Abstract
Evidence-based recommendations for physical activity following spinal fusion surgeries for idiopathic scoliosis are limited, specifically in the adolescent population. Individuals with scoliosis treated operatively or non-operatively have been reported to participate in less than 1–3 days/week of even mildly strenuous physical exercises. Over 40% of individuals with scoliosis returned to sports at a level lower than pre-operative participation levels or did not return at all post spinal fusion. It is particularly important for human movement specialists, such as physical therapists, occupational therapists, athletic trainers and kinesiologists to assist these individuals effectively transition to and maintain engagement in physical activity. This review provides a snapshot of common considerations and potential factors influencing individuals with spinal-fusion for scoliosis to participate in safe physical activity.
Keywords: Scoliosis, adolescent idiopathic scoliosis, spinal fusion, arthrodesis, physical therapy, sports
INTRODUCTION
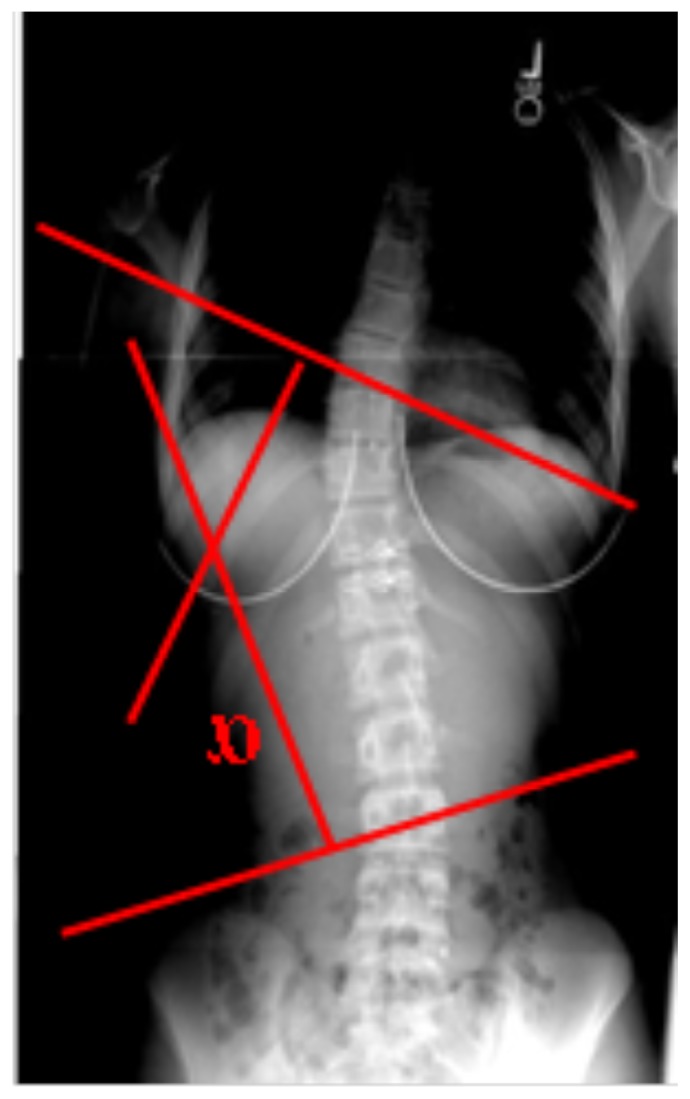
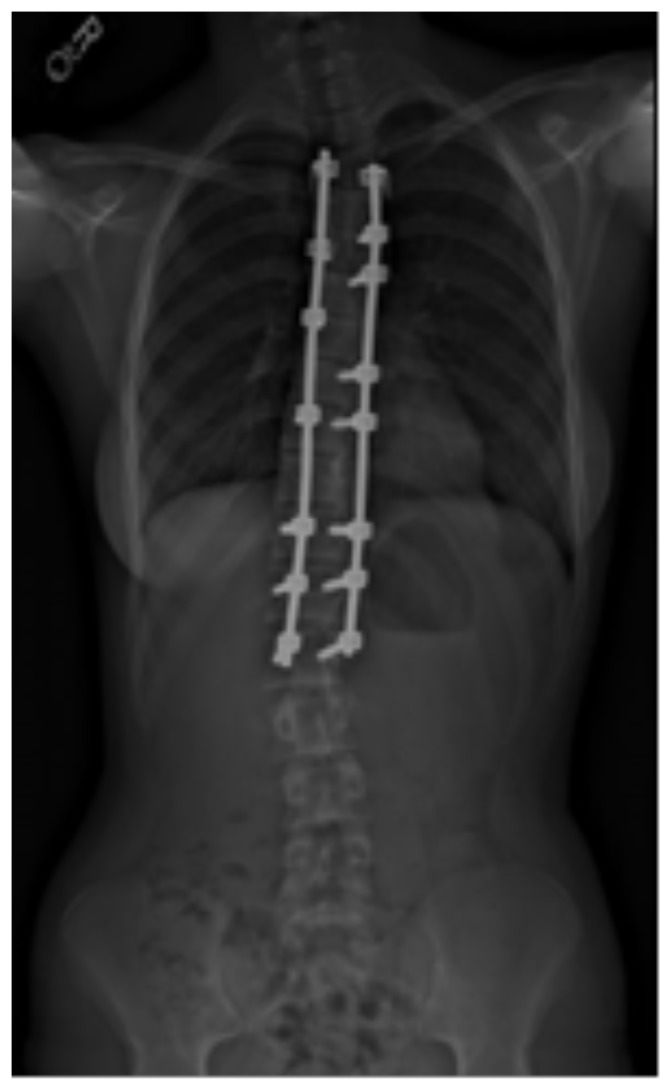
Idiopathic scoliosis (IS) is defined as the development of abnormal 3D curvatures of the spine, primarily those in the frontal plane (Figure 1), with no clear etiology (11). Most IS occurs during adolescence (10–19 years old, skeletally immature) and is the age group most likely to undergo arthrodesis of the vertebral segments, commonly known as ‘spinal fusion’ (Figure 2), to halt scoliotic progression and reduce severe spinal curvature and other possible symptoms, such as pain and reduced pulmonary function (16). Based on limited evidence, physical activity or sports participation of individuals with IS may be reduced compared to healthy individuals without scoliosis due to a wide variety of reasons such as loss of flexibility, back pain and deconditioning to name a few, especially in those who have had spinal fusion (18, 39, 41). Fewer than 60% of individuals with spinal fusion returned to physical activity levels equal or higher than pre-operative levels (18).
Figure 1.
Radiographic image of a scoliotic spine. α = Cobb angle. Curvature of >10° indicates scoliosis.
Figure 2.
Radiographic image of a scoliotic spine post spinal fusion surgery.
Reduction in physical activity can have detrimental effects on general health and well being, especially in younger populations, such as those with adolescent idiopathic scoliosis (AIS). (8, 10, 29, 30). Thus, it will be helpful to explore potential reasons fewer individuals with spinal fusion for AIS engage in sport and physical activity than their peers. In this way, health care professionals may be more successful in promoting physical activity to their clients. Moreover, postoperatively, the decreased trunk flexibility due to the spinal fusion requires individuals to adapt altered movements patterns during certain activities (60). Hence, human movement specialists need to know how to work effectively with these individuals who have had spinal fusion surgery for scoliosis. The objective of this review is to provide a brief background on scoliosis, review factors to be aware of for individuals with scoliosis to participate in safe physical activity, and promote physical activity participation.
Background
Approximately 7 million individuals in the United States are affected by scoliosis (19). In adolescents and juveniles, scoliosis is diagnosed as idiopathic in 70% of the structural deformities of the spine (20). AIS is the most common variant of scoliosis(3) and the most common spinal deformity witnessed by pediatricians and primary care physicians (1). AIS is present in 2% to 4% of children between 10 and 16 years of age (47). Higher rates of prevalence are observed for girls than boys, ranging from 1.5 times greater for scoliosis curves less than 10° to approximately 7.2–10 times for curves greater than 40° (27, 47).
Etiology, Pathogenesis and Treatment Options
AIS curvature begins during adolescence. Although the etiology is not well understood, causation likely is multifactorial. The causes and rate of progression has been linked to genetics, premature osteoarthrosis, repetitive tensile stresses on the spine, compression of the patient’s body prenatally, imbalanced growth among soft and hard tissue components of the spine during childhood and adolescence, and generalized osteopenia, among other etiological factors (56, 57). Recently pathogenesis of AIS has been linked to the conditions of neuromuscular system and disorders of the connective tissue that aid in stability of the spine (1, 14). Discussed later, some of these associated factors also may need to be considered when working with individuals with spinal fusion for AIS.
The majority of individuals diagnosed with AIS require some form of treatment. Untreated scoliotic curvatures can have significant detrimental effects on physical activity, appearance, lifestyle, quality of life (58), along with pulmonary impairment of an individual and may even lead to premature death (3). The effects can be direct, such as the loss in spinal range of motion, or indirect but critical, such as decreased cardio-vascular conditioning (40) and reduced bone mineral density (22). In untreated individuals, there is an increased change for morbidity due to abnormal lung function(40) and substantial reduction in physical activity (41). For an adolescent who is very conscious of appearance and social status among peers, physical activity has been shown to be particularly beneficial with increasing body image perception, decreasing associated depression and increasing self-esteem (15, 61).
For an adolescent diagnosed with scoliosis, treatment is based on the magnitude of spinal curvature, and considered more aggressive if the curvature continues to increase and/or the rate of curvature formation increases. (35) For individuals with Cobb angles (curvature of the spine calculated using a radiograph) of less than 25°, careful monitoring every 4–6 months is done until he/she reaches skeletal maturity. Individuals are prescribed physical therapy and exercise for postural correction and strengthening of postural muscles but its effectiveness is yet to be established. (32) For adolescents with curves of ~25° to ~40°, brace treatment is used. The individual is instructed to wear the brace for about 23 hours/day for the treatment to be effective. Bracing has only been reported to be effective in preventing spinal fusion surgery if the patient is highly compliant (49). About 68% to 79% of these adolescents will have spinal curvature (Cobb angle > 40° to 50°; see Figure 1) that continues to progress (53). Spinal fusion surgery then may be recommended, based on assessment of a combination of factors, including current severity of the spinal curvature, likelihood of continued progression and/or rate of progression and potential for pain reduction (35). Spinal fusion has had good success, as individuals with spinal fusion have reported better quality of life scores on a Scoliosis Research Society (SRS) questionnaire 10 years post-surgery(2) than those treated with back bracing.
Understanding how to work with clients with spinal fusion is important, as there has been an exponential increase in the number of spinal fusion surgeries being performed in the last two decades. Researchers report a 137% increase in successful discharges from 1998 to 2008(45), averaging to about 10.2 per 100,000 population in 2011 (37).
PHYSICAL ACTIVITY: A LACK THEROF FOR INDIVIDUALS WITH SCOLIOSIS
Potential Factors Influencing Physical Activity
There are several factors that may be responsible for individuals with AIS participating in physical activity post spinal fusion. These factors could be broadly classified into participant-related and clinician/surgeon-related.
For participant-related factors, functional limitations and back pain are considered some of the main reasons that discourage activity (41). Decreased flexibility (17), reduced balance (7), physical deconditioning, and loss of desire have also been reported as some potential reasons (9, 18). Fear of injury and self-consciousness about appearance have also been reported to reduce physical and social activity participation (13).
For the surgeon/clinician factors, caution to avoid a patient from undergoing spinal trauma during movements involving spinal rotations and bending is the biggest reason (39). Long-term consequences of repetitive loading of the spine, intervertebral discs and the fusion components also are of concern (21, 23).
A body of evidence is available suggesting that there are structural changes to the vertebrae adjacent to the lowest instrumented vertebra (LIV). Degenerative disc degeneration has also been reported in segments adjacent to fusion via Harrington instrumentation (21). This has also been linked to low back pain and retrolisthesis, more so with patients with L4 level fusion (21). Researchers have proposed that spinal fusion can have long-term adverse effects on vertebral health especially in young scoliotic patients (23). There have also been reports of association of degenerative disc degeneration with postoperative thoracal flat-back (6). Although there have been considerable improvements in surgical methodologies in the recent years, more evidence is needed to understand long-term effects of the surgery. LIV may also be one factor used by a surgeon in deciding to allow return to particular physical activities or sports, such as collision sports, possibly because of its inverse relation to total available trunk range of motion (31). These are all valid associations and propositions of spinal fusion with long-term effects on spinal vertebrae that can accentuate with physical activity, potentially because of increased torsional loads and movement at the non-fused segments to compensate for the fused segments.
Among surgeons, there is wide variation in prescription of physical activities for individuals with spinal fusion (48). In a survey by Rubery et al., in 2002, 60% of the surgeons reported never recommending any collision sports (48), and only 13% felt contact sports could be allowed 6–12 months after surgery (48). The majority of the surgeons disallowed physical therapy (48) at that time, despite no scientific evidence to contraindicate it. Some surgeons, however, permit patients to engage in low-intensity physical education classes 6–12 months post-operatively (31, 48). A recent survey reported that about 78% of surgeons still do not allow post-surgical physical therapy but allow noncontact and contact sports postoperatively by 6 months and collision sports by 12 months respectively (31). One-fifth of surgeons do not allow these individuals to participate in any form of collision sports (31).
Evidence of Participation in Physical Activity
It is has been reported that individuals who have had a spinal fusion for AIS can perform maximal-effort sport movements without inducing an acute injury (12, 25, 26, 34, 38, 41, 48). Current literature supports safe participation post spinal fusion in competitive sports requiring extreme levels of spinal and pelvic movements, such as gymnastics (38) and golf (12). Additionally, Sarwahi (50) observed that many patients return to physical activity much earlier than surgeons recommended. The majority of patients (93% non-contact and 96% contact sports) surveyed returned to their preoperative level within one year. As there is little evidence, however, of the spinal loading that occurs during such movements, nor the long-term effects, professionals do not know what activities really are safe. Consequently, there is a lack of scientific evidence based recommendations or guidelines surgeons and other health care providers can follow.
Researchers have observed that after surgical fusion of the spine, individuals with AIS participated in sports equally as strenuous as age-matched controls (41). Parsch et al., reported the Sports Score (41) for individuals treated non operatively and operatively for scoliosis was 46.3 and 44.8, respectively, compared to 66.1 for healthy individuals without scoliosis (31). The score is combination of number of days/week and exertion, where, 100 = maximum score possible based on 4 – 7 days of ‘strenuous’ sport. However, the scale only asks about sports and activities of daily living, and exertion may not be accurate.
Recent studies have shown that individuals with spinal fusion can produce comparable trunk and lower extremity mechanics and balance as their healthy, non-scoliotic peers while participating in high intensity activities, such as running and jumping (25, 26, 33, 34, 52, 55). Although the maximum ranges of motion that can be achieved in the trunk is limited post-spinal fusion, the trunk and lower extremities can create adaptive strategies to achieve performance goals when participating in sports activities (25, 26, 54). Moreover, there is minimal demand for extreme ranges of trunk motion in activities such as running and jumping and is thus manageable by individuals with AIS with or without spinal fusions. (25, 26).
Public Health Impact
Prescription of physical activity post-spinal fusion has significant public health impact for scoliosis management. As stated previously, for individuals with scoliosis, physical activity may be particularly beneficial for decreasing body fat and improving aerobic capacity and muscle power (5) and is associated with improved proprioception (39), improved body image perception (15), resulting in increased self-esteem and decreased associated depression (61). Conversely, for girls with AIS, insufficient time spent performing weight-bearing physical activity during the peripubertal period has been observed by some (8), but not all researchers (42) to be a major determinant of low bone mass observed.
Lack of physical activity, in general, can cause other serious problems, such as increased risk of heart disease; stroke; certain types of cancer, gradual weakness of muscles, bones, and connective tissue; and decline of physical function in activities of daily living (59). Promoting moderate amounts of physical activity therefore can considerably improve the patient’s quality of life (42).
RECOMMENDATIONS
We believe that the physical activity recommendations for children and adolescents with scoliosis, in general, should be similar to those without scoliosis, that is, adolescents should obtain at least 60 minutes of physical activity daily (44). We suggest, though, that the client be approved medically for this level of participation, choice of physical activity and postoperative return time, as individuals without spinal fusion may have compromised pulmonary function or be experiencing back pain (41). Some authors have also reported no effect of the extent of spinal fusion or the number of fused vertebrae on choice of physical activity for individuals with spinal fusion. Although, some studies claim the distal fusion is a strong predictor of time needed to return to sports in individuals with scoliosis post spinal fusion (9, 18). After a spinal fusion, the intensity, volume and types of activities allowable likely will depend on the surgeon, especially during the first year (31, 48). Whether postoperative standard physical therapy is valuable prior to gradually returning to physical activity is not yet proven (36).
As there are no specific guidelines available for physical activity participation of individuals with scoliosis, particularly those with spinal fusion, recommendations are anecdotal and based on the author’s clinical experience, American College of Sports Medicine recommendations for physical activity for children and adolescents (44) and some research evidence of the effectiveness of activity programs for adolescents with scoliosis
The individuals with scoliosis have been reported to be able to participate in equally strenuous physical activities regardless of the spinal fusion. A comprehensive physical activity plan for individuals with scoliosis should incorporate three components: aerobic activity, muscle strengthening, and building bone mass. These components are not mutually exclusive and many physical activities incorporate all three components (44). Alongside the aforementioned components, the spinal fusion specific factor of increasing flexibility to compensate for loss of trunk range of motion should be incorporated. The majority of daily physical activity should be aerobic activity. Short-term aerobic training programs have shown to significantly improve aerobic capacity and decrease body fat composition in adolescents with scoliosis (4, 5). Aerobic activity should be at least moderate-intensity, with moderate – vigorous intensity being incorporated into the routine at least 3 days per week (43). Aerobic activity can also improve cardiovascular fitness when paired with mild resistance training (24). Some examples of aerobic activities are running, swimming, and bicycling.
Individuals with scoliosis should participate in muscle strengthening activities, either unstructured or structured, at least 2–3 days per week (43). These activities should be age and ability appropriate and individuals should target each major muscle group. It is advised to wait at least 48 hours before training the same muscle group again (43). Examples include exercises using free weights, body weight (e.g. push-ups, pull-ups etc.) and resistance bands (43).
Finally, children and adolescents should, at least 3 days per week, incorporate weight bearing activities and resistance training into their activities that can stimulate bone mineral density improvement (43). This is particularly crucial for pre-pubertal females, the group of individuals who develop severe AIS (8, 10, 29, 46). Mechanically, the amount of loading and speed that the load is applied to bone must be greater than those experienced daily and should include new loading strains even if it is through exercises performed for short durations (28) such as weight-bearing ‘power’ activities that utilize explosive movements like jumping/landing and jogging and running (51). Examples of bone strengthening activities include jumping rope, hopscotch, and running. These can be combined with aerobic activities such as playing tennis and stair maneuvering.
Certain sports specific training including balance and posture control, core strengthening and increasing flexibility have been reported as being useful in preparing individuals to return back to sports post spinal fusion.(12) Neuromotor exercises for functional training involving but not limited to balance, agility, coordination and gait training should be performed at least 2–3 days per week as well. (43) Furthermore, returning athletes can benefit from training/retraining for aerobic and/or anaerobic conditioning and proper movement techniques for activities like running, cycling, swimming, jumping and landing to decrease joint loading and increasing efficiency. For example, beneficial cardiorespiratory and anthropometric adaptations especially in girls with AIS and decrease in body fat among other benefits have been observed with cycling training 3 times per week for 6 week (5).
CAUTIONS AND CAVEATS
While there are clear benefits for individuals with AIS with/without spinal fusion, of engaging in physical activity, we don’t know the potential long-term negative consequences on the spine or fusion components. Patients and health care providers cannot rule out the long-term effects of physical activity post spinal fusion and should take precautionary measures to avoid abnormal stresses on the vertebrae, since there is still lack of concrete evidence.
There is also limited evidence that exercise as recommended for healthy individuals and mentioned above will produce the same benefits. For example, we don’t know whether bone mass of the spine will improve, both in the fused and non-fused parts of the vertebral column via the suggested ‘bone-strengthening’ activities. Furthermore, there is lack of concrete evidence suggesting a universal progression or potential adaptations/modifications to build up to this level of activity that will provide health benefits. Further research is warranted to understand vertebral and disc stresses both immediate and long-term after spinal fusion in physically active individuals.
CONCLUSION
Research has demonstrated children and adolescents who are active in their youth are healthier adults (44). We encourage individuals with adolescent idiopathic scoliosis who have had spinal fusion surgery to engage in age and skill level appropriate physical activities and/or supervised sports/other formal activities. Health care professionals need to remember that some movements will be limited by the rigidity of the fused spine and may need to be adapted. Understanding altered movement patterns and teaching exercises accordingly is especially important to avoid injury. It is also suggested that further research should be done to create evidence- based guidelines targeted specifically for this population that would be beneficial for the participants, clinicians, other human movement specialists.
REFERENCES
- 1.Altaf F, Gibson A, Dannawi Z, Noordeen H. Adolescent idiopathic scoliosis. Brit Med J. 2013;346(7906):30–34. doi: 10.1136/bmj.f2508. [DOI] [PubMed] [Google Scholar]
- 2.Andersen MO, Christensen SB, Thomsen K. Outcome at 10 Years After Treatment for Adolescent Idiopathic Scoliosis. Spine. 2006;31(3):350–354. doi: 10.1097/01.brs.0000197649.29712.de. [DOI] [PubMed] [Google Scholar]
- 3.Asher MA, Burton DC. Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis Spinal Disord. 2006;1:2–10. doi: 10.1186/1748-7161-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Athanasopoulos S, Paxinos T, Tsafantakis E, Zachariou K, Chatziconstantinou S. The effect of aerobic training in girls with idiopathic scoliosis. Scand J Med Sci Spor. 1999;9(1):36–40. doi: 10.1111/j.1600-0838.1999.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 5.Bas P, Romagnoli M, Gomez-Cabrera M, Bas JL, Aura JV, Franco N, Bas T. Beneficial effects of aerobic training in adolescent patients with moderate idiopathic scoliosis. Eur Spine J. 2011;20(Suppl 3):415–419. doi: 10.1007/s00586-011-1902-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernstein P, Hentschel S, Platzek I, Huhne S, Ettrich U, Hartmann A, Seifert J. Thoracal flat back is a risk factor for lumbar disc degeneration after scoliosis surgery. Spine J. 2014;14(6):925–932. doi: 10.1016/j.spinee.2013.07.426. [DOI] [PubMed] [Google Scholar]
- 7.Bustamante Valles KD, Long JT, Riedel SA, Graf A, Krzak J, Hassani S, Riordan M, Zaharski K, Sturm PF, Harris GF. Analysis of postural stability following posterior spinal fusion in adolescents with idiopathic scoliosis. ST Heal T. 2010;158:127–131. [PubMed] [Google Scholar]
- 8.Cheung CSK, Lee WTK, Tse YK, Lee KM, Guo X, Qin L, Cheng JCY. Generalized osteopenia in adolescent idiopathic scoliosis -- association with abnormal pubertal growth, bone turnover, and calcium intake? Spine. 2006;31(3):330–338. doi: 10.1097/01.brs.0000197410.92525.10. [DOI] [PubMed] [Google Scholar]
- 9.Christman T, Li Y. Pediatric Return to Sports After Spinal Surgery. Sports Health. 2016;8(4):331–335. doi: 10.1177/1941738116634685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Courtois I, Collet P, Mouilleseaux B, Alexandre C. Bone mineral density at the femur and lumbar spine in a population of young women treated for scoliosis in adolescence. Revue du rhumatisme (English ed) 1999;66(12):705–710. [PubMed] [Google Scholar]
- 11.Courvoisier A, Drevelle X, Dubousset J, Skalli W. Transverse plane 3D analysis of mild scoliosis. Eur Spine J. 2013;22(11):2427–2432. doi: 10.1007/s00586-013-2862-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cox SM, Dingle CR. Adolescent Idiopathic Scoliosis in a College Golfer. Int J Athl Ther Train. 2011;16(2):8–11. [Google Scholar]
- 13.Danielsson AJ, Wiklund I, Pehrsson K, Nachemson AL. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J. 2001;10(4):278–288. doi: 10.1007/s005860100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dayer R, Haumont T, Belaieff W, Lascombes P. Idiopathic scoliosis: etiological concepts and hypotheses. J Child Orthop. 2013;7(1):11–16. doi: 10.1007/s11832-012-0458-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dekel Y, Tenenbaum G, Kudar K. An exploratory study on the relationship between postural deformities and body-image and self-esteem in adolescents: the mediating role of physical activity. Int J Sport Psychol. 1996;27(2):183–196. [Google Scholar]
- 16.El-Hawary R, Chukwunyerenwa C. Update on Evaluation and Treatment of Scoliosis. Pediatr Clin N Am. 2014;61:1223–1241. doi: 10.1016/j.pcl.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Engsberg JR, Lenke LG, Uhrich ML, Ross SA, Bridwell KH. Prospective Comparison of Gait and Trunk Range of Motion in Adolescents With Idiopathic Thoracic Scoliosis Undergoing Anterior or Posterior Spinal Fusion. Spine. 2003;28(17):1993–2000. doi: 10.1097/01.BRS.0000087209.34602.42. [DOI] [PubMed] [Google Scholar]
- 18.Fabricant PD, Admoni S-H, Green DW, Ipp LS, Widmann RF. Return to athletic activity after posterior spinal fusion for adolescent idiopathic scoliosis: analysis of independent predictors. J Pediatr Orthop. 2012;32(3):259–265. doi: 10.1097/BPO.0b013e31824b285f. [DOI] [PubMed] [Google Scholar]
- 19.Good CR. Evolution in the Treatment of Spinal Deformity and Spinal Instrumentation. J Spin Res Found. 2010;5(1):19–25. [Google Scholar]
- 20.Gummerson NW, Millner PA. (ii) Scoliosis in children and teenagers. Orthop Trauma. 2011;25(6):403–412. [Google Scholar]
- 21.Hayes MA, Tompkins SF, Herndon WA, Gruel CR, Kopta JA, Howard TC. Clinical and radiological evaluation of lumbosacral motion below fusion levels in idiopathic scoliosis. Spine. 1988;13(10):1161–1167. doi: 10.1097/00007632-198810000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Hung VW-y, Qin L, Yeung H-y, Cheng JC-y. Status of bone quality in adolescent idiopathic scoliosis patients with low bone mass—using calcaneal quantitative ultrasound. Bone. 2008;43(S1):S85. [Google Scholar]
- 23.Ilharreborde B, Morel E, Mazda K, Dekutoski MB. Adjacent Segment Disease After Instrumented Fusion for Idiopathic Scoliosis Review of Current Trends and Controversies. J Spinal Disord Tech. 2009;22(7):530–539. doi: 10.1097/BSD.0b013e31818d64b7. [DOI] [PubMed] [Google Scholar]
- 24.Jwa Jun KIM, Gui Bin S, Eun Cho P. Effects of Swiss ball exercise and resistance exercise on respiratory function and trunk control ability in patients with scoliosis. J Phys Ther Sci. 2015;27(6):1775–1778. doi: 10.1589/jpts.27.1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kakar RS. Biomechanics displayed during the stop-jump movement by individuals with spinal fusion surgery for adolescent idiopathic scoliosis. [electronic resource] University of Georgia Lib; 2014. 2014. [Google Scholar]
- 26.Kakar RS, Li Y, Fu Y-C, Brown C, Simpson KJ. Spine Kinematics Exhibited During Running by Adolescent Idiopathic Scoliosis Patients with Spinal Fusion. Spine J. 2015;15(10):S177. [Google Scholar]
- 27.Konieczny MR, Senyurt H, Krauspe R. Epidemiology of adolescent idiopathic scoliosis. J Child Orthop. 2013;7(1):3–9. doi: 10.1007/s11832-012-0457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lanyon LE. Using Functional Loading to Influence Bone Mass and Architecture: Objectives, Mechanisms, and Relationship With Estrogen of the Mechanically Adaptive Process in Bone. Bone. 1996;18(1):S37–S43. doi: 10.1016/8756-3282(95)00378-9. [DOI] [PubMed] [Google Scholar]
- 29.Lee WTK, Cheung CSK, Tse YK, Chau WW, Qin L, Cheng JCY. Persistent osteopenia in adolescent idiopathic scoliosis (AIS) – Factors predisposing to generalized osteopenia, a cross-sectional and longitudinal investigation. Int Congr Ser. 2007;1297:25–31. [Google Scholar]
- 30.Lee WTK, Cheung CSK, Tse YK, Guo X, Qin L, Lam TP, Ng BKW, Cheng JCY. Association of osteopenia with curve severity in adolescent idiopathic scoliosis: a study of 919 girls. Osteoporos Int. 2005;16(12):1924–1932. doi: 10.1007/s00198-005-1964-7. [DOI] [PubMed] [Google Scholar]
- 31.Lehman RA, Jr, Kang DG, Lenke LG, Sucato DJ, Bevevino AJ Spinal Deformity Study Group. Return to sports after surgery to correct adolescent idiopathic scoliosis: a survey of the Spinal Deformity Study Group. Spine J. 2013;15(1):951–958. doi: 10.1016/j.spinee.2013.06.035. [DOI] [PubMed] [Google Scholar]
- 32.Lenssinck M-LB, Frijlink AC, Berger MY, Bierma-Zeinstra SMA, Verkerk K, Verhagen AP. Effect of Bracing and Other Conservative Interventions in the Treatment of Idiopathic Scoliosis in Adolescents: A Systematic Review of Clinical Trials. Phys Ther. 2005;85(12):1329–1339. [PubMed] [Google Scholar]
- 33.Li Y, Kakar RS, Fu Y-C, Oswald T, Brown C, Simpson KJ. Intra-Trunk Coordination Exhibited During Treadmill Running By Individuals With Spinal Fusion For Adolescent Idiopathic Scoliosis. Proceedings of the 25th Congr Int Soc Biomech; 2015; Glasgow, UK. [Google Scholar]
- 34.Li Y, Kakar RS, Fu Y-C, Oswald T, Simpson KJ. Pelvic and Lower Extremity Kinematic Analysis of Individuals with Spinal Fusion for Adolescent Idiopathic Scoliosis During Treadmill Running. Proceedings of the 7th World Congr Biomech; 2014; Boston, MA. [Google Scholar]
- 35.Lonstein JE. Scoliosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:248–259. doi: 10.1097/01.blo.0000198725.54891.73. [DOI] [PubMed] [Google Scholar]
- 36.Marti CL, Glassman SD, Knott PT, Carreon LY, Hresko MT. Scoliosis Research Society members attitudes towards physical therapy and physiotherapeutic scoliosis specific exercises for adolescent idiopathic scoliosis. Scoliosis (17487161) 2015;10(1):1–7. doi: 10.1186/s13013-015-0041-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martin CT, Pugely AJ, Gao YB, Mendoza-Lattes SA, Ilgenfritz RM, Callaghan JJ, Weinstein SL. Increasing Hospital Charges for Adolescent Idiopathic Scoliosis in the United States. Spine. 2014;39(20):1676–1682. doi: 10.1097/BRS.0000000000000501. [DOI] [PubMed] [Google Scholar]
- 38.Meyer C, Cammarata E, Haumont T, Deviterne D, Gauchard GC, Leheup B, Lascombes P, Perrin PP. Why do idiopathic scoliosis patients participate more in gymnastics? Scand J Med Sci Spor. 2006;16(4):231–236. doi: 10.1111/j.1600-0838.2005.00482.x. [DOI] [PubMed] [Google Scholar]
- 39.Meyer C, Haumont T, Gauchard GC, Leheup B, Lascombes P, Perrin PP. The practice of physical and sporting activity in teenagers with idiopathic scoliosis is related to the curve type. Scand J Med Sci Spor. 2008;18(6):751–755. doi: 10.1111/j.1600-0838.2007.00750.x. [DOI] [PubMed] [Google Scholar]
- 40.Nachemson A. A long term follow-up study of non-treated scoliosis. Acta Orthop Scand. 1968;39(4):466–476. doi: 10.3109/17453676808989664. [DOI] [PubMed] [Google Scholar]
- 41.Parsch D, Gärtner V, Brocai DRC, Carstens C, Schmitt H. Sports activity of patients with idiopathic scoliosis at long-term follow-up. Clin J Sport Med. 2002;12(2):95–98. doi: 10.1097/00042752-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18(2):189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 43.Pescatello LS, Arena R, Riebe D, Thompson PD. ACSM’s Guidelines for Exercise Testing and Prescription. Ninth Editon 9th edn ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 44.Physical Activity Guidelines Advisory Committee. Physical activity guidelines advisory committee report, 2008. Washington, DC: US Department of Health and Human Services; 2008. pp. A1–H14. [DOI] [PubMed] [Google Scholar]
- 45.Rajaee SS, Bae HW, Kanim LEA, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine. 2012;37(1):67–76. doi: 10.1097/BRS.0b013e31820cccfb. [DOI] [PubMed] [Google Scholar]
- 46.Rantalainen T, Weeks BK, Nogueira RC, Beck BR. Effects of bone-specific physical activity, gender and maturity on tibial cross-sectional bone material distribution: a cross-sectional pQCT comparison of children and young adults aged 5–29 years. Bone. 2015;72:101–108. doi: 10.1016/j.bone.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 47.Reamy BV, Slakey JB. Adolescent idiopathic scoliosis: review and current concepts. Am Fam Physician. 2001;64(1):111–116. [PubMed] [Google Scholar]
- 48.Rubery PT, Bradford DS. Athletic activity after spine surgery in children and adolescents: results of a survey. Spine. 2002;27(4):423–427. doi: 10.1097/00007632-200202150-00019. [DOI] [PubMed] [Google Scholar]
- 49.Sanders JO, Newton PO, Browne RH, Katz DE, Birch JG, Herring JA. Bracing for idiopathic scoliosis: how many patients require treatment to prevent one surgery? J Bone Joint Surg Am, American Volume. 2014;96(8):649–653. doi: 10.2106/JBJS.M.00290. [DOI] [PubMed] [Google Scholar]
- 50.Sarwahi V, Wollowick AL, Sugarman EP, Horn JJ, Gambassi M, Amaral TD. Minimally invasive scoliosis surgery: an innovative technique in patients with adolescent idiopathic scoliosis. Scoliosis. 2011;6:16. doi: 10.1186/1748-7161-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sayers A, Mattocks C, Deere K, Ness A, Riddoch C, Tobias JH. Habitual levels of vigorous, but not moderate or light, physical activity is positively related to cortical bone mass in adolescents. J Clin Endocrinol Metab. 2011;96(5):E793–E802. doi: 10.1210/jc.2010-2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schmitt H, Carstens C. Skoliose und Sport. / Scoliosis and sport. Dtsch Z Sportmed. 2004;55(6):163–164. [Google Scholar]
- 53.Shaughnessy WJ. Advances in Scoliosis Brace Treatment for Adolescent Idiopathic Scoliosis. Orthop Clin North Am. 2007;38(4):469–475. doi: 10.1016/j.ocl.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 54.Simpson KJ, Kakar RS, Fu Y-C, Li Y, Walker M, Brown C, Oswald T. How Do Individuals With Fused Spinal Segments For Adolescent Idiopathic Scoliosis (AIS) Compensate For The Loss Of Spinal Range Of Motion During Running?. Proceedings of the 21st Int Meet Adv Spine Tech 2014; Valencia, Spain. [Google Scholar]
- 55.Simpson KJ, Kakar RS, Fu Y-C, Walker M, Li Y, Brown C, Oswald T. Balance of Moderately-Active Individuals with Spinal Fusion for Adolescent Idiopathic Scoliosis is Mildly Compromised. Proceedings of the 27th Ann Conf Assoc Spine Surg India Scoliosis Res Soc; 2014; Kolkata, India. [Google Scholar]
- 56.Stehbens WE. Pathogenesis of idiopathic scoliosis revisited. Exp Mol Pathol. 2003;74(1):49–60. doi: 10.1016/s0014-4800(03)80008-4. [DOI] [PubMed] [Google Scholar]
- 57.Tanaka M, Nishi S, Ebara S, Matsumoto T, Naito H. Imbalanced bone growth and muscle forces affecting on spinal curve deformation of idiopathic scoliosis. J Biomech. 2006;39(S1):S103. [Google Scholar]
- 58.Tsutsui S, Pawelek J, Bastrom T, Lenke L, Lowe T, Betz R, Clements D, Newton PO. Dissecting the effects of spinal fusion and deformity magnitude on quality of life in patients with adolescent idiopathic scoliosis. Spine. 2009;34(18):E653–E658. doi: 10.1097/BRS.0b013e3181b2008f. [DOI] [PubMed] [Google Scholar]
- 59.US Department of Health and Human Services. Physical Activity Guidelines for Americans. 2008. [Google Scholar]
- 60.Wang T-Y, Pao J-L, Yang R-S, Jang J-SR, Hsu WL. The adaptive changes in muscle coordination following lumbar spinal fusion. Hum Mov Sci. 2015;40:284–297. doi: 10.1016/j.humov.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 61.Zhang J, He D, Gao J, Yu X, Sun H, Chen Z, Li M. Changes in life satisfaction and self-esteem in patients with adolescent idiopathic scoliosis with and without surgical intervention. Spine. 2011;36(9):741–745. doi: 10.1097/BRS.0b013e3181e0f034. [DOI] [PubMed] [Google Scholar]