Abstract
This study examined the effect of obesity on the use of indwelling urinary catheters among long-term care facility residents and found initial increases in usage by weight category, which declined during the next 12 months.
Keywords: Obesity, older adults, long-term care facilities, indwelling urinary catheters
Long-term use of indwelling urinary catheters for urinary incontinence (Ul) is not recommended (Centers for Disease Control and Prevention [CDC]/National Healthcare Safety Network, 2009; Centers for Medicare & Medicaid Services [CMS], 2005) because indwelling urinary catheters can increase the risk for urinary tract infections, urethral complications, bladder stones, and bladder cancer (Igawa, Wyndaele, & Nishizawa, 2008), as well as mortality (Landi et al., 2004). Nevertheless, their use can be considered for management of UI in very specific circumstances (see Table 1). However, overuse or inappropriate use of indwelling urinary catheters may occur (Doughty & Kisanga, 2010).
Table 1.
Indications for Indwelling Urinary Catheter
|
Long-term care facilities provide a range of medical and nonmedical services to individuals who need assistance with activities of daily living due to disability or chronic illness. Although long-term care can be provided in the home or other community-based settings, it is most often provided in long-term care facilities, such as nursing homes. After substandard care in longterm care facilities was documented in the mid-1980s, federal efforts to reform and monitor long-term care increased. These efforts included the development of a standardized resident assessment tool (the Minimum Data Set [MDS]) (see Figure 1) and a set of 24 quality indicators, one of which focuses on the prevalence of indwelling urinary catheters (Capitman, Leutz, Bishop, & Casler, 2005). Additionally, federal tags (F-tags) have been developed to provide care protocols for certain conditions. F-tag 315 provides detailed guidance to longterm care facilities for the management of UI, including appropriate use and management of indwelling urinary catheters (Doughty & Kisanga, 2010).
Figure 1.
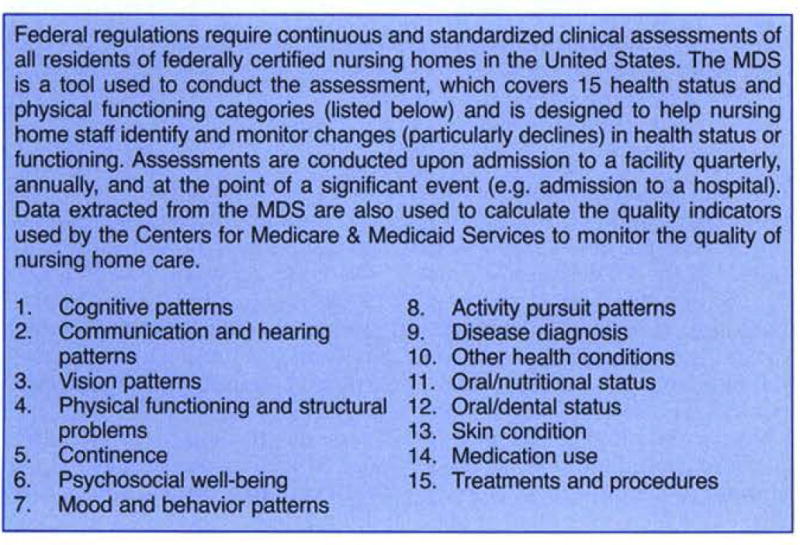
Minimum Data Set (MDS)
The current national indwelling urinary catheter prevalence rate of 5% of long-term care facility residents (CMS, 2011) is within recommended thresholds, which range from 2.1% to 6.5% (Rantz et al., 2000). Certain longterm care facility residents, however, may be at risk for overuse of indwelling urinary catheters. Research has shown that obesity (body mass index [BMI] greater than or equal to 30) is associated with UI (Hunskaar, 2008). Obese long-term care facility residents require significantly more assistance from staff for the performance of activities of daily living, including using the toilet (Felix, 2008). One long-term care facility staff member reported in a qualitative study on the provision of continence care for obese longterm care facility residents that “it’s more difficult for us [caregivers] … it always takes two [nursing aides] to clean [the resident] up after every incontinent episode…” (Bradway, Miller, Heivly, & Fleshner, 2010, p. 125).
Because of staff burden to address UI among obese residents, we hypothesized these residents may be more likely to have an indwelling urinary catheter. At least one study that examined indwelling urinary catheters in long-term care facilities in five states found that those weighing 250 or more pounds were more likely to have an indwelling urinary catheter at admission, at quarterly assessments, and at one year (Rogers et al., 2008). However, this disparity in use is not regularly monitored, nor has it been recently examined. Given the rising rates of obesity among older Americans (Flegal, Carroll, Ogden, & Curtin, 2010), and the association between obesity and long-term care facility admission (Elkins et al., 2006; Valiyeva, Russell, Miller, & Safford, 2006), further examination of this issue is warranted, and it prompted the current analysis to assess differences in the utilization rates of indwelling urinary catheters among obese and non-obese long-term care facility residents.
Methods
This study utilized a longitudinal cohort design that followed all older adults (65 years of age or older) admitted to any federally certified long-term care facility in Arkansas and resided there for at least one year.
Data Source
Data were obtained from the Arkansas MDS. The MDS contains federally required assessment data on physical and mental health conditions, quality of life, and well-being (among other domains) of all residents in federally certified long-term care facilities in the United States (see Figure 1) (Wunderlich & Kohler, 2001).
Variables
The dependent variables on indwelling urinary catheter use for quarters two, three, and four were created using the Quality Measures User’s Manual formula of long-term care facility residents with an indwelling urinary catheter in the numerator and all residents in denominator (Abt Associates, Inc., 2004). The indwelling urinary catheter quality measure formula excludes the admission assessment. Therefore, the indwelling urinary catheter-dependent variable at admission in quarter one used the response from the MDS question on continence applications and programs (question H3) on the admission assessment. Section H of the MDS assesses bladder and bowel continence of long-term care facility residents in the 14 days prior to the date of the assessment. Continence self-control is assessed on a five-point scale ranging from complete control (continent) to inadequate control (incontinent). Questions also assess use of continent appliances and programs (e.g. toileting plan, pads, or catheters) and whether continence control is achieved with the assistance of appliances.
The primary independent variable of interest was BMI, which was calculated using the standard formula of weight (in kilograms) divided by height (in meters) squared (National Heart, Lung & Blood Institute [NHLBI] Obesity Education Initiative Expert Panel, 1998), and resident height and weight as recorded on the MDS admission assessment. BMI was categorized into five levels (see Table 2), with normal weight serving as the reference category in multivariate analyses. Age, gender, race/ethnicity, and assessment time were included as additional covariates. Other clinical characteristics (e.g. ADL score, cognitive status) obtained from the MDS and facility characteristics (e.g. number of beds, staff) obtained from the Nursing Home Compare database, as well as a race-weight status interaction term, were included in initial models but were not retained in the final model for parsimony sake because they were not significant and did not contribute to the model.
Table 2.
Characteristics of Older Arkansas Long-Term Care Facility Residents (N = 3,879) at Admission and Associations with Indwelling Urinary Catheter Use over One Year from GEE Model
| Characteristics at Admission | GEE Model Results | ||
|---|---|---|---|
| Continuous Variables | Mean (SD) at Admission | OR (95% Cl) | p-Value |
| Age, years | 84.1 (8.4) | 0.985 (0.96, 1.01) | 0.27 |
| Categorical Variables | % (n) | OR (95% Cl) | p-Value |
| Underweight (BMI < 18.5) | 9.0 (346) | 1.00 (0.50, 2.00) | 0.99 |
| Normal weight (BMI = 18.5 to 24.9) | 43.5 (1673) | Referent | – |
| Overweight (BMI = 25 to 29.9) | 27.8 (1067) | 0.982 (0.67, 1.43) | 0.93 |
| Obesity (30 to 34.9) | 11.89 (456) | 0.770 (0.42, 1.41) | 0.40 |
| Severe obesity (≥ 35) | 7.9 (302) | 1.686 (0.91,3.12) | 0.10 |
| Time (quarter intervals) | – | 0.998 (1.00, 1.00) | 0.04 |
| Female | 66.9 (2593) | 0.673 (0.43, 1.06) | 0.09 |
| African American | 10.2 (393) | 1.586 (0.94, 1.67) | 0.08 |
Notes: BMI = body mass index, Cl = confidence interval, n = number, OR = odds ratio, SD = standard deviation; ORs generated using generalized estimating equation (GEE) model.
Analytic Methods
Descriptive statistics were used to characterize long-term care facility residents in the analytic file. Two-sample t-tests and Chi-square tests were used to assess the equality of demographic characteristics of longterm care facility residents based on BMI category. To account for repeated measures on residents and the clustering of residents within long-term care facilities, a generalized estimating equation (GEE) model was used to examine the effect of obesity on the indwelling urinary catheter indicator over time.
The University of Arkansas for Medical Sciences Institutional Review Board approved the study under expedited procedures.
Results
Table 2 lists characteristics of the 3,879 Arkansas long-term care facility residents included in the analysis. These residents were mostly female (66.9%) and were on average 84.1 years of age (8.4 SD). The average BMI was 25.8 (6.5 SD), with 19.5% of residents at admission being classified as obese (BMI ≥ 30). At admission, 24.2% of African Americans were obese, compared to 19.2% of Caucasians (p = 0.02), and 22.7% of females were obese compared to 15.7% of males (p < 0.0001). Table 3 shows the percentage of all residents with indwelling urinary catheters at admission and at quarter points over the observation year, as well as by residents by obesity status. At admission, the prevalence rate of indwelling urinary catheters among all residents was 16.8%, which declined to 4.1% by the fourth quarter. Obese residents had a significantly higher prevalence rate of indwelling urinary catheters than non-obese residents at admission (19. 4% vs. 16.2%, p = 0.034) and a borderline significantly higher prevalence rate (p = 0.09, suggesting a trend toward statistical significance) at the second quarter than non-obese residents (7.3% vs. 4.6%). However, rates were not statistically different at quarters three and four.
Table 3.
Percent of Older Long-Term Care Facility Residents in Arkansas with Indwelling Urinary Catheters over Four Quarters (2008) by Obesity Status, and by Race and Gender
| All (%) | O (%) | NO (%) | p-Value | |
|---|---|---|---|---|
| All Residents | ||||
| Admission (Quarter 1) | 16.8 | 19.4 | 16.2 | 0.03 |
| Quarter 2 | 5.1 | 7.3 | 4.6 | 0.09 |
| Quarter 3 | 4.6 | 5.3 | 4.4 | 0.55 |
| Quarter 4 | 4.1 | 4.7 | 3.9 | 0.64 |
| Caucasian Residents | ||||
| Admission (Quarter 1) | 16.7 | 19.7 | 16.0 | 0.02 |
| Quarter 2 | 4.8 | 6.7 | 4.3 | 0.15 |
| Quarter 3 | 4.0 | 4.1 | 4.0 | 0.94 |
| Quarter 4 | 4.0 | 5.4 | 3.6 | 0.28 |
| African-American Residents | ||||
| Admission (Quarter 1) | 17.9 | 18.3 | 17.8 | 0.92 |
| Quarter 2 | 7.3 | 8.6 | 7.0 | 0.75 |
| Quarter 3 | 8.1 | 9.7 | 7.6 | 0.71 |
| Quarter 4 | 5.2 | 0.0 | 7.0 | 0.16 |
| Female Residents | ||||
| Admission (Quarter 1) | 16.9 | 19.2 | 16.2 | 0.09 |
| Quarter 2 | 4.5 | 7.6 | 3.7 | 0.02 |
| Quarter 3 | 4.2 | 4.7 | 4.0 | 0.69 |
| Quarter 4 | 3.3 | 4.1 | 3.1 | 0.55 |
| Male Residents | ||||
| Admission (Quarter 1) | 16.7 | 19.9 | 16.1 | 0.19 |
| Quarter 2 | 6.6 | 6.4 | 6.6 | 0.94 |
| Quarter 3 | 5.6 | 7.1 | 5.3 | 0.58 |
| Quarter 4 | 6.0 | 6.3 | 5.9 | 0.93 |
Notes: O = obese, NO = non-obese; p values generated using Chi-square.
Results of the GEE model (see Table 2) indicate that residents with severe obesity had an increased odds (odds ratio [OR] = 1.69) of having an indwelling urinary catheter; however, the odds were not statistically significant. The only variable for which a significant association was detected was time; as time (by quarter of the year) progressed, the likelihood of an indwelling urinary catheter was significantly lower (p = 0.04). In addition to severe obesity (BMI > 35), two other variables trended toward a statistically significant association with indwelling urinary catheter use: gender and race. There was a trend toward females being less likely (OR = 0.67, p = 0.09) to have an indwelling urinary catheter than males. There was also a trend toward African Americans being more likely (OR = 1.6, p = 0.08) to have an indwelling urinary catheter than Caucasians.
Discussion
The use of indwelling urinary catheters among older residents in federally certified long-term care facilities in Arkansas in 2008 at admission was 16.8% among all new residents, and was significantly higher among newly admitted obese, older long-term care facility residents (19.4%). These rates were considerably higher than the national quality benchmark for indwelling urinary catheter (Rantz et al., 2000). However, over one year, the use of indwelling urinary catheters among older longterm care facility residents, both obese and non-obese, decreased substantially, with no statistical difference persisting among residents based on obesity status. Federal guidelines call for minimal use of indwelling urinary catheters with long-term care facility residents. High indwelling urinary catheter rates at admission, with sharp declines in the following three months, suggest nursing staff, in collaboration with other health care providers and the long-term care facility resident, are able to either achieve continence or implement strategies (other than use of an indwelling urinary catheter) to successfully manage the resident’s UI.
Indwelling urinary catheter use can increase risk for infections, other medical complications (Igawa et al., 2008), and even death (Landi et al., 2004), and are therefore not recommended for the long-term. Findings from the study reported here are congruent with national guidelines and best-practice models that require long-term care facility staff to carefully assess the resident’s need for an indwelling urinary catheter, develop individualized plans of care for catheter removal, and manage UI with a variety of evidence-based interventions that do not include a long-term indwelling urinary catheter (e.g., scheduled or prompted voiding, judicious medication use for overactive bladder or urgency UI, behavioral strategies) CDC/National Healthcare Safety Network, 2009; CMS, 2005; Newman & Wein, 2009), as indicated by the sharp decrease in indwelling urinary catheter use found from admission to quarter four. These findings indicate that quality improvement efforts – consistent continence care monitoring and treatment by nursing staff – can improve long-term care and resident outcomes. Counter to our hypothesis and previous research (Rogers et al., 2008), we did not detect a high likelihood for the use of indwelling urinary catheters among severely obese, older long-term care facility residents compared to those of normal weight, except at admission. Our study did not identify the location from which new residents were admitted (e.g. hospital or home). Admission from one location versus another may explain differences in indwelling urinary catheter rates at admission and warrants further investigation.
Despite negative consequences and national guidelines, little evidence exists regarding the consequences or any potential benefits of indwelling urinary catheter use in an obese longterm care facility population. Bradway et al. (2010) observed that some obese long-term care facility residents and their caregivers may prefer indwelling urinary catheters over other incontinence control strategies to minimize the day-to-day bathing and skin care challenges associated with using absorbent pads and reduce barriers to engaging with others residents. This observation may account for the higher odds (albeit not significantly different) for indwelling urinary catheter usage among obese long-term care facility residents found in the current study. However, the current study did not examine individual patient or caregiver preferences for UI management. Future research should examine this issue further with obese long-term care facility residents taking into account this limitation of the current study by assessing indwelling urinary catheter usage rates, positive and negative outcomes of catheterization, and patient and caregiver preferences in choosing UI management strategies. Further, future research should also support development and testing of protocols for continence care and best practices associated with indwelling urinary catheter use in obese long-term care facility residents.
Finally, male long-term care facility residents were more likely than female long-term care facility residents to have an indwelling urinary catheter, and African-American long-term care facility residents were more likely than Caucasian long-term care facility residents to have an indwelling urinary catheter. The increased likelihoods were not statistically significant but could have implications for future research. Older men are at high risk for urinary retention due to prostate disease (Meigs et al., 1999), which could explain the higher use of indwelling urinary catheters among this group. However, in numerous studies of both community-dwelling and long-term care facility older adults, women are disproportionately affected by UI (Aslan, Beji, Erkan, Yalcin, & Gungor, 2009; Boyington et al., 2007; Goode et al., 2008; Landefeld et al., 2008; Moore & Gray, 2004). How or if this relates to gender differences in indwelling urinary catheter use in long-term care facility residents requires further exploration. In addition, relatively little is known about racial differences in UI, particularly in the long-term care facility setting. In one study (Boyington et al., 2007), African-American longterm care facility residents were more likely to have UI than their Caucasian counterparts (OR = 1.07, 95% Cl: 1.01-1.14) with a significantly higher prevalence in specific regions of the United States; indwelling urinary catheter use was not described in that study. To our knowledge, racial differences in UI and indwelling urinary catheter use between obese and non-obese long-term care facility residents have not been described. This is strongly recommended as an area for future research.
Limitations
There are several limitations to this work that should be noted. First, this study was unable to identify why a catheter was in place and for how long it had been in place at the time of admission. It is possible that the catheter was in place for a medical reason, such as to prevent urine contamination while treating a non-healing wound. Being able to differentiate the reason(s) for catheterization in the analysis would have been helpful in identifying the characteristics of residents who were inappropriately catheterized and determining the duration of indwelling urinary catheter use in our study subjects. Finer detail on factors associated with indwelling urinary catheters, such as duration of use, would add important information useful to caregivers involved in developing interventions for catheter removal and targeting other residents at highest risk for indwelling urinary catheters.
Second, this study was limited to data from long-term care facilities in one state and from one year. Additional data from more states and from multiple years would allow trends in catheterization to be monitored.
Conclusion/Recommendations
This study examined the association between indwelling urinary catheter usage and obesity among long-term care facility residents. The results of this study determined that there are higher rates of indwelling urinary catheter usage at admission overall and significantly higher rates of indwelling urinary catheter usage if obesity is present at the time of admission to a longterm care facility. However, indwelling urinary catheter usage rates declined within 12 months after admission, and statistical differences associated with obesity disappeared. These results suggest that long-term care facility staff are able to assist residents to achieve continence or employ alternate strategies to address persistent incontinence.
Despite these positive findings, additional research for this study population should be performed. Obesity has been correlated to other health conditions, and the effect obesity has with or without other co-morbidities on incontinence is unknown. The type of admission to the long-term care facility may have an impact on the presence of an indwelling urinary catheter; data from residents admitted from acute care facilities may have a higher prevalence of indwelling urinary catheter than those admitted from home. The intervention(s) employed by the staff of the longterm care facility should be evaluated, as this will determine which intervention is most successful. Comparison of any intervention to the standard practice will identify the strength, cost savings, and timing of the intervention. While the most appropriate evidence-based care has yet to be determined, results of this study indicate that the use of indwelling urinary catheters among long-term care facility residents can be decreased.
Research Summary.
Background/Objectives
Use of indwelling urinary catheters among residents of long-term care facilities is low and within recommended thresholds. Utilization rates may be different by individual characteristics, including obesity status. We hypothesized that the challenges of providing continence care for obese (body mass index ≥ 30) long-term care facility residents might increase the use of indwelling urinary catheters among these residents.
Design
Longitudinal cohort design.
Setting
All federally certified long-term care facilities in Arkansas.
Participants
All older adults (N = 3,879) admitted to federally certified long-term care facilities in Arkansas in quarter one of 2008.
Measurements
Minimum Data Set assessments at admission and at each quarter were used to determine indwelling urinary catheter use and to obtain height and weight to calculate body mass index.
Results
There were significantly higher rates of indwelling urinary catheter use among obese residents at admission and in the second quarter of the year. However, no differences between obese and non-obese residents were detected in the third and fourth quarter when usage rates were nearly the same.
Conclusions
This research found initial differences in the usage of indwelling urinary catheters among long-term care facility residents by weight status, with a higher percentage of obese residents having indwelling urinary catheters than non-obese residents over the six months post-admission. Although lower usage rates of indwelling urinary catheters are preferred for clinical reasons, obese long-term care facility residents may prefer them to other incontinence strategies, which should be explored in future research.
Level – II
(Polit & Beck, 2012)
Acknowledgments
The authors acknowledge support from the Arkansas Center for Minority Health Disparities, funded by the National Institute for Minority Health Disparities under award 5PO20MD002329.
Contributor Information
Holly C. Felix, University of Arkansas for Medical Sciences, Little Rock, AR.
Jeffrey D. Thostenson, University of Arkansas for Medical Sciences, Little Rock AR.
Zoran Bursac, University of Arkansas for Medical Sciences, Little Rock, AR.
Christine Bradway, University of Pennsylvania School of Nursing, Philadelphia, PA; and a member of the Urologic Nursing Editorial Board.
References
- Abt Associates, Inc. Notional nursing home quality measures user’s manual. Cambridge MA: 2004. [Google Scholar]
- Aslan E, Beji NK, Erkan HA, Yalcin O, Gungor F. The prevalence of and the related factors for urinary and fecal incontinence among older esiding in nursing homes. Journal of Clinical Nursing. 2009;18:3290–3298. doi: 10.1111/j.1365-2702.2009.02936.x. [DOI] [PubMed] [Google Scholar]
- Boyington J, Howard D, Carter-Edwards L, Gooden K, Erdem N, Jallah Y, Busby-Whitehead J, et al. Differences in resident characteristics and prevalence of urinary incontinence in nursing homes in the southeastern United States. Nursing Research. 56(2):97–107. doi: 10.1097/01.NNR.0000263969.08878.51. [DOI] [PubMed] [Google Scholar]
- Bradway C, Miller E, Heivly A, Fleshner I. Continence care for obese nursing home residents. Urologic Nursing. 2010;30(2):121–129. [PubMed] [Google Scholar]
- Capitman J, Leutz W, Bishop C, Casler R. Long-term care quality: Historical overview and current initiatives. Waltham, MA: Schneider Institute for Health Policy, Heller School for Social Policy and Management, Brandeis University; 2005. [Google Scholar]
- Centers for Disease Control and Prevention (CDG)/National Healthcare Safety Network. Catheter-associated urinaryr tract infections (CAUTI) event. Atlanta: CDC; 2009. [Google Scholar]
- Centers for Medicare & Medicaid Services (CMS) CMS manual system: Pub 100-07 state operations provider certification. Washington, DC: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- Centers for Medicare & Medicaid Services (CMS) Nursing home compare. 2011 Retrieved from http://www.medicare.gov/NHCompare/Include/DataSection/Questions/SearchCriteriaNEW.asp?version=default&browser=IE%7C8%7CWinXP&1anguage=English&defaultstatus=0&agelist=Home&CookiesEnabledStatus=True.
- Doughty D, Kisanga J. Regulatory guidelines for bladder management in long-term care. Journal of Wound, Ostomy Continence Nursing. 2010;37:399–411. doi: 10.1097/WON.0b013e3181e3a32c. [DOI] [PubMed] [Google Scholar]
- Elkins J, Whitmer R, Sidney S, Sorel M, Yaffe K, Johnston S. Midlife obesity and long-term risk of nursing home admission. Obesity. 2006;14(8):1472–1478. doi: 10.1038/oby.2006.167. [DOI] [PubMed] [Google Scholar]
- Felix H. Personal care assistance needs of obese elders entering nursing homes. Journal of the American Medical Directors Association. 2008;9(5):319–326. doi: 10.1016/j.jamda.2008.01.011. [DOI] [PubMed] [Google Scholar]
- Flegal K, Carroll M, Ogden C, Curtin L. Prevalence and trends in obesity among U.S. adults. 1999-2008. Journal of the American Medical Association. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Goode PS, Burgio KL, Redden DT, Markland A, Richter HE, Sawyer P, Allman RM. Population based study of incidence and predictors of urinary incontinence in black and white older adults. The Journal of Urology. 2008;179:1449–1454. doi: 10.1016/j.juro.2007.11.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunskaar S. A systematic review of overweight and obesity as risk factors and targets for clinical intervention for urinary incontinence in women. Neurourology and Urodynamics. 2008;27(8):749–757. doi: 10.1002/nau.20635. [DOI] [PubMed] [Google Scholar]
- Igawa Y, Wyndaele JJ, Nishizawa O. Catheterization: Possible complications and their prevention and treatment. International Journal of Urology. 15:481–85. doi: 10.1111/j.1442-2042.2008.02075.x. [DOI] [PubMed] [Google Scholar]
- Landefeld C, Bowers B, Feld A, Hartmann K, Hoffman E, Ingber M, Trock BJ. National Institutes of Health state of the science conference statement: Prevention of fecal and urinary incontinence in adults. Annals of Internal Medicine. 2008;148:449–458. doi: 10.7326/0003-4819-148-6-200803180-00210. [DOI] [PubMed] [Google Scholar]
- Landi F, Cesari M, Onder G, Zamboni V, Barillaro C, Lattanzio F, Bemabel R. Indwelling urethral catheter and mortality in frail elderly women living in community. Neurourology and Urodynamics. 2004;23(7):697–701. doi: 10.1002/nau.20059. [DOI] [PubMed] [Google Scholar]
- Meigs JB, Barry MJ, Giovannucci E, Rimm EB, Stampfer MJ, Kawachi I. Incidence rates and risk factors for acute urinary retention: The Health Professionals Follow-Up Study. Journal of Urology. 1999;162:376–382. [PubMed] [Google Scholar]
- Moore KN, Gray M. Urinary incontinence in men: Current status and future directions. Nursing Research. 2004;53(Suppl):S36–S41. doi: 10.1097/00006199-200411006-00006. [DOI] [PubMed] [Google Scholar]
- Newman DK, Wein AJ. Managing and treating urinary’ incontinence. 2. Baltimore: Health Professions Press; 2009. [Google Scholar]
- National Heart, Lung and Blood Institute (NHLBI) Obesity Education Initiative Expert Panel. Clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults: The evidence report. Washington DC: National Institutes of Health; 1998. [Google Scholar]
- Rantz M, Petroski G, Madsen R, Mehr D, Popejoy L, Hicks L, Grando V. Setting thresholds for quality indicators derived from MDS data for nursing home quality improvement reports: An update. Journal of Quality Improvement. 2000;20(2):101–110. doi: 10.1016/s1070-3241(00)26008-2. [DOI] [PubMed] [Google Scholar]
- Rogers M, Mody L, Kaufman S, Fries B, McMahon L, Saint S. Use of urinary collection devices in skilled nursing facilities in five states. Journal of the American Geriatrics Society. 2008;56:854–861. doi: 10.1111/j.1532-5415.2008.01675.x. [DOI] [PubMed] [Google Scholar]
- Valiyeva E, Russell L, Miller J, Safford M. Lifestyle-related risk factors and risk of future nursing home admission. Archives of Internal Medicine. 2006;166:985–990. doi: 10.1001/archinte.166.9.985. [DOI] [PubMed] [Google Scholar]
- Wunderlich G, Kohler P. Improving the quality of long-term care. Washington, DC: NAP; 2001. [PubMed] [Google Scholar]
- Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized controlled trial. Journal of the American Medical Association. 1999;281:613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Brooten DA, Campbell RL, Maislin GM, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: A randomized clinical trial. Journal of the American Geriatrics Society. 2004;52:675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- Naylor M, Brooten D, Jones R, Lavizzo-Mourev R, Mezey M, Pauly M. Comprehensive discharge planning for the hospitalized elderly: A randomized clinical trial. Annals of Internal Medicine. 1994;120:999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Hirschman KB, Bowles KH, Bixby MB, Konick-McMahan J, Stephens C. Care coordination for cognitively impaired older adults and their caregivers. Home Health Care Semces Quarterly. 2007;26:57–78. doi: 10.1300/J027v26n04_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor MD, Hirschman KB, Hanlon AL, Bowles KH, Bradway C, McCauley KM. Enhancing care coordination for cognitively impaired older adults and their family caregivers. The Gerontologist. 2010;50(Suppl. 1):50. doi: 10.1093/geront/gnq115. [DOI] [Google Scholar]
- Naylor MD, Stephens C, Bowles KH, Bixby MB. Cognitively impaired older adults: From hospital to home. American Journal of Nursing. 2005;105:52–61. doi: 10.1097/00000446-200502000-00028. [DOI] [PubMed] [Google Scholar]
- Rudolph JL, Zanin NM, Jones RN, Marcantonio ER, Fong TG, Yang FM, Inouye SK. Hospitalization in community-dwelling persons with Alzheimer’s disease: Frequency and causes. Journal of the American Geriatrics Society 58. 2010:1542–1548. doi: 10.1111/j.1532-5415.2010.02924.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuccala G, Pedone C, Cesari M, Onder G, Pahor M, Marzetti E, Bernabei R. The effects of cognitive impairment on mortality among hospitalized patients with heart failure. American Journal of Medicine. 2003;115:97–103. doi: 10.1016/S0002-9343(03)00264-X. [DOI] [PubMed] [Google Scholar]


