 55). “The overall concordance between the preliminary and final diagnosis was 84% for telecytopathology and 87% for conventional microscopy.”
The feasibility and diagnostic accuracy of telecytopathology were evaluated for FNA of para tracheal lymph nodes in endoscopic bronchial ultrasound.96 The study was conducted in three phases: (1) a retrospective review of 2 sets of 20 cases (total n = 40) by 2 sets of 4 pathologists and cytotechnologists; (2) a prospective assessment of 56 telecytology cases, compared with CLM; and (3) an in-person diagnosis of 100 cases without telecytology. Concordance was measured by diagnostic agreement on a final diagnosis of “benign, atypical, or malignant.” The results for Phase 1 showed the following accuracy rates: 95% for malignancy and 96.2% for benign diagnosis. In Phase 2A, complete concordance was obtained in 95% of the cases, and in Phase 2B concordance without telecytology was 97%.
A third U.S. study (n = 60) assessed the application of telecytopathology for real-time FNA of endobronchial ultrasound (EBUS)-guided mediastinal and pulmonary cases.97 It was preceded by a learning phase in which 22 endoscopic ultrasound-fine needle aspiration (EUS-FNAs) were examined to determine time (for diagnosis) and efficiency of telecytopathology. In the evaluation stage, 38 pancreatic endoscopic ultrasound (EUS) cases were assessed. The cytopathologist was blinded to the results of the diagnosis in both phases. The results indicated that time to preliminary diagnosis was 53 s in the learning phase and 49 s in the validation phase. “There was 100% correlation between (fine needle aspiration interpretation) RFI and (telecytopathology) TeleCyp assessment for specimen adequacy.” Hence, the authors concluded that telecytopathology is “…a powerful alternative, time-efficient strategy” for providing specimen triaging and interpretations of FNA.
A fourth U.S. study (n = 29) investigated the feasibility of static image telepathology for performing accurate dermatopathology consultations originating in Africa.98 The diagnostic interpretations were provided by a U.S. academic medical center at no cost to the sender. Diagnostic accuracy was obtained on average in 91% of the cases (ranging from 86% to 95%). “Comparison with the glass slides showed that the technology diagnosis was limited by inappropriate field selection in one case.” Interobserver concordance was high (κ = 0.86).
A fifth U.S. study (n = 109) evaluated the use of static digital telepathology for diagnostic and educational support for pathologists in the developing world over a period of 40 months.99 A total of 109 cases were submitted (dermatopathology [n = 29], hematopathology [n = 14], cytology [n = 13], and soft tissue [n = 13]). “The static images enabled a complete or partial diagnosis in 91.7% of the cases.” According to the authors, the system was “simple, cost-effective, reliable, and efficient.”
Three studies were conducted in Canada in 2012. The first (n = 103) was designed to (1) validate the effectiveness of teledermatopathology as a diagnostic tool, (2) test its effectiveness in inflammatory and melanocytic lesions, and (3) assess diagnostic accuracy at two resolutions (20 × 0.5 vs. 40 × 0.25).100 The study had three arms: (1) routine cases (n = 79), (2) inflammatory cases (n = 12), and (3) melanocytic cases (n = 12). Diagnostic concordance was 96% in the first arm and 100% in the second and third arms. As expected, higher resolution of images improved diagnostic accuracy.
The second Canadian study (n = 30) compared remote assessment of digitized FS and smear preparations for intraoperative neurotelepathology versus CLM.101 A sample of brain tumors was submitted for IOC. In two cases, the tumor was on the tissue smear but not on the FS, and in one case, the tumor was only on the FS. Both problems were attributed to sampling issues (i.e., not the telepathology aspect). The findings indicated that “digitized tissue smears are suitable for intraoperative neurotelepathology and provide comparable information to digitized frozen sections at medium power magnification.”
The third Canadian study described the challenges of implementing a “patient-oriented” telepathology network in Eastern Quebec.102 Whereas this report was mostly descriptive, it provided detailed information on the time required for FSs: average time required was 23.25 min, macroscopy 5.9 min, section 7.7 min, slide scanning 2.6 min, access to image 2.1 min, and interpretation 2.8 min. More importantly, the challenges included the need to adapt to the new system, reassigning staff responsibilities for greater efficiency, and the importance of providing active support for participating centers.
Two Japanese studies focused on teledermatopathology and telecytopathology. The teledermatopathology study (n = 36) investigated the performance of a consultation system using VSs.103 The authors described the convenience of this system: “The quickest diagnosis was received only 18 minutes after sending our data,” and “…no major problems relating to the diagnosis.” Only minor differences of opinion were encountered. The telecytopathology study (n = 53) evaluated the consistency of ruling out high-grade squamous cell intraepithelial lesions in uterine cervical cancer.104 VSs were presented on a Web site: 42 sampled by brush and 11 by cotton swab scraping. Diagnosis on the Web was low: 29.2% for brush scraped and 26.2% for cotton swab. Consistency was also low, 22.4%. “Three-dimensionality, coarse chromatin and irregular nuclei were significantly different between high-grade squamous intraepithelial lesions and benign cancer.” The authors suggested that sharing information online may increase interobserver consistency and also “…avoid geographical and temporal limitations.” The accuracy of diagnosing breast lymph nodes by telepathology was evaluated in an Australian study (quasi-experiment: experimental group, n = 52, control group, n = 239).105 The study was based on a nonequivalent control group design without randomization. As indicators of accuracy, FPs and FNs were computed, and FNs for the experimental and control groups were 11.5% and 10.04% respectively. The missed cases were mostly micrometastases and isolated tumor cells. Overall, “…the accuracy of remote FS was equivalent to that of in-house FS (88.5% versus 89.9%).”
Diagnostic accuracy of VM for GI tract neoplasia was compared with that for CLM in a U.K. study (comparative analysis, n = 61).106 Here again, “…there was substantial reliability of diagnostic agreement (κ = 0.712) scoring the 61 biopsies and moderate agreement scoring the subgroup of 33 positive biopsies with both conventional microscopy (κ = 0.598) and virtual microscopy (κ = 0.436). Interobserver diagnostic agreement between two pathologists by virtual microscopy was substantial (κ = 0.76). Comparison of panel consensus neoplasia scores between conventional and virtual microscopy was almost perfect (κ = 0.877).” This level of agreement is especially important in this challenging area of diagnostic practice.
From The Netherlands, another study (n = 100) investigated the feasibility of WSI for diagnosing GI tract pathology.107 The study cases were diagnosed a year earlier using CLM and rediagnosed using WSI. The results were concordant in 95% of the cases.
The feasibility of telecytology was investigated in East Africa (n = 40) using a static imaging system.108 Diagnostic agreement among six pathologists ranged from 71% to 93%, and was higher among those with more experience. “Reasons for discordance include, poor image quality, presence of diagnostic cells in thick areas of smears, sampling bias and screening error.” Nonetheless, accuracy rates for individual pathologists ranged from 65% to 88%.
Finally, in 2012, a multinational consortium (Italy, France, Japan, Ireland, Switzerland, the United Kingdom, France, and the United States) investigated diagnostic reliability of TB in colorectal cancer using VM.109 Five methods evaluated diagnostic reproducibility among the investigators. The researchers concluded that there was “…an overall fair level of diagnostic agreement for tumor budding (TB) and colorectal cancer, which was improved significantly among experienced GI pathology observers and, above all, in early cancer.”
In 2013, six studies met the selection criteria: three from the United States and one each from Cambodia, Turkey, and Canada. The first U.S. study was an evaluation (prospective analysis, no randomization, n = 67) of the feasibility of FNA for the remote diagnosis of thyroid nodules.110 A single provider aspirated 92 nodules in 67 patients. The digitized images were captured and transmitted over the Internet. “The unsatisfactory sample rate in the transmitted group was 13% (6 out of 45) and that of the non-transmitted group was 23% (11 out of 47). The results indicated that “preliminary onsite telecytopathology was highly accurate when compared to final diagnosis.”
The second U.S. study (n = 25) evaluated the reliability of WSI for renal allograft biopsies.111 Diagnostic reliability was assessed by comparing WSI with conventional GSs in terms of morphological features (form and structure) and diagnostic categories. Substantial agreement was observed in the two modalities for both morphological features and diagnostic categories (κ = 0.68 and 0.74, respectively). “These data indicate that WSIs are as reliable as glass slides for the evaluation of renal allograft biopsies.”
The third was a small pilot study (n = 11) that investigated the accuracy and efficiency of WSI compared with GSs in diagnosing cervicovaginal cytology.112 The results indicated higher accuracy and shorter average time per case with GSs compared with WSI. However, diagnostic accuracy and interpretation time were better when the digital images had higher resolution ( × 40).
From Cambodia, a study investigated the effectiveness of a hybrid system in a telepathology network using store-and-forward and videoconferencing.113 Initially, there were 115 pediatric patients in the histopathology group: 38 were referred to telemedicine consultation. It took an average of 5 days to complete the consultation process (range 0–15). An average of six cases was discussed at each videoconference. “All 38 cases had a final agreed diagnosis, and firm management plans were made. Of the 24 cases where proactive management was advised, 17 patients followed through with the recommendations.”
A Turkish study (n = 17) assessed discrepancies in diagnosing salivary gland tumors by telepathology.114 Tumors were categorized as malignant or benign, and either showing or not showing myoepithelial differentiation. Agreement on malignancy and myoepithelial differentiation was 81% and 86%, respectively. Agreement on benign diagnosis was 70%, with the highest percentage observed on basal cell adenoma (91%). The authors concluded that telepathology “may be used to obtain second opinion about salivary gland tumors.”
A survey (n = 157, response rate = 17%) of pathologists was conducted among members of the Canadian Association of Pathologists to determine current experiences and attitudes toward digital pathology.115 Among those who responded, 43% of their institutions had used telepathology, and 91% thought that “informatics should be part of residency training.” However, these findings are not generalizable in view of low response rate.
Five studies met the selection criteria in 2014: one each from the United States, Canada, Ireland, Iran, and the United Kingdom The U.S. study was focused on human factors in telepathology.116 Surgical pathology report reviews and telepathology service logs for 1,862 consecutive telepathology QA cases were audited. These accrued in a single rural hospital over 51 months. Ten subspecialty university-based telepathologists handled all incoming cases. About 91% of cases were immediately signed out and 9.13% were deferred. Case concurrence with the provisional surgical pathology diagnosis of the referring pathologist averaged 94.3% (range 88.46–100%). Deferral rates ranged from 4.79% to 21.26%. Differences in concordance and deferral rates were significant, but did not correlate with years of experience in pathology practice. Subspecialty surgical pathologists effectively served as general surgical pathologists on a telepathology-based surgical pathology QA service.
A Canadian study (n = 104) evaluated diagnostic concordance and turnaround times of telepathology IOCs in Eastern Quebec.117 Of 104 cases, 8 were slightly discrepant because of differences in terminology and 2 were significantly discrepant. Hence, “…98.1% of the diagnoses were either concordant or had no clinically significant discrepancies.” Average turnaround time was 20 min (range of 8–43): 68% were signed out within 24 h and 85.1% within 72 h. The study concluded that “The Eastern Quebec Telepathology Network allows a rapid, high-quality IOC service to be maintained for a hospital where no pathologist was available on site.”
From Ireland, a pilot study (n = 100) had a dual purpose: (1) to determine the accuracy of WSI in broad range of histopathology cases and (2) to ascertain the acceptability of digital histopatholgy.118 Concordance between original CLM diagnosis and WSI was observed in 95% of the cases. The remaining 5% had slight discordance, but were not clinically significant. The participants had “mixed experiences using digital pathology technology.”
Diagnoses from WSI rendered by remote expert consultants were assessed for 42 cases of patients with atypical small acinar proliferations of the prostate in Iran.119 Despite some loss of information from immunohistochemistry (IHC) staining, “there was high concordance between the results of IHC and electronic consultation in the group of benign cases.” Among the seven cases diagnosed as having malignancy by the consultant pathologist, five were classified as malignant, one as benign, and one as inconclusive. The authors concluded that “This approach can be used as an adjunct to other diagnostic activities like IHC or even as an independent source of information to reach more accurate diagnoses in [atypical small acinar proliferations] ASAP cases, particularly in institutions with limited resources.”
From the United Kingdom, a small study (n = 12) evaluated the feasibility of using VSs in the diagnosis of major cancer resection specimen to improve efficiency in surgical pathology.120 VM was used for real-time rendering of diagnoses. “Total time taken and diagnostic confidence were similar for the microscope and the virtual microscope, as was the mean slide viewing time.” Moreover, it was expected that further practice would improve diagnostic efficiency in VM.
Six studies met the selection criteria in 2015: four from the United States and one each from Canada and Columbia. We start this section with the four U.S. studies.
The first was an evaluation (n = 103) of the utility of telepathology for IOC in the diagnosis of lung neoplasms, where an expert pathologist was not available onsite.121 In this case, the nearest pathologist was 2 miles away. Telepathology consultations were conducted live through video streaming. The consultant was provided access to relevant clinical information about the patient in addition to the images. “There was an agreement between the thoracic pathologist diagnosis and the final diagnosis in 98% of total cases including 8/9 (88.9%) of the total discordant cases.” Moreover, none of the discordant diagnoses were clinically significant.
A prospective nonrandomized trial (n = 46) examined the performance of a telecytopathology system in terms of operative time for EBUS-FNA in diagnosing mediastinal lymphadenopathy.122 Specimens were initially diagnosed in a pathology laboratory and subsequently by remote cytology. Lung cancer was the most common malignancy. “There was no difference in mean number of lymph node stations sampled (1.3 telecytology vs. 0.76 control).” However, telecytology was associated “…with fewer needle passes, fewer slides for interpretation, and shorter time to result confirmation.”
Another test of the reliability of telecytology was conducted in a small study (n = 10).123 Six pathologists initially diagnosed 10 FNAs by CLM and, after at least 6 weeks, by telepathology. The average concordance was 96.7% for interpathologists and 95% for intrapathologist. “All participants passed the assessment with a rate of 90% or better, proving evidence of competency.” The authors concluded that “…telepathology provides increased efficiency for the pathologists by allowing increased time for sign-out, administration, or academic pursuits.”
The use of a smartphone fitted with a 3D printed adapter was evaluated for diagnostic adequacy at the AFIP.124 “Nine pathologists worldwide evaluated the images for quality, adequacy for telepathology consultation, and confidence rendering a diagnosis based on the imaged viewed on the web.” In total, there were 45 reviews, but videos were reviewed in only 30 cases, as some could not be opened. There was a strong correlation between image quality and confidence in diagnosis (r = 0.78) and between image quality and adequacy of image (r = 0.73). “Accuracy was weakly correlated to both quality (r = 0.17) and adequacy of images (n = 0.19). No correlations were found between video and confidence, referring and accuracy, and video and accuracy.” It was concluded that “smartphones allow pathologists and other image dependent disciplines in low resource areas to transmit consultations to experts anywhere in the world.”
The Canadian study (n = 100) evaluated the performance of a dynamic telepathology system in the diagnosis of peripheral abnormalities (23 different hematologic diseases).125 Correct interpretations of morphological abnormalities were observed in 98.81% (83/84) of hematologic diseases and 100% of reactive/normal conditions (12/12). When static images were used, these rates declined, hence, it was concluded that dynamic telepathology was superior.
From Columbia, a study (n = 20) evaluated the performance of VM from mobile platforms.126 Two expert pathologists successfully reviewed 20 VSs on mobile platforms. The important findings from this research point to the importance of a smart decoding strategy, flexible data management, and an architecture that adapts to device resources and network bandwidth.
It should be pointed out that this review of the literature on telepathology included only the first 6 months of 2016. During this period, five studies met the selection criteria: two from the United States and one each from Canada, Italy–the United Kingdom, and Singapore.
The first U.S. study (n = 20) evaluated the performance of panoramic WSI for diagnosing genitourinary surgical pathology versus CLM.127 In addition, this study demonstrated the unique advantages of telepathology for IOC in terms of “…the ability to obtain a distant expert pathologist's opinion in a timely manner,” while also allowing archiving of scanned images. “The diagnostic concordance with glass slides was 98.3% for panoramic images and 100% for WSI. Panoptic images were comparable to the glass slide viewing experience in terms of image quality and diagnostic confidence.” The authors concluded that panoramic digital images were “…a novel tool that can be used for frozen section telepathology.” In addition, they were easy to make especially for small size files. However, they were operator dependent because the individual creating the files can affect final diagnosis.
The second U.S. study (n = 50) investigated the adequacy of FNA in telecytology using mobile video streaming (FaceTime).128 The study had two phases: Phase 1 was a retrospective assessment of 25 samples by a pathologist in-person and a second pathologist by video streaming, Phase 2 was a prospective assessment also by on-site and remote pathologists. Phase 1 had 88% (22 of 25 cases) agreement and 12% (3 cases) disagreement. Two of the three cases were diagnosed as inadequate on FaceTime and adequate onsite. In Phase 2, the corresponding percentage was 85% agreement.
The Canadian study (survey, n = 45: 34 clinicians and 11 managers) assessed the benefits of a large decentralized telepathology network in eastern Quebec.129 The network included 18 hospitals, “…one of the largest telepathology networks in the world.” The primary goals of the network were to improve speed and quality of surgical services in remote areas, as well as avoid unnecessary transfers of patients to urban centers and facilitate recruitment and retention of surgeons in remote regions. “As of January 2015, in total, 1,733 IOCs have been performed.” The authors concluded that “…the deployment of the telepathology project in Eastern Quebec has helped to ensure continuous coverage of IOCs in remote hospitals that do not have a pathologist on site, and consequently, prevent service disruptions.” Also, “from an organizational perspective, telepathology has contributed, at least to some extent, to the recruitment and retention of surgeons in remote regions.”
The safety and suitability of digital reporting of WSI were evaluated for quality in preimplantation renal biopsies in Italy.130 The sample consisted of 62 consecutive prereported kidney biopsies that were subsequently digitized and reassessed by two pathologists using the opposite mode after 2 weeks. Intraobserver concordance was high for both pathologists (κ = 0.84–0.97). “The overall scores obtained by both pathologists and using both methods were identical.” The times required to assess the biopsies were 14 min using CLM, and 18 min using VM (including scanning time). The study concluded that VM was reliable, fast, and safe.
Finally, from Singapore, digital pathology in an academic medical center was described.131 In addition to this report, results from an investigation of diagnostic concordance of telepathology with CLM were provided. Based on 83 cases, concordance between GSs and telepathology ranged from 93% to 100%. Overall concordance was 96%.
Intermediate Effects and Health Outcomes
This section focusses on findings from studies that investigated the intermediate effects and health outcomes of telepathology, with special emphasis on diagnostic accuracy and reliability of telepathology in various forms and applications.
We identified 57 studies from 19 countries that investigated the intermediate effects and health outcomes of telepathology. Because very few studies investigated health outcomes or cost, we included in this section findings pertaining to intermediate outcomes, health outcomes, and cost, as long as they met the selection criteria in terms of empirical studies and minimal sample size of 150 cases. However, although we set out to limit our review to studies with samples of 150 cases or more, there were several studies with samples somewhat less than 150 cases that had worthwhile or significant findings. Hence, we relaxed the sample size rule somewhat, and included studies that had samples of 120 or more cases.
The typical methodology in these studies consisted of comparisons between various applications and modalities of telepathology and CLM. The typical outcome measures in most studies were diagnostic accuracy and reliability as applied to cytology, histology, cancer detection, and neuropathology. A few studies included measures of processing and response time as indicators of efficiency and access.
Two studies met the selection criteria in 2005: one each from the United States and the United Kingdom. The U.S. study (n = 524) was based on 3-year experience with telepathology in diagnosing excisional and aspirate biopsies of breast lesions.132 A dynamic telepathology system was used to assess 315 biopsies and 209 FNAs, all submitted by surgeons who lived about 20 km away. The findings were reported in terms of gross and microscopic telepathology diagnoses compared with final microscopic diagnoses. For FSs, sensitivity, specificity, and accuracy of telepathology were 81.6%, 100%, and 94%, respectively. For malignant tumors, the positive and negative predictive values of telepathology were 100% and 94%, respectively. For FNAs, telepathology agreed with conventional cytology in 78% of the cases. This long-term study demonstrated that “…routine use of telepathology compares well with conventional microscopy in the assessment of both frozen sections and fine need aspirates of breast lesions.”
The U.K. study (survey, n = 166) investigated the reliability of VSs in assessing hematologic morphology.133 A total of 166 participants were involved in this study, and “…substantial concordance of observations made using the slides with those reported in previous glass slide surveys that used identical cases.” When queried about their experience with telepathology, 92% of the participants found the navigation easy; as also, 82% and 76% found image size and field size adequate. However, when assessing for the malaria parasite, only 51% found field size adequate.
Five studies met the selection criteria in 2006: two each from Austria and the United States and one from Switzerland.
The first Austrian study (record review, n = 343) reported on a 4-year experience (2002–2005) with teleneuropathology for intraoperative FS diagnosis.134 The remote neuropathologist was able to control the robotic microscope and communicate through a hands-free telephone. The main challenge was the combination of cytological and histological examinations on a robotic microscope. Average time for diagnosis was 26.1 min, but 83% of the cases were diagnosed in 15–40 min. “Telemicroscopy of a smear slide took 16 times longer than with light microscopy.” The authors indicated that this application of telepathology is worthwhile when the time between the operating area and the diagnosing pathology is more than 15 min. Technical problems were encountered in 6% of the cases. Nonetheless, system reliability was 100%. “After eliminating sampling errors (i.e., cases with no diagnostic material in the frozen section slides and/or in smear preparations), the diagnostic accuracy for telepathology was 97.9%.” Hence, the system “proved to be reliable for intraoperative frozen section.”
The second Austrian study (case control, n = 560) focused on diagnostic accuracy of digital histopathological images, using a robotic microscope.135 Images were reviewed by four dermatopathologists. Telepathology diagnosis was concordant with original diagnosis in 90.4–96% of cases. Median time was 22 s, significantly higher for melanomas than for nevi. These findings demonstrated that digital histopathology was possible, and transmission over ISDN lines offered compression that did not impact diagnoses. “Our results confirm that the assignment of telepathology represents a valuable method for quality assurance in dermatopathology.”
The variability in the diagnosis of dysplasia (“…the enlargement of an organ or tissue by the proliferation of cells of an abnormal type, as a developmental disorder or an early stage in the development of cancer” often requiring expert consultation) with dynamic telepathology was investigated in a collaborative German–U.S. study (comparative analysis, n = 152).136 Interobserver agreement was low (κ = 0.32) among the seven participating pathologists “…after analysis of the cases by dynamic telepathology.” The lowest level of agreement was observed in the indefinite and low-grade dysplasia, whereas the highest agreement was in the negative and high-grade dysplasia. Grouping high and low grades did not affect the level of agreement. In other words, the use of dynamic telepathology in the diagnosis of dysplasia was associated with a poor level of interobserver agreement, but this did not differ from diagnosis obtained by CLM. The authors suggested that “more specific criteria are needed in the general categorization of dysplasia” in chronic ulcerative colitis.
Another U.S. study (survey, n = 202) investigated exposure to intrapathology decision-making among surgical residents.137 “Most residents (78%) reported that they have been exposed to FS surgical pathology (≤10% of the time).” This rate increased to 80% in telepathology, but the difference is not statistically significant.
From Switzerland, an online quiz on urinary cytology was used to test the performance of 246 international participants.138 The quiz included 42 urinary specimens with equivocal morphological features and 10 control cases with definite cytological diagnosis. “High-grade cancers were diagnosed correctly in 76%, and low-grade cancers in only 33.9%.” More than one-half (54.5%) of the participants misclassified decoy cells as malignant, but no further explanation was given. Overall, this study revealed that rendering a diagnosis by viewing static images is not equivalent to making a diagnosis using CLM.
In 2007, four studies met the selection criteria: two from the United States and one each from China and India. The first study from the United States was based on a 5-year database (n = 1,629) from two hospitals separated by 18 city blocks that provided remote intraoperative neuropathological consultations.139 Of this large set of consultations, 1,227 were conducted by conventional microscopy, and only 42 by telemicroscopy. “Discrepancy rates for conventionally diagnosed intra-operative cases varied from as high as 5.8% in 2004 to as low as 2.4% in 2005,” and it remained at that low level in 2006. Overall, concordance between conventional and telemicroscopy ranged from 85% to 87%. It averaged about 81% in telepathology when discrepancies and inexact intraoperative diagnoses were compared. Deferral rates for conventional consultations were stable between 2002 and 2006, with an average of 10.6%, whereas deferral rates for telepathology were significantly higher, at an average of 19.7%. Of the 66 deferred telepathology cases, 64% proved to be correct in the final diagnosis. Of the CLM cases, 67% proved to be ultimately correct in the final diagnosis. In addition, the authors pointed out that remote consultations require sophisticated technology with substantial planning, communication, and training.
The second U.S. study (n = 103, with participants from 23 countries) investigated current international practices regarding visceral pleural invasion to identify relevant histological features.140 This was done through an online quiz on 15 nonsmall cell lung carcinomas. Of these participants, 84.5% were in academic practice, and 42.7% had a subspecialty interest in pulmonary pathology. Interobserver agreement ranged widely from 36.9% to 93.2% (κ = 0.35). Nonetheless, the authors concluded that “…the formation of internationally recognized guidelines for assessing visceral pleural invasion by non-small cell lung carcinomas is likely to improve diagnostic consensus.”
The Chinese study (RCT, n = 400) investigated the accuracy and feasibility of VSs in surgical pathology.141 Two pathologists participated. Diagnostic accuracies of CLM and VSs were 97.25% and 95.5% for pathologist A and 96.25% and 94.75% for pathologist B. There were no statistically significant diagnostic discrepancies. Times for VSs ranged from 3.4 to 5.2 min, and those for CLM ranged from 1.6 to 3.35 min. The authors concluded that VSs enabled “…an acceptable diagnostic accuracy that is of practical value and may be suitable for application in China.”
The Indian study (n = 346) analyzed deferral reasons in a static telepathology consultation service.142 GSs and paraffin blocks were reviewed at a later date by telepathology and results were compared with the initial diagnoses. Of a subset of 251 teleconsults, diagnosis was rendered in 205 cases, and 46 were deferred. Reasons for deferral included need for ancillary studies (40 cases), need for clinical details (5 cases), and poor quality image (1 case). Overall, the “probable” diagnosis matched the final diagnosis in 47% of the cases.
In 2008, two studies met the selection criteria: one from the United States and one from a China–U.S. collaborative. The U.S. study was a retrospective review of 191 gynecological cytology slides viewed remotely through the Internet.143 The images were reviewed by three cytotechnologists and three cytopathologists. Results were expressed in terms of whether the images were “satisfactory/unsatisfactory” for evaluation and whether the diagnosis was negative or malignant for intraepithelial lesions. Two or more reviewers agreed on “unsatisfactory for evaluation” in 89% of the cases and “abnormal” in 83%. “This procedure may have comparable sensitivity and specificity and possibly could provide effective initial triage to further evaluation. A review of individual cases suggests that further accuracy can be achieved with additional training and experience.”
The Chinese–U.S. study (n = 600) assessed the diagnostic accuracy and feasibility of dynamic telepathology.144 The test cases included a wide variety of lesions from 16 organ systems. The cases were initially examined by telepathology by four pathologists, and subsequently reviewed by the same pathologists using CLM. The correct diagnosis was based on the consensus of two experienced pathologists. Diagnostic accuracy of telepathology was 94.8% (pathologist A), 93.3% (pathologist B), 91.6% (pathologist C), and 97% (pathologist D) for the four pathologists. The majority of cases were diagnosed in 15–40 min by telepathology, with an average of 17 min. “The time needed to review a slide by telepathology was 3 to 4 times longer than that of standard light microscopy.” Nonetheless, the authors concluded that “…robotic technology is sufficiently accurate for primary diagnosis in all cases. Our results showed that robotic telepathology is sufficiently accurate for primary diagnosis in surgical pathology, but modifications in laboratory protocols, technology hardware, and Internet speeds are needed to reduce the time necessary for diagnosis by telepathology before this method may be deemed suitable for use in a busy practice.”
In 2009, seven studies met the selection criteria: four from the United States and one each from Canada, Germany, and Poland. The first U.S. study investigated the accuracy of telepathology using VSs in QA program at an academic teaching hospital.43 The sample consisted of 329 consecutive QA cases, which were rereviewed to ascertain the incidence of diagnostic discrepancies. Diagnostic concordance was 91.8% and only 1.5% represented major discrepancies. Another 1.8% were deferred for additional testing. In addition, the implementation of VS telepathology improved clinician job satisfaction.
The second U.S. study (n = 1,321) was conducted over a 7-year period.145 It compared neuropathological intraoperative telepathology consultations versus protocol-driven conventional IOCs. The overall concordance between the two modalities was high for the majority of diagnostic classes. However, concordance for nonneoplastic/reactive lesions was lower in telepathology. Some diagnostic classes were relatively uncommon in telepathology. Overall, “…about 70–72% of intra-operative diagnoses by conventional light microscopy were exactly concordant with the final diagnosis.” The authors concluded that progress in telepathology has now made it feasible to handle challenging intraoperative diagnoses remotely, and for the less common pathological cases, remote consultations improved diagnosis, thereby, supporting the use of telepathology for intraoperative diagnoses. At the same time, they suggested that differences in surgical procedures and types of cases must be considered.
The third U.S. study (n = 11,553), conducted at the Veterans Health Administration, was implemented in three phases over a 12-year period.146 The remote site did not have a pathologist. Instead, a pathology assistant was responsible for tissue grossing and sectioning, as well as referral of cases to the remote pathologist. He placed the slides under a remotely controlled robotic microscope. “The major discordance rates in Phases I, II, and III were 0.33%, 0.45%, and 0.20%, respectively with an overall rate of 0.35%.” Deferral rates ranged from 2.5% to 28.8%, and the differences were statistically significant. Overall, no relationship was observed between deferral rates and discordance rates, and remote site clinicians were satisfied with the quality of the service provided by offsite pathologists.
The fourth U.S. study evaluated telepathology for rapid breast cancer detection in an academic setting (n = 154).34 Telepathology was used for prompt QA readouts at the academic medical center. Concurrence with the primary diagnosis was observed in 90.3% of cases; 2.3% had major discrepancies and 1.9% had minor discrepancies. The authors concluded that telepathology encountered only a small number of significant diagnostic discrepancies. In addition, it increased job satisfaction among specialty pathologists who did not have special training in breast pathology.
From Canada, an analysis of diagnostic accuracy (n = 790) of primary FS diagnosis by robotic microscopy was compared with that of VS telepathology within a heath network consisting of three academic institutions.31 Typically, FSs were submitted by neurosurgeons to confirm the presence of lesions and establish a tissue diagnosis. Initially, 350 primary FSs diagnoses were made by robotic microscopy, followed by 633 VSs. Of 983 FSs from 790 patients, 88% were single specimens with turnaround times averaging between 15.68 and 19.98 min per case. Pathologists required an average of 9.65 min to review a slide by robotic microscopy. This decreased to 2.25 min after the change to VSs. “Diagnostic accuracy has been 98% with both modalities, and our overall deferral rate has been 7.7%.” Typically, discordant diagnoses consisted of minor interpretative errors in telepathology. The authors concluded that the superior speed and equivalent quality of VS telepathology proved to be helpful in consultations with colleagues, especially in difficult cases. Moreover, the availability of the service contributed to overall pathologist satisfaction.
From Germany, a study (n = 257) evaluated the integration and acceleration of VM into the routine diagnostic process.147 This evaluation was based on a review of the files available on the Web server to reconstruct the movements of the pathologist reviewing the slides. “Tests demonstrated that 95% of diagnostic paths could be located without any deletion of entries in the cache (cache size = 12.2 megapixels). If the image parts are stored after JPEG compression this complies with less than 2 MB.”
From Poland, the use of VSs and dynamic telepathology was evaluated for intraoperative diagnosis in thoracic/pulmonary pathology (n = 304).148 The primary diagnosis was based on (1) FSs of lung tumors, bronchial margins, and lymph nodes, (2) FNA, (3) oligo biopsies of bronchus, esophagus, and skin, and (4) exfoliate cytology. Diagnostic concordance between telepathology and CLM ranged between 87.5% and 100%. “For the frozen sections, the primary telediagnoses were concordant with the light microscopy paraffin section diagnoses in 100% for Aperio; and in 97.5% for Coolscope. An excellent agreement (100%) was seen in the telediagnoses and conventional slide diagnoses for FNA, oligo biopsies, and cytology—in both telepathology systems. These results provide some encouragement for the implementation of Coolscope and virtual slide-based telepathology (Aperio) system to the routine histopathological diagnostics.”
In 2010, three studies met the selection criteria: one each from the United States, Republic of Georgia, and Italy. The U.S. study (comparative analysis, n = 792) evaluated telecytopathology of FNA.149 Dynamic images of cytology smears were captured and processed using a digital camera and transmitted through Ethernet. A total of 429 telecytopathology cases were compared with 363 conventional cases, including specimens from the pancreas, GI tract, liver, and lymph nodes. Telepathology was adequate in 94% of cases and conventional on-site review was adequate in 97.7% of cases. Preliminary diagnoses measured as “unsatisfactory, adequate, negative/benign, atypical, neoplasm, suspicious, and positive for malignancy” were 6.3%, 13.5%, 14.9%, 17.9%, 7.2%, 8.6%, and 31.5% for telecytopathology. The results for conventional cases were 3.9%, 30.6%, 21.5%, 9.6%, 5.0%, 5.2%, and 24.2%. The authors concluded that FNA through telepathology provides adequate and accurate preliminary diagnosis compared with the conventional method. Moreover, pathologists can use their time more efficiently and deliver evaluations at remote sites.
The Republic of Georgia study (n = 420) evaluated the effectiveness of digital images for telecytology diagnosis.150 Four cytologists provided diagnoses using digital images. “There was 94% concordance in average between routine versus digital images diagnostic. Intra-cytologists concordance averaged 95.5%. Image sharpness and quality were rated ‘good’ and ‘excellent’ in 97% [of] cases.” Accordingly, the quality of digital images for cytological diagnosis was deemed to be of adequate quality.
From Italy, a study (n = 457) evaluated the accuracy of VM in terms of reliability and diagnostic concordance in colorectal cancer screening.151 The study cases consisted of consecutive lesions detected during colonoscopy. VM increased interobserver agreement over traditional microscopy (κ = 0.66 vs. 0.52). Hence, VM was demonstrated as an effective tool for diagnosis of colorectal cancer.
In 2011, six studies met the selection criteria: three from the United States and one each from Greece, Zambia, and Brazil. The first U.S. study (n = 1,229) was a comprehensive analysis of a Web-based dermatopathology second opinion consultation practice.152 It was focused on analyzing the needs for and performance of this program. The findings indicate shorter turn-around time from biopsy to report: 82% of cases were reported on the same day and 82% of consultations were concerned with melanocytic lesions, inflammatory dermatoses, and squamous lesions. The remaining cases were mostly soft tissue tumors, adnexal neoplasms, alopecia, and other lesions. In 69% of cases, the consultant report contained information favored by the submitting pathologists. Hence, it was concluded that “…Web-based communication facilitates rapid turn-around time and reduces costs and barriers to second opinion consultation.”
The second U.S. study (n = 606) examined novel anatomic pathology techniques that allow pathologists to view and diagnose cases digitally.153 The results indicated a high level of intrapathologist diagnostic consistency between GSs and VSs. There were no discrepancies between the two modalities in 75%, 87%, and 83% of cases, as reported by the three pathologists. Significant discrepancies were observed in 3%, 3%, and 7%, as reported by the three pathologists.
The third U.S. study (n = 520) compared the reading of immunohistochemical and CLM for estrogen and progesterone receptors.154 Formalin-fixed breast tissue specimens were assayed at three clinical sites. At each site, three pathologists performed a blinded reading of the GSs and later the VSs. Conventional readings were similar to digital; 91.3% versus 99.0%, respectively. Therefore, computer reading of estrogen receptors compared favorably with that of CLM. Interpathologist agreement for VSs and CLM was 91.3–100.0% and 91.3–99.0%, respectively.
From Greece, a study (n = 270) evaluated diagnostic concordance and usefulness of telecytology using VSs from thyroid FNA.155 The specimens were remotely viewed by five cytopathologists. Their reports were recorded and classified. Subsequently, they were transferred in random order to the same cytopathologists for a final reading. There were no significant differences in diagnostic accuracy between initial and subsequent reviews. Interobserver agreement was nearly perfect with κ values of 0.869 and 0.939. Similarly, intraobserver agreement ranged from κ = 0.967 to 1.0
From Zambia, a project (n = 322) investigated the benefits of virtual pathology in a developing country.156 All surgical specimens obtained in one hospital in Zambia were submitted for remote microscopic examination through WSI. Two Italian pathologists evaluated the cases and submitted their diagnoses through the Internet. About 40% of the gynecological samples were human papilloma virus. Of the nongynecological specimens, there was a wide variety of diagnoses, including skin and soft-tissue diseases, infectious diseases, and atypical mycobacterium. The diagnostic accuracy of the virtual system was fairly high. No major changes in diagnosis were made in 12.3% of the cases. Further examination of differences between telepathology and traditional diagnosis revealed only 1 of 12 cervical samples as undifferentiated carcinoma. There were 10 cases of partial disagreement in dermatopathology. “The use of telepathology in a developing nation offered Zambian clinicians the possibility of receiving diagnoses and providing appropriate treatment closer to the standards of Westernized countries. With telepathology, clinicians can be guided to perform appropriate biopsies, conization, and surgical treatment of cervical cancer.”
From Brazil, a study (n = 135) evaluated the concordance between histopathological second-opinion consultations of skin diseases (neoplastic, infectious, and noninfectious) versus CLM using two consultants.157 The first consultant obtained agreement of 88.1%, whereas the second had 80.7%. Interobserver agreement for CLM was 81.5%, and that for microphotography was 85.9%. κ percentage for consultant 1 was 98.6% and that for consultant 2 was 95.8%. The authors concluded that “the evaluation of microphotographs shows a good level of reproducibility when compared to traditional microscopy and, therefore, is a viable option for a second opinion consultation in dermatopathology.”
In 2012, eight studies met the selection criteria:four from the United States and one each from Egypt, Greece, Australia–the United Kingdom, and Hungary. The first U.S. study (n = 251) investigated diagnostic concordance between WSI and CLM for routine surgical pathology.158 The sample consisted of 251 consecutive surgical pathology cases from a single pathology service. All cases were presented to two pathologists in both modalities. Their findings were assessed by a third pathologist. Concordance was 97.7%. Five cases were discordant, two of these were significant. Technical difficulties were encountered in 13% of the cases, and were associated with the inability to observe nuclear detail or microscopic organisms. The authors concluded that these difficulties were the most significant obstacle to the use of WSI in general surgical pathology.
The second U.S. study (n = 250) investigated the impact of color calibration methods of a liquid crystal display on observer performance in virtual pathology.159 One-half of the cases were malignant and one-half were benign. They were shown to six pathologists, once using a dedicated calibration protocol and once on the same display in an uncalibrated state. No statistically significant differences were observed in the two calibration methods in terms of diagnostic accuracy, but the viewing times with the calibrated display were significantly shorter. This is important as clinical use of telepathology and WSI cannot be hindered by slower viewing times if it is going to be accepted and used routinely.
The third U.S. study (n = 240) evaluated telecytology of EUS-FNA compared with conventional on-site evaluation.160 The telecytologists captured the images and transmitted them over the Internet. Subsequently, the cytopathologist accessed the images on a computer and rendered the diagnoses. Two-thirds of the cases used telecytology and 1/3 did not. The average time for both CLM and telecytology evaluations was 1.1 h. The average procedure time for cytopathologists was 0.74 h and that for telecytology was 0.2 h. Hence, telecytology improved system efficiency.
The fourth study (n = 127) examined diagnostic accuracy of telepathology in pediatric malignancies in a low-resource setting.161 The project provides training in pediatric cancer through telepathology to meet the needs for pediatric oncology in developing countries. The diagnostic accuracy of the trainees was compared with that of an experienced pathologist. Subsequently, the effectiveness of static versus dynamic telepathology was compared. The findings indicated an overall concordance of 90.6% between telepathology and original diagnosis, whereas dynamic and static telepathologies were equally effective for diagnostic review. The authors concluded that “brief, focused training in pediatric histopathology can improve diagnostic accuracy.”
From Egypt, a pilot study (n = 250) investigated the merit of applications of WSI for e-education and telepathology.162 As of 2004, four centers were involved in Cairo, Venice, London, and Pittsburg. Consultations focused on difficult cases. “Over eight years we consulted on many problematic pathological cases with specialized pathological centers in Italy, U.K., and U.S. In addition to the highly specialized scientific value, we saved a lot of time and money.” The authors concluded that telepathology was very useful in remote consultations, especially in emerging countries, but this report was not intended as an empirical analysis.
From Greece, a study (n = 404) evaluated the accuracy and reproducibility of telecytological diagnosis for cervical smears.163 Study cases included 135 benign, 92 atypical squamous cells, 62 low-grade squamous epithelial lesions, 26 high-grade squamous intraepithelial lesions, 26 squamous cells, and 2 adenocarcinomas. Digital images were transmitted to four board-certified cytopathologists. After 12 and 24 months, first and second round diagnoses were compared with the original diagnoses. No significant differences were observed in diagnostic accuracy. Overall, interobserver agreement ranged between κ = 0.79 and 0.97, and intraobserver agreement ranged between κ = 0.76 and 1.0 in all diagnostic rounds. Hence, the authors concluded that “digital images of cervical smears can be used for rapid and accurate diagnosis, by diminishing turn-around times and improving small cytology departments' quality indices.”
From Australia and the United Kingdom, a prospective study (n = 316) compared VM with CLM in the assessment of morphological characteristics of breast cancer.164 Thirteen histopathologists from the United Kingdom and Australia assessed multiple morphological features, including tumor grade and type, and comparisons were made between virtual images and GSs. Diagnosis was comparable, especially for vascular invasion, necrosis, and presence of central scar (κ = 0.37–0.78). However, it was poor for subjective interpretations, such as pleomorphism, stroma, tumor border, and degree of lymphocytic infiltrate (κ = 0.1). Hence, the authors concluded that “virtual slides represent an acceptable methodology for central review of breast cancer histopathology and can circumvent the need for either travel to review material, or the potential problems of sending it by post.”
A study of diagnostic accuracy of VSs in routine histopathology was conducted in Hungary using 306 randomly selected cases from a national database.165 Pathologists used their office computers for evaluating VSs transmitted through the Internet. “Good to excellent image quality of slides was recorded in 96%.” Poor image quality was related to section folds. Digital diagnoses were in full agreement with the consensus in 88.2% of the cases. The results demonstrated that VSs compared favorably with CLM; however, the competency of the pathologist was more important than the quality of the digital slides. At the same time, poor VSs quality did not endanger patients' safety because such errors were readily recognizable by the pathologists.
In 2013, five studies met the selection criteria: two each from the United States and The Netherlands, and one was a collaborative study from Italy and the United States. The first U.S. study (n = 200) focused on the performance of dynamic telecytopathology for rapid on-site diagnosis of transbronchial FNA.166 Real-time images of stained cytology smears were obtained with a digital camera and transmitted through Ethernet to a cytopathologist who rendered an initial diagnosis while communicating with an on-site cytologist. Initial results were assessed in terms of “negative/benign, atypical/suspicious, and positive” for malignancy. For telecytopathology, the results were 58%, 14%, and 24%, respectively. The corresponding figures for CLM were 57%, 10%, and 31%, respectively. The concordance between preliminary and final diagnoses was 96% for telecytopathology and 93% for CLM. The reasons for discordant preliminary and final diagnoses were attributed to the difficulty of distinguishing between small-cell carcinoma and reactive lymph node because of an artifact. Accordingly, this research demonstrated that telecytopathology was comparable with CLM.
The second U.S. study (n = 500) compared cervical histopathology using VSs versus GSs.167 Pathologists' evaluations of GSs and the corresponding VSs were compared in a state-wide surveillance program of cervical cancer in New Mexico. The distribution of cases included 70% cervical intraepithelial neoplasia grade 2 or higher, 20% grade 1, and 10% negative cases. Three pathologists read the slides two or three times each, but without access to medical history or previous readings. Overall, within-reader and between-reader κ values were between 0.7 and 0.8 and between 0.6 and 0.7, respectively. “For the discrepant set, most within- and between-reader κ values were 0.4 to 0.6.” Overall, diagnosis of cervical intraepithelial neoplasia did not differ.
An evaluation (n = 628) of the benefits of intraoperative FSs analysis of sentinel lymph nodes in breast cancer was conducted in The Netherlands.168 This type of analysis “allows for immediate axillary (or armpit) lymph node dissection (ALND) in cases of metastatic disease in patients with breast cancer,” which can reduce the FN rate in intraoperative diagnosis. Data for 628 patients over a 4-year period were retrospectively analyzed to ascertain metastatic disease. FSs analysis predicted axillary status in 83.6% of cases. True positive findings were 12.4%, FPs were 0.3%, and FNs were 16.1%. Hence, FS findings were associated with a high FN rate, and the use of telepathology increased this rate. “Only 12.4% of the patients benefited from intraoperative FS, as secondary ALND could be avoided, so FS may be indicated for a selected group of patients.”
Also from The Netherlands, two related telepathology studies investigated the feasibility and reliability of telepathology in organ transplantation involving liver and pancreas grafts.169 For liver graft, 130 cases simulated remote image examinations and assessed sensitivity and specificity. The results showed “injuries (sensitivity = 96%), injuries of the capsula (sensitivity of 91.7%), hematomas (sensitivity = 91.7%), non neoplasmatic diseases (specificity = 100%), tumors (sensitivity = 100%).” A second study used the same methodology for evaluating pancreatic grafts. This analysis had the following results: “Injuries (sensitivity = 100%), injuries of the capsula (sensitivity = 84.6%), hematomas (sensitivity = 92.3%), non-neoplasmatic diseases (specificity = 92.3%), tumors (specificity = 72%).”
Finally, a collaborative U.S.–Italian study (n = 334) compared bedside diagnostic accuracy and distant reader of reflectance confocal microscopy (RCM) for observation of cellular detail without biopsy.170 RCM images were evaluated by two readers, one onsite and the other at a distance. Sensitivity was greater than 90%, and specificity was greater than 60% for both readers. The combined sensitivity was 98% and combined specificity was 44%. RCM provided high diagnostic accuracy in teleconsultation. However, the authors pointed out that “RCM may be limited in the correct classification of epithelial tumors.”
There were 12 studies in 2014 that met the selection criteria: 6 from the United States 1 each from a collaborative project between Rwanda and the United States and another collaborative project between China and Canada, and 1 each from Canada, Germany, the United Kingdom, and Brazil. The first U.S. study (n = 335) compared WSI pap smears versus liquid-based thin layer cervical cytology.171 The study focused on detecting organisms and non-neoplastic findings. The authors emphasized that cervical cancer is one of the most prevalent malignancies globally, whereas it is also treatable by screening and early intervention, and now preventable by early vaccination. WSI from pap cell block preparations was analyzed to assess their adequacy in terms of diagnosing bacterial vaginosis, fungi, Trichomonas vaginalis, and herpes simplex virus, and for non-neoplastic findings. “Squamous metaplasia, keratosis and reactive/reparative and inflammatory changes were easily identifiable by WSI.” However, multiple focusing was required because of differences in smear thickness and the presence of overlapping backgrounds. This could be implemented in CLM. Whereas a reviewer (or consultant) would need to rely on the skills of the individual capturing the still images, the problem is obviated with robotic images, which can be controlled remotely. With WSI, the reviewer may be unable to focus on different regions of interest on the slide as already noted in the Z-plane discussion. Results confirmed that evaluation of cell block from pap samples was feasible and of high quality. Merging samples of cell block preparations with digital pathology has strong potential value in overcoming hurdles in the adoption of WSI. Remote consultation eliminated the need for an on-site pathologist/cytotechnologist, as well as provided a time saving platform for improved collaboration and exchange of ideas.
The second U.S. study (n = 300) was focused on validating WSI for primary diagnosis in surgical pathology.172 The system used the validation guidelines commissioned by the College of American Pathologists. Six pathologists rereviewed 300 previously diagnosed specimens, equally divided between GSs and WSI over an 8-month period. A minimum of 3 months was used as the washout period. “The traditional microscopy and WSI discordance rates ranged from 3.3% to 13.3% and from 2.1% to 10.1%, respectively.” Overall, no statistically significant differences were observed among the pathologists, and no differences were observed between WSI and CLM.
The third U.S. study (n = 217) tested intraobserver variability of WSI in cases submitted for surgical pathology consultations by 11 subspecialty groups.173 The images were interpreted by 26 pathologists. Discrepancies between CLM and WSI were identified by independent pathologists. Accordingly, two major and eight minor discrepancies were identified. “One major discrepancy reflected atypical versus non-atypical endometrial hyperplasia; the other related to reactive squamous changes versus carcinoma.” The authors concluded that their study supported the safety and ethics of WSI for surgical pathology diagnosis.
The fourth U.S. study (n = 217) compared the nondiagnostic rate for remote EUS-FNA of pancreatic lesions with on-site evaluation.174 One group of patients had a telecytopathology evaluation and the other did not. Telecytology was provided for 43.8% of the cases. “The non-diagnostic rates for solid lesions in Group 1 and Group 2 were 3.7% and 25.6%, respectively.” The findings indicated that telecytology reduced the nondiagnostic rate, especially in lesions with solid characteristics. “Telecytopathology on-site assessment of EUS-FNA of both solid and cystic lesions of the pancreas yielded lower percentages of nondiagnostic specimens compared with the group that did not undergo any on-site assessment.” However, this trend was statistically significant for solid lesions only. Overall, telecytopathology consultations resulted in significant reductions in the nondiagnostic rate, especially for solid lesions. In addition, telecytopathology improved efficiency and down time over on-site evaluation.
The fifth U.S. study (n = 200) evaluated a novel RT platform for neuropathology intraoperative touch preparations.175 “One intraoperative touch preparation slide from each of 100 cases was examined twice (200 total cases) using glass slides and RT, with a 3-week washout period between findings, on two different scanners at two remote sites.” Of the 200 cases under study, only 1 failed on RT. However, there were 47 interpretive variances. Of these, 4.5% had potentially significant clinical indications. Hence, the study demonstrated that RT was reasonable for providing remote neuropathology consultations for intraoperative interpretations. At the same time, it was limited by the slowness of the robotics, crude focusing, and the difficulty of determining where to examine the slide using thumbnail images.
The sixth U.S. study (n = 298) focused on technology and assessed the importance of image resolution on diagnostic concordance.176 The concordance index was 0.943 for NetCam and 0.951 for iMedHD. No differences were observed in the concordance indexes between preliminary and final diagnosis or in the number of passes necessary to render an adequate diagnosis.
Also in 2014, an assessment of a phased approach to anatomic pathology services was conducted in rural Rwanda (n = 437).177 This was an attempt to introduce anatomic pathology services into a resource-limited setting. Tissue specimens were submitted to remote consultants for their diagnoses. Median time from receipt of specimen to final reporting was 32 days. Among the specimens received, 55.8% were confirmed as malignant, 37.3 as benign, and 6.4 as inconclusive. Less than 1% were not available at the time of analysis. Full implementation of telepathology services, introduced in 2013, was expected to shorten the time for receiving a diagnosis in many centers. In addition, local laboratory technicians were being trained to process the specimens. “This model can serve as a roadmap for the development of pathology laboratory services in other resource-limited settings, which can be a major step forward in the provision of high-quality cancer care to those in need.”
A Canadian study (n = 7,440) reported on a 3-year experience of a telepathology network in eastern Quebec.178 Services included IOCs, expert opinions, urgent analyses, and supervision of macroscopic descriptions. Expert opinions were signed out in 24 h in 68% of cases and within 72 h in 85% of cases. “The study also demonstrated that wider adoption of telepathology would require technological improvement, and that the sustainability of the network requires better coordination and the development of a super-regional pathology organization.” Overall, the network allowed rapid and high-quality pathology services in a very large territory, including more than 20 sites. Plans called for expanding the network to other regions in Quebec.
A nationwide telepathology consultation and quality control program was conducted in China from 2011 to 2013 (n = 16,247).179 Pathology cases included digestive disorders (17.3%), gynecological (16.7%), head and neck (15.7%), bone and soft tissue (10.4%), lung and mediastinum (8.6), breast (7.6%), urinary tract (7.5%) hematology (6.4%), skin (5%), neuropathology (2.5%), and cytopathology (1.3%). In all cases, remote expert consultations were provided, including an assessment of the quality of slide preparation and staining as well as the delivery of lectures on quality control. Agreement between initial diagnosis and expert opinion was observed in 59.8% of the cases, disagreement in 24.2%, and 16% did not have a preliminary diagnosis. After 2 years of implementation, this project demonstrated that telepathology “…could solve the problem of uneven distribution of pathology resources, and to provide a solution for countrywide pathology quality control in China.”
A German study (n = 1,204) evaluated the accuracy of telepathology for intraoperative FS consultation over the course of 2.5 years.180 Tissue assessments were mainly for urological, gynecological, and dermatological resections. Accurate diagnosis was achieved in 98.59% of intraoperative FSs in the initial telepathological consultations, sensitivity of 92.6%, and discrepant diagnosis in only 1.41% as compared with the final diagnosis. The authors concluded that “…the quality of services is highly acceptable and the investment costs and the labor costs of virtual slide technology are lower than those of robotic microscopy.”
A British–Malawi study (n = 197) investigated remote and rapid pathological diagnosis in a resource-constrained setting.181 The results of the first 197 consecutive consultations on patients who used the system were reported. The majority of the samples were FNAs (53%). The remainder consisted of bone marrow aspirates, peripheral blood films, and other fluid collections. A diagnosis was received in 52% of the samples. There were 23.35% discordant results, 19.2% could not make a diagnosis. At least a quarter of the cases resulted in a changed diagnosis and treatment plan. “This simple telepathology initiative has had a positive impact on clinical management, and could be used in other less resourced centres twinned with better resourced ones.”
A moderately large study (n = 2,592) investigated diagnostic accuracy of digital photography in skin cancer screening by mobile units in remote areas of Brazil.182 All digital photographs were transmitted to two oncologists, who evaluated the images and provided a diagnosis (benign or malignant). The actual skin biopsy was used as the gold standard. The absolute agreement rates with visual inspection were 85.8% for oncologist number 1 and 93.5% for oncologist number 2. Overall accuracy of the two oncologists did not differ significantly from each other. Sensitivity and specificity of the two oncologists were 89.3% versus 96.2% and 38.5% versus 25.0%, respectively. Their overall accuracies were 85.3% and 87.3%, respectively.
In 2015, four studies met the selection criteria: two from the United States and one each from combined United States and China, and multinational. The first U.S. study (n = 1,000) evaluated the validity of WSI on the basis of guidelines issued by the College of American Pathologists.183 Cases were selected consecutively from internal consultations and malignancies, and pathologists reviewed both GSs and WSI. Intraobserver agreement was observed in 79% of the cases; major discrepancies were noted in 1.8%. Agreement was especially high in a subset of the cases concerned with neoplasia (n = 504): κ = 0.878. The findings from this analysis “were felt to validate the use of the WSI for the intended applications” in this multi-institutional setting.
The second study was also an evaluation of WSI (n = 130 and 347) compared with GSs in a multi-institutional setting.184 Diagnostic discrepancies were adjudicated to determine a reference (or accurate) diagnosis. During the training period (n = 130), there was 94.6% concordance, whereas minor and major discrepancies were encountered in 4.6% and 0.8% of the cases, respectively. Most discrepancies occurred during the first seven cases diagnosed by the pathologist. During the clinical trial (n = 347), 5.4% had major discrepancies after adjudication, including a gastric antrum biopsy, an abdominal shave biopsy, a skin excision, and a wedge lung biopsy. The case analysis from second-opinion consultations indicated 94.6% where both WSI and GSs were correct, 2.7% where GS was incorrect, and 1.4% where WSI was incorrect. The authors concluded that “…WSI is adequate for inter-institutional second-opinion consultations in surgical pathology.” Moreover, none of the cases in this study involved had an inadequate image for diagnosis that actually led to a discrepancy. Nonetheless, potential issues in interinstitutional image sharing remain to be resolved, including information technology (IT) collaboration, work flow, and technical division of labor.
A U.S.–Chinese study (n = 1,561) reported on 3 years of experience in international telepathology consultation.185 The cases were referred by Chinese pathologists from an independent pathology laboratory to an academic medical center in the United States. Cases included hematopathology (23.7%), bone/soft tissue (21.0%), gynecological/breast (20.2%), and other subspecialties. Average turnaround time was 5.4 days, which decreased from 6.8 to 5.0 days over 2 years. Final diagnoses by the U.S. specialists were identical in 25.6% of the cases, and significantly modified (i.e., required change in treatment plan) in 50.8%. The authors concluded that “…international telepathology consultation can significantly improve patient care…” in host countries.
Finally, an international multicenter interobserver study (n = 351) was conducted to evaluate VM for the study of adrenal tumors involving 10 countries.186 The study ascertained interobserver variability among expert endocrine pathologists using Internet-based VM in a large multicenter pheochromocytomas/paraganglioma cohort. “Substantial agreement among all reviewers was observed either with a two-tiered classification (SDHB κ = 0.7338; SDHA κ = 0.6707) or a three-tiered classification (SDHB κ = 0.6543; SDHB κ = 7516).” SDHB and SDHA are genetic mutations inherited as autosomal dominant traits. The authors concluded that “…SDHB/SDHA immunohistochemistry is a reliable tool to identify patients with SDH-x mutations.”
Summary of Findings
This article reviewed the empirical evidence regarding the feasibility/acceptance and impact of various forms of telepathology as reported in the published literature during the past decade, 2005 to early 2016. We identified a total of 134 studies that met the selection criteria for this review and analysis. Of these, 77 studies were focused on feasibility/acceptance and 57 on intermediate outcomes, namely diagnostic concordance between telepathology and CLM. Intermediate outcomes refer to an interim outcome stage between changes in process and true outcomes. They are important in and of themselves because normally they are correlated with, or are predictive of, health outcomes. They were necessary in this analysis because health outcomes are either not feasible or not readily observable at least in the short run.
Feasibility/acceptance studies were conducted in 27 countries, typically using observational designs and smaller samples. Sample sizes varied from a low of 10 to a high of 1,862, adding up to a total of 6,727 cases and an average of 94. These studies investigated the feasibility of a broad range of telepathology applications, including histopathology, cytopathology, tumor banking, and IOCs. The proliferation of the nomenclature in telepathology (including the use of terms such as telecytology, telehistology, teledermatopathology, VSs, and digital slides) reflects both the growth of this modality of practice in pathology and the wide range of interests among pathologists in using IT in their daily practice. The empirical evidence supports the feasibility/acceptance of a variety of telepathology systems and technologies for numerous clinical and educational applications in a variety of settings both in the United States. and internationally. In addition to this overall trend, several notable findings can be summarized as follows:
• There was more agreement (i.e., diagnostic concordance) in cancer detection for higher grade cancers, and such concordance also varied by type of pathology. Grading of some cancers was only fair.
• The experience of the pathologist in IT proved to be a significant predictor of diagnostic accuracy.
• Higher resolution improved digital interpretations and correlated with diagnostic confidence.
• Pathologists were generally satisfied with telepathology as a modality of service.
The benefits of telepathology can be summarized as follows:
• General diagnostic accuracy, although varied by observer.
• Ready availability of expertise in resource-constrained settings.
• More efficient use of time, improved workflow, and information integration.
• Data sharing worldwide, but diagnostic agreement is not uniform.
• No further need for incisions in Mohs surgery.
• Assist in QA programs, education, and collaboration.
• Enables virtual tumor banking.
A total of 57 studies from 19 countries investigated the intermediate effects of telepathology, mostly in terms of diagnostic concordance between various modalities of remote diagnosis and the traditional mode. Sample size varied from a low of 103 to a high of 16,247, for a total of 29,563 cases and an average of 519. Here again, the majority of studies confirmed high levels of diagnostic accuracy and reliability of various modalities of telepathology as compared with light microscopy. However, some of this evidence was not consistent in terms of hematologic morphology, detection of the malaria parasite, low-grade dysplasia, tumor grade and type, observation of nuclear detail and microscopic organisms, diagnosis of intraepithelial neoplasia, and robotic speed. Overall, the percentage of diagnostic concordance was observed in more than 90% of the cases. The most significant difficulties were encountered in terms of limitations to observe nuclear detail abnormal chromosomes, microorganisms, and complex cytopathology. There was no clear-cut relationship between discordant rates and deferral rates. Reasons for deferrals included the need for additional clinical information and poor quality images. Benefits of telepathology can be summarized as follows:
• Greater efficiency in terms of time for diagnosis and turn-around time, especially where a pathologist is not available onsite. Pathologists can use their time more efficiently and deliver evaluations at remote sites.
• Effective tool for colorectal, breast, and cervical cancer screening, especially in resource-poor settings. In breast cancer, telepathology is good for identifying malignant tumors and evaluating vascular invasion, necrosis, and central scar.
• Additional training and experience can improve diagnostic sensitivity and specificity. Moreover, experience of the pathologist proved to be more important than quality of images in some cases. Diagnostic errors were readily recognizable by the pathologists.
• Telepathology proved to be an effective substitute for having an on-site pathologist, especially in resource-poor settings.
• RCM provided cellular detail, but was still limited in use in the classification of epithelial tumors.
• Safety and ethics of WSI were demonstrated for surgical pathology diagnosis.
• Telepathology can improve cancer care in a large country such as China.
Concluding Comments
One area of concern is pathologists' apparent lack of enthusiasm for performing their work functioning as telepathologists.187–195 Where significant travel can be avoided, the technology sparks some interest.10,11,196 However, this represents a very small fraction of what surgical pathologists do in their everyday practices. The greater test will be to see whether pathologists can, or would be willing to, move into a digital pathology framework for their routine surgical pathology work, functioning as either general pathologists or subspecialty pathologists. A current challenge worldwide is to overcome the perceived cynicism within the pathology community regarding the practicality of telepathology, engendered by equipment costs, poor reimbursement, concerns over diagnostic accuracy and efficiency, and more than a few false starts.
What system developers, and even telepathology proponents, need to appreciate is that surgical pathologists are under great pressure to avoid “sins of omission” when diagnosing surgical pathology cases.197 In U.S. courts, “sins of omission” are incurred if a surgical pathologist fails to examine all of the GSs in a surgical pathology case, or the diagnostic areas on a histopathology slide. Well beyond that, the “sins of omission” concern is embedded in Western culture and is widely regarded as a “sin” of biblical proportions. According to Wikipedia, “…a person may be guilty of a sin of omission if he (or she) fails to do something which he (or she) is able to do and which he (or she) ought to do because he has put himself into a state or situation whereby he is unable to complete the action.”196 Opportunities for “sins of omission” are abound in the performance of WSI telepathology, and they deeply concern surgical pathologists. A fundamental concept taught to pathology residents is to carry out “complete examinations” of every histopathology GS that comes their way. WSI telepathology, without the possibility of Z-stack or Z-plane adjustments, potentially compromises the telepathologists' analysis of a surgical pathology or cytopathology case.
Pathologists fully understand that visual sampling of surgical pathology slides is rarely totally inclusive as a practical matter nor is it necessary. Visual sampling varies from case to case and is dependent on a number of variables. However, for certain types of surgical pathology cases, pathologists are taught to look for visual clues as to where to focus their attention next, and complete their visual sampling of slides to the point of where they can render a surgical pathology or cytopathology report, with confidence of the adequacy, and appropriateness, of their sampling of the specimen. With WSI telepathology, critically important sampling could be hampered by at least two different ways: first, the pathway of the optical plane within the 3D tissue section they might wish to explore is determined by the autofocus mechanism built into the WSI telepathology system, and is not necessarily of the telepathologists' choosing; second, without a Z-stack or Z-plane focusing feature, the telepathologist relinquishes the capability to follow visual clues 360° from every new origination point created during the search process. Pathologists cannot freely explore the tissue section, wherever their curiosity might lead them in the course of their WSI examination.
Pathologists realize that a diagnosis may rest on the identification of even a small cluster of abnormal cells, or other small subtle features. The feature may occupy a small percentage of the volume of the actual tissue section. It may escape notice if the WSI optical section does not intersect with the optical plane sampled to create the WSI. Every surgical pathologist has handled cases where a small malignant focus was detected only after multiple serial sections of a paraffin block were examined carefully by CLM. They have also learned, from experience, that the solidification of diagnostic impressions of tissue can be a cumulative visual process in which visual information from multiple adjacent microscopic fields is sequentially accessioned into their memories by a process involving the continuous searching of tissue sections and mentally linking images together. With WSI telepathology imaging, such a visual search process might be interrupted, and even aborted, either by (1) reaching the upper or lower surface of the thin, optically created, tissue slice image, representing the tissue within the zone, of the thickness of a finite depth of focus, within the rectangle representing the nearly horizontal whole slide image, yet being only a split-thickness of that actual tissue section it represents or (2) by gaps in visual information as the telepathologist jumps from one optical slice to the next, while navigating their way through a stack of discontinuous Z-stacks or Z-planes, mentally jumping through the gaps between the optical slices.
Although the light microscopist's actual sampling of tissue sections is, in reality, intentionally selective, the sense of this being “adequate sampling” comes from navigating through a self-directed visual search process. This visual search process is interrupted repetitively during the WSI telepathology Z-stack or Z-plane examinations, which can be challenging and distracting to even an experienced light microscopist.26 It remains to be seen whether incorporating a robotic microscopy feature into WSI telepathology systems alleviates this barrier to WSI acceptance while moving the curve on telepathology diagnostic accuracy upward. Innovators in telepathology have several challenges. There have been major equipment issues that have encouraged innovation in telepathology system design but side stepped other issues with respect to their possible impact on telepathology diagnostic accuracy.5,23 Innovators have yet to produce a single, standardized digital imaging solution that will meet the requirement to equal or surpass a level of diagnostic accuracy for attainable CLM surgical pathology. The diagnostic accuracy bar is set exceptionally high compared with almost any other medical imaging application. Currently, it requires the employment of expensive technologies that bend the return-on-investment curve in a negative direction.17,26
The issues surrounding the designs and performances of WSI instruments, and issues related to the FDA approval of WSI telepathology for specific uses, are intertwined and complex. The pathway to eventual approval of WSI telepathology for primary diagnosis has seemed convoluted although recent U.S. governmental clarifications52 and the guidelines of professional organizations should be helpful.6,40 Our sense is that there are important unresolved issues that may seem minor to engineers, or even Chief Executive Officers of companies in the medical device industry, but that are not “minor” to many diagnostic pathologists who are being asked to embrace WSI telepathology technology. In this regard, it is relevant to ask, “Can the viewing of WSI adequately substitute for the positive, and even enjoyable, visualization experience of pathologists exploring tissue sections mounted on GSs?” “Are levels of user satisfaction with the two slide imaging modalities nearly equivalent?” “Is the diagnostic information gathered by a pathologist exploring a GS using CLM comparable with the information gathered by a pathologist viewing a WSI at a distance?”17,19 “Does incorporating a robotic telepathology feature into a WSI telepathology scanner level the playing field for CLM-based pathologists and WSI-based pathologists?”23,27 Experience has shown that these fundamental issues cannot be simply wished away by medical imaging companies selling WSI products.38,39 The digital pathology industry needs to be convinced that small incremental differences in diagnostic accuracy really matter in the pathology world.27,29,30
Furthermore, pathology and radiology are not equivalent because many radiology diagnoses are provisional, unlike the vast majority of pathology diagnoses. The diagnostic accuracy expectations are generally higher for pathology than for radiology. Until these challenging issues are addressed and resolved, and a consensus is reached among practicing surgical pathologists and cytopathologists on the suitability of telepathology for routine diagnostic work, widespread use of WSI telepathology may remain, essentially, in limbo in the United States, although not necessarily in the other countries that are further along in adopting telepathology into their everyday laboratory workflow.7,26,70,186 The long range prospects for telepathology may be considerably brighter.11,20,23,27,39
Acknowledgments
The research leading to this publication was supported by the NLM (The National Institutes of Health) in the form of Intergovernmental Personnel Act No. F037249 to R.L.B. Although this support is gratefully acknowledged, responsibility for the accuracy, interpretation, and analysis of materials presented in this article are the sole responsibility of the authors. We wish to thank Bruce Friedman, MD, for reading the article and offering important suggestions, and Carol Shannon, MPH, for helping us with the literature search and the organization of the citations.
Disclaimer
The authors of this article are responsible for the literature selection, analysis, accuracy, and interpretation of the data presented in this article.
Disclosure Statement
No competing financial interests exist.
References
- 1.Bashshur RL, Krupinski EA, Thrall JH, Bashshur N. The empirical foundations of teleradiology and related applications: A review of the evidence. Telemed J E Health 2016;22:868–898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Inoué S, Spring KR. Video microscopy: The fundamentals. New York: Plenum Press, 1997 [Google Scholar]
- 3.Weinstein RS. Prospects for telepathology. Hum Pathol 1986;17:433–434 [DOI] [PubMed] [Google Scholar]
- 4.Weinstein RS. Static image telepathology in perspective. Hum Pathol 1996;27:99–101 [DOI] [PubMed] [Google Scholar]
- 5.Kaplan K, Weinstein R, Pantanowit ZL. Telepathology. In: Pantanowitz L, Tuthill JM, Balis UJ, eds. Pathology informatics: Theory & practice. Chicago, IL: American Society for Clinical Pathology Press, 2012:257–272 [Google Scholar]
- 6.Pantanowitz L, Dickinson K, Evans AJ, et al. ATA clinical guidelines for telepathology. Telemed J E Health 2014;20:1049–1056 [DOI] [PubMed] [Google Scholar]
- 7.Bernard C, Chandrakanth SA, Cornell IS, et al. Guidelines from the Canadian Association of Pathologists for establishing a telepathology service for anatomic pathology using whole-slide imaging. J Pathol Inform 2014;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Della Mea V. 25 years of telepathology research: A bibliometric analysis. Diagn Pathol 2011;6(Suppl 1):S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cucoranu IC, Parwani AV, Vepa S, Weinstein RS, Pantanowitz L. Digital pathology: A systematic evaluation of the patent landscape. J Pathol Inform 2014;5:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunn BE, Almagro UA, Choi H, et al. Dynamic-robotic telepathology: Department of Veterans Affairs feasibility study. Hum Pathol 1997;28:8–12 [DOI] [PubMed] [Google Scholar]
- 11.Dunn BE, Choi H, Recla DL, Kerr SE, Wagenman BL. Robotic surgical telepathology between the Iron Mountain and Milwaukee Department of Veterans Affairs Medical Centers: A 12-year experience. Hum Pathol 2009;40:1092–1099 [DOI] [PubMed] [Google Scholar]
- 12.Weinstein RS, Bloom KJ, Rozek LS. Telepathology and the networking of pathology diagnostic services. Arch Pathol Lab Med 1987;111:646–652 [PubMed] [Google Scholar]
- 13.Weinstein RS, Bloom KJ, Rozek LS. Telepathology: System design and specifications. Proc SPIE Visual Commun Image Proc. 1987;0845:404–407 [Google Scholar]
- 14.Weinstein RS, Bloom KJ, Rozek LS. Static and dynamic imaging in pathology. Proceedings of the First International Conference on Image Management and Communication Washington, DC: 1990 [Google Scholar]
- 15.Krupinski EA, Weinstein RS, Bloom KJ, Rozek LS. Progress in telepathology: System implementation and testing. Adv Pathol Lab Med 1993;6:63–87 [Google Scholar]
- 16.Nordrum I, Engum B, Rinde E, et al. Remote frozen section service: A telepathology project in northern Norway. Hum Pathol 1991;22:514–518 [DOI] [PubMed] [Google Scholar]
- 17.Weinstein RS, Graham AR, Richter LC, et al. Overview of telepathology, virtual microscopy, and whole slide imaging: Prospects for the future. Hum Pathol 2009;40:1057–1069 [DOI] [PubMed] [Google Scholar]
- 18.Medovyi V, Pyatnitskiy A. Robotic microscopy and information technology to increase accuracy, sensitivity and availability of blood cell analysis. In: Mendez-Vilas A, ed. Current microscopy contributions to advances in science and technology, Vol. 5 Badajoz, Spain: FORMATEX, 2012:775–781 [Google Scholar]
- 19.Goacher E, Randell R, Williams B, Treanor D. The Diagnostic concordance of whole slide imaging and light microscopy: A systematic review. Arch Pathol Lab Med 2017;141:151–161 [DOI] [PubMed] [Google Scholar]
- 20.Ghaznavi F, Evans A, Madabhushi A, Feldman M. Digital imaging in pathology: Whole-slide imaging and beyond. Annu Rev Pathol 2013;8:331–359 [DOI] [PubMed] [Google Scholar]
- 21.Wilbur DC. Digital cytology: Current state of the art and prospects for the future. Acta Cytol 2011;55:227–238 [DOI] [PubMed] [Google Scholar]
- 22.Collins BT. Telepathology in cytopathology: Challenges and opportunities. Acta Cytol 2013;57:221–232 [DOI] [PubMed] [Google Scholar]
- 23.Weinstein RS. Telepathology system development and implementation. In: Eren H, ed. The e-medicine, e-health, m-health, telemedicine, and telehealth handbook: Telemedicine and electronic medicine. Vol 1 Boca Raton, FL: CRC Press, Taylor & Francis Group, 2015:577–591 [Google Scholar]
- 24.Fisher SI, Nandedkar MA, Williams BH, Abbondanzo SL. Telehematopathology in a clinical consultative practice. Hum Pathol 2001;32:1327–1333 [DOI] [PubMed] [Google Scholar]
- 25.McLaughlin WJ, Schifman RB, Ryan KJ, et al. Telemicrobiology: Feasibility study. Telemed J 1998;4:11–17 [DOI] [PubMed] [Google Scholar]
- 26.Weinstein RS, Graham AR, Lian F, et al. Reconciliation of diverse telepathology system designs. Historic issues and implications for emerging markets and new applications. Acta Pathol Microbiol Immunol Scand 2012;120:256–275 [DOI] [PubMed] [Google Scholar]
- 27.Weinstein RS, Graham AR, Barker GR. Second opinion telepathology services for cancer patients. In: Ternullo J, ed. Thought leaders in medical informatics. Minneapolis, MN: Bierbaum Publishing, 2012;16–28 [Google Scholar]
- 28.Wilbur DC, Madi K, Colvin RB, et al. Whole-slide imaging digital pathology as a platform for teleconsultation: A pilot study using paired subspecialist correlations. Arch Pathol Lab Med 2009;133:1949–1953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frable WJ. Surgical pathology—Second reviews, institutional reviews, audits, and correlations: What's out there? Error or diagnostic variation? Arch Pathol Lab Med 2006;130:620–625 [DOI] [PubMed] [Google Scholar]
- 30.Kronz JD, Westra WH, Epstein JI. Mandatory second opinion surgical pathology at a large referral hospital. Cancer 1999;86:2426–2435 [PubMed] [Google Scholar]
- 31.Evans AJ, Chetty R, Clarke BA, et al. Primary frozen section diagnosis by robotic microscopy and virtual slide telepathology: The University Health Network experience. Hum Pathol 2009;40:1070–1081 [DOI] [PubMed] [Google Scholar]
- 32.Pantanowitz LTJMBUJ. Pathology informatics: Theory & practice. Chicago, IL: American Society for Clinical Pathology Press, 2012 [Google Scholar]
- 33.Weinstein RS, Lopez AM, Barker GP, et al. The innovative bundling of teleradiology, telepathology, and teleoncology services. IBM Syst J 2007;46:69–84 [Google Scholar]
- 34.Lopez AM, Graham AR, Barker GP, et al. Virtual slide telepathology enables an innovative telehealth rapid breast care clinic. Semin Diagn Pathol 2009;26:177–186 [DOI] [PubMed] [Google Scholar]
- 35.Whole Slide Imaging. 2016. Available at www.ncbi.nlm.nih.gov/pubmed/?term=%22Whole+Slide+Imaging%22 (last accessed September30, 2016)
- 36.Lowe A, Chlipala E, Elin J, Kawano Y, Long RE, Tillman D. Validation of digital pathology in a healthcare environment. Madison, WI: Digital Pathology Association, 2011 [Google Scholar]
- 37.Park B. Communications aspects of telemedicine. In: Bashshur R, Armstrong PA, Youssef ZI, eds. Telemedicine; explorations in the use of telecommunications in health care. Springfield, IL: Charles C. Thomas, 1975:54–86 [Google Scholar]
- 38.Rojo MG, Garcia GB, Mateos CP, Garcia JG, Vicente MC. Critical comparison of 31 commercially available digital slide systems in pathology. Int J Surg Pathol 2006;14:285–305 [DOI] [PubMed] [Google Scholar]
- 39.Farahani N, Parwani AV, Pantanowitz L. Whole slide imaging in pathology: Advantages, limitations, and emerging perspectives. Path Lab Med Intern 2015;7:23–33 [Google Scholar]
- 40.Pantanowitz L, Dickinson K, Evans AJ, et al. American Telemedicine Association clinical guidelines for telepathology. J Pathol Inform 2014;5:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams BH, Mullick FG, Butler DR, Herring RF, O'Leary TJ. Clinical evaluation of an international static image-based telepathology service. Hum Pathol 2001;32:1309–1317 [DOI] [PubMed] [Google Scholar]
- 42.Halliday BE, Bhattacharyya AK, Graham AR, et al. Diagnostic accuracy of an international static-imaging telepathology consultation service. Hum Pathol 1997;28:17–21 [DOI] [PubMed] [Google Scholar]
- 43.Graham AR, Bhattacharyya AK, Scott KM, et al. Virtual slide telepathology for an academic teaching hospital surgical pathology quality assurance program. Hum Pathol 2009;40:1129–1136 [DOI] [PubMed] [Google Scholar]
- 44.Lopez AM, Graham AR, Barker GP, et al. Virtual slide telepathology enables an innovative telehealth rapid breast care clinic. Hum Pathol 2009;40:1082–1091 [DOI] [PubMed] [Google Scholar]
- 45.Martin E, Dusserre P, Fages A, Hauri P, Vieillefond A, Bastien H. Telepathology: A new tool of pathology? Presentation of a French national network. Zentralbl Pathol 1992;138:419–423 [PubMed] [Google Scholar]
- 46.Weinstein LJ, Epstein JI, Edlow D, Westra WH. Static image analysis of skin specimens: The application of telepathology to frozen section evaluation. Hum Pathol 1997;28:30–35 [DOI] [PubMed] [Google Scholar]
- 47.Weinstein MH, Epstein JI. Telepathology diagnosis of prostrate needle biopsies. Hum Pathol 1997;28:22–29 [DOI] [PubMed] [Google Scholar]
- 48.Weinstein RS, Bhattacharyya AK, Graham AR, Davis JR. Telepathology: A ten-year progress report. Hum Pathol 1997;28:1–7 [DOI] [PubMed] [Google Scholar]
- 49.Sharma G, Kelly S, Wiehagen L, Palekar A, Pantanowit ZL, Parwani A. Implementation of whole slide imaging for multi-site review of performance improvement program (PIP) slides. Arch Path Lab Med 2011;135:1227–1228 [Google Scholar]
- 50.Bauer TW, Schoenfield L, Slaw RJ, Yerian L, Sun Z, Henricks WH. Validation of whole slide imaging for primary diagnosis in surgical pathology. Arch Pathol Lab Med 2013;137:518–524 [DOI] [PubMed] [Google Scholar]
- 51.Parwani AV, Hassell L, Glassy E, Pantanowitz L. Regulatory barriers surrounding the use of whole slide imaging in the United States of America. J Pathol Inform 2014;5:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Food and Drug Administration. Technical performance assessment of digital pathology whole slide imaging devices. Guidance for industry and food and drug administration staff. 2016. https://www.federalregister.gov/documents/2015/02/25/2015-03843/technical-performance-assessment-of-digital-pathology-whole-slide-imaging-devices-draft-guidance-for (last accessed January20, 2017)
- 53.Dennis T, Start RD, Cross SS. The use of digital imaging, video conferencing, and telepathology in histopathology: A national survey. J Clin Pathol 2005;58:254–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crimmins D, Crooks D, Pickles A, Morris K. [Use of telepathology to provide rapid diagnosis of neurosurgical specimens]. Neurochirurgie 2005;51:84–88 [DOI] [PubMed] [Google Scholar]
- 55.Sukal SA, Busam KJ, Nehal KS, et al. Clinical application of dynamic telepathology in Mohs surgery. Dermatol Surg 2005;31:1700–1703 [DOI] [PubMed] [Google Scholar]
- 56.Eichhorn JH, Brauns TA, Gelfand JA, Crothers BA, Wilbur DC. A novel automated screening and interpretation process for cervical cytology using the internet transmission of low-resolution images: A feasibility study. Cancer 2005;105:199–206 [DOI] [PubMed] [Google Scholar]
- 57.Johnston DJ, Costello SP, Dervan PA, O'Shea DG. Development and preliminary evaluation of the VPS ReplaySuite: A virtual double-headed microscope for pathology. BMC Med Inform Decis Making 2005;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Helin H, Lundin M, Lundin J, et al. Web-based virtual microscopy in teaching and standardizing Gleason grading. Hum Pathol 2005;36:381–386 [DOI] [PubMed] [Google Scholar]
- 59.Vari S, Cserneky M, Kadar A, Szende B. Development of present and future of telepathology in Hungary. Pathol Oncol Res 2005;11:174–177 [DOI] [PubMed] [Google Scholar]
- 60.Krupinski EA, Tillack AA, Richter L, et al. Eye-movement study and human performance using telepathology virtual slides: Implications for medical education and differences with experience. Hum Pathol 2006;37:1543–1556 [DOI] [PubMed] [Google Scholar]
- 61.Jialdasani R, Desai S, Gupta M, et al. An analysis of 46 static telecytology cases over a period of two years. J Telemed Telecare 2006;12:311–314 [DOI] [PubMed] [Google Scholar]
- 62.Abdirad A, Sarrafpour B, Ghaderi-Sohi S. Static telepathology in cancer institute of Tehran university: Report of the first academic experience in Iran. Diagn Pathol 2006;1:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Teodorovic I, Isabelle M, Carbone A, et al. TuBaFrost 6: Virtual microscopy in virtual tumour banking. Eur J Cancer 2006;42:3110–3116 [DOI] [PubMed] [Google Scholar]
- 64.Frierson HF, Jr., Galgano MT. Frozen-section diagnosis by wireless telepathology and ultra portable computer: Use in pathology resident/faculty consultation. Hum Pathol 2007;38:1330–1334 [DOI] [PubMed] [Google Scholar]
- 65.Ayatollahi H, Khoei A, Mohammadian N, et al. Telemedicine in diagnostic pleural cytology: A feasibility study between universities in Iran and the USA. J Telemed Telecare 2007;13:363–368 [DOI] [PubMed] [Google Scholar]
- 66.Massone C, Soyer HP, Lozzi GP, et al. Feasibility and diagnostic agreement in teledermatopathology using a virtual slide system. Hum Pathol 2007;38:546–554 [DOI] [PubMed] [Google Scholar]
- 67.Kerr SE, Bellizzi AM, Stelow EB, Frierson HF, Jr., Policarpio-Nicolas ML. Initial assessment of fine-needle aspiration specimens by telepathology: Validation for use in pathology resident-faculty consultations. Am J Clin Pathol 2008;130:409–413 [DOI] [PubMed] [Google Scholar]
- 68.Slodkowska J, Chyczewski L, Wojciechowski M. Virtual slides: Application in pulmonary pathology consultations. Folia Histochem et Cytobiol 2008;46:121–124 [DOI] [PubMed] [Google Scholar]
- 69.Liang WY, Hsu CY, Lai CR, Ho DM, Chiang IJ. Low-cost telepathology system for intraoperative frozen-section consultation: Our experience and review of the literature. Hum Pathol 2008;39:56–62 [DOI] [PubMed] [Google Scholar]
- 70.Tsuchihashi Y, Takamatsu T, Hashimoto Y, Takashima T, Nakano K, Fujita S. Use of virtual slide system for quick frozen intra-operative telepathology diagnosis in Kyoto, Japan. Diagn Pathol 2008;3(Suppl 1):S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chandler I, Houlston RS. Interobserver agreement in grading of colorectal cancers-findings from a nationwide web-based survey of histopathologists. Histopathology 2008;52:494–499 [DOI] [PubMed] [Google Scholar]
- 72.Banach L, Stepien A, Schneider J, Wichrzycka-Lancaster E. Dynamic active telepathology over National Health Laboratory service network, South Africa: Feasibility study using Nikon Coolscope. Diagn Pathol 2008;3(Suppl 1):S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ayad E, Sicurello F. Telepathology in emerging countries pilot project between Italy and Egypt. Diagn Pathol 2008;3(Suppl 1):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Giansanti D, Castrichella L, Giovagnoli MR. Telepathology requires specific training for the technician in the biomedical laboratory. Telemed J E Health 2008;14:801–807 [DOI] [PubMed] [Google Scholar]
- 75.Glotsos D, Georgiadis P, Kostopoulos S, et al. A pilot study investigating the minimum requirements necessary for grading astrocytomas remotely. Anal Quant Cytol Histol 2009;31:262–268 [PubMed] [Google Scholar]
- 76.Kldiashvili E, Schrader T. Implementation of telepathology in the republic of georgia. Telemed J E Health 2009;15:479–483 [DOI] [PubMed] [Google Scholar]
- 77.Potts SJ. Digital pathology in drug discovery and development: Multisite integration. Drug Discov Today 2009;14:935–941 [DOI] [PubMed] [Google Scholar]
- 78.Shirts BH, Gundlapalli AV, Jackson B. Pilot study of linking Web-based supplemental interpretive information to laboratory test reports. Am J Clin Pathol 2009;132:818–823 [DOI] [PubMed] [Google Scholar]
- 79.Horbinski C, Hamilton RL. Application of telepathology for neuropathologic intraoperative consultations. Brain Pathol (Zurich, Switzerland) 2009;19:317–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nielsen PS, Lindebjerg J, Rasmussen J, Starklint H, Waldstrom M, Nielsen B. Virtual microscopy: An evaluation of its validity and diagnostic performance in routine histologic diagnosis of skin tumors. Hum Pathol 2010;41:1770–1776 [DOI] [PubMed] [Google Scholar]
- 81.Ryskal O, Muschinskaja M, Gobel U, et al. Telemicroscopic conferences for children of the Perm territory with suspected or proven malignant solid tumors. Klin Padiatr 2010;222:199–202 [DOI] [PubMed] [Google Scholar]
- 82.Giansanti D, Cerroni F, Amodeo R, Filoni M, Giovagnoli MR. A pilot study for the integration of cytometry reports in digital cytology telemedicine applications. Ann Ist Super Sanita 2010;46:138–143 [DOI] [PubMed] [Google Scholar]
- 83.Khurana KK, Swati I, Kasturi R, Lambert R, Izquierdo R. Telecytopathology for rapid preliminary diagnosis of ultrasound-guided fine-needle aspiration of thyroid nodules. Telemed J E Health 2011;17:763–767 [DOI] [PubMed] [Google Scholar]
- 84.Marotti JD, Glatz K, Parkash V, Hecht JL. International Internet-based assessment of observer variability for diagnostically challenging endometrial biopsies. Arch Pathol Lab Med 2011;135:464–470 [DOI] [PubMed] [Google Scholar]
- 85.Wiley CA, Murdoch G, Parwani A, et al. Interinstitutional and interstate teleneuropathology. J Pathol Inform 2011;2:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ramey J, Fung KM, Hassell LA. Use of mobile high-resolution device for remote frozen section evaluation of whole slide images. J Pathol Inform 2011;2:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Slodkowska J, Markiewicz T, Grala B, et al. Accuracy of a remote quantitative image analysis in the whole slide images. Diagn Pathol 2011;6(Suppl 1):S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wamala D, Katamba A, Dworak O. Feasibility and diagnostic accuracy of Internet-based dynamic telepathology between Uganda and Germany. J Telemed Telecare 2011;17:222–225 [DOI] [PubMed] [Google Scholar]
- 89.Intersimone D, Snoj V, Riosa F, et al. Transnational telepathology consultations using a basic digital microscope: Experience in the Italy-Slovenjia INTERREG project “patient without borders.” Diagn Pathol 2011;6(Suppl 1):S25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ayad E. Virtual telepathology in Egypt, applications of WSI in Cairo University. Diagn Pathol 2011;6(Suppl 1):S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Prosch H, Hoffmann E, Bernhardt K, et al. Dynamic telecytologic evaluation of imprint cytology samples from CT-guided lung biopsies: A feasibility study. Eur Radiol 2011;21:1922–1927 [DOI] [PubMed] [Google Scholar]
- 92.Kldiashvili E, Schrader T. Reproducibility of telecytology diagnosis of cervical smears in a quality assurance program: The Georgian experience. Telemed J E Health 2011;17:565–568 [DOI] [PubMed] [Google Scholar]
- 93.Harnden P, Coleman D, Moss S, Kodikara S, Griffin NR, Melia J. Evaluation of the use of digital images for a national prostate core external quality assurance scheme. Histopathology 2011;59:703–709 [DOI] [PubMed] [Google Scholar]
- 94.Angelini A, Andersen CB, Bartoloni G, et al. A web-based pilot study of inter-pathologist reproducibility using the ISHLT 2004 working formulation for biopsy diagnosis of cardiac allograft rejection: The European experience. J Heart Lung Transplant 2011;30:1214–1220 [DOI] [PubMed] [Google Scholar]
- 95.Khurana KK, Rong R, Wang D, Roy A. Dynamic telecytopathology for on-site preliminary diagnosis of endoscopic ultrasound-guided fine needle aspiration of pancreatic masses. J Telemed Telecare 2012;18:253–259 [DOI] [PubMed] [Google Scholar]
- 96.Heimann A, Maini G, Hwang S, Shroyer KR, Singh M. Use of telecytology for the immediate assessment of CT guided and endoscopic FNA cytology: Diagnostic accuracy, advantages, and pitfalls. Diagn Cytopathol 2012;40:575–581 [DOI] [PubMed] [Google Scholar]
- 97.Goyal A, Jhala N, Gupta P. TeleCyP (Telecytopathology): Real-time fine-needle aspiration interpretation. Acta Cytol 2012;56:669–677 [DOI] [PubMed] [Google Scholar]
- 98.Gimbel DC, Sohani AR, Prasad Busarla SV, et al. A static-image telepathology system for dermatopathology consultation in East Africa: The Massachusetts General Hospital Experience. J Am Acad Dermatol 2012;67:997–1007 [DOI] [PubMed] [Google Scholar]
- 99.Sohani AR, Sohani MA. Static digital telepathology: A model for diagnostic and educational support to pathologists in the developing world. Anal Cell Pathol (Amst) 2012;35:25–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Al Habeeb A, Evans A, Ghazarian D. Virtual microscopy using whole-slide imaging as an enabler for teledermatopathology: A paired consultant validation study. J Pathol Inform 2012;3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gould PV, Saikali S. A comparison of digitized frozen section and smear preparations for intraoperative neurotelepathology. Anal Cell Pathol (Amst) 2012;35:85–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tetu B, Fortin JP, Gagnon MP, Louahlia S. The challenges of implementing a “patient-oriented” telepathology network; the Eastern Quebec telepathology project experience. Anal Cell Pathol (Amst) 2012;35:11–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nakayama I, Matsumura T, Kamataki A, et al. Development of a teledermatopathology consultation system using virtual slides. Diagn Pathol 2012;7:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Washiya K, Takamizu R, Kumagai Y, et al. World wide web-based cytological analysis of atypical squamous cells cannot exclude high-grade intraepithelial lesions. Acta Cytol 2012;56:47–54 [DOI] [PubMed] [Google Scholar]
- 105.Gifford AJ, Colebatch AJ, Litkouhi S, et al. Remote frozen section examination of breast sentinel lymph nodes by telepathology. ANZ J Surg 2012;82:803–808 [DOI] [PubMed] [Google Scholar]
- 106.Sanders DS, Grabsch H, Harrison R, et al. Comparing virtual with conventional microscopy for the consensus diagnosis of Barrett's neoplasia in the AspECT Barrett's chemoprevention trial pathology audit. Histopathology 2012;61:795–800 [DOI] [PubMed] [Google Scholar]
- 107.Al-Janabi S, Huisman A, Van Diest PJ. Digital pathology: Current status and future perspectives. Histopathology 2012;61:1–9 [DOI] [PubMed] [Google Scholar]
- 108.Kumar N, Busarla SV, Sayed S, et al. Telecytology in East Africa: A feasibility study of forty cases using a static imaging system. J Telemed Telecare 2012;18:7–12 [DOI] [PubMed] [Google Scholar]
- 109.Puppa G, Senore C, Sheahan K, et al. Diagnostic reproducibility of tumour budding in colorectal cancer: A multicentre, multinational study using virtual microscopy. Histopathology 2012;61:562–575 [DOI] [PubMed] [Google Scholar]
- 110.Izquierdo RE, Kasturi R, Khurana K, Hopkins R, Swati I. Feasibility of immediate assessment of fine needle aspirates of thyroid nodules by telecytopathology. Endocr Pract 2013;19:14–18 [DOI] [PubMed] [Google Scholar]
- 111.Jen KY, Olson JL, Brodsky S, Zhou XJ, Nadasdy T, Laszik ZG. Reliability of whole slide images as a diagnostic modality for renal allograft biopsies. Hum Pathol 2013;44:888–894 [DOI] [PubMed] [Google Scholar]
- 112.Wright AM, Smith D, Dhurandhar B, et al. Digital slide imaging in cervicovaginal cytology: A pilot study. Arch Pathol Lab Med 2013;137:618–624 [DOI] [PubMed] [Google Scholar]
- 113.Kadaba V, Ly T, Noor S, et al. A hybrid approach to telepathology in Cambodia. J Telemed Telecare 2013;19:475–478 [DOI] [PubMed] [Google Scholar]
- 114.Etit D, Tan A, Bakir K, et al. Interobserver agreement in salivary gland neoplasms by telepathology: An analysis of 47 cases. Anal Quant Cytopathol Histopathol 2013;35:114–120 [PubMed] [Google Scholar]
- 115.Bellis M, Metias S, Naugler C, Pollett A, Jothy S, Yousef GM. Digital pathology: Attitudes and practices in the Canadian pathology community. J Pathol Inform 2013;4:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Braunhut BL, Graham AR, Lian F, et al. Subspecialty surgical pathologist's performances as triage pathologists on a telepathology-enabled quality assurance surgical pathology service: A human factors study. J Pathol Inform 2014;5:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Perron E, Louahlia S, Nadeau L, et al. Telepathology for intraoperative consultations and expert opinions: The experience of the Eastern Quebec Telepathology Network. Arch Pathol Lab Med 2014;138:1223–1228 [DOI] [PubMed] [Google Scholar]
- 118.Houghton JP, Ervine AJ, Kenny SL, et al. Concordance between digital pathology and light microscopy in general surgical pathology: A pilot study of 100 cases. J Clin Pathol 2014;67:1052–1055 [DOI] [PubMed] [Google Scholar]
- 119.Banihashemi A, Asgari M, Shooshtarizade T, Abolhasani M, Mireskandari M. Electronic expert consultation using digital still images for evaluation of atypical small acinar proliferations of the prostate: A comparison with immunohistochemistry. Ann Diagn Pathol 2014;18:163–170 [DOI] [PubMed] [Google Scholar]
- 120.Randell R, Ruddle RA, Thomas RG, Mello-Thoms C, Treanor D. Diagnosis of major cancer resection specimens with virtual slides: Impact of a novel digital pathology workstation. Hum Pathol 2014;45:2101–2106 [DOI] [PubMed] [Google Scholar]
- 121.Vitkovski T, Bhuiya T, Esposito M. Utility of telepathology as a consultation tool between an off-site surgical pathology suite and affiliated hospitals in the frozen section diagnosis of lung neoplasms. J Pathol Inform 2015;6:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bott MJ, James B, Collins BT, et al. A prospective clinical trial of telecytopathology for rapid interpretation of specimens obtained during endobronchial ultrasound-fine needle aspiration. Ann Thorac Surg 2015;100:201–205; discussion 205–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.McCarthy EE, McMahon RQ, Das K, Stewart J., 3rd Internal validation testing for new technologies: Bringing telecytopathology into the mainstream. Diagn Pathol 2015;43:3–7 [DOI] [PubMed] [Google Scholar]
- 124.Fontelo P, Liu F, Yagi Y. Evaluation of a smartphone for telepathology: Lessons learned. J Pathol Inform 2015;6:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Goswami R, Pi D, Pal J, Cheng K, Hudoba De Badyn M. Performance evaluation of a dynamic telepathology system (Panoptiq) in the morphologic assessment of peripheral blood film abnormalities. Intern J Lab Hematol 2015;37:365–371 [DOI] [PubMed] [Google Scholar]
- 126.Corredor G, Romero E, Iregui M. An adaptable navigation strategy for virtual microscopy from mobile platforms. J Biomed Inform 2015;54:39–49 [DOI] [PubMed] [Google Scholar]
- 127.Pradhan D, Monaco SE, Parwani AV, Ahmed I, Duboy J, Pantanowitz L. Evaluation of panoramic digital images using Panoptiq for frozen section diagnosis. J Pathol Inform 2016;7:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Agarwal S, Zhao L, Zhang R, Hassell L. FaceTime validation study: Low-cost streaming video for cytology adequacy assessment. Cancer Cytopathol 2016;124:213–220 [DOI] [PubMed] [Google Scholar]
- 129.Pare G, Meyer J, Trudel MC, Tetu B. Impacts of a large decentralized telepathology network in Canada. Telemed J E Health 2016;22:246–250 [DOI] [PubMed] [Google Scholar]
- 130.Eccher A, Neil D, Ciangherotti A, et al. Digital reporting of whole-slide images is safe and suitable for assessing organ quality in preimplantation renal biopsies. Hum Pathol 2016;47:115–120 [DOI] [PubMed] [Google Scholar]
- 131.Cheng CL, Azhar R, Sng SH, et al. Enabling digital pathology in the diagnostic setting: Navigating through the implementation journey in an academic medical centre. J Clin Pathol 2016;0:1–9 [DOI] [PubMed] [Google Scholar]
- 132.Hitchcock CL, Hitchcock LE. Three years of experience with routine use of telepathology in assessment of excisional and aspirate biopsies of breast lesions. Croatian Med J 2005;46:449–457 [PubMed] [Google Scholar]
- 133.Burthem J, Brereton M, Ardern J, et al. The use of digital ‘virtual slides’ in the quality assessment of haematological morphology: Results of a pilot exercise involving UK NEQAS(H) participants. Br J Haematol 2005;130:293–296 [DOI] [PubMed] [Google Scholar]
- 134.Hutarew G, Schlicker HU, Idriceanu C, Strasser F, Dietze O. Four years experience with teleneuropathology. J Telemed Telecare 2006;12:387–391 [DOI] [PubMed] [Google Scholar]
- 135.Leinweber B, Massone C, Kodama K, et al. Teledermatopathology: A controlled study about diagnostic validity and technical requirements for digital transmission. Am J Dermatopathol 2006;28:413–416 [DOI] [PubMed] [Google Scholar]
- 136.Odze RD, Tomaszewski JE, Furth EE, et al. Variability in the diagnosis of dysplasia in ulcerative colitis by dynamic telepathology. Oncol Rep 2006;16:1123–1129 [PubMed] [Google Scholar]
- 137.McLemore EC, Schlinkert RT, Schlinkert DK, Williams JW, Bailey DP. Telepathy: Maximizing resident exposure to surgical pathology decision making. Am J Surg 2006;191:538–541 [DOI] [PubMed] [Google Scholar]
- 138.Glatz K, Willi N, Glatz D, et al. An international telecytologic quiz on urinary cytology reveals educational deficits and absence of a commonly used classification system. Am J Clin Pathol 2006;126:294–301 [DOI] [PubMed] [Google Scholar]
- 139.Horbinski C, Fine JL, Medina-Flores R, Yagi Y, Wiley CA. Telepathology for intraoperative neuropathologic consultations at an academic medical center: A 5-year report. J Neuropathol Exper Neurol 2007;66:750–759 [DOI] [PubMed] [Google Scholar]
- 140.Butnor KJ, Vollmer RT, Blaszyk H, Glatz K. Interobserver agreement on what constitutes visceral pleural invasion by non-small cell lung carcinoma: An internet-based assessment of international current practices. Am J Clin Pathol 2007;128:638–647 [DOI] [PubMed] [Google Scholar]
- 141.Li X, Liu J, Xu H, et al. A feasibility study of virtual slides in surgical pathology in China. Hum Pathol 2007;38:1842–1848 [DOI] [PubMed] [Google Scholar]
- 142.Bhele S, Jialdasani R, Kothari A, Bhosale S, Desai S. Analysis of deferrals on static telepathology consultation service. Ind J Pathol Microbiol 2007;50:749–753 [PubMed] [Google Scholar]
- 143.Eichhorn JH, Buckner L, Buckner SB, et al. Internet-based gynecologic telecytology with remote automated image selection: Results of a first-phase developmental trial. Am J Clin Pathol 2008;129:686–696 [DOI] [PubMed] [Google Scholar]
- 144.Li X, Gong E, McNutt MA, et al. Assessment of diagnostic accuracy and feasibility of dynamic telepathology in China. Hum Pathol 2008;39:236–242 [DOI] [PubMed] [Google Scholar]
- 145.Horbinski C, Wiley CA. Comparison of telepathology systems in neuropathological intraoperative consultations. Neuropathology 2009;29:655–663 [DOI] [PubMed] [Google Scholar]
- 146.Dunn BE, Choi H, Recla DL, Kerr SE, Wagenman BL. Robotic surgical telepathology between the Iron Mountain and Milwaukee Department of Veterans Affairs Medical Centers: A twelve year experience. Semin Diagn Pathol 2009;26:187–193 [DOI] [PubMed] [Google Scholar]
- 147.Wienert S, Beil M, Saeger K, Hufnagl P, Schrader T. Integration and acceleration of virtual microscopy as the key to successful implementation into the routine diagnostic process. Diagn Pathol 2009;4:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Slodkowska J, Pankowski J, Siemiatkowska K, Chyczewski L. Use of the virtual slide and the dynamic real-time telepathology systems for a consultation and the frozen section intra-operative diagnosis in thoracic/pulmonary pathology. Folia Histochem Cytobiol 2009;47:679–684 [DOI] [PubMed] [Google Scholar]
- 149.Alsharif M, Carlo-Demovich J, Massey C, et al. Telecytopathology for immediate evaluation of fine-needle aspiration specimens. Cancer Cytopathol 2010;118:119–126 [DOI] [PubMed] [Google Scholar]
- 150.Kldiashvili E, Schrader T. Diagnostic accuracy and image quality using a USB digital eyepiece camera for telecytology-Georgian experience. Telemed J E Health 2010;16:1051–1052 [DOI] [PubMed] [Google Scholar]
- 151.Risio M, Bussolati G, Senore C, et al. Virtual microscopy for histology quality assurance of screen-detected polyps. J Clin Pathol 2010;63:916–920 [DOI] [PubMed] [Google Scholar]
- 152.Zembowicz A, Ahmad A, Lyle SR. A comprehensive analysis of a web-based dermatopathology second opinion consultation practice. Arch Pathol Lab Med 2011;135:379–383 [DOI] [PubMed] [Google Scholar]
- 153.Jukic DM, Drogowski LM, Martina J, Parwani AV. Clinical examination and validation of primary diagnosis in anatomic pathology using whole slide digital images. Arch Pathol Lab Med 2011;135:372–378 [DOI] [PubMed] [Google Scholar]
- 154.Nassar A, Cohen C, Agersborg SS, et al. A multisite performance study comparing the reading of immunohistochemical slides on a computer monitor with conventional manual microscopy for estrogen and progesterone receptor analysis. Am J Clin Pathol 2011;135:461–467 [DOI] [PubMed] [Google Scholar]
- 155.Georgoulakis J, Archondakis S, Panayiotides I, et al. Study on the reproducibility of thyroid lesions telecytology diagnoses based upon digitized images. Diagn Cyopathol 2011;39:495–499 [DOI] [PubMed] [Google Scholar]
- 156.Pagni F, Bono F, Di Bella C, Faravelli A, Cappellini A. Virtual surgical pathology in underdeveloped countries: The Zambia Project. Arch Pathol Lab Med 2011;135:215–219 [DOI] [PubMed] [Google Scholar]
- 157.Schettini FA, Ferreira LC, Schettini AP, Camelo RT. Reproducibility of histopathologic diagnosis of skin diseases by digital photomicrographs versus conventional optical microscopy. An Bras Dermatol 2011;86:491–496 [DOI] [PubMed] [Google Scholar]
- 158.Campbell WS, Lele SM, West WW, Lazenby AJ, Smith LM, Hinrichs SH. Concordance between whole-slide imaging and light microscopy for routine surgical pathology. Hum Pathol 2012;43:1739–1744 [DOI] [PubMed] [Google Scholar]
- 159.Krupinski EA, Silverstein LD, Hashmi SF, Graham AR, Weinstein RS, Roehrig H. Observer performance using virtual pathology slides: Impact of LCD color reproduction accuracy. J Digit Imaging 2012;25:738–743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Marotti JD, Johncox V, Ng D, Gonzalez JL, Padmanabhan V. Implementation of telecytology for immediate assessment of endoscopic ultrasound-guided fine-needle aspirations compared to conventional on-site evaluation: Analysis of 240 consecutive cases. Acta Cytol 2012;56:548–553 [DOI] [PubMed] [Google Scholar]
- 161.Santiago TC, Jenkins JJ, Pedrosa F, et al. Improving the histopathologic diagnosis of pediatric malignancies in a low-resource setting by combining focused training and telepathology strategies. Pediatr Blood Cancer 2012;59:221–225 [DOI] [PubMed] [Google Scholar]
- 162.Ayad E, Yagi Y. Virtual microscopy beyond the pyramids, applications of WSI in Cairo University for E-education & telepathology. Anal Cell Pathol (Amst) 2012;35:93–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Tsilalis T, Archondakis S, Meristoudis C, et al. Assessment of static telecytological diagnoses' reproducibility in cervical smears prepared by means of liquid-based cytology. Telemed J E Health 2012;18:516–520 [DOI] [PubMed] [Google Scholar]
- 164.Shaw EC, Hanby AM, Wheeler K, et al. Observer agreement comparing the use of virtual slides with glass slides in the pathology review component of the POSH breast cancer cohort study. J Clin Pathol 2012;65:403–408 [DOI] [PubMed] [Google Scholar]
- 165.Fonyad L, Krenacs T, Nagy P, et al. Validation of diagnostic accuracy using digital slides in routine histopathology. Diagn Pathol 2012;7:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Khurana KK, Kovalovsky A, Wang D, Lenox R. Feasibility of dynamic telecytopathology for rapid on-site evaluation of endobronchial ultrasound-guided transbronchial fine needle aspiration. Telemed J E Health 2013;19:265–271 [DOI] [PubMed] [Google Scholar]
- 167.Gage JC, Joste N, Ronnett BM, et al. A comparison of cervical histopathology variability using whole slide digitized images versus glass slides: Experience with a statewide registry. Hum Pathol 2013;44:2542–2548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Francissen CM, van la Parra RF, Mulder AH, Bosch AM, de Roos WK. Evaluation of the benefit of routine intraoperative frozen section analysis of sentinel lymph nodes in breast cancer. ISRN Oncol 2013;2013:843793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Mammas CS, Geropoulos S, Saatsakis G, Konstantinidou A, Lemonidou C, Patsouris E. Telepathology as a method to optimize quality in organ transplantation: A feasibility and reliability study of the virtual benching of liver graft. Stud Health Technol Inform 2013;190:276–278 [PubMed] [Google Scholar]
- 170.Rao BK, Mateus R, Wassef C, Pellacani G. In vivo confocal microscopy in clinical practice: Comparison of bedside diagnostic accuracy of a trained physician and distant diagnosis of an expert reader. J Am Acad Dermatol 2013;69:e295–e300 [DOI] [PubMed] [Google Scholar]
- 171.Tawfik O, Davis M, Dillon S, Tawfik L, Diaz FJ, Fan F. Whole slide imaging of pap cell block preparations versus liquid-based thin-layer cervical cytology: A comparative study evaluating the detection of organisms and nonneoplastic findings. Acta Cytol 2014;58:388–397 [DOI] [PubMed] [Google Scholar]
- 172.Buck TP, Dilorio R, Havrilla L, O'Neill DG. Validation of a whole slide imaging system for primary diagnosis in surgical pathology: A community hospital experience. J Pathol Inform 2014;5:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Bauer TW, Slaw RJ. Validating whole-slide imaging for consultation diagnoses in surgical pathology. Arch Pathol Lab Med 2014;138:1459–1465 [DOI] [PubMed] [Google Scholar]
- 174.Khurana KK, Graber B, Wang D, Roy A. Telecytopathology for on-site adequacy evaluation decreases the nondiagnostic rate in endoscopic ultrasound-guided fine-needle aspiration of pancreatic lesions. Telemed J E Health 2014;20:822–827 [DOI] [PubMed] [Google Scholar]
- 175.Thrall MJ, Rivera AL, Takei H, Powell SZ. Validation of a novel robotic telepathology platform for neuropathology intraoperative touch preparations. J Pathol Inform 2014;5:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.McMahon RQ, McCarthy EE, Hetzel SJ, Das K, Stewart J., 3rd Focus on technology: How important is resolution in telecytopathology? Cancer Cytopathol 2014;122:546–552 [DOI] [PubMed] [Google Scholar]
- 177.Mpunga T, Tapela N, Hedt-Gauthier BL, et al. Diagnosis of cancer in rural Rwanda: Early outcomes of a phased approach to implement anatomic pathology services in resource-limited settings. Am J Clin Pathol 2014;142:541–545 [DOI] [PubMed] [Google Scholar]
- 178.Tetu B, Perron E, Louahlia S, Pare G, Trudel MC, Meyer J. The Eastern Quebec Telepathology Network: A three-year experience of clinical diagnostic services. Diagn Pathol 2014;9(Suppl 1):S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Chen J, Jiao Y, Lu C, Zhou J, Zhang Z, Zhou C. A nationwide telepathology consultation and quality control program in China: Implementation and result analysis. Diagn Pathol 2014;9(Suppl 1):S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Ribback S, Flessa S, Gromoll-Bergmann K, Evert M, Dombrowski F. Virtual slide telepathology with scanner systems for intraoperative frozen-section consultation. Pathol Res Pract 2014;210:377–382 [DOI] [PubMed] [Google Scholar]
- 181.Carey P, Fudzulani R, Scholfield D, et al. Remote and rapid pathological diagnosis in a resource challenged unit. J Clin Pathol 2014;67:540–543 [DOI] [PubMed] [Google Scholar]
- 182.Silveira CE, Silva TB, Fregnani JH, et al. Digital photography in skin cancer screening by mobile units in remote areas of Brazil. BMC Dermatol 2014;14:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Thrall MJ, Wimmer JL, Schwartz MR. Validation of multiple whole slide imaging scanners based on the guideline from the College of American Pathologists Pathology and Laboratory Quality Center. Arch Pathol Lab Med 2015;139:656–664 [DOI] [PubMed] [Google Scholar]
- 184.Jones NC, Nazarian RM, Duncan LM, et al. Interinstitutional whole slide imaging teleconsultation service development: Assessment using internal training and clinical consultation cases. Arch Pathol Lab Med 2015;139:627–635 [DOI] [PubMed] [Google Scholar]
- 185.Zhao C, Wu T, Ding X, et al. International telepathology consultation: Three years of experience between the University of Pittsburgh Medical Center and KingMed Diagnostics in China. J Pathol Inform 2015;6:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Papathomas TG, Oudijk L, Persu A, et al. SDHB/SDHA immunohistochemistry in pheochromocytomas and paragangliomas: A multicenter interobserver variation analysis using virtual microscopy: A multinational study of the European Network for the Study of Adrenal Tumors. Mod Pathol 2015;28:807–821 [DOI] [PubMed] [Google Scholar]
- 187.Sinard JH. Practical pathology informatics: Demystifying informatics for the practicing anatomic pathologist. Springer Science+Business Media; Materials specified: Table of content. 2006. Avaiable at: http://catdir.loc.gov/catdir/enhancements/fy0818/2005050011-t.html (last accessed January20, 2017)
- 188.Cross SS, Dennis T, Start RD. Telepathology: Current status and future prospects in diagnostic histopathology. Histopathology 2002;41:91–109 [DOI] [PubMed] [Google Scholar]
- 189.Mairinger T. Acceptance of telepathology in daily practice. Anal Cell Pathol 2000;21:135–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.O'Malley DP. Practical applications of telepathology using morphology-based anatomic pathology. Arch Pathol Lab Med 2008;132:743–744 [DOI] [PubMed] [Google Scholar]
- 191.Kumar S. Introduction to telepathology. In: Kumar S, Dunn BE, eds. Telepathology, Vol 1 Berlin: Springer, 2009:1–4 [Google Scholar]
- 192.Williams S, Henricks WH, Becich MJ, Toscano M, Carter AB. Telepathology for patient care: What am I getting myself into? Adv Anat Pathol 2010;17:130–149 [DOI] [PubMed] [Google Scholar]
- 193.Hedvat CV. Digital microscopy: Past, present, and future. Arch Pathol Lab Med 2010;134:1666–1670 [DOI] [PubMed] [Google Scholar]
- 194.Montalto MC. An industry perspective: An update on the adoption of whole slide imaging. J Pathol Inform 2016;7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Prayaga A. Telecytology: A retrospect and prospect. In: Kumar S, Dunn BE, eds. Telepathology, Vol 12 Berlin: Springer, 2009:149–162 [Google Scholar]
- 196.Weisz-Carrington P, Blount M, Kipreos B, et al. Telepathology between Richmond and Beckley Veterans Affairs Hospitals: Report on the first 1000 cases. Telemed J 1999;5:367–373 [DOI] [PubMed] [Google Scholar]
- 197.Sin of omission (definition). 2016. Available at: https://en.wikipedia.org/wiki/Sin_of_omission (last accessed October11, 2016)