Abstract
Patients are increasingly being asked for feedback about their healthcare experiences. However, healthcare staff often find it difficult to act on this feedback in order to make improvements to services. This paper draws upon notions of legitimacy and readiness to develop a conceptual framework (Patient Feedback Response Framework – PFRF) which outlines why staff may find it problematic to respond to patient feedback.
A large qualitative study was conducted with 17 ward based teams between 2013 and 2014, across three hospital Trusts in the North of England. This was a process evaluation of a wider study where ward staff were encouraged to make action plans based on patient feedback. We focus on three methods here: i) examination of taped discussion between ward staff during action planning meetings ii) facilitators notes of these meetings iii) telephone interviews with staff focusing on whether action plans had been achieved six months later. Analysis employed an abductive approach.
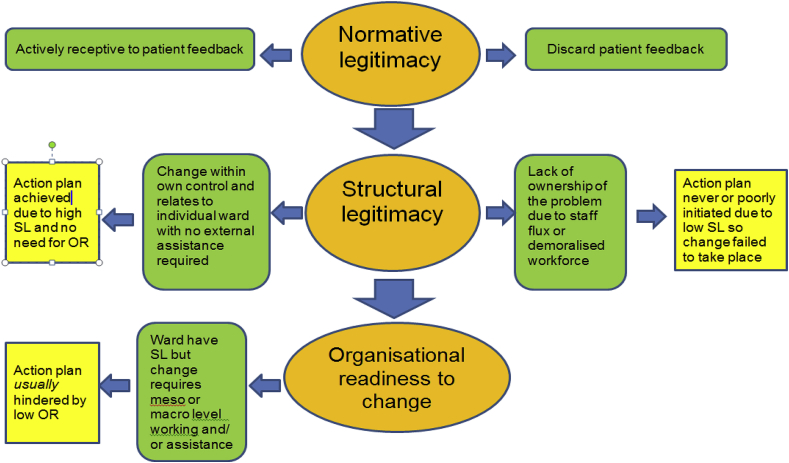
Through the development of the PFRF, we found that making changes based on patient feedback is a complex multi-tiered process and not something that ward staff can simply ‘do’. First, staff must exhibit normative legitimacy – the belief that listening to patients is a worthwhile exercise. Second, structural legitimacy has to be in place – ward teams need adequate autonomy, ownership and resource to enact change. Some ward teams are able to make improvements within their immediate control and environment. Third, for those staff who require interdepartmental co-operation or high level assistance to achieve change, organisational readiness must exist at the level of the hospital otherwise improvement will rarely be enacted. Case studies drawn from our empirical data demonstrate the above. It is only when appropriate levels of individual and organisational capacity to change exist, that patient feedback is likely to be acted upon to improve services.
Keywords: United Kingdom, Patient feedback, Patient experience, Patient safety, Qualitative research, Health services organisations, Health services research
Highlights
-
•
Hospital staff find it difficult to make improvements based on patient feedback.
-
•
We propose a conceptual framework - Patient Feedback Response Framework.
-
•
Draws on notions of normative/ structural legitimacy and organisational readiness.
-
•
Weak structural legitimacy and lack of organisational readiness are problematic.
-
•
Individual and organisational capacity for change must align to achieve improvement.
1. Introduction
The last decade has witnessed an explosion in the collection of feedback from patients about their opinion of healthcare services throughout many countries across the world. This activity had largely taken place in the United States, Europe (particularly the UK) and Australia (Davidson et al., 2016, Edwards et al., 2015, Gleeson et al., 2016). The methods used can be both quantitative and qualitative and range from the level of large, national surveys through to the micro level of local patient narratives of their journey through the hospital system (Health Foundation, 2013). Other methods of gathering patient feedback may include: focus groups with patients, patient panels, official complaints and compliments, feedback delivered in real time via postcards or electronic kiosks, postal and online surveys. Recently, social media and websites such as Patient Opinion in the UK allow patients to give feedback in an unsolicited manner. Patient feedback through all the above channels, and many more besides, can relate to several important aspects of a patient’s care; most noticeably patient experience, safety and quality. Integral to a high quality patient experience in hospital are: efficient processes, good clinical outcomes, the physical environment, how patients felt about the care they received and how staff interacted with them (NHS Confederation, 2010). A growing international body of evidence suggests that patient experience, safety and clinical effectiveness are inextricably linked (Doyle et al., 2013).
Despite the wealth of feedback now available to healthcare services, there is little evidence that this feedback has led to improvement in the quality of healthcare (Coulter et al., 2014). A review of the UK National Inpatient Survey concluded that “simply providing hospitals with patient feedback does not automatically have a positive effect on quality standards” (DeCourcy et al., 2012). Yet, there appears to be an assumption that merely giving staff feedback from their patients will drive ward based improvements (Reeves et al., 2013), with the complexity of how hospital staff manage to turn feedback into concrete improvements largely neglected. Indeed, the emphasis until recently has been on data collection in and of itself rather than data being used to improve the quality of care (Reeves et al., 2013).
Several reasons may explain why change could be difficult for clinical staff to achieve in relation to working on issues which patients have identified. Using data sources to change practice demands creativity and skills from staff who may have had little or no training in quality improvement and currently there is a tendency to present staff with data and expect change to happen as a result (Gkeredakis et al., 2011). Clinicians may be mistrustful of the data, defensive, merely lack interest (Asprey et al., 2013) or may not wish to claim issues as their own (Robert and Cornwell, 2013). Cornwell (2015) writes that improvement work based on patient experience data often draws attention to the attitudes and behaviours of frontline staff, which can cause anxiety amongst individuals. Until recently, there has been an unspoken but widely held belief by some healthcare professionals that providing a good patient experience is considered perhaps a luxury or ‘nice but not necessary’ (NHS Confederation, 2010).
At the level of the healthcare organisation, meso and macro factors come into play which may explain why it is difficult to enact change based on patient feedback. Dixon-Woods et al. (2013) articulate the difference between ‘problem sensing’ and ‘comfort seeking’ behaviours by hospitals. Problem sensing involves seeking out weaknesses in organisational systems by making use of multiple sources of data, including soft intelligence. Comfort seeking requires reassurance that all is well and that the organisation looks ‘good’ externally. When a hospital organisation tips towards comfort seeking behaviours, “data collection activities were prone to being treated by sharp end staff as wearisome and fruitless accountability exercises”. The relationship between how frontline ward staff and executive board members consider patient feedback is said to be problematic in some organisations. A focus on surveys and targets may have “contributed to a tick box or compliance mentality” lulling hospital boards into thinking they were paying attention to patient experience (Robert and Cornwell, 2013) when the situation on the ground is somewhat different. Furthermore, there is said to be a ‘chasm’ between hospital management and frontline clinicians with the former investing heavily in providing the means to collect patient feedback but providing little structure in how the latter can act on this data to improve patient experience (Rozenblum et al., 2013). It has been said that an ever growing battery of targets, tools, metrics and inspections simply allows organisations to measure how compassionate their staff are rather than the task of changing the culture to enable more compassionate care to be delivered (Locock et al., 2014). Expansion of metrics to measure quality, safety and experience could become counterproductive with the unintended consequence being that they “add more to the noise without amplifying the signal” (Martin et al., 2015).
In this paper, we bring together three linked concepts which have previously been employed in the theoretical literature on institutional change in healthcare and more broadly in organisational sociology. These are: normative legitimacy (NL), structural legitimacy (SL) and organisational readiness (OR). We sought out conceptualisations of the link between the actions of individuals with their wider organisational context, and the ways in which they may navigate this complexity. We were interested in this link because the growing agenda for patient feedback to be used to improve services is not necessarily supported by healthcare organisations' dominant procedures and processes (Rozenblum et al., 2013). Equally, interventions designed to promote patient experience, quality and safety may often be targeted at specific individuals or groups to lead on, but ultimately they seek to effect change at a whole-system level, requiring cooperation between actors in different, often quite disparate parts of a healthcare organisation (Benn et al., 2009).
We looked to emerging interpretations of institutional theory to assist us. Macfarlane et al. (2013) states that the tendency in institutional theory has previously been overly deterministic, focusing on the influence of structure at the expense of individual agency, so that the structure exerts a particular logic and individuals will seek to maintain this status quo. With the advent of concepts such as ‘institutional entrepreneurship’ (Battilana et al., 2009), there is recognition that some individuals are not confined by the status quo, and do attempt to transform their organisations from within. Macfarlane welcomes the application by Lockett et al. (2012) of this concept to healthcare and their use of the concepts of legitimacy to understand the behaviour of individuals with respect to transforming their own contexts and institutionalising new agendas which they support. Lockett et al argue that a subject's position in an institution will vary depending on two types of 'legitimacy' that they hold. The first is their 'normative legitimacy' (NL) which Lockett defines as a “moral orientation being based on the ability to convince others of ‘what ought to be’ or ‘what is the right thing to do”'. The second is their 'structural legitimacy' (SL) relating to “the power that emanates from professional hierarchy and jurisdiction” and this element will affect a subject’s chances of effecting change. We note that Lockett’s use of these concepts is a divergence from the original offering of Suchman (1995) who introduced concepts of legitimacy to organisational studies in order to understand whether or not the actions of an organisation as a whole are viewed as socially acceptable within dominant societal structures and norms. For our purposes, it is Lockett's application to the individuals within organisations that we draw upon in order to begin to unpick where action for change arises within our case study.
Lockett's proposal goes someway to understanding the behaviour of individuals and how their actions relate to the context they find themselves in. However, we believe that an additional layer can be added to enhance understanding of the relationship between an individual subject’s position and the organisation as a whole. This especially relates to understanding the link between multiple members of an organisation (often from different divisions/ services) who need to come together collectively for a cross-department agenda such as improving patient experience. We propose that Weiner's (2009) conceptualisation of ‘organisational readiness to change’ (OR) is helpful here. This refers to the extent to which there is a collective, or shared “resolve to pursue the courses of action involved in change implementation”. Crucially, this collective resolve needs to be perceived as such by whoever is leading the change - they need to believe they will find support to be effective in their efforts.
We chose these concepts (NL, SL and OR) because they help us understand change effort relating to the ability of individuals and teams to generate action in response to patient experience feedback. We believe that bringing these three distinct, yet related, concepts together can help reveal the complexity resident in how healthcare staff try to (and do) respond to patient feedback. We recognise that application of these concepts to assist understanding of our empirical findings is still in its infancy so we take care to define our interpretations which may be different to others. It is worth noting that whilst NL and SL have been used together before to understand individuals’ actions (Lockett et al., 2012), the three concepts of NL, SL and OR have not been – to our knowledge - conceptually entwined previously. Our interpretations of how each concept can be used to identify different influences at play are detailed in Table 1. Distinctly, we acknowledge that our conceptualisation of SL may be slightly different to that of Lockett’s which is firmly rooted in the consequences of one’s professional and hierarchical position within an organisation. We are more interested in ideas around the availability of autonomy, ownership and resource, which we will outline in full later.
Table 1.
Theoretical and empirical definitions of each concept.
| Theoretical definition | Application to our empirical data | |
|---|---|---|
| NL | “Moral in orientation, being based on the ability to convince others of ‘what ought to be’ or ‘what is the right thing to do’” (Lockett et al, 2012) | Staff members express a personal belief in the importance of responding to patient feedback and a desire to act. |
| SL | “the power that emanates from professional hierarchy and jurisdiction” (Lockett et al, 2012) | Staff perceive they have sufficient ownership, autonomy and resource available to them in order to establish a coherent plan of action in response to patient feedback |
| OR | There is a collective, or shared “resolve to pursue the courses of action involved in change implementation” at the organisational level (Weiner, 2009) | Meso level OR - the capacity for inter-departmental working and collaboration to achieve improvement. |
| Macro level OR - the capacity in which senior hospital management and the high level systems of the organisation support and facilitate ward staff to work on improvement. |
We recognise the seminal institutional work of Scott et al. (2000) in ensuring that organisations cannot be fully understood in isolation from the external influences arising from a wider 'institutional field' of regulation and continuing political shifts between actor groups. Analyses of these influences on organisational activity are certainly worthy of exploration in their own right but are beyond the scope of our study.
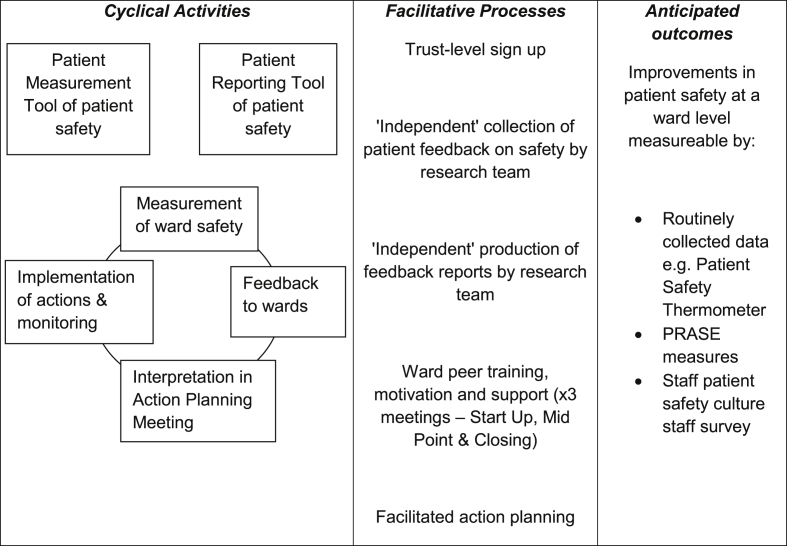
We take the above concepts and embed them in an empirically derived multi-component, multi-faceted framework which theorises the necessary conditions essential to allowing ward staff to effectively respond to patient feedback (Fig. 1). We have called this the ‘Patient Feedback Response Framework’ (PFRF). The empirical data arose from a process evaluation of a large scale randomised controlled trial of a complex patient safety intervention - Patient Reporting and Action for a Safe Environment (PRASE) (Lawton et al., 2017; Sheard et al., 2017 in press). Our aim in this paper is to understand why hospital staff may find it difficult to respond to feedback about safety, quality and experience from their own patients. We consider explanations where we actively seek to scrutinise and problematise the interplay between the individual and the organisational level through a broad theoretical account.
Figure 1.
Patient Feedback Response Framework.
2. Method
We conducted a large qualitative study with 17 ward based teams across three UK hospital Trusts in the North of England. A hospital ‘Trust’ is an organisation that provides secondary health care services to a locality within the English National Health Service system. The study was part of a process evaluation of a randomised controlled trial of a patient safety intervention. The methods of the process evaluation have been described in detail elsewhere (Sheard et al., 2014), as have the process evaluation findings (Sheard et al., 2017 in press) and the results of the trial (Lawton et al., 2017). We provide a synopsis of the intervention in Box 1 for the reader to be able to view our current paper in context. Briefly, the intervention centred on gathering patient feedback about safety on the ward and feeding this data back to ward staff via a structured ‘feedback report’. Staff then considered this information in an action planning meeting (APM) and were facilitated to make improvements based on the patient feedback. When reference is made to a ‘facilitator’ of the APM, the person undertaking this role was always a senior member of the research team. The above activities took place in two phases, spaced six months apart.
Box 1. Intervention synopsis.
Alt-text: Box 1
Three methods were utilised for this paper:
-
•
Critical examination of the APM voice files
-
•
Facilitator’s field notes about the APM
-
•
Follow up telephone interviews six months post APM
Data collection occurred between August 2013 and November 2014. Ethical approval was secured in March 2013. All participants gave informed consent to take part in this study. We draw upon qualitative data from both phases of the study – two sets of APMs and two sets of telephone interviews, per ward. A key member of staff – one for each of the 17 wards in the intervention arm – was asked to form an action planning group consisting of a range of staff members from that ward, who would then take part in an APM. The average number of people in a group was four although in several instances the facilitator met with only one person. The largest group consisted of nine people. Nurses were the majority of participants with a smaller input from medical staff, allied health professionals and support staff. In the first phase of action planning, 63 staff were involved and in the second phase 38 staff. More detail on each unit of analysis is given below:
Critical examination of APM voice files - APMs were digitally recorded for all 17 wards at both phases. At phase two, one ward did not meet so we considered the recordings of 33 APMs (27 to 80 minutes, average = 43 minutes). Our examination focused on which areas of patient feedback the staff chose to make action plans on and which areas they chose not to take forward. The rationale behind these decisions were of key interest. We wrote detailed notes whilst listening to the whole voice file and noted verbatim comments, as warranted.
Facilitator’s field notes - Written shortly after each APM had taken place, they sought to capture: i) implicit dynamics between staff, ii) the environment, iii) the facilitator’s immediate reaction to the meeting. Field notes tended to be brief and were devised to give a ‘snapshot’ of the meeting from the facilitator’s perspective.
Follow up telephone interviews conducted with the APM lead - The purpose was to ascertain whether action plans had been successfully implemented or not. They were conducted around six months after the APM had been held with the ward ‘PRASE lead’ (usually a senior nurse), in both phases of the study. In the first phase, two wards (out of 17 intervention wards) declined to take part in the phone interview but all wards took part in the second phase, leading to a dataset of 32 interviews. The phone interviews were structured and the majority were short (around 15 minutes). The interviews began by proceeding through each action point made, asking about implementation. The context of why or why not an action plan had been implemented was of critical importance.
For the purposes of this paper, we re-analysed the data gathered for the original process evaluation and chose to concentrate on examining it in relation to the three concepts in the Patient Feedback Response Framework described previously: normative legitimacy, structural legitimacy and organisational readiness. We became interested in applying the literature from organisational sociology after noticing that the three concepts seemed to intuitively make sense of what our data was telling us. We took an abductive approach to analysis (Timmermans and Tavory, 2012) which involves iterative cycles of analytical interpretation between the literature and empirical data in order to construct theory. Taking an abductive approach involves engaging in “imaginative thinking about intriguing findings and then return[ing] to the field to check our conjectures” (Charmaz, 2009). One specific aim of this approach is to generate novel theoretical insights which reframe empirical findings in contrast to existing theories (Timmermans and Tavory, 2012). Existing theory can be thought of as a heuristic tool in order to take ideas beyond the data itself (Coffey and Atkinson, 1996).
LS and CM held an intense analysis session where we focused on testing pertinent case studies from our empirical data by mapping these onto where they sat in relation to the three concepts, to see if our preliminary framework was justified and to guard against unsubstantiated retrofitting. This exercise strengthened both our framework and our understanding of how our data related to the literature. Furthermore, it allowed us to further define and hone our own understanding of the three concepts – and how they are linked - in relation to the data which was in front of us. We decided that, to provide rigour, once we had arrived at an outline framework we would return to our empirical data and code the data sources described above based on the three concepts. We did this initial coding in a traditional manner, creating grids of data which gathered all the evidence pertaining to the main action planning activity of an individual ward from the differing data sources of the process evaluation. With the abundance of empirical data in front of us, we then ascribed a summative assessment of where individual wards sat in relation to the three concepts of NL, SL and OR.
3. Findings
Our findings are presented in three main sections. The first section – normative legitimacy – examines whether staff believe there is a moral case for listening to and acting on patient feedback about safety. Second, the section on structural legitimacy explores whether staff believe they are in a position to be able to respond to feedback. That is, whether they have the adequate autonomy, ownership and resource to believe they can enact change. Finally, the third section observes whether the wider organisation was ready to facilitate change on behalf of the ward staff. A summary of the findings is detailed in Table 2 so the reader can see the classification of the whole dataset at a glance. We elaborate on all of the above by providing explanatory cases from the data. We depart from the usual qualitative tradition of providing excerpts of direct quotations from individual participants in order to allow for the meta level of analysis to be portrayed effectively. This approach avoids privileging specific data sources when our intention is for the analysis of all data sources to exist and be presented as a holistic representation. Instead, we offer illustrative case study examples pertaining to ward teams, all developed from multiple data sources described in the Methods section. All ward names and names of individuals are pseudonyms.
Table 2.
Summary of findings.
| Ward | Hospital Trust | Normative legitimacy |
Structural legitimacy |
Organisational readiness |
|||
|---|---|---|---|---|---|---|---|
| Phase one | Phase two | Phase one | Phase two | Phase one | Phase two | ||
| Beech | A | Yes | Yes | No | No | - | - |
| Elm | A | No | No | - | - | - | - |
| Maple | A | No | Yes | - | Yes | - | Yes |
| Oak | A | Yes | Yes | Yes | No | No | - |
| Cherry | B | No | No | - | - | - | - |
| Apple | B | Yes | Yes | Yes | No | No | - |
| Holly | B | Yes | Yes | Yes | Yes | No | No |
| Willow | B | Yes | Yes | Yes | Yes | No | Action plan did not need OR to complete |
| Pine | B | No | Yes | - | No | - | - |
| Rowan | C | No | No | - | - | - | - |
| Birch | C | No | No | - | - | - | - |
| Sycamore | C | Yes | Yes | Yes | Yes | Action plan did not need OR to complete | Action plan did not need OR to complete |
| Hawthorn | C | Yes | Yes | Yes | Yes | Action plan did not need OR to complete | No |
| Poplar | C | Yes | Yes | Yes | Yes | Action plan did not need OR to complete | No |
| Chestnut | C | Yes | Yes | No | No | - | - |
| Juniper | C | Yes | Yes | No | No | - | - |
| Linden | C | Yes | Yes | Yes | Yes | Action plan did not need OR to complete | Action plan did not need OR to complete |
3.1. Stage one of PFRF: normative legitimacy
The majority of ward teams were open and receptive to receiving feedback from their patients and genuinely wanted to make improvements to the ward based on this data. Some teams spontaneously mentioned during the APM to the facilitator that they were “excited” about receiving the patient feedback and couldn’t wait to start responding to the issues which their patients had raised. Throughout, there was a sense that listening to patients and acting on issues they had raised was ‘the right thing to do’ and that the staff really wanted to make authentic improvements. Members of Willow and Holly wards were striking in their commitment to acting on patient feedback in that several staff members attended the APM on their day off. The characteristics of teams who had sufficient NL tended to be: A multidisciplinary group, who had all read the feedback report prior to the APM, had thought carefully about its contents and had allowed themselves time and space to discuss patient feedback arising from the report and how they were going to act on this in a considered manner. These teams tended to appreciate what the research team were trying to achieve and the purpose and ethos of the study, as they themselves already had a firm commitment to the patient voice. Of the 17 intervention wards, we have classified 11 ward teams as having NL although the extent to which this matches the description above pertains to nine ward teams with the other two (Oak and Juniper) engaged with NL in a more restricted manner. These two teams, whilst on the surface seemingly engaged in the moral imperative to respond to patient feedback, often discussed the report in a ‘clinician knows best’ manner. For both teams, responses to the patient data were firmly entrenched in a rhetoric of ‘managing patient expectations’ rather than seeking to tackle the underlying issue at hand which patients had raised.
Of the remaining six ward teams, four (Elm, Cherry, Rowan and Birch) can be classified as having minimal or zero NL throughout the life course of the study whilst a further two (Maple and Pine) had minimal or zero in phase one but then began to understand the importance of listening to patient feedback and came to embrace this approach in phase two. For the former group, research facilitators were often met with hostility. A defensive stance was taken by ward staff when asked to consider the patient feedback in the APM coupled with concerns about who else had access to the data, despite reassurance the data was confidential to the individual ward. Elm ward in particular encapsulates this approach as when asked to consider the patient feedback data for their ward, staff members became irritated about comments which patients had made and dismissed the feedback as irrelevant. The facilitator left the APM feeling deflated and demoralised about the attitude of staff towards the feedback.
The two ward teams who began with minimal NL in phase one but proceeded to sufficient NL in phase two (Maple and Pine) are of particular interest as they show that NL is not necessarily static and can change in a relatively short space of time – around six months in this case. The reasons why they changed their stance are complex although one discernible reason relates to their respective ward managers not seeing any value in acting on patient feedback. A key turning point for both managers of these wards – despite them being at different hospital Trusts - appears to be the Mid-Point Meeting (described in Box 1) where they heard their nursing peers in other wards attest to the implicit value of listening to and acting on the patient voice.
Overall, it is reassuring to see that the majority of ward teams did have sufficient NL capacity and actively strived to act on patient feedback. The four teams who had minimal or zero NL largely fell down at this stage and failed to enact action plans which would benefit their patients. We now turn our attention to the next concept in our framework: structural legitimacy.
3.2. Stage 2 of PFRF: structural legitimacy
Based on our empirical data, we propose that SL consists of three inter-related concepts. Staff must perceive that they have a sufficient amount of each in order for them to be able to act on patient feedback. These are:
-
•
autonomy - freedom from external control or having free will to act on an issue (“it’s ok for me to carry out this action plan without having to check with the matron”)
-
•
ownership - the state and/or right to possess something (“this is my issue or problem to deal with”)
-
•
resource – sufficient sources of (and freedom of) finance, time and logistical commitment to enable change to happen.
We focus this findings section on the rationale behind why staff did or did not perceive they had sufficient SL to enact change based on patient feedback. Nearly all of the 17 ward teams for both phases of the study fit into three distinct responses concerning SL. First, we saw that sufficient SL was demonstrated when the change which staff sought to enact was perceived as being within their own control and it related only to the environment or systems of the individual ward on which they worked. That is, ownership and autonomy were strong with little or no resource required. Second, one of the main reasons why SL was not present within some ward teams relates to a lack of ownership of the initial problem either related to staff flux or a demoralised workforce. Third, some teams proceeded determinedly with their action plans but were set back or blocked by meso-level organisational factors. Usually, they needed assistance from others external to the ward but this was often not forthcoming and the collective ethos needed to solve a problem did not exist. We have not classified ward teams in relation to SL based on whether their action plan was achieved or not as we believe it to be tautological to ascribe a retrospective assignment of a team’s belief about their capacity to enact change based on the end result. It is the ‘why’ behind what helped or hindered their implementation of action plans which we are interested in here.
For the analysis of SL in phase one, 11 out of 17 ward teams were considered and in phase two this amounts to 13 out of 17 teams. We excluded those who did not demonstrate sufficient NL from our SL analysis. Out of the 11 ward teams in phase one, it appears that the majority (eight) can be classified as believing they had sufficient SL. Four made changes within their direct control and the other four sought to make wider changes but were set back by organisational factors. The other three ward teams could not tackle a problem raised by their patients from the start as they lacked ownership of it. Out of the 13 teams we considered in phase two, slightly less than half (six) believed they had sufficient SL with three making changes within their control and the other three being thwarted by organisational factors. Most of the rest of this phase two cohort (five teams) lacked ownership of the problem from the offset. Maple (in phase two), bucks the above classifications as significant external resource and collaborative working were required to achieve change but the wider organisation responded positively to achieve this. (See Table 2 for a visual summary). We now proceed to discuss the three findings in more detail with relevant case studies drawn from the empirical data.
SL is high when the improvement is within the control of staff initiating it – we can see that when staff sought to make changes to the structures or processes of the individual ward on which they worked, this often led to success. This amounted to four ward teams in phase one and three in phase two. In fact, very few actions based on patient feedback fell down when the change (however great) was confined to amending the systems or processes of one ward. This was often because ownership and autonomy to solve an issue was high, especially for senior nursing staff. An example of this comes from Hawthorn ward in phase one. They decided to alter and extend their visiting hours to the ward in order to prevent a rush of relatives requesting information at the same time. The standard visiting hours had previously been 2pm to 4pm and then 6pm to 8pm – as was traditional across most of the rest of the hospital - but Hawthorn staff changed them to 2pm to 8pm. The members of staff involved in this action plan considered it “radical” as it was a major change to the structural workings and processes of the ward. Yet, the necessary autonomy and ownership to make this change existed in the action planning group. Additionally, very little resource was required to make this change happen.
The other types of action plans which staff made which were within their control sometimes related to modifying the role of a staff member in order to benefit patient experience. This related to three ward teams across both phases. The team on Poplar ward were concerned that their patients had reported they were frustrated by conflicting information being given about the discharge process. They decided to modify the role of the discharge nurse so that dedicated time was given to each patient to discuss discharge and – most importantly – patients were kept informed if their discharge was going to be delayed. As before, autonomy and ownership to implement this improvement was high but no resource was required. The ward manager stated in the follow up interview six months later that complaints about the discharge process had reduced and the ward team believed this was directly attributable to the action plan instigated.
SL is low when there is lack of ownership about the problem - this relates to three teams in phase one and five in phase two. Lack of ownership can be divided into two distinct reasons: 1) the change initiative hindered by what we have termed ‘staff flux’ 2) a demoralised approach to action planning. Staff flux in this context means a high movement of ward staff around the NHS estate. That is, ward teams being significantly restructured or staff leaving their role to work on another ward within the same hospital or at a different hospital. Sometimes, staff who left were not replaced or recruitment to replace them was unsuccessful. Equally, new team members may have arrived and were not expected to take part in action planning about long standing issues. This movement of staff during the life course of the study was much higher than the research team had anticipated.
Staff flux is a serious problem when it comes to a team of ward staff taking ownership of an action plan and seeing it through to completion. The reasons are that one team member would sometimes take responsibility to initiate an action plan but completion of that work then fell down if that person permanently left the ward environment. We found little evidence of action plans being delegated appropriately for other staff to complete them. In times of change and uncertainty around staffing levels, some wards focussed their attention on direct patient care and decided to return to improvement initiatives once the core team had been strengthened. For a few teams who were under significant stress, the action plan was inappropriately delegated to a more junior member of staff who lacked the ownership of the problem and also the necessary autonomy to solve it. We can see that staff flux is a problem on Chestnut and Juniper wards in phase one and Pine and Juniper wards again in phase two.
The second reason ward teams lacked ownership of an issue relates to a demoralised approach to action planning. This was evident in phase two on Oak and Apple wards and to a lesser extent on Juniper ward. Demoralisation in phase two is directly related to the team’s prior experience of making action plans in phase one of the study which were then hindered in some manner and prevented from coming to fruition. For the above teams, action planning in phase two therefore sometimes felt like ‘going through the motions’ with the action planning team agreeing to meet with the researcher but the meeting concentrating on prior frustrations and new patient feedback being considered in a lacklustre manner. It is useful to note that not all teams who were thwarted in phase one action planning reacted in a demoralised manner in phase two.
SL is hindered by inadequate organisational working – when ward staff tried to instigate meso-level change which involved actors external to the individual ward environment, action planning often became problematic. This classification applies to four ward teams in phase one and three in phase two. Difficulties arose when the proposed improvement required any of the following: negotiation with external contractors, the approval of committees, extensive input or assistance from another department/ service and structural changes at the level of the whole organisation. Of interest, these difficulties were sometimes not related to how far reaching the change appeared to be with relatively simple improvements being thwarted by a lack of collaborative working on the part of other departments or services elsewhere in the hospital. Ward teams in this classification believed they had sufficient SL but were effectively being blocked by inadequate organisational readiness to change (OR), which is the next component of our framework.
At this juncture, we take forward into the analysis those teams who had their action planning thwarted by insufficient OR (seven across both phases) to unpick why this occurred. We also discuss the case of Maple ward who were the only ward team to achieve change which relied on extensive collaboration and resource outside of the individual ward environment. We leave behind the majority of ward teams: those where SL was high and their action plan did not depend on OR to succeed and also those who lacked ownership of the problem, therefore SL was low to begin with.
3.3. Stage 3 of PFRF: organisational readiness
The ability for ward teams with a perceived sense of SL to be able to realise change is inextricably linked to whether OR exists at the level of the organisation (the hospital Trust) and in turn whether OR facilitates the change staff wish to make. This can be broken down into meso OR and macro OR. Meso OR refers to the capacity for inter-departmental working and collaboration to achieve improvement. Macro OR refers to the capacity in which senior hospital management and the high level systems of the organisation support and facilitate ward staff to work on improvement.
OR at the meso level of inter-departmental working was poor for most of the teams who tried to instigate change where it depended on the buy in of others external to the individual ward. For instance, staff on Apple ward needed assistance from the pharmacy department in order to change procedures around controlled drug dispensing and they could not complete their action plan without this help. Yet the pharmacy department were not willing to help their colleagues on Apple ward to achieve this change. Similarly, the Holly ward team wanted to improve communication between theatre staff and ward staff but found that theatre management were not interested in assisting the ward to achieve this. Other teams found their action plans hindered by macro OR processes which curtailed effective action planning due to inflexibility and bureaucracy. Willow ward team wanted to physically alter part of the ward environment but found that there was a complicated hierarchy of estates and leaseholders to gain approval from before work could begin. In a different manner, but still resident at the level of macro OR, staff on Oak ward found that a leaflet they wrote had stalled for several months with the hospital’s ‘reading panel’ and had not been implemented six months after it was written. Perhaps one of the most interesting examples of macro OR preventing an action plan being realised is that of Poplar ward in phase two. Ward staff worked hard to implement an action plan which sought to prevent a noisy and too bright assessment area being used as an extra bed bay during high occupancy periods. They were blocked by hospital management who repeatedly declined their attempts to make the improvement.
Our discordant case is that of the Maple ward team. This team had tacit knowledge over a long period of time that there were not enough nursing staff on a night shift but it was difficult to prove this by virtue of anecdote alone. The PRASE data showed that five separate patients had reported to researchers – over a three week data collection period – that they had waited a significantly long time for staff to answer their call buzzer and this had compromised patient experience and safety. Critically, this most often related to patients becoming incontinent as a result of needing assistance with toileting and no staff being available to perform this. The ward manager wanted an extra qualified nurse for three nights a week in order to address these problems and the Maple team made an action plan to achieve this. The ward manager reported these concerns to the corporate nursing department (via an electronic system which records patient safety incidents) and escalated them to the hospital board. Senior management responded to this and authorised the ward manager to go over budget to ensure there were three qualified nurses every night. This is a clear example where macro OR was present and assisted in achieving concrete improvements for patients.
4. Discussion
Through a consideration of the empirical data and the resultant formulation of the Patient Feedback Response Framework (Fig. 1), we can see that effecting change based on patient feedback relies heavily on sufficient NL, SL and OR being present in relation to the improvement which is being made. NL is the first component of the PFRF. Without the moral imperative to listen to the patient voice, improvement rarely takes place. The second component of the PFRF is SL, where staff must have sufficient autonomy, ownership and resource in relation to a problem in order to enact change. Where SL is high, the desired change is within control of the staff and wholly within the environment of the ward they work on then action plans are likely to be successfully implemented. When SL is low, we identified that there is a lack of ownership of a problem and this most often pertains to staff flux or demoralisation with action plans failing to be initiated. In some instances, action planning gets underway and staff believe they have SL but the wider organisational working to achieve change (OR) is not sufficient to enable change to occur. The third component of our framework is OR, which can be divided into the meso (inter-departmental collegiate working) and macro (high level system support for change) levels. Insufficient OR usually blocks action planning even for wards which are high in SL.
It is useful to consider the interplay and relationships between the levels of the framework in order to develop our understanding of the myriad of contextual issues at play. Sufficient levels of NL and SL are needed in order for change to proceed but some action plans do occur without the need for OR. It is interesting to see that sufficiency of NL may bear no relation to the capacity for SL which actors have. Whilst it would be intuitive to believe that the two are perhaps related, our analysis has shown that minimal SL can exist even when NL is high. That is, an ethical imperative to pay attention to and listen to the patient voice does not instil the necessary in situ conditions for improvement to happen. This failure of successful transition between NL and SL is an important element of the inability of ward staff to respond to patient feedback.
Equally as problematic is the relationship between SL and OR and the dependency which some action plans have on OR being in place even when SL to achieve the change is very high. When looking at the types of action plans which ward staff attempted to make, we can see two clear trends: changes made only to the ward processes which were under direct control of the action planning team or changes which sought wider external support at a systematic level. The former succeeded and the latter usually failed. In the current movement for continuous quality improvement within healthcare, ward staff are being asked to perform an onerous task when the wider organisational support or working is insufficient to be able to assist them in their improvement goals. Indeed, Rozenblum et al. (2013) describes a patient feedback ‘chasm’ between hospital managers and frontline clinicians whereby managers invest heavily in measuring patient feedback but have little or no plans for how to facilitate staff to enact subsequent improvement. We believe there needs to be less concentration by senior management on the formal metrics and targets of individual wards and an increased fostering of a culture where interdisciplinary and inter-departmental working is encouraged and rewarded. Large parts of hospital organisations are working in silos, each trying to respond individually to patient feedback, when patient care and experience would be significantly improved if these actors came together in a collaborative working arrangement. As Burnett et al. (2010) have commented, effective integration of parallel improvement activities is vital to reduce the ‘improvement strain’ on staff.
Likewise, it is beginning to be perceived as unethical to ask patients to give feedback if little or nothing will be acted upon (Coulter et al., 2014). Given the knowledge gained from our empirical work, we believe that until ward staff are given robust organisational support to implement changes then the value of Trusts collecting patient feedback is questionable. This speaks to both the unethical nature of asking patients to feedback without subsequent change occurring but also the demoralising effect on staff when they try to make changes to improve patient care but become thwarted and stymied in the process of doing this. We saw empirical evidence of this when SL was low due to previous failed attempts at action planning. When staff attempt system level changes which repeatedly flounder, future efforts may then be directed towards small scale immediate improvements within the actor’s control. This does more than merely hinder the original issue at hand and becomes a broader concern about the inability of individuals to successfully enact change. Tucker et al. (2002) argue that problem solving behaviours which focus solely on overcoming immediate obstacles prevent organisational learning. In part, this is because short term success limits motivation to remove the underlying causes of problems. Indeed, some of the changes we saw enacted in our study were often centred on providing ‘quick fixes’ – immediate solutions to concrete problems. Whilst some of these were entirely appropriate as a solution to the problem in hand, others were not. In many organisations, an adequate SL and OR culture – coming together to achieve change - needs creating and sustaining. However, as Power et al. (2016) have noted, change initiatives are difficult to embed in times of ‘structural turbulence’ which the NHS is currently living through. In a climate of ‘do more with less’, and considerable constraint on the NHS budget, fostering of an effective SL and OR culture is unlikely to be achieved even in the medium term future.
Yet, some staff are able to work within the system in order to use it to their – and their patients' - advantage. These people have been described as “institutional entrepreneurs” (Battilana et al., 2009) as they are more likely than others to see and act on opportunities for institutional change. We found several examples of these people during our analysis – such as the ward manager on Maple ward – but they consisted of a minority of ward staff. Entrepreneurship in this regard often centred on strengthening elements of SL within their grasp (mostly in relation to the ward itself) in order to benefit patient care. Understanding the motivations of these people and how they operate may be critical in unpicking what are the essential elements of SL which lead to fruitful change based on patient feedback.
4.1. Limitations
Some ward teams changed over the course of the study in relation to where they sat in terms of NL and SL and their corresponding sufficiency here. We have tried to encapsulate this throughout the findings section by clearly demarcating the wards that changed their ethos. For instance, two wards progressed from minimal NL in phase one to sufficient NL in phase two. Defining why and how teams changed their ethos regarding NL is hard – it may relate to the trajectory of the study itself in that ward staff were being continually encouraged to consider patient feedback and the first phase of this was problematic for them as it was novel. It could be that ward teams were getting used to working with an external research team rather than an in house quality improvement facilitator and the different dynamic this entailed. Or it could be related to broader cultural movement at the level of the organisation alongside a general political awakening of the importance of the patient voice (Cornwell, 2015) which largely came to fruition during the timescale of the study.
In this paper, we provide a theoretical framework for understanding why ward staff may find it difficult to respond to patient feedback. Our framework helps us make sense of the interplays and disjunctures between context (be that social, cultural or political) and individuals working within organisational systems. It is inherently embedded in a medical sociology analysis and offers up explanatory factors which may impact on attempts to respond to patient feedback. Therefore, we would caution against our resultant framework being used as an ‘off the shelf’ tool by healthcare organisations which could lead to a reductionist re-appropriation of its core messages.
5. Conclusion
Patient feedback is only likely to be acted upon when all the levels of the PFRF are sufficiently in place, as appropriate to the desired change. NL and SL are always needed to make change happen but some teams require OR if the improvement necessitates external assistance. We found that the majority of ward teams possessed NL but SL appeared to be a problematic area for some who were demoralised or in a state of staff flux. For those where SL was high, implementation of action plans largely depended on whether the change was in the immediate control of the ward staff themselves. When this was the case, improvement usually succeeded. Where SL was high but OR was required, improvement usually failed. Poor OR was a major barrier to the realisation of action plans in this study. A critical reason why ward staff fail to progress with enacting change relates to insufficient inter-departmental working and high level systems which hinder structural changes. This paper contributes to understanding the landscape of patient feedback which to date has largely focused on which data should be collected and how this should be conducted rather than how staff can use feedback to improve care. The value of collecting evermore data is questionable without a change to the conditions under which staff find it difficult to respond.
Acknowledgements
We would like to thank the three anonymous reviewers for their insightful and constructive feedback which we believe has immeasurably improved the paper.
We are grateful to all the ward staff who participated in this study.
Thanks for Gemma Louch, Jane Heyhoe and Yvonne Birks for research assistance in conducting some of the telephone interviews.
This study was funded by the National Institute for Health Research under its Programme Grants for Applied Research scheme (‘Improving patient safety through the involvement of patients’, RP-PG-0108-10049). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- Asprey A., Campbell J., Newbould J. Challenges to the credibility of patient feedback in primary healthcare settings: a qualitative study. Br. J. General Pract. 2013;63(608):e200–e208. doi: 10.3399/bjgp13X664252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battilana J., Leca B., Boxenbaum E. How actors change institutions: towards a theory of institutional entrepreneurship. Acad. Manag. Ann. 2009:65–107. [Google Scholar]
- Benn J., Burnett S., Parand A., Pinto A., Iskander C., Vincent C. Studying large-scale programmes to improve patient safety in whole care systems: challenges for research. Soc. Sci. Med. 2009;69:1767–1776. doi: 10.1016/j.socscimed.2009.09.051. [DOI] [PubMed] [Google Scholar]
- Burnett S., Benn J., Pinto A. Organisational readiness: exploring preconditions for success in organisation-wide patient safety improvement programmes. Qual. Saf. Health Care. 2010;19:313–317. doi: 10.1136/qshc.2008.030759. [DOI] [PubMed] [Google Scholar]
- Charmaz K. Shifting the grounds: constructivist grounded theory methods. In: Morse J., Stern P., Corbin B., editors. Developing Grounded Theory: the Second Generation. Left Coast Press; Walnut Creek: 2009. [Google Scholar]
- Coffey A., Atkinson P. Sage; London: 1996. Making Sense of Qualitative Data: Complementary Research Strategies. [Google Scholar]
- Cornwell J. Reframing the work on patient experience improvement. Patient Exp. J. 2015;2(1):11–14. [Google Scholar]
- Coulter A., Locock L., Ziebland S. Collecting data on patient experience is not enough: they must be used to improve care. BMJ. 2014;348:2225. doi: 10.1136/bmj.g2225. [DOI] [PubMed] [Google Scholar]
- Davidson K., Shaffer J., Ye S. Interventions to improve hospital patient satisfaction with healthcare providers and systems: a systematic review. BMJ Qual. Saf. 2016 doi: 10.1136/bmjqs-2015-004758. 3/8/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeCourcy A., West E., Barron D. The national adult inpatient survey conducted in the english national health service from 2002-2009: how have the data been used and what do we know as a result? BMC Health Serv. Res. 2012;12:71. doi: 10.1186/1472-6963-12-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon-Woods M., Baker R., Charles K. Culture and behaviour in the english national health service: overview of lessons from a large multi method study. BMJ Qual. Saf. 2013;0:1–10. doi: 10.1136/bmjqs-2013-001947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle C., Lennox L., Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1) doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards K., Walker K., Duff J. Instruments to measure the inpatient hospital experience: a literature review. Patient Exp. J. 2015;2(2):11. [Google Scholar]
- Gkeredakis E., Swan J., Powell J. Mind the Gap: understanding utilisation of evidence and policy in health care management practice. J. Health Organ. Manag. 2011;25(3):298–314. doi: 10.1108/14777261111143545. [DOI] [PubMed] [Google Scholar]
- Gleeson H., Calderon A., Swami V. Systematic review of approaches to using patient experience data for quality improvement in healthcare settings. BMJ Open. 2016;6:e011907. doi: 10.1136/bmjopen-2016-011907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Foundation . Health Foundation; London: 2013. Measuring patient experience: evidence scan. [Google Scholar]
- Lawton R., O'Hara J., Sheard L. Can patient involvement improve patient safety? A cluster randomized control trial of the patient reporting and action for a safe environment (PRASE) intervention. BMJ Qual. Saf. 2017 doi: 10.1136/bmjqs-2016-005570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockett A., Currie G., Waring J. The role of institutional entrepreneurs in reforming healthcare. Soc. Sci. Med. 2012;74:356–363. doi: 10.1016/j.socscimed.2011.02.031. [DOI] [PubMed] [Google Scholar]
- Locock L., Robert G., Boaz A. Using a national archive of patient experience narratives to promote local patient centred quality improvement: an ethnographic process evaluation of ‘accelerated’ experience-based co-design. J. Health Serv. Res. Policy. 2014;19(4):200–207. doi: 10.1177/1355819614531565. [DOI] [PubMed] [Google Scholar]
- Macfarlane F., Barton-Sweeney C., Woodard F. Achieving and sustaining profound institutional change in healthcare: case study using neo-institutional theory. Soc. Sci. Med. 2013;80:10–18. doi: 10.1016/j.socscimed.2013.01.005. [DOI] [PubMed] [Google Scholar]
- Martin G., McKee L., Dixon-Woods M. Beyond metrics? Utilizing ‘soft intelligence’ for healthcare quality and safety. Soc. Sci. Med. 2015;142:19–26. doi: 10.1016/j.socscimed.2015.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS Confederation . NHS Confederation; London: 2010. Feeling Better? Improving Patient Experience in Hospital. [Google Scholar]
- Power M., Brewster L., Parry G. Multi method study of a large scale programme to improve patient safety using a harm free care approach. BMJ Open. 2016;6:e011886. doi: 10.1136/bmjopen-2016-011886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves R., West E., Barron D. Facilitated patient experience feedback can improve nursing care: a pilot study for a phase III cluster randomised controlled trial. BMC Health Serv. Res. 2013;13:259. doi: 10.1186/1472-6963-13-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert G., Cornwell J. Rethinking policy approaches to measuring and improving patient experience. J. Health Serv. Res. Policy. 2013;18(2):67–69. [Google Scholar]
- Rozenblum R., Lisby M., Hockey P. The patient satisfaction chasm: the gap between hospital management and frontline clinicians. BMJ Qual. Saf. 2013;22:242–250. doi: 10.1136/bmjqs-2012-001045. [DOI] [PubMed] [Google Scholar]
- Scott W.R., Reuf M., Mendel P.J. University of Chicago Press; Chicago: 2000. Institutional Change and Healthcare Organizations: from Professional Dominance to Managed Care. [Google Scholar]
- Sheard L., O’Hara J., Armitage G. Evaluating the PRASE patient safety intervention-a multi-centre, cluster trial with a qualitative process evaluation: study protocol for a randomised controlled trial. Trials. 2014;15:420. doi: 10.1186/1745-6215-15-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheard L., Marsh C., O’Hara J. Understanding how organisational context affects the implementation of a patient safety intervention: a qualitative process evaluation. BMJ Open. 2017 doi: 10.1136/bmjopen-2016-014558. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman M. Managing legitimacy: strategic and institutional approaches. Acad. Manag. Rev. 1995;20(3):571–610. [Google Scholar]
- Timmermans S., Tavory I. Theory construction in qualitative research: from grounded theory to abductive analysis. Sociol. Theory. 2012;30(3):167–186. [Google Scholar]
- Tucker A., Edmondson A., Spear S. When problem solving prevents organisational learning. J. Organ. Change Manag. 2002;15(2) [Google Scholar]
- Weiner B. A theory of organisational readiness for change. Implement. Sci. 2009;4:61. doi: 10.1186/1748-5908-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]