Abstract
Background
The objectives of this study were to assess current variability in management preferences for blunt trauma patients with pericardial fluid, and to identify characteristics associated with operative intervention for patients with pericardial fluid on admission computed tomography (CT) scan.
Methods
This was a mixed-methods study of blunt trauma patients with pericardial fluid. The first portion was a research survey of members of the Eastern Association for the Surgery of Trauma conducted in 2016, in which surgeons were presented with four clinical scenarios of blunt trauma patients with pericardial fluid. The second portion of the study was a retrospective evaluation of all blunt trauma patients ≥14 years treated at our Level I trauma center between 1/1/2010 and 11/1/2015 with pericardial fluid on admission CT scan.
Results
For the survey portion of our study, 393 surgeons responded (27% response rate). There was significant variability in management preferences for scenarios depicting trace pericardial fluid on CT with concerning hemodynamics, and for scenarios depicting hemopericardium intraoperatively. For the separate retrospective portion of our study, we identified 75 blunt trauma patients with pericardial fluid on admission CT scan. Seven underwent operative management; six of these had hypotension and/or electrocardiogram changes. In multivariable analysis, pericardial fluid amount was a significant predictor of receiving pericardial window (relative risk for one category increase in pericardial fluid amount: 3.99, 95% CI 1.47-10.81) but not of mortality.
Conclusions
There is significant variability in management preferences for patients with pericardial fluid from blunt trauma, indicating a need for evidence-based research. Our institutional data suggest that patients with minimal to small amounts of pericardial fluid without concerning clinical findings may be observed. Patients with moderate to large amounts of pericardial fluid who are clinically stable with normal hemodynamics may also appear appropriate for observation, although confirmation in larger studies is needed. Patients with hemodynamic instability should undergo operative exploration.
Level of Evidence
Level IV, Therapeutic/Care Management
Keywords: Blunt trauma, Pericardial fluid, Hemopericardium, Pericardial effusion, Pericardial window
BACKGROUND
Patients with blunt trauma routinely undergo diagnostic Computed Tomography (CT) imaging during the initial trauma workup. Given technological advances that have increased the sensitivity of CT imaging, these scans may detect even subtle findings including small amounts of pericardial fluid and pericardial tears.1, 2 The finding of pericardial fluid is concerning for potential hemopericardium and life-threatening cardiac injury; however, not all findings are of clinical significance and affect patient outcome.
In the setting of trauma, where little past medical history may be known, the presence of pericardial fluid presents a broad differential diagnosis. Patients may have a chronic effusion, acute post-traumatic effusion or hemopericardium, and the hemopericardium may be either self-limited or represent life threatening cardiac injury.3-5 A scant amount of fluid may be physiologic or can radiographically mimic pericardial thickening or calcification. Case reports suggest that even apparently minor blunt chest trauma may produce significant post-traumatic effusion or delayed bleeding and later tamponade.6, 7 As a result, surgical drainage has been advocated for patients found to have pericardial fluid following blunt trauma.4, 8, 9 Still, studies of Focused Assessment with Sonography for Trauma (FAST) and CT have shown that pericardial fluid in trauma patients is not always clinically significant.5, 10, 11
For patients who are hemodynamically unstable or who sustained penetrating chest trauma, the identification of pericardial fluid mandates operative exploration. In a series of ten patients who presented with blunt cardiac rupture and concomitant shock and/or tamponade, expeditious operative intervention resulted in survival to hospital discharge in seven.12 In this series, all ten patients were found to have right atrial injuries; some also had additional inferior vena cava, superior vena cava or pericardial injuries. For patients with blunt trauma without frank hemodynamic compromise, however, there are no practice management guidelines to guide treatment decisions. This is particularly true for patients with essentially “incidental” findings of pericardial fluid. This is important because while pericardial window is the gold standard for definitive diagnosis, this procedure is not risk-free13, 14 and inherently requires significant use of hospital resources.
The objectives of this study were to assess how surgeons choose to manage these patients given the lack of data, and to identify characteristics associated with need for operative intervention and mortality among blunt trauma patients found to have pericardial fluid on diagnostic CT scan. We performed two separate but complementary studies to address these aims: the first portion of the study was a research survey of the Eastern Association for the Surgery of Trauma (EAST) to assess management preference of North American trauma surgeons. The second portion of the study was a retrospective evaluation of all blunt trauma patients with pericardial fluid on admission CT scan at our Level I trauma center to examine clinical and radiographic characteristics associated with outcomes. Based upon our survey results and institutional experience, we suggest a framework for clinical management of blunt chest trauma patients with pericardial fluid detected on CT scan.
METHODS
Research survey
A multiple choice survey was designed, which consisted of four brief clinical scenarios regarding blunt trauma patients found to have pericardial fluid. The complete text of the scenarios and answer choices are available as Supplemental Digital Content. In addition, we asked background questions regarding active practice of trauma surgery, fellowship training, board certification, number of years in practice, number of trauma patients seen annually at the surgeon’s primary institution, and trauma designation. Free-text comments about the survey or scenarios were also solicited. The survey was created and disseminated using secure, web-based REDCap electronic data capture tools hosted at the University of Washington.15 Surveys were disseminated via email to active and senior members of EAST in September 2016, which included licensed, board-certified surgeons either above or below the age of 50, active in trauma. The survey, and used of the EAST web mail system to solicit member participation, was approved by the EAST Research and Scholarship Section. This project was determined to be exempt from the University of Washington Institutional Review Board.
Results of the research survey were assessed using descriptive and bivariable analyses, and stratified based on surgeons’ self-reported years in practice. Years in practice was categorized as <5 years, 5 to 9 years, 10 to 19 years, and ≥20 years.
Retrospective study of patients with pericardial fluid on CT scan
This was a single-center retrospective study performed at Harborview Medical Center in Seattle, WA, and was approved by the University of Washington Institutional Review Board. Harborview Medical Center is the only Level I adult and pediatric trauma center in Washington State, and is a regional trauma referral center for Alaska, Montana and Idaho. We included patients 14 years of age or older with blunt trauma, who were treated between 1/1/2010 and 11/1/2015, and who were found to have pericardial fluid on initial CT scan. We were unable to assess point of care pericardial ultrasound such as FAST in our population as there was no means to retrospectively assess fluid amount quantitatively, and no standardized reporting system.
Potential patients were identified using a combined approach including the institutional trauma registry and the institutional radiology database. The institutional trauma registry contains all patients with trauma ICD-9 discharge codes who met one or more of the following: admission to our institution, activation of the Trauma Resuscitation Team, transfer to or from our institution via EMS, airlift to our institution, death in our institution including the emergency department (ED), or death on arrival. This registry was broadly queried by ICD-9 and AIS 2005 codes for relevant cardiac, pericardial, thoracic and great vessel injuries (ICD-9 codes 861-861.13, 901.0, 901.2, 901.4-901.42; AIS 2005 codes 413000.6, 420099.9-421009.6, 421299.3-421207.6, 421899.3-421808.5, 441099.1-441200.5, 441699.2-441606.5), as well as for ICD-9 procedure codes for operations on the heart, pericardium, exploratory thoracotomy, incision of mediastinum, and other thoracic operations; 35-37.9, 34.0, 34.1, 34.9, respectively). In addition, radiology records were queried for chest, abdominal, and pan-CT scans performed in Emergency Radiology. Potential patients were identified based on the absence of institutionally-standardized structured reporting indicating a normal exam (absence of terms such as “pericardial fluid: absent” or “no pericardial fluid”). Medical record numbers were narrowed to those patients involved in blunt trauma by comparison to the institutional trauma registry. Radiology reports were screened for language indicating pericardial fluid or pericardial abnormality. If the report had any question of pericardial abnormality, images were obtained for further evaluation by the study attending emergency radiologist (KFL).
The query results were combined, yielding 109 potential patients. For each, detailed clinical data was obtained via chart review, and CT scans were reviewed in detail by the study attending radiologist (KFL) blinded to clinical data. CT scan data collected included time, contrast use, concomitant upper abdominal and thoracic injuries, maximum radial dimension of pericardial fluid, categorized pericardial fluid amount, density of pericardial fluid in Houndsfield units, CT signs associated with tamponade (defined as the presence of inferior vena cava distention, renal vein distention and periportal edema), cardiac rupture, pericardial rupture, pneumopericardium, right ventricle: left ventricle ratio and inferior vena cava flattening. Given no pre-existing categorization schemes for amount of CT-detected pericardial fluid, we created the following categories: minimal <5mm but noncircumferential, small <5mm and circumferential, moderate ≥5mm to <10 mm and circumferential, large ≥10 mm and circumferential. Additional demographic, injury, and hospitalization information was obtained from the trauma registry. Dichotomous variables demarking age ≥65 years and Hounsfield units ≥35 were created. Hypotension was defined as systolic blood pressure less than 90 mmHg.
Of the 109 manually-screened patients undergoing detailed review, 75 were included in the final study population. Patients felt to have “questionable” fluid on CT scan were included in the study, given that such patients may be the source of diagnostic dilemmas for providers caring for patients in the trauma bay. Excluded patients were determined not to have CT evidence of pericardial fluid. Among the excluded patients were two who underwent pericardial window then sternotomy without undergoing CT scan (both had right ventricular lacerations; one survived to hospital discharge and one died during intraoperative resuscitation), and seven who underwent resuscitative thoracotomy for loss of vital signs and were found to have pericardial fluid intraoperatively (one patient receiving resuscitative thoracotomy survived to hospital discharge after repair of an apical cardiac laceration).
Descriptive statistics were performed to assess demographics and injury characteristics in patients who required operative intervention and in those managed nonoperatively. Detailed tables of radiographic findings for patients who underwent CT scan, and intraoperative findings and decision making for patients managed operatively, were created given the complex clinical decision making inherent to this population. Multivariable analysis was conducted using Poisson regression with robust confidence intervals, and Akaike’s information criterion was applied to determine the appropriate number of predictive variables to avoid overfitting. The final multivariable model to predict need for operation included categorized pericardial fluid amount, dichotomized age (≥65 or <65), and lowest systolic blood pressure in the ED. Statistical analysis was performed using Stata version 14 (StataCorp LP, College Station, TX). Model performance was assessed via Pearson chi square goodness of fit tests. Management recommendations were developed through review of the data by each of the surgeons on the project; consensus was achieved regarding language of the final set.
RESULTS
Research survey
The survey was disseminated to 1454 active and senior members of EAST; there were 383 complete responses and 10 partial responses, for a response rate of 27.0%. Of survey participants, 98% reported actively practicing trauma surgery; 72% reported practicing at a Level I trauma center and 21% at a Level II trauma center; 71% completed a dedicated trauma surgery fellowship, and 91% were board certified in surgical critical care. Seventeen percent had been in practice less than 5 years, 23% had been in practice 5-9 years, 34% had been in practice 10-19 years, and 27% had been in practice at least 20 years.
Surgeons’ responses to the survey are shown in Table 1. The first scenario depicted a hemodynamically normal polytrauma patient with trace pericardial fluid; 94.4% of surgeons responded that they would admit the patient to the ICU for resuscitation. Response distributions were similar across categories of surgeon experience (p=0.34). The second scenario depicted a similar patient but with a blood pressure of 92/70 mmHg and heart rate of 105 beats per minute; in this scenario, 72.8% of surgeons responded that they would admit to ICU for resuscitation and 24.9% would proceed to the operating room for pericardial window. We observed a trend toward surgeons with fewer years of experience preferring operative intervention to ICU admission for this scenario (p=0.08).
Table 1.
Responses to survey by members of the Eastern Association for the Surgery of Trauma
| All | Years in practice | |||||
|---|---|---|---|---|---|---|
| <5 | 5-9 | 10-19 | ≥20 | P value | ||
|
Scenario 1: Polytrauma patient; Computed tomography scan
and echocardiogram show trace pericardial fluid; blood pressure 140/90mmHg, heart rate 96 bpm |
||||||
| Admit ICU with resuscitation and observe | 94.4% | 93.8% | 96.6% | 93.9% | 95.2% | 0.34 |
| To OR for pericardial window | 4.8% | 4.7% | 2.3% | 6.1% | 4.8% | |
| To OR for sternotomy | 0.5% | 0.0% | 1.2% | 0.0% | 0.0% | |
| To cardiac cath for pericardial drain | 0.3% | 1.6% | 0.0% | 0.0% | 0.0% | |
|
Scenario 2: Polytrauma patient; Computed tomography scan
and echocardiogram show trace pericardial fluid; blood pressure 92/70mmHg, heart rate 105 bpm |
||||||
| Admit ICU with resuscitation and observe | 72.8% | 67.2% | 75.9% | 69.5% | 78.9% | 0.08 |
| To OR for pericardial window | 24.9% | 31.3% | 24.1% | 25.2% | 21.2% | |
| To OR for sternotomy | 1.0% | 1.6% | 0.0% | 3.8% | 0.0% | |
| To cardiac cath for pericardial drain | 1.3% | 0.0% | 0.0% | 1.5% | 0.0% | |
|
Scenario 3: Polytrauma patient with 80 mL blood on pericardial
window without active bleeding; blood pressure 140/90mmHg, heart rate 96 bpm |
||||||
| Place a drain in the pericardium and admit patient for observation | 53.9% | 53.1% | 58.6% | 44.3% | 62.5% | 0.12 |
| Proceed to sternotomy and open heart exam | 42.0% | 43.8% | 35.6% | 51.2% | 34.6% | |
| Close the pericardial window without drain and observe patient | 4.1% | 3.1% | 5.8% | 4.6% | 2.9% | |
|
Scenario 4: Polytrauma patient with 80 mL blood on pericardial
window without active bleeding; blood pressure 92/70mmHg, heart rate 105 bpm |
||||||
| Place a drain in the pericardium and admit patient for observation | 41.1% | 34.4% | 46.0% | 31.1% | 53.9% | 0.03 |
| Proceed to sternotomy and open heart exam | 55.8% | 62.5% | 50.6% | 64.9% | 43.3% | |
| Close the pericardial window without drain and observe patient | 3.1% | 3.1% | 3.5% | 3.1% | 2.9% | |
The third and fourth scenarios asked about intraoperative decision making for patients found to have 80 mL of pericardial blood upon pericardial window without active or ongoing bleeding. In the third scenario the patient had normal hemodynamics; 53.9% of surgeons preferred pericardial drain placement while 42% preferred sternotomy. There was not a significant association between years in practice and response (p=0.12). In the fourth scenario the patient had a blood pressure of 92/70 mmHg and heart rate of 105 beats per minute; 41.1% preferred pericardial drain placement while 55.6% preferred sternotomy. Again, surgeons with fewer years of experience preferred sternotomy to less aggressive options (p=0.03).
Some surgeons provided additional comments for context. Many commented that hemodynamics and response to resuscitation were of greater importance than CT findings, or as one surgeon stated, “If it ain’t broke, don’t fix it. Perfect is the sworn enemy of good enough.” However, some felt strongly that patients with fluid on CT should undergo pericardial window for more accurate diagnosis: “Fluid equals blood, blood equals injury, injury requires repair. In any other circumstance, I believe you may be able to ‘watch’ blood in a closed space but, in the case of a tight, non-pliable sac, such as the pericardium, the risk is too high to allow pride to get in the way of the diagnostic test of certainty.” Regarding the operative scenarios, there was wide variability in responses; some noted that any finding of blood would prompt cardiac exploration while others felt that it was safe to avoid sternotomy in the absence of active and ongoing bleeding. In addition, we received comments on the need for management algorithms based on blood quantities and the potential for a multi-center trial to prospectively assess management decisions and outcomes among patients found to have pericardial fluid.
Retrospective study of patients with pericardial fluid on CT scan
Seventy-five patients who had CT evidence of pericardial fluid following blunt trauma were included in the final study population. Demographic and injury characteristics are shown in Table 2 for patients receiving operative intervention (n=7) and patients managed nonoperatively (n=68). Mean age was similar, patients were predominantly male, and mean Injury Severity Score (ISS) was 18.8 in the nonoperative group and 33 in the operative group. For context, the total number of patients aged ≥14 years with blunt trauma at our institution over the same timeframe was 23,948. Seven patients in nearly 6 years received pericardial operations, corresponding to just over one per year on average.
Table 2.
Demographic and injury characteristics of blunt trauma patients with pericardial fluid, Harborview Medical Center 2010-2015
| Patients who did not receive operative intervention (n=68) |
Patients receiving operative intervention (n=7) |
P value | |
|---|---|---|---|
| Mean age (SD) | 58.0 (22.0) | 53.7 (24.6) | 0.63 |
| Male sex | 60.3% | 57.1% | 0.87 |
| Cause of injury | 0.75 | ||
| Traffic related | 69.1% | 57.1% | |
| Fall | 23.5% | 28.6% | |
| Other | 7.4% | 14.3% | |
| Admitted to ICU | 80.9% | 100% | 0.20 |
| Intubated during hospital stay | 39.7% | 57.1% | 0.37 |
| Rapid response in hospital | 14.7% | 0.0% | 0.28 |
| Unplanned ICU readmission | 5.9% | 0.0% | 0.51 |
| Blood transfusion within 4 hours of arrival | 8.8% | 14.3% | 0.64 |
| Blood transfusion during hospital stay | 25.0% | 42.9% | 0.31 |
| ED systolic blood pressure <90mmHg | 31.3% | 71.4% | 0.04 |
| Ever required vasopressors | 13.4% | 14.4% | 0.95 |
| Echocardiogram performed (at least one) | 37.3% | 71.4% | 0.08 |
| Troponin obtained (at least one) | 61.2% | 85.7% | 0.20 |
| Troponin abnormal (at least one troponin >0.05 ng/ml; denominator is patients who had at least one troponin drawn) |
17/41 (41.5%) | 6/6 (100%) | 0.01 |
| Mean ISS (SD) | 18.8 (15.2) | 33.3 (9.8) | 0.02 |
| In-hospital death | 10.3% | 0.0% | 0.37 |
Radiographic characteristics of the population are shown in Table 3. The operative group had significantly higher mean maximal radial dimension of pericardial fluid and were more likely to have CT signs of cardiac tamponade as based on venous distention and periportal edema. There were trends toward operative patients having higher frequency of IVC flattening on CT scan, and toward having concomitant findings such as mediastinal hematoma, sternal fracture, rib fractures, pulmonary injuries and upper abdominal injuries.
Table 3.
Radiographic characteristics of blunt trauma patients with pericardial fluid
| Patients who did not receive operative intervention (n=68) |
Patients receiving operative intervention (n=7) |
P value | |
|---|---|---|---|
| Pericardium-related radiographic findings | |||
| Mean Hounsfield units of pericardial fluid (SD) | 30.9 (78.2) | 36.1 (12.5) | 0.86 |
| Mean maximum radial dimension of pericardial fluid (SD) |
5.7 mm (5.3 mm) | 10.3 mm (6.2 mm) | 0.04 |
| CT evidence of cardiac tamponade | 2.9% | 42.9% | <0.001 |
| Pneumopericardium | 1.5% | 14.3% | 0.13 |
| Mean RV to LV ratio (SD) | 0.94 (0.15) | 0.95 (0.10) | 0.80 |
| CT signs of IVC flattening | 4.4% | 14.3% | 0.27 |
|
| |||
| Concomitant radiographic findings | |||
| Mediastinal hematoma | 38.2% | 57.1% | 0.33 |
| Sternal fracture | 19.4% | 28.6% | 0.57 |
| Anterior rib fractures | 31.8% | 57.1% | 0.18 |
| Any rib fractures | 45.6% | 57.1% | 0.56 |
| Thoracic spine fracture | 16.2% | 28.6% | 0.41 |
| Pulmonary contusions | 27.9% | 42.9% | 0.41 |
| Pulmonary lacerations | 7.5% | 28.6% | 0.07 |
| Hemothorax | 20.6% | 14.3% | 0.69 |
| Thoracic aortic injury | 16.2% | 0.0% | 0.25 |
| Upper abdominal injury | 17.7% | 42.9% | 0.12 |
All patients who underwent CT scan were stratified by estimated amount of pericardial fluid. Their outcomes are shown in Table 4, including operative procedures and deaths. As the descriptions indicate, all but one patients receiving operative intervention had development of hypotension and/or electrocardiogram abnormalities in addition to their radiographic abnormalities. Only one patient required reoperation, which was performed for re-accumulation of fluid and hypotension; all operative patients survived to hospital discharge. There were two patients who had improvement in hemodynamics upon pericardiotomy, but no patient was found to have a cardiac injury requiring repair. Notably, all operations described were performed early (i.e. patient proceeded directly from ED to operating room, or from ED to angiography to operating room) except for the thoracotomy in the “small” pericardial fluid category, which was electively performed on hospital day 2 with the intent to repair the visualized pericardial laceration. Of patients in the nonoperative category, there were none who had later decompensation resulting in death or operation. Evaluation of causes of death for those patients with CT scans shows that six of seven died from multisystem organ failure or other injuries; one patient died after having pulseless electrical activity in the setting of known blunt aortic injury and pelvic extravasation.
Table 4.
Patient outcomes and surgical management according to computed tomography scan estimates of pericardial fluid amount
| Pericardial fluid category |
N (total 75 patients) |
Operative procedures performed | In-hospital mortality |
|---|---|---|---|
| Minimal | 32 | 1 /32 (3%)
|
2 /32 (6%)
|
| Small | 20 | 2 /20 (10%)
|
2 /20 (10%)
|
| Moderate | 8 | 1 /8 (13%)
|
2 /8 (25%)
|
| Large | 5 | 3 /5 (60%)
|
0 /5 (0%) |
| Questionable pericardial fluid |
9 | 0 /9 (0%) | 1 /9 (11%)
|
Footnote:
Pericardial fluid categories were defined as: minimal <5mm but noncircumferential, small <5mm and circumferential, moderate ≥5mm to <10 mm and circumferential, large ≥10 mm and circumferential.
Two distinct measurements of pericardial fluid were performed on radiology review: the maximum radial dimension of pericardial fluid in millimeters, and categorized fluid amount. These were each tested in a Poisson regression models, as well as a categorized version of the maximum radial dimension measure in 5mm increments. Of the three, categorized fluid amount was most predictive of decision to proceed to pericardial window in both bivariable and multivariable models, so was used for the remaining analyses. On bivariable analysis, the relative risk associated with a one category increase in amount of pericardial fluid was 4.62 (95% CI 2.09, 10.22).
Multivariable analysis was conducted to predict likelihood of receiving pericardial window following CT scan at our institution, with or without subsequent sternotomy. The final model included categorized pericardial fluid amount, dichotomized age (≥65 or <65), and the patient’s lowest systolic blood pressure in the ED. In this model, a one category increase in categorized pericardial fluid amount increased the risk of pericardial window 3.99 fold (95% CI 1.47, 10.81) as shown in Table 5. The Pearson goodness-of-fit chi square statistic was 34.9, p = 0.9998, indicating good model performance. The model with the outcome of any operative procedure similarly showed pericardial fluid category to be a significant predictor (p=0.04).
Table 5.
Adjusted relative risk of pericardial window and mortality as a function of estimated amount of pericardial fluid
| Outcome | Adjusted relative riska associated with one category increase in estimated amount of pericardial fluid |
95% confidence interval |
|---|---|---|
| Pericardial window operation | 3.99 | 1.47, 10.81 |
| In-hospital mortality | 0.90 | 0.41, 1.94 |
Footnote:
relative risks were adjusted for categorized pericardial fluid amount (minimal <5mm but noncircumferential, small <5mm and circumferential, moderate ≥5mm to <10 mm and circumferential, large ≥10 mm and circumferential), dichotomized age (≥65 or <65), and the patient’s lowest systolic blood pressure in the ED.
In addition, the regression model was applied to the outcome of in hospital death as shown in Table 5; pericardial fluid amount was not significantly predictive of mortality (relative risk 0.90, 95% CI 0.41, 1.94), while lowest systolic blood pressure in the ED was predictive (relative risk associated with 10mmHg decrease in lowest systolic blood pressure was 1.90, 95% CI 1.33, 2.71).
DISCUSSION
There is currently no published or widely-accepted standard of care for management of CT-detected pericardial fluid in patients with blunt trauma. Pericardial window remains the gold standard for diagnosis of clinically-significant hemopericardium; however, this may lead to complications and may be low yield in a sizeable proportion of patients.5, 10, 11 Still, the increased frequency of thoracic CT imaging1, 2 in hemodynamically stable patients with blunt trauma in the modern era gives rise to the middle-of-the-night dilemma of whether or not to operate when imaging shows definite or even questionable pericardial fluid. In response to this information gap, we conducted a survey of trauma surgeons to assess current practice preferences, and reviewed our 6-year institutional experience with management of pericardial fluid in blunt trauma patients presenting to our Level 1 trauma center.
Our survey results showed substantial variability in management of patients found to have pericardial fluid among participating surgeons. While most surgeons felt that a hemodynamically stable patient found to have trace pericardial fluid on CT scan could be safely observed in the ICU for initial management, responses for a similarly-injured patient with mild tachycardia and lower blood pressure were much more variable and management preferences for patients found to have pericardial blood without active bleeding intraoperatively varied widely. Experience in practice significantly influenced some management decisions, wherein more experienced surgeons tended to be less aggressive operatively. The observed variability in this survey highlights the need for further research and production of evidence-based practice management guidelines, which was also independently mentioned by several of the surveyed surgeons.
In an attempt to address the question of which patients with pericardial fluid on CT scan require operative intervention, we reviewed our institutional experience over 6 years. The amount of pericardial fluid seen on CT scan was predictive of decision to proceed to operative intervention at our institution (each category increase was associated with a four-fold increase in likelihood of operation). However, review of the clinical courses of these 75 patients indicates that of patients managed operatively, none had a cardiac injury requiring repair. This suggests that drainage alone may be an adequate intervention among patients stable enough to receive CT scan, who develop hemodynamic or electrocardiogram (ECG) changes. Furthermore, of patients with CT-detected fluid of any amount who were managed nonoperatively, none required subsequent operation and none died because of this injury. Thus, our data suggest that patients found to have incidental, CT-detected pericardial fluid without hemodynamic compromise or ECG changes do not need surgical intervention; those who do develop hemodynamic compromise or ECG changes can likely be treated with drainage alone. As we have a limited sample size, particularly for patients with larger amounts of fluid, we do strongly advocate for admission of all such patients to monitor for possible decompensation and need for drainage. This study, while preliminary, serves as a starting point for larger-scale examination of optimal decision making and treatments for patients with blunt trauma.
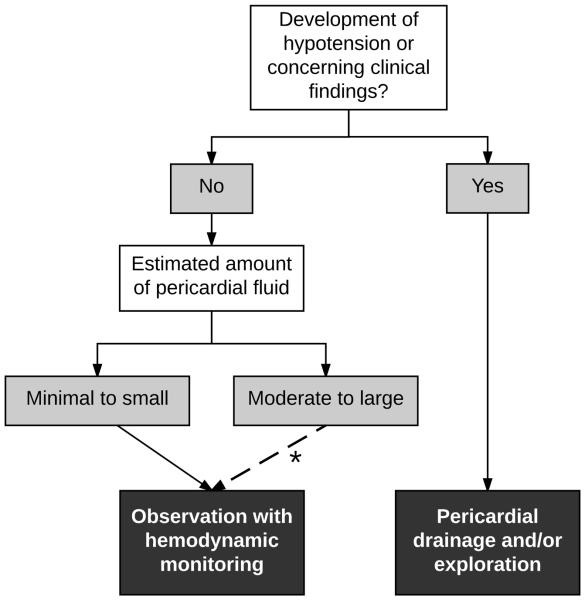
Based upon our results, we recommend a suggested framework for clinical management of blunt chest trauma patients with pericardial fluid on CT scan, which is shown in Figure 1. For patients with normal hemodynamics and without ECG changes, found to have minimal to small amounts of pericardial fluid, our data suggests that observation is appropriate; this is consistent with our survey results showing that 95% would observe a hemodynamically normal patient with trace pericardial fluid on CT scan. When a moderate to large amount of fluid is present, our data suggests that those with normal hemodynamics may also be observed. However, given our small sample size and potential consequences of cardiac injury, further study is needed to confirm this. In the setting of abnormal hemodynamics or concerning clinical findings such as new ECG changes, regardless of the amount of fluid, operative drainage and/or exploration remains the gold standard.
Figure 1. Suggested framework for clinical management of blunt chest trauma patients with pericardial fluid on computed tomography scan.
* The institutional data presented suggest that hemodynamically normal patients with moderate to large amounts of fluid may be observed; however, given small sample sizes, this recommendation must be confirmed in larger studies.
Currently, there is debate and absence of high quality data to determine whether a pericardial drain should be left after pericardial window. Our sample size is insufficient to make firm recommendations regarding pericardial drain placement. Two of the four patients in our study who had pericardial window without subsequent sternotomy had pericardial drains placed; one patient who did not receive a drain required reoperation due to accumulation of fluid.
We acknowledge several limitations to this mixed-methods paper. Our survey was voluntary; as such we received at complete or partial responses from 27% of the EAST members. While the response rate is very typical of physician surveys16-19 and 90% of those who opened the survey completed it, we recognize that a minority of the surgeons to whom the survey was emailed responded. Respondents may differ from those who did not respond; for instance, surgeons with more frequent exposure to patients with pericardial fluid might have greater interest in the topic and be more likely to respond. Since our data suggests that more experienced surgeons sometimes had different management preferences from less experienced surgeons (wherein experienced surgeons favored less aggressive interventions), our results may be skewed toward their preferences. By sampling members of EAST, our goal was to gather the opinions of experts in the field. Still, many trauma patients are evaluated by providers who do not specialize in trauma, who may make decisions for these patients based on varying levels of experience and training. We hypothesize that our sampling frame attenuated variability in response from what we would have seen if sampling providers more broadly. Similarly, we note that the majority of respondents practiced at Level I and II trauma centers. As a result, their responses may not generalize to what may be safe or feasible at centers lacking comparable resources.
There were also several limitations to institutional evaluation of patients with pericardial fluid on CT scan. This was retrospective, with a limited sample size, and some of the clinical subtleties guiding real-time operative decision making were not available in the medical record. It was difficult to choose an ideal primary outcome for this nonrandomized and retrospective study. All-cause mortality was not ideal given a polytrauma population wherein deaths were unrelated to cardiac injury or tamponade, and attributed mortality is also not ideal given that operative intervention should prevent death. While the selected primary outcome, operative intervention, was surgeon-driven, we felt that it was the best available outcome measure. We note that no patients died because of tamponade or cardiac injury in the group managed nonoperatively. Considering only patients undergoing a therapeutic operation (e.g. pericardial window prompting sternotomy with repair of cardiac injury) was felt to be clinically and statistically impractical as an outcome for this study. As such, we provided details on operative findings for all patients.
Evaluation of the pericardium using FAST is also an important diagnostic tool in workup of blunt trauma patients. In hemodynamically unstable patients, FAST-detected pericardial fluid typically prompts operative intervention. Still, small studies have shown that pericardial fluid detected on FAST exam in hemodynamically stable patients may not be pathologic.5, 11 FAST exam was not assessed in detail in our population given inability to retrospectively assess fluid amount quantitatively, and lack of a standardized reporting system.
In summary, we studied North American practice management preferences for patients found to have pericardial fluid on CT scan or in the operating room, and observed substantial variability. In addition, we evaluated all patients found to have pericardial fluid on CT scan at a Level I trauma center over 6 years. Among those receiving CT scans the measured amount of pericardial fluid was highly predictive of receiving pericardial window at our institution. Still, no patient managed nonoperatively decompensated to require operation or died from tamponade or cardiac injury, regardless of the amount of fluid present. Based on our data, we have developed a simple suggested framework to guide clinical decision making. However, given the rarity of pericardial fluid in blunt trauma patients and especially of cardiac injury or tamponade, we strongly advocate for further study across multiple institutions.
Supplementary Material
Acknowledgments
Disclosure of funding
Funding support for this research was from the National Institute of Health, Institute of Child Health and Human Development (2T32HD057822-06); Drs. Frederick Rivara, Monica Vavilala).
Footnotes
Conflicts of interest:
The authors report no conflicts of interest.
Meetings at which paper was presented: This research has not previously been presented or submitted for presentation.
AUTHOR CONTRIBUTIONS
Dr. Witt contributed to literature search, study design, data collection, data analysis, data interpretation, writing and critical revision. Dr. Linnau contributed to study design, data collection, data analysis, data interpretation and critical revision. Dr. Rivara contributed to study design, data analysis, data interpretation and critical revision. Dr. Vavilala contributed to study design, data analysis, data interpretation and critical revision. Dr. Bulger contributed to data interpretation and critical revision. Dr. Maier contributed to data interpretation and critical revision. Dr. Arbabi contributed to study design, data interpretation and critical revision.
REFERENCES
- 1.Plurad D, Green D, Demetriades D, Rhee P. The increasing use of chest computed tomography for trauma: is it being overutilized? J Trauma. 2007;62(3):631–5. doi: 10.1097/TA.0b013e31802bf009. [DOI] [PubMed] [Google Scholar]
- 2.Clancy K, Velopulos C, Bilaniuk JW, Collier B, Crowley W, Kurek S, Lui F, Nayduch D, Sangosanya A, Tucker B, et al. Screening for blunt cardiac injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma. 2012;73(5 Suppl 4):S301–6. doi: 10.1097/TA.0b013e318270193a. [DOI] [PubMed] [Google Scholar]
- 3.Brathwaite CE, Rodriguez A, Turney SZ, Dunham CM, Cowley R. Blunt traumatic cardiac rupture. A 5-year experience. Ann Surg. 1990;212(6):701–4. doi: 10.1097/00000658-199012000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fulda G, Brathwaite CE, Rodriguez A, Turney SZ, Dunham CM, Cowley RA. Blunt traumatic rupture of the heart and pericardium: a ten-year experience (1979-1989) J Trauma. 1991;31(2):167–72. discussion 72-3. [PubMed] [Google Scholar]
- 5.Press GM, Miller S. Utility of the cardiac component of FAST in blunt trauma. J Emerg Med. 2013;44(1):9–16. doi: 10.1016/j.jemermed.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 6.Solomon D. Delayed cardiac tamponade after blunt chest trauma: case report. J Trauma. 1991;31(9):1322–4. doi: 10.1097/00005373-199109000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Hermens JA, Wajon EM, Grandjean JG, Haalebos MM, von Birgelen C. Delayed cardiac tamponade in a patient with previous minor blunt chest trauma. Int J Cardiol. 2009;131(3):e124–6. doi: 10.1016/j.ijcard.2007.07.080. [DOI] [PubMed] [Google Scholar]
- 8.Asensio JA, Garcia-Nunez LM, Petrone P. Trauma to the Heart. 2008 7/12/2016. 6. McGraw-Hill; New York, NY: TRAUMA [Internet] Available from: http://www.r2library.com/Resource/Title/0071469125. [Google Scholar]
- 9.Huang YK, Lu MS, Liu KS, Liu EH, Chu JJ, Tsai FC, Lin PJ. Traumatic pericardial effusion: impact of diagnostic and surgical approaches. Resuscitation. 2010;81(12):1682–6. doi: 10.1016/j.resuscitation.2010.06.026. [DOI] [PubMed] [Google Scholar]
- 10.Kaiser ML, Whealon MD, Barrios C, Jr., Dobson SC, Malinoski DJ, Dolich MO, Lekawa ME, Hoyt DB, Cinat ME. Risk factors for traumatic injury findings on thoracic computed tomography among patients with blunt trauma having a normal chest radiograph. Arch Surg. 2011;146(4):459–63. doi: 10.1001/archsurg.2011.56. [DOI] [PubMed] [Google Scholar]
- 11.Lukan JK, Franklin GA, Spain DA, Carrillo EH. "Incidental" pericardial effusion during surgeon-performed ultrasonography in patients with blunt torso trauma. J Trauma. 2001;50(4):743–5. doi: 10.1097/00005373-200104000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Calhoon JH, Hoffmann TH, Trinkle JK, Harman PK, Grover FL. Management of blunt rupture of the heart. J Trauma. 1986;26(6):495–502. doi: 10.1097/00005373-198606000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Hommes M, Nicol AJ, van der Stok J, Kodde I, Navsaria PH. Subxiphoid pericardial window to exclude occult cardiac injury after penetrating thoracoabdominal trauma. Br J Surg. 2013;100(11):1454–8. doi: 10.1002/bjs.9241. [DOI] [PubMed] [Google Scholar]
- 14.Miller FB, Bond SJ, Shumate CR, Polk HC, Jr., Richardson JD. Diagnostic pericardial window. A safe alternative to exploratory thoracotomy for suspected heart injuries. Arch Surg. 1987;122(5):605–9. doi: 10.1001/archsurg.1987.01400170111016. [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma GK, Sofferman RA, Armstrong WB. Evaluation of the American college of surgeons thyroid and parathyroid ultrasound course: Results of a web-based survey. Laryngoscope. 2016 doi: 10.1002/lary.26335. [DOI] [PubMed] [Google Scholar]
- 17.Obremskey W, Molina C, Collinge C, Nana A, Tornetta P, 3rd, Sagi C, Schmidt A, Probe R, Ahn J, Browner BD. Current Practice in the Management of Open Fractures Among Orthopaedic Trauma Surgeons. Part A: Initial Management. A Survey of Orthopaedic Trauma Surgeons. J Orthop Trauma. 2014;28(8):e198–202. doi: 10.1097/BOT.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 18.Rajasekhar A, Elmariah H, Lottenberg L, Beyth R, Lottenberg R, Ang D. Inferior vena cava filters in trauma patients: a national practice patterns survey of U.S. Trauma centers. Am Surg. 2014;80(12):1237–44. [PubMed] [Google Scholar]
- 19.Haut ER, Schneider EB, Patel A, Streiff MB, Haider AH, Stevens KA, Chang DC, Neal ML, Hoeft C, Nathens AB, et al. Duplex ultrasound screening for deep vein thrombosis in asymptomatic trauma patients: a survey of individual trauma surgeon opinions and current trauma center practices. J Trauma. 2011;70(1):27–33. doi: 10.1097/TA.0b013e3182077d55. discussion -4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.