Abstract
OBJECTIVE
To examine temporal trends in utilization of glucose-lowering medications, glycemic control, and rate of severe hypoglycemia among patients with type 2 diabetes (T2DM).
RESEARCH DESIGN AND METHODS
Using claims data from 1.66 million privately insured and Medicare Advantage patients with T2DM from 2006 to 2013, we estimated the annual 1) age- and sex-standardized proportion of patients who filled each class of agents; 2) age-, sex-, race-, and region-standardized proportion with hemoglobin A1c (HbA1c) <6%, 6 to <7%, 7 to <8%, 8 to <9%, ≥9%; and 3) age- and sex-standardized rate of severe hypoglycemia among those using medications. Proportions were calculated overall and stratified by age-group (18–44, 45–64, 65–74, and ≥75 years) and number of chronic comorbidities (zero, one, and two or more).
RESULTS
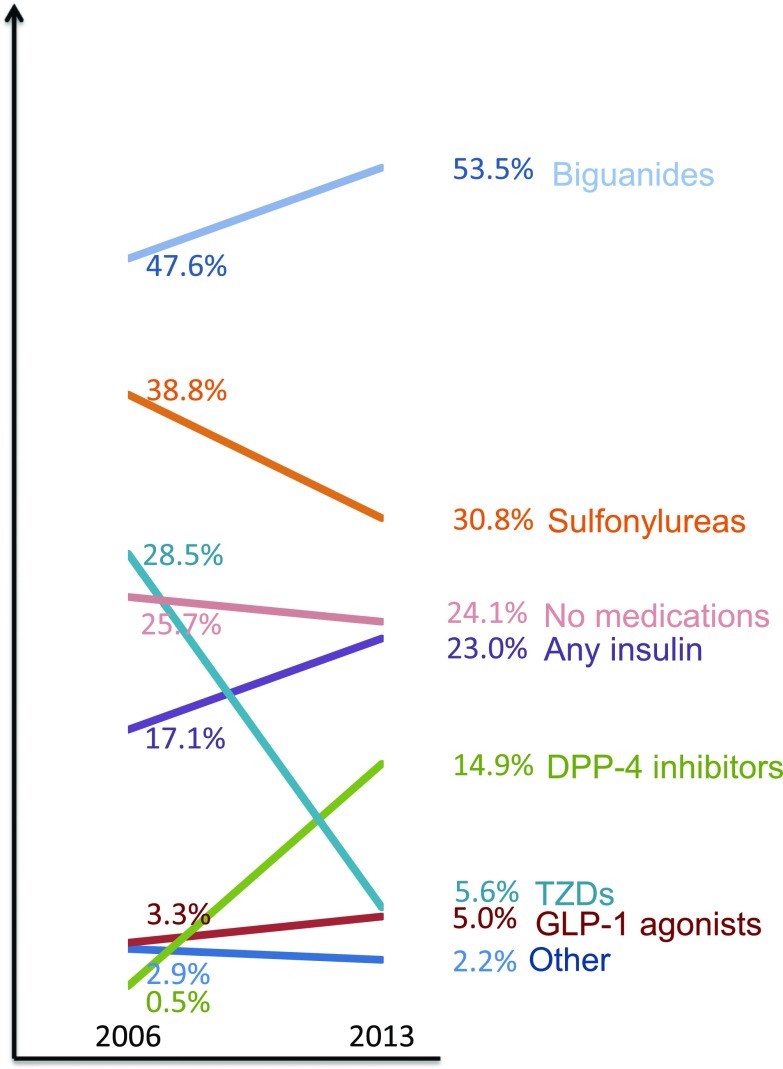
From 2006 to 2013, use increased for metformin (from 47.6 to 53.5%), dipeptidyl peptidase 4 inhibitors (0.5 to 14.9%), and insulin (17.1 to 23.0%) but declined for sulfonylureas (38.8 to 30.8%) and thiazolidinediones (28.5 to 5.6%; all P < 0.001). The proportion of patients with HbA1c <7% declined (from 56.4 to 54.2%; P < 0.001) and with HbA1c ≥9% increased (9.9 to 12.2%; P < 0.001). Glycemic control varied by age and was poor among 23.3% of the youngest and 6.3% of the oldest patients in 2013. The overall rate of severe hypoglycemia remained the same (1.3 per 100 person-years; P = 0.72), declined modestly among the oldest patients (from 2.9 to 2.3; P < 0.001), and remained high among those with two or more comorbidities (3.2 to 3.5; P = 0.36).
CONCLUSIONS
During the recent 8-year period, the use of glucose-lowering drugs has changed dramatically among patients with T2DM. Overall glycemic control has not improved and remains poor among nearly a quarter of the youngest patients. The overall rate of severe hypoglycemia remains largely unchanged.
Introduction
Glycemic management of type 2 diabetes (T2DM) has changed considerably over the past decade (1,2). Clinicians and patients can now choose from 12 different classes of glucose-lowering medications to manage hyperglycemia. Unlike insulin or sulfonylurea drugs, most of the newer agents have not been implicated as a cause of hypoglycemia, which can be a serious complication of glucose-lowering therapy, particularly in the elderly (3). However, utilization of these newer agents has significantly contributed to increasing costs of diabetes management (4,5).
In addition to changes in drug therapies to reduce glucose levels, the recommended target glucose levels have changed as well. In 2009, based on new evidence from randomized clinical trials (6–8), the American Diabetes Association (ADA) clinical practice guidelines specifically recommended individualization of glycemic targets according to age and multimorbidity (9). In 2012, the ADA and the American Geriatrics Society developed a consensus statement that recognized that older adults with life-limiting comorbidities are less likely to benefit from tight glycemic control (i.e., reaching a hemoglobin A1c [HbA1c] <7%) and are more vulnerable to hypoglycemia compared with younger, healthier patients (10). Therefore, less stringent glycemic targets (i.e., HbA1c <8 or <9%) may be appropriate in older patients, particularly in those with multiple chronic conditions and established vascular complications (11).
Given these changes in management approaches, it is important to examine the temporal trends in glucose-lowering medication use, as well as resultant glycemic control and rates of severe hypoglycemia. These trends provide information about care patterns in response to changes in treatment options and treatment targets and can identify gaps in diabetes care and areas for potential improvement.
A number of studies have separately examined some of these trends (2,12–16). Data from physician audits have shown that patients with diabetes are being prescribed an increasing number of glucose-lowering medications in ambulatory care settings (1,2). Separate analysis of data from the National Health and Nutrition Examination Survey (NHANES) suggested that glycemic control has improved, and just over half of patients achieved an HbA1c <7% in 2007–2010 (13). Several other studies indicated that treatment-related hypoglycemia continues to pose a significant health threat, particularly for older adults and for those with multiple chronic conditions (12,14,15,17,18).
However, studies looking at medication prescribing patterns were conducted at different times and in different patient populations compared with the studies looking at glycemic control, precluding potential inferences about any association between medication use, glycemic control, and hypoglycemia. Moreover, they did not examine how these trends differ across age and comorbidity subgroups.
Accordingly, we examined trends in utilization of drug treatment for diabetes, as well as concurrent trends in glycemic control and rates of hypoglycemia among privately insured and Medicare Advantage patients with T2DM from geographically diverse regions across the U.S. using OptumLabs Data Warehouse (OLDW). We examined these trends in the overall population and in subgroups of younger and older patients and among patients with a varying number of other serious chronic conditions.
Research Design and Methods
Data Source
We conducted a retrospective analysis of medical and pharmacy administrative claims from a large database, OLDW, which includes privately insured and Medicare Advantage enrollees throughout the U.S. (19). The database contains data on more than 100 million enrollees from geographically diverse regions across the U.S., with the greatest representation from the South and Midwest (20). We included commercial health plans in OLDW that provided full coverage for inpatient, outpatient, and pharmacy services. Medical claims from inpatient and outpatient visits include ICD-9-CM (ICD-9, clinical modification) diagnosis codes, ICD-9 procedure codes, Current Procedural Terminology, version 4 procedure codes, Healthcare Common Procedure Coding System procedure codes, site of service codes, and provider specialty codes. Pharmacy claims include information on medications dispensed and size and dates of prescriptions. Study data were accessed using techniques compliant with the Health Insurance Portability and Accountability Act of 1996. Because this study involved an analysis of preexisting, de-identified data, it was exempt from institutional review board approval.
Study Population
All adults (age ≥18 years) with at least 1 year of continuous enrollment between 2006 and 2013 were included if they met criteria for T2DM during at least 1 year of the study period. The definition of diabetes was based on Health Plan Employer Data and Information Set criteria: two face-to-face encounters with a diagnosis of diabetes (ICD-9 codes 250.x, 357.2, 362.0, and 366.41 [21] in any position on the claim [22–24]) on different dates of service in an outpatient setting or nonacute inpatient setting, or one face-to-face encounter in an acute inpatient or emergency department (ED) setting, or use of insulin or oral antihyperglycemic agents (except metformin monotherapy) based on pharmacy data. We examined claims for diabetes ICD-9 codes over a 2-year period, which included the year of interest and the preceding year. Once patients met criteria for diabetes in 1 year, they were considered to have the diagnosis in subsequent years. We excluded adults with a diagnosis of gestational diabetes (ICD-9 code 648.0) and those with codes for T1DM (250.x1 and 250.x3). If patients had codes for both T1DM and T2DM, we excluded patients who had no claims for oral glucose-lowering medications.
Main Outcomes
In each year, we determined the proportion of the study population with one or more pharmacy fills for the different classes of glucose-lowering agents. Combination agents were counted as two different agents filled on the same date. Because patients could fill more than one class of agent during each year, the proportion of patients in each year could exceed 100%. Because patterns of medication fills may change over time, we also calculated the mean number of days covered for each oral glucose-lowering class of medications in each year based on the date of fill and days’ supply. In each year, we determined glycemic control category (HbA1c <6, 6 to <7, 7 to <8, 8 to <9, or ≥9%) based on the last HbA1c obtained during that calendar year. Data for HbA1c were available for a subset of patients based on specific lab vendor. In each year, we also determined rates of severe hypoglycemia requiring ED visit or hospital admission or observation stay based on validated principal discharge diagnosis ICD-9 codes (25) among people who filled at least one glucose-lowering agent. These values were reported as events per 100 person-years at risk. Person-years at risk were calculated based on days the patient was alive, enrolled in the health plan, and not hospitalized. A separate analysis was performed among people who filled insulin or insulin secretagogues, other glucose-lowering medications, and no diabetes agents.
Independent Variables
Independent variables included baseline age (18–44, 45–64, 65–74, and ≥75 years), sex, race (white, black, Hispanic, Asian, or unknown), region (Midwest, Northeast, South, and West), and the number of serious chronic conditions (zero, one, and two or more). The serious chronic conditions were based on ICD-9 codes and included chronic kidney disease, chronic lung disease, heart failure, myocardial infarction or coronary artery disease, dementia, depression, atrial fibrillation, and stroke (see Supplementary Table 1 for definitions). Household income was based on data from AmeriLINK (obtained through KnowledgeBase Marketing) and linked to claims data.
Statistical Analyses
We summarized the characteristics of the cohort by year. For drug utilization, glycemic control, and rates of severe hypoglycemia, we calculated age- and sex-standardized rates for each year using 2013 as the reference year. Because HbA1c was available only for a subset of the total sample, which varied nonrandomly by year, we estimated the annual proportions of patients in each glycemic control category using multinomial logistic regression with HbA1c category as the outcome and age, sex, race, and region as independent variables. We used this model to estimate the HbA1c category distribution for each year. We used logistic regression to assess annual trends in the use of each diabetes medication class and assess trends in each glycemic control category from 2006 to 2013. The trend in the number of hypoglycemia events was assessed using linear regression.
Sensitivity Analyses
Some patients were captured in multiple years of data, raising concern that increasing disease severity over time could contribute to secular trends. We performed sensitivity analyses that included only 1 year of data per patient, selected at random from all available years for that patient (2006–2013). Analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC) and Stata 14.1 (Stata Corp, College Station, TX).
Results
There were 1,657,610 unique patients with T2DM who met the inclusion criteria between 2006 and 2013. Among the study cohort, 33.7% were included in 1 year only, 25.1% were included in 2 years only, and 41.2% were included in 3 or more years.
From 2006 to 2013, as the OLDW expanded, and as diabetes prevalence increased, the number of patients with T2DM who contributed data nearly doubled, from ∼385,000 in 2006 to ∼700,000 in 2013 (Table 1). Most notably, the annual proportion of patients aged 65–74 years and 75 years or older increased over this 8-year period as OLDW captured an increasing number of Medicare Advantage enrollees. The burden of comorbidities and the proportion of patients with two or more serious chronic conditions also increased during the observation period.
Table 1.
Characteristics of privately insured patients with T2DM included in the study, 2006–2013
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | |
|---|---|---|---|---|---|---|---|---|
| Total, n | 384,964 | 447,634 | 469,528 | 538,239 | 593,422 | 642,817 | 682,310 | 700,117 |
| Age (years) | ||||||||
| 18–44 | 15.0 | 14.1 | 13.4 | 11.7 | 10.1 | 9.3 | 8.5 | 8.0 |
| 45–64 | 58.7 | 56.3 | 54.9 | 50.3 | 45.8 | 44.0 | 41.6 | 41.1 |
| 65–74 | 14.8 | 16.5 | 17.7 | 21.3 | 25.0 | 26.7 | 28.7 | 29.1 |
| ≥75 | 11.5 | 13.1 | 14.0 | 16.7 | 19.0 | 20.0 | 21.2 | 21.7 |
| Sex | ||||||||
| Female | 47.3 | 48.2 | 48.3 | 48.8 | 49.2 | 49.3 | 49.2 | 49.0 |
| Male | 52.7 | 51.8 | 51.7 | 51.2 | 50.8 | 50.7 | 50.8 | 51.0 |
| Race | ||||||||
| White | 63.3 | 64.6 | 66.2 | 66.4 | 67.5 | 67.3 | 67.1 | 64.1 |
| Black | 9.6 | 10.5 | 11.2 | 13.1 | 13.6 | 14.0 | 14.1 | 15.9 |
| Hispanic | 10.4 | 10.9 | 11.0 | 10.7 | 9.8 | 9.8 | 9.7 | 10.8 |
| Asian | 4.2 | 4.5 | 4.7 | 4.5 | 4.3 | 4.3 | 4.3 | 4.5 |
| Unknown | 12.5 | 9.5 | 6.9 | 5.4 | 4.8 | 4.7 | 4.8 | 4.8 |
| Region | ||||||||
| Midwest | 25.0 | 22.6 | 22.3 | 23.0 | 23.6 | 24.2 | 24.8 | 25.5 |
| Northeast | 19.1 | 19.5 | 20.0 | 18.8 | 17.9 | 19.7 | 20.5 | 20.3 |
| South | 40.1 | 42.3 | 43.0 | 44.4 | 45.7 | 44.7 | 43.5 | 43.0 |
| West | 14.9 | 14.2 | 13.1 | 12.6 | 12.0 | 10.8 | 10.6 | 10.6 |
| Unknown | 0.9 | 1.4 | 1.7 | 1.3 | 0.7 | 0.6 | 0.6 | 0.6 |
| Household income ($) | ||||||||
| <40K | 14.5 | 18.5 | 22.5 | 26.1 | 28.5 | 28.6 | 28.7 | 28.4 |
| 40–49K | 5.2 | 6.3 | 7.6 | 8.5 | 8.8 | 9.0 | 9.1 | 9.3 |
| 50–59K | 5.0 | 5.9 | 7.2 | 7.9 | 8.1 | 8.2 | 8.3 | 8.4 |
| 60–74K | 6.7 | 7.8 | 9.5 | 10.2 | 10.2 | 10.4 | 10.5 | 10.6 |
| 75–99K | 8.9 | 10.5 | 12.6 | 13.2 | 12.9 | 13.1 | 13.0 | 13.1 |
| ≥100K | 17.2 | 19.7 | 23.3 | 23.6 | 22.3 | 22.2 | 22.0 | 21.8 |
| Unknown | 42.5 | 31.3 | 17.3 | 10.4 | 9.2 | 8.4 | 8.5 | 8.4 |
| Comorbidities | ||||||||
| CAD/MI | 18.7 | 19.1 | 19.7 | 21.1 | 21.8 | 21.9 | 22.0 | 21.9 |
| CHF | 8.3 | 8.7 | 8.8 | 9.7 | 10.2 | 10.4 | 10.6 | 10.7 |
| Lung disease | 13.8 | 14.5 | 15.3 | 16.4 | 17.0 | 17.2 | 17.7 | 18.0 |
| CKD | 6.1 | 6.9 | 7.9 | 9.8 | 11.1 | 11.9 | 12.8 | 13.9 |
| Depression | 6.1 | 6.3 | 6.5 | 7.2 | 7.5 | 7.7 | 8.1 | 8.4 |
| Dementia | 2.4 | 2.8 | 3.0 | 3.4 | 3.6 | 3.8 | 4.3 | 4.5 |
| Stroke | 2.9 | 3.1 | 3.2 | 3.5 | 3.6 | 3.6 | 3.8 | 3.9 |
| Atrial fibrillation | 4.5 | 5.0 | 5.3 | 6.1 | 6.9 | 7.3 | 7.7 | 8.0 |
| Number of chronic conditions | ||||||||
| 0 | 61.9 | 60.6 | 59.0 | 55.8 | 54.0 | 53.1 | 52.1 | 51.3 |
| 1 | 23.2 | 23.5 | 24.4 | 25.3 | 25.8 | 26.0 | 26.1 | 26.2 |
| ≥2 | 14.9 | 15.9 | 16.6 | 18.9 | 20.2 | 20.9 | 21.8 | 22.5 |
Data are presented as % unless otherwise indicated. CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; MI, myocardial infarction.
Drug Utilization
Standardized utilization trends are shown in Fig. 1 and Supplementary Table 2. From 2006 to 2013, use increased for metformin (from 47.6 to 53.5%), dipeptidyl peptidase 4 (DPP-4) inhibitors (0.5 to 14.9%), glucagon-like peptide 1 agonists (3.3 to 5.0%), and insulin (17.1 to 23.0%) but declined for sulfonylureas (38.8 to 30.8%) and thiazolidinediones (28.5 to 5.6%; all P < 0.001). The increased utilization of insulin was primarily driven by adoption of basal insulin analogs (10.9 to 19.3%; P < 0.001) and rapid-acting insulin analogs (6.7 to 11.6%; P < 0.001). The use of human insulin products actually declined (11.6 to 5.6%; P < 0.001). The proportion of patients with a diagnosis of diabetes who did not fill any glucose-lowering medications declined slightly (25.7 to 24.1%; P < 0.001). When considering treatment complexity, the use of oral monotherapy increased slightly (from 24.3 to 26.4%) and the use of multiple (two or more) oral agents declined (from 33.0 to 26.5%), whereas the use of insulin alone and in combination with oral agents increased (from 6.0 to 8.5% and from 11.1 to 14.6%, respectively; all P values <0.001).
Figure 1.
Age- and sex-standardized proportion of patients with T2DM who filled each class of glucose-lowering agents, 2006 and 2013 (see Supplementary Table 2 for annual data). Since patients may fill more than one class in each year, percentages do not add up to 100%. Other medications were comprised of meglitinides, α-glucosidase inhibitors, SGLT-2 inhibitors, and amylin analogs. Patients with no fills for glucose-lowering medications were included in the “No medications” group.
The mean number of days covered for each class of oral glucose-lowering medications per year increased over the study period (Supplementary Table 3), even for drug classes with reduced rates of utilization.
Drug utilization varied by age, but overall trends were qualitatively similar (Supplementary Table 4). The use of metformin was most prevalent among the youngest age-group (18–44 years). Among the oldest patients, metformin surpassed sulfonylureas as the most prevalent diabetes drug class after 2010. DPP-4 inhibitor use increased among all age subgroups, with the highest rates of use among middle-age patients (45–64 years) in 2013. Use of any insulin increased across all age subgroups, most steeply among middle-age and older patients.
Drug utilization also varied by comorbidity burden (Supplementary Table 5). Among patients with two or more serious comorbidities, metformin, insulin, and sulfonylureas were all used to a similar extent, with a slight increase in metformin and insulin use and slight decline in sulfonylureas by 2013.
Glycemic Control
Laboratory testing for HbA1c was available on a subset of the total sample (25.6%). There were regional differences among patients with and without HbA1c available (Supplementary Table 6).
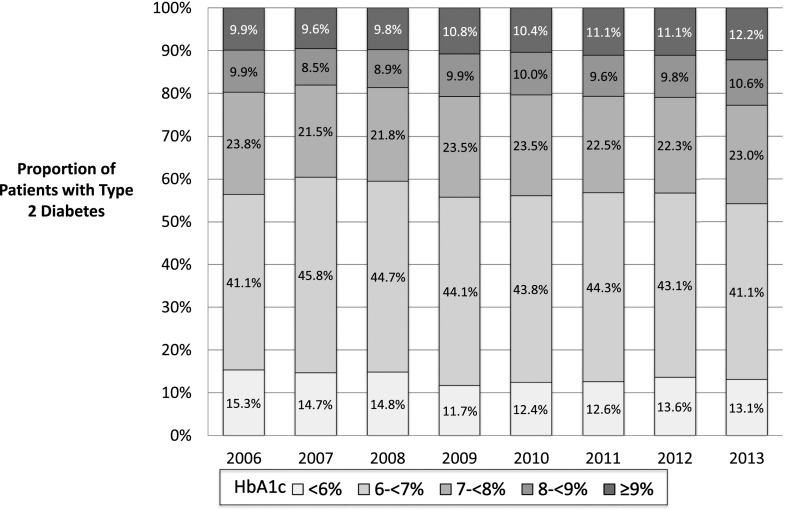
Standardized rates of glycemic control are shown in Fig. 2. From 2006 to 2013, there were increasing trends in the proportion of patients with HbA1c ≥9% and HbA1c 8 to <9% (from 9.9 to 12.2% and 9.9 to 10.6%, respectively; P < 0.001). The trend in the proportion of patients with HbA1c 7 to <8% was not significant (from 23.8 to 23.0%; P = 0.31). In contrast, there were decreasing trends in the proportion with HbA1c 6 to <7% (41.1 to 43.1%) and HbA1c <6% (15.3 to 13.1%; both P < 0.001). Of note, the overall slight decreasing trend for HbA1c 6 to <7% occurred despite a slightly higher proportion of patients in this glycemic category in 2013. Finally, the overall proportion of patients with HbA1c <7% declined over this 8-year period: 56.4% in 2006 and 54.2% in 2013, P < 0.001.
Figure 2.
Glycemic control among patients with T2DM, 2006–2013. Estimates were standardized by age, sex, race, and region to the 2013 cohort of people included in the study.
Glycemic control varied by age (Supplementary Fig. 1) and number of serious comorbidities (Supplementary Fig. 2). Poor glycemic control (HbA1c ≥9%) was most common among the youngest patients but increased slightly over time across all age subgroups (among the youngest: 21.1 to 23.3%, P = 0.001; and among the oldest: 5.3 to 6.3%, P < 0.001). Similarly, poor glycemic control was most common among patients without comorbidities but increased slightly across all comorbidity subgroups (no comorbidities: 14.0 to 14.8%, one comorbidity: 12.0 to 12.5%, and two or more comorbidities: 10.6 to 11.8%; all P < 0.001).
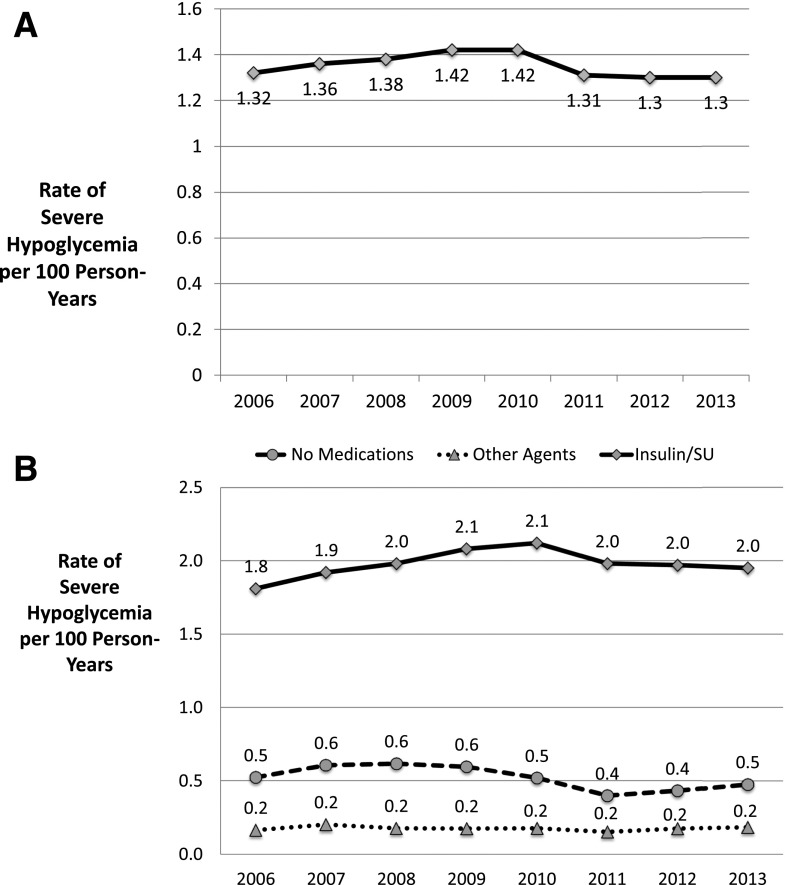
Severe Hypoglycemia
The age- and sex-standardized rate of severe hypoglycemia among people who filled at least one prescription for diabetes medications was 1.3 events per 100 person-years in both years 2006 and 2013 (P value for trend over time 0.72) (Fig. 3A). The proportion of severe hypoglycemia that led to hospital admission declined from 19.2 to 18.2% over this time period. Rates of severe hypoglycemia among patients using insulin or insulin secretagogues or other glucose-lowering agents and among those who filled no medications are shown in Fig. 3B.
Figure 3.
Age- and sex-standardized rate of severe hypoglycemia resulting in hospital admission, observation stay, or emergency department visit per 100 person-years, 2006–2013. A: Patients with T2DM who filled at least one glucose-lowering agent. B: Patients with T2DM who filled insulin or insulin secretagogues (diamonds), other glucose-lowering agents (triangles), and no glucose-lowering agents (circles). SU, sulfonylurea.
Rates of severe hypoglycemia were highest among the oldest patients and those with multiple comorbidities compared with younger, healthier adults (Supplementary Figs. 3 and 4). Rates of severe hypoglycemia increased slightly among the youngest (from 0.8 to 0.9 events per 100 person-years; P = 0.025) and middle-age (0.6 to 0.9 events per 100 person-years; P < 0.001) patients and decreased among the older (1.4 to 1.3 events per 100 person-years; P < 0.001) and oldest (2.9 to 2.3 events per 100 person-years; P < 0.001) patients over the study period. Rates of severe hypoglycemia were also highest among patients with two or more comorbidities compared with those with one or no comorbidities and did not significantly change over time (3.2 to 3.5 events per 100 person-years; P = 0.36).
Sensitivity Analyses
Analyses that included only 1 year of data per patient showed qualitatively similar results for trends in glycemic control (Supplementary Table 7). However, in analyses of severe hypoglycemia, the standardized rate decreased from 1.5 to 1.2 events per 100 person-years with a trend P value of <0.01 (Supplementary Fig. 5).
Conclusions
The landscape of glucose-lowering medications available for T2DM has changed dramatically over the past two decades. From 2006 to 2013, utilization of newer glucose-lowering agents, such as DPP-4 inhibitors and newer insulin analogs and their formulations, increased considerably among privately insured patients with T2DM. The use of older classes of medications, such as sulfonylureas and thiazolidinediones, declined. During this time, glycemic control of T2DM did not improve in the overall population and remained poor among nearly a quarter of the youngest patients. Rates of severe hypoglycemia remained largely unchanged, with the oldest patients and those with multiple comorbidities at highest risk. These findings raise questions about the value of the observed shifts in drug utilization toward newer and costlier medications.
Our findings are consistent with a prior study of drug prescribing in U.S. ambulatory practice conducted from 1997 to 2012 (2). In that study, similar increases in DPP-4 inhibitor and insulin analog prescribing were observed; these changes were accompanied by a 61% increase in drug expenditures (2). Our study extends these findings to drug utilization and demonstrates that these increases occurred in all age and comorbidity subgroups.
In contrast, metformin use increased only modestly between 2006 and 2013 and remained relatively low among older patients and those with two or more comorbidities. Although metformin is recommended as first-line therapy (26), it may be underutilized as the initial agent for the treatment of T2DM (27). Its use may be additionally limited by coexisting contraindications, such as chronic kidney disease (28). Recently, the U.S. Food and Drug Administration (FDA) issued a labeling change, congruent with recommendations from the ADA (26), which permits cautious use of metformin in those with mild to moderate kidney disease (29). As a result, it is possible that use of metformin in these patients may increase further.
We found no overall improvements in glycemic control among patients with T2DM; in fact, the proportion of patients with poor glycemic control increased. A prior study based on NHANES data showed an overall 8% increase in the proportion of patients with HbA1c <7% from 1999–2002 to 2007–2010 (13). However, the increase occurred early on in the study, with no significant change in this proportion from 2003–2006 to 2007–2010. It is possible that enthusiasm for intensive glycemic control may have been dampened by the findings of increased mortality with this strategy in one trial published in 2008 (8) and the lack of cardiovascular benefit reported in two others (6,7). In addition, the expected glucose-lowering efficacy associated with some newer agents, such as the DPP-4 inhibitors, may be relatively modest (30). In our study, the mean number of days covered for each class of glucose-lowering medications increased over the study period, thereby reducing the likelihood that the overall trend in poor glycemic control was due to declining adherence.
Since the balance of benefits and harms of glycemic control differs by age and comorbidity burden, we examined glycemic control trends in relevant subgroups. In our study, less than half of the youngest patients (48.0%) but >60% of the oldest patients (61.6%) achieved an HbA1c <7% by 2013. In contrast, nearly a quarter of the youngest patients (23.3%) but only a small minority of the oldest patients (6.3%) had poor glycemic control at the end of the study period. The youngest adults in NHANES were also least likely to achieve recommended HbA1c targets (13). Limited access to care and lack of insurance coverage for medications are known to contribute to suboptimal glycemic control and may partly explain poor control among the youngest NHANES participants (31). However, our study included adults with full medical and pharmacy benefits coverage, so lack of access to care is unlikely to explain our findings. Young age at diabetes onset has been associated with worse glycemic control (32) and more aggressive disease (33,34). Younger adults also use health care less often. However, the youngest adults are generally expected to derive the most benefit from glycemic control in the long-term (35). In contrast, many older adults are less likely to benefit and are more likely to be harmed by overly aggressive glycemic control, especially those with multiple competing health problems (10,36). At the population level, the quality of glycemic control in our study appears to be misaligned given the likelihood of benefits and harms expected from intensive glycemic control.
Greater utilization of newer, more expensive drugs that do not typically cause hypoglycemia might be expected to result in lower rates of severe hypoglycemia over time. In addition, recent guidelines have specifically called for more relaxed glycemic targets and less intensive treatment among patients at risk for hypoglycemia (37). However, we found that the rate of hypoglycemic events leading to either ED visit or hospitalization did not improve over time. We did find an overall increase in insulin use (predominantly insulin analogs), which could have contributed to these trends, although we also found a decline in the use of sulfonylureas.
Consistent with prior studies, rates of severe hypoglycemia were highest among oldest adults and those with multiple comorbidities (18,38,39). These differences likely reflect greater vulnerability to hypoglycemia among these patients, greater prevalence of comorbidities that increase the risk of events (such as renal failure and dementia), as well as differences in drug utilization among these age and comorbidity subgroups, as discussed above. Despite the well-known adverse impacts of hypoglycemia on health-related quality of life and on multiple health outcomes (40–42), severe hypoglycemia continues to pose a threat to the oldest adults and those with multiple comorbidities.
Our results should be interpreted cautiously, in light of several limitations. Our analyses were based on medical and pharmacy claims data, supplemented by laboratory data. Our large sample of privately insured patients with T2DM may not be representative of all privately insured patients in the U.S. Lower rates of adoption of newer, costlier medications might be expected in an uninsured population. Moreover, our database (OLDW) included an increasing number of adults over time, requiring us to standardize data by age, race, sex, and region. This may incompletely capture changes in the types of patients included in the study. Our analyses of glycemic control relied on HbA1c obtained during routine care in a subset of the total sample; it is possible that differences in HbA1c testing may have occurred over time. In addition, some patients were captured in multiple years of data, raising concern that increasing disease severity over time contributed to secular trends. Our sensitivity analyses showed qualitatively similar trends but with a reduction in overall hypoglycemia over time; however, these analyses included the greatest representation of patients who became eligible to enter the cohort during the last year, and thus with the shortest duration of diabetes. Our analyses of severe hypoglycemia captured only those events that led to hospital or emergency department use, but did not capture events treated outside of those settings. Finally, our study design precludes causal inference regarding the relationships between the trends in drug utilization, glycemic control, and hypoglycemia. Therefore, our discussion with respect to causality remains speculative.
Costs of diabetes care have dramatically increased (2,4,43). Between 1987 and 2011, per person medical spending attributable to diabetes doubled (4). More than half of the increase was due to prescription drug spending (4). Despite these spending increases and greater utilization of newly developed medications, we showed no concurrent improvements in overall glycemic control or the rates of severe hypoglycemia in our study. Although the use of newer and more expensive agents may have other important benefits (44), further studies are needed to define the value and cost-effectiveness of current treatment options.
Supplementary Material
Article Information
Funding. This publication was made possible in part by the National Center for Advancing Translational Sciences, a component of the National Institutes of Health (NIH) (CTSA grant UL1 TR000135). K.J.L. receives support from the National Institute on Aging and the American Federation of Aging Research through the Paul Beeson Career Development Award (K23AG048359) and the Yale Claude D. Pepper Older Americans Independence Center (P30AG021342). X.Y., R.G.M., and N.D.S. receive support from the Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery at the Mayo Clinic. M.A.S. receives support from the NIH (K24AG049057 and P30AG044281). T.M.G. is the recipient of an Academic Leadership Award from the National Institute on Aging (K07AG3587).
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of the NIH.
Duality of Interest. K.J.L., J.S.R., and H.M.K. work under contract for the Centers for Medicare & Medicaid Services to develop and maintain performance measures that are used for public reporting. J.S.R. and H.M.K. report receiving research support through Yale University from Medtronic, Inc., and Johnson & Johnson (Janssen) to develop methods of clinical trial data sharing and from the FDA to develop methods for postmarket surveillance of medical devices. J.S.R. receives research support from the Blue Cross Blue Shield Association to better understand medical technology evidence generation. M.A.S. is a paid consultant for iodine.com. S.E.I. serves as a consultant or research study committee member for Boehringer Ingelheim, Merck, AstraZeneca, Sanofi, Janssen, Daiichi Sankyo, and Novo Nordisk. Takeda has provided study supplies to a trial on which S.E.I. has served as a co-investigator. H.M.K. chairs a cardiac scientific advisory board for UnitedHealthcare. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. K.J.L. conceived the study protocol and analysis plan, researched data, wrote the first draft of the manuscript, and reviewed and edited the manuscript. X.Y. completed all statistical analyses, contributed to the discussion, and reviewed and edited the manuscript. J.H., R.G.M., J.S.R., M.A.S., S.E.I., and T.M.G. contributed to the discussion and reviewed and edited the manuscript. H.M.K. and N.D.S. conceived the study protocol and analysis plan, researched data, and reviewed and edited the manuscript. K.J.L. and N.D.S. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Part of this work was presented as an oral presentation at the 76th Scientific Sessions of the ADA, New Orleans, LA, 10–14 June 2016.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-0985/-/DC1.
This article is featured in a podcast available at http://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.Alexander GC, Sehgal NL, Moloney RM, Stafford RS. National trends in treatment of type 2 diabetes mellitus, 1994-2007. Arch Intern Med 2008;168:2088–2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turner LW, Nartey D, Stafford RS, Singh S, Alexander GC. Ambulatory treatment of type 2 diabetes in the U.S., 1997–2012. Diabetes Care 2014;37:985–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Hypoglycaemia Study Group. Minimizing hypoglycemia in diabetes. Diabetes Care 2015;38:1583–1591 [DOI] [PubMed] [Google Scholar]
- 4.Zhuo X, Zhang P, Kahn HS, Bardenheier BH, Li R, Gregg EW. Change in medical spending attributable to diabetes: national data from 1987 to 2011. Diabetes Care 2015;38:581–587 [DOI] [PubMed] [Google Scholar]
- 5.Lipska KJ, Ross JS, Van Houten HK, Beran D, Yudkin JS, Shah ND. Use and out-of-pocket costs of insulin for type 2 diabetes mellitus from 2000 through 2010. JAMA 2014;311:2331–2333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duckworth W, Abraira C, Moritz T, et al.; VADT Investigators . Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–139 [DOI] [PubMed] [Google Scholar]
- 7.Patel A, MacMahon S, Chalmers J, et al.; ADVANCE Collaborative Group . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 8.Gerstein HC, Miller ME, Byington RP, et al.; Action to Control Cardiovascular Risk in Diabetes Study Group . Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Diabetes Association Standards of medical care in diabetes—2009. Diabetes Care 2009;32(Suppl. 1):S13–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care 2012;35:2650–2664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Diabetes Association. Summary of revisions. In Standards of Medical Care in Diabetes—2016. Diabetes Care 2016;39(Suppl. 1):S4–S5 [DOI] [PubMed] [Google Scholar]
- 12.Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med 2014;174:1116–1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999-2010. N Engl J Med 2013;368:1613–1624 [DOI] [PubMed] [Google Scholar]
- 14.Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med 2014;174:678–686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011;365:2002–2012 [DOI] [PubMed] [Google Scholar]
- 16.McCoy RG, Zhang Y, Herrin J, et al. Changing trends in type 2 diabetes mellitus treatment intensification, 2002-2010. Am J Manag Care 2015;21:e288–e296 [PubMed] [Google Scholar]
- 17.Zoungas S, Patel A, Chalmers J, et al.; ADVANCE Collaborative Group . Severe hypoglycemia and risks of vascular events and death. N Engl J Med 2010;363:1410–1418 [DOI] [PubMed] [Google Scholar]
- 18.McCoy RG, Lipska KJ, Yao X, Ross JS, Montori VM, Shah ND. Intensive treatment and severe hypoglycemia among adults with type 2 diabetes. JAMA Intern Med 2016;176:969–978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wallace PJ, Shah ND, Dennen T, Bleicher PA, Crown WH. Optum Labs: building a novel node in the learning health care system [published correction appears in Health Aff (Millwood) 2014;33:1703]. Health Aff (Millwood) 2014;33:1187–1194 [DOI] [PubMed] [Google Scholar]
- 20. Optum Labs. Optum research data assets. Available from https://www.optum.com/content/dam/optum/resources/productSheets/5302_Data_Assets_Chart_Sheet_ISPOR.pdf. Accessed 15 September 2016.
- 21.National Committee for Quality Assurance. HEDIS 2009 Volume 2 Technical Update [Internet]. National Committee for Quality Assurance. Available from http://www.ncqa.org/portals/0/PolicyUpdates/HEDIS%20Technical%20Updates/09_CDC_Spec.pdf. Accessed 16 September 2016
- 22.Chen G, Khan N, Walker R, Quan H. Validating ICD coding algorithms for diabetes mellitus from administrative data. Diabetes Res Clin Pract 2010;89:189–195 [DOI] [PubMed] [Google Scholar]
- 23.Hebert PL, Geiss LS, Tierney EF, Engelgau MM, Yawn BP, McBean AM. Identifying persons with diabetes using Medicare claims data. Am J Med Qual 1999;14:270–277 [DOI] [PubMed] [Google Scholar]
- 24.Leong A, Dasgupta K, Bernatsky S, Lacaille D, Avina-Zubieta A, Rahme E. Systematic review and meta-analysis of validation studies on a diabetes case definition from health administrative records. PLoS One 2013;8:e75256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ginde AA, Blanc PG, Lieberman RM, Camargo CA Jr. Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr Disord 2008;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American Diabetes Association. Standards of Medical Care in Diabetes—2015 Diabetes Care 2015;38(Suppl. 1):S1–S93 [Google Scholar]
- 27.Berkowitz SA, Krumme AA, Avorn J, et al. Initial choice of oral glucose-lowering medication for diabetes mellitus: a patient-centered comparative effectiveness study. JAMA Intern Med 2014;174:1955–1962 [DOI] [PubMed] [Google Scholar]
- 28.Inzucchi SE, Lipska KJ, Mayo H, Bailey CJ, McGuire DK. Metformin in patients with type 2 diabetes and kidney disease: a systematic review. JAMA 2014;312:2668–2675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA Revises Warnings Regarding Use of the Diabetes Medicine Metformin in Certain Patients with Reduced Kidney Function. Silver Spring, MD, U.S. Food and Drug Administration, 2016 [Google Scholar]
- 30.Amori RE, Lau J, Pittas AG. Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA 2007;298:194–206 [DOI] [PubMed] [Google Scholar]
- 31.Zhang X, Bullard KM, Gregg EW, et al. Access to health care and control of ABCs of diabetes. Diabetes Care 2012;35:1566–1571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berkowitz SA, Meigs JB, Wexler DJ. Age at type 2 diabetes onset and glycaemic control: results from the National Health and Nutrition Examination Survey (NHANES) 2005-2010. Diabetologia 2013;56:2593–2600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Constantino MI, Molyneaux L, Limacher-Gisler F, et al. Long-term complications and mortality in young-onset diabetes: type 2 diabetes is more hazardous and lethal than type 1 diabetes. Diabetes Care 2013;36:3863–3869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wong J, Molyneaux L, Constantino M, Twigg SM, Yue DK. Timing is everything: age of onset influences long-term retinopathy risk in type 2 diabetes, independent of traditional risk factors. Diabetes Care 2008;31:1985–1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Inzucchi SE, Bergenstal RM, Buse JB, et al.; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD) . Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lipska KJ, Montori VM. Glucose control in older adults with diabetes mellitus--more harm than good? JAMA Intern Med 2013;173:1306–1307 [DOI] [PubMed] [Google Scholar]
- 37.Kirkman MS, Briscoe VJ, Clark N, et al.; Consensus Development Conference on Diabetes and Older Adults . Diabetes in older adults: a consensus report. J Am Geriatr Soc 2012;60:2342–2356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Miller ME, Bonds DE, Gerstein HC, et al.; ACCORD Investigators . The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: post hoc epidemiological analysis of the ACCORD study. BMJ 2010;340:b5444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davis TM, Brown SG, Jacobs IG, Bulsara M, Bruce DG, Davis WA. Determinants of severe hypoglycemia complicating type 2 diabetes: the Fremantle Diabetes Study. J Clin Endocrinol Metab 2010;95:2240–2247 [DOI] [PubMed] [Google Scholar]
- 40.McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Self-report of hypoglycemia and health-related quality of life in patients with type 1 and type 2 diabetes. Endocr Pract 2013;19:792–799 [DOI] [PubMed] [Google Scholar]
- 41.McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care 2012;35:1897–1901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bloomfield HE, Greer N, Newman D, et al. Predictors and Consequences of Severe Hypoglycemia in Adults With Diabetes - A Systematic Review of the Evidence. Washington, DC, U.S. Department of Veterans Affairs, 2012 [PubMed] [Google Scholar]
- 43.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zinman B, Wanner C, Lachin JM, et al.; EMPA-REG OUTCOME Investigators . Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–2128 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.