Abstract
Objective
The purpose of this study was to evaluate the influence of patient age on the effects of conservative treatment of the anterior cruciate ligament (ACL).
Methods
A total of 102 consecutive patients with acute ACL injury were allowed to heal without surgery. Final magnetic resonance imaging images of the ACL were classified from grade I, indicating good morphological recovery, to grade IV, indicating poor recovery. Chi-square analysis was used to determine significant differences in the incidence of grades I and II among those less than 20 versus those 20 years or more of age.
Results
The mean follow-up to final magnetic resonance imaging was 9 months. A significant difference in the frequency of grades I and II was observed between age groups (<20 years, 13.0%; ≥20 years, 69.6%; P < 0.0001).
Conclusion
ACL injury was more severe, and morphological recovery with conservative treatment was poorer among younger patients than among adults.
Key Words: MRI, ACL, healing, age
The anterior cruciate ligament (ACL) rarely heals with the application of current surgical and conventional conservative methods.1–3 In contrast, good results have been reported for healing of the medial collateral ligament (MCL) with nonoperative, early mobilization.4–7 In comparison to injuries of the MCL, the intrinsic characteristics of ACL injuries may play a role in healing capacity.8 One reason ACL injuries may be refractory to treatment is failure of blood clots to form during initial healing, resulting in a lack of scaffolding between the 2 ruptured ends. Moreover, a layer of synovial tissue can form over the ruptured ACL surfaces, which may impede healing.9 However, it is clear that the healing capacity of the ACL has been underestimated, especially when studies report results from retracted ACLs instead of fully healed ACLs.9
Primary reconstruction is the most common surgical option because of the poor healing capacity of the ACL. Recent studies have reported an incidence of secondary ACL injury greater than 10% after initial reconstruction in athletes.10–13 Secondary ACL injuries include damage to the ACL graft or to the contralateral ACL.
We previously reported on a study of ACL healing with conservative treatment and proposed that applying mechanical stress to the joint and ligament after injury promotes healing.14–16 However, because most acute ACL injuries in that study received the same treatment regardless of patient age and tear type, treatment outcomes were inconsistent. The purpose of the present study was to assess the relationship between age at the time of injury and the progress of morphological recovery based on magnetic resonance imaging (MRI) images in patients who underwent conservative treatment for acute injury of the ACL. Our hypothesis was that morphological recovery in younger patients would be poorer than in adult patients.
MATERIALS AND METHODS
Patient Selection
Between February 2007 and November 2014, 105 consecutive acute ACL injuries were allowed to heal without surgery. Patients were excluded if the rupture was older than 20 days. Additional exclusion criteria included concomitant posterior cruciate ligament injury, lower extremity injury that made wearing a knee brace impossible, and unwillingness to participate in the study. We did not limit patient age and included patients with concomitant MCL injury. Three patients were lost to follow-up during the first 6 months; thus, 102 patients who were examined with MRI at a minimum of 6 months after injury were analyzed. The cohort consisted of 44 male and 58 female patients. The mean age at injury was 28.3 ± 13.4 years, ranging from 13 to 70 years. Thirty-nine patients were less than 20 years of age, whereas 63 were 20 years and older. Associated MCL injuries were found in 19 patients.
All patients were evaluated with MRI at the start of treatment (initial MRI). The mean time between injury and the initial MRI was 5.9 ± 4.6 days. The progress of healing was evaluated with MRI at 6 months. If possible, MRI assessment was performed after 6 months at the time of final follow-up (final MRI).
Conservative Treatment
Conservative treatment began with mobilization of the knee, muscle strengthening exercises, and full weight bearing. A brace was used to protect the joint. To minimize abnormal sagittal deviation between the femur and tibia within the range of knee motion, patients wore a knee brace (Kyuro knee brace; Nishinihon Rinsho Igaku Kenkyujo, Nakatsu, Japan) with a traction system consisting of 2 pairs of coil springs, with each spring contained in a housing.14,15 The knee brace was applied as soon as acute ACL tears were confirmed, so that mobilization of the knee could begin promptly without further damage to the injured fibers. Several temporary braces of different sizes were fabricated in advance for immediate use until the custom knee brace fitting was complete, typically within 1 week. The knee brace was removed after 3 months. Patients were allowed to begin running 5 months after the beginning of treatment, and contact sports were allowed 12 months after the beginning of treatment for those who wished.
All patients gave consent for participation in this study. This study was approved by the ethical board of our institution.
Magnetic Resonance Imaging
Patients were scanned in the supine position with a dedicated knee MRI coil and with the knee placed in slight flexion. The scanning protocol included sagittal and coronal imaging, but only sagittal imaging was considered for the purpose of this study. Scans in the sagittal plane were obtained parallel to the ACL in the coronal scout mode. Until May 2011, images were acquired with a 1.5-T MR system (Signa Advantage 1.5 T; GE Healthcare, Tokyo, Japan), with a fast spin echo sequence included proton density weighted of TR = 2000 ms, TE = 20 ms, slice thickness = 3 mm, field of view = 16 × 16 cm, reconstruction matrix of 512 × 512, and number of excitations of 1. Thereafter, we used a 3.0-T MRI system (Signa HDX 3.0 T; GE Healthcare), with a fast spin echo sequence included proton density weighted of TR = 1800 to 2000 ms, TE = 16.8 ms, slice thickness = 3 mm, field of view = 16 × 16 cm, reconstruction matrix of 512 × 512, and number of excitations of 1. From all available sequences, a slice in which the femoral insertion site of the ACL to bone was clearly visible was selected to evaluate the progress of morphological recovery.
Images of the injury in the sagittal plane were classified into 4 types according to the degree of injury, as follows: type I, straight and continuous band; type II, curved and continuous band; type III, displacement; and type IV, disrupted or horizontally oriented or unclear (Fig. 1). Types I and II combined were considered the type I + II group, and types III and IV combined were considered the type III + IV group.
FIGURE 1.
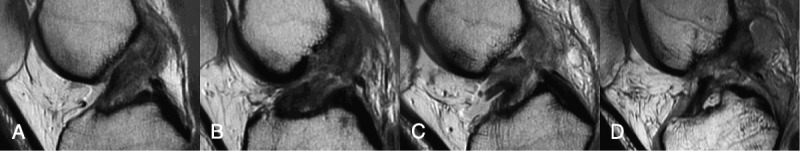
The initial MRI was classified into 4 types according to the degree of injury, from type I for mild injuries to type IV for severe injuries. A, Type I: straight and continuous band. B, Type II: curved and continuous band. C, Type III: displacement. D, Type IV: disrupted or horizontally oriented or unclear.
Similarly, images of the treated ACL in the sagittal plane at the time of follow-up were classified into 4 grades according to the degree of morphological recovery as follows: grade I, taut and straight band; grade II, straight band with partial thinning; grade III, thinned; and grade IV, unclear (Fig. 2). Grades I and II combined were considered the grade I + II group, and grades III and IV combined were considered the grade III + IV group.
FIGURE 2.
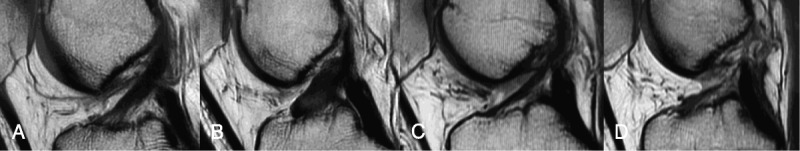
Magnetic resonance imaging at the time of follow-up was classified into 4 grades from grade I for good morphological recovery to grade IV for poor recovery. A, Grade I: taut and straight band. B Grade II: straight band with partial thinning. C Grade III: thinned. D, Grade IV: unclear.
The second author categorized the MRI scans using the criteria described above and calculated the χ2 coefficients for each parameter to determine relationships between the type of tear and the grade of healing.
Laxity Testing
Ligament stability was assessed with a KT-1000 arthrometer (MEDmetric Corp, San Diego, Calif) at manual maximum stress at the time of injury and at final follow-up. The pivot shift phenomenon was not assessed at the time of injury because its value would not be accurate because of pain; however, it was assessed at the final follow-up.
Statistical Analysis
Patients were grouped by age at the time of injury as less than 20 years of age or 20 or more years of age. Because of the nonnormality of the data, we computed Spearman correlation coefficients between the type of injury on initial MRI and the morphological grade on final MRI, between the type of injury on initial MRI and patient age, and between the morphological grade on final MRI and patient age. Chi-square analysis was used to determine significant differences in the incidence of type I + II and grade I + II groups in those less than 20 years of age versus those 20 or more years of age, and in males versus females. Paired Student t tests were used to compare arthrometer laxity values at the time of injury and at final follow-up. All statistical analyses were performed with JMP version 8 (SAS Institute Japan, Tokyo). Statistical significance was set at P < 0.05.
RESULTS
Magnetic resonance imaging at 6 months revealed that the ligament was completely retracted and no longer visible in 7 patients; this time point was therefore considered the final MRI for these patients. The 6-month MRI was considered the final MRI in an additional 41 patients. The 61 remaining patients returned for follow-up after 6 months, with a mean duration of 12.6 ± 7.9 months. The mean duration to the final MRI for all 102 patients was 9.2 ± 7.5 months.
Injury classification on initial MRI was as follows: 23 (22.5%) were type I; 34 (33.3%) were type II; 24 (23.5%) were type III; and 21 (20.6%) were type IV.
The classification of morphological healing at the 6-month MRI was as follows: 35 (34.3%) were grade I; 28 (27.5%), grade II; 20 (19.6%), grade III; and 19 (18.6%), grade IV. Of the 61 patients who underwent MRI assessment after 6 months, the subsequent grade assessment changed in 18 patients. Patients assessed as grade I or grade IV at 6 months exhibited no change. The grade changed in 15 grade II patients, improving to grade I in 6 and deteriorating to grade III in 9. One grade-III patient improved to grade I and 1 improved to grade II.
The classification of morphological healing on the final MRI was as follows: 41 (40.2%) were grade I; 17 (16.7%), grade II; 25 (24.5%), grade III; and 19 (18.6%), grade IV. We evaluated the percentage of patients classified as grade I, according to initial MRI type. In initial type I, 53.7% of patients were grade I on final MRI; in type II, 39.0% were grade I; in type III, 7.7% were grade I (Fig. 3); and in type IV, none were grade I. The percentage of the initial grade I + II group in the type I + II group was 84.2% (48 of 57 patients; Table 1). There was a significant relationship between the initial injury type and morphological healing grade categories (rs = 0.7390, P < 0.0001; Fig. 4).
FIGURE 3.
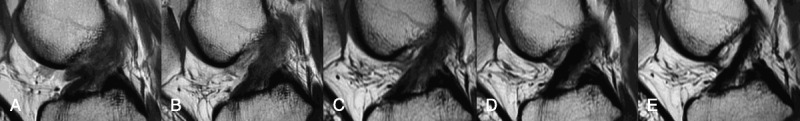
Magnetic resonance imaging of an acutely torn ACL in a 28-year-old woman treated conservatively. Magnetic resonance imaging taken the second day after injury (type III) (A), 2 months after injury (B), 6 months after injury (C), 12 months after injury (D), and 3 years after injury (grade I) (E).
TABLE 1.
Results of the Final Morphological Grade According to the Initial Injury Type
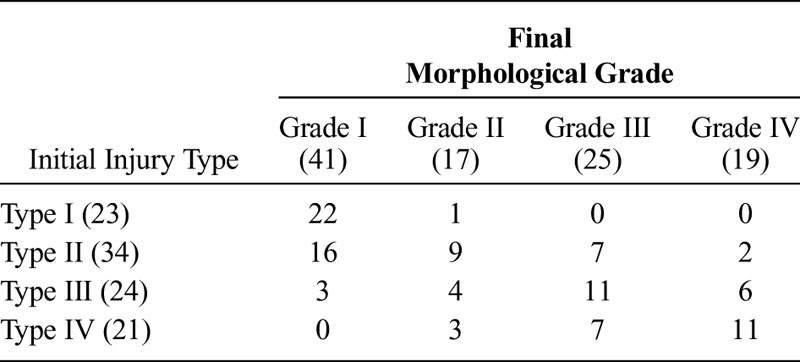
FIGURE 4.
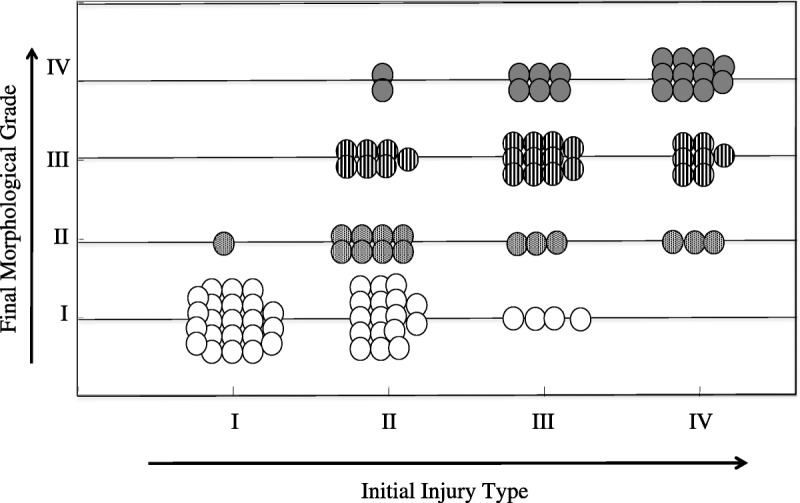
Scatter diagram of the initial injury type and final morphological grade. There was a significant relationship between the initial type and final grade categories (rs = 0.7550; P < 0.0001).
The final MRI assessment categorized by age indicated poor outcomes in patients less than 20 years of age. Of the 39 patients less than 20 years of age, 14 (35.9%) were in the type I + II group at initial assessment. In contrast, of those 20 or more years of age, 43 patients (68.3%) were in the type I + II group; there was a significant difference in the frequency of type I + II between age groups (P = 0.0014; Fig. 5). Of the patients less than 20 years of age, the final MRI revealed that 12 (30.8%) were in the grade I + II group. In contrast, among patients 20 or more years of age, 46 (73.0%) were in the grade I + II group; there was a significant difference in the frequency of grade I + II between age groups (P < 0.0001; Fig. 6).
FIGURE 5.
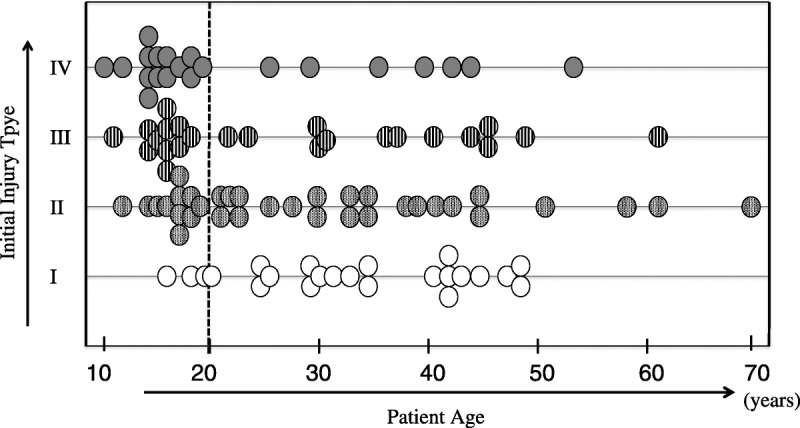
Scatter diagram of the initial injury type and patient age. Of patients less than 20 years of age, 64.1% were in the type III + IV group. There was a significant difference in the frequency of type III + IV between age groups (age <20 vs. ≥20 years; P = 0.0014).
FIGURE 6.
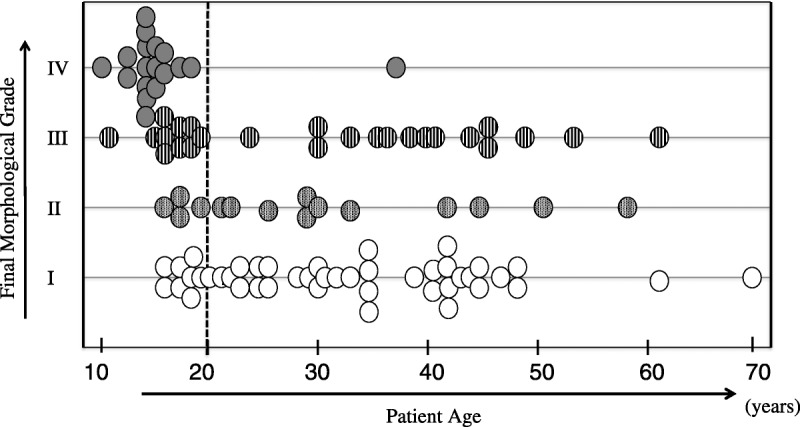
Scatter diagram of final grade and patient age. Of patients less than 20 years of age, the final MRI revealed that 69.2% were in the grade III + IV group. There was a significant difference in the frequency of grade III + IV between age groups (age <20 vs. ≥20 years; P < 0.0001).
There was no significant difference in the incidence of type I + II or grade I + II between the sexes.
The side-to-side differences measured by the arthrometer at the time of injury and at final follow-up were 5.3 ± 1.7 and 1.3 ± 1.6 mm, respectively. The pivot shift negative rate was 81.4% overall, and was 98.4% in the grade I + II group at the final follow-up.
The chi-square coefficients for interrelation were 0.75 for type of injury on initial MRI and 0.92 for morphological grade on final MRI.
DISCUSSION
The poor healing capacity of the ACL has been noted both histologically in animal models and clinically.3,8,9 Animal studies investigating conventional conservative treatment lack the conditions needed to evaluate the effect of early application of mechanical stress at physiological levels. To achieve those conditions, a knee brace with dynamic control is required; however, such a brace is very difficult to use in an animal model.
Early mobilization of the knee creates a time-dependent response of the injured ACL to physiological mechanical stress, caused by the condylar geometry of the knee. The mechanism of the crossed 4-bar linkage and the viscoelastic properties of the tissues are activated with mechanical stress, which induces the continuity and geometrical arrangement of the fibers.17,18 Newly synthesized collagen fibers form to resist those mechanical stresses. Importantly, this motion should be within normal physiological strain limits and with adequate protection because stress beyond the normal limits may cause further damage. An effective knee brace is essential to control the motion of the knee and minimize abnormal sagittal deviations between the femur and tibia within the range of motion appropriate for ACL injury treatment, while maintaining adequate stress on the injured fibers.
Several studies have reported results of ACL healing with conservative treatment alone.19 Fujimoto et al20 examined 31 consecutive patients with acute ACL injury and demonstrated that by moving the knee early with a simple brace limited to flexion and extension, 21 patients were able to maintain the ACL morphology as assessed with MRI taken after a minimum of 6 months. Costa-Paz et al21 reported that of 14 acute ACL injuries left untreated without any particular training or bracing, after a minimum of 2 years, the ACL had healed and the knee was stabilized in all patients and that the patients were able to return to sports activities at or near the same level as before injury. The published images of 5 cases from Cost-Paz et al as assessed with the classification system used in the present study included 4 cases of type I injury, and 1 of type II injury. All 5 cases presented with tears that were favorable to healing, and all patients were 23 or more years of age.
Recently, Deie et al22 used an organ culture model to show that the human ACL has a high intrinsic healing capacity. The ACL remnant contributes to anterior knee passive motion limits.23 Furthermore, ACL reconstructions performed with the ACL remnant have better outcomes than those not utilizing the ACL remnant.24–26
Two important points have been revealed by the present study. First, outcomes were poor in patients less than 20 years of age. This is an age at which the healing ability of ligaments is generally considered high. However, patients 20 or more years of age had better outcomes in the present study. We believe that one reason for this finding is that the initial injuries were more severe in the younger age group. In a review of reports on reinjury after ligament reconstruction, Ahldén et al27 found that reinjury occurred in 9.1% of patients overall, and in 22.0% of female soccer players aged 15 to 18 years. Shelbourne et al28 reported reinjury in 3.9% of patients more than 25 years of age compared with 17.4% of those less than 18 years of age. Webb et al29 reported an odds ratio for reinjury of 2.9 in patients less than 18 years of age. Maletis et al30 found that patients less than 21 years of age had a higher risk of requiring revision after ACL reconstruction. Vigorous sports activity has been identified as the underlying cause of this increased risk.31 It is believed that young adolescent and preadolescent individuals do not have fully developed neuromuscular coordination and that the damage sustained at the time of injury is severe.32 Further training may be needed to improve these conditions.33,34 The present study showed similar trends, with inferior outcomes in patients less than 20 years of age. Even those patients aged less than 20 years with type II injuries showed quickly progressive abnormal reactions of the ligament compared with adults. Therefore, patients classified with type III + IV injuries and those with type II injury who are aged less than 20 years should be considered not suitable for conservative treatment.
Second, in tears limited to a straight and continuous band at the time of injury (type I + II group), good outcomes (grade I + II group) were achieved in 84.2% of patients; this indicated a strong tendency toward healing. The good outcome group showed an improvement in laxity, as measured with the arthrometer, and 98.4% had negative results for the pivot shift phenomenon. These findings demonstrate that restoration of the mechanical function of the ACL occurred. We believe that the type I + II group included avulsion injuries at the site of femoral attachment, injuries with a considerable amount of residual synovial membrane covering the ACL, and injuries in which the fibers formed a bundle with only minor displacement. The degree of laxity in type I injuries was similar to that in the other types; given that all 50 patients in our previous study had complete tears based on arthroscopic findings, we believe that the type I group included mostly complete tears and not partial tears.16 The type III + IV group included severe mop-end tears with major displacement. If the indication for our conservative treatment was limited to the type I + II group, better outcomes might have been achieved.
There were several limitations to the present study. First, there was no control group receiving conventional conservative treatment, which promotes healing of the ACL but does not actually restore its morphology. Administering conventional conservative treatment may, therefore, raise ethical questions. Second, MRI assessments were performed over a relatively short period. Complete observation of ACL healing requires more than 1 year of follow-up. However, although it has been generally accepted that the ACL does not heal with conservative treatment, the injured ACLs showed morphological improvement on MRI over the short term of this study; this suggests the need to review the theory that the healing capacity of the ACL is poor. Third, this study aimed to demonstrate the capacity of the ACL to heal naturally through the use of early protective mobilization with a controllable knee brace, but not to evaluate functional outcomes after follow-up. Fourth, 2 different MRI magnets were used. However, a previous publication showed that a 1.5-T magnet did not cause difficulties in classification of ACL tears and healing,16 and hence, these 2 different magnets would allow for equal evaluation of the ACL.
The present study demonstrated that in ACL tears limited to a straight and continuous band, placing physiological mechanical stress on the injured ACL as soon as possible after injury as a conservative treatment helps restore the ACL morphologically and mechanically. Our findings indicate that the human ACL has a high intrinsic healing capacity. In younger patients, however, ACL injuries were more severe and the progress of morphological recovery was poorer than in adult patients. Patients who had good outcomes on the final MRI should be followed up in the future to see what types of sports activities they are able to perform and their rate of reinjury.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Hefti FL, Kress A, Fasel J, et al. Healing of the transected anterior cruciate ligament in the rabbit. J Bone Joint Surg Am. 1991;73:373–383. [PubMed] [Google Scholar]
- 2.Mitsou A, Markakis P, Markaki S, et al. Acute rupture of anterior cruciate ligament: histological study of fifteen cases. Arch Anat Cytol Path. 1990;38:212–214. [PubMed] [Google Scholar]
- 3.O'Donoghue DH, Rockwood CA, Jr, Frank GR, et al. Repair of the anterior cruciate ligament in dogs. J Bone Joint Surg Am. 1966;48:503–519. [PubMed] [Google Scholar]
- 4.Ballmer PM, Jakob RP. The non operative treatment of isolated complete ears of the medial collateral ligament of the Knee: a prospective study. Arch Orthop Trauma Surg. 1988;107:273–276. [DOI] [PubMed] [Google Scholar]
- 5.Ellsasser JC, Reynolds FC, Omohundro JR. The non-operative treatment of collateral ligament injuries of the knee in professional football players: an analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56:1185–1190. [PubMed] [Google Scholar]
- 6.Sandberg R, Balkfors B, Nilsson B, et al. Operative versus non-operative treatment of recent injuries to the ligaments of the knee: a prospective randomized study. J Bone Joint Surg Am. 1987;69:1120–1126. [PubMed] [Google Scholar]
- 7.Woo SL, Inoue M, McGurk-Burleson E, et al. Treatment of the medial collateral ligament injury: II: structure and function of canine knees in response to differing treatment regimens. Am J Sports Med. 1987;15:22–29. [DOI] [PubMed] [Google Scholar]
- 8.Lyon RM, Akeson WH, Amiel D, et al. Ultrastructural differences between the cells of the medical collateral and the anterior cruciate ligaments. Clin Orthop Relat Res. 1991:279–286. [PubMed] [Google Scholar]
- 9.Murray MM, Martin SD, Martin TL, et al. Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am. 2000;82-A:1387–1397. [DOI] [PubMed] [Google Scholar]
- 10.Barrett AM, Craft JA, Replogle WH, et al. Anterior cruciate ligament graft failure: a comparison of graft type based on age and Tegner activity level. Am J Sports Med. 2011;39:2194–2198. [DOI] [PubMed] [Google Scholar]
- 11.Bourke HE, Salmon LJ, Waller A, et al. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40:1985–1992. [DOI] [PubMed] [Google Scholar]
- 12.Hettrich CM, Dunn WR, Reinke EK, et al. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41:1534–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinczewski LA, Lyman J, Salmon LJ, et al. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35:564–574. [DOI] [PubMed] [Google Scholar]
- 14.Ihara H, Miwa M, Takayanagi K, et al. Acute torn meniscus combined with acute cruciate ligament injury: second look arthroscopy after 3-month conservative treatment. Clin Orthop Relat Res. 1994:146–154. [PubMed] [Google Scholar]
- 15.Ihara H, Miwa M, Takayanagi K, et al. Acute tears of the anterior cruciate ligament treated by early protective motion: second-look arthroscopy after 3-month conservative treatment. Orthopaedics International Edition. 1995;3:475–483. [Google Scholar]
- 16.Ihara H, Miwa M, Deya K, et al. MRI of anterior cruciate ligament healing. J Comput Assist Tomogr. 1996;20:317–321. [DOI] [PubMed] [Google Scholar]
- 17.Kapandji IA. The Physiology of The Joints. Vol 2. Edinburgh: Churchill Livingstone; 1970:86–87. [Google Scholar]
- 18.Müller W. The Knee: Form, Function, and Ligament Reconstruction. New York: Springer-Verlag; 1983:9–12. [Google Scholar]
- 19.Kurosaka M, Yoshiya S, Mizuno T, et al. Spontaneous healing of a tear of the anterior cruciate ligament: a report of two cases. J Bone Joint Surg Am. 1998;80:1200–1203. [DOI] [PubMed] [Google Scholar]
- 20.Fujimoto E, Sumen Y, Ochi M, et al. Spontaneous healing of acute anterior cruciate ligament (ACL) injuries—conservative treatment using an extension block soft brace without anterior stabilization. Arch Orthop Trauma Surg. 2002;122:212–216. [DOI] [PubMed] [Google Scholar]
- 21.Costa-Paz M, Ayerza MA, Tanoira I, et al. Spontaneous healing in complete ACL ruptures: a clinical and MRI study. Clin Orthop Relat Res. 2012;470:979–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deie M, Ochi M, Ikuta Y. High intrinsic healing potential of human anterior cruciate ligament: organ culture experiments. Acta Orthop Scand. 1995;66:28–32. [DOI] [PubMed] [Google Scholar]
- 23.Crain EH, Fithian DC, Paxton EW, et al. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005;21:19–24. [DOI] [PubMed] [Google Scholar]
- 24.Adachi N, Ochi M, Uchio Y, et al. Anterior cruciate ligament augmentation under arthroscopy: a minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg. 2000;120:128–133. [DOI] [PubMed] [Google Scholar]
- 25.Lee BI, Kwon SW, Kim JB, et al. Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy. 2008;24:560–568. [DOI] [PubMed] [Google Scholar]
- 26.Muneta T, Koga H, Ju YJ, et al. Remnant volume of anterior cruciate ligament correlates preoperative patients' status and postoperative outcome. Knee Surg Sports Traumatol Arthrosc. 2013;21:906–913. [DOI] [PubMed] [Google Scholar]
- 27.Ahldén M, Samuelsson K, Sernert N, et al. The Swedish national anterior cruciate ligament register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230–2235. [DOI] [PubMed] [Google Scholar]
- 28.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251. [DOI] [PubMed] [Google Scholar]
- 29.Webb JM, Salmon LJ, Leclerc E, et al. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41:2800–2804. [DOI] [PubMed] [Google Scholar]
- 30.Maletis GB, Chen J, Inacio MC, et al. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente Anterior Cruciate Ligament Registry. Am J Sports Med. 2016;44:331–336. [DOI] [PubMed] [Google Scholar]
- 31.Webster KE, Feller JA, Leigh WB, et al. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641–647. [DOI] [PubMed] [Google Scholar]
- 32.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noyes FR, Barber-Westin SD. Neuromuscular retraining intervention programs: do they reduce noncontact anterior cruciate ligament injury rates in adolescent female athletes? Arthroscopy. 2014;30:245–255. [DOI] [PubMed] [Google Scholar]


