Abstract
Probiotics or health-beneficial bacteria have only recently been introduced in dentistry after years of successful use in mainly gastrointestinal disorders. The concept of bacteriotherapy was first introduced in the beginning of 20th century. They are administered in different quantities that allow for colon colonization. These products help in stimulating health promoting flora and also suppressing the pathologic colonization and disease spread. The use of probiotic plays an important aspect in dentistry too, ever since the oral infections occupied the prime spot among the other infections affecting the humans. Probiotics strengthen the immune system to combat allergies, stress, exposure to toxic substances, and other diseases. This review is an attempt to discuss briefly the role of probiotics in oral health.
Keywords: Caries, Lactobacillus, mucosal immunity, periodontal disease, probiotics
Introduction
The human gut contains 10 times more bacteria than anywhere else in the body. The enormous biomass consists of over 400 known bacterial species that leads to various metabolic activities which plays a key role in human health. These microflora activities get disrupted when exposed to toxins in the form of either injudicious use of medicine like antibiotics or contaminated water and food. To revert back to normal activities which have been disrupted due to toxins, use of beneficial bacteria, the probiotics can be one such alternative.[1]
Food and Agriculture Organization and the World Health Organization defined probiotics in 2001 as “live microorganisms which when administered in adequate amounts confer health benefits on the host.”[2]
History
The concept of probiotics have been first proposed by Nobel laureate Elie Metchnikoff, as early as 1908, suggested that the long life of Bulgarian peasants resulted from their utilization of fermented milk products.[3,4] Lilley and Stillwell (1965) introduced the term probiotics. In 1991, Holocombh was the first person to do research on Bifidobacterium bifidum as probiotics species. In 1994, World Health Organization deemed probiotics to be the next – most important immune defense system when commonly prescribed antibiotics are rendered as useless by antibiotic resistance. These incidences of antibiotic resistance opened the door for a new concept of probiotics in medicine and dentistry.[5]
Species and Health Benefits
Probiotics can be varied as yeast, bacteria or molds, but bacterial species are most commonly predominant. The most commonly used probiotics mainly come from two genera Lactobacillus and Bifidobacterium species [Table 1].
Table 1.
Most commonly used probiotics
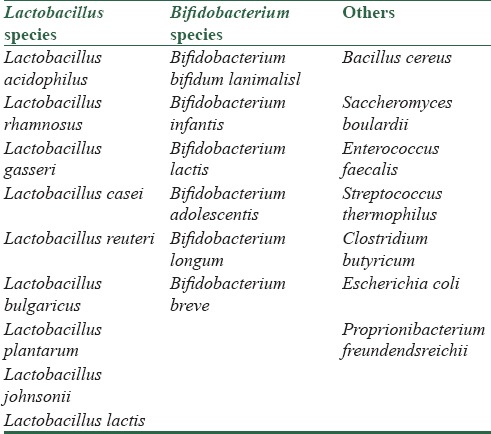
More than 100 species of Lactobacillus have been identified like Lactobacillus acidophilus, Lactobacillus brevis, Lactobacillus casei, Lactobacillus rhamnous, Lactobacillus salivarius which produces digestive enzymes for metabolizing proteins and carbohydrates. The Lactobacillus species help in synthesis of Vitamin B, Vitamin K, and also helps in the breakdown of bile salts. They help in enhancing innate and acquired immunity as well as help in inhibition of Pro-inflammatory mediators.
In dentistry, studies with Lactobacillus rhamnosus GG, and Lactobacillus reuteri have defined their potential role in interacting with Streptococcus mutans by reducing the number of this caries pathogen, thus suggesting a role of probiotics in caries prophylaxis. Similarly, researchers found that probiotic administration reduced oral Candida counts in the elderly-a finding that might offer a new strategy for controlling oral yeast infections. Yet, there is a lack of information regarding the contributions of probiotics in oral health.[6]
Mechanism of Action
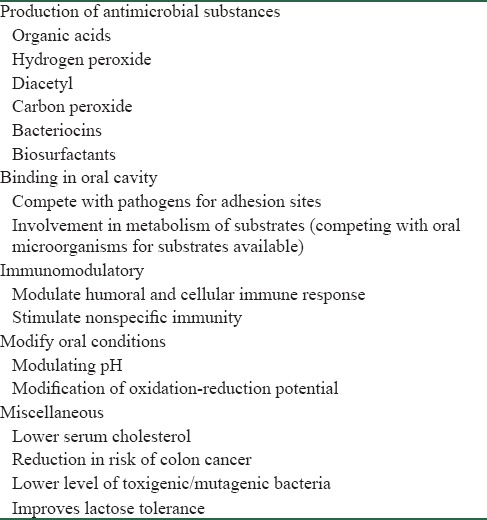
The suggested mechanisms of probiotic action on oral health are drawn entirely from gastrointestinal studies. Regulatory T lymphocytes (Tregs) have been implicated to play a decisive role in reducing inflammation in response to nonpathogenic antigens. Recent studies suggested that toll-like receptor (TLR) pathways may mediate interactions among dendritic cells, T lymphocytes, and mast cells. The interaction between them helps in modulating allergic immune responses.[5] Signaling of TLR by the commensals intestinal microbiota is essential for hemostasis of the intestinal epithelium protection from epithelial injury and plays a critical role in immune regulation. By recognizing pattern recognition molecules from commensal microorganisms, TLRs stimulate the production of epithelial repair factors. This is likely to be an important mechanism through which probiotic act. It has been documented that probiotic can interact with epithelial and immune cells and can alter signal production pathways in the presence or absence of pathogenic bacteria and cytokines. Probiotics play a very important role in day to day life enriching both oral and general health [Table 2].
Table 2.
Probiotics role in oral and general health
Probiotics and Oral Health
In various researches, it has been suggested that probiotic bacteria could also be beneficial to oral health. Species of Lactobacillus and Bifidobacteria inhibit the growth of streptococci and Candida species.
The mechanism of action of probiotic by which they exert their effects may involve from modifying pH, antagonizing pathogens through production of antimicrobial compounds, competing for pathogen binding and receptor sites, stimulating immune modulatory cells to production of lactase. It is also showed that they have the influence to the immune system through several molecular mechanisms.
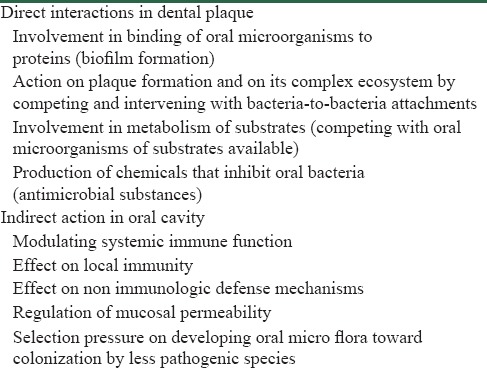
To have a beneficial effect in the oral cavity, probiotics should form a biofilm that acts as a protective lining for oral tissues against oral diseases. Probiotic bacteria's adhesion to oral soft tissues is another aspect that promotes their health effect to the host. Cell adhesion is a complex process which involves contact between the bacterial cell and interaction with surfaces. The epithelial lining of the oral cavity despite its function as a physical barrier, actively participates in the immune response. It has been shown that probiotic bacteria can stimulate local immunity and modulate the inflammatory response. Probiotics action in oral cavity can also be divided into direct action and indirect action [Table 3].
Table 3.
Probiotics action in oral cavity
Clinical Relevance of Probiotics in Oral Diseases
Caries management
The efficacy of probiotics on dental caries has been studied worldwide utilizing different strains species of Lactobacillus like L. rhamnosus GG and L. casei inhibits the growth of oral streptococci. S. mutans is the most common organism that leads to development of caries.[7]
S. mutans have acidogenic properties and it rapidly metabolizes carbohydrates resulting in lowering of pH in the oral cavity that leads to disturbance of hemostasis in the oral microbial community.[8]
Dental caries is an irreversible microbial disease of the calcified tissues of the teeth, characterized by demineralization of the inorganic portion and destruction of the organic substance of the tooth, which results in cavitation. To have a beneficial effect in caries management, probiotics should adhere to dental surfaces. Probiotics must prevent the proliferation of cariogenic bacterial species. Metabolism of carbohydrates results in raising the pH value. This property of probiotics of neutralizing acidic condition, and thus helps in the management of caries is the reason why they are nowadays incorporated in the dairy products.
The first study to examine the efficacy of probiotics (L. rhamnosus GG) on caries was conducted on children in 2011 probiotic milk was able to reduce S. mutans counts at the end of the trial and a significant reduction of caries risk was also observed. The putative caries prophylactic effect of probiotics has been also confirmed by daily intake of cheese containing L. rhamnosus GG and L. rhamnosus LC 705.[9] Bifidobacterium DN-173 010, Bifid bacterium lactis Bb-12, lead to significant S. mutans level reduction.[10]
In a study conducted by Nikawa et al. in 2004, it was clearly shown that the concentration of S. mutans was reduced up to 80% when yoghurt containing L. reuteri was consumed for 2 weeks.[11]
A study was conducted by Meurman in 2005, showed that L. rhamnosus GG inhibit action of S. mutans when pH is low. In vivo studies have also confirmed the role of probiotics in decreasing the Streptococcus mutans count and reducing the risk of dental caries.[6]
Another study was conducted to evaluate the efficacy of L. rhamnosus used in milk products on dental caries by Nase et al. on 594 children aged between 1 and 6 years over a period of 7 months. The authors reported in their study that children aged between 3 and 4 years, consuming milk containing L. rhamnosus, had significant less incidence of dental caries and S. mutans count in saliva than controls.[12] These evidence-based studies both in vivo and in vitro show the efficacy of probiotics in prevention of dental caries.
Candida species management
Candida albicans is an opportunistic fungal pathology found as a normal microflora in the human digestive tract as well as oral microflora. It is just one of approximately 200 species in the genus Candida, but accounts for up to 75% of all Candida infections. Infection caused by Candida may be divided into superficial or systemic. Incidence of Candida infection is found more in older age group.[13] Hatakka et al. were the first person to study the effect of probiotics on the prevalence of oral Candida. The study conducted by Hatakka et al. showed a reduction of C. albicans after taking probiotics (L. rhamnosus GG and Propionibacterium freudenreichii ssp. shermanii JS) in cheese. A probiotic intervention study was done in which it was demonstrated that a significant reduction by 75% of high yeast counts occur in the elderly who were taking probiotics continuously for 16 weeks.[14]
Periodontal Disease
Periodontal disease is classified mainly into two types, that is, gingivitis and periodontitis. Gingivitis is an inflammation of the unattached gingiva, whereas periodontitis is a progressive and destructive disease that affects all supporting tissues of the teeth, including the alveolar bone.
The main pathogenic agents associated with periodontitis are Porphyromonas gingivalis, Treponema denticola, Aggregatibacter actinomycetemcomitans, and Tannerella forsythia. These bacteria have virulent character varying from colonization at the subgingival sites, escape the host's defense system till tissue damage. The persistence of the host's immune response is also a determining factor in progression of the disease.
Various studies worldwide have reported that periodontal disease could also benefit from the oral probiotic intake. This may be due to the probiotic species like Lactobacillus property to inhibit the growth of periodontopathogens for, e.g. P. gingivalis, Prevotella intermedia, and A. actinomycetemcomitans. The result of studies showed that lactobacilli play an important role in the maintenance of balance of oral microflora.
A 14-day intake of L. reuteri led to significant reduction of gingivitis and plaque in patients with moderate to severe gingivitis.[15] This mechanisms of action of L. reuteri could be explained via three possible mechanisms. They are: First, L. reuteri secretes bacteriocins, reuterin, and reutericyclin that inhibit the growth of a wide variety of pathogens; second, L. reuteri has a strong capacity to adhere to the host tissues, and thus competing with pathogenic bacteria; and third, the anti-inflammatory effects of L. reuteri and its property to inhibit the secretion of cytokines could be the reason of this bacterium to have beneficial effects on people with periodontal disease.
Another study showed the efficacy of L. brevis in a group of patients suffering from chronic periodontitis. These patients suffering from chronic periodontitis were asked to suck lozenges containing L. brevis for a period of 4 days. After 4 days, significant improvement was noted in targeted clinical parameters (plaque index, gingival index, bleeding on probing) for all patients with significant reduction in salivary levels of prostaglandin E2 (PGE2) and matrix metalloproteinases (MMPs). The authors emphasized that the anti-inflammatory effects of L. brevis could be due to its capacity to prevent the production of nitric oxide which in turn prevent the release of PGE2 and activation of MMPs.[16]
Another probiotic species, Lactobacillus helveticus, produces short peptides during fermentation of milk that act on osteoblasts and increase osteoblasts activity in bone formation.[17] These bioactive peptides could thereby contribute to reducing the bone resorption associated with periodontitis.
Probiotic intake improved the clinical condition in smokers and reduced salivary lactoferrin at the end of the 8-week trial.[18]
Probiotics strains when given in a concentration of 108 CFU/ml in periodontal dressing have shown to reduce the number of periodontal pathogens like Bacteroides sp., Streptococcus intermedius, Actinomyces sp., and C. albicans.[19] Pharmaceutical companies have marketed probiotics either in the form of lozenges, chewing gums, tablet, etc., in fighting periodontal disease.
Halitosis
Halitosis has several causes which include consumption of particular foods, respiratory tract infections, metabolic disorders, but in most of the cases it is associated with a disturbance of the microflora of the oral cavity. An unbalanced oral microflora has been associated with the production of volatile sulfur compounds (VSCs) including hydrogen sulfide and methanethiol. VSCs are by-products of degradation of salivary and food proteins due to anaerobic bacteria. Various microorganisms causing halitosis generally resides within the oropharynx.
Current treatments of halitosis emphasize on the use of chemical or physical antibacterial regimes to reduce the number of bacteria. Antimicrobial treatment indiscriminately depletes populations of both kinds of bacteria, the problematic and those that have not been implicated in halitosis, but which are important for maintenance of a normal microflora in the oral cavity. However, the result of antimicrobial treatment is only a temporary reduction in halitosis, till the time halitosis causing bacteria again establish themselves.
Streptococcus salivarius produces bacteriocins, which helps in reducing VSCs which in turn help in reducing oral malodor. The administration of S. salivarius K12 either in the form of gum or lozenges reduced levels of VSCs in halitosis patients.[20]
Over years, various studies, have found that use of Weissella cibaria helps in reducing halitosis.
Safety Aspects of Probiotics
The safety issue of probiotics is of concern over years due to the excess probiotic supplementation in different food products. As a safety measure, probiotic bacteria should be nonpathogenic, should not cause any growth-stimulating effect on bacteria causing diarrhea. Probiotics should not be able to transfer antibiotic-resistant genes. Probiotics should maintain microflora ecosystem.
Although probiotics can affect most important caries pathogens, Lactobacillus species together with S. mutans, play a vital role in the development of dental caries. The organic acids produced from dietary carbohydrates are also a main factor in the progression of dental caries. If lactobacilli are administered orally, they establish themselves in the oral environment; their mechanism of action should not support caries induction. Various studies have also highlighted the acidogenic potential of probiotics.
More clinical investigations are required to support the true effectiveness of probiotics in the prevention of oral and dental diseases. Patients having the immunocompromised condition should be cautious with the administration of probiotics as it leads to blood sepsis in such patients. However, in some case patients have developed septic shock too. Many lactobacilli strains are resistant to vancomycin, which raises concern regarding the possible transfer of such resistance to more pathogenic organism, particularly enterococci and Staphylococcus aureus. Bifidobacteria, does not have any side effects except it may, occasionally cause mild diarrhea in children.
Future Trends
Probiotics can be used as a passive local immunization against dental caries. Probiotic bacteria like Escherichia coliif colonized early in newborn; they may stimulate the mucosal immune system to produce antibodies and immunoglobulins. Current findings on the potential use of probiotics against oral conditions are very encouraging. Preliminary data obtained by various studies have been encouraging, but still more research is needed in this field to make probiotics safe and establish it in preventing and treating oral infections.
Conclusion
The concept of probiotics has opened a new horizon on the relationship between diet and oral health. Numerous in vitro and in vivo studies have shown that probiotic bacteria administered in any form are safe for human use to a large extent. Properties of probiotics have made it a subject of interest for various fields such as biotechnology, microbiology, etc. The existence of probiotics in the indigenous oral microflora of humans warrants exploration because these bacteria offer the advantage of being perfectly adapted to the human oral ecosystem.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Salminen MK, Tynkkynen S, Rautelin H, Saxelin M, Vaara M, Ruutu P, et al. Lactobacillus bacteremia during a rapid increase in probiotic use of Lactobacillus rhamnosus GG in Finland. Clin Infect Dis. 2002;35:1155–60. doi: 10.1086/342912. [DOI] [PubMed] [Google Scholar]
- 2.Stamatova I, Meurman JH. Probiotics: Health benefits in the mouth. Am J Dent. 2009;22:329–38. [PubMed] [Google Scholar]
- 3.Mercenier A, Pavan S, Pot B. Probiotics as biotherapeutic agents: Present knowledge and future prospects. Curr Pharm Des. 2003;9:175–91. doi: 10.2174/1381612033392224. [DOI] [PubMed] [Google Scholar]
- 4.Tannock GW. Probiotics: Time for a dose of realism. Curr Issues Intest Microbiol. 2003;4:33–42. [PubMed] [Google Scholar]
- 5.Boden EK, Snapper SB. Regulatory T cells in inflammatory bowel disease. Curr Opin Gastroenterol. 2008;24:733–41. doi: 10.1097/mog.0b013e328311f26e. [DOI] [PubMed] [Google Scholar]
- 6.Meurman JH. Probiotics: Do they have a role in oral medicine and dentistry? Eur J Oral Sci. 2005;113:188–96. doi: 10.1111/j.1600-0722.2005.00191.x. [DOI] [PubMed] [Google Scholar]
- 7.Beighton D. The complex oral microflora of high-risk individuals and groups and its role in the caries process. Community Dent Oral Epidemiol. 2005;33:248–55. doi: 10.1111/j.1600-0528.2005.00232.x. [DOI] [PubMed] [Google Scholar]
- 8.Hedberg M, Hasslöf P, Sjöström I, Twetman S, Stecksén-Blicks C. Sugar fermentation in probiotic bacteria – An in vitro study. Oral Microbiol Immunol. 2008;23:482–5. doi: 10.1111/j.1399-302X.2008.00457.x. [DOI] [PubMed] [Google Scholar]
- 9.Ahola AJ, Yli-Knuuttila H, Suomalainen T, Poussa T, Ahlström A, Meurman JH, et al. Short-term consumption of probiotic-containing cheese and its effect on dental caries risk factors. Arch Oral Biol. 2002;47:799–804. doi: 10.1016/s0003-9969(02)00112-7. [DOI] [PubMed] [Google Scholar]
- 10.Caglar E, Kuscu OO, Selvi Kuvvetli S, Kavaloglu Cildir S, Sandalli N, Twetman S. Short-term effect of ice-cream containing Bifidobacterium lactis Bb-12 on the number of salivary mutans streptococci and lactobacilli. Acta Odontol Scand. 2008;66:154–8. doi: 10.1080/00016350802089467. [DOI] [PubMed] [Google Scholar]
- 11.Nikawa H, Makihira S, Fukushima H, Nishimura H, Ozaki Y, Ishida K, et al. Lactobacillus reuteri in bovine milk fermented decreases the oral carriage of mutans streptococci. Int J Food Microbiol. 2004;95:219–23. doi: 10.1016/j.ijfoodmicro.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 12.Näse L, Hatakka K, Savilahti E, Saxelin M, Pönkä A, Poussa T, et al. Effect of long-term consumption of a probiotic bacterium, Lactobacillus rhamnosus GG, in milk on dental caries and caries risk in children. Caries Res. 2001;35:412–20. doi: 10.1159/000047484. [DOI] [PubMed] [Google Scholar]
- 13.Parker RB. Probiotics, the other half of the antibiotic story. Anim Nutr Health. 1974;29:4–8. [Google Scholar]
- 14.Hatakka K, Ahola AJ, Yli-Knuuttila H, Richardson M, Poussa T, Meurman JH, et al. Probiotics reduce the prevalence of oral Candida in the elderly – A randomized controlled trial. J Dent Res. 2007;86:125–30. doi: 10.1177/154405910708600204. [DOI] [PubMed] [Google Scholar]
- 15.Krasse P, Carlsson B, Dahl C, Paulsson A, Nilsson A, Sinkiewicz G. Decreased gum bleeding and reduced gingivitis by the probiotic Lactobacillus reuteri. Swed Dent J. 2006;30:55–60. [PubMed] [Google Scholar]
- 16.DN, Bizzini F, Perilli MG, Polimeni A, Trinchieri V, Amicosante G, et al. Anti-inflammatory effects of Lactobacillus brevis (CD2) on periodontal disease. Oral Dis. 2007;13:376–85. doi: 10.1111/j.1601-0825.2006.01291.x. [DOI] [PubMed] [Google Scholar]
- 17.Narva M, Halleen J, Väänänen K, Korpela R. Effects of Lactobacillus helveticus fermented milk on bone cells in vitro. Life Sci. 2004;75:1727–34. doi: 10.1016/j.lfs.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Shimauchi H, Mayanagi G, Nakaya S, Minamibuchi M, Ito Y, Yamaki K, et al. Improvement of periodontal condition by probiotics with Lactobacillus salivarius WB21: A randomized, double-blind, placebo-controlled study. J Clin Periodontol. 2008;35:897–905. doi: 10.1111/j.1600-051X.2008.01306.x. [DOI] [PubMed] [Google Scholar]
- 19.Volozhin AI, Il’in VK, Maksimovskii IuM, Sidorenko AB, Istranov LP, Tsarev VN, et al. Development and use of periodontal dressing of collagen and Lactobacillus casei 37 cell suspension in combined treatment of periodontal disease of inflammatory origin (a microbiological study) Stomatologiia (Mosk) 2004;83:6–8. [PubMed] [Google Scholar]
- 20.Burton JP, Chilcott CN, Moore CJ, Speiser G, Tagg JR. A preliminary study of the effect of probiotic Streptococcus salivarius K12 on oral malodour parameters. J Appl Microbiol. 2006;100:754–64. doi: 10.1111/j.1365-2672.2006.02837.x. [DOI] [PubMed] [Google Scholar]


