Abstract
Introduction
Gender-based violence (GBV) threatens women’s health and safety. Few prospective studies examine physical and sexual violence predictors. Baseline/index GBV history and polyvictimization (intimate partner violence, non-partner sexual assault, and childhood sexual abuse) were characterized. Predictors of physical and sexual violence were evaluated over follow-up.
Methods
HIV-infected and uninfected participants (N=2,838) in the Women’s Interagency HIV Study (WIHS) provided GBV history; 2,669 participants contributed 26,363 person years of follow-up from 1994 to 2014. In 2015–2016, multivariate log-binomial/Poisson regression models examined violence predictors including GBV history, substance use, HIV status, and transactional sex.
Results
Overall, 61% reported index GBV history; over follow-up, 10% reported sexual and 21% reported physical violence. Having experienced all three forms of past GBV posed greatest risk (adjusted incidence rate ratio [AIRR]physical=2.23, 95% CI=1.57, 3.19; AIRRsexual=3.17, 95% CI=1.89, 5.31). Time-varying risk factors included recent transactional sex (AIRRphysical=1.29, 95% CI=1.03, 1.61; AIRRsexual=2.98, 95% CI=2.12, 4.19), low income (AIRRphysical=1.22, 95% CI=1.01, 1.45; AIRRsexual=1.38, 95% CI=1.03, 1.85), and marijuana use (AIRRphysical=1.43, 95% CI=1.22, 1.68; AIRRsexual=1.57, 95% CI=1.19, 2.08). For physical violence, time-varying risk factors additionally included housing instability (AIRR=1.37, 95% CI=1.15, 1.62); unemployment (AIRR=1.38, 95% CI=1.14, 1.67), exceeding seven drinks/week (AIRR=1.44, 95% CI=1.21, 1.71), and use of crack, cocaine, or heroin (AIRR=1.76, 95% CI=1.46, 2.11).
Conclusions
Urban women living with HIV and their uninfected counterparts face sustained GBV risk. Past experiences of violence create sustained risk. Trauma-informed care, and addressing polyvictimization, structural inequality, transactional sex, and substance use treatment, can improve women’s safety.
Introduction
Gender-based violence (GBV), that is, violence perpetrated based on sex or gender identity,1 has been recognized as a public health and human rights issue since 1993.2 Globally, an estimated one in three women experiences physical or sexual violence.3 Resulting physical, sexual, and mental health morbidities are well established,4,5 and include sexual and drug-related HIV risk behavior6–8 and incident infection.9 The 2015 U.S. National HIV/AIDS Strategy prioritized addressing violence and trauma in mitigating HIV risk for women and girls.10
Prospective research on risk factors for physical and sexual violence is limited. In addition to demographics and relationship characteristics, past experiences of violence are implicated.11–13 Dominant forms of GBV include intimate partner violence (IPV),14 which is responsible for more than one third of homicides of women globally and in the U.S.15,16 Women also experience non-partner sexual assault (NPSA), that is, forced and coercive sexual experiences from non-partners. Abuse can begin early, as in childhood sexual abuse (CSA). GBV experiences can interact and accumulate over time,6,11,13,17–20 thus a polyvictimization lens—one that explores the intersections of victimization across multiple domains—has been recommended to understand the accumulation of trauma and its implications for health and safety.21
Structural and behavioral factors can impart risk for violence. Substance use is linked with violence via complex, mutually reinforcing pathways,17,20 whereby it can enable abuse17,20,22 and serve as a coping mechanism.22–24 These relationships, coupled with the HIV risk therein,6–9 are known as the “Substance Abuse, Violence and AIDS (SAVA) syndemic”, i.e., mutually reinforcing epidemics that synergistically perpetuate risk and compromise health.25–27 Structural factors including financial and housing instability28 can create risk where women compromise safety given limited options for housing, or economic security.29 Severe violence has been documented among women involved in transactional sex or sex work30,31; it remains unclear whether trading sex is a violence risk factor.
Preventing and responding to GBV are global priorities. This study clarifies predictors of physical and sexual violence. To account for cumulative abuse exposure, the polyvictimization framework considers specific forms and combinations of past GBV, extending summary score approaches.32 Time-varying exposures include substance use, transactional sex, and structural determinants including housing and economic instability. The objectives were to:
characterize history of leading GBV forms and polyvictimization (specifically IPV, NPSA, or CSA) at baseline/index; and
describe predictors of physical and sexual violence experienced during 20 years of follow-up, in a cohort of urban U.S. women living with HIV and their uninfected counterparts.
Methods
Study Population
The Women’s Interagency HIV Study (WIHS) is the largest ongoing prospective cohort study of HIV infection among U.S. women, and includes a demographically matched uninfected comparison group; details are elsewhere.33–35 Six urban clinical consortia recruited participants in the first and largest wave; more than half of those women were living in poverty at baseline.35 A total of 4,137 (3,067 HIV+, 1,070 HIV−) participants were enrolled for baseline and semiannual visits following informed consent in three waves: 2,623 (2,054 HIV+, 569 HIV−) in 1994–1995, 1,143 (737 HIV+, 406 HIV−) in 2001–2002, and 371 (276 HIV+, 95 HIV−) in 2011–2012. All procedures were approved by IRBs at participating sites. GBV data were collected from women aged ≥18 years. Most sites collected these data starting in 1994; in 2006, the San Francisco site obtained IRB approval to obtain retrospective and prospective abuse data. The index visit was defined as the visit when GBV history was assessed. The baseline visit served as the index visit for most (n=1,975); for some (n=863) it was a later visit. For cross-sectional analysis of index data, a total of 2,838 women aged ≥18 years were included; of these, 2,669 women provided 26,363 person years of follow-up.
Outcome Measures: Characterization of Gender-Based Violence History and Incident Events
Enzyme-linked immunosorbent assay determined HIV infection with western blot confirmation, repeated at each visit for seronegative women. A standardized interviewer-administered survey conducted at enrollment and semiannually collected demographics (age, race/ethnicity, marital status), housing status, household income, employment, sexual identity, and transactional sex (sex for drugs, money, or shelter; per UNAIDS definition of sex work, which specifies trade of sex for money or other goods, including occasional transactions).36 A substance use inventory captured frequency and method where relevant of the following substances since the last visit: alcohol, marijuana, cocaine, crack, and heroin. Alcohol use frequency was dichotomized at more than seven drinks/week37; crack, cocaine, and heroin were grouped for analysis.
Violence victimization was behaviorally assessed consistent with the Revised Conflict Tactics Scale.38 Participants were asked:
At any time in your life, has anyone ever pressured or forced you to have sexual contact, defined as touching your sexual parts, you touching their sexual parts, or sexual intercourse?
Have you ever experienced serious physical violence (physical harm by another person), defined as hurt by a person using an object or slapped, hit, punched, or kicked?
Assessments referred to “anyone”; follow-up measures at baseline/index classified perpetrator(s) and age at onset. These assessments enabled definition of three forms of past GBV1:
CSA by any perpetrator before age 13 years;
NPSA by any perpetrator other than an intimate partner starting at age 13 years or older; and
IPV starting at age 13 years or older.
Although CSA is often defined as sexual violence prior to age 18 years,6 national data indicate that adolescents experience IPV14; hence, sexual assault occurring after age 13 years is classified as IPV or NPSA based on perpetrator designation. Women reporting abuse were referred to local crisis services.
Perpetrator assessment was not sustained over follow-up. Thus, for longitudinal analysis, physical and sexual violence were defined as two distinct, binary outcomes for each annual visit, based on the behavioral measures described above. Women contributed incident abuse experiences at multiple time points.
Statistical Analysis
Characterization of index GBV history
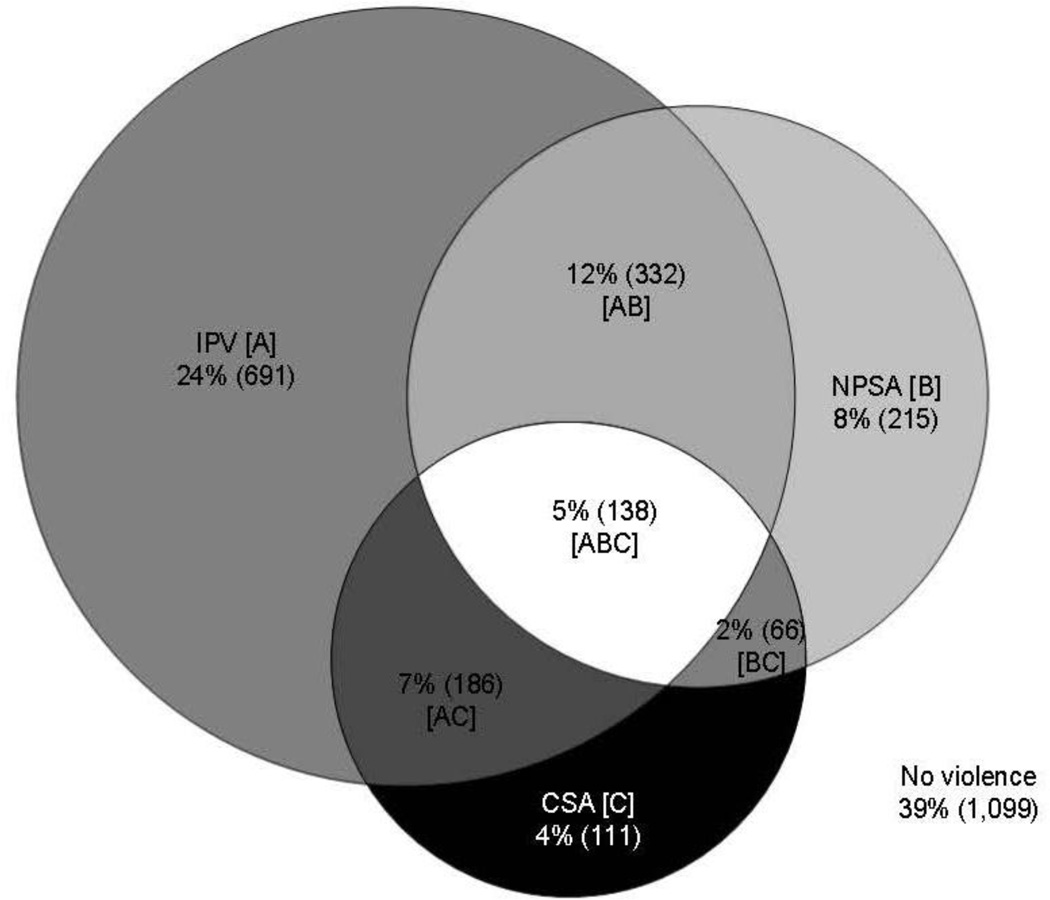
Analysis was conducted in 2015–2016. Prevalence was calculated for CSA, NPSA, and IPV and any of the three. Chi-square and Wilcoxon rank sum tests compared demographics, substance use, and structural determinants across GBV forms. A Venn diagram was constructed to describe GBV polyvictimization. Single-chain Markov chain Monte Carlo multiple imputation methods completed missing data for 338 participants (12%) with missing data (≤5% for each GBV form). Thirty complete data sets were generated; average values rounded to the nearest whole number generated frequencies.
Longitudinal analysis to predict physical and sexual violence over follow-up
Physical and sexual violence incidence, respectively, was calculated. Participants could contribute multiple incidences of violence; visits with and without each outcome were compared using predictors derived from the visit prior for clarity in temporal ordering. For each outcome, three multivariate log-binomial/Poisson regression models evaluated the effect of index GBV history on subsequent risk:
dose response (zero to three index risks) with the three potential risks being CSA, NPSA, and IPV;
main effects (none, CSA, NPSA, IPV); and
specific index GBV polyvictimization clusters.
Models adjusted for non-varying factors: age at index, year of index, race/ethnicity, HIV status, education, sexual identity, index history of injected and non-injected drug use and transactional sex; and time varying factors: years since index, marital status, housing status, annual household income, employment, substance use, and transactional sex. To account for co-occurrence of physical and sexual violence within visit, each model adjusted for the other form of violence.
Single-chain Markov-chain Monte Carlo multiple imputation methods handled missing data39 for predictors and outcomes, for 3,345 records (12%). Data sets were transformed from long to wide format to generate 30 complete data sets, and transformed back to long format.40,41 Separate imputations were run based on years of follow-up. Generalized estimating equations were used to adjust SEs to account for repeated measures.42 Models were run for each of the 30 imputed data sets and results were combined using Rubin’s estimator of the variance.43 Analyses were conducted in SAS, version 9; p-values <0.05 were considered statistically significant.
Results
Overall, 61% of participants (N=2,838) reported a GBV history at index, 18% reported CSA, 26% reported NPSA, and 47% reported IPV (Table 1; categories not mutually exclusive). Lifetime GBV history was prevalent among white women (72%), as well as women who did not identify as heterosexual (74%), were currently homeless or unstably housed (80%), had an annual household income of ≤$18,000 (64%), and were unemployed (64%). GBV history was highly prevalent (81%) among women with a transactional sex history. GBV history was more prevalent among women using alcohol in excess of seven drinks/week (69%), and prior or recent (past 6 months) injection and non-injection drug use, marijuana, and crack/cocaine/heroin use, as compared with non-users, respectively.
Table 1.
Index Characteristics by GBV Reported at Index
| CSAb | NPSAc | IPVd | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | None (ref) |
Any GBV |
No | Yes | No | Yes | No | Yes | |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Characteristica | 2,838 | 1,099 (39) |
1,739 (61) |
1,238 (44) |
501 (18) |
988 (35) |
751 (26) |
392 (14) |
1,347 (47) |
|
Timing of enrollment and follow-up |
|||||||||
| Year of index visit | *** | *** | *** | *** | |||||
| 1994–1995 | 1,642 (58) |
539 (33) |
1,103 (67) |
752 (46) |
351 (21) |
593 (36) |
510 (31) |
284 (17) |
819 (50) |
| 2006–2007 | 863 (30) |
439 (51) |
424 (49) |
330 (38) |
94 (11) |
266 (31) |
158 (18) |
72 (8) |
352 (41) |
| 2011–2012 | 333 (12) |
121 (36) |
212 (64) |
156 (47) |
56 (17) |
129 (39) |
83 (25) | 36 (11) |
176 (53) |
| Years of follow-up, median (IQR) |
8 (4– 17) |
8 (4– 10) |
8 (4– 18)** |
8 (4– 18) |
8 (4– 18) |
8 (4– 18) |
8 (4– 18)** |
8 (4– 20) |
8 (4– 18)** |
| Demographics | |||||||||
| Age, median (IQR) | 37 (32–43) |
37 (30– 43) |
** 38 (32– 44) |
38 (32– 44) |
** 37 (32– 43) |
38 (32– 44) |
** 37 (32– 43) |
36 (31– 42) |
*** 38 (33– 44) |
| Race/ethnicity | ** | ** | *** | *** | |||||
| African-American | 1,853 (65) |
754 (41) |
1,099 (59) |
787 (42) |
312 (17) |
6,359(3 4) |
460 (25) |
247 (13) |
852 (46) |
| Hispanic/Latina | 546 (19) |
216 (40) |
330 (60) |
232 (42) |
97 (18) |
203 (37) |
127 (23) |
69 (13) |
261 (48) |
| Asian/Native American/Other |
99 (3) | 33 (33) | 66 (67) | 45 (45) | 21 (21) | 43 (43) | 23 (23) | 8 (8) | 58 (59) |
| White | 340 (12) |
96 (28) |
244 (72) |
174 (51) |
70 (21) |
103 (30) |
141 (41) |
68 (20) |
176 (52) |
| Sexual preference | *** | *** | *** | *** | |||||
| Heterosexual | 2450 (86) |
997 (41) |
1453 (59) |
1066 (44) |
387 (16) |
864 (35) |
589 (24) |
308 (13) |
1145 (47) |
| Lesbian/Bisexual/Othe r |
388 (14) |
102 (26) |
286 (74) |
172 (44) |
114 (29) |
124 (32) |
162 (42) |
84 (22) |
202 (52) |
| Structural factors | |||||||||
| Marital status | |||||||||
| Married or partnered | 958 (34) |
392 (41) |
566 (59) |
400 (42) |
166 (17) |
322 (34) |
244 (25) |
131 (14) |
435 (45) |
| Not married or partnered |
1,880 (66) |
707 (38) |
1,173 (62) |
838 (45) |
335 (18) |
666 (35) |
507 (27) |
261 (14) |
912 (49) |
| Education | |||||||||
| High school or higher | 1,832 (65) |
687 (38) |
1,145 (63) |
812 (44) |
333 (18) |
655 (36) |
490 (27) |
264 (14) |
881 (48) |
| Less than high school | 1,006 (35) |
412 (41) |
594 (59) |
426 (42) |
168 (17) |
333 (33) |
261 (26) |
128 (13) |
466 (46) |
| Housing status | *** | *** | *** | *** | |||||
| Stable | 2,588 (91) |
1,048 (40) |
1540 (60) |
1106 (43) |
434 (17) |
882 (34) |
658 (25) |
358 (14) |
1,182 (46) |
| Homeless or unstable | 250 (9) | 51 (20) |
199 (80) |
132 (53) |
67 (27) |
106 (42) |
93 (37) | 34 (14) |
165 (66) |
| Household annual income | *** | *** | *** | *** | |||||
| >$18,000 | 845 (30) |
388 (45) |
461 (55) |
340 (40) |
121 (14) |
250 (30) |
211 (25) |
121 (14) |
343 (40) |
| ≤$18,000 | 1,993 (70) |
715 (36) |
1,278 (64) |
898 (45) |
380 (19) |
738 (37) |
540 (27) |
269 (14) |
1,004 (51) |
| Employment status | *** | *** | *** | *** | |||||
| Employed | 860 (30) |
394 (46) |
466 (54) |
336 (39) |
130 (15) |
261 (30) |
205 (24) |
123 (14) |
343 (40) |
| Unemployed | 1,978 (70) |
705 (36) |
1,273 (64) |
902 (46) |
371 (19) |
727 (37) |
546 (28) |
269 (14) |
1,004 (51) |
|
Transactional sex and HIV status |
|||||||||
| Transactional sex ever | *** | *** | *** | *** | |||||
| Not reported | 1,764 (62) |
895 (51) |
869 (49) |
660 (37) |
209 (12) |
582 (33) |
287 (16) |
189 (11) |
680 (39) |
| Reported | 1,074 (38) |
204 (19) |
870 (81) |
578 (54) |
292 (27) |
406 (38) |
464 (43) |
203 (19) |
667 (62) |
| HIV status | |||||||||
| Seronegative | 740 (26) |
299 (40) |
441 (60) |
323 (44) |
118 (16) |
249 (34) |
192 (26) |
111 (15) |
330 (45) |
| Seropositive | 2,098 (74) |
800 (38) |
1,298 (62) |
915 (44) |
383 (18) |
739 (35) |
559 (27) |
281 (13) |
1,017 (48) |
| Substance use | |||||||||
| Alcohol use | ** | * | * | ** | |||||
| 7 or fewer drinks/week | 2,436 (86) |
975 (40) |
1461 (60) |
1,038 (43) |
423 (17) |
831 (34) |
630 (26) |
342 (14) |
1,119 (46) |
| More than 7 drinks/ week |
402 (14) |
124 (31) |
278 (69) |
200 (50) |
78 (19) |
157 (39) |
121 (30) |
50 (12) |
228 (57) |
| Any drug use | *** | *** | *** | *** | |||||
| Never | 564 (20) |
360 (64) |
204 (36) |
166 (29) |
38 (7) |
141 (25) |
63 (11) | 50 (9) |
154 (27) |
| More than 6 months ago |
1,271 (45) |
452 (36) |
819 (64) |
574 (45) |
245 (19) |
468 (37) |
351 (28) |
173 (14) |
646 (51) |
| Past 6 months | 1,003 (35) |
287 (29) |
716 (71) |
498 (50) |
218 (22) |
379 (38) |
337 (34) |
169 (17) |
547 (55) |
| Injected drug use | *** | *** | *** | *** | |||||
| Never | 1,947 (69) |
877 (45) |
1,070 (55) |
788 (40) |
282 (14) |
658 (34) |
411 (21) |
249 (13) |
821 (42) |
| More than 6 months ago |
722 (25) |
185 (26) |
537 (74) |
356 (49) |
181 (25) |
263 (36) |
274 (38) |
114 (16) |
423 (59) |
| Past 6 months | 169 (6) | 37 (22) |
132 (78) |
92 (55) | 38 (22) | 66 (39) | 66 (39) | 29 (17) |
103 (61) |
| Non-injected drug use | *** | *** | *** | *** | |||||
| Never | 623(22) |
390 (63) |
233 (37) |
190 (31) |
43 (7) |
158 (25) |
75 (12) | 55 (9) |
178 (29) |
| More than 6 months ago |
1,268 (45) |
440 (35) |
828 (65) |
576 (45) |
252 (20) |
474 (37) |
354 (28) |
174 (14) |
654 (52) |
| Past 6 months | 947 (33) |
269 (28) |
678 (72) |
472 (50) |
206 (22) |
356 (38) |
322 (34) |
163 (17) |
515 (54) |
| Marijuana use | *** | *** | *** | *** | |||||
| Never | 778 (27) |
456 (59) |
322 (41) |
259 (33) |
63 (8) |
211 (27) |
111 (14) |
74 (10) |
248 (32) |
| More than 6 months ago |
1,411 (50) |
453 (32) |
958 (68) |
656 (46) |
302 (21) |
538 (38) |
420 (30) |
210 (15) |
748 (53) |
| Past 6 months | 649 (23) |
190 (29) |
459 (71) |
323 (50) |
136 (21) |
239 (37) |
220 (34) |
108 (17) |
351 (54) |
| Crack/Cocaine/Heroin | *** | *** | *** | *** | |||||
| Never | 1,052 (37) |
599 (57) |
453 (43) |
337 (32) |
116 (11) |
309 (29) |
144 (14) |
109 (10) |
344 (33) |
| More than 6 months ago |
1,145 (40) |
340 (30) |
805 (70) |
559 (49) |
246 (21) |
438 (38) |
367 (32) |
173 (15) |
632 (55) |
| Past 6 months | 641 (23) |
160 (25) |
481 (75) |
342 (53) |
139 (22) |
241 (38) |
240 (37) |
110 (17) |
371 (58) |
Notes: Boldface indicates statistical significance
p<0.01;
p<0.001;
p<0.0001.
Overall column shows column percents in parentheses; all other columns show row percents in parentheses.
Multiple imputation was used to complete missing data described in methods.
Three groups are compared: (1) no GBV [None (ref)], (2) NPSA and/or IP but not CSA [No], (3) CSA with or without NPSA and/or IP [Yes]
Three groups are compared: (1) no GBV [None (ref)], (2) CSA and/or IP but not NPSA [No], (3) NPSA with or without CSA and/or IP [Yes]
Three groups are compared: (1) no GBV [None (ref)], (2) CSA and/or NPSA but not IP [No], (3) IP with or without CSA and/or NPSA [Yes]
IQR, interquartile range; GBV, gender-based violence; CSA, childhood sexual abuse; NPSA, non-partner sexual assault; IPV, intimate partner violence
In the absence of other forms of GBV, IPV was the most common profile (24%; Figure 1). History of both IPV and NSPA was reported by 12% of participants. CSA alone was reported by 4%. Stratification by HIV status showed comparable patterns of GBV types (data not shown).
Figure 1.
Polyvictimization Venn diagram depicting GBV exposures at index (n=2,838).a
acells are mutually exclusive
[A] Intimate Partner Violence (IPV); [B] Non-partner Sexual Assault (NPSA); [C] Childhood Sexual Abuse (CSA); [AB] IPV and NPSA; [AC] IPV and CSA; [ABC] IPV, NPSA and CSA; [BC] NPSA and CSA
During follow-up, 10% (266/2,669) reported sexual violence and 21% (567/2,669) reported physical abuse (not shown). The incidence rates were 1.6/100 person years for sexual violence and 3.8/100 person years for physical violence (Table 2). The dose–response model suggested a risk gradient whereby risk of physical or sexual violence over follow-up increased with the number of types of index GBV experiences. The risk conferred based on number of forms of GBV experienced ranged from (adjusted incidence rate ratio [AIRR]sexual=1.44, 95% CI=0.96, 2.14; AIRRphysical=1.60; 95% CI=1.25, 2.04) for one form of index GBV, (AIRRsexual=2.16, 95% CI=1.45, 3.23; AIRRphysical=2.11, 95% CI=1.63, 2.73) for two forms, to (AIRRsexual=3.12, 95% CI=1.86, 5.23; AIRRphysical=2.21, 95% CI=1.55, 3.13) for all three forms of GBV history. In the main effects model, index IPV increased risk for subsequent violence (AIRRsexual=1.69, 95% CI=1.26, 2.26; AIRRphysical=1.38, 95% CI=1.16, 1.65), as did NPSA (AIRRsexual=1.60, 95% CI=1.21, 2.11; AIRRphysical=1.47, 95% CI=1.22, 1.76).
Table 2.
Incidence and Predictors of Sexual and Physical Violence Over Follow-up
| Sexual violence | Physical violence | |||||
|---|---|---|---|---|---|---|
| Incidence rate/100 person years |
Adjusted Incidence Rate Ratio (aIRR)a |
95% CI | Incidence rate/ 100 person years |
Adjusted Incidence Rate Ratio (aIRR)a |
95% CI | |
| Total over the follow-up | 1.6 (425/26,363) |
-- | -- | 3.8 (996/26,363) |
-- | -- |
| Model 1: Dose Response (number of GBV types at index) a | ||||||
| 0 | 0.7 | 1.00 | -- | 1.8 | 1.00 | -- |
| 1 | 1.3 | 1.44 | 0.96–2.14 | 3.4 | 1.60*** | 1.25–2.04 |
| 2 | 2.5 | 2.16*** |
1.45– 3.23 |
5.6 | 2.11**** | 1.63–2.73 |
| 3 | 4.6 | 3.12**** | 1.86–5.23 | 7.4 | 2.21**** | 1.55–3.13 |
| Model 2: Main Effects (type of GBV at index) a | ||||||
| None | 0.7 | 1.00 | -- | 1.8 | 1.00 | -- |
| CSA | 2.4 | 1.17 | 0.88–1.56 | 5.2 | 1.14 | 0.95–1.37 |
| IPV | 2.2 | 1.69*** | 1.26–2.26 | 4.8 | 1.38*** | 1.16–1.65 |
| NPSA | 2.8 | 1.60** | 1.21–2.11 | 6.0 | 1.47**** | 1.22–1.76 |
| Model 3: GBV Polyvictimization groupings at indexa | ||||||
| None | 0.7 | 1.00 | -- | 1.8 | 1.00 | -- |
| CSA only | 0.4 | 0.59 | 0.23–1.51 | 2.0 | 1.12 | 0.71–1.77 |
| IPV only | 1.2 | 1.44 | 0.93–2.23 | 3.2 | 1.61*** | 1.24–2.08 |
| NPSA only | 1.7 | 1.74* | 1.01–2.99 | 4.4 | 1.76** | 1.24–2.48 |
| IPV & NPSA only | 2.9 | 2.45**** | 1.57–3.82 | 6.1 | 2.19**** | 1.64–2.93 |
| CSA with IPV or NPSA | 1.9 | 1.84** | 1.16–2.93 | 4.8 | 2.02**** | 1.50–2.72 |
| IPV, NPSA and CSA | 4.6 | 3.17**** | 1.89–5.31 | 7.4 | 2.23**** | 1.57–3.19 |
| Covariates included in all adjusted models (estimates presented from Model 3) | ||||||
| Timing of enrollment and follow-up | ||||||
| Years from index visit | 0.92**** | 0.90–0.95 | 0.91**** | 0.90–0.93 | ||
| Year of index visit | ||||||
| 1994–1995 | 1.6 | 1.00 | -- | 4.0 | 1.00 | -- |
| 2006–2007 | 1.3 | 0.79 | 0.57–1.10 | 3.1 | 0.74** | 0.60–0.92 |
| 2011–2012 | 2.1 | 1.04 | 0.60–1.80 | 3.3 | 0.69* | 0.48–0.99 |
| Demographics | ||||||
| Age at index visit (per 10 years) | 0.87 | 0.74–1.03 | 0.71**** | 0.63–0.80 | ||
| Race/ethnicity | ||||||
| African-American | 1.7 | 1.03 | 0.69–1.55 | 3.9 | 0.85 | 0.67–1.07 |
| Hispanic/Latina | 0.8 | 0.58* | 0.36–0.96 | 2.9 | 0.67** | 0.50–0.89 |
| Asian/Native American/Other | 3.3 | 1.61 | 0.79–3.26 | 4.4 | 0.76 | 0.49–1.20 |
| White | 1.8 | 1.00 | -- | 4.7 | 1.00 | -- |
| Sexual identity: lesbian/bisexual/other | 2.4 (vs. 1.5) | 1.00 | 0.74–1.37 | 5.7 (vs. 3.5) | 1.12 | 0.92–1.36 |
| Structural factors | ||||||
| Not married or partneredb | 1.8 (vs. 1.3) | 1.34* | 1.02–1.75 | 3.8 (vs. 3.8) | 0.91 | 0.78–1.05 |
| Less than high school education | 1.5 (vs. 1.7) | 0.90 | 0.68–1.18 | 4.3 (vs. 3.5) | 1.01 | 0.85–1.19 |
| Annual income less than $18,000b | 2.0 (vs. 1.0) | 1.38* | 1.03–1.85 | 4.6 (vs. 2.4) | 1.22* | 1.01–1.45 |
| Housing status: unstable or housingb |
3.9 (vs. 1.5) | 1.10 | 0.81–1.48 | 9.5 (vs. 3.4) | 1.37*** | 1.15–1.62 |
| Not employedb | 1.8 (vs. 1.2) | 0.81 | 0.60–1.09 | 4.6 (vs. 2.1) | 1.38** | 1.14–1.67 |
| Transactional sex and HIV status | ||||||
| HIV status | 1.6 (vs. 1.5) | 1.17 | 0.89–1.52 | 3.7 (vs. 4.1) | 0.89 | 0.75–1.07 |
| Transactional sex | ||||||
| Ever, reported at index visit | 2.4 (vs. 1.2) | 0.82 | 0.59–1.15 | 5.6 (vs. 2.7) | 0.99 | 0.80–1.22 |
| Recent transactional sexb | 12.2 (vs. 1.2) |
2.98**** | 2.12–4.19 | 18.2 (vs. 3.3) |
1.29* | 1.03–1.61 |
| Alcohol and drug use | ||||||
| Drank more than 7 drinks per weekb |
2.4 (vs. 1.5) | 0.80 | 0.60–1.07 | 7.6 (vs. 3.1) | 1.44**** | 1.21–1.71 |
| Injected drug use at index visit | 1.9 (vs. 1.5) | 0.96 | 0.71–1.29 | 4.9 (vs. 3.3) | 1.09 | 0.89–1.33 |
| Non-injected drug use at index visit |
1.9 (vs. 0.7) | 1.24 | 0.76–2.02 | 4.4 (vs. 1.5) | 1.30 | 0.95–1.78 |
| Marijuana useb | 3.5 (vs. 1.1) | 1.57** | 1.19–2.08 | 7.8 (vs. 2.7) | 1.43**** | 1.22–1.68 |
| Crack/cocaine/heroin useb | 4.4 (vs. 1.1) | 1.15 | 0.83–1.59 | 10.7 (vs. 2.6) | 1.76**** | 1.46–2.11 |
|
Opposite form of violence, same time period |
-- | 6.56**** | 4.84–8.88 | -- | 4.57**** | 3.70–5.63 |
Note: Boldface indicates statistical significance
p<0.05;
p<0.01;
p<0.001;
p<0.0001
All models adjusted for the full set of covariates presented for model 3.
Time-varying
CSA, childhood sexual abuse; IPV, intimate partner violence; NPSA, non-partner sexual assault
The final model considered GBV polyvictimization clusters. IPV in isolation predicted subsequent violence (AIRRphysical=1.61, 95% CI=1.24, 2.08), as did NPSA in isolation (AIRRsexual=1.74, 95% CI=1.01, 2.99; AIRRphysical=1.76, 95% CI=1.24, 2.48). The combination of IPV and NPSA increased risk for violence (AIRRsexual=2.45, 95% CI=1.57, 3.82; AIRRphysical=2.19, 95% CI=1.64, 2.93), as did the combination of CSA with either IPV or NPSA (AIRRsexual=1.84, 95% CI=1.16, 2.93; AIRRphysical=2.02, 95% CI=1.50, 2.72). Experiencing IPV, NPSA, and CSA most strongly predicted subsequent violence (AIRRsexual=3.17, 95% CI=1.89, 5.31; AIRRphysical=2.23, 95% CI=1.57, 3.19). CSA in isolation did not significantly relate to subsequent violence.
Recent transactional sex was a strong predictor of violence (AIRRsexual=2.98, 95% CI=2.12, 4.19; AIRRphysical=1.29, 95% CI=1.03, 1.61). Relative to non-substance users, risk for violence was heightened after periods of alcohol use in excess of seven drinks weekly (AIRRphysical=1.44, 95% CI=1.21, 1.71), marijuana use (AIRRsexual=1.57, 95% CI=1.19, 2.08; AIRRphysical=1.43, 95% CI=1.22, 1.68), and use of crack, cocaine, or heroin (AIRRphysical=1.76, 95% CI=1.46, 2.11). Risk of violence was increased following time periods characterized by household income <$18,000 (AIRRsexual=1.38, 95% CI=1.03, 1.85; AIRRphysical=1.22, 95% CI=1.01, 1.45), housing instability (AIRRphysical=1.37, 95% CI =.15, 1.62), and unemployment (AIRRphysical=1.38, 95% CI=1.14, 1.67). Years since index provided relative protection (AIRRsexual=0.92, 95% CI=0.90, 0.95; AIRRphysical=0.91, 95% CI=0.90, 0.93). Over time, Hispanic women were less likely to report violence (AIRRsexual=0.58, 95% CI=0.36, 0.96; AIRRphysical=0.67, 95% CI=0.50, 0.89), relative to white women. Experiencing physical violence in a given time period was significantly associated with sexual violence in that same time period (AIRR=6.56, 95% CI=4.84, 8.88); sexual violence was significantly associated with physical violence in that same time period (AIRR=4.57, 95% CI=3.70, 5.63).
Given the associations identified between both substance use and transactional sex with violence, post hoc analyses stratified results by index history of injection drug use. Alcohol use exceeding seven drinks/week, marijuana, and crack, cocaine, or heroin use remained significant risk factors for physical violence among both injectors and non-injectors. Among injectors, recent transactional sex was also a risk factor for physical violence; among non-injectors, periods of housing instability and unemployment were significant risk factors. For sexual violence, transactional sex remained a significant risk factor for both injectors and non-injectors; recent marijuana use predicted sexual violence only for those without an injection history (data not shown).
Discussion
Extensive GBV and GBV polyvictimization were identified in this longstanding cohort of urban women living with HIV and their uninfected counterparts. Polyvictimization conferred significant risk for subsequent physical and sexual violence. More than 61% of participants had experienced at least one type of GBV, and the majority experienced multiple forms. Much of the GBV experienced occurred prior to cohort enrollment, consistent with national data that demonstrate youth as the primary risk period.14 Together, findings demonstrate the need to understand and address polyvictimization for violence prevention and health promotion. Results support the U.S. 2015 National HIV/AIDS Strategy recommendations to address violence and trauma for women both at risk for and living with HIV.10 Meeting the violence-related needs of women and girls within and beyond the context of HIV care and prevention requires a trauma-informed approach—one that is grounded in recognizing and responding to trauma, emphasizes safety, and provides opportunities to regain a sense of control and empowerment.44
In practice, trauma-informed practices routinely and universally inquire about trauma (screening), and respond appropriately by providing support and linkage to care and access to justice, within an environment that is calm, safe, and empowering, and an organizational foundation that supports providers and collaborates with related services.45
Longitudinal results additionally suggest access to safe housing and substance use treatment as potential violence prevention strategies, and identify women who trade sex as a high-risk population for violence prevention and intervention.
Results extend current knowledge on nature and impact of GBV polyvictimization for urban women living with and at risk for HIV. IPV was pervasive with 47% affected, and 24% reporting IPV only, without other forms of violence. The majority of women who had experienced IPV did not report CSA. The most complex index GBV profiles conferred the greatest risk for subsequent violence, demonstrating a persistence of GBV for those highly affected. Importantly, CSA influenced risk differently in the presence or absence of other forms of GBV. The small proportion of participants (4%) who experienced CSA but no other form of GBV had no heightened risk for subsequent violence over follow-up. CSA did confer risk for subsequent physical and sexual violence when experienced with other forms of GBV. Early intervention to interrupt violence trajectories and prevent polyvictimization may confer long-term protective effects and buffer against violence in adulthood. Findings indicate the value of the IPV screening provisions of the Affordable Care Act to identify survivors and link them with support services and safety planning.
Transactional sex was a robust predictor of violence, extending evidence from female sex workers.30,31 Survival biases may have underestimated results: In the U.S., the homicide rate for women in sex work is 17 times higher than the general population46 and transactional sex has been associated with mortality in the Women’s Interagency HIV Study.47 Findings indicate significant unmet safety needs for women who trade sex. Currently, the Violence Against Women Act does not include provisions specific to the sex trade, with the exception of guidance specific to minors. Changes to policy and practice are needed to meet violence-related support and justice needs of women who trade sex, as they are subject to discrimination, police harassment, criminalization, and other barriers to accessing care.30
The Substance Abuse, Violence, and AIDS (SAVA) syndemic25,26 is informed by current results, which extend knowledge on how substance use relates to violence. Although substance use history was not a predictor of subsequent violence in adjusted models, time periods of marijuana, crack, cocaine, or heroin use increased risk. The social or physical environments surrounding substance use may enable risk, substance use may hamper executive function, and the low social status of drug-involved women and demands of addiction may threaten safety or enable sustained violence.17,20,22 Engaging women in drug treatment and maintenance may improve their safety. HIV status did not confer risk for physical or sexual violence victimization, indicating that both low-income urban women living with HIV and their uninfected counterparts are at considerable risk for physical and sexual violence. Polyvictimization profiles were also comparable based on HIV status. Post-hoc analyses revealed recent transactional sex history as a sexual violence risk factor for women both with and without injection drug use history, and recent substance use as physical violence risk factor across both groups. Results indicate the relevance of these factors independent of prior injection drug use.
Results implicating low household income, housing instability, and unemployment as violence risk factors suggest the value of structural interventions including stable, affordable housing for women, and economic and educational means to achieve these goals, to enhance women’s safety. Settings where these services are provided can additionally support survivors by embedding trauma-informed care, violence intervention, and support.
Limitations
Study limitations include lack of data on abuse severity, violence response (i.e., access to and use of support services and criminal justice), social norms tolerant of abuse, and violence perpetrators over the follow-up period. Perpetrator specificity is needed to inform dynamics of IPV versus NPSA, and patterns of abuse in new versus sustained relationships. Multiple experiences of violence reported within a given time period may reflect a singular experience of both physical and sexual violence, or distinct experiences. The non-probability sample limits generalizability; results are best generalized to urban U.S. women in high-prevalence settings. A more nuanced understanding of the sex trade would aid in interpretation of findings. Substance use assessments characterized use rather than substance use disorder, and mental health diagnosis data were not available.
Conclusions
This study demonstrates entrenched GBV among urban women living with HIV and their uninfected counterparts. Polyvictimization is a core risk factor for physical and sexual violence, which are leading determinants of health and well-being for U.S. women. Women with abuse histories have persistent needs for violence prevention and intervention. Violence prevention and health promotion strategies for women must address accumulated trauma, underlying structural drivers of economic vulnerability, and persistent substance use to improve women’s health and safety.
Acknowledgments
This work was supported by the National Institute on Drug Abuse (NIDA; R03DA03569102), and the Johns Hopkins University Center for AIDS Research (1P30AI094189). Data in this manuscript were collected by the Women’s Interagency HIV Study (WIHS). The contents of this publication are solely the responsibility of the authors and do not represent the official views of NIH. WIHS (Principal Investigators): UAB-MS WIHS (Michael Saag, Mirjam-Colette Kempf, and Deborah Konkle-Parker), U01-AI-103401; Atlanta WIHS (Ighovwerha Ofotokun and Gina Wingood), U01-AI-103408; Bronx WIHS (Kathryn Anastos), U01-AI-035004; Brooklyn WIHS (Howard Minkoff and Deborah Gustafson), U01-AI-031834; Chicago WIHS (Mardge Cohen and Audrey French), U01-AI-034993; Metropolitan Washington WIHS (Mary Young and Seble Kassaye), U01-AI-034994; Miami WIHS (Margaret Fischl and Lisa Metsch), U01-AI-103397; UNC WIHS (Adaora Adimora), U01-AI-103390; Connie Wofsy Women’s HIV Study, Northern California (Ruth Greenblatt, Bradley Aouizerat, and Phyllis Tien), U01-AI-034989; WIHS Data Management and Analysis Center (Stephen Gange and Elizabeth Golub), U01-AI-042590; Southern California WIHS (Alexandra Levine and Marek Nowicki), U01-HD-032632 (WIHS I – WIHS IV). WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases, with additional co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Cancer Institute, NIDA, and the National Institute on Mental Health. Targeted supplemental funding for specific projects is also provided by the National Institute of Dental and Craniofacial Research, the National Institute on Alcohol Abuse and Alcoholism, the National Institute on Deafness and other Communication Disorders, and the NIH Office of Research on Women’s Health. WIHS data collection is also supported by UL1-TR000004 (UCSF CTSA) and UL1-TR000454 (Atlanta CTSA).
Conception and design of the study or acquisition, analysis, and interpretation of data: MRD, LB, KMW, SGS, AA, TEW, CJ, MP, MC, ETG. Drafting the manuscript: MRD, LB, KMW, ETG. Critical review of drafts for intellectual content: SGS, AA, TEW, JC, MP, MC. Final approval of the submitted version: MRD, LB, KMW, SGS, AA, TEW, JC, MP, MC, ETG.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.USAID, U.S. Department of State. United States Strategy to Prevent and Respond to Gender-Based Violence Globally. USAID and Department of State, Government of the United States of America; 2012. [Google Scholar]
- 2.UN General Assembly. Declaration on the Elimination of Violence Against Women. Geneva: UN; 1993. [Google Scholar]
- 3.Devries KM, Mak JY, Garcia-Moreno C, et al. Global health. The global prevalence of intimate partner violence against women. Science. 2013;340(6140):1527–1528. doi: 10.1126/science.1240937. http://dx.doi.org/10.1126/science.1240937. [DOI] [PubMed] [Google Scholar]
- 4.Ellsberg M, Jansen HA, Heise L, et al. Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: an observational study. Lancet. 2008;371(9619):1165–1172. doi: 10.1016/S0140-6736(08)60522-X. http://dx.doi.org/10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- 5.Campbell JC. Health consequences of intimate partner violence. Lancet. 2002;359(9314):1331–1336. doi: 10.1016/S0140-6736(02)08336-8. http://dx.doi.org/10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 6.Cohen M, Deamant C, Barkan S, et al. Domestic violence and childhood sexual abuse in HIV-infected women and women at risk for HIV. Am J Public Health. 2000;90(4):560–565. doi: 10.2105/ajph.90.4.560. http://dx.doi.org/10.2105/AJPH.90.4.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lang DL, Sales JM, Salazar LF, et al. Rape victimization and high risk sexual behaviors: longitudinal study of african-american adolescent females. West J Emerg Med. 2011;12(3):333–342. [PMC free article] [PubMed] [Google Scholar]
- 8.Wingood GM, DiClemente RJ, McCree DH, Harrington K, Davies SL. Dating violence and the sexual health of black adolescent females. Pediatrics. 2001;107(5):E72. doi: 10.1542/peds.107.5.e72. http://dx.doi.org/10.1542/peds.107.5.e72. [DOI] [PubMed] [Google Scholar]
- 9.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–48. doi: 10.1016/S0140-6736(10)60548-X. http://dx.doi.org/10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 10.White House Office of National AIDS Policy. The National HIV/AIDS Strategy: Updated to 2020. Washington, DC: White House Office of National AIDS Policy; 2015. [Google Scholar]
- 11.Exner-Cortens D, Eckenrode J, Rothman E. Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics. 2013;131(1):71–78. doi: 10.1542/peds.2012-1029. http://dx.doi.org/10.1542/peds.2012-1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filipas HH, Ullman SE. Child sexual abuse, coping responses, self-blame, posttraumatic stress disorder, and adult sexual revictimization. J Interpers Violence. 2006;21(5):652–672. doi: 10.1177/0886260506286879. http://dx.doi.org/10.1177/0886260506286879. [DOI] [PubMed] [Google Scholar]
- 13.Widom CS, Czaja SJ, Dutton MA. Childhood victimization and lifetime revictimization. Child Abuse Negl. 2008;32(8):785–796. doi: 10.1016/j.chiabu.2007.12.006. http://dx.doi.org/10.1016/j.chiabu.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Black MC, Basile KC, Breiding MJ, et al. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. [Google Scholar]
- 15.Stockl H, Devries K, Rotstein A, et al. The global prevalence of intimate partner homicide: a systematic review. Lancet. 2013;382(9895):859–865. doi: 10.1016/S0140-6736(13)61030-2. http://dx.doi.org/10.1016/S0140-6736(13)61030-2. [DOI] [PubMed] [Google Scholar]
- 16.Cooper A, Smith E. Homicide Trends in the United States, 1980–2008. Washington, DC: Bureau of Justice Statistics; 2011. [Google Scholar]
- 17.El-Bassel N, Gilbert L, Witte S, Wu E, Chang M. Intimate partner violence and HIV among drug-involved women: contexts linking these two epidemics--challenges and implications for prevention and treatment. Subst Use Misuse. 2011;46(2–3):295–306. doi: 10.3109/10826084.2011.523296. http://dx.doi.org/10.3109/10826084.2011.523296. [DOI] [PubMed] [Google Scholar]
- 18.Lang AJ, Stein MB, Kennedy CM, Foy DW. Adult psychopathology and intimate partner violence among survivors of childhood maltreatment. J Interpers Violence. 2004;19(10):1102–1118. doi: 10.1177/0886260504269090. http://dx.doi.org/10.1177/0886260504269090. [DOI] [PubMed] [Google Scholar]
- 19.Campbell R, Greeson MR, Bybee D, Raja S. The co-occurrence of childhood sexual abuse, adult sexual assault, intimate partner violence, and sexual harassment: a mediational model of posttraumatic stress disorder and physical health outcomes. J Consult Clin Psychol. 2008;76(2):194–207. doi: 10.1037/0022-006X.76.2.194. http://dx.doi.org/10.1037/0022-006X.76.2.194. [DOI] [PubMed] [Google Scholar]
- 20.El-Bassel N, Gilbert L, Rajah V, Foleno A, Frye V. Fear and violence: raising the HIV stakes. AIDS Educ Prev. 2000;12(2):154–170. [PubMed] [Google Scholar]
- 21.Turner HA, Shattuck A, Finkelhor D, Hamby S. Polyvictimization and Youth Violence Exposure Across Contexts. J Adolesc Health. 2016;58(2):208–214. doi: 10.1016/j.jadohealth.2015.09.021. http://dx.doi.org/10.1016/j.jadohealth.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 22.El-Bassel N, Caldeira NA, Ruglass LM, Gilbert L. Addressing the unique needs of African American women in HIV prevention. Am J Public Health. 2009;99(6):996–1001. doi: 10.2105/AJPH.2008.140541. http://dx.doi.org/10.2105/AJPH.2008.140541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gilbert L, El-Bassel N, Rajah V, Foleno A, Frye V. Linking drug-related activities with experiences of partner violence: a focus group study of women in methadone treatment. Violence Vict. 2001;16(5):517–536. [PubMed] [Google Scholar]
- 24.Plotzker RE, Metzger DS, Holmes WC. Childhood sexual and physical abuse histories, PTSD, depression, and HIV risk outcomes in women injection drug users: a potential mediating pathway. Am J Addict. 2007;16(6):431–438. doi: 10.1080/10550490701643161. http://dx.doi.org/10.1080/10550490701643161. [DOI] [PubMed] [Google Scholar]
- 25.Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq Creat Sociol. 1996;24(2):99–110. [Google Scholar]
- 26.Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. J Womens Health (Larchmt) 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. http://dx.doi.org/10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gilbert L, Raj A, Hien D, Stockman J, Terlikbayeva A, Wyatt G. Targeting the SAVA (Substance Abuse, Violence, and AIDS) Syndemic Among Women and Girls: A Global Review of Epidemiology and Integrated Interventions. J Acquir Immune Defic Syndr. 2015;69(Suppl 2):S118–S127. doi: 10.1097/QAI.0000000000000626. http://dx.doi.org/10.1097/QAI.0000000000000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riley ED, Cohen J, Knight KR, Decker A, Marson K, Shumway M. Recent violence in a community-based sample of homeless and unstably housed women with high levels of psychiatric comorbidity. Am J Public Health. 2014;104(9):1657–1663. doi: 10.2105/AJPH.2014.301958. http://dx.doi.org/10.2105/AJPH.2014.301958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilson PR, Laughon K. House to house, shelter to shelter: experiences of black women seeking housing after leaving abusive relationships. J Forensic Nurs. 2015;11(2):77–83. doi: 10.1097/JFN.0000000000000067. http://dx.doi.org/10.1097/JFN.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 30.Decker MR, Crago AL, Chu SK, et al. Human rights violations against sex workers: burden and effect on HIV. Lancet. 2015;385(9963):186–199. doi: 10.1016/S0140-6736(14)60800-X. http://dx.doi.org/10.1016/S0140-6736(14)60800-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deering KN, Amin A, Shoveller J, et al. A systematic review of the correlates of violence against sex workers. Am J Public Health. 2014;104(5):e42–e54. doi: 10.2105/AJPH.2014.301909. http://dx.doi.org/10.2105/AJPH.2014.301909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. http://dx.doi.org/10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 33.Hessol NA, Weber KM, Holman S, et al. Retention and attendance of women enrolled in a large prospective study of HIV-1 in the United States. J Womens Health (Larchmt) 2009;18(10):1627–1637. doi: 10.1089/jwh.2008.1337. http://dx.doi.org/10.1089/jwh.2008.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bacon MC, von Wyl V, Alden C, et al. The Women's Interagency HIV Study: an observational cohort brings clinical sciences to the bench. Clin Diagn Lab Immunol. 2005;12(9):1013–1019. doi: 10.1128/CDLI.12.9.1013-1019.2005. http://dx.doi.org/10.1128/cdli.12.9.1013-1019.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barkan SE, Melnick SL, Preston-Martin S, et al. The Women's Interagency HIV Study. WIHS Collaborative Study Group. Epidemiology. 1998;9(2):117–125. http://dx.doi.org/10.1097/00001648-199803000-00004. [PubMed] [Google Scholar]
- 36.UNAIDS. UNAIDS Guidance Note on HIV and Sex Work. Geneva: UNAIDS; 2012. [Google Scholar]
- 37.NIAAA. Drinking levels defined. [Accessed April 7, 2016]; www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking.
- 38.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2) J Fam Issues. 1996;17(3):283–316. http://dx.doi.org/10.1177/019251396017003001. [Google Scholar]
- 39.von Hippel PT. Regression with missing Y’s: an improved strategy for analyzing multiply-imputed data. Sociol Methodol. 2007;37(1):83–117. http://dx.doi.org/10.1111/j.1467-9531.2007.00180.x. [Google Scholar]
- 40.UCLA: Statistical Consulting Group. Multiple Imputation in SAS, Part 2 [Google Scholar]
- 41.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A Multivariate Technique for Multiply Imputing Missing Values Using a Sequence of Regression Models. Surv Methodol. 2001;27(1):85–95. [Google Scholar]
- 42.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. http://dx.doi.org/10.2307/2531248. [PubMed] [Google Scholar]
- 43.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons; 1987. http://dx.doi.org/10.1002/9780470316696. [Google Scholar]
- 44.Hopper EK, Bassuk EL, Olivet J. Shelter from the storm: Trauma-informed care in homeless service settings. Open Health Serv Policy J. 2010;3:80–100. http://dx.doi.org/10.2174/1874924001003020080. [Google Scholar]
- 45.Machtinger EL, Cuca YP, Khanna N, Rose CD, Kimberg LS. From treatment to healing: the promise of trauma-informed primary care. Womens Health Issues. 2015;25(3):193–197. doi: 10.1016/j.whi.2015.03.008. http://dx.doi.org/10.1016/j.whi.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 46.Potterat JJ, Brewer DD, Muth SQ, et al. Mortality in a long-term open cohort of prostitute women. Am J Epidemiol. 2004;159(8):778–785. doi: 10.1093/aje/kwh110. http://dx.doi.org/10.1093/aje/kwh110. [DOI] [PubMed] [Google Scholar]
- 47.Cohen MH, Hotton AL, Hershow RC, et al. Gender-related risk factors improve mortality predictive ability of VACS Index among HIV-infected women. J Acquir Immune Defic Syndr. 2015;70(5):538–544. doi: 10.1097/QAI.0000000000000795. http://dx.doi.org/10.1097/QAI.0000000000000795. [DOI] [PMC free article] [PubMed] [Google Scholar]