Obesity is frequently associated with chronic low-grade systemic inflammation, which is believed to underlie the onset of secondary complications of this disease (1,2). In 2005, studies from the laboratory of Dr. Licio Velloso in Brazil indicated that inflammatory processes in the hypothalamus are also activated in response to diet-induced obesity and that if this inflammatory signaling is blocked, systemic glucose metabolism is improved (3). This same group later demonstrated that microglia participate in diet-induced obesity–associated hypothalamic inflammation (4), with subsequent reports suggesting that hypothalamic inflammation occurs very rapidly in response to high-fat diet (HFD) intake, even prior to substantial weight gain (5). These observations have given rise to the hypothesis that hypothalamic inflammation is a critical process in the onset of obesity and the development of its secondary complications. However, some investigators question whether central inflammation is the initial trigger or only a consequence and remain skeptical as to the real importance of this process.
In a study published in this issue of Diabetes, André et al. (6) investigated whether inhibition of microglial proliferation in the hypothalamus can improve the metabolic response to an HFD. They infused the antimitotic drug arabinofuranosyl cytidine (AraC) intracerebroventricularly to prevent proliferation of microglia. They report that AraC prevented HFD-induced proliferation of microglia specifically in the medial basal hypothalamus and blunted the hyperphagia and increased fat mass accrual normally observed in response to this diet. This was interpreted to indicate that microglial proliferation is involved in the detrimental response to an HFD. No apparent effect of AraC was observed in mice on a control chow diet, which, as the authors suggest, could indicate that blockage of this process may only be relevant when counterregulatory mechanisms are invoked in response to some challenge or change. This, however, must be placed into the context of the relatively short period of time that central cell proliferation is blocked, as basal cell turnover is surely important for normal long-term maintenance.
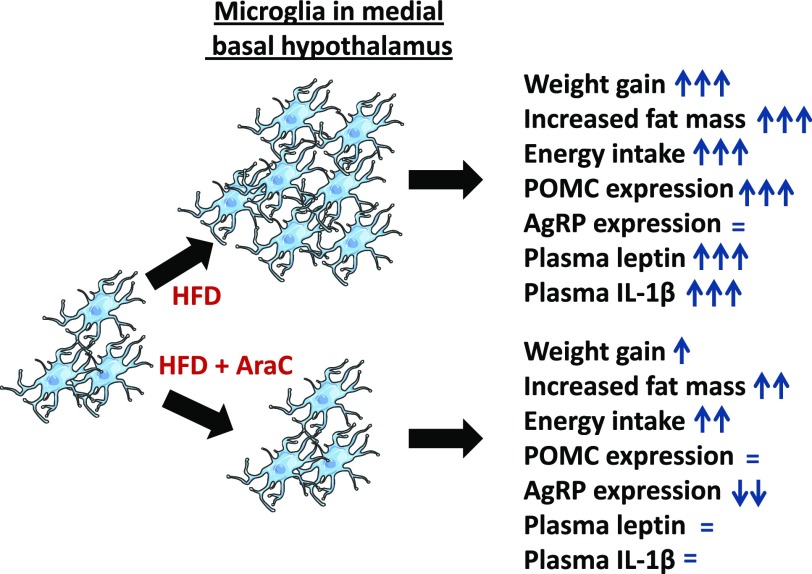
Although André et al. (6) report that AraC infusion in mice consuming an HFD normalized central inflammatory markers and microglial density while reducing food intake and weight gain, these mice continued to eat significantly more and gain more fat mass than mice on the control diet (as summarized in Fig. 1). Thus, although not discussed, other mechanisms are clearly involved in aberrant appetite control. Moreover, parameters such as circulating interleukin (IL)-1β and leptin levels returned to control levels, which is inconsistent with the persistent increase in fat mass. It remains to be determined whether systemic inflammation occurs when increased fat mass is maintained over a longer period of time even in the absence of central microglial proliferation, which would indicate alternative cause-and-effect mechanisms.
Figure 1.
André et al. (6) report that microglia proliferate specifically in the medial basal hypothalamus in response to an HFD. This is associated with increased weight gain, fat mass, energy intake, POMC expression, and serum leptin and IL-1β levels. When treated intracerebroventricularly with AraC, microglia do not proliferate in response to HFD intake, and HFD-induced weight gain and fat mass are reduced, while plasma leptin and IL-1β levels remain at control levels. Hypothalamic neuropeptide expression is modified, such that the mRNA levels of POMC are unchanged and AgRP decreased. Thus, although microglial proliferation is blocked, weight and fat mass accrual are only partially inhibited but systemic inflammation is constrained. AgRP, agouti-related protein; POMC, proopiomelanocortin.
The temporal analysis of inflammatory processes is indeed important because the first response of glial cells is generally considered to be protective against harmful substances, even in response to HFD intake (7,8). Here, the “rapid” response was measured 1 week after HFD initiation. What occurs during the first day of HFD intake? If the initial inflammatory/glial response is to protect, i.e., reduce food intake, is there a rapid increase in hyperphagia if microglia are not activated in response to an HFD? The fact that we are most likely looking at different inflammatory responses should be taken into consideration when interpreting the results reported by André et al. (6).
One important observation that is not discussed or analyzed in depth is that when given a very high-fat, very low-carbohydrate diet (VHFD), mice did not present increased microglial proliferation. As this VHFD is deficient in carbohydrates, it is in essence a ketogenic diet. The authors suggest that a minimum amount of carbohydrate intake is necessary for the pathological response to fatty acids. This observation questions studies indicating that fatty acids themselves are one of the crucial initial signals for the induction of gliosis in response to an HFD (4,9,10). The lack of sufficient carbohydrates as fuel would necessitate increased fatty acid catabolism, even centrally, and thus would modify the local nutrient-sensing mechanisms. Further investigation of this observation could shed light on how combinations of nutrients are sensed centrally, as well as the role of glial cells in this process.
This study clearly supports the concept that microglial proliferation is implicated in the weight-gain response to an HFD, and it confirms previous studies demonstrating that activation of hypothalamic inflammatory mechanisms is involved in obesity-associated complications. Intriguingly, a recent study argues for a role of arcuate nucleus microglia activation in the aphagia associated with sickness (11). Thus, more than clarifying the relationship between microglial activation and metabolic phenotype, a vast number of important questions arise. Under AraC treatment, no increase in energy intake explains the lack of weight gain, but is the HFD-associated hyperphagia blocked because of inhibition of microglial proliferation? Or is the response to HFD modified due to the blockage of neuronal proliferation/reorganization in metabolic circuits that has been reported by others (12,13)? Why does a VHFD not cause microglia activation? These studies were all performed in male mice. Do females respond equally? Can hypothalamic inflammatory processes be specifically manipulated by less invasive treatments to improve dietary habits and thus control weight gain? Is hypothalamic inflammation a nonspecific category of a vast array of different signaling events that need to be more carefully addressed and interpreted? The studies reported here clearly indicate that addressing these issues is crucial in order to develop strategies to target explicit aspects of hypothalamic inflammation for treatment of metabolic disorders.
Article Information
Funding. The authors are funded by grants from the Spanish Ministry of Science and Innovation (BFU2014-51836-C2-2 to J.A.C.), Fondo de Investigación Sanitaria (PI1302195, PI1600485, and Centro de Investigación Biomédica en Red de Obesidad y Nutrición to J.A.), Fondo Europeo de Desarrollo Regional, the National Institutes of Health (DK-006850 and AG-040236 to T.L.H.), and American Diabetes Association (to T.L.H.).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying article, p. 908.
References
- 1.Esser N, Legrand-Poels S, Piette J, Scheen AJ, Paquot N. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract 2014;105:141–150 [DOI] [PubMed] [Google Scholar]
- 2.Schenk S, Saberi M, Olefsky JM. Insulin sensitivity: modulation by nutrients and inflammation. J Clin Invest 2008;118:2992–3002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Souza CT, Araujo EP, Bordin S, et al. . Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology 2005;146:4192–4199 [DOI] [PubMed] [Google Scholar]
- 4.Milanski M, Degasperi G, Coope A, et al. . Saturated fatty acids produce an inflammatory response predominantly through the activation of TLR4 signaling in hypothalamus: implications for the pathogenesis of obesity. J Neurosci 2009;29:359–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thaler JP, Yi CX, Schur EA, et al. . Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest 2012;122:153–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.André C, Guzman-Quevedo O, Rey C, et al. Inhibiting microglia expansion prevents diet-induced hypothalamic and peripheral inflammation. Diabetes 2017;66:908–919 [DOI] [PubMed]
- 7.Benani A, Hryhorczuk C, Gouazé A, et al. . Food intake adaptation to dietary fat involves PSA-dependent rewiring of the arcuate melanocortin system in mice. J Neurosci 2012;32:11970–11979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buckman LB, Thompson MM, Lippert RN, Blackwell TS, Yull FE, Ellacott KL. Evidence for a novel functional role of astrocytes in the acute homeostatic response to high-fat diet intake in mice. Mol Metab 2014;4:58–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta S, Knight AG, Gupta S, Keller JN, Bruce-Keller AJ. Saturated long-chain fatty acids activate inflammatory signaling in astrocytes. J Neurochem 2012;120:1060–1071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valdearcos M, Robblee MM, Benjamin DI, Nomura DK, Xu AW, Koliwad SK. Microglia dictate the impact of saturated fat consumption on hypothalamic inflammation and neuronal function. Cell Reports 2014;9:2124–2138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jin S, Kim JG, Park JW, Koch M, Horvath TL, Lee BJ. Hypothalamic TLR2 triggers sickness behavior via a microglia-neuronal axis. Sci Rep 2016;6:29424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horvath TL, Sarman B, García-Cáceres C, et al. . Synaptic input organization of the melanocortin system predicts diet-induced hypothalamic reactive gliosis and obesity. Proc Natl Acad Sci U S A 2010;107:14875–14880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee DA, Bedont JL, Pak T, et al. . Tanycytes of the hypothalamic median eminence form a diet-responsive neurogenic niche. Nat Neurosci 2012;15:700–702 [DOI] [PMC free article] [PubMed] [Google Scholar]