Abstract
Background:
Unreliable compliance with infection prevention procedures necessitates an analysis of contributing factors.
Methods:
A retrospective study explored utility of 3236 nursing hygiene notes in the electronic healthcare record system (EHR). This 2012–2013 study identified defects in the chlorhexidine (CHG) bathing practice for a hospital unit.
Results:
The overall compliance with CHG bathing was 22.99%. Patients with length of stay less than 3 days, in most cases, did not have documentation for CHG bathing. Patient refusal to bathe was the most prevalent documented reason (66%) of the unsuccessful initial and repeated offers to bathe. The regular staff were statistically less successful in convincing patients to bathe. The 1455 notes produced by the regular staff (n = 10) demonstrated a significantly higher failure rate (56.08%) to execute this procedure in comparison with 1770 notes documented by the 246 temporary staff (31.19% failure rate) (P value <0.001) .
Discussion:
This analysis yielded three main insights: lack of the CHG documentation in a large number of short admissions; inconsistent use of CHG baths; and presence of workarounds due to patient refusals to bathe. The study concluded that EHR structured and unstructured data can unlock the opportunity for identifying hidden defects and inform decision-makers about the need for change.
Keywords: Healthcare-associated infections, compliance, qualitative research
Introduction
Hospitals represent a major source for the emergence, selection and spread of multidrug-resistant organisms. Low compliance with infection prevention and control practice is one reason that 5–10% of hospitalised patients acquire at least one healthcare-associated infection (HAI) (Department of Health and Human Services, 2012). Day-to-day infection prevention and control tasks, such as hand hygiene, patient chlorhexidine bathing, environmental cleaning and care for invasive devices, may be compromised due to time constraints, urgency of care and unpredicted demands for health services. High labour intensive healthcare environments can create conditions where some ‘low-priority’ tasks, such as hand hygiene, may be traded for emergency care or for healthcare workers’ (HCWs) workarounds.
Providing individuals with performance feedback is associated with the desirable behavioural changes, such as improved compliance with infection prevention guidelines (Eckmanns et al., 2006; Kohli et al., 2009). Today electronic healthcare record systems (EHRs) generate a large amount of granular data convenient for automatic quality measurements. We hypothesise that a complementary analysis of electronic documentation could be beneficial for revealing hidden defects in healthcare processes.
One behaviour important for preventing the spread of resistant pathogens and developing device-associated infections is the use of patient bathing with chlorhexidine (CHG). CHG bathing has not been universally accepted as the best practice. However, several quasi-experimental studies in intensive care units (ICUs) demonstrated a significant reduction of the concentration of bacteria on the patient body surface after the use of CHG (Bleasdale et al., 2007; Climo et al., 2009, 2013; Huang et al., 2013; Popovich et al., 2009; Vernon et al., 2006). As a result, patients developed fewer bloodstream infections, surgical-site infections and urinary catheter-associated infections from all pathogens. Compliance with CHG bathing may be critical to overall efforts to reduce the incidence of HAIs in hospitals and long-term care facilities where many colonised asymptomatic patients remain undetected. One cluster-randomised clinical trial reported a wide variation in the compliance with CHG bathing in ICUs, in the range of 54–98% (Huang et al., 2013). The compliance and potential issues with CHG bathing in non-ICU hospital settings are not reported.
Aim
The aim of this research is to explore the utility of nursing hygiene notes recorded in the EHR: do those notes provide insights on CHG bathing practices in a high risk for infections non-ICU hospital unit?
Method
This was an exploratory, retrospective qualitative study with the secondary use of EHR data. Ethical approval was granted by the university.
Study setting
We selected a 50-bed medical-surgical unit. The unit has a daily prevalence of patients colonised with antibiotic-resistant organisms in the range of 10–25%. The unit patient population consisted of solid organ transplant patients (45%), cancer patients (20%), non-surgical patients (20%), and general surgery patients (15%). Unit compliance with CHG bathing, reported by the hospital, was approximately 30% during 2012–2013. The hospital implemented a policy requiring daily patient hygiene using CHG. This policy recommends using a 2% chlorhexidine gluconate solution on the patient’s body with a washcloth. The hospital policy-makers set a goal for each hospital unit to bathe at least 60% of the patients daily. This threshold was determined by the hospital daily admission and discharge rates that permitted approximately 40% patient-days to be free of bathing. The procedure was overseen by nurses and delivered by care technicians. The unit nurses and nursing assistants recorded CHG bathing in the EHR’s standardised template. The template lists the following selections: full bath; partial bath; showered; peri-wash; pre-procedure scrub; Chlorhexidine used; Chlorhexidine not used; and patient refused. During the study, the staff did not use specific tools in the EHR for tracking patient hygiene outcomes. The infectious diseases department measured compliance to hospital policy with the number of bottles utilised during the month divided by the unit patient-days (census). Monthly reports were provided to the units.
Analysis
The objectives of this analysis were to measure both a CHG bathing documentation rate and a CHG compliance rate and to identify hidden defects and barriers for the CHG bathing by analysing the EHR notes’ time stamps, authorship and content. First, we explored: (1) the CHG bathing documentation rate defined as a number of the EHR hygiene notes per 100-unit patient-days; and (2) the unit CHG bathing compliance rate defined as a number of notes that indicated the CHG bath delivery per 100-unit patient-days. Then we examined a distribution of the CHG baths in the four length of stay (LOS) groups: LOS group 1 (1–5 days); LOS group 2 (6–10 days); LOS group 3 (11–20 days); and LOS group 4 (21+ days). Finally, we applied word counting for analysis of the note content to reveal some potential hidden issues.
We extracted and analysed 3236 CHG hygiene notes documented by 256 HCWs for a total of 678 patients with complete LOS from October 2012 to July 2013.
Data sources
We created a one-time electronic report abstracting patient medical record number; dates of admission and discharge; plus timestamp, authorship and content of each bathing note. All patient personal data were de-identified and replaced with an anonymised number. The two outcomes of interest included: ‘success’ indicating a receipt of a CHG bath versus ‘no success’ denoting a failure to administer a CHG bath. ‘Success’ was detected when the note included ‘Chlorhexidine used’. ‘No success’ was detected when the note indicated ‘Chlorhexidine not used’.
Results
The hygiene documentation rate and the chlorhexidine-bathing rate were 32.81% and 22.99%, respectively, in 678 patients (Table 1). Among these patients, 301 patients (mean LOS, 3.24±3.56) did not have a single hygiene note (0% compliance with the CHG bathing) documented in the EHR (Table 2). The remaining 377 patients (mean LOS, 7.54±15.53) had at least one nursing hygiene note indicating 70.05% compliance with CHG bathing. In this group, 23 patients (mean LOS, 2.39±1.34) had notes indicating no baths delivery (‘no success’ group) and 354 patients (mean LOS, 7.83±15.91) had notes indicating the administration of at least one bath (‘success’ group) (Table 2). The CHG compliance rates in these two groups were 0% and 71.27%, respectively.
Table 1.
The characteristics of the chlorhexidine bathing practice.
| Measure | Value |
|---|---|
| Encounters with full LOS (n) | 2245 |
| Patients (n) | 678 |
| Patient-days (days) | 9860 |
| Nursing notes (n) | 3236 |
| Chlorhexidine baths (n) | 2267 |
| Documentation rate (%) | 32.81 |
| CHG compliance rate (%) | 22.99 |
| Mean LOS/SD (days) | 5.43±19.68 |
Documentation rate: number of nursing notes per 100 patient-days.
Compliance rate: number of baths per 100 patient-days.
Table 2.
The characteristics of chlorhexidine bathing compliance derived from hygiene notes.
| Patient groups | Encounters (n) |
Patients (n) |
Patient-days (days) |
Chlorhexidine baths (n) | Mean LOS/SD (days) |
CHG compliance rate (%) |
|---|---|---|---|---|---|---|
| Group 1: patients without hygiene notes | 1815 | 301 | 6624 | 0 | 3.44±3.56 | 0% |
| Group 2: patients with at least one note | 429 | 377 | 3236 | 2267 | 7.54±15.53 | 70.05% |
| ‘No success’ group | 23 | 23 | 55 | 0 | 2.39±1.34 | 0% |
| ‘Success’ group | 407 | 354 | 3181 | 2267 | 7.83±15.91 | 71.27% |
| Group 2 compliance with CHG bathing by LOS | ||||||
| Group 1: 1–5 days | 253 | 231 | 873 | 584 | 3.23±1.19 | 70.99% |
| Group 2: 6–10 days | 91 | 89 | 671 | 523 | 7.37±1.22 | 77.44% |
| Group 3: 11–20 days | 42 | 41 | 606 | 450 | 14.43±2.79 | 74.29% |
| Group 4: 21+ days | 21 | 21 | 1107 | 710 | 52.71±49.96 | 65.69% |
Encounter is a patient hospital admission longer than 24 h.
Compliance is measured as the number of baths per 100 patient-days.
After categorising the ‘success’ group of patients into the four LOS groups, the CHG compliance in LOS group 1 (n = 231 patients) was 70.99%, LOS group 2 (n = 89 patients) was 77.44%, LOS group 3 (n = 41 patients) was 74.29% and LOS group 4 (n = 21 patients) was 65.69% (Table 2). The mean LOS in these groups was 3.23±1.19 days, 7.37±1.22 days, 14.43±2.79 days and 52.71±49.96 days, respectively.
Furthermore, we identified the ten HCWs (3.24%) who produced 1455 documents (45.11%). The remaining—246 (96.10%) of authors—collectively recorded 1770 notes (54.89%) (Table 3). A total of 816 notes (56.08%) produced by the ten HCWs indicated ‘no success’. The documentation of the remaining authors showed only 31.19% (n = 554) of ‘no success’, which was significantly lower in comparison with the first group (P value <0.001).
Table 3.
Healthcare workers’ (HCW) compliance with chlorhexidine bathing.
| HCW groups | Providers per group (n) | Rate of records per group | Total records (n) | ‘No success’ | Rate of ‘No success’ |
Enrichment | P value |
|---|---|---|---|---|---|---|---|
| Group of 10 HCWs | 10 | 145 | 1458 | 817 | 56.08% | 1.798 | 0.00 |
| Group of the remaining HCWs | 264 | 1 | 1778 | 554 | 31.19% |
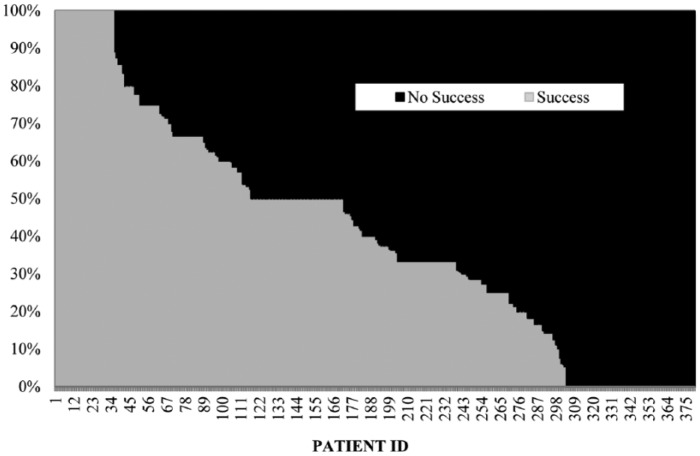
The individual patient’s CHG bathing rate was in the range of 0–100% (Figure 1). The note’s content analysis showed that among 1368 notes with ‘no success’, 902 records (66%) indicated ‘patient refusal’ to bathe. A qualitative analysis showed the following reasons for refusal: nine (1%) due to imminent discharge, 334 (37%) due to the inconvenient timing of the bath offer, 12 (1%) due to health issues (tired, in pain, want to sleep) and 550 (61%) due to unknown reasons. Patient refusals were classified using word counting. The comments were entered with a refusal or ‘no success’. Of 1368 records, there were 597 unique comment ‘values’, while 491 records did not include refusal reasons. To profile this information, we employed a basic word counting algorithm to define major categories used in ‘no success’ comments. Comments were formatted to all lower case with punctuation removed. The algorithm examined each comment for a comment based on observed keywords.
Figure 1.
A distribution of the hygiene compliance (‘success’) in individual patients.
In 80 occurrences, 28 patients had a first refusal event that was followed up. In total, 41 of the refusals (51.80%) were followed up with ‘success’ in the first or second follow-up. Therefore, 41 of the patients (51.8%) later received a bath on the same day of ‘no success’, whereas 39 of the patients (48.2%) did not eventually receive a bath. For those patients who continued to refuse bathing, five were followed up a third time, and one patient had a fourth follow-up.
Discussion
A lack of information about potential issues related to delivery of a preventive intervention keeps decision-makers unaware of the needed changes. The EHR structured and unstructured data can unlock opportunities for identifying hidden defects in care delivery. Hospitals may benefit from a systematic analysis of EHR documentation in order to better understand the causes of non-compliance with CHG bathing.
Our study had several important findings. The nurses and nursing assistants who worked in the 50-bed non-ICU hospital unit recorded nearly 4000 notes on CHG bathing in the EHR during a nine-month period. In other words, they recorded approximately 15 notes a day. Overall compliance with CHG bathing, derived from the EHR data, was 23%. Approximately 44% of the patients did not have a single nursing hygiene note documented in the EHR. On average, these patients spent three days in hospital. More than 50% of the patients had at least one nursing hygiene note documented and, on average, these patients stayed seven days in the hospital.
A patient’s LOS has some effects on the CHG compliance. Our study shows first, the lowest CHG compliance was observed in patients with LOS less than six days. Half of these patients lacked nursing documentation. A group of patients with LOS in the range of 6–10 days had the highest CHG compliance (77.44%). A group of patients with LOS greater than 10 days showed a gradual decrease in CHG compliance (65%). This finding leads to a conclusion that infection prevention may be altered in patients with prolonged LOS. It may be important to further explore the role of prolonged LOS as a non-compliance risk factor. More importantly, a better understanding of the relationship between LOS and compliance with infection prevention may help develop targeted approaches for patients with different LOSs. Many studies have demonstrated that prolonged LOS is associated with high risk of HAIs (Cosgrove et al., 2005; Fagon et al., 1993; Pittet et al., 1994; Wilcox et al., 1996).
One potential explanation of CHG non-compliance in patients with extended LOS could be the development of CHG-related side effects. It is known that prolonged use of CHG causes skin reactions (Kampf and Kramer, 2004). Therefore, it would be beneficial to systematically measure the infection prevention side effects, in addition to quality measures and process defects.
Furthermore, we also explored some characteristics of the participating workforce. Nurses and nursing assistants play a critical role in the spread of infection. This is due to their repeated close contacts with patients (Machens et al., 2013; Vanhems et al., 2013). Our findings show that bathing documentation was recorded by a large number of temporary workers. Those temporary workers comprised nursing students and irregular personnel, including floating nurses and care technicians. This group documented, on average, one hygiene note during the study period. Collectively, they produced more than 50% of the all bathing notes. At the same time, we identified a small group of ten nurses and nursing assistants who recorded the rest of the hygiene notes. These ten HCWs had a significantly higher rate of failure to execute this preventive procedure when compared with the documentation of the irregular HCWs. Several studies showed that ‘temporary nursing staff and reduced number of full FTE’ are significantly associated with less than the recommended standard of infection control (Ferguson, 2009; Fukuda et al., 2009; Griffiths et al., 2009; Weinstein et al., 2008). In contrast, our findings demonstrated that the performance was lower among the regular staff. Thus, prioritising this group for interventions may be beneficial for improving the overall compliance with infection prevention.
In addition, we explored the role of patients and identified that half of the notes communicated a failure to administer CHG bathing due to patient refusal. In most cases, the reason of refusal was not documented, but some notes indicated an inconvenient time of the bath offer and patients’ health issues as contributing factors. Some patients systematically refused to bathe and that led to workarounds by HCWs.
We categorised the observed findings into the three major defects: (1) a lack of the documentation about the intervention; (2) a high varaibility of the CHG bathing in individual patients; and (3) the workarounds due to patient refusal to bathe. These defects need to be recognised in real time in order to improve both the efficiency and the quality of healthcare.
The EHR data used in this study are rich in information and ideal for the type of analysis performed – identifying trends and patterns in patient bathing with CHG. The results can directly inform policy and procedural decisions in future work, particularly where quality standards are not met or are mediocre. Additionally, these data are readily available and this analysis can be performed whenever questions about infection prevention practice arise.
Yet, there is a drawback related to data quality. For example, the procedure could be done but not documented. Also, time stamps may be artificial since a procedure could be done earlier or later than actually documented. The findings also point out that some CHG bathing practices can be altered by both LOS and patient attitudes.
In summary, the effectiveness of daily CHG bathing in non-ICU hospital settings may be compromised due to low compliance. The EHR time-stamped structured template for CHG bathing permits the identification of some hidden risk factors for compliance with CHG bathing. These may include a measurement of cumulative CHG bathing rate in individual patients, causes and frequency of patient refusals, individual HCW’s performance and adverse events associated with the use of CHG.
Acknowledgments
We thank the Information Technology staff for their help with this study.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. (2007) Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Archives of Internal Medicine 167: 2073–2079. [DOI] [PubMed] [Google Scholar]
- Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, Speck K, Jernigan JA, Robles JR, Wong ES. (2009) The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Critical Care Medicine 37: 1858–1865. [DOI] [PubMed] [Google Scholar]
- Climo MW, Yokoe DS, Warren DK, Perl TM, Bolon M, Herwaldt LA, Weinstein RA, Sepkowitz KA, Jernigal JA, Sanogo K, Wong ES. (2013) Effect of daily chlorhexidine bathing on hospital-acquired infection. New England Journal of Medicine 368: 533–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosgrove SE, QI Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y. (2005) The impact of methicillin resistance in Staphylococcus aureus bacteremia on patient outcomes: mortality, length of stay, and hospital charges. Infection Control and Hospital Epidemiology 26: 166–174. [DOI] [PubMed] [Google Scholar]
- Department of Health & Human Services. (2012) National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination. Available at: http://www.hhs.gov/ash/initiatives/hai/actionplan/hai-action-plan-executive-summary.pdf (accessed November 2014).
- Eckmanns T, Bessert J, Behnke M, Gastmeier P, Rüden H. (2006) Compliance with antiseptic hand rub use in intensive care units the Hawthorne effect. Infection Control 27: 931–934. [DOI] [PubMed] [Google Scholar]
- Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C. (1993) Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. American Journal of Medicine 94: 281–288. [DOI] [PubMed] [Google Scholar]
- Ferguson J. (2009) Preventing healthcare-associated infection: risks, healthcare systems and behaviour. Internal Medicine Journal 39: 574–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuda H, Imanaka Y, Hirose M, Hayashida K. (2009) Factors associated with system-level activities for patient safety and infection control. Health Policy 89: 26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths P, Renz A, Hughes J, Rafferty A. (2009). Impact of organisation and management factors on infection control in hospitals: a scoping review. Journal of Hospital Infection 73: 1–14. [DOI] [PubMed] [Google Scholar]
- Huang SS, Septimus E, Kleiman K, Moody J, Hickok J, Avery TR, Lankiewicz J, Gombosev A, Terpstra L, Hartford F, Hayden MK, Jernigan JA, Weinstein RA, Fraser VJ, Haffrenreffer K, Cui E, Kaganov RE, Lolans K, Perlin JB, Platt R; CDC Prevention Epicenters Program; AHRQ DECIDE Network and Healthcare-Associated Infections Program. (2013) Targeted versus universal decolonization to prevent ICU infection. New England Journal of Medicine 368: 2255–2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampf G, Kramer A. (2004). Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clinical Microbiology Reviews 17: 863–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohli E, Ptak J, Smith R, Taylor E, Talbot EA, Kirldand KB. (2009) Variability in the Hawthorne effect with regard to hand hygiene performance in high-and low-performing inpatient care units. Infection Control 30: 222–225. [DOI] [PubMed] [Google Scholar]
- Machens A, Gesualdo F, Rizzo C, Tozzi A, Barrat A, Cattuto C. (2013) An infectious disease model on empirical networks of human contact: bridging the gap between dynamic network data and contact matrices. BMC Infectious Diseases 13: 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittet D, Tarara D, Wenzel RP. (1994) Nosocomial bloodstream infection in critically ill patients. Excess length of stay, extra costs, and attributable mortality. Journal of the American Medical Association 271: 1598–1601. [DOI] [PubMed] [Google Scholar]
- Popovich KJ, Hota B, Hayes R, Weinstein RA, Hayden MK. (2009) Effectiveness of routine patient cleansing with chlorhexidine gluconate for infection prevention in the medical intensive care unit. Infection Control and Hospital Epidemiology 30: 959–963. [DOI] [PubMed] [Google Scholar]
- Vanhems P, Barrat A, Cattuto C, Pinton JF, Khanafer N, Regis C, Kim B, Comte B, Voirin N. (2013) Estimating potential infection transmission routes in hospital wards using wearable proximity sensors. PloS One 8: e73970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon MO, Hayden MK, Trick WE, Hayes RA, Blom DW, Weinstein RA. (2006) Chlorhexidine gluconate to cleanse patients in a medical intensive care unit: the effectiveness of source control to reduce the bioburden of vancomycin-resistant enterococci. Archives of Internal Medicine 166: 306–312. [DOI] [PubMed] [Google Scholar]
- Weinstein RA, Stone PW, Pogorzelska M, Kunches L, Hirschhorn LR. (2008) Hospital staffing and health care–associated infections: a systematic review of the literature. Clinical Infectious Diseases 47: 937–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox M, Cunniffe J, Trundle C, Redpath C. (1996) Financial burden of hospital-acquired Clostridium difficile infection. Journal of Hospital Infection 34: 23–30. [DOI] [PubMed] [Google Scholar]