Abstract
Monoclonal antibodies that block immune regulatory proteins such as programmed death-1 (PD-1) have demonstrated remarkable efficacy in controlling the growth of multiple tumor types. Unresectable or metastatic basal cell carcinoma, however, has largely gone untested. Because PD-Ligand-1 (PD-L1) expression in other tumor types has been associated with response to anti-PD-1, we investigated the expression of PD-L1 and its association with PD-1 expression in the basal cell carcinoma tumor microenvironment. Among 40 basal cell carcinoma specimens, 9/40 (22%) demonstrated PD-L1 expression on tumor cells, and 33/40 (82%) demonstrated PD-L1 expression on tumor-infiltrating lymphocytes and associated macrophages. PD-L1 was observed in close geographic association to PD-1+ tumor infiltrating lymphocytes. Additionally, we present, here, the first report of an objective anti-tumor response to pembrolizumab (anti-PD-1) in a patient with metastatic PD-L1 (+) basal cell carcinoma, whose disease had previously progressed through hedgehog pathway-directed therapy. The patient remains in a partial response 14 months after initiation of therapy. Taken together, our findings provide a rationale for testing anti-PD-1 therapy in patients with advanced basal cell carcinoma, either as initial treatment or after acquired resistance to hedgehog pathway inhibition.
Keywords: PD-L1, Anti-PD-1, Basal cell carcinoma, Hedgehog, Pembrolizumab
Background
Basal cell carcinoma (BCC) is the most common human cancer, though most tumors are eradicated using locally-directed therapies [1]. In the small minority of patients that develop surgically unresectable locally-advanced or metastatic disease, currently available systemic therapies, such as agents that curtail aberrant signaling along the hedgehog (Hh) pathway, are frequently ineffective in bringing about durable anti-tumor responses [2–6].
Over the past several years, monoclonal antibodies that block immune checkpoint proteins (e.g., anti-programmed death-1 (PD-1), PD-Ligand-1 (PD-L1)), have demonstrated remarkable efficacy in controlling the growth of multiple tumor types [7]. In several studies, the expression of PD-L1 – a major ligand of PD-1 – in the tumor microenvironment has been associated with an increased likelihood of an anti-tumor response to anti-PD-1. BCC, however, has largely gone untested and little is known about the expression of immunoregulatory molecules in the BCC microenvironment or about the capacity of PD-1-pathway-directed therapies to trigger an effective anti-tumor response [8–10].
In the current study, we characterized PD-L1 and PD-1 expression patterns in the tumor microenvironment of 40 archived BCC specimens. Additionally, we studied a pre-treatment tumor specimen and clinical and radiographic response characteristics from one patient who experienced a durable, objective anti-tumor response to pembrolizumab (anti-PD-1) monotherapy.
Materials and methods
Following Institutional Review Board approval, 40 surgical pathology specimens from 40 unique patients with BCC were identified from the Johns Hopkins Hospital surgical pathology archives. Slides were reviewed by a board-certified dermatopathologist (JMT) to confirm the diagnosis, and one representative paraffin block was chosen for PD-L1 and PD-1 immunohistochemistry (IHC). PD-L1 expression was assessed using the murine anti-human PD-L1 monoclonal antibody 5H1 (from Lieping Chen, Yale University, New Haven, CT) at a concentration of 0.1 μg/mL, as previously described [11]. PD-L1 expression on tumor cells and immune cells were scored separately. Cases demonstrating at least 5% membranous (cell surface) expression of PD-L1 were considered positive. Immunohistochemistry for PD-1 was performed using a primary mouse anti-human mAb (clone Nat105, at 1:1000), following an antigen retrieval of 10 min in citrate buffer, pH 6.0 at 120 C. A secondary anti-mouse IgG1 antibody was used at 1.0 μg/ml. Amplification was performed by using Perkin Elmer biotin TSA, Dako streptavidin HRP and then visualized by DAB staining. The geographic association between PD-L1 and PD-1 expression in the tumor microenvironment was also assessed. For the specimen from the patient demonstrating a response to anti-PD-1, an extended panel of IHC markers (CD4, CD8, TIA-1 and CD68) was performed according to standard automated methods.
Results
Forty specimens from 40 unique patients were evaluable. All were primary lesions that were locally aggressive or recurrent. The tumors ranged in size from 2 to15 cm in greatest dimension. Nine of forty (22%) demonstrated PD-L1 expression on tumor cells, and 33/40 (82%) demonstrated PD-L1 expression on tumor-infiltrating lymphocytes (TIL) and associated macrophages. All (40/40, 100%) of cases had varying degrees of either true TIL present or lymphocytes present in the immediate extratumoral stroma. PD-1 expression was seen on lymphocytes in the tumor microenvironment of each case, including the 16/40 (40%) cases that had only rare lymphocytes present. All (33/33) cases with PD-L1 expression on tumor or macrophages showed an association with PD-1+ TIL (Fig. 1). There were no cases that demonstrated constitutive PD-L1 expression, independent of TIL [11].
Fig. 1.
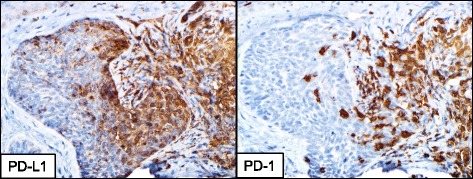
Geographic co-localization of PD-L1+ tumor cells and associated immune cells with PD-1+ infiltrating immune cells in BCC. PD-1, programmed death-1; PD-L1, programmed death ligand-1. 200× original magnification, all panels
Case presentation
A 67-year-old woman presented in 2007 with a large BCC of the skin of the right posterior neck. She underwent wide local excision followed by adjuvant electron radiotherapy. In 2011 she developed a surgically unresectable recurrence and began therapy on a phase 1 clinical trial of the Hh pathway inhibitor saridegib (IPI-926; clinicaltrials.gov ID# NCT00761696). Although radiographically her best overall response per RECIST criteria was stable disease, clinically, her symptoms related to tumor growth improved dramatically for several months, then worsened about 12 months after having initiated therapy.
She then pursued treatment on a phase 1 clinical trial of AZD6244 (MEK inhibitor) and IMC-A12 (a fully human IgG1 monoclonal antibody directed against insulin-like growth factor-1 receptor (IGF-1R); clinicaltrials.gov ID# NCT01061749). Her disease progressed within 6 months, requiring palliative radiotherapy.
In late 2014 her neck pain increased and CT scans demonstrated multiple lung metastases. Re-initiation of Hh inhibition was considered but, based on previous clinical experience, the likelihood of anti-tumor activity was felt to be low [12]. The patient preferred to avoid the toxicity associated with standard cytotoxic chemotherapy.
Although we had not yet assessed PD-L1 expression in this patient’s tumor, support for the use of PD-1 pathway-directed therapy came from pre-clinical studies demonstrating that BCC typically caries a high genetic mutation burden, a characteristic associated with response to PD-1 blockade in other tumor types [13, 14]. Additionally, BCCs undergoing spontaneous regression (presumably immune-mediated) contain elevated levels of T-helper type-1 (Th1) cytokines (e.g., interferon gamma) and infiltrating activated T cells [15, 16].
Pembrolizumab (anti-PD-1) was administered at 2 mg/kg IV every 3 weeks beginning in December 2015. The following month, the patient reported that her pain medication requirement had decreased substantially. CT scans performed 4 months into therapy demonstrated a partial response (PR) to therapy per RECIST 1.1 criteria (Fig. 2). Fourteen months into therapy, a PR is ongoing. The patient has experienced subclinical hypothyroidism, possibly drug-related.
Fig. 2.
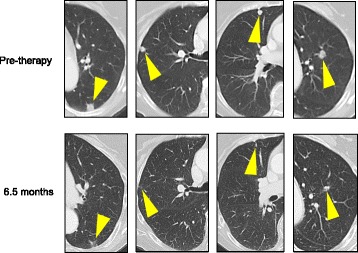
Partial response of metastatic basal cell carcinoma to pembrolizumab (anti-PD-1). Computed tomography (CT) scans performed pre-therapy (top row) and 6.5 months after initiating pembrolizumab (anti-PD-1, bottom row) demonstrate regression of basal cell carcinoma lung metastases. Yellow arrowheads indicate sites of metastases
Immunohistochemical evaluation of the patient’s pre-treatment BCC demonstrated PD-L1 expression on immune cells but not tumor cells (Fig. 3). This immune infiltrate was composed of a mixture of CD4 and CD8+ T cells as well as CD68+ macrophages. Approximately 50% of the lymphocytes present expressed PD-1. Immunohistochemical stains for HLA-I and II were not performed, as they are not yet fully validated in our laboratories.
Fig. 3.
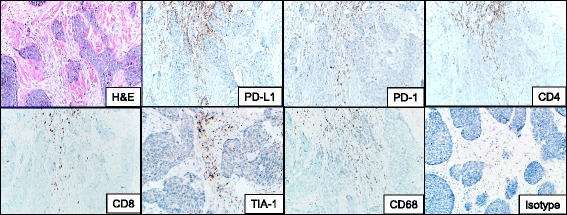
Immune elements in the microenvironment of a pre-treatment basal cell carcinoma from a patient who responded to anti-PD-1 therapy. The immune infiltrate abuts the tumor islands and is composed of a mixture of CD4 and CD8+ T-cells at a ratio of approximately 2:1. The CD8 cells are cytotoxic, as supported by the punctate cytoplasmic TIA-1 immunostaining. The lymphocytic infiltrate is accompanied by CD68+ macrophages. PD-1 is seen on approximately half of the lymphocytes present, and is immediately adjacent to PD-L1 expression in the tumor microenvironment, consistent with an immune microenvironment primed for potential response to PD-1/PD-L1 checkpoint blockade. PD-L1 is expressed predominantly on immune cells, rather than tumor cells in this example. H & E, hematoxylin and eosin, PD-(L)1, programmed death-(Ligand)1. 200× original magnification, all panels
Discussion
The biology of BCC presents opportunities for both immune-mediated tumor regression and escape from immune surveillance. Factors that may increase BCC’s immunogenicity include its high rate of cancer-testis antigen expression [17], copious numbers of tumor-infiltrating CD8+ T cells [18], and a genetic mutational burden which is among the highest reported in any human cancer type [14, 19–21]. Indeed, many of the cancers against which immune checkpoint therapy is effective (e.g., melanoma, non-virus-associated Merkel cell carcinoma and microsatellite unstable neoplasms) harbor large genetic mutational loads [22, 23]. A recent case report from Ikeda and colleagues describes a near-complete response to nivolumab (anti-PD-1) in a patient with metastatic BCC whose tumor carried a particularly high mutational burden (450 mutations per megabase) [9]. Conversely, BCCs demonstrate low levels of MHC-I expression [24] and contain abundant regulatory T cells in the tumor microenvironment [18], both of which may suppress anti-tumor immunity and allow for immune escape.
The administration of various anti-neoplastic therapies may alter the immunological profile in BCCs. For example, application of imiquimod to BCC results in upregulation of MHC-I expression [17]. Likewise, administration of the Hh pathway inhibitors vismodegib or sonidegib to patients with BCC triggers increases in tumor-infiltrating T cells and tumor cell MHC-I expression [25]. Despite these seemingly beneficial immunological effects, Hh pathway inhibitors have demonstrated sub-optimal objective response rates of 15–60%, with median durations of response often <12 months [3, 4, 6, 26].
Taken together, these findings suggest that appropriately-activated immune responses directed against BCC may control tumor growth. In the current study, we present a pre-clinical rationale for, and clinical evidence of, potential long-term anti-tumor immunity after administration of anti-PD-1, an immune checkpoint blocker. Agents targeting immune checkpoints represent “common denominator” therapies which can bring about durable anti-tumor responses in patients with multiple tumor types [27]. PD-L1 expression on tumor cells and immune cells has been shown to enrich for response to anti-PD-1/L1 in various solid malignancies [7]. Here, we demonstrate prominent expression of two of the checkpoint pathway’s component molecules, PD-1 and PD-L1, in BCC. Moreover, the cases in the current series exhibit PD-1 and PD-L1 expression in close geographic proximity to each other, a pattern consistent with adaptive (i.e., interferon-gamma-mediated) immune resistance [11]. The adaptive pattern of PD-L1 expression in the tumor microenvironment can be further accentuated by amplification of the 9p24.1 locus, which contains PD-L1, −L2 and JAK2, the latter of which is an interferon-gamma-responsive element. This alteration was first described in Hodgkin lymphoma [28], then recently illustrated in a case report of a patient with BCC whose tumors regressed after administration of anti-PD-1 [9]. Importantly, mutational burden and PD-1/PD-L1 expression in the tumor microenvironment do not appear to be directly linked [29]. Thus, the current report highlights a novel biomarker suggesting potential efficacy of anti-PD-1 in patients with advanced BCC.
Of note, the immune marker panel used in our study was intended to support the aim of our investigation: to explore expression of molecules comprising the PD-L1 axis in BCC as a rationale for clinical application of anti-PD-1/PD-L1 agents. Development of an optimized multiplex biomarker panel for BCC will likely include assessment of additional immunoregulatory elements (e.g., HLA-I and -II expression status), and will require a large cohort of patients.
In conclusion, our laboratory and clinical findings suggest that PD-1 blockade should be considered as salvage therapy in patients with advanced BCC whose disease has progressed after standard Hh pathway inhibition. Our results also provide a rationale for ongoing clinical trials of PD-1 pathway blockade agents in patients with advanced BCC, either as first-line therapy or in combination with or after treatment with Hh inhibitors (e.g., NCT02690948).
Acknowledgements
The authors thank Susan Markus, RN for helpful discussions.
Funding
This work is supported by Stand Up to Cancer (EJL, JMT), The Barney Foundation (EJL, WHS, JMT), the Dermatology Foundation (JMT), grants R01 (CA142779) (JMT) and P30 CA006973 (EJL, WHS, JMT) from the National Cancer Institute, and the Bloomberg ~ Kimmel Institute for Cancer Immunotherapy (EJL, WHS, JMT).
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Authors’ contributions
EJL contributed to the conception and coordination of the study, data acquisition, drafting and final revision of the manuscript. MTL participated in data acquisition and final revision of the manuscript. AO participated in data acquisition and final revision of the manuscript. JE participated in data acquisition and final revision of the manuscript. HX participated in data acquisition and final revision of the manuscript. PB participated in data acquisition and final revision of the manuscript. MS participated in data acquisition and final revision of the manuscript. WHS participated in data acquisition and final revision of the manuscript. JMT contributed to the conception and coordination of the study, data acquisition, drafting and final revision of the manuscript. All authors read and approved the manuscript.
Competing interests
EJL: consultant for Bristol-Myers Squibb, EMD Serono, Merck, Novartis; research funding from Bristol-Myers Squibb, Merck
PB: consultant for Bristol-Myers Squibb
WHS: consultant for Bristol-Myers Squibb, Merck, Novartis, Castle Biosciences
JMT: consultant for Bristol-Myers Squibb, Merck, AstraZeneca; research funding from Bristol-Myers Squibb
Consent for publication
Written informed consent was obtained from the patient described in this manuscript. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics approval and consent to participate
Evaluation of archived pathology specimens described in this manuscript is covered under a study approved by the Johns Hopkins University Institutional Review Board which does not require individual patient consent. No consent was needed for the patient described in the case report, as treatment was not administered as part of a clinical investigation.
Abbreviations
- BCC
Basal cell carcinoma
- Hh
Hedgehog
- PD-1
Programmed Death-1
- PD-L1
Programmed Death Ligand-1
Contributor Information
Evan J. Lipson, Phone: 410-502-5977, Email: evanlipson@jhmi.edu
Mohammed T. Lilo, Email: mlilo1@jhmi.edu
Aleksandra Ogurtsova, Email: aogurts1@jhmi.edu.
Jessica Esandrio, Email: jesandr1@jhmi.edu.
Haiying Xu, Email: hxu12@jhmi.edu.
Patricia Brothers, Email: pbrothe1@jhmi.edu.
Megan Schollenberger, Email: mscholl3@jhmi.edu.
William H. Sharfman, Email: sharfwi@jhmi.edu
Janis M. Taube, Email: jtaube1@jhmi.edu
References
- 1.Lo JS, Snow SN, Reizner GT, Mohs FE, Larson PO, Hruza GJ. Metastatic basal cell carcinoma: Report of twelve cases with a review of the literature. J Am Acad Dermatol. 1991;24:715–9. doi: 10.1016/0190-9622(91)70108-E. [DOI] [PubMed] [Google Scholar]
- 2.Chang ALS, Oro AE. Initial assessment of tumor regrowth after vismodegib in advanced basal cell carcinoma. Arch Dermatol. 2012;148:1324–5. doi: 10.1001/archdermatol.2012.2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sekulic A, Migden MR, Oro AE, Dirix L, Lewis KD, Hainsworth JD, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366:2171–9. doi: 10.1056/NEJMoa1113713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LoRusso PM, Rudin CM, Reddy JC, Tibes R, Weiss GJ, Borad MJ, et al. Phase I trial of hedgehog pathway inhibitor vismodegib (GDC-0449) in patients with refractory, locally advanced or metastatic solid tumors. Clin Cancer Res. 2011;17:2502–11. doi: 10.1158/1078-0432.CCR-10-2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodon J, Tawbi HA, Thomas AL, Stoller RG, Turtschi CP, Baselga J, et al. A phase I, multicenter, open-label, first-in-human, dose-escalation study of the oral smoothened inhibitor sonidegib (LDE225) in patients with advanced solid tumors. Clin Cancer Res. 2014;20:1900–9. doi: 10.1158/1078-0432.CCR-13-1710. [DOI] [PubMed] [Google Scholar]
- 6.Von Hoff DD, LoRusso PM, Rudin CM, Reddy JC, Yauch RL, Tibes R, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164–72. doi: 10.1056/NEJMoa0905360. [DOI] [PubMed] [Google Scholar]
- 7.Lipson EJ, Forde PM, Hammers H, Emens LA, Taube JM, Topalian SL. Antagonists of PD-1 and PD-L1 in cancer treatment. Semin Oncol. 2015;42:587–600. doi: 10.1053/j.seminoncol.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Winkler JK, Schneiderbauer R, Bender C, Sedlaczek O, Frohling S, Penzel R, et al. Anti-PD-1 therapy in nonmelanoma skin cancer. Br J Dermatol. 2016. doi:10.1111/bjd.14664. [DOI] [PubMed]
- 9.Ikeda S, Goodman AM, Cohen PR, Jensen TJ, Ellison CK, Frampton G, et al. Metastatic basal cell carcinoma with amplification of PD-L1: Exceptional response to anti-PD1 therapy. NPJ Genom Med. 2016;1:16037. doi: 10.1038/npjgenmed.2016.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falchook G, Leidner R, Stankevich E, Piening B, Bifulco C, Lowy I, et al. Responses of metastatic basal cell and cutaneous squamous cell carcinomas to anti-PD1 monoclonal antibody REGN2810. J Immunother Cancer. 2016;4(1):70. doi: 10.1186/s40425-016-0176-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taube JM, Anders RA, Young GD, Xu H, Sharma R, McMiller TL, et al. Co-localization of inflammatory response with B7-H1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med. 2012;4:127ra37. doi: 10.1126/scitranslmed.3003689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Danial C, Sarin KY, Oro AE, Chang AL. An investigator-initiated open-label trial of sonidegib in advanced basal cell carcinoma patients resistant to vismodegib. Clin Cancer Res. 2016;22:1325–9. doi: 10.1158/1078-0432.CCR-15-1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. Cancer immunology. mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–8. doi: 10.1126/science.aaa1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jayaraman SS, Rayhan DJ, Hazany S, Kolodney MS. Mutational landscape of basal cell carcinomas by whole-exome sequencing. J Invest Dermatol. 2014;134:213–20. doi: 10.1038/jid.2013.276. [DOI] [PubMed] [Google Scholar]
- 15.Wong D, Bishop G, Lowes M, Cooke B, Barnetson R, Halliday G. Cytokine profiles in spontaneously regressing basal cell carcinomas. Br J Dermatol. 2000;143:91–8. doi: 10.1046/j.1365-2133.2000.03596.x. [DOI] [PubMed] [Google Scholar]
- 16.Hunt M, Halliday G, Dea W, Cooke B, Barnetson RS. Regression in basal cell carcinoma: An immunohistochemical analysis. Br J Dermatol. 1994;130:1–8. doi: 10.1111/j.1365-2133.1994.tb06873.x. [DOI] [PubMed] [Google Scholar]
- 17.Walter A, Barysch MJ, Behnke S, Dziunycz P, Schmid B, Ritter E, et al. Cancer-testis antigens and immunosurveillance in human cutaneous squamous cell and basal cell carcinomas. Clin Cancer Res. 2010;16:3562–70. doi: 10.1158/1078-0432.CCR-09-3136. [DOI] [PubMed] [Google Scholar]
- 18.Kaporis HG, Guttman-Yassky E, Lowes MA, Haider AS, Fuentes-Duculan J, Darabi K, et al. Human basal cell carcinoma is associated with Foxp3 & plus; T cells in a Th2 dominant microenvironment. J Invest Dermatol. 2007;127:2391–8. doi: 10.1038/sj.jid.5700884. [DOI] [PubMed] [Google Scholar]
- 19.Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, et al. Signatures of mutational processes in human cancer. Nature. 2013;500:415–21. doi: 10.1038/nature12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bonilla X, Parmentier L, King B, Bezrukov F, Kaya G, Zoete V, et al. Genomic analysis identifies new drivers and progression pathways in skin basal cell carcinoma. Nat Genet. 2016;48:398–406. doi: 10.1038/ng.3525. [DOI] [PubMed] [Google Scholar]
- 21.Sharpe HJ, Pau G, Dijkgraaf GJ, Basset-Seguin N, Modrusan Z, Januario T, et al. Genomic analysis of smoothened inhibitor resistance in basal cell carcinoma. Cancer Cell. 2015;27:327–41. doi: 10.1016/j.ccell.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le DT, Azad NS, Laheru D, Browner IS, Wang H, Uram JN, et al. Phase 2 study of programmed death-1 antibody (anti-PD-1, MK-3475) in patients with microsatellite unstable (MSI) tumors. J Clin Oncol. 2014;32(15_suppl):TPS3128. [Google Scholar]
- 23.Nghiem PT, Bhatia S, Lipson EJ, Kudchadkar RR, Miller NJ, Annamalai L, et al. PD-1 blockade with pembrolizumab in advanced merkel-cell carcinoma. N Engl J Med. 2016;374:2542–52. doi: 10.1056/NEJMoa1603702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cabrera T, Garrido V, Concha A, Martin J, Esquivias J, Oliva MR, et al. HLA molecules in basal cell carcinoma of the skin. Immunobiology. 1992;185:440–52. doi: 10.1016/S0171-2985(11)80086-0. [DOI] [PubMed] [Google Scholar]
- 25.Otsuka A, Dreier J, Cheng PF, Nageli M, Lehmann H, Felderer L, et al. Hedgehog pathway inhibitors promote adaptive immune responses in basal cell carcinoma. Clin Cancer Res. 2015;21:1289–97. doi: 10.1158/1078-0432.CCR-14-2110. [DOI] [PubMed] [Google Scholar]
- 26.Migden MR, Guminski A, Gutzmer R, Dirix L, Lewis KD, Combemale P, et al. Treatment with two different doses of sonidegib in patients with locally advanced or metastatic basal cell carcinoma (BOLT): A multicentre, randomised, double-blind phase 2 trial. Lancet Oncol. 2015;16:716–28. doi: 10.1016/S1470-2045(15)70100-2. [DOI] [PubMed] [Google Scholar]
- 27.Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–61. doi: 10.1016/j.ccell.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green MR, Monti S, Rodig SJ, Juszczynski P, Currie T, O’Donnell E, et al. Integrative analysis reveals selective 9p24.1 amplification, increased PD-1 ligand expression, and further induction via JAK2 in nodular sclerosing hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood. 2010;116:3268–77. doi: 10.1182/blood-2010-05-282780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Danilova L, Wang H, Sunshine J, Kaunitz GJ, Cottrell TR, Xu H, et al. Association of PD-1/PD-L axis expression with cytolytic activity, mutational load, and prognosis in melanoma and other solid tumors. Proc Natl Acad Sci U S A. 2016;113:E7769–77. doi: 10.1073/pnas.1607836113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.


